Abstract
Background
Pregnancy induces dramatic cardiovascular changes in order to meet the increasing metabolic needs. Adaptive change of left ventricle (LV) might be modified in pregnancy complicated by hypertension.
Methods
Data from 193 consecutive pregnant women were analyzed. Clinical and echocardiographic data were compared in normotensive and hypertensive women.
Results
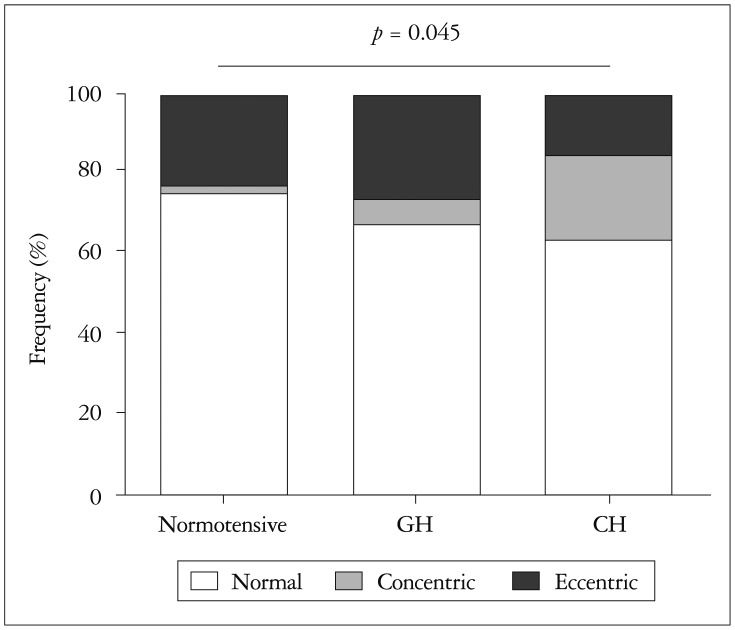
Significantly higher LV mass indexed by height was observed in hypertensive women compared with normotensive women (84 ± 21 g/m vs. 97 ± 20 g/m, p = 0.001). Diastolic function measured by the ratio of peak velocity of early diastolic transmitral blood flow to early diastolic mitral annular velocity was impaired in hypertensive women (11.0 ± 3.0 vs. 9.2 ± 2.5, p < 0.001). Such change was more prominent in women with gestational hypertension (GH) than those with chronic hypertension (CH). Heavy maternal weight was an independent factor associated with LV hypertrophy (LVH) in both normotensive and hypertensive women. Overt eccentric LVH was more frequent than concentric remodeling/hypertrophy (24% vs. 8.4%) in GH, while the opposite result was observed in CH (14% vs. 23%).
Conclusion
Hypertensive pregnancy is associated with significant LVH and diastolic dysfunction. CH seems to induce different LV remodeling pattern from GH. Heavy maternal weight during pregnancy might intensify the unfavorable remodeling of LV, particularly in hypertensive pregnancy.
Keywords: Echocardiography, Hypertension, Pregnancy
Introduction
Pregnancy induces dramatic cardiovascular changes in order to meet the maternal and growing fetal metabolic needs.1),2) Along with progressive placental growth, blood volume increases and peripheral vascular resistance decreases. Cardiac output and heart rate also increase during pregnancy. Such changes result in compensatory cardiac remodeling.3) In pregnancy complicated by hypertension, abnormal pressure overloading would lead to different cardiac remodeling compared to that of normal pregnancy. In the present study, we have performed comprehensive echocardiographic assessment for pregnancy-related hypertension in real world practice.
