Abstract
Background:
We compared efficacy and treatment persistence in treatment-naive patients with relapsing-remitting multiple sclerosis (RRMS) initiating natalizumab compared with interferon-β (IFN-β)/glatiramer acetate (GA) therapies, using propensity score–matched cohorts from observational multiple sclerosis registries.
Methods:
The study population initiated IFN-β/GA in the MSBase Registry or natalizumab in the Tysabri Observational Program, had ≥3 months of on-treatment follow-up, and had active RRMS, defined as ≥1 gadolinium-enhancing lesion on cerebral MRI at baseline or ≥1 relapse within the 12 months prior to baseline. Baseline demographics and disease characteristics were balanced between propensity-matched groups. Annualized relapse rate (ARR), time to first relapse, treatment persistence, and disability outcomes were compared between matched treatment arms in the total population (n = 366/group) and subgroups with higher baseline disease activity.
Results:
First-line natalizumab was associated with a 68% relative reduction in ARR from a mean (SD) of 0.63 (0.92) on IFN-β/GA to 0.20 (0.63) (p [signed-rank] < 0.0001), a 64% reduction in the rate of first relapse (hazard ratio [HR] 0.36, 95% confidence interval [CI] 0.28–0.47; p < 0.001), and a 27% reduction in the rate of discontinuation (HR 0.73, 95% CI 0.58–0.93; p = 0.01), compared with first-line IFN-β/GA therapy. Confirmed disability progression and area under the Expanded Disability Status Scale–time curve analyses were not significant. Similar relapse and treatment persistence results were observed in each of the higher disease activity subgroups.
Conclusions:
This study provides Class IV evidence that first-line natalizumab for RRMS improves relapse and treatment persistence outcomes compared to first-line IFN-β/GA. This needs to be balanced against the risk of progressive multifocal leukoencephalopathy in natalizumab-treated patients.
Classification of evidence:
This study provides Class IV evidence that first-line natalizumab for RRMS improves relapse rates and treatment persistence outcomes compared to first-line IFN-β/GA.
In the pivotal phase III Natalizumab Safety and Efficacy in Relapsing-Remitting Multiple Sclerosis (AFFIRM) trial, natalizumab demonstrated high efficacy in patients who were mostly (90%) naive to disease-modifying therapy (DMT).1 Despite this, in clinical practice natalizumab is often recommended for patients with multiple sclerosis (MS) with inadequate response to other treatments or patients with high levels of disease activity.2 For much of the world, the indicated use of natalizumab as a first-line therapy is restricted to patients with ≥2 relapses within 1 year and ≥1 gadolinium (Gd+)-enhancing lesion or a significant increase in T2 lesions on MRI.3 In settings where first-line use of natalizumab is not restricted, it is important for physicians to balance the potential efficacy benefits of natalizumab against a patient's risk of progressive multifocal leukoencephalopathy (PML) before initiating natalizumab.4
While factors that stratify natalizumab-associated PML risk, particularly anti–JC virus antibody status, have been identified,5 the potential efficacy advantage of natalizumab specifically as first-line therapy over other DMTs has not been fully explored. Placebo-controlled trials such as AFFIRM1 and those comparing natalizumab as an adjunct therapy to interferon-β (IFN-β) and glatiramer acetate (GA) vs IFN-β or GA monotherapy6–8 do not provide information on outcomes associated with initiating natalizumab monotherapy vs other treatment options commonly considered in clinical practice. There are no head-to-head clinical trials comparing the efficacy of first-line natalizumab treatment to other first-line DMTs.
In the respective pivotal clinical trials comparing active treatment to placebo, natalizumab monotherapy reduced annualized relapse rate (ARR) by 68%9–16 compared to an around 30% reduction for IFN-β preparations and GA. Although these trials largely enrolled treatment-naive patients, they were conducted in different epochs resulting in different absolute ARRs (ranging from 0.73 to 1.28 in the placebo groups). A head-to-head comparison is therefore needed to establish the comparative effectiveness of first-line natalizumab vs IFN-β or GA.
The primary objective of this study was to compare time to first relapse and treatment discontinuation in DMT-naive patients with active MS disease who initiated first-line natalizumab treatment compared with first-line Betaferon/Betaseron, Rebif, Avonex, Copaxone, or Extavia (BRACE) treatments. Confirmed disability progression was studied as a secondary endpoint. Propensity score-matching was employed to reduce the confounding inherent to observational studies.17–20 The study group has recently successfully employed this technique for MS treatment comparisons in the MSBase registry dataset and also in a combined MSBase/Tysabri Observational Program (TOP) dual dataset, 2 contemporaneous, real-world cohorts.21–23
METHODS
Standard protocol approvals, registrations, and patient consents
Patients treated with BRACE or natalizumab were extracted from the MSBase and TOP registries, respectively. Details of these registries have been published previously.16,24 In both registries, relapse is characterized according to the McDonald criteria,25 while interactive neurostatus training is used for consistent assessment of Expanded Disability Status Scale (EDSS). Project approval from an ethical standards committee on human experimentation (institutional or regional) for any experiments using human subjects was obtained by each clinical center contributing data to either MSBase or TOP registries. Written informed consent was obtained from all patients contributing data to either registry in accordance with the local regulations and laws applicable at each clinic.
Study design
Patients and subgroups
DMT-naive patients exhibiting disease activity (defined by ≥1 relapse within 12 months of baseline or ≥1 Gd+-enhancing lesion at baseline) were eligible for analysis. Baseline was defined as the time of DMT commencement. Patients were censored at the date of recording a first relapse, discontinuation, or progression event for each analysis, or the date of last clinician assessment point. Comparisons were made between propensity score–matched patients who initiated natalizumab vs BRACE therapy as their first-line DMT. Participants with <3 months of follow-up or no recorded cerebral MRI within 6 months prior to DMT commencement were excluded (figure 1).
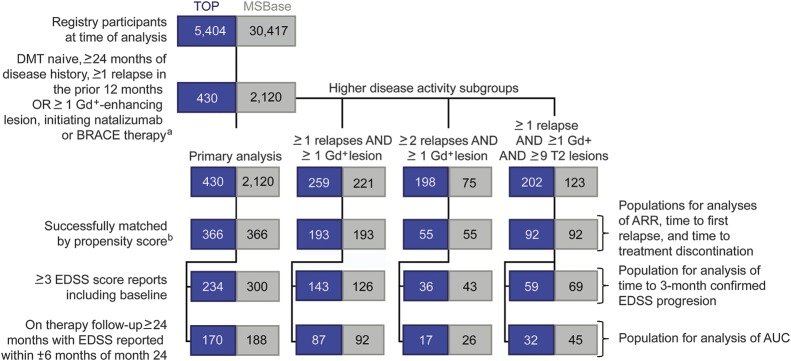
Figure 1. Study profile.
