Abstract
BACKGROUND
Patients may have lower (white coat hypertension) or higher (masked hypertension) blood pressure (BP) at home compared to the clinic, resulting in misdiagnosis and suboptimal management of hypertension. This study aimed to systematically review the literature and establish the most important predictors of the home-clinic BP difference.
METHODS
A systematic review was conducted using a MEDLINE search strategy, adapted for use in 6 literature databases. Studies examining factors that predict the home-clinic BP difference were included in the review. Odds ratios (ORs) describing the association between patient characteristics and white coat or masked hypertension were extracted and entered into a random-effects meta-analysis.
RESULTS
The search strategy identified 3,743 articles of which 70 were eligible for this review. Studies examined a total of 86,167 patients (47% female) and reported a total of 60 significant predictors of the home-clinic BP difference. Masked hypertension was associated with male sex (OR 1.47, 95% confidence interval (CI) 1.18–1.75), body mass index (BMI, per kg/m2 increase, OR 1.07, 95% CI 1.01–1.14), current smoking status (OR 1.32, 95% CI 1.13–1.50), and systolic clinic BP (per mm Hg increase, OR 1.10, 95% CI 1.01–1.19). Female sex was the only significant predictor of white coat hypertension (OR 3.38, 95% CI 1.64–6.96).
CONCLUSIONS
There are a number of common patient characteristics that predict the home-clinic BP difference, in particular for people with masked hypertension. There is scope to incorporate such predictors into a clinical prediction tool which could be used to identify those patients displaying a significant masked or white coat effect in routine clinical practice.
Keywords: ambulatory blood pressure monitoring, hypertension, masked hypertension, primary care, white coat hypertension.
Hypertension is an important risk factor for cardiovascular disease,1 the major cause of morbidity and mortality worldwide.2 Effective diagnosis and management of hypertension depends on accurate measurement of blood pressure, which allows appropriate targeting of antihypertensive treatment. Ambulatory blood pressure monitoring (ABPM) is considered to be the “gold standard” measure of blood pressure, because multiple readings are taken and because it is associated with a range of cardiovascular outcomes and end organ damage.3–7 Ambulatory blood pressure is usually lower than clinic blood pressure8–11 due to the white coat effect (Table 1),12 and as such, clinical guidelines recommend that ABPM (or home) blood pressure targets are 5mm Hg lower than the corresponding clinic values.13,14 However, this “home-clinic blood pressure difference” is not always consistent. In some patients, blood pressures measured at home or with ABPM are higher than would be expected for the corresponding clinic blood pressure, the so-called masked effect (Table 1).15 Such patients are likely to be undertreated and have increased target organ damage16,17 with subsequent increased cardiovascular mortality compared to normotensive patients.18,19
Table 1.
Definitions of the home-clinic blood pressure difference
| Term | Definition |
|---|---|
| Home-clinic blood pressure difference | The difference between blood pressure measured with ABPM or at home (self-monitored) and blood pressure measured in the clinic. |
| White coat effect | A negative home-clinic blood pressure difference. Blood pressure measured with ABPM (or at home) is lower than the corresponding clinic blood pressure. |
| White coat hypertension | A negative home-clinic blood pressure difference. Blood pressure measured with ABPM (or at home) is <135/85mm Hg but the corresponding clinic blood pressure is ≥140/90mm Hg. |
| Masked effect | A positive home-clinic blood pressure difference. Blood pressure measured with ABPM (or at home) is higher than the corresponding clinic blood pressure. |
| Masked hypertension | A positive home-clinic blood pressure difference. Blood pressure measured with ABPM (or at home) is ≥135/85mm Hg but the corresponding clinic blood pressure is <140/90mm Hg. |
| Masked uncontrolled hypertension | A positive home-clinic blood pressure difference in patients with a previous diagnosis of hypertension. Blood pressure measured with ABPM (or at home) is ≥135/85mm Hg but the corresponding clinic blood pressure is <140/90mm Hg (incorrectly suggesting the patient is controlled). |
Abbreviation: ABPM, ambulatory blood pressure monitoring.
Clinic blood pressure monitoring is still recommended for initial screening of blood pressure in routine clinical practice,13,14 and thus, identifying those patients most likely to display a white coat or masked effect is important to avoid misdiagnosis and mismanagement of hypertension. There is a large body of literature proposing factors that predict white coat or masked hypertension,20–22 but no studies have systematically reviewed the evidence. Consequently there is little consensus as to which factors are most important or how they should be used in clinical practice to guide diagnosis and management decisions. The present study aimed to systematically review the literature and establish the most important predictors of a significant home-clinic blood pressure difference to inform interventions that might identify those with discordant clinic and ambulatory blood pressure in routine clinical practice.
METHODS
This study systematically reviewed all existing literature examining factors that predict the home-clinic blood pressure difference. The protocol is available in the Supplementary Appendix.
Search strategy
A scoping search was carried out to identify background literature and provide an estimate of the volume of literature on the topic. A search strategy (see Supplementary Appendix) was then designed for use with MEDLINE and then adapted to run across the following databases: CINAHL (EBSCO), The Cochrane (Wiley) CENTRAL Register of Controlled Trials, EMBASE (Ovid), MEDLINE (Ovid) and MEDLINE In Process (Ovid), Science Citation Index – Expanded & Conference Proceedings Citation Index – Science, and The ZETOC (Mimas) database. Searches were carried out up to and including March 2014. In order to capture as broad a range of studies as possible, no language or date limits were applied, although animal studies, letters, comments, and review articles were excluded. In addition to searches of electronic databases, reference lists of studies included in the review were checked to identify any further relevant papers.
Selection of studies and inclusion criteria
Two authors (J.P.S. and B.F.) reviewed the titles (10% independently) and abstracts (100% independently) of potentially relevant articles for inclusion. Studies were selected for full document screening and data extraction based on the following criteria:
- Included a measure out-of-office blood pressure (home or ambulatory blood pressure).
- Included a measure of clinic blood pressure.
- A cross-sectional study examining data from a single time point.
- Examined independent variables routinely available or measurable in a primary care clinic setting.
- Examined the association between these variables and the home-clinic blood pressure difference, white coat or masked hypertension (outcome variable).
- Included primary data.
The review aimed to identify factors that could be utilized by clinicians in the routine diagnosis and management of hypertension in a Primary Care setting. Thus, studies were excluded from the review if they:
- Examined patients in hospital for surgery or treatment for a specialist condition (e.g., haemodialysis, pregnancy)
- Examined measurements taken in a nonclinical or pharmacy setting.
- Studied patients aged below 18 years.
Data collection
Data were extracted from all relevant articles identified in the search strategy by J.P.S. and B.F. This included the study setting and population, basic patient demographics, clinic blood pressure, out-of-office blood pressure, and the outcome of interest (home-clinic blood pressure difference, white coat or masked effect, white coat or masked hypertension). Where a logistic regression analysis was performed examining the association between specific variables and the home-clinic blood pressure difference, relevant odds ratios (ORs) for each predictor of this difference were extracted. The form used for data extraction is available in the Supplementary Appendix.