Methods
Study design and subjects
This was a retrospective study using medical record in a single tertiary care center from January 2008 to June 2012. Consecutive pregnant women referred for echocardiography with a diagnosis of hypertension were assigned to hypertensive women. Non-hypertensive pregnant women with normal echocardiographic finding during the same period were assigned to a normotensive control group. Exclusion criteria were pregnancy other than singleton, significant non-cardiac comorbidities and any significant structural heart diseases including systolic left ventricular (LV) dysfunction of LV ejection fraction (EF) < 50%, hypertrophic or restrictive cardiomyopathy, more than moderate degree of valvular heart disease and congenital heart disease. Demographic, laboratory and echocardiographic data were reviewed. Height and body weight were measured just before echocardiography, and those values were used to calculate body mass index (BMI) and body surface area (BSA). Systolic and diastolic blood pressure (BP) obtained from the brachial artery in the sitting position immediately before echocardiography was recorded. Gestational hypertension (GH) was defined as hypertension diagnosed after the 20th gestational week and previously having normal BP. Chronic hypertension (CH) was defined as pre-existing hypertension diagnosed before pregnancy or the 20th gestational week. The Institutional Review Board of a university affiliated hospital approved the study protocol.
Echocardiography
Standard two dimensional and Doppler echocardiography were performed in the left decubitus position using a 3.5-MHz transducer (Vivid 7 Dimension ultrasound equipment, General Electric, Horten, Norway) according to the current practice guidelines.4),5),6) LV wall thickness and LV end diastolic diameter (LVEDD) and LV end systolic diameter (LVESD) were measured from parasternal long and short axis views with M-mode recording under two-dimensional guidance. LV mass was calculated according to the formula of Devereux et al.7) Relative wall thickness (RWT) was calculated using the formula (2 × posterior wall thickness)/LVEDD.8) LV mass index (LVMI) was calculated by the normalization of LV mass by height and BSA.4) Value of LVMI calculated with BSA was used only for classification of LV geometry. Otherwise value of LVMI calculated with height was used throughout the study. LV geometry was classified according to LVMI normalized by BSA and RWT as follows: normal geometry if LVMI ≤ 95 g/m2 and RWT ≤ 0.42, concentric remodeling if LVMI ≤ 95 g/m2 and RWT > 0.42, concentric hypertrophy if LVMI > 95 g/m2 and RWT > 0.42 and eccentric hypertrophy if LVMI > 95 g/m2 and RWT ≤ 0.42.8) LV EF was derived from modified Simpson's method from apical 4-chamber and 2-chamber views. Left atrial volume was estimated using the biplane discs method using apical views. Peak velocity of early (E) and late (A) diastolic transmitral blood flow were measured with pulsed wave Doppler recording. Tissue Doppler indices of early diastolic mitral annular velocity (e') and peak systolic mitral annular velocity (s') were measured at the septal mitral annulus. LV and right ventricular (RV) Tei indices were obtained with pulsed wave Doppler recording. RV systolic pressure was calculated by simplified Bernoulli equation using peak systolic tricuspid regurgitation velocity. Tricuspid annular plane systolic excursion was obtained from M-mode recording in four chamber view.
Statistical analysis
Continuous data are presented as mean ± SD or median with 25–75th interquartile range (IQR). Frequency data are presented as numbers and percentages. Student's t-test or Mann-Whitney U test was used for comparison of continuous variables of two different groups. Chi-square test was used for frequency variables. Linear regression analysis was used to determine the factors associated with LVMI. Variables with a p < 0.1 in univariate analysis were included in the multiple regression model according to collinearity test. Standardized regression coefficient (β) was used to present the degree of correlation. p < 0.05 was considered statistically significant. SPSS for Windows version 16.0 (SPSS Inc., Chicago, IL, USA) was used for all analyses.