Of the 5,404 Tysabri Observational Program (TOP) participants at time of analysis, 518 were treatment-naive at baseline, all of whom recorded a minimum 24 months of prebaseline follow-up, while 430 of these also recorded at least 1 relapse in the 12 months prior to baseline or at least 1 gadolinium (Gd+) lesion on baseline MRI. Of the 30,417 enrolled MSBase participants, 11,564 were treatment-naive at baseline, 9,018 recorded a minimum of 24 months prebaseline activity, and 2,120 of these also recorded at least 1 relapse in the 12 months prior to baseline or at least 1 Gd+ lesion on baseline MRI. ARR = annualized relapse rate; AUC = area under the curve; BRACE = Betaferon/Betaseron, Rebif, Avonex, Copaxone, or Extavia; DMT = disease-modifying therapy; EDSS = Expanded Disability Status Scale.
aPatients in TOP initiated natalizumab. Patients in MSBase initiated a BRACE therapy.
bPropensity score matching was performed independently for the primary analysis and in each higher disease activity subgroup.
Subgroup analyses compared treatment efficacy and persistence in patients with various levels of baseline MS disease activity. The 3 subgroups considered were (1) ≥1 relapse and ≥1 Gd+-enhancing lesion; (2) ≥2 relapses and ≥1 + Gd+-enhancing lesion; or (3) ≥1 relapse and ≥1 Gd+-enhancing lesion and ≥9 T2 hyperintense lesions. Matching treatment arms by propensity score was performed separately for the total eligible sample of the primary analysis and then repeated for each analysis subgroup (figure 1).
Efficacy measures
The primary research question was whether there was a difference in the rate of first relapse or treatment discontinuation in patients on first-line natalizumab relative to first-line BRACE. A classification of Class IV evidence applies to both outcomes. ARR, time to first on-treatment relapse, and treatment persistence were analyzed as primary outcomes. Secondary endpoints included time to 3-month confirmed disability progression and 24-month change in area under the serial disability/time curve (AUC). Confirmed disability progression events were defined as minimum 3-month confirmed increases of ≥0.5, ≥1.0, and ≥1.5 points for patients with baseline EDSS >5.5, between 1.0 and 5.5, and 0, respectively.23 EDSS scores recorded within 30 days postrelapse were excluded.23 The comparison of disability progression by treatment arm was limited to patients contributing at least 3 EDSS assessment points, as the minimum required to first observe and then confirm a progression event.23
Serial disability/time AUC change comparisons were performed to estimate patients' cumulative on-treatment disability experience. EDSS scores assessed within a 24-month interval from baseline were initially plotted, and AUC calculated as previously described in our published reports.22,23 As a sensitivity analysis, AUC change in EDSS was also calculated using the trapezoidal rule.26
Statistical analyses
Data from the MSBase and TOP registries were aggregated according to a prespecified protocol. Categorical variables were summarized using frequency and percentage and continuous factors summarized using median and interquartile range (IQR) or mean and SD as appropriate.
For both the primary analysis group and each of the 3 high disease activity subgroups, patients from the natalizumab group were matched to a comparable patient in the BRACE arm using propensity matching. Sex, age, EDSS, disease duration, and the count of both total relapses and steroid-treated relapses in the 12 and 24 months prior to baseline were used to 1:1 match patients employing a 5:1 digit “greedy” matching algorithm as previously described by this study group.21-23,27 As a sensitivity analysis, clinic country was included for the derivation of the propensity score. A 1:1 match was preferred over a 1-to-many match as the latter introduced unacceptable imbalance secondary to the poorer quality of the secondary and tertiary matches. Balance of baseline covariates by treatment arm postmatching was assessed via analysis of standardized differences and matched Wilcoxon signed-rank and McNemar tests. Wilcoxon rank-sum for continuous factors and a χ2 test for categorical variables were used to compare unmatched baseline characteristics by treatment arm.21-23
A Cox marginal model was used to test for differences in time to first on-treatment relapse event, treatment persistence, and disability progression by treatment arm. Scaled Schoenfeld residuals were used to test each model for underlying hazard proportionality. The potential influence of informative censoring secondary to group differences in follow-up time on event ascertainment was studied by extending the Cox models to include follow-up differentials as competing risks for observing endpoint events. A test for interaction was used to assess the subgroups for treatment effects.
Quantile median regression was used to compare AUC change in EDSS across treatment arms adjusting for the matched pairs via censored least absolute deviations. A Royston extension of the Cochran-Armitage test28 was used to check for nonlinearity in associations between AUC change in EDSS and treatment arm. An a priori specified Rosenbaum sensitivity analyses was applied postestimation across all outcomes to test the sensitivity of the matched models to unobserved heterogeneity secondary to baseline characteristics that were either not collected or incompletely observed.29 As a sensitivity analysis, the relapse, discontinuation, and progression models were rerun using first-line natalizumab initiations sourced from within MSBase. In all analyses, p < 0.05 was considered significant. All analyses were conducted in Stata version 13 (StataCorp, College Station, TX).
RESULTS
Patients
Of the eligible patients (figure 1, natalizumab, 430; BRACE, 2,120), 366 (85.1%) first-line natalizumab commencements were successfully matched to a first-line BRACE initiation. Significant imbalance in prematching baseline covariates were observed across treatment arms; patients commencing natalizumab were younger and had shorter disease duration, higher median EDSS, and greater pretreatment relapse activity compared to those commencing BRACE (table 1). Conversely, there was no significant observed imbalance between treatment arms after matching (table 2). Mean (SD) number of relapses in the 12 months prior to treatment initiation was 1.9 in both arms while median baseline was 3 across both arms, representing a relatively active and severe disease cohort. Mean (SD) on-treatment follow-up was 3.1 years (2.7) in the BRACE group compared to 2.0 years (1.4) in the first-line natalizumab treatment arm (p[signed-rank] = 0.001). Mean (SD) time between on-treatment assessments was 5.9 months (5.2) on first-line BRACE therapy relative to the 6.4 months (2.7) observed in the natalizumab arm (p[signed-rank] = 0.103). Similarly, there was no difference in the median on-study visit density between the matched groups with the natalizumab group recording a median (IQR) number of visits per year of 2.41 (1.94, 3.09) compared with 2.57 (1.91, 3.85) in the BRACE arm (p[signed-rank] = 0.142).
Table 1.