During data extraction, the methodological quality and risk of bias of individual studies were assessed. This quality assessment covered domains of selection bias, detection bias, accuracy of measurement, analysis, and adjustment for confounding using a combination of questions from the QUADAS-223 and CASP24 checklists for the assessment of cohort studies.
Statistical analysis
The primary outcome of this review was to identify the most important factors that predict a significant home-clinic blood pressure difference. This was defined by (a) the number of studies citing specific risk factors for the home-clinic blood pressure difference, white coat or masked hypertension and (b) a pooled OR for the most commonly cited predictors of white coat or masked hypertension. This pooled estimate was based on log OR estimates and their confidence intervals (CIs) synthesized in a random-effects meta-analysis using the method of DerSimonian and Laird.25 This method allows for between-study heterogeneity in the true ORs and produces a pooled estimate and 95% CIs to summarize the association between independent predictors and white coat or masked hypertension. Where 95% CIs were not presented in an included article, they were estimated from the corresponding P values using the methods described by Altman and Bland.26
Sensitivity analyses were conducted focusing on those high quality studies that identified and corrected their analysis for confounding variables including age and sex. Where sufficient data were available, further sensitivity analyses explored the association between independent predictors and white coat or masked hypertension defined according to ambulatory blood pressure (daytime or 24 hour) or home monitoring and in subgroup populations: unselected patients and those with diagnosed hypertension (in patients with hypertension, studies examined predictors of white coat hypertension or masked uncontrolled hypertension).27
All analyses were conducted using STATA version 13.1 (MP parallel edition, StataCorp, College Station, TX). Data are presented as proportions of the total study population, means with SD or ORs with 95% CIs unless otherwise stated.
RESULTS
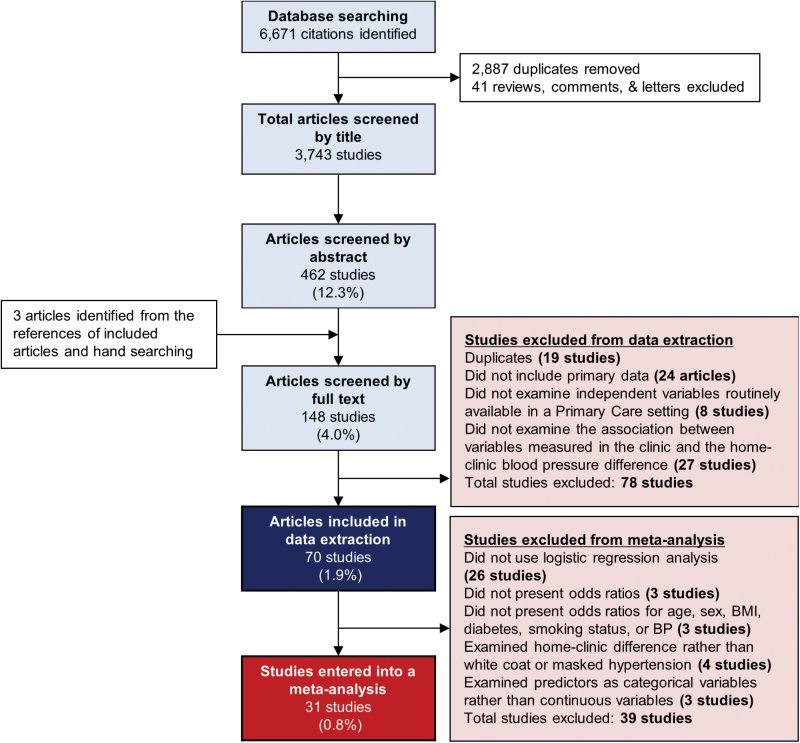
The search strategy identified 3,743 unique articles of which 70 were eligible for this review after title, abstract, and full text screening (Figure 1). Studies were conducted in 27 different countries in a community, primary care or hospital outpatient setting (Table 2). A total of 86,167 patients (mean age 54.5 years) were examined, including 40,622 females (47%) and 40,840 patients on antihypertensive treatment. Study populations varied from unselected cohorts to those with normotension, hypertension, diabetes, or chronic kidney disease.
Figure 1.
Screening and selection of studies to include in analysis of predictors of the home-clinic blood pressure difference. Abbreviations: BMI, body mass index; sBP, systolic blood pressure; dBP, diastolic blood pressure.
Table 2.
Characteristics of included studies
| Author | Year | Country | Setting | Population | Sample size | Mean age (years) | Sex (% female) | Out-of-office monitoring | Outcome of interest |
|---|---|---|---|---|---|---|---|---|---|
| Abir-Khalil et al. | 2009 | Morocco | Outpatient clinic | Admitted to cardiology unit | 2,462 | 50.5 | 58% | ABPM | White coat hypertension |
| Afsar et al. | 2013 | Turkey | Outpatient clinic | Diabetic | 102 | 48.9 | 61% | ABPM | Masked hypertension |
| Akilli et al. | 2014 | Turkey | Outpatient clinic | Diabetic | 85 | 50.7 | 41% | ABPM | Masked hypertension |
| Andalib et al. | 2010 | Canada | Primary Care | Hypertensives | 2,728 | 60.3 | 55% | Home | Masked hypertension |
| Asayama et al. | 2009 | Japan | Community | Unselected | 395 | 63.5 | 70% | Home | Masked hypertension |
| Azizi et al. | 2013 | Morocco | Outpatient clinic | Normotensives | 438 | 47.3 | 49% | ABPM | Masked hypertension |
| Bakalakou et al. | 2013 | Greece | n/a | Hypertensives | 305 | 57.2 | 59% | ABPM | Masked nocturnal hypertension |
| Barochiner et al. | 2013 | Argentina | Outpatient clinic | Hypertensives | 172 | 64.8 | 69% | Home | Masked hypertension |
| Ben-Dov et al. | 2007a | Israel | Outpatient clinic | Referred for ABPM | 3,928 | 55.1 | 53% | ABPM | Home-clinic difference |
| Ben-Dov et al. | 2007b | Israel | Outpatient clinic | Referred for ABPM | 3,957 | 54.8 | 58% | ABPM | White coat and masked hypertension |
| Bucio et al. | 2011 | Mexico | Outpatient clinic | Unselected | 49 | 40.9 | 53% | ABPM | White coat hypertension |
| Cacciolati et al. | 2011 | France | Community | Unselected | 690 | 78.8 | 65% | Home | Masked hypertension |
| Calvo-Vargas et al. | 1999 | Mexico | Outpatient clinic | n/a | 243 | 56.5 | 80 % | Home | Home-clinic difference |
| Charvat et al. | 2010 | Czech Rep. | n/a | Diabetic | 64 | — | — | ABPM | Masked hypertension |
| Dolan et al. | 2004 | Ireland | Outpatient clinic | Referred for ABPM | 5,716 | 53.6 | 53% | ABPM | White coat hypertension |
| Florian et al. | 2013 | USA | Community | Unselected | 1,652 | — | — | Home | Masked hypertension |
| Gorostidi et al. | 2013 | Spain | Primary Care/ clinic | Chronic kidney disease | 5,693 | 67.0 | 42% | ABPM | White coat and masked hypertension |
| Gualdiero et al. | 2000 | UK | Outpatient clinic | Referred for ABPM | 1,553 | 53.4 | 49% | ABPM | Home-clinic difference |
| Hanninen et al. | 2011 | Finland | Community | Unselected | 1,459 | 55.8 | 53% | Home | Masked hypertension |
| Hermida et al. | 2004 | Spain | n/a | Hypertensives | 837 | 49.5 | 51% | ABPM | Home-clinic difference |
| Hernández del Ray | 1996 | Spain | Outpatient clinic | Hypertensives | 106 | 43.0 | 52% | ABPM | White coat hypertension |
| Hiraizumi et al. | 1998 | Japan | n/a | Patients with raised office BP | 86 | — | 62% | ABPM | Home-clinic difference |