Results
Baseline characteristics
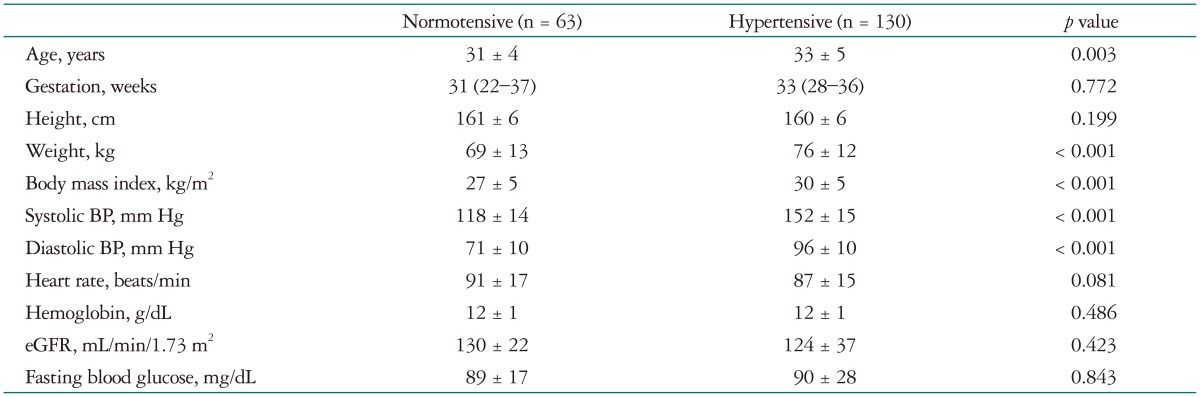
A total of 193 women were included in the final analysis and the participants were categorized into two groups as normotensive and hypertensive; 63 women were normotensive and 130 women were hypertensive (Table 1). Among hypertensive women, 76 women had GH and 54 had CH. Median (IQR) gestational age was similar in the two groups, that is, 31 (22-37) weeks in normotensive group and 33 (28-36) weeks in hypertensive group. Compared to the normotensive group, the hypertensive group was older (31 ± 4 years vs. 33 ± 5 years, p = 0.003) with heavier weight (69 ± 13 kg vs. 76 ± 12 kg, p < 0.001) and higher BMI (27 ± 5 kg/m2 vs. 30 ± 5 kg/m2, p < 0.001). Systolic and diastolic BP of the hypertensive group were 152 ± 15 mm Hg and 96 ± 10 mm Hg, which were significantly higher than those of the normotensive group with 118 ± 14 mm Hg (p < 0.001) and 71 ± 10 mm Hg (p < 0.001).
Table 1. Baseline characteristics according to hypertension status.
BP: blood pressure, eGFR: estimated glomerular filtration rate