Baseline characteristics of unmatched patients
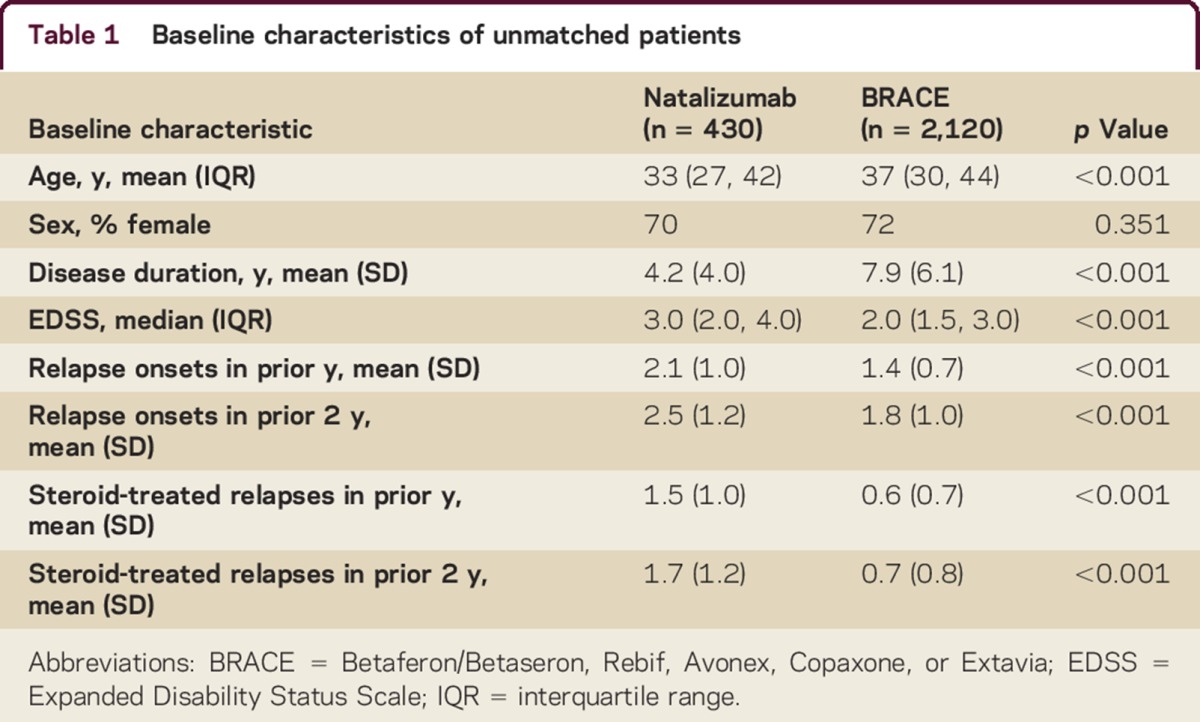
Table 2.
Baseline characteristics of propensity score–matched patients

On-treatment relapse
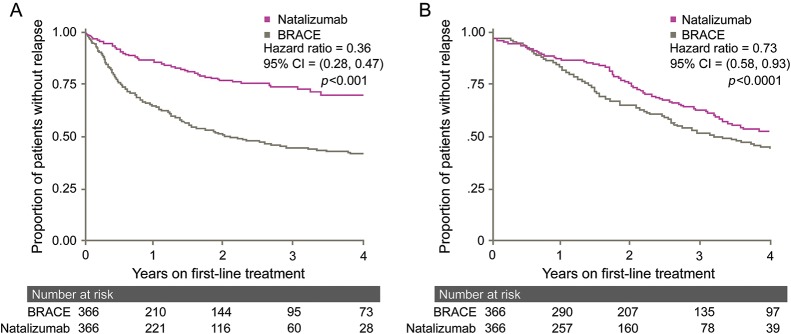
On-treatment ARR was lower (relative reduction, 68%; p[signed-rank] < 0.0001) for patients who initiated natalizumab (mean 0.20; SD 0.63) as their first-line DMT compared to BRACE (mean 0.63; SD 0.92) (table 3). During the study, 76 (20.7%) natalizumab patients experienced an on-treatment relapse at a rate of 12.7 first relapse events per 100 person-years; 224 (61.2%) BRACE patients experienced an on-treatment relapse at a rate of 25.1 first relapse events per 100 person-years of on-treatment follow-up, corresponding to a 64% reduction in the relapse rate for patients who initiated natalizumab (hazard ratio [HR] 0.36, 95% confidence interval [CI] 0.28–0.47) (figure 2A).
Table 3.
Summary of propensity-matched treatment group outcomes by prior disease activity
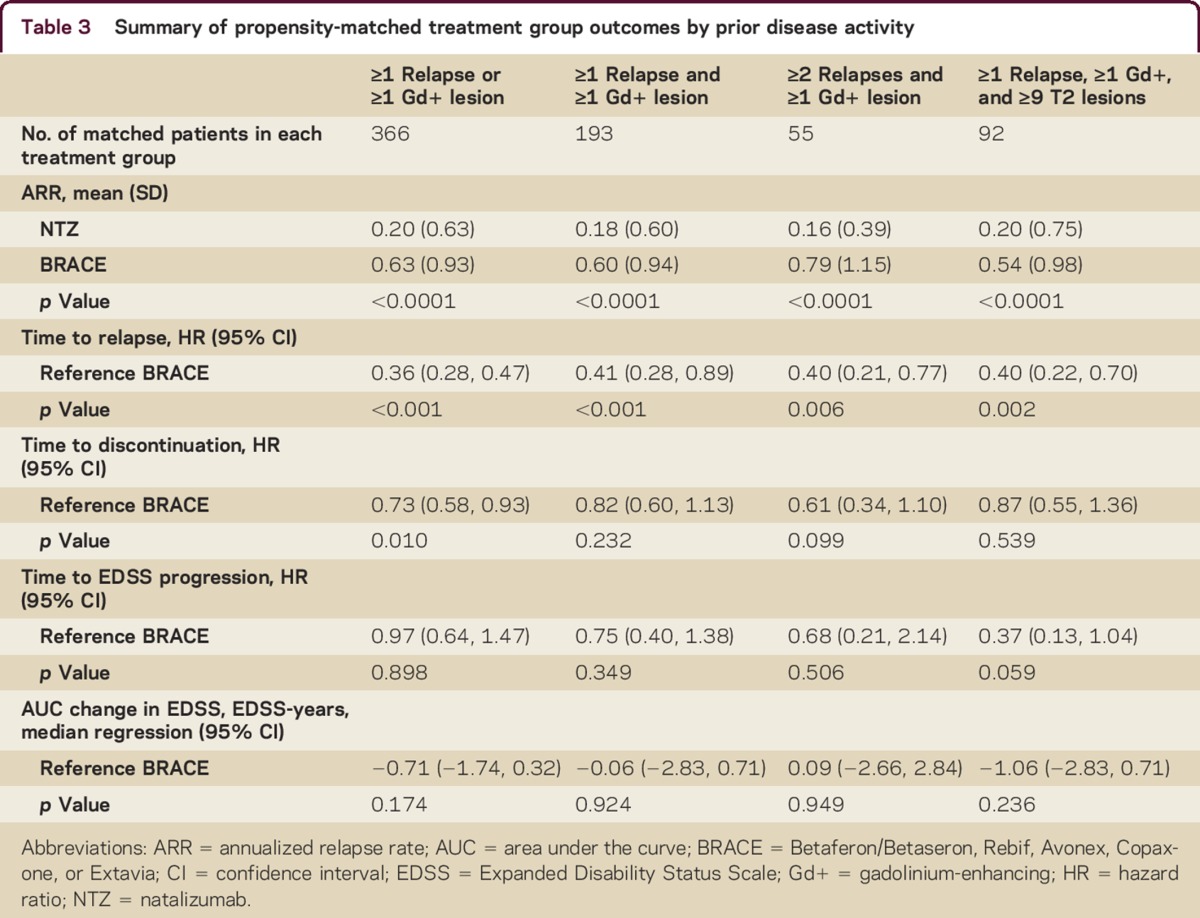
Figure 2. Time to (A) first relapse and (B) treatment discontinuation on first-line treatment.