| Horikawa et al. | 2008 | Japan | Primary Care | Hypertensives | 3,308 | 66.2 | 56% | Home | Home-clinic difference |
| Hozawa et al. | 2001 | Japan | Community | Unselected | 1,789 | — | — | Home | Home-clinic difference |
| Huang et al. | 2010 | Taiwan | Outpatient clinic | Hypertensives | 121 | 45.7 | 37% | ABPM | Home-clinic difference |
| Hwang et al. | 2007 | Korea | Outpatient clinic | Referred for ABPM | 967 | 51.9 | 48% | ABPM | White coat and masked hypertension |
| Iimuro et al. | 2013 | Japan | Outpatient clinic | Chronic kidney disease | 1,075 | 60.7 | 37% | ABPM | Home-clinic difference |
| Ishikawa et al. | 2007 | Japan | Outpatient clinic | Hypertensives | 405 | 66.9 | 45% | Home | Masked (morning) hypertension |
| Jhalani et al. | 2005 | USA | Outpatient clinic | Hypertensives | 226 | 52.0 | 53% | ABPM | Home-clinic difference |
| Kabutoya et al. | 2009 | Japan | Outpatient clinic | Hypertensives | 969 | 66.5 | 58% | Home | Home-clinic difference |
| Kayrak et al. | 2010 | Turkey | Outpatient clinic | Ungoing exercise testing | 61 | 47.3 | 21% | ABPM | Masked hypertension |
| Kim et al. | 2011 | Korea | Community | Normotensives | 84 | 33.1 | 37% | ABPM | Masked hypertension |
| Koupil et al. | 2005 | Sweden | Community | Unselected (aged ~70 years) | 736 | 70.9 | 0% | ABPM | White coat and masked hypertension |
| Labinson et al. | 2008 | USA | Primary Care | Patients with raised office BP | 65 | 54.0 | 55% | ABPM | Home-clinic difference |
| Lee et al. | 2008 | Korea | Primary Care | Hypertensives | 4,435 | 57.1 | 51% | Home | Masked hypertension |
| Lerman et al. | 1989 | USA | Primary Care | Hypertensives | 98 | 54.6 | 43% | ABPM | Home-clinic difference |
| Lindbaek et al. | 2003 | Norway | Primary Care | Suspected/treated hypertension | 221 | 58.0 | 48% | ABPM | Home-clinic difference |
| MacDonald et al. | 1999 | Canada | Outpatient clinic | Hypertensives | 103 | 59.3 | 47% | ABPM | White coat hypertension |
| Mallion et al. | 2006 | France | Primary Care | Hypertensives | 1,150 | 69.0 | 63% | Home | Masked hypertension |
| Manios et al. | 2008 | Greece | Outpatient clinic | Unselected | 2,004 | 50.9 | 53% | ABPM | Home-clinic difference |
| Mansoor et al. | 1996 | USA | Outpatient clinic | Hypertensives | 64 | 56.0 | 64% | ABPM | Home-clinic difference |
| Markis et al. | 2009 | Greece | Outpatient clinic | Unselected | 254 | 55.0 | 60% | ABPM | Masked hypertension |
| Martinez et al. | 1999 | Spain | Primary Care | Hypertensives | 345 | 51.8 | 52% | ABPM | White coat hypertension |
| Nasothimiou et al. | 2012 | Greece | Outpatient clinic | Referred for ABPM | 613 | 53.0 | 43% | ABPM/Home | White coat and masked hypertension |
| Niiranen et al. | 2006 | Finland | Community | Unselected | 1,440 | 55.0 | 53% | Home | White coat hypertension |
| Obara et al. | 2005 | Japan | Primary Care | Hypertensives | 3,400 | 66.2 | 55% | Home | White coat and masked hypertension |
| Parati et al. | 2012 | Worldwide | Outpatient clinic | Unselected | 9,753 | 56.0 | 51% | ABPM | Masked hypertension |
| Park et al. | 2011 | Korea | Outpatient clinic | Hypertensives | 511 | 57.2 | 55% | Home | Masked hypertension |
| Rassmussen et al. | 1998 | Denmark | Outpatient clinic | Unselected | 1,855 | — | 48% | ABPM | Home-clinic difference |
| Rodrigues et al. | 2009 | Brazil | n/a | Diabetic | 566 | 49.1 | 47% | ABPM | Home-clinic difference |
| Sandvik et al. | 1998 | Norway | Primary Care | Hypertensives | 75 | 50.1 | 65% | Home | White coat hypertension |
| Schoenthaler et al. | 2010 | USA | Community | Normotensives | 240 | 35.9 | 61% | ABPM | (Marked) masked hypertension |
| Sheppard et al. | 2014 | UK | Primary Care | Hypertensives | 220 | 67.0 | 53% | Home | White coat/masked effect |
| Smirnova et al. | 2009 | Russia | n/a | Hypertensives | 39 | 53.7 | 51% | ABPM | Home-clinic difference |
| Sobrino et al. | 2013 | Spain | Outpatient clinic | Normotensives | 485 | 43.1 | 55% | ABPM | Masked hypertension |
| Sobrino et al. | 2011 | Spain | Outpatient clinic | Hypertensives | 302 | 56.2 | 56% | ABPM | Masked hypertension |
| Spruill et al. | 2007 | USA | Outpatient clinic | Unselected | 214 | 51.7 | 55% | ABPM | Home-clinic difference |
| Streitel et al. | 2011 | USA | Outpatient clinic | Unselected | 252 | 45.2 | 53% | ABPM | Home-clinic difference |
| Sung et al. | 2013 | Taiwan | Community | Unselected | 1,257 | 53.0 | 47% | ABPM | Home-clinic difference |
| Tam et al. | 2007 | Hong Kong | Primary Care | Referred for ABPM | 617 | 52.9 | — | ABPM | White coat hypertension |
| Tardif et al. | 2009 | Canada | Primary Care | Hypertensives | 3,247 | — | — | Home | Masked hypertension |
| Thomas et al. | 2012 | UK | Outpatient clinic | Unselected | 2,381 | 56.0 | 53% | ABPM | Home-clinic difference |
| Trudel et al. | 2009 | Canada | Community | Unselected | 2,370 | 44.0 | 61% | ABPM | White coat and masked hypertension |
| Tsai et al. | 2003 | Taiwan | n/a | Unselected | 41 | 42.6 | 59% | ABPM | Home-clinic difference |
| Uze et al. | 2012 | Japan | Outpatient clinic | Diabetic | 193 | 62.7 | 55% | ABPM | Masked hypertension |
| Verdecchia et al. | 2001 | Italy | Outpatient clinic | Hypertensives | 1,546 | 39.0 | 34% | ABPM | White coat hypertension |
| Wang et al. | 2007 | China | Community | Unselected | 694 | 48.5 | 54% | ABPM | White coat and masked hypertension |
| Wing et al. | 2002 | Australia | Primary Care | Hypertensives | 713 | 72.0 | 47% | ABPM | Masked hypertension |
| Yoon et al. | 2012 | Korea | Outpatient clinic | Hypertensives | 1,087 | 57.0 | 52% | Home | Home-clinic difference |
| Zhou et al. | 2013 | China | Outpatient clinic | Diabetic | 856 | 45.1 | 45% | ABPM | Masked hypertension |
References mentioned in the table are found in the Supplementary Appendix.