LV remodeling in hypertensive pregnancy
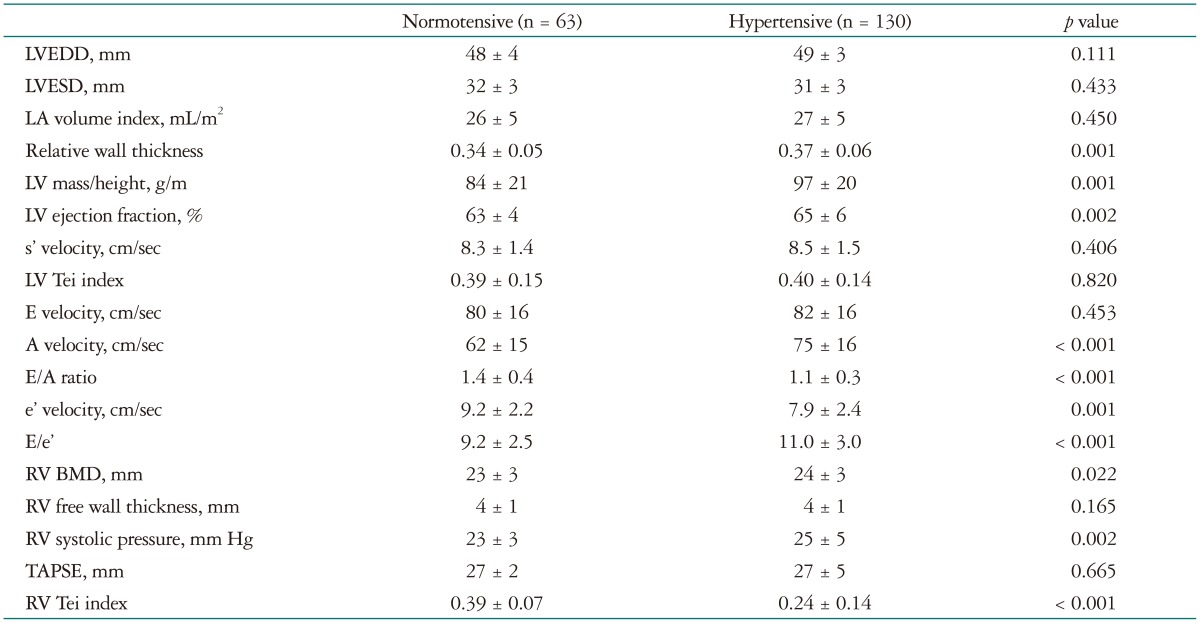
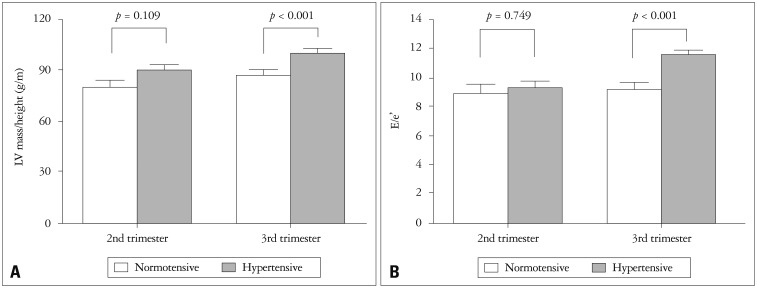
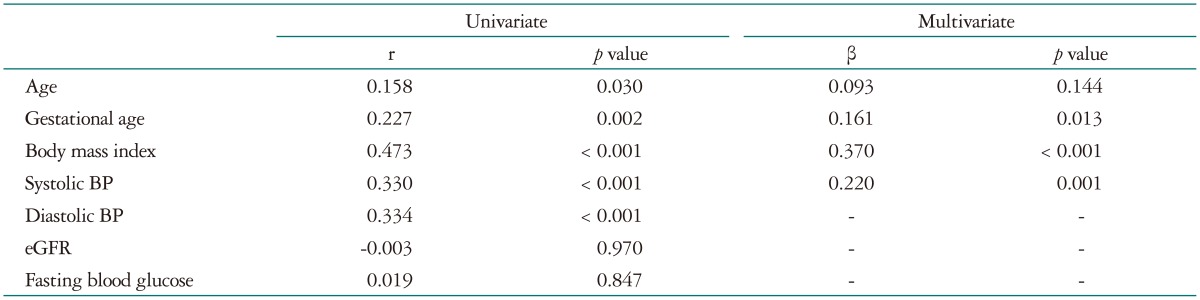
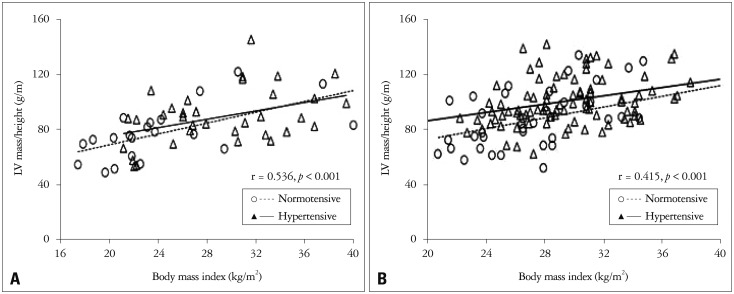
Echocardiographic findings are listed in Table 2. Mean LVEDD normalized by BSA was 28 ± 2 mm/m2 in the normotensive group. LVEDD and LVESD did not differ between the normotensive and hypertensive group. However, significantly higher RWT (0.34 ± 0.05 vs. 0.37 ± 0.06, p = 0.001) and LVMI (84 ± 21 g/m vs. 97 ± 20 g/m, p = 0.001) were observed in the hypertensive group compared with the normotensive group (Fig. 1A). LVMI showed correlation with gestational age (r = 0.227, p = 0.002), BMI (r = 0.473, p < 0.001), and systolic (r = 0.330, p < 0.001) and diastolic (r = 0.334, p < 0.001) BP (Table 3). In multivariate analysis, gestational age (β = 0.161, p = 0.013), BMI (β = 0.370, p < 0.001), and systolic BP (β = 0.220, p = 0.001) were significant factors for increased LVMI during pregnancy. For LV systolic function, the hypertensive group showed higher LV EF (63 ± 4% vs. 65 ± 6%, p = 0.002).
