Abstract
Background
Nipah virus (NiV), a zoonotic pathogen causing severe respiratory illness and encephalitis in humans, emerged in Malaysia in 1998 with subsequent outbreaks on an almost annual basis since 2001 in parts of the Indian subcontinent. The high case fatality rate, human-to-human transmission, wide-ranging reservoir distribution and lack of licensed intervention options are making NiV a serious regional and potential global public health problem. The objective of this study was to develop a fast-acting, single-dose NiV vaccine that could be implemented in a ring vaccination approach during outbreaks.
Methods
In this study we have designed new live-attenuated vaccine vectors based on recombinant vesicular stomatitis viruses (rVSV) expressing NiV glycoproteins (G or F) or nucleoprotein (N) and evaluated their protective efficacy in Syrian hamsters, an established NiV animal disease model. We further characterized the humoral immune response to vaccination in hamsters using ELISA and neutralization assays and performed serum transfer studies.
Results
Vaccination of Syrian hamsters with a single dose of the rVSV vaccine vectors resulted in strong humoral immune responses with neutralizing activities found only in those animals vaccinated with rVSV expressing NiV G or F proteins. Vaccinated animals with neutralizing antibody responses were completely protected from lethal NiV disease, whereas animals vaccinated with rVSV expressing NiV N showed only partial protection. Protection of NiV G or F vaccinated animals was conferred by antibodies, most likely the neutralizing fraction, as demonstrated by serum transfer studies. Protection of N-vaccinated hamsters was not antibody-dependent indicating a role of adaptive cellular responses for protection.
Conclusions
The rVSV vectors expressing Nipah virus G or F are prime candidates for new ‘emergency vaccines’ to be utilized for NiV outbreak management.
Keywords: Nipah virus, Vaccines, Recombinant vesicular stomatitis virus, Humoral immune responses, Neutralizing antibodies, Serum transfer
1. Introduction
Nipah virus (NiV; family Paramyxoviridae, genus Henipavirus) was discovered to be the causative agent of an outbreak of viral encephalitis in pig farmers in Malaysia in 1998. This initial large outbreak has been followed by smaller nearly annual outbreaks in Bangladesh and India [1,2]. Disease in humans is characterized by respiratory distress and/or encephalitis, with histopathologic changes in the lung and brain showing multinucleated giant cells throughout the microvasculature [1-3]. NiV is highly pathogenic in humans and has reached up to 100% case fatality rates (average 70%) [4]. Transmission of NiV from its natural reservoir, Pteropus fruit bats, to pigs and humans has been documented, as well as human-to-human transmission [5-7].
Currently there are no approved vaccines or therapeutics for human use against NiV infections. Although a public health concern to regional, national and even international authorities, a widespread campaign to vaccinate a large percentage of the at-risk human population against NiV infection currently seems unfounded. Outbreaks are rare, result in relatively few cases, are focal and isolated, and human-to-human transmission is generally confined to health care workers and family members engaging in close contact with exposed individuals, thus, rather favoring a ring vaccination approach. Therefore, a vaccine that produces a rapid and robust immune response after a single immunization with the potential for peri-exposure application (‘emergency vaccine’) would be most beneficial.
Current vaccine approaches for protection from NiV infection have focused on the use of NiV glycoprotein (G) and/or fusion protein (F) as immunogens in various platforms, including DNA vaccines, subunit vaccines, non-replicating vectors, as well as replicating vectors [8-23]. Efficacy of most of the previously tested vaccine candidates required a prime/boost(s) approach, which would not favor their use in an emergency situation for rapid dissemination during an outbreak.
In order to develop a vaccine appropriate for ring vaccination, we generated live-attenuated recombinant vesicular stomatitis viruses (rVSVs) encoding individual NiV proteins using the established reverse genetic system for VSV [24]. The VSV system has been used to generate vaccine candidates for many disease-causing viruses [25-28]. As a fast-acting single-dose vaccine, rVSV-based vaccines have been reported to elicit effective humoral and cellular immune responses, as well as to protect peri-exposure [26,29].