Abbreviations: ABPM, ambulatory blood pressure monitoring; Home, home blood pressure monitoring; BP, blood pressure.
Included studies varied in methodological quality with sampling strategies and the representativeness of the study population described in only 21/70 studies (Supplementary Table 2). Most studies (55/57) defined the threshold for white coat or masked hypertension (where appropriate) and examined the home-clinic blood pressure difference as the primary focus of the study (68/70). Forty-six studies identified important confounding variables and 44 of these corrected for this confounding in their analysis. Full details of the multivariate analysis conducted in each study are given in Supplementary Table 3).
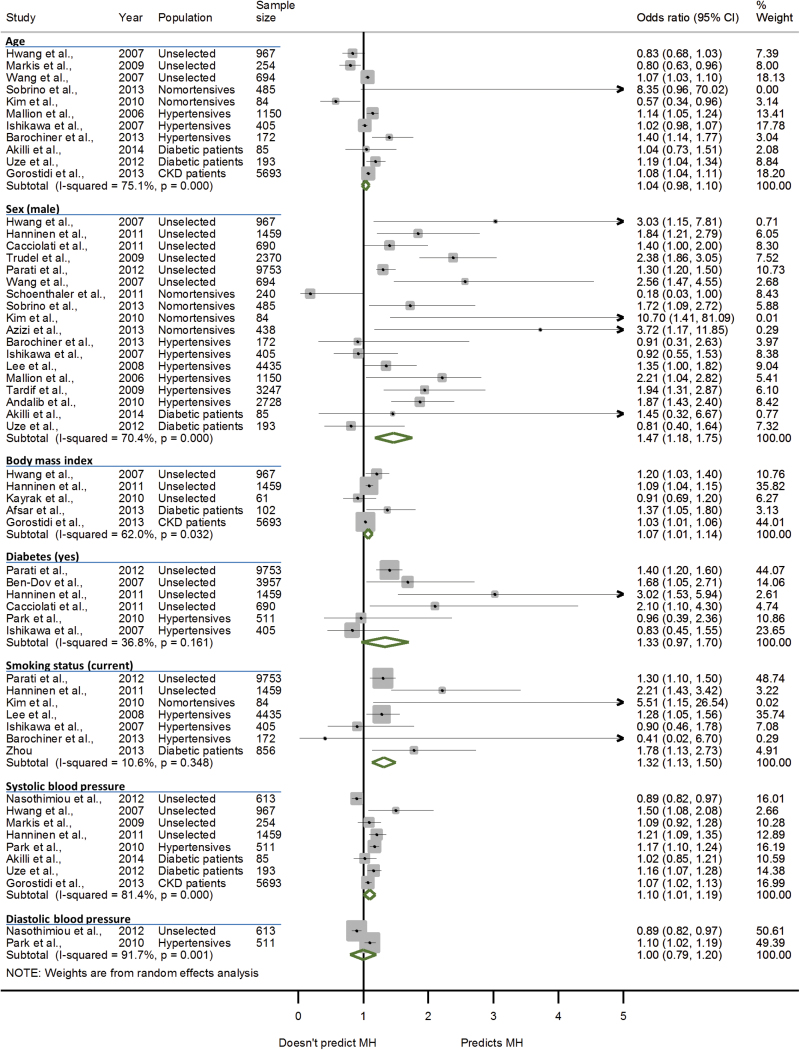
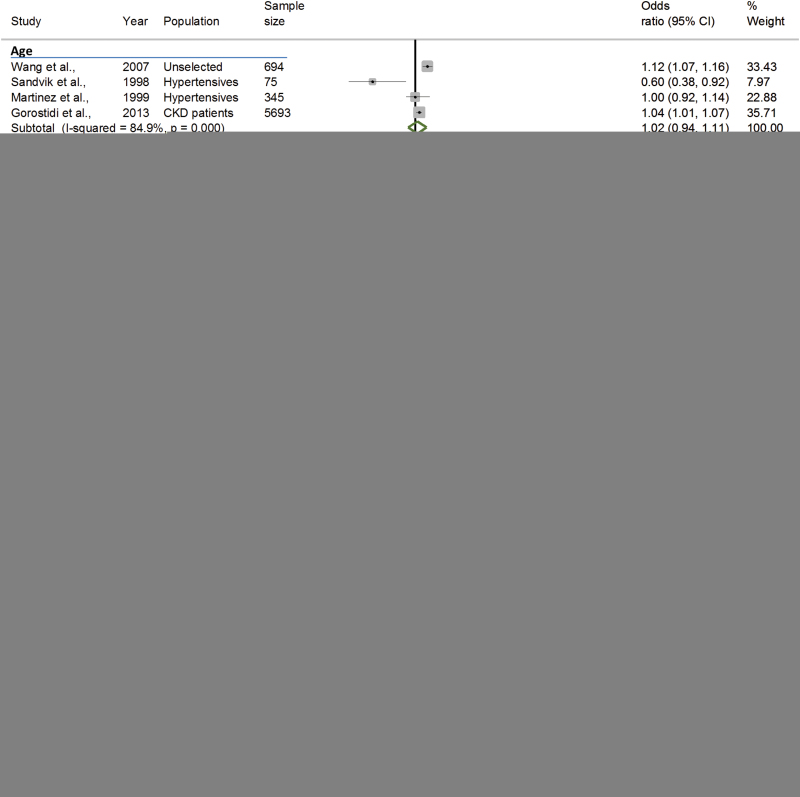
Included studies reported a total of 60 significant predictors of the home-clinic blood pressure difference, white coat or masked hypertension. The most commonly cited predictors of the home-clinic blood pressure difference were sex (14 studies), age (11 studies), body mass index (BMI, 7 studies), and systolic (12 studies) and diastolic blood pressure (5 studies) (Supplementary Table 4). These factors were also commonly cited as predictors of both white coat and masked hypertension with the addition of diabetes and smoking status (Tables 3 and 4). The overall association between these factors and white coat or masked hypertension was established by pooling ORs for each predictor from 31 studies in a random-effects meta-analysis. Male sex (OR 1.47, 95% CI 1.18–1.75), increasing BMI (per kg/m2 increase, OR 1.07, 95% CI 1.01–1.14), current smoking status (OR 1.32, 95% CI 1.13–1.50), and systolic clinic blood pressure (per 1mm Hg increase, OR 1.10, 95% CI 1.01–1.19) were all found to be significant predictors of masked hypertension (Figure 2). Male sex was found to be predictive of not having white coat hypertension (OR 0.57, 95% CI 0.42–0.72) (Figure 3): analyzed with male sex as the reference, female sex was a significant predictor of white coat hypertension (OR 3.38, 95% CI 1.64–6.96). The heterogeneity between studies for sex (I 2 = 70.4% (masked hypertension); I 2 = 75.7% (white coat hypertension)), BMI (I 2 = 62.0%), and systolic blood pressure (I 2 = 81.4%) predictors of white coat and masked hypertension was significant (P < 0.05).