Table 2. Echocardiography according to hypertension status.
A: late diastolic transmitral blood flow velocity, BMD: basal minor diameter, E: early diastolic transmitral blood flow velocity, e': early diastolic mitral annular velocity, LA: left atrial, LV: left ventricular, LVEDD: LV end diastolic diameter, LVESD: LV end systolic diameter, RV: right ventricular, s': peak systolic mitral annular velocity, TAPSE: tricuspid annular plane systolic excursion
Fig. 1. Effects of hypertension on left ventricular (LV) mass and diastolic function. Hypertensive women show high LV mass index (A) and diastolic function index of E/e' ratio (B) compared with normotensive women in both middle and late trimester of pregnancy. Normotensive: normotensive women, Hypertensive: hypertensive women, E: early diastolic transmitral blood flow velocity, e': early diastolic mitral annular velocity.
Table 3. Factors influencing to left ventricular mass index in pregnant women.
BP: blood pressure, eGFR: estimated glomerular filtration rate
LV diastolic function in hypertensive pregnancy
Diastolic functional parameters were significantly reduced in hypertensive women compared to normotensive women. Significantly low E/A ratio (1.4 ± 0.4 vs. 1.1 ± 0.3, p < 0.001) and e' velocity (9.2 ± 2.2 vs. 7.9 ± 2.4, p = 0.001) were observed in hypertensive women. Significantly high peak A wave velocity (62 ± 15 vs. 75 ± 16, p < 0.001) and E/e' ratio (9.2 ± 2.5 vs. 11.0 ± 3.0, p < 0.001) were observed in hypertensive women (Table 2, Fig. 1B).
RV function in hypertensive pregnancy
Higher estimated RV systolic pressure was observed in hypertensive women compared to normotensive women (25 ± 5 mm Hg vs. 23 ± 3 mm Hg, p = 0.002). RV contractility did not differ between the groups.
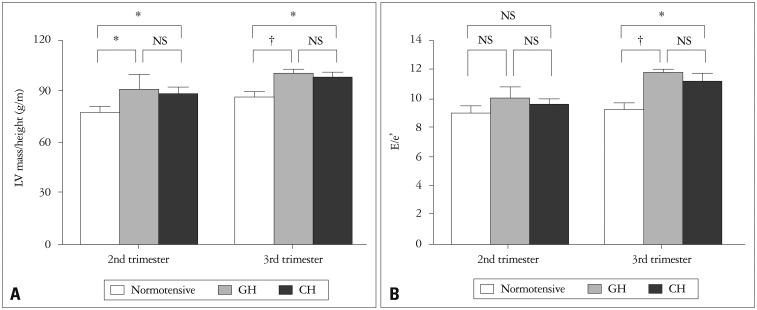
The effect of heavy body weight on LV remodeling
BMI was a significant factor for increased LVMI. There was a positive correlation between BMI and LVMI both in the second (r = 0.536, p < 0.001) and third trimester (r = 0.415, p < 0.001) (Fig. 2). The effect of BMI on LVMI was consistent in both normotensive and hypertensive women.
Fig. 2. Effects of body mass index on left ventricular (LV) mass in second (A) and third (B) trimester of pregnancy. Normotensive: normotensive women, Hypertensive: hypertensive women.
Gestational vs. chronic hypertension
To determine the effect of hypertension subtype on cardiac remodeling, LVMI and E/e' ratios were compared in normotensive, GH and CH women. Women with GH tended to have higher LVMI and E/e' ratio compared to those with CH although statistical significance was not reached (Fig. 3). LV geometry was analyzed for women in the third trimester (Fig. 4). In normotensive women, eccentric LV hypertrophy (LVH) was observed in 24%. In women with GH, eccentric LVH was observed in 24%. However, in women with CH, concentric remodeling/hypertrophy was more frequent (23%) than eccentric LVH (14%). The rate of concentric remodeling/hypertrophy was significantly higher in women with CH compared to those with GH (p = 0.003).