BRACE = Betaferon/Betaseron, Rebif, Avonex, Copaxone, or Extavia; CI = confidence interval.
Treatment persistence
During the study, 108 (29.5%) patients who initiated natalizumab ceased treatment compared with 229 (62.6%) BRACE patients. This translated into a modeled 27% decrease in discontinuation rate (HR 0.73, 95% CI 0.58–0.93) favoring first-line natalizumab (figure 2B). Among those patients who discontinued, treatment cessation occurred earlier in the natalizumab arm than in BRACE (median [IQR] years to discontinuation: natalizumab, 1.7 [0.9–2.8]; BRACE, 2.3 [1.1–4.2]) (p[signed-rank] < 0.0001).
While patients on first-line BRACE therapy recorded a longer mean follow-up duration, the competing risks extension to the primary Cox marginal models for both relative relapse and discontinuation rates did not significantly alter the results of the primary models, suggesting that the follow-up differential observed did not significantly influence the estimated HRs, either in the presence or absence of simultaneous censoring of the matched pair. In a sensitivity analysis, patients were rematched with clinic country included as a baseline covariate. Although results were largely concordant with those demonstrated in the primary analysis, effect sizes were generally less significant, consistent with the smaller size and reduced power of these groups (table e-1 at Neurology.org/cp).
Disability progression
A total of 534 patients (natalizumab, 234; BRACE, 300) were included in the analysis of disability progression metrics. There was no significant imbalance in baseline factors between the subset treatment groups. There were no differences in 3-month confirmed disability progression events between groups (natalizumab, 16.2%; BRACE, 22.0%, p[McNemar] = 0.095). There was no difference in rate of confirmed progression across either the first 12 months of treatment (HR 0.74, 95% CI 0.37–2.68, reference = BRACE) or the full treatment period (HR 0.97, 95% CI 0.64–1.47, reference = BRACE) (table 3).
AUC change in EDSS
Of the 732 matched patients, 358 (natalizumab, 170; BRACE, 188) were eligible for the exploratory AUC analysis. No difference in baseline factors was observed by subset treatment group. First-line natalizumab was associated with a decrease in EDSS of a median 0.71 points per year relative to BRACE (annualized AUC change = −0.71, 95% CI −1.74, 0.32; reference = BRACE), although this difference was not significant. The proportion of patients in this subgroup recording a confirmed disability progression event over the 2 years was lower in the natalizumab group (17.1% vs 26.6%, p[McNemar χ] = 0.030) and there was no difference in progression rate by treatment group (HR 0.99, 95% CI 0.59–1.56; reference = BRACE).
Subgroup analyses
In higher prebaseline disease activity subgroups, there were imbalance in baseline matching factors between the treatment groups after propensity matching patients in each subgroup (table 3). Patients who initiated natalizumab as first-line therapy within all subgroups exhibited lower on-treatment ARR relative to first-line BRACE (relative reductions, 63%–80%) with the largest benefit observed in patients recording at least 2 relapses prior to initiating treatment (table 3). Similarly, first relapse rate was lower for patients initiating natalizumab with comparable risk reductions observed in each subgroup (59%–60%) (table 3). No differences were observed between treatment arms in treatment discontinuation, EDSS progression, or AUC in any of the subgroups (table 3).
Sensitivity analyses
To test the validity of combining data from 2 registries, we repeated the analysis sourcing first-line natalizumab initiations from within the MSBase registry. Compared with the 430 first-line natalizumab commencements available from the TOP registry, only 288 were extracted from within MSBase, of which 212 (73.6%) were able to be successfully matched on a 1:1 basis to a comparable BRACE patient. Repeating the modeling, natalizumab was again associated with both a reduction in the rate of first on-treatment relapse (HR 0.40, 95% CI 0.26, 0.63) and treatment discontinuation (HR 0.77, 95% CI 0.61, 0.99) relative to BRACE. There was no difference in disability progression (HR 0.85, 95% CI 0.22, 3.23).
Rosenbaum sensitivity analysis for the influence of unmeasured confounding
Postestimation Rosenbaum sensitivity analyses of the outcome models estimated that a minimum 3.27-, 2.90-, and 2.69-fold increase in the rate of relapse, treatment discontinuation, and confirmed disability progression, respectively, would be required for an unobserved prognostic confounder to prompt a revision of each model and reject any inference of an effect attributable to the first-line treatment arm in favor of selection effects. In the context of the HRs observed, these changes represent improbably large fold increases and thus the treatment differentials observed were reasonably robust to unmeasured influences.
DISCUSSION
This is a large, head-to-head comparison of on-treatment relapse occurrence, therapy persistence, and disability outcomes in patients who either initiated natalizumab or a BRACE therapy as first-line treatment. Initiating natalizumab was associated with lower ARR, lower risk of first on-treatment relapse, and lower risk of treatment discontinuation, compared to initiating a BRACE therapy. Most disability outcomes were not significantly different between the treatment groups in the primary analysis. In matched pairs completing 24 months of treatment, however, several EDSS progression measures favored the natalizumab treatment arm, especially in patients with combined clinical and MRI disease activity and ≥9 T2 lesions.
The efficacy advantage of natalizumab compared to BRACE treatments in this study is consistent with other studies comparing these treatment options in patients who switched treatment.23,30,31 As the population here was wholly treatment-naive, our results extend these findings to potentially inform first-line treatment decisions in clinical practice. Several studies suggest that use of high efficacy treatments earlier in disease course or earlier in treatment sequence could improve long-term patient outcomes. In STRATA, an extension study for patients completing the phase III natalizumab trials, efficacy benefits associated with natalizumab (vs placebo, IFN-β, or GA) persisted after all patients were switched to natalizumab over all 6 years of observation.15 In the 5-year interim analysis of TOP, patients who initiated natalizumab as first-line therapy or those with lower baseline EDSS had the lowest on-treatment disease activity.16 Several smaller studies also suggest greater treatment response to natalizumab occurs in younger patients with lower baseline EDSS and shorter disease duration,32-34 suggesting a potential advantage for earlier natalizumab treatment initiation. Where indications permit, physicians consider the use of natalizumab as a first-line therapy, and the current study validates this strategy.
Prior studies have suggested that not all patients are likely to benefit equally from natalizumab as a first-line therapy, with larger relative natalizumab treatment effects in patients with higher ARR in the 12 months prior to treatment initiation.6,32,35 Consistent with these studies, prior relapse activity appeared to influence the relative treatment effect; the relative ARR reduction seen with natalizumab treatment over BRACE therapies was observed to be highest in the patient subgroup with ≥2 relapses in the prior year (ARR was roughly 5-fold higher for BRACE) compared to groups that included patients with ≥1 relapse in the prior year (ARR was roughly 3-fold higher). Maximal relative benefits to ARR were observed in patients with more aggressive MS. While this suggests that relapse activity in treatment-naive patients may enable early identification of patients who may benefit most from timely treatment intervention, efficacy benefits were apparent with natalizumab first-line treatment across all levels of disease activity. Conversely, the improvement in first-line treatment persistence in favor of natalizumab observed in the primary analysis was not replicated in any of the subgroup analyses. While this may in part be secondary to underpowering associated with the smaller subgroup sample sizes, this may suggest that discontinuation decisions may in part be influenced by baseline disease severity.
