Abstract
Background: Incident reporting is widely used in both patient safety improvement programmes, and in research on patient safety.
Objective: To identify the key requirements for incident reporting systems in primary care; to develop an Internet-based incident reporting and learning system for primary care.
Methods: A literature review looking at the purpose, design and requirements of an incident reporting system (IRS) was used to update an existing incident reporting system, widely used in Germany. Then, an international expert panel with knowledge on IRS developed the criteria for the design of a new web-based incident reporting system for European primary care. A small demonstration project was used to create a web-based reporting system, to be made freely available for practitioners and researchers. The expert group compiled recommendations regarding the desirable features of an incident reporting system for European primary care. These features covered the purpose of reporting, who should be involved in reporting, the mode of reporting, design considerations, feedback mechanisms and preconditions necessary for the implementation of an IRS.
Results: A freely available web-based reporting form was developed, based on these criteria. It can be modified for local contexts. Practitioners and researchers can use this system as a means of recording patient safety incidents in their locality and use it as a basis for learning from errors.
Conclusion: The LINNEAUS collaboration has provided a freely available incident reporting system that can be modified for a local context and used throughout Europe.
Keywords: Incident-reporting system, primary care, patient safety, LINNEAUS collaboration
KEY MESSAGE:
Incident reporting is a critical first step in learning from errors.
A web-based incident reporting system allows practitioners to record incidents as a means for learning from errors.
The LINNEAUS collaboration has provided a freely available incident reporting system that can be modified for a local context and used throughout Europe.
Introduction
A patient safety incident in primary care is any unintended event or hazardous condition resulting from the process of care, rather than due to the patient's underlying disease, that led or could have led to unintended health consequences for the patient (1). Incident reporting systems (IRS) in patient safety are tools to communicate safety-relevant information and allow clinicians to learn about and from patient safety incidents (2). Following the experience of their use in the aviation industry, incident-reporting systems became widely used in healthcare settings, especially in hospitals (3,4). They have also been used as part of well-established national and regional reporting systems in healthcare settings (2).
In 2005, to improve the usefulness of reporting systems, the WHO defined the basic design and implementation principles for successful IRS in healthcare organizations. These guidelines are intended for healthcare organizations in general and focus on the purpose of reporting systems, on the processes incorporated in such systems and summarize the characteristics of successful reporting systems, i.e. they are non-punitive, confidential and independent. The report also describes the limitations of IRS and the design considerations for an IRS (5).
Initially, the primary purpose of incident reporting systems was to provide information on the frequency of occurrence of patient safety incidents so that the causes could be mitigated and improvements to prevent further incidents could be developed. However, following the initial enthusiasm, the value of an incident reporting system began to be questioned. Several problems were identified. It became clear that under-reporting decreases the potential usefulness of incident reporting, that reports can be biased by hindsight and that the quality of data collected by reporting systems limits their usefulness (6–9). Makeham and colleagues (10) identified incident reporting as being the most commonly used means of gathering information in patient safety research in primary care. Incident reporting can also enhance the awareness of the importance of patient safety in family practices. For instance, Zwart (11) found that the implementation of incident reporting changed GPs’ understanding of safety problems.
The challenges for using IRS in primary care may be greater because of specific complexities related to improving patient safety in primary care. An additional challenge is that whilst nurses provide most incident alerts in the hospital setting; physicians are important reporters of incidents in primary care (12,13). All these factors are likely to influence both the type of incidents that are recorded in this setting and the nature of incident reports, suggesting that the development of a sector-specific IRS is necessary. O’Beirne also suggested that strong leadership, voluntary reporting, legal protection and feedback to reporters are all crucial (12).
In this article, we describe the findings from our literature review, focusing on the purpose of reporting, the structure of the reporting form, issues related to data protection and mechanisms for feedback. Subsequently, we used an expert panel that had extensive experience of working with European reporting systems to develop a series of recommendations on the content and structure of an IRS. Finally, we describe the process for developing the reporting tool, which could be used and modified for use in primary care throughout Europe.