Herein, we tested the protective efficacy of three rVSVs expressing either the nucleoprotein (N), F or G of the Malaysian strain of NiV. Following a single dose, the vaccine vectors expressing G and F fully protected Syrian hamsters from lethal NiV challenge, whereas the N expressing vector conferred only partial protection. Using passive serum transfer, we further determined that full protection is conferred by glycoprotein (F, G)-specific antibodies, most likely the neutralizing fraction, elicited by the rVSV vaccines. However, other components of the immune system, such as cellular responses, also contribute to protection as demonstrated by partial efficacy and lack of protection in passive transfer studies in the case of the N expressing vaccine vector.
2. Materials and methods
2.1. Cells and viruses
Vero C1008 cells (European Collection of Cell Cultures, Salisbury, UK) and baby hamster kidney cells expressing the bacteriophage T7 promoter (BHK-T7) (kindly provided by Dr. Naoto Ito, Gifu University, Japan [30]) were used. NiV (Malaysian strain) was kindly provided by the Special Pathogens Branch, Center for Disease Control and Prevention, Atlanta, and propagated as previously described [31].
2.2. Generation of rVSV vectors
The plasmid pVSVXN2 (kindly provided by J. Rose, Yale University, New Haven) was modified as previously described to encode the open reading frame (ORF) for Zaire ebolavirus (ZEBOV) glycoprotein (GP) in place of that encoding the VSV glycoprotein (G) [32,33]. NiV F, G, or N ORFs from the Malaysian strain of NiV, were amplified similarly and cloned into pVSVXN2ΔG/ZEBOV-GP downstream of ZEBOV-GP (Fig. 1A). BHK-T7 cells were transfected using transit-LT1 Transfection Reagent (Mirus, Madison, WI) along with individual plasmids encoding the VSV N, P, and L ORFs and the modified VSV genomic plasmids as shown in Fig. 1A. Cells were incubated at 37 °C for 7 days, at which time supernatant was collected and passaged once on fresh Vero cells. Cultures were monitored daily for cytopathogenic effect (CPE) and supernatants or cells were collected for sequence confirmation and analysis of protein expression. The rescued viruses are referred to as rVSV-ZEBOV-GP-NiVF, rVSV-ZEBOV-GP-NiVG and rVSV-ZEBOV-GP-NiVN.
Fig. 1. Construction and characterization of recombinant VSV (rVSV) vectors expressing NiV glycoprotein (G), fusion protein (F), or nucleoprotein (N).
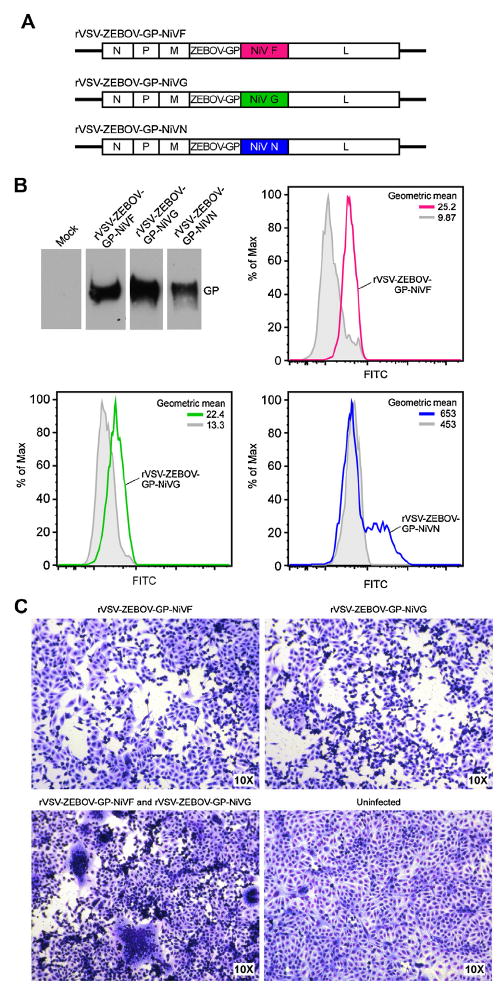