Table 3.
Predictors of masked hypertension reported in included studies (n = 34)
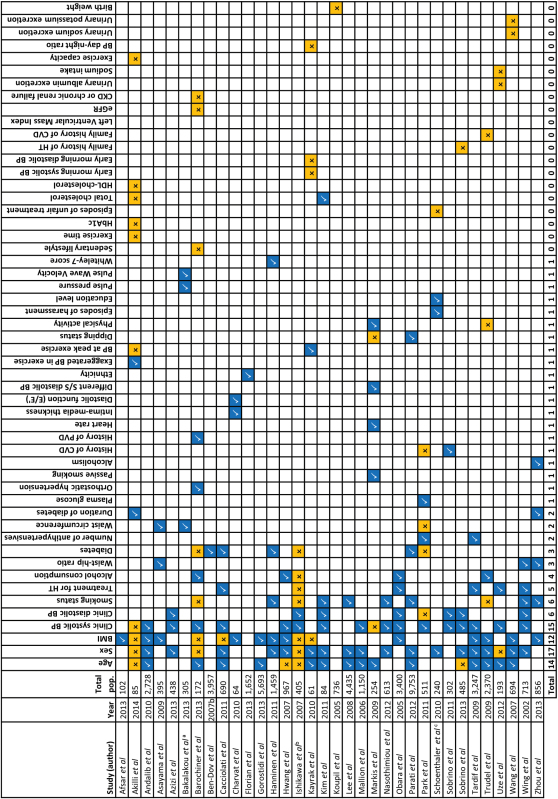
|
Last row indicates total number of studies citing each factor as a significant predictor of masked hypertension. References mentioned in the table are found in the Supplementary Appendix.
Abbreviations: CVD, cardiovascular disease; PVD, peripheral vascular disease; BP, blood pressure; eGFR, estimated glomerular filtration rate; CKD, chronic kidney disease; HT, hypertension; BMI, body mass index.
aExamined masked nocturnal hypertension as the outcome. bExamined masked morning hypertension as the outcome. cExamined “marked” masked hypertension as the outcome.
Significant predictor.
Nonsignificant predictor.
Significant predictor defined as an OR or ß coefficient with an associated P value of <0.05.
Table 4.
Predictors of white coat hypertension reported in included studies (n = 18)

|
Last row indicates total number of studies citing each factor as a significant predictor of masked hypertension. References mentioned in the table are found in the Supplementary Appendix.
Abbreviations: CVD, cardiovascular disease; BP, blood pressure; BMI, body mass index.
aExamined using the Centre for Epidemiological Studies Depression Scale.
Significant predictor.
Nonsignificant predictor.
Significant predictor defined as an OR or ß coefficient with an associated P value of <0.05.
Figure 2.
Forest-plot showing pooled odds ratio estimates for the 7 most commonly cited predictors of masked hypertension. Abbreviations: MH, masked hypertension; CKD, chronic kidney disease. Binary predictors were defined using Female sex, no diabetes, and nonsmoker as the reference values (respectively). Continuous predictors were defined as increases in age per 10 years, BMI per 1kg/m2 and systolic/diastolic blood pressure per 1mm Hg.
Figure 3.
Forest-plot showing pooled odds ratio estimates for the 7 most commonly cited predictors of white coat hypertension. WCH, white coat hypertension; CKD, chronic kidney disease. Binary predictors were defined using female sex, no diabetes, and nonsmoker as the reference values (respectively). Continuous predictors were defined as increases in age per 10 years, BMI per 1kg/m2, and systolic/diastolic blood pressure per 1mm Hg.
Sensitivity analysis
Inclusion of only those studies that used ambulatory blood pressure to define masked hypertension resulted in diabetes becoming a significant predictor (OR 1.42, 95% CI 1.22–1.61) but BMI and systolic blood pressure no longer being predictive. When only studies that used home blood pressure to define masked hypertension were included, only sex remained a significant predictor, although there were insufficient studies to examine the relationship between BMI and masked hypertension. Using ambulatory blood pressure or home blood pressure to define white coat hypertension had no impact on the findings of the primary analysis although there were no longer sufficient data to examine the association with diabetes, smoking status and diastolic blood pressure (studies using ambulatory blood pressure), or age, BMI, and systolic and diastolic blood pressure (studies using home blood pressure). Similar findings were observed in the sensitivity analysis excluding low quality studies that did not account for confounding variables.
In an unselected population, male sex and diabetes were predictive of masked hypertension (OR 1.76, 95% CI 1.29–2.24 (sex); OR 1.48, 95% CI 1.22–1.70 (diabetes)), while in hypertensive patients, only male sex remained significant (OR 1.52, 95% CI 1.11–1.93) for masked uncontrolled hypertension, although there were no longer sufficient data to examine the association with systolic and diastolic blood pressure. Examining only patients from an unselected population, male sex was predictive of not having white coat hypertension (OR 0.47, 95% CI 0.33–0.61) and systolic blood pressure was predictive of having white coat hypertension (OR 1.06, 95% CI 1.04–1.08). In hypertensive patients, male sex remained predictive of not having white coat hypertension (OR 0.62, 95% CI 0.48–0.76), although again, insufficient data were available to examine associations with BMI and systolic or diastolic blood pressure. The observed heterogeneity was not reduced in any sensitivity analyses examining studies by outcome measurement, sample populations, or methodological quality.