METHODS
Literature review
Our literature review updated a review that we had previously carried out over five years ago when developing the national reporting system in Germany. We also supplemented our review with advice from the panel of experts who highlighted relevant articles, which enabled us to gather information on purpose, design, requirements, obstacles and maintenance of incident reporting systems.
Search strategy. Searches in PubMed, EMBASE and CINAHL were completed in November 2011. The searches employed the primary search terms ‘error reporting system,’ ‘incident reporting system’ and ‘learning system’ and were limited to the German and English languages.
Selection of relevant articles. Eligible papers reported on the development or implementation of an incident reporting system. Reviews or research papers on design considerations were also included. We also identified publications, which provided lessons learnt with respect to individual and organizational barriers and facilitators that influence the reporting process. Papers dealing with patient safety and reporting systems in a more general manner, (for example editorials) were excluded.
Summarizing content. The information obtained from the literature review was summarized and given to the expert panel that then used it as part of the background information in developing the criteria for an IRS for primary care.
Expert group
Selection of experts. We invited five persons with extensive experience of working with incident reporting systems to join an expert group. We used our contacts from the wider LINNEAUS collaboration to identify these experts. The group members came from different countries and were each familiar with a particular reporting system: the NRLS (England/Wales) (DL), Jeder-fehler-zählt.de (Germany) (BH), incident reporting guidelines from the Dutch College of General Practitioners, the incident reporting guidelines for all primary care professions of the Dutch Ministry of Health in The Netherlands (DZ), and a national patient safety reporting system in Denmark (TH, JH). We were not aware of any other European-based reporting systems, which could have fed into this process.
Expert group meetings. The group met for two days in December 2011. Day one was devoted to the identification of the most desirable features of an incident reporting system in primary care. The group was provided with a summary of characteristics extracted from the literature whose relevance for primary care they then discussed. A list of key issues was discussed and formulated into recommendations.
Day two was used to develop a reporting form for incident reporting in primary care, based on the results of the previous day and to find a consensual formulation of recommendations on the content and structure of an incident reporting system for European primary care.
Results
Review of the literature
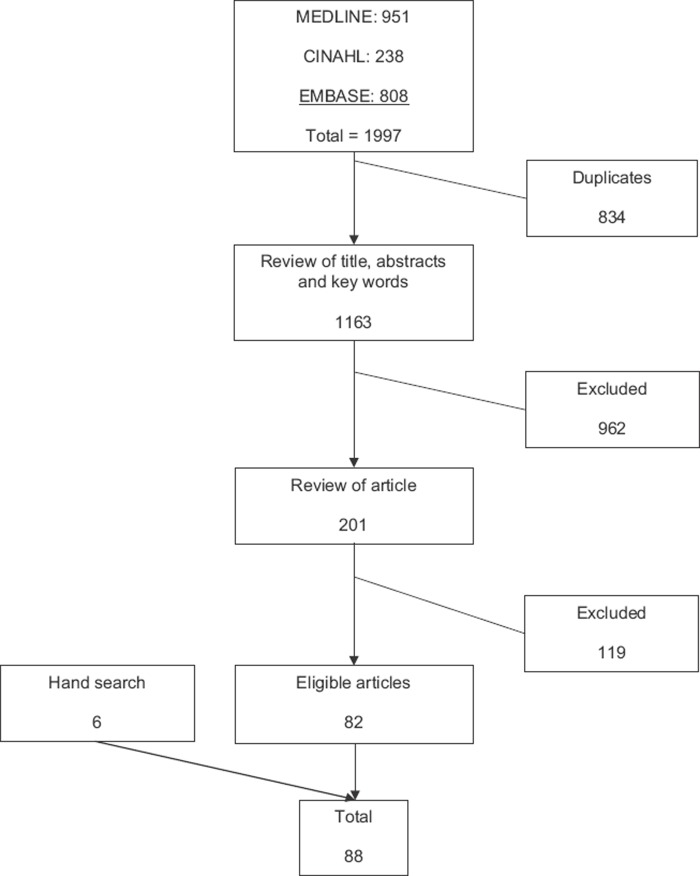
The review retrieved 88 studies on several reporting systems from throughout the world and from different settings. Only eight articles described reporting systems based primary care. Figure 1 describes a flow chart, which shows how we identified the relevant articles.