Fig. 3. Comparison of left ventricular (LV) mass (A) and diastolic function (B) in normotensive women, women with gestational hypertension (GH) and chronic hypertension (CH). *P < 0.05, †P < 0.01. E: early diastolic transmitral blood flow velocity, e': early diastolic mitral annular velocity, NS: not significant.
Fig. 4. Left ventricular geometry at the third trimester in normotensive women, women with gestational hypertension (GH) and women with chronic hypertension (CH). Eccentric left ventricular hypertrophy is more frequent in women with GH while concentric hypertrophy/remodeling is more frequent in those with CH.
Discussion
This study showed the recent echocardiographic data for normal and hypertensive pregnant women. Hypertensive pregnancy was associated with significant LVH and diastolic dysfunction. Maternal excessive body weight was significantly associated with LVH in hypertensive pregnancy. In contrast to women with GH, concentric remodeling pattern was more prevalent in pregnant women with CH.
Profound cardiovascular adaptive changes occur during normal pregnancy. The noticeable change is the increase in cardiac output and blood volume, which starts as early as the sixth week of pregnancy. Progressive decreases in systemic vascular resistance and BP occur accordingly with gestational age.1),2) The primary stimulus to LV remodeling during normal pregnancy is volume overload, which leads to compensatory cardiac remodeling including progressive mild dilation of all cardiac chambers and increase in LV mass.9) During normal pregnancy, peripheral resistance keeps low despite elevated blood concentrations of renin and angiotensin II.10) Possible explanation for such vascular refractoriness to activated renin-angiotensin system is the role of humoral factors such as progesterone and prostaglandin.11) Overall result of these modifications in a physiologic condition is the LV geometry of eccentric remodeling pattern.12) Although data regarding diastolic function during pregnancy are limited, a progressive decrease in E-wave velocity has been reported during normal pregnancy in a small study.12),13)
In severe form of pregnancy-related hypertension, including severe preeclampsia and eclampsia, decreased circulatory volume and low central venous pressure in addition to elevated systemic vascular resistance result in hyperdynamic LV function, elevated LV filling pressure, decreased cardiac output, and decreased peripheral perfusion.14) Although the pathogenesis of GH is largely unknown, defects in uteroplacental vascular bed and endothelial dysfunction are thought to play critical roles.15) Aggressive LV remodeling, predominantly eccentric LVH, was reported to be preceded pre-eclampsia.16) There are few reports about LV geometry and function in pregnancy complicated with CH. In hypertensive pregnancy, effects to vascular resistance and heart might be more complicated. Previous study reported that degree of LVH was matched with the cardiac work load during pregnancy and was more prominent in pre-eclamptic pregnancy than normotensive pregnancy.12) Concentric pattern of LV remodeling was frequently observed in pregnancy complicated by essential hypertension. Coexistence of pregnancy and hypertension tended to result in intensified LV hypertrophy and increased RWT.17) In the current study, LVH was exaggerated in hypertensive pregnancy and LV geometry was quite different between the women with GH and CH, which were in agreement with the previous report. Whether such different patterns of LV remodeling in GH and CH induce different clinical outcome is needed to be confirmed in future study. In the current study, LV mass and diastolic dysfunction parameter of E/e' ratio was higher in women with GH than those with CH. Considering the short disease duration of GH, such findings might be due to inadequate cardiac adaptation or more severe vascular damaging process compared to CH.
RV change during hypertensive pregnancy was not prominent in the current study. Contrary to our expectation, RV Tei index was lower in hypertensive women than in normotensive women. RV might be hyperdynamic as LV in hypertensive women (Table 2).
Maternal obesity has known to have many negative impacts on mothers and fetuses, including spontaneous abortion, unexplained stillbirth, operative delivery, and future cardiovascular disease.18) Risk of poor pregnancy outcomes associated with maternal obesity is proportional to the pre-gestational BMI. Pregnancy-related hypertensive disorders are thought to be the major mechanism of such dismal pregnancy outcomes.18) In the current study, LVMI was proportional to BMI, which was shown in both normotensive and hypertensive women. Although BMI during pregnancy is very limited tool to assess maternal obesity, our result suggests that heavy maternal body weight might accentuate unfavorable LV remodeling in hypertensive pregnancy. Control of maternal obesity might reduce the cardiac risk of hypertensive pregnancy.