(A) Schematic representation of the vaccine constructs. rVSV-ZEBOV-GP-NiV constructs were engineered by cloning NiV protein open reading frames into the vector directly downstream of the ZEBOV-GP, which replaced VSV-G. (B) Verification of foreign protein expression. ZEBOV-GP expression was verified by western blot analysis of rVSV vector-infected cell lysates using the anti-ZEBOV-GP antibody 43.3.7. Expression of NiV proteins was verified by flow cytometry. Cells were infected with the different NiV protein-expressing rVSV vaccines (colored lines) or uninfected (gray lines) and surfaced stained with antibodies specific for the respective protein, anti-G 1187 and anti-F 835. In the case of N expression (colored line), cells were fixed in 4%PFA, then per-meabilized using saponin, followed by intracellular N-specific antibody staining. (C) Verification of fusogenic activity of F and G. Vero C1008 cells were infected with rVSV-ZEBOV-GP-NiVF, rVSV-ZEBOV-GP-NiVG, or co-infected with rVSV-ZEBOV-GP-NiVF and rVSV-ZEBOV-GP-NiVG at an MOI of 0.1, incubated for 2 days and stained with the Kwik Diff Kit. Medium (DMEM) alone was used as a negative control. (For interpretation of the references to color in this figure legend, the reader is referred to the web version of this article.)
2.3. Analysis of protein expression
Vero cells were infected with the different rVSVs at a multiplicity of infection (MOI) of 1. Two days later, cell culture supernatants were collected, centrifuged, and the resulting pellet was subjected to 10% SDS-polyacrylamide gel electrophoresis. Proteins were transferred to a PVDF membrane (GE healthcare, UK) and ZEBOV-GP was detected using the monoclonal antibody 43.3.7 (kindly provided by A. Takada, Hokkaido University, Sapporo, Japan). Flow cytometry was performed to detect NiV F, G and N expression. Virus-infected Vero cells (12 h post infection) were collected and washed in PBS containing 15 mM EDTA. For surface staining, cells were incubated with the primary antibodies anti-G 1187 [34] and anti-F 835 (kindly provided by Hector Aguilar-Carreno, Washington State University, USA), followed by incubation with goat anti-rabbit antibodies conjugated to Alexa 488 (Life Technologies) and fixed in 4% paraformaldehyde (PFA). For intracellular staining, cells were fixed in 4% PFA for 10 min, then washed and incubated in buffer containing 0.2% saponin (Sigma) for 10 min. After permeabiliza-tion, cells were incubated with an anti-NiV N rabbit antiserum [13] (kindly provided by Wang, CSIRO Livestock Industries, Geelong, Australia), followed by the above mentioned goat anti-rabbit antibodies in the presence of saponin. Flow cytometry was performed using an LSR II (BD Biosciences, San Jose, CA) and data were analyzed using FlowJo software (Treestar Inc., Ashland, OR). To measure the fusogenic activity of expressed NiV F and G, Vero cells were grown in 48-well plates and infected with individual rVSVs or co-infected with rVSV-ZEBOV-GP-NiVF and rVSV-ZEBOV-GP-NiVG for 1 h at a MOI of 0.1. After 2 days, cells were stained and fixed with the Kwik Diff kit (Thermo Scientific).