Figure 1. Flow chart of literature search and selection of papers on safety incident reporting systems in primary care.
The main themes identified in the 88 papers are described in Table 1.
Table 1. Number of papers identified under each theme in the literature review on safety incident reporting systems in primary care.
| Themes identified from the literature review | Number of papers |
|---|---|
| Purpose of reporting | 13 |
| Preconditions of a reporting system | 10 |
| Issues related to reporting persons | 18 |
| Mode of reporting | 19 |
| Structure and content of the reporting form | 21 |
| Design considerations | 14 |
| Feedback | 15 |
| Barriers to reporting | 17 |
For the purposes of this study, we amalgamated these themes into six dimensions covering
the purpose of reporting,
the reporting persons,
the mode of reporting,
design considerations,
feedback and preconditions required for the IRS.
Although very few articles provided information related specifically to the primary care setting, we were able to identify relevant information pertaining to the development of IRS for primary care from most of the papers we reviewed. This provided the basis for the expert group to make recommendations on the most desirable features of an incident reporting system for primary care, identify the key features of a form for incident reporting in primary care and then modify the content and structure of the incident reporting system for European primary care form.
Recommendations for an incident reporting system in primary care
The expert group compiled recommendations on the desirable features of an incident reporting system for European primary care for the six dimensions that were extracted from the literature review. The following recommendations are made on the assumption that the legal and social environment supports the implementation of reporting systems and acknowledges their importance for patient safety improvements. It was clear that diverging conditions in specific countries or organizations would necessitate certain adaptations. The first step was to determine the purpose of the intended reporting system. All subsequent propositions are necessary features of such a system. The recommendations comprise six domains and refer to the results of the literature search (see Box 1).
Box 1. Recommendations on the necessary features of an Independent Reporting System for primary care.
Purpose of reporting
to collect, systematically analyse and learn from patient safety incidents.
to improve patient safety and patient safety culture.
The purpose is NOT to create a quantitative database for actual incidents.
Reporting persons
Any member of staffs who witnessed or were involved in a patient safety incident or its consequences.
Mode of reporting
confidential; with the opportunity to report anonymously.
Design considerations
The system is designed to support the reporting process and analysis via:
access without login or passwords and be integrated into daily routines.
a simple definition of the events to be reported.
use of a common classification system.
use of individual and aggregated data
web-based, supporting safe print-outs (without identifiers)
to be launched locally and linked with other systems if desired
Feedback
Three kinds of feedback are required:
to the individual reporter in order to acknowledge the effort (‘Thank you for the report’ and details how it will be processed).
feedback to a target group (e.g. physicians or laboratory staff) with the purpose of learning from it. This will contain details of the analysis and the resulting solution
general feedback to the community to encourage cultural change and promote reporting and learning
Preconditions
Cultural and legal preconditions must be satisfied if the system is to be effective:
Non-punitive: reports cannot provide the basis for legal action against anyone involved in an incident, and should not be used in a court of law.
A just or no-blame-cultural environment including respect for professional accountability
Strong leadership throughout the practice or organization by management and respected front line staff
Shared understanding of what a patient safety incident is, and of the purpose of incident reporting
Development of a form for incident reporting in primary care
After gaining agreement on the recommendations, the expert group determined the content and structure of the reporting form. The experts agreed that the form should collect information on the event, its outcome and persons involved (Box 2).