The current study was conducted retrospectively and data were obtained with a single measurement at different gestational ages. Serial examination might have provided more valuable information about progressive cardiac remodeling and postpartum resolution, particularly in patients with CH. The proportion of patients with severe preeclampsia was small. The result of GH might be intensified in a more severe form of pregnancy-related hypertension such as severe preeclampsia or eclampsia. Lack of data regarding peripheral resistance and pregnancy outcome may limit the interpretation of results. Small sample size was an additional limitation.
In conclusion, hypertensive pregnancy is associated with significant LVH and diastolic dysfunction. CH seems to induce different LV remodeling pattern from GH. Excessive heavy maternal weight during pregnancy might intensify the unfavorable remodeling of LV, particularly in hypertensive pregnancy.
Acknowledgements
This study was supported by a grant from the Korean Society of Echocardiography (2011).
References
- 1.Warnes CA. Pregnancy and heart disease. In: Mann DL, Zipes DP, Libby P, Bonow RO, editors. Braunwald's heart disease: a textbook of cardiovascular medicine. 10th ed. Philadelphia: Elsevier Saunders; 2014. pp. 1755–1770. [Google Scholar]
- 2.European Society of Gynecology (ESG); Association for European Paediatric Cardiology (AEPC); German Society for Gender Medicine (DGesGM) Regitz-Zagrosek V, Blomstrom Lundqvist C, Borghi C, Cifkova R, Ferreira R, Foidart JM, Gibbs JS, Gohlke-Baerwolf C, Gorenek B, Iung B, Kirby M, Maas AH, Morais J, Nihoyannopoulos P, Pieper PG, Presbitero P, Roos-Hesselink JW, Schaufelberger M, Seeland U, Torracca L, ESC Committee for Practice Guidelines ESC Guidelines on the management of cardiovascular diseases during pregnancy: the Task Force on the Management of Cardiovascular Diseases during Pregnancy of the European Society of Cardiology (ESC) Eur Heart J. 2011;32:3147–3197. doi: 10.1093/eurheartj/ehr218. [DOI] [PubMed] [Google Scholar]
- 3.Geva T, Mauer MB, Striker L, Kirshon B, Pivarnik JM. Effects of physiologic load of pregnancy on left ventricular contractility and remodeling. Am Heart J. 1997;133:53–59. doi: 10.1016/s0002-8703(97)70247-3. [DOI] [PubMed] [Google Scholar]
- 4.Lang RM, Bierig M, Devereux RB, Flachskampf FA, Foster E, Pellikka PA, Picard MH, Roman MJ, Seward J, Shanewise JS, Solomon SD, Spencer KT, Sutton MS, Stewart WJ, Chamber Quantification Writing Group. American Society of Echocardiography's Guidelines and Standards Committee. European Association of Echocardiography Recommendations for chamber quantification: a report from the American Society of Echocardiography's Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr. 2005;18:1440–1463. doi: 10.1016/j.echo.2005.10.005. [DOI] [PubMed] [Google Scholar]
- 5.Nagueh SF, Appleton CP, Gillebert TC, Marino PN, Oh JK, Smiseth OA, Waggoner AD, Flachskampf FA, Pellikka PA, Evangelista A. Recommendations for the evaluation of left ventricular diastolic function by echocardiography. J Am Soc Echocardiogr. 2009;22:107–133. doi: 10.1016/j.echo.2008.11.023. [DOI] [PubMed] [Google Scholar]