2.4. Immunization and challenge of Syrian hamsters
Groups of 10, 4–5 week old, Syrian hamsters (Harlan, Indianapolis, IN) were vaccinated intraperitoneally (i.p.) with 105 plaque forming units (PFU) of the specified rVSV vectors, or mock-vaccinated with DMEM in a total volume of 500 μL. Two days prior to NiV challenge (day 26 post vaccination), blood was collected by retro-orbital bleeding for analysis of antibody responses. After 28 days, animals were challenged i.p. with 1000 LD50 (6.8 × 104 TCID50) of NiV and monitored for clinical signs of disease. Necropsies were performed on four animals from each group 5 days post challenge to measure viral load, attempt virus isolation, and assess histopathology. Brain, lung, and spleen tissues were collected and placed in RLT lysis buffer (Qiagen, Valencia, CA) for RNA extraction, and in 10% formalin for histopathology and immunohistochemistry (IHC) analysis. The remaining six animals were used to monitor survival for 42 days post challenge.
2.5. Immune response to vaccination
Antibody responses were measured by enzyme-linked immunosorbent assay (ELISA) as described previously [35]. Neutralizing titers were determined by a neutralizing tissue culture infections dose 50% (NTCID50) assay.
2.6. Histopathology and immunohistochemistry
Hamsters tissues were collected and processed as described previously [31]. Embedded tissues were sectioned and stained with hematoxylin and eosin (H&E) or the above mentioned anti-NiV N rabbit antiserum at a 1:5000 dilution for immunohistochemistry (IHC) [13].
2.7. Quantitative real-time RT-PCR (qRT-PCR) and virus titration
Tissues were processed for qRT-PCR as described previously targeting the NiV N [31]. Defined dilutions of NiV RNA were used in triplicate to generate a standard curve from which sample TCID50 equivalents were extrapolated. NiV isolation and titration was performed as previously described [35]. A similar method was used in a qRT-PCR assay targeting VSV N with the Fwd primer: CGGAG-GATTGACGACTAATGC, Rev primer: CGAGCCATTCGACCACATC and probe: FAM-CGC CAC AAG GCA G-MGB.
2.8. Passive transfer of antibodies
Groups of 18, 4–5 week old, hamsters were vaccinated i.p. with 105 PFU of the specified rVSV vaccine vectors. After 28 days, animals were exsanguinated via cardiac puncture, serum was inactivated by gamma-irradiation (5 Mrad) and measured for antibody titers by ELISA and NTCID50 assay as described above. Positive sera were pooled from each group. Groups of six naïve hamsters were given 1 mL of serum i.p. 1 day prior to, and 1 day post i.p. challenge with 1000 LD50 (6.8 × 104 TCID50) of NiV and monitored for clinical signs for 42 days.
2.9. Ethics and biosafety
All work with NiV was completed in the BSL4 facility at the Rocky Mountain Laboratories, NIAID, NIH under standard operating procedures approved by the Institutional Biosafety Committee. All animal experiments were approved by the Institutional Animal Care and Use Committee and performed following the guidelines of the Association for Assessment and Accreditation of Laboratory Animal Care, International (AAALAC) by certified staff in an AAALAC-approved facility.
3. Results
3.1. Rescue of replication-competent rVSV vectors
To generate rVSVs expressing NiV proteins, the F, G, or N ORFs were amplified and individually inserted into pVSVXN2ΔG/ZEBOV-GP downstream of the ZEBOV-GP gene as previously described [33] (Fig. 1A). Individual genome constructs were transfected together with the VSV helper plasmids into BHK-T7 cells and the supernatants were passaged once onto fresh Vero cells. Cultures demonstrating CPE were verified for viral protein expression using western blotting of whole cell lysates for the detection of ZEBOV-GP, and flow cytometry for the detection of NiV F and G on the cell surface and NiV N intracellular. All three rescued rVSVs expressed ZEBOV-GP, and the individual viruses also expressed either NiV F, G, or N (Fig. 1B). To verify the structural and functional integrity of surface expressed NiV F and G, their fusogenic activity was tested by co-infecting a monolayer of Vero cells with rVSV-ZEBOV-GP-NiVF and rVSV-ZEBOV-GP-NiVG. We observed large-scale cell-to-cell fusion resulting in multinucle-ated syncytia formation, a phenomenon that requires the presence of functional NiV F and G on the cell surface (Fig. 1C).