DISCUSSION
This study has systematically reviewed all existing literature evaluating the association between patient characteristics and the home-clinic blood pressure difference. A large number of studies were identified examining a number of common factors which predict the home-clinic blood pressure difference or white coat or masked hypertension. Meta-analyses of the most commonly cited predictors revealed that sex, BMI, smoking status, and systolic blood pressure level were the most important predictors, although these associations were mediated by the method of out-of-office blood pressure monitoring and the population studied. There is scope to incorporate such predictors into a clinical prediction tool which could be used to identify those patients more likely to display a significant masked or white coat effect and therefore better target the use of out-of-office blood pressure monitoring in routine clinical practice.
Strengths and limitations
This is the largest systematic review to date of studies examining the association between patient factors and the home-clinic blood pressure difference. An extensive search strategy was used in multiple research literature databases to comprehensively capture all published articles relating to the study research question. Not all of the identified studies were directly comparable due to a lack of relevant data or the use of different statistical methods in the original study analyses. Thus, only 31/70 studies could be included in the meta-analysis. While sufficient data were available to analyze the primary outcome of this review, the lower number of studies eligible for meta-analysis meant some sensitivity and subgroup analyses were not possible. For instance, previous studies have suggested that the degree of white coat or masked effect may be affected by attributes of the person taking the clinic blood pressure measurement.28 Although an attempt was made to extract details of the person taking clinic blood pressure from each included study, many did not report this or used both doctors and nurses to take readings without distinguishing between the 2, meaning a subgroup analysis by the type of person taking the clinic measurement was not possible.
The methodological quality of studies and the population of study varied widely between included studies and this may have contributed to the observed statistical heterogeneity. Indeed, the significant predictors of masked hypertension changed in sensitivity analyses excluding low quality studies that did not correct for confounding variables, although the statistical heterogeneity between studies remained significant. Only sex remained a significant predictor of both white coat and masked hypertension across patient populations and study quality.
Comparison with previous literature
A number of previous reviews20–22 and clinical guidelines14 have discussed possible predictors of white coat and masked hypertension. Indeed, the present review demonstrates that the literature is becoming saturated with studies describing predictors of white coat or masked hypertension. Despite the large volume of articles studying this topic, little insight has been gained over the last 20 years and the patient factors commonly cited as significant predictors of the home-clinic blood pressure difference remain the same: age, sex, BMI, smoking status, and clinic blood pressure level.
Recent studies have examined the influence of patient ethnicity on the home-clinic blood pressure difference. Martin et al., 29 studied 770 individuals of White British, South Asian, or African-Caribbean ethnicity and found that when clinic blood pressure was defined using a single reading, non-hypertensive South Asian or African-Caribbean patients displayed less of a home-clinic blood pressure difference compared to White British patients. In contrast, hypertensive patients of South Asian or African-Caribbean origin had a greater home-clinic difference. The present review found only 2 studies examining ethnicity as a predictor of the home-clinic blood pressure difference30,31 and neither could be included in the meta-analysis. However, the recent Jackson Heart study32 (published after the searches in the present study were conducted) examined a population of 972 African-Americans and found male sex, current smoking status, diabetes, prescribed medication, and clinic blood pressure were significant predictors of masked hypertension. These findings are similar to those of the present review and suggest that our findings may be applicable to some ethnic minority groups.
This is the first systematic review to summarize all available evidence and present pooled estimates describing the most important predictors of white coat and masked hypertension. Seventy studies fulfilled our strict inclusion criteria and 60 different predictors of the home-clinic blood pressure difference were identified. It is unclear from the data included in this review as to why certain factors predict a white coat or masked effect to a greater degree than others. However, it is of interest that, in our analysis, significant predictors appeared to be related to the underlying cardiovascular disease risk associated with each condition: masked hypertension (associated with high cardiovascular disease risk)18,19 was more common in patients with characteristics associated with increased cardiovascular risk such as male sex, current smoking status, increasing BMI, and increasing blood pressure.33,34 White coat hypertension (associated with lower cardiovascular disease risk)18,19 was associated with female sex, which is also associated with lower cardiovascular disease risk (compared to male sex).33,34
Implications for clinical practice
It is important to identify patients with white coat and masked hypertension because failure to do so can result in significant misdiagnosis and mismanagement of hypertension.35 Those with white coat hypertension may be prescribed therapy when they do not need it while patients with masked hypertension are likely to be denied potentially beneficial treatment.15 Despite the large number of studies citing predictors of white coat and masked hypertension identified in this review, few have proposed a practical method for screening patients in routine clinical practice.21 Indeed, screening for white coat or masked hypertension is only useful if it reduces the number of patients potentially eligible for out-of-office monitoring. The number of predictive factors identified in this review makes their use to guide targeting of out-of-office monitoring impractical because a significant proportion of patients attending routine clinical practice are likely to present with at least one of these characteristics.
Some previous studies have suggested methods for targeted use of ABPM, mostly suggesting specific clinic blood pressure thresholds to target monitoring.36,37 Viera et al. 38 examined optimal clinic blood pressure levels for referral for ambulatory monitoring in patients with normal clinic pressure for detection of masked hypertension. They identified a threshold of greater than 120/82mm Hg as optimal but concluded that using clinic blood pressure alone was not an effective method of triaging for out-of-office monitoring because of high referral rates and moderate specificity. They suggested that a combination of factors, perhaps such as those identified in the present review, might be more effective at targeting ABPM efficiently.
The European Society of Hypertension14 suggests that practicing physicians consider screening for masked hypertension in high risk patients with normal clinic blood pressure, or screening for white coat hypertension in low risk patients with raised clinic blood pressure. This is still likely to result in a large number of patients being indicated for out-of-office blood pressure monitoring and future work should therefore focus on developing a single, practical, decision aid for targeted screening of white coat or masked hypertension, incorporating all of the significant predictors identified in this review.
There are a number of common patient characteristics that predict the home-clinic blood pressure difference including sex, current smoking status, increasing BMI, and increasing systolic blood pressure. There is scope to incorporate such predictors into a clinical prediction tool which could be used to identify those patients displaying a significant masked or white coat effect in routine clinical practice. Identification of such patients could help to better target antihypertensive treatment at those people with the most to gain.
DISCLOSURE
R.J.M. has received research funding from Omron and Lloyds Pharmacies in terms of blood pressure monitoring equipment. All other authors declared no conflict of interest.