- 6.Rudski LG, Lai WW, Afilalo J, Hua L, Handschumacher MD, Chandrasekaran K, Solomon SD, Louie EK, Schiller NB. Guidelines for the echocardiographic assessment of the right heart in adults: a report from the American Society of Echocardiography endorsed by the European Association of Echocardiography, a registered branch of the European Society of Cardiology, and the Canadian Society of Echocardiography. J Am Soc Echocardiogr. 2010;23:685–713. quiz 786-8. doi: 10.1016/j.echo.2010.05.010. [DOI] [PubMed] [Google Scholar]
- 7.Devereux RB, Alonso DR, Lutas EM, Gottlieb GJ, Campo E, Sachs I, Reichek N. Echocardiographic assessment of left ventricular hypertrophy: comparison to necropsy findings. Am J Cardiol. 1986;57:450–458. doi: 10.1016/0002-9149(86)90771-x. [DOI] [PubMed] [Google Scholar]
- 8.Ganau A, Devereux RB, Roman MJ, de Simone G, Pickering TG, Saba PS, Vargiu P, Simongini I, Laragh JH. Patterns of left ventricular hypertrophy and geometric remodeling in essential hypertension. J Am Coll Cardiol. 1992;19:1550–1558. doi: 10.1016/0735-1097(92)90617-v. [DOI] [PubMed] [Google Scholar]
- 9.Katz R, Karliner JS, Resnik R. Effects of a natural volume overload state (pregnancy) on left ventricular performance in normal human subjects. Circulation. 1978;58(3 Pt 1):434–441. doi: 10.1161/01.cir.58.3.434. [DOI] [PubMed] [Google Scholar]
- 10.Gant NF, Daley GL, Chand S, Whalley PJ, MacDonald PC. A study of angiotensin II pressor response throughout primigravid pregnancy. J Clin Invest. 1973;52:2682–2689. doi: 10.1172/JCI107462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gant NF, Worley RJ, Everett RB, MacDonald PC. Control of vascular responsiveness during human pregnancy. Kidney Int. 1980;18:253–258. doi: 10.1038/ki.1980.133. [DOI] [PubMed] [Google Scholar]
- 12.Simmons LA, Gillin AG, Jeremy RW. Structural and functional changes in left ventricle during normotensive and preeclamptic pregnancy. Am J Physiol Heart Circ Physiol. 2002;283:H1627–H1633. doi: 10.1152/ajpheart.00966.2001. [DOI] [PubMed] [Google Scholar]
- 13.Ghi T, degli Esposti D, Montaguti E, Rosticci M, Tancredi S, Youssef A, di Giovanni MV, Pilu G, Borghi C, Rizzo N. Maternal cardiac evaluation during uncomplicated twin pregnancy with emphasis on the diastolic function. Am J Obstet Gynecol. 2015;213:376.e1–376.e8. doi: 10.1016/j.ajog.2015.05.003. [DOI] [PubMed] [Google Scholar]
- 14.Easterling TR, Benedetti TJ, Schmucker BC, Millard SP. Maternal hemodynamics in normal and preeclamptic pregnancies: a longitudinal study. Obstet Gynecol. 1990;76:1061–1069. [PubMed] [Google Scholar]
- 15.Chaiworapongsa T, Chaemsaithong P, Yeo L, Romero R. Pre-eclampsia part 1: current understanding of its pathophysiology. Nat Rev Nephrol. 2014;10:466–480. doi: 10.1038/nrneph.2014.102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cho KI, Kim SM, Shin MS, Kim EJ, Cho EJ, Seo HS, Shin SH, Yoon SJ, Choi JH. Impact of gestational hypertension on left ventricular function and geometric pattern. Circ J. 2011;75:1170–1176. doi: 10.1253/circj.cj-10-0763. [DOI] [PubMed] [Google Scholar]
- 17.Zanati Bazan SG, Borges VM, Martin LC, Magalhães CG, Hueb JC, de Arruda Silveira LV, Peracoli JC, Matsubara BB. Disproportionate pregnancy-induced myocardial hypertrophy in women with essential hypertension. Am J Hypertens. 2013;26:816–821. doi: 10.1093/ajh/hpt023. [DOI] [PubMed] [Google Scholar]
- 18.Leddy MA, Power ML, Schulkin J. The impact of maternal obesity on maternal and fetal health. Rev Obstet Gynecol. 2008;1:170–178. [PMC free article] [PubMed] [Google Scholar]