Box 2. Suggested content of a safety incident reporting form for primary care.
What happened?
Details of medication, equipment, etc. involved?
Incident type?
Why did it happen?
How could the incident have been prevented?
Date and time of incident?
Outcome of incident (for patient, for family, for healthcare provider, for organization)?
Patient details (age and gender)?
Data on reporter (function within the organization, contact details)?
Questions 1, 2, 4, 5 and 9 should be presented as free-text fields.
Questions 3, 6, 7 and 8 should be presented with check boxes for a list of choices.
Recommendations on the content and structure of an incident reporting system for European primary care
The expert group oversaw the development of an incident reporting system, which can be specifically used in the European context. The system that was finally agreed builds on existing reporting systems, which have been used by the LINNEAUS partners in the UK, Germany and the Netherlands. The modified system was used in Poland and Greece where new initiatives related to patient safety were trialled and implemented as part of the LINNEAUS collaboration. The elements needed to set up a local system are now available on the homepage of the LINNEAUS EURO-PC collaboration (http://www.linneaus-pc.eu/) and have been developed so that researchers and clinicians can download the form, make changes specific to their local requirements and use it as part of a local or even national incident reporting system.
DISCUSSION
Main findings
We were able to identify information that enabled our expert panel to develop recommendations for an ideal IRS for primary care, a template for a reporting form and a web-based reporting tool.
Strengths and limitations
All fundamental aspects pertaining to the content and functionality of IRS for primary care were considered in this study and we believe that it could form the basis of an IRS for primary care irrespective of how primary care is organized.
Our study has some limitations. The development of the recommendations and the subsequent reporting model were based on the experiences of an expert team that did not come from all European countries. However, we tried to overcome this shortcoming by not restricting the literature search to specific countries. Another weakness is that we did not extensively test the feasibility and usefulness of the system in practice apart from using it in Poland and Greece as part of the LINNEAUS collaboration (14,15). However, the experience from these two pilots confirms our view that the form and web-based system can be used irrespective of the organization of primary care. In future studies, the implementation process of this model solution should be evaluated to identify implementation problems, to ascertain the cost, and to survey user experiences. It would also be interesting to monitor changes in practice following implementation to demonstrate the impact of improvement measures derived from the reports.
Implications
Reporting systems play an important role in improving patient safety, not by providing a means to determine the incidence rate of adverse events but rather by changing the way such events are dealt with (11). Reporting systems can encourage a stronger focus on eliminating shortcomings in practice processes and highlight the need for the whole practice team to share responsibility for patient safety (2). Thus, IRS can be a means to improve patient safety in organizations of all shapes and sizes. In their national summary report, the NHS Quality Improvement Scotland showed that professionals in primary care are particularly proactive in responding to reported incidents (16).
CONCLUSION
Based on the considerations described in the literature and on the group's personal expertise, we have developed a model solution for a reporting system that is tailor-made for primary care, both in terms of technical features and content. It is freely available, and it will enable GPs to initiate patient safety improvements in their practices. It can be easily implemented and adapted to suit individual needs, which will vary across different European jurisdictions. If used by a network of practices it can provide an excellent tool with which to learn from incidents within the organization. The online IRS is particularly useful for primary care practices providing healthcare as small independent units that are spread over a large area.
ACKNOWLEDGEMENTS
The authors should like to thank Juliane Albrecht for supporting the review process. The authors also thank Frank Aluttis for the technical implementation of the reporting system. Finally, special thanks go to Phillip Elliott for his linguistic support and to Corina Güthlin for her critical review.
FUNDING
The research leading to these results has received funding from the European Community's Seventh Framework Programme FP7/2008–2012 under grant agreement no. 223424.