3.2. Immunization with rVSV vectors elicits strong specific antibody responses
The humoral immune response to vaccination was assessed in Syrian hamsters, a well-established NiV animal disease model [36,37]. Groups of 10 hamsters were immunized with a single i.p. dose of 105 PFU of the different rVSV vectors (rVSV-ZEBOV-GP-NiVF, rVSV-ZEBOV-GP-NiVG or rVSV-ZEBOV-GP-NiVN) and rVSV-ZEBOV-GP as the control. After 26 days, blood samples were obtained and tested for NiV-specific antibodies by ELISA using antigen prepared from whole inactivated NiV particles. In contrast to the animals in the control group (rVSV-ZEBOV-GP), all other vaccinated animals showed high levels of antibodies titers ranging from 1600 to ≥3200 (Table 1). In addition, we tested all sera for the presence of neutralizing antibodies against NiV. As expected, vaccination of hamsters with rVSV-ZEBOV-GP or rVSV-ZEBOV-GP-NiVN did not result in the generation of neutralizing antibodies (Table 1). In contrast, all animals from the groups vaccinated with rVSV-ZEBOV-GP-NiVF and rVSV-ZEBOV-GP-NiVG generated neutralizing antibody titers ranging from 80 to ≥640 (Table 1).
Table 1.
Humoral immune responses to foreign proteins 26 days after rVSV vaccination as measured by ELISA (whole inactivated NiV particle antigen) and NTCID50 assay (against live Nipah virus).
| Animal | ZEBOV-GP
|
NiV F
|
NiV G
|
NiV N
|
||||
|---|---|---|---|---|---|---|---|---|
| ELISA titer | Neut. titer | ELISA titer | Neut. titer | ELISA titer | Neut. titer | ELISA titer | Neut. titer | |
| 1 | <20 | <20 | ≥3200 | 160 | ≥3200 | 640 | 1600 | <20 |
| 2 | <20 | <20 | ≥3200 | 80 | ≥3200 | 320 | ≥ 3200 | <20 |
| 3 | <20 | <20 | ≥3200 | 160 | ≥3200 | ≥640 | ≥ 3200 | <20 |
| 4 | <20 | <20 | ≥3200 | 80 | ≥3200 | ≥640 | ≥ 3200 | <20 |
| 5 | <20 | <20 | ≥3200 | 320 | ≥3200 | ≥640 | ≥ 3200 | <20 |
| 6 | <20 | <20 | ≥3200 | 180 | ≥3200 | 320 | ≥ 3200 | <20 |
| 7 | <20 | <20 | ≥3200 | 320 | ≥3200 | ≥640 | 1600 | <20 |
| 8 | <20 | <20 | ≥3200 | 320 | ≥3200 | ≥640 | ≥ 3200 | <20 |
| 9 | <20 | <20 | ≥3200 | 320 | ≥3200 | 320 | 1600 | <20 |
| 10 | <20 | <20 | ≥3200 | 320 | ≥3200 | ≥640 | 1600 | <20 |
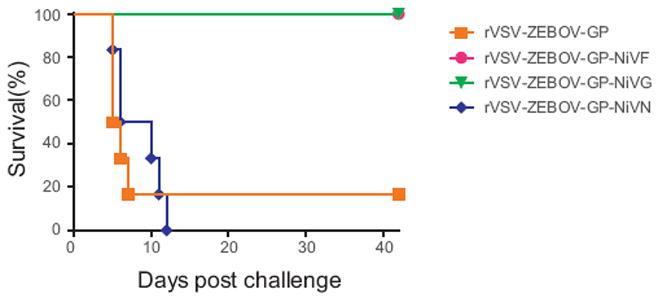
3.3. Vaccination confers protection against lethal Nipah virus infection
The animals (10 per group) from the immune response study above were subsequently challenged i.p. with 1000 LD50 of NiV. For the protection study we added a group of six hamsters that was mock-vaccinated (DMEM). Six animals in each group were monitored for survival. Animals in both control groups, DMEM and rVSV-ZEBOV-GP, developed clinical signs of disease between days 5 and 10 post challenge, resulting in respiratory distress with varying degree of neurologic dysfunction, and were euthanized according to the approved protocol (Fig. 2A). All animals in the groups vaccinated with rVSV-ZEBOV-GP-NiVF and rVSV-ZEBOV-GP-NiVG were completely protected from clinical disease with no significant weight loss (Fig. 2A and B). Hamsters vaccinated with rVSV-ZEBOV-GP-NiVN were partially protected (two of six animals) with no clinical signs of disease, while the remaining four animals had to be euthanized 9 days post challenge (Fig. 2A and B).