Supplementary Material
ACKNOWLEDGMENTS
We thank Dr Ignacio Ricci-Cabello for his assistance in translating the Spanish language articles identified in this review and Dr Richard Stevens and Dr Jason Oke for their statistical support.
Contributors: J.P.S. and R.J.M. had the original idea. N.R. designed the search strategy with J.P.S. and undertook the literature review. J.P.S. and B.F. screened the articles for inclusion and completed the data extraction. J.P.S. conducted the analyses and wrote the first draft. All authors subsequently refined the manuscript and approved the final version. J.P.S. is the guarantor.
Funding: This work was funded by a Medical Research Council Strategic Skills Post-doctoral Fellowship held by J.P.S. (MR/K022032/1), with support from a National Institute for Health Research (NIHR) Programme Grant (RP-PG-1209–10051). R.J.M. holds an NIHR Professorship. The views and opinions expressed are those of the authors and do not necessarily reflect those of the MRC, NHS, NIHR, or the Department of Health.
Ethical approval: Ethical approval was not required to conduct this review.
Data sharing: Proposals for data sharing should be made to the corresponding author.
REFERENCES
- 1. Lewington S, Clarke R, Qizilbash N, Peto R, Collins R. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet 2002; 360:1903–1913. [DOI] [PubMed] [Google Scholar]
- 2. Ezzati M, Lopez AD, Rodgers A, Vander Hoorn S, Murray CJ. Selected major risk factors and global and regional burden of disease. Lancet 2002; 360:1347–1360. [DOI] [PubMed] [Google Scholar]
- 3. Staessen JA, Thijs L, Fagard R, O’Brien ET, Clement D, de Leeuw PW, Mancia G, Nachev C, Palatini P, Parati G, Tuomilehto J, Webster J. Predicting cardiovascular risk using conventional vs ambulatory blood pressure in older patients with systolic hypertension. Systolic Hypertension in Europe Trial Investigators. JAMA 1999; 282:539–546. [DOI] [PubMed] [Google Scholar]
- 4. Ohkubo T, Hozawa A, Nagai K, Kikuya M, Tsuji I, Ito S, Satoh H, Hisamichi S, Imai Y. Prediction of stroke by ambulatory blood pressure monitoring versus screening blood pressure measurements in a general population: the Ohasama study. J Hypertens 2000; 18:847–854. [DOI] [PubMed] [Google Scholar]
- 5. Mancia G, Zanchetti A, Agabiti-Rosei E, Benemio G, De Cesaris R, Fogari R, Pessina A, Porcellati C, Rappelli A, Salvetti A, Trimarco B. Ambulatory blood pressure is superior to clinic blood pressure in predicting treatment-induced regression of left ventricular hypertrophy. SAMPLE Study Group. Study on ambulatory monitoring of blood pressure and lisinopril evaluation. Circulation 1997; 95:1464–1470. [DOI] [PubMed] [Google Scholar]
- 6. Imai Y, Ohkubo T, Sakuma M, Tsuji II, Satoh H, Nagai K, Hisamichi S, Abe K. Predictive power of screening blood pressure, ambulatory blood pressure and blood pressure measured at home for overall and cardiovascular mortality: a prospective observation in a cohort from Ohasama, northern Japan. Blood Press Monit 1996; 1:251–254. [PubMed] [Google Scholar]
- 7. Fagard RH, Staessen JA, Thijs L. Prediction of cardiac structure and function by repeated clinic and ambulatory blood pressure. Hypertension 1997; 29:22–29. [DOI] [PubMed] [Google Scholar]
- 8. Schettini C, Bianchi M, Nieto F, Sandoya E, Senra H. Ambulatory blood pressure: normality and comparison with other measurements. Hypertension Working Group. Hypertension 1999; 34:818–825. [DOI] [PubMed] [Google Scholar]
- 9. Rasmussen SL, Torp-Pedersen C, Borch-Johnsen K, Ibsen H. Normal values for ambulatory blood pressure and differences between casual blood pressure and ambulatory blood pressure: results from a Danish population survey. J Hypertens 1998; 16:1415–1424. [DOI] [PubMed] [Google Scholar]
- 10. Mancia G, Sega R, Bravi C, De Vito G, Valagussa F, Cesana G, Zanchetti A. Ambulatory blood pressure normality: results from the PAMELA study. J Hypertens 1995; 13(12 Pt 1):1377–1390. [PubMed] [Google Scholar]
- 11. Bjorklund K, Lind L, Lithell H. Twenty-four hour ambulatory blood pressure in a population of elderly men. J Intern Med 2000; 248:501–510. [DOI] [PubMed] [Google Scholar]
- 12. Pickering TG, Coats A, Mallion JM, Mancia G, Verdecchia P. Blood Pressure Monitoring. Task Force V: white-coat hypertension. Blood Press Monit 1999; 4:333–341. [DOI] [PubMed] [Google Scholar]
- 13. National Clinical Guideline C. National Institute for Health and Clinical Excellence Guidance CG127. Hypertension: The Clinical Management of Primary Hypertension in Adults: Update of Clinical Guidelines 18 and 34. Royal College of Physicians (UK): London, 2011. [PubMed] [Google Scholar]
- 14. Mancia G, Fagard R, Narkiewicz K, Redon J, Zanchetti A, Bohm M, Christiaens T, Cifkova R, De Backer G, Dominiczak A, Galderisi M, Grobbee DE, Jaarsma T, Kirchhof P, Kjeldsen SE, Laurent S, Manolis AJ, Nilsson PM, Ruilope LM, Schmieder RE, Sirnes PA, Sleight P, Viigimaa M, Waeber B, Zannad F, Redon J, Dominiczak A, Narkiewicz K, Nilsson PM, Burnier M, Viigimaa M, Ambrosioni E, Caufield M, Coca A, Olsen MH, Schmieder RE, Tsioufis C, van de Borne P, Zamorano JL, Achenbach S, Baumgartner H, Bax JJ, Bueno H, Dean V, Deaton C, Erol C, Fagard R, Ferrari R, Hasdai D, Hoes AW, Kirchhof P, Knuuti J, Kolh P, Lancellotti P, Linhart A, Nihoyannopoulos P, Piepoli MF, Ponikowski P, Sirnes PA, Tamargo JL, Tendera M, Torbicki A, Wijns W, Windecker S, Clement DL, Coca A, Gillebert TC, Tendera M, Rosei EA, Ambrosioni E, Anker SD, Bauersachs J, Hitij JB, Caulfield M, De Buyzere M, De Geest S, Derumeaux GA, Erdine S, Farsang C, Funck-Brentano C, Gerc V, Germano G, Gielen S, Haller H, Hoes AW, Jordan J, Kahan T, Komajda M, Lovic D, Mahrholdt H, Olsen MH, Ostergren J, Parati G, Perk J, Polonia J, Popescu BA, Reiner Z, Ryden L, Sirenko Y, Stanton A, Struijker-Boudier H, Tsioufis C, van de Borne P, Vlachopoulos C, Volpe M, Wood DA. 2013 ESH/ESC guidelines for the management of arterial hypertension: the Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J 2013; 34:2159–2219. [DOI] [PubMed] [Google Scholar]