Confirmed disability progression, as both a proportion of sample and as a time to event outcome, was generally not different between treatment arms. By requiring a minimum of 3 temporally separated EDSS assessment points, disability progression is more follow-up intensive and thus this part of the analysis is likely to be underpowered relative to either the relapse or discontinuation modeling. Matching natalizumab initiators with comparable BRACE patients on baseline similarities in disease activity favors inclusion of more benign natalizumab patients. Exclusion therefore of the most active natalizumab patients, while ensuring balance in these disease activity metrics across treatment arms, also biases against observation of a difference in progression by treatment group. Furthermore, higher treatment discontinuation in the BRACE group limited the total sample size available for these analyses, so that a larger sample is required to determine if disability outcome differences exist between these treatments when used as first-line therapies. We were unable to adjust for the influence of JC virus antibody titer on the probability of early natalizumab discontinuation secondary to incomplete data. Even so, this suggests our observation of a significant decrease in natalizumab discontinuation rate relative to BRACE is likely to be a conservative estimate. Recent observations by Prosperini et al.36 of an increased risk of disease worsening following natalizumab discontinuation suggests that concerns around disease reactivation may in part contribute to the observed reduction in natalizumab discontinuation rate relative to BRACE, although this was not able to be directly assessed.
This study is limited by nonrandom assignment of patients. Unlike a truly randomized design, our results may be biased from residual confounding secondary to imbalance of unobserved factors not included as a matching variable. The retrospective nature of the study means the analysis is more prone to selection and ascertainment bias, relative to a prospective design. It is, however, unlikely that residual bias would favor the natalizumab arm, since measured variables suggest patients initiating natalizumab had, as expected, much worse disease. While propensity matching cannot eliminate residual confounding secondary to unobserved influences, the Rosenbaum sensitivity analysis suggested that any confounding contributed by unmeasured influences was highly unlikely to be large enough to change these inferences. Generalization of the efficacy advantages observed in this study could be limited by the characteristics of this population or by potential treatment indication bias that were not adjusted for in the matched datasets. The efficacy measures addressed in this study are not the only factors to consider when selecting MS treatments. Whether considering natalizumab as first-line therapy or later in treatment sequence, it is important to weigh the potential efficacy benefits of natalizumab against a patient's individualized risk for PML when making treatment decisions. Recent observations of possible rebound disease activity following cessation of natalizumab further suggest such risk stratification may also extend to decisions around discontinuing, as well as initiating, natalizumab.37 A comparative analysis of safety and adverse event data was unable to be conducted secondary to insufficient data availability. A larger dataset with more complete data and longer follow-up would be required to better analyze both cessation reason and subsequent postdiscontinuation outcomes. We were unable to compare MRI lesion activity outcomes by treatment group secondary to incomplete recording of postbaseline MRI. Similarly, reason for treatment discontinuation by treatment arm was only partially recorded and was thus insufficiently available to analyze. Finally, a larger dataset with longer cumulative follow-up would be required to validate the AUC analysis against hard disability endpoints such as time to EDSS 6.
Our results suggest that use of natalizumab as a first-line treatment for RRMS greatly reduces relapse rate and improves medication persistence compared to the common practice of BRACE initiation. Further analyses for these first-line treatment comparisons might include cost-effectiveness and quality of life metrics, since comparative cost-effectiveness between first-line BRACE therapies has been well-studied,38 and natalizumab treatment has demonstrated benefits to quality of life and patient-reported outcomes in other treatment contexts.39-41
Supplementary Material
ACKNOWLEDGMENT
The authors thank the MSBase Study Group contributors for data contribution and registry administration (appendix e-1) and the following additional contributors: Samir Méchati (Rodanotech, data entry system technical support); Alexandru Bulla (Rodanotech, data entry system technical support); Matthieu Corageoud (Rodanotech, data entry system technical support); Nolan Campbell (Biogen, provided editorial assistance which involved reference management and manuscript versioning management, data contributor); Patrick Campbell (Biogen, provided minor graphic design assistance with a subset of figures during the development of this manuscript, data contributor).
Footnotes
Editorial, page 97
Supplemental data at Neurology.org/cp
Contributor Information
Collaborators: MSBase Investigators and the TOP investigators, Cees Zwanikken, Maria Edite Rio, Imre Piroska, Fraser Moore, Tunde Erdelyi, Olga Skibina, Vincent Van Pesch, Gerardo Iuliano, Erik van Munster, Marcela Fiol, Jorge Correale, Celica Ysrraelit, Maria Pia Amato, Leontien den Braber-Moerland, Ilya Kister, Krisztian Kasa, Carmen-Adella Sirbu, Cameron Shaw, Santiago Vetere, Steve Vucic, Tatjana Petkovska-Boskova, Bhim Singhal., Elizabeth Alejandra Bacile Bacile, Walter Oleschko Arruda, Elaine Roger, Pierre Despault, Mark Marriott, Anneke Van der Walt, John King, Jill Byron, Lisa Morgan, Jodi Haartsen, Giovanna De Luca, Valeria Di Tommaso, Daniela Travaglini, Erika Pietrolongo, Maria di Ioia, Deborah Farina, Luca Mancinelli, Juan Ignacio Rojas, Liliana Patrucco, Elisabetta Cartechini, Giorgio Giuliani, David Williams, Lisa Dark, Aldo Savino, Joab Chapman, Shlomo Flechter, Edgardo Cristiano, Jose Antonio Cabrera-Gomez, Maria Laura Saladino, Norma Deri, Orla Gray, Mark Paine, and Norbert Vella
AUTHOR CONTRIBUTIONS
T. Spelman conceptualized and designed the study, conducted the statistical analysis, interpreted the analysis, and drafted and revised the paper. T. Kalincik conceptualized and designed the study, interpreted the analysis, and revised the paper. V.G. Jokubaitis interpreted the analysis and revised the paper. A. Zhang conceptualized and designed the study and revised the paper. F. Pelligrini conceptualized and designed the study and revised the paper. H. Wiendl interpreted the analysis and revised the paper. S. Belachew conceptualized and designed the study, interpreted the analysis, and revised the paper. R. Hyde conceptualized and designed the study, interpreted the analysis, and revised the paper. F. Verheul interpreted the analysis and revised the paper. A. Lugaresi interpreted the analysis and revised the paper. E. Havrdová interpreted the analysis and revised the paper. D. Horáková interpreted the analysis and revised the paper. P. Grammond interpreted the analysis and revised the paper. P. Duquette interpreted the analysis and revised the paper. A. Prat interpreted the analysis and revised the paper. G. Iuliano interpreted the analysis and revised the paper. M. Terzi interpreted the analysis and revised the paper. G. Izquierdo interpreted the analysis and revised the paper. R.M.M. Hupperts interpreted the analysis and revised the paper. C. Boz interpreted the analysis and revised the paper. E. Pucci interpreted the analysis and revised the paper. G. Giuliani interpreted the analysis and revised the paper. P. Sola interpreted the analysis and revised the paper. D.L.A. Spitaleri interpreted the analysis and revised the paper. J. Lechner-Scott interpreted the analysis and revised the paper. R. Bergamaschi interpreted the analysis and revised the paper. F. Grand'Maison interpreted the analysis and revised the paper. F. Granella interpreted the analysis and revised the paper. L. Kappos interpreted the analysis and revised the paper. M. Trojano interpreted the analysis and revised the paper. H. Butzkueven conceptualized and designed the study, interpreted the analysis, and revised the paper.