Fig. 2. Survival of vaccinated hamsters following Nipah virus challenge.
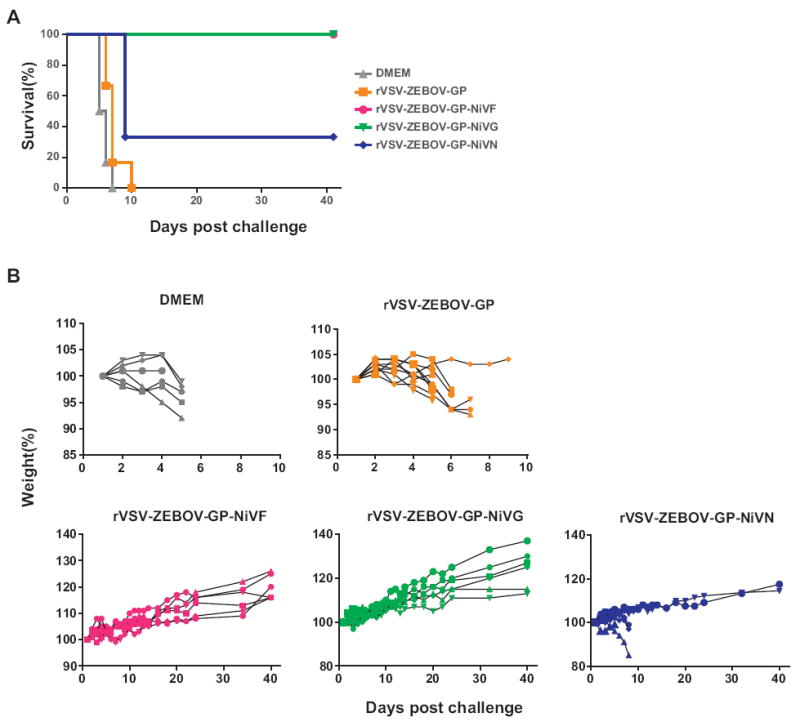
Groups of six hamsters were vaccinated i.p. with 105 PFU of rVSV-ZEBOV-GP, rVSV-ZEBOV-GP-NiVF, rVSV-ZEBOV-GP-NiVG, rVSV-ZEBOV-GP-NiVN or mock vaccinated (DMEM) 28 days prior to challenge with 1000 LD50 of NiV. (A) The percentage of animals surviving over time. (B) Body weight loss over time. Weights are shown as percentage of starting body weight.