- 15. Pickering TG, Davidson K, Gerin W, Schwartz JE. Masked hypertension. Hypertension 2002; 40:795–796. [DOI] [PubMed] [Google Scholar]
- 16. Sega R, Trocino G, Lanzarotti A, Carugo S, Cesana G, Schiavina R, Valagussa F, Bombelli M, Giannattasio C, Zanchetti A, Mancia G. Alterations of cardiac structure in patients with isolated office, ambulatory, or home hypertension: data from the general population (Pressione Arteriose Monitorate E Loro Associazioni [PAMELA] Study). Circulation 2001; 104:1385–1392. [DOI] [PubMed] [Google Scholar]
- 17. Liu JE, Roman MJ, Pini R, Schwartz JE, Pickering TG, Devereux RB. Cardiac and arterial target organ damage in adults with elevated ambulatory and normal office blood pressure. Ann Intern Med 1999; 131:564–572. [DOI] [PubMed] [Google Scholar]
- 18. Ohkubo T, Kikuya M, Metoki H, Asayama K, Obara T, Hashimoto J, Totsune K, Hoshi H, Satoh H, Imai Y. Prognosis of “masked” hypertension and “white-coat” hypertension detected by 24-h ambulatory blood pressure monitoring 10-year follow-up from the Ohasama study. J Am Coll Cardiol 2005; 46:508–515. [DOI] [PubMed] [Google Scholar]
- 19. Mancia G, Facchetti R, Bombelli M, Grassi G, Sega R. Long-term risk of mortality associated with selective and combined elevation in office, home, and ambulatory blood pressure. Hypertension 2006; 47:846–853. [DOI] [PubMed] [Google Scholar]
- 20. Peacock J, Diaz KM, Viera AJ, Schwartz JE, Shimbo D. Unmasking masked hypertension: prevalence, clinical implications, diagnosis, correlates and future directions. J Hum Hypertens 2014; 28:521–528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Yano Y, Bakris GL. Recognition and management of masked hypertension: a review and novel approach. J Am Soc Hypertens 2013; 7:244–252. [DOI] [PubMed] [Google Scholar]
- 22. Verdecchia P, O’Brien E, Pickering T, Staessen JA, Parati G, Myers M, Palatini P. When can the practicing physician suspect white coat hypertension? Statement from the Working Group on Blood Pressure Monitoring of the European Society of Hypertension. Am J Hypertens 2003; 16:87–91. [DOI] [PubMed] [Google Scholar]
- 23. Whiting PF, Rutjes AW, Westwood ME, Mallett S, Deeks JJ, Reitsma JB, Leeflang MM, Sterne JA, Bossuyt PM. QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med 2011; 155 :529–536. [DOI] [PubMed] [Google Scholar]
- 24. Critical Appraisal Skills Programme (CASP). Cohort Study Checklist. CASP UK; 2013. <http://www.casp-uk.net/>.
- 25. DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials 1986; 7:177–188. [DOI] [PubMed] [Google Scholar]
- 26. Altman DG, Bland JM. How to obtain the confidence interval from a P value. BMJ (Clinical Research Ed) 2011; 343:d2090. [DOI] [PubMed] [Google Scholar]
- 27. Banegas JR, Ruilope LM, de la Sierra A, de la Cruz JJ, Gorostidi M, Segura J, Martell N, Garcia-Puig J, Deanfield J, Williams B. High prevalence of masked uncontrolled hypertension in people with treated hypertension. Eur Heart J 2014; 35:3304–3312. [DOI] [PubMed] [Google Scholar]
- 28. Clark CE, Horvath IA, Taylor RS, Campbell JL. Doctors record higher blood pressures than nurses: systematic review and meta-analysis. Br J Gen Prac 2014; 64:e223–e232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Martin U, Haque MS, Wood S, Greenfield SM, Gill PS, Mant J, Mohammed MA, Heer G, Johal A, Kaur R, Schwartz C, McManus RJ. Ethnicity and differences between clinic and ambulatory blood pressure measurements. Am J Hypertens 2015; 28:729–738. [DOI] [PubMed] [Google Scholar]
- 30. Thomas O, Day K, Martin U, Thomas M, Dasgupta I. White coat hypertension in treated hypertensive patients and factors influencing it. J Hum Hypertens 2012; 26:618. [Google Scholar]
- 31. Gualdiero P, Niebauer J, Addison C, Clark SJ, Coats AJ. Clinical features, anthropometric characteristics, and racial influences on the ‘white-coat effect’ in a single-centre cohort of 1553 consecutive subjects undergoing routine ambulatory blood pressure monitoring. Blood Press Monit 2000; 5:53–57. [PubMed] [Google Scholar]
- 32. Diaz KM, Veerabhadrappa P, Brown MD, Whited MC, Dubbert PM, Hickson DA. Prevalence, determinants, and clinical significance of masked hypertension in a population-based sample of African Americans: the Jackson Heart Study. Am J Hypertens 2015; 28:900–908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Anderson KM, Odell PM, Wilson PW, Kannel WB. Cardiovascular disease risk profiles. Am Heart J 1991; 121:293–298. [DOI] [PubMed] [Google Scholar]
- 34. Hippisley-Cox J, Coupland C, Vinogradova Y, Robson J, Minhas R, Sheikh A, Brindle P. Predicting cardiovascular risk in England and Wales: prospective derivation and validation of QRISK2. BMJ (Clinical Research Ed) 2008; 336:1475–1482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Lovibond K, Jowett S, Barton P, Caulfield M, Heneghan C, Hobbs FD, Hodgkinson J, Mant J, Martin U, Williams B, Wonderling D, McManus RJ. Cost-effectiveness of options for the diagnosis of high blood pressure in primary care: a modelling study. Lancet 2011; 378:1219–1230. [DOI] [PubMed] [Google Scholar]
- 36. Godwin M, Birtwhistle R, Delva D, Lam M, Casson I, MacDonald S, Seguin R. Manual and automated office measurements in relation to awake ambulatory blood pressure monitoring. Fam Pract 2011; 28: 110–117. [DOI] [PubMed] [Google Scholar]
- 37. Myers MG. A proposed algorithm for diagnosing hypertension using automated office blood pressure measurement. J Hypertens 2010; 28:703–708. [DOI] [PubMed] [Google Scholar]
- 38. Viera AJ, Lin FC, Tuttle LA, Shimbo D, Diaz KM, Olsson E, Stankevitz K, Hinderliter AL. Levels of office blood pressure and their operating characteristics for detecting masked hypertension based on ambulatory blood pressure monitoring. Am J Hypertens 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.