STUDY FUNDING
Supported by the NHMRC Career Development Award (Clinical) to H.B. (ID628856), NHMRC Early Career Fellowship (1071124), NHMRC Project Grants (1032484 and 1083539), NHMRC Center for Research Excellence (Grant ID 1001216), and the MSBase Foundation. The MSBase Foundation is a not-for-profit organization that receives support from Merck Serono, Biogen, Novartis Pharma, Bayer-Schering, Sanofi-Aventis, and BioCSL. The Tysabri Observational Program is fully funded by Biogen. E. Havrdová and D. Horáková have been supported by Research Grant of Czech Ministry of Education, PRVOUK–P26/LF1/4.
DISCLOSURES
T. Spelman serves on a scientific advisory board for Biogen; has received funding for travel and speaker honoraria from Novartis and Biogen; and serves on the editorial board of Journal of the International AIDS Society and as Guest Lead Editor for Biomedical Research International. T. Kalincik serves on scientific advisory boards for Novartis, Merck, and Biogen; has received compensation for travel from Novartis, Biogen, Sanofi Aventis, Teva, and Merck Serono; serves on speakers' bureaus for Biogen, Novartis, Genzyme, and BioCSL; and received a postdoctoral research fellowship from Multiple Sclerosis Research Australia. V.G. Jokubaitis has received funding for travel and speaker honoraria from Novartis, funding for travel from Merck Serono, and speaker honoraria from Biogen; and receives research support from NHMRC and MSBase Foundation. A. Zhang is employed by Biogen as Director of Global Medical and holds stock/stock options in Biogen. F. Pellegrini is employed by Biogen as Senior Principal Biostatistician and holds stock options in Biogen. H. Wiendl serves on scientific advisory boards for Bayer Healthcare, Biogen, Sanofi-Genzyme, Merck Serono, Novartis, Roche, and Teva; has received funding for travel or speaker honoraria from Bayer Vital GmbH, Bayer Schering AG, Biogen, CSL Behring, EMD Serono, Fresenius Medical Care, GlaxoSmithKline, GW Pharmaceuticals, Sanofi-Genzyme, Merck Serono, Omniamed, Novartis, and Teva; serves on the editorial boards of Journal of Clinical Practice, Journal of Neuroinflammation, and PLOS ONE; serves as a consultant for Biogen, Merck Serono, Novartis, Omniamed, Roche, and Sanofi-Genzyme; and receives research support from Bayer Healthcare, Bayer Vital, Biogen, Merck Serono, Novartis, Sanofi-Genzyme, Sanofi US, Teva Pharma, German Ministry for Education and Research (BMBF), Deutsche Forschungsgesellschaft (DFG), European Union, Else Kröner Fresenius Foundation, Fresenius Foundation, Hertie Foundation, NRW Ministry of Education and Research, Interdisciplinary Center for Clinical Studies (IZKF) Muenster, and RE Children's Foundation. S. Belachew is employed by Biogen International GmbH as a Medical Director and has equity interests in Biogen Inc. R. Hyde is employed by Biogen as Senior Director in the Medical Department in Europe and holds stock in Biogen. F. Verheul serves on a scientific advisory boards for Teva, Biogen, Merck Serono, and Novartis. A. Lugaresi serves on a scientific advisory board for Merck Serono; has received funding for travel or speaker honoraria from Bayer, Biogen, Merck Serono, Novartis, Sanofi-Genzyme, Teva, and Fondazione Italiana Sclerosi Multipla; serves as a consultant for Bayer Schering, Biogen, Merck Serono, Novartis, Sanofi-Genzyme, and Fondazione Italiana Sclerosi Multipla; and receives research support from Bayer, Biogen, Merck Serono, Sanofi, Novartis, Teva, and Associazione Italiana Sclerosi Multipla. E. Havrdová serves on scientific advisory boards for Biogen, Novartis, Teva, and Genzyme; has received funding for travel or speaker honoraria from Biogen, Novartis, Teva, Genzyme, Alkermes, and Roche; serves as a consultant for Biogen, Novartis, Teva, Genzyme, Alkermes, and Roche; and receives research support from Biogen, Merck Serono, European Commission, and Czech Ministry of Education. D. Horáková has received compensation for travel, speaker honoraria, and consultant fees from Biogen, Novartis, Merck, Bayer Schering, and Teva; serves as an Associate Editor for BMC Neurology; and receives research support from Biogen and Czech Ministries of Education and Health. P. Grammond serves on scientific advisory boards for Biogen, Merck Serono, Genzyme, Novartis, and Teva Neuroscience; has received funding for travel from Teva Neuroscience, Novartis, and Merck Serono and speaker honoraria from Biogen and Merck Serono, Teva-Neuroscience, and Canadian Multiple Sclerosis Society; and receives research support from Biogen, Sanofi-Aventis, and MSBase Foundation. P. Duquette serves on scientific advisory boards for Biogen, EMD Serono, Novartis, Teva Neuroscience, and Genzyme; has received support to attend meetings from Biogen, EMD Serono, Novartis, Teva Neuroscience, and Genzyme; is author on a patent re: a cellular adhesion molecule; participates in the organization of CME activities with Biogen, EMD Serono, Novartis, Teva Neuroscience, and Genzyme; and receives research support from Biogen, Novartis, Genzyme, EMD Serono, CIHR, and MS Society of Canada. A. Prat serves as an Associate Editor for Multiple Sclerosis Journal and Cellular Immunology. G. Iuliano has had received travel/accommodations/meeting expenses funded by Bayer Schering, Biogen, Merck Serono, Novartis, Sanofi Aventis, and Teva. M. Terzi has received travel grants from Merck Serono, Novartis, Bayer Schering, and Teva; and has received research support from Sanofi Aventis, Roche, and Novartis. G. Izquierdo serves on scientific advisory boards for Biogen, Bayer Schering, Sanofi, Novartis, Merck Serono, and Teva; and serves as a consultant for Sanofi, Merck Serono, and Novartis. R.M.M. Hupperts has served on scientific advisory boards for Biogen, Novartis, Teva, Merck Serono, and Genzyme-Sanofi; has received speaker honoraria from Biogen, Teva, and Sanofi-Genzyme; and has received research support from Biogen and Merck. C. Boz has received travel grants from Merck Serono, Biogen, Novartis, Bayer Schering, and Teva; and has received research support from Sanofi Aventis, Roche, and Novartis. E. Pucci serves on scientific advisory boards for Biogen, Novartis, and Genzyme; has received funding for travel from Associazione Marchigiana sclerosi multipla e altre malattie neurologiche and funding for travel and speaker honoraria from Biogen, Genzyme, Merck Serono, Sanofi Aventis, Teva, and Novartis; serves on the editorial board of The Scientific World Journal–Geriatrics; and receives research support from Associazione marchigiana sclerosi multipla e altre malattie neurologiche. G. Giuliani reports no disclosures. P. Sola has received travel grants from Merck Serono, Novartis, and Bayer Schering and travel grants and speaker honoraria from Teva and Biogen. D.L.A. Spitaleri serves on a scientific advisory board for C.I.C. Edizioni Internazionali; has received funding for travel or speaker honoraria from Novartis, Bayer, Sanofi Aventis, Biogen, Teva, and Merck Serono; serves as a consultant for Novartis, Sanofi-Aventis, and Bayer; and receives research support from Merck Serono, Novartis, and Schering. J. Lechner-Scott has served on scientific advisory boards for Bayer Health Care, Merck Serono, Biogen, Novartis, CSL, Genzyme-Sanofi, and Teva; has received travel compensation