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
REFERENCES
- Klemp K, Dovey S, Valderas JM, Rohe J, Godycki-Cwirko M, Elliott P, et al. Developing a patient safety incident classification system for primary care. A literature review and Dephi-survey by the LINNEAUS collaboration on patient safety in primary care. Eur J Gen Pract. 2015;21((S1)):35–38. doi: 10.3109/13814788.2015.1043723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vincent C. Reporting and learning systems. In Patient safety. 2nd ed. Chichester: Wiley-Blackwell; 2010:. pp. 75–95. [Google Scholar]
- Dovey SM, Wallis KA. Incident reporting in primary care: Epidemiology or culture change? BMJ Qual Saf. 2011;20:1001–3. doi: 10.1136/bmjqs-2011-000465. [DOI] [PubMed] [Google Scholar]
- Vincent C. Incident reporting and patient safety. Br Med J. 2007;334:51. doi: 10.1136/bmj.39071.441609.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Alliance for Patient Safety . WHO draft guidelines for adverse event reporting and learning systems. Geneva, Switzerland: World Health Organization; 2005. [Google Scholar]
- Stanhope N, Crowley-Murphy M, Vincent C, O’Connor A, Taylor-Adams SE. An evaluation of adverse incident reporting. J Eval Clin Pract. 1999;5:5–12. doi: 10.1046/j.1365-2753.1999.00146.x. [DOI] [PubMed] [Google Scholar]
- Vincent C, Stanhope N, Crowley-Murphy M. Reasons for not reporting adverse incidents: An empirical study. J Eval Clin Pract. 1999;5:13–21. doi: 10.1046/j.1365-2753.1999.00147.x. [DOI] [PubMed] [Google Scholar]
- Leape LL. Reporting of adverse events. N Engl J Med. 2002;347:1633–8. doi: 10.1056/NEJMNEJMhpr011493. [DOI] [PubMed] [Google Scholar]
- Thomas MJ, Schultz TJ, Hannaford N, Runciman WB. Mapping the limits of safety reporting systems in health care—what lessons can we actually learn? Med J Aust. 2011;194:635–9. doi: 10.5694/j.1326-5377.2011.tb03146.x. [DOI] [PubMed] [Google Scholar]
- Makeham M, Dovey S, Runciman WB, Larizgoitia I. Methods and measures used in primary care patient safety research. Results of a literature review. World Health Organization; 2008 [Google Scholar]
- Zwart DL, Steerneman AH, van Rensen EL, Kalkman CJ, Verheij TJ. Feasibility of centre-based incident reporting in primary healthcare: The SPIEGEL study. BMJ Qual Saf. 2011;20:121–7. doi: 10.1136/bmjqs.2009.033472. [DOI] [PubMed] [Google Scholar]
- O’Beirne M, Sterling P, Reid R, Tink W, Hohman S, Norton P. Safety learning system development-incident reporting component for family practice. Qual Saf Health Care. 2010;19:252–7. doi: 10.1136/qshc.2008.027748. [DOI] [PubMed] [Google Scholar]
- Fernald D, Pace W, Harris D, West D, Main D, Westfall J. Event reporting to a primary care patient safety reporting system: A report from the ASIPS collaborative. Ann Fam Med. 2004;2:327–32. doi: 10.1370/afm.221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Godycki-Cwirko M, Esmail A, Dovey S, Wensing M, Parker D, Kowalczyk A, et al. Patient safety initiatives in Central and Eastern Europe: A mixed methods approach by the LINNEAUS collaboration on patient safety in primary care. Eur J Gen Pract. 2015;21((S1)):62–68. doi: 10.3109/13814788.2015.1043727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skalkidis Y, Manoli A, Evagelos D, Nikolaos T, Sekeri Z, Dantsi F, et al. First experiences with patient safety initiatives in Greek rural primary care. (S1) Vol. 21. Informa Healthcare; 2015. pp. 69–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scotland NQI. NHS Quality Improvement Scotland; 2007. NHS Scotland incident reporting culture; extended study—national summary report. [Google Scholar]