and honoraria from Biogen, Novartis, and Merck Serono; and receives research support from Biogen, Novartis, Hunter Medical Research Institute, University of Newcastle Australia, and John Hunter Hospital Charitable Trust. R. Bergamaschi has received funding for travel and speaker honoraria from Sanofi-Aventis, Genzyme, Biogen, Bayer Schering, Teva Neurosciences, Merck Serono, Almirall, and Novartis; has received research support from Merck Serono, Biogen, Teva Neurosciences, Bayer Schering, Novartis, and Sanofi-Aventis; and is an Associate Editor for BMC Neurology and on the editorial boards of Multiple Sclerosis International and Clinical Forum. F. Grand'Maison serves on scientific advisory boards for Genzyme and Biogen; and receives research support from Novartis, Genzyme, Mitsubishi, Biogen, Sanofi, Genentech, Chugai, and Opexa Therapeutics. F. Granella serves on scientific advisory boards for Biogen Italy, Novartis, and Sanofi-Aventis; and has received funding for travel or speaker honoraria from Biogen, Novartis, Merck Serono, and Almirall. L. Kappos serves on the editorial boards of Multiple Sclerosis Journal, Multiple Sclerosis and Related Disorders, and Journal of Neurology; has received research support from Acorda, Allozyne, BaroFold, Bayer Schering, Bayhill Therapeutics, Elan, Genmab, Gianni Rubatto Foundation, GlaxoSmithKline, Glenmark, MediciNova, Wyeth, Actelion, Addex, Alkermes, Almirall, Bayer Health Care, Biogen, CSL Behring, Genentech, GeNeuro SA, Genzyme, Merck Serono, Mitsubishi, Novartis, Octapharma, Pfizer, Receptos, Roche, Sanofi-Aventis, Santhera, Teva, UCB, Swiss National Research Foundation, European Union, Swiss MS Society, Novartis Research Foundation, and Roche Research Foundation; and receives royalty payments from Neurostatus Systems AG (transferred to the research account of the University Hospital Basel). M. Trojano has served on scientific advisory boards for Biogen, Novartis, Almirall, and Roche; has received honoraria for travel and speaking from Merck Serono, Novartis, Almirall, Teva, Genzyme-Sanofi, and Biogen; and has received research support from Novartis, Biogen, Teva, and Merck Serono. H. Butzkueven has served on scientific advisory boards for the MSBase Foundation, Novartis Australia and Novartis International, Biogen Australia and International, Genzyme International, and Multiple Sclerosis Research Australia; has received support from Novartis Australia (speaker honoraria), Merck Serono Australia (speaker honoraria, travel support), Biogen Australia (speaker honoraria, travel support), Genzyme Australia (travel support, speaker honoraria), and Medscape (speaker honoraria); serves on the editorial boards of Multiple Sclerosis International, Multiple Sclerosis and Related Disorders, and Frontiers in Neuro-ophthalmology; holds patents for treatment application of LIF in MS and treatment application of EPHA4 blockade in MS; has received research support from Biogen Australia, Merck Serono Australia, Novartis Australia, CASS Foundation (Australia), the Royal Melbourne Hospital Friends of the Neurosciences Foundation, the University of Melbourne, and the National Health and Medical Research Council. Full disclosure form information provided by the authors is available with the full text of this article at Neurology.org/cp.
REFERENCES
- 1.Polman CH, O'Connor PW, Havrdová E, et al. A randomized, placebo-controlled trial of natalizumab for relapsing multiple sclerosis. N Engl J Med 2006;354:899–910. [DOI] [PubMed] [Google Scholar]
- 2.Kappos L, Bates D, Edan G, et al. Natalizumab treatment for multiple sclerosis: updated recommendations for patient selection and monitoring. Lancet Neurol 2011;10:745–758. [DOI] [PubMed] [Google Scholar]
- 3.TYSABRI Summary of Product Characteristics from the European Medicines Agency [online]. Available at: http://www.ema.europa.eu/ema/. Accessed August 21, 2014.
- 4.Nicholas JA, Racke MK, Imitola J, Boster AL. First-line natalizumab in multiple sclerosis: rationale, patient selection, benefits and risks. Ther Adv Chronic Dis 2014;5:62–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bloomgren G, Richman S, Hotermans C, et al. Risk of natalizumab-associated progressive multifocal leukoencephalopathy. N Engl J Med 2012;366:1870–1880. [DOI] [PubMed] [Google Scholar]
- 6.Hutchinson M, Kappos L, Calabresi PA, et al. The efficacy of natalizumab in patients with relapsing multiple sclerosis: subgroup analyses of AFFIRM and SENTINEL. J Neurol 2009;256:405–415. [DOI] [PubMed] [Google Scholar]
- 7.Goodman AD, Rossman H, Bar-Or A, et al. GLANCE: results of a phase 2, randomized, double-blind, placebo-controlled study. Neurology 2009;72:806–812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rudick RA, Stuart WH, Calabresi PA, et al. Natalizumab plus interferon beta-1a for relapsing multiple sclerosis. N Engl J Med 2006;354:911–923. [DOI] [PubMed] [Google Scholar]
- 9.Duquette P, Despault L, Knobler L, et al. Interferon beta-1B in the treatment of multiple sclerosis: final outcome of the randomized controlled trial. Neurology 1995;45:1277–1285. [PubMed] [Google Scholar]
- 10.Jacobs LD, Cookfair DL, Rudick RA, et al. Intramuscular interferon beta-1a for disease progression in relapsing multiple sclerosis. Ann Neurol 1996;39:285–294. [DOI] [PubMed] [Google Scholar]
- 11.Ebers GC. Randomised double-blind placebo-controlled study of interferon β-1a in relapsing/remitting multiple sclerosis. Lancet 1998;352:498–1504. [Google Scholar]
- 12.Johnson KP, Brooks BR, Cohen JA, et al. Copolymer 1 reduces relapse rate and improves disability in relapsing-remitting multiple sclerosis: results of a phase III multicenter, double-blind, placebo-controlled trial. Neurology 1995;45:1268–1276. [DOI] [PubMed] [Google Scholar]
- 13.Romeo M, Martinelli-Boneschi F, Rodegher M, Esposito F, Martinelli V, Comi G. Clinical and MRI predictors of response to interferon-beta and glatiramer acetate in relapsing-remitting multiple sclerosis patients. Eur J Neurol 2013;20:1060–1067. [DOI] [PubMed] [Google Scholar]
- 14.Ebers GC, Traboulsee A, Li D, et al. Analysis of clinical outcomes according to original treatment groups 16 years after the pivotal IFNB-1b trial. J Neurol Neurosurg Psychiatry 2010;81:907–912. [DOI] [PubMed] [Google Scholar]
- 15.O'Connor P, Goodman A, Kappos L, et al. Long-term safety and effectiveness of natalizumab redosing and treatment in the STRATA MS Study. Neurology 2014;83:78–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Butzkueven H, Kappos L, Pellegrini F, et al. Efficacy and safety of natalizumab in multiple sclerosis: interim observational programme results. J Neurol Neurosurg Psychiatry 2014;85:1190–1197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rosenbaum PR, Rubin DB. Constructing a control group using multivariate matched sampling methods that incorporate the propensity score. Am Stat 1985;39:33–38. [Google Scholar]
- 18.D'Agostino RB., Jr Propensity score methods for bias reduction in the comparison of a treatment to a non-randomized control group. Stat Med 1998;17:2265–2281. [DOI] [PubMed] [Google Scholar]
- 19.Parsons LS. Reducing bias in a propensity score matched-pair sample using greedy matching techniques. Proceedings of the Twenty-sixth annual SAS users Group International Conference 2001;26:214–226.
- 20.Kurth T, Walker AM, Glynn RJ, et al. Results of multivariable logistic regression, propensity matching, propensity adjustment, and propensity-based weighting under conditions of nonuniform effect. Am J Epidemiol 2006;163:262–270. [DOI] [PubMed] [Google Scholar]
- 21.Kalincik T, Jokubaitis V, Izquierdo G, et al. Comparative effectiveness of glatiramer acetate and interferon beta formulations in relapsing-remitting multiple sclerosis. Mult Scler 2014;21:1159–1171. [DOI] [PubMed] [Google Scholar]
- 22.Kalincik T, Horáková D, Spelman T, et al. Switch to natalizumab versus fingolimod in active relapsing-remitting multiple sclerosis. Ann Neurol 2015;77:425–435. [DOI] [PubMed] [Google Scholar]
- 23.Spelman T, Kalincik T, Zhang A, et al. Comparative efficacy of switching to natalizumab in active multiple sclerosis. Ann Clin Transl Neurol 2015;2:373–387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Butzkueven H, Chapman J, Cristiano E, et al. MSBase: an international, online registry and platform for collaborative outcomes research in multiple sclerosis. Mult Scler 2006;12:769–774. [DOI] [PubMed] [Google Scholar]
- 25.McDonald WI, Compston A, Edan G, et al. Recommended diagnostic criteria for multiple sclerosis: guidelines from the International panel on the diagnosis of multiple sclerosis. Ann Neurol 2001;50:121–127. [DOI] [PubMed] [Google Scholar]
- 26.Liu C, Blumhardt LD. Benefits of glatiramer acetate on disability in relapsing-remitting multiple sclerosis. An analysis by area under disability/time curves: The Copolymer 1 Multiple Sclerosis Study Group. J Neurol Sci 2000;181:33–37. [DOI] [PubMed] [Google Scholar]
- 27.Rassen JA, Shelat AA, Myers J, et al. One-to-many propensity score matching in cohort studies. Pharmacoepidemiol Drug Saf 2012;21:69–80. [DOI] [PubMed] [Google Scholar]
- 28.Royston P. PTREND: Stata module for trend analysis for proportions. Stat Softw Comp 2002. [Google Scholar]
- 29.DiPrete TA, Gangl M. Assessing bias in the estimation of causal effects: Rosenbaum bounds on matching estimators and instrumental variables estimation with imperfect instruments. Sociol Methodol 2004;34:271–310. [Google Scholar]
- 30.Prosperini L, Gianni C, Leonardi L, et al. Escalation to natalizumab or switching among immunomodulators in relapsing multiple sclerosis. Mult Scler 2012;18:64–71. [DOI] [PubMed] [Google Scholar]
- 31.Lanzillo R, Quarantelli M, Bonavita S, et al. Natalizumab vs interferon beta 1a in relapsing-remitting multiple sclerosis: a head-to-head retrospective study. Acta Neurol Scand 2012;126:306–314. [DOI] [PubMed] [Google Scholar]
- 32.Sargento-Freitas J, Batista S, Macario C, Matias F, Sousa L. Clinical predictors of an optimal response to natalizumab in multiple sclerosis. J Clin Neurosci 2013;20:659–662. [DOI] [PubMed] [Google Scholar]
- 33.Prosperini L, Gianni C, Barletta V, et al. Predictors of freedom from disease activity in natalizumab treated-patients with multiple sclerosis. J Neurol Sci 2012;323:104–112. [DOI] [PubMed] [Google Scholar]
- 34.Wickstrom A, Nystrom J, Svenningsson A. Improved ability to work after one year of natalizumab treatment in multiple sclerosis. Analysis of disease-specific and work-related factors that influence the effect of treatment. Mult Scler 2013;19:622–630. [DOI] [PubMed] [Google Scholar]
- 35.Laroni A, Gandoglia I, Solaro C, et al. Clinical baseline factors predict response to natalizumab: their usefulness in patient selection. BMC Neurol 2014;14:103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Prosperini L, Annovazzi P, Capobianco M, et al. Natalizumab discontinuation in patients with multiple sclerosis: Profiling risk and benefits at therapeutic crossroads. Mult Scler 2015;21:1713–1722. [DOI] [PubMed] [Google Scholar]
- 37.Fox RJ, Cree BA, De Sèze J, et al. MS disease activity in RESTORE: a randomized 24-week natalizumab treatment interruption study. Neurology 2014;82:1491–1498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Goldberg LD, Edwards NC, Fincher C, Doan QV, Al-Sabbagh A, Meletiche DM. Comparing the cost-effectiveness of disease-modifying drugs for the first-line treatment of relapsing-remitting multiple sclerosis. J Manag Care Pharm 2009;15:543–555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Walker A, Watson C, Alexopoulos ST, Deniz B, Arnold R, Bates D. A benefit-risk analysis of natalizumab in the treatment of patients with multiple sclerosis when considering the risk of progressive multifocal leukoencephalopathy. Curr Med Res Opin 2014;30:629–635. [DOI] [PubMed] [Google Scholar]
- 40.Planas R, Martin R, Sospedra M. Long-term safety and efficacy of natalizumab in relapsing-remitting multiple sclerosis: impact on quality of life. Patient Relat Outcome Meas 2014;5:25–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kamat SA, Rajagopalan K, Stephenson JJ, Agarwal S. Impact of natalizumab on patient-reported outcomes in a clinical practice setting: a cross-sectional survey. Patient 2009;2:105–112. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.