3.4. Vaccinated animals showed reduced viral loads and less pathology
In order to determine the impact of vaccination on virus replication, we collected brain, lung and spleen tissues 5 days post NiV challenge from four hamsters of each group described above for NiV load determination and isolation. Viral loads were determined using a NiV N-specific qRT-PCR assay (Fig. 3). All NiV-vaccinated animals had lower organ levels of viral RNA compared to the animals in the control groups (>103 TCID50 equivalent/mg tissue), with rVSV-ZEBOV-GP-NiVF and rVSV-ZEBOV-GP-NiVG vaccinated animals showing organ loads <1 TCID50 equivalent/mg tissue. rVSV-ZEBOV-GP-NiVN vaccinated animals showed a greater than 2-log reduction in viral organ loads compared to the rVSV-ZEBOV-GP vaccinated controls. In order to confirm that the positive immunohistochemistry described below (Fig. 4) represents replication of the challenge virus (NiV) rather than N expressed by the vaccine vector (rVSV-ZEBOV-GP-NiVN), we performed a VSV N-specific qRT-PCR assay. No VSV N RNA could be detected in lung tissue of the rVSV-ZEBOV-GP-NiVN vaccinated animals. NiV isolation was only successful from control animals (rVSV-ZEBOV-GP group).
Fig. 3. Vaccination reduces Nipah virus load in tissues.
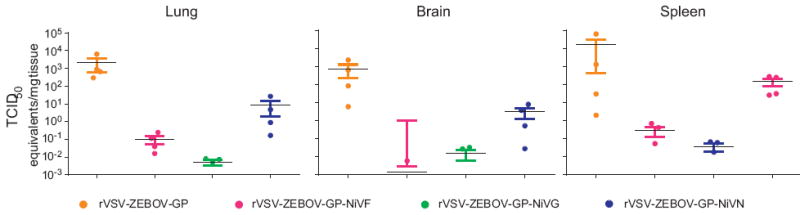
Tissues (brain, spleen, lung) were collected in RLT buffer from four animals per group on day 5 after challenge and homogenized prior to total RNA extraction. Quantitative RT-PCR using an N-specific primer and probe set was used to determine TCID50 equivalents by extrapolating from a standard curve from a NiV seed stock of known titer. Individual animals are represented by dots and horizontal lines represent the mean, error bars indicate standard error of the mean (SEM).
Fig. 4. Vaccination reduces Nipah virus pathology.
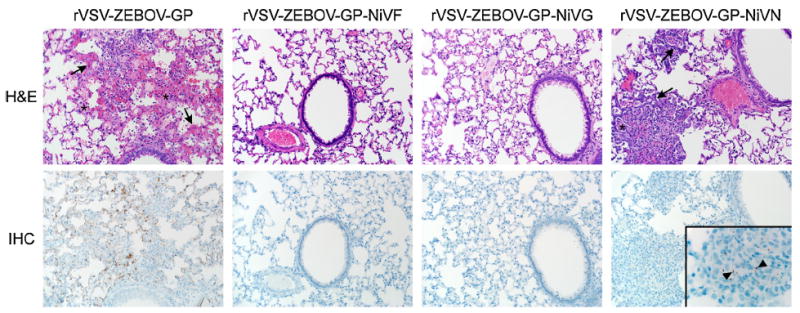
Four hamsters per group were euthanized 5 days post challenge and lung sections were stained with H&E (top panel) for histopathology evaluation and IHC targeting NiV N protein for virus replication (bottom panel). Infected lungs showed thickening of the alveolar septae (arrows) by congestion, fibrin, edema, and small numbers of inflammatory cells. Alveolar spaces are filled with fibrin, edema, and inflammatory cells (asterisk). Inset in IHC panel demonstrates positive staining of NiV N-antigen (arrow heads). Images were taken at a magnification of 200× and inset at 1000×.
Staining for histological analysis was performed on lung tissue derived from the same 4 animals euthanized 5 days post challenge. All rVSV-ZEBOV-GP vaccinated control animals developed multifocal interstitial pneumonia characterized by thickening of the alveolar septae by small to moderate numbers of macrophages, fewer neutrophils, congestion, fibrin and edema (Fig. 4). Occasionally, small numbers of inflammatory cells, fibrin and edema filled the adjacent alveolar spaces. There was also multifocal pleural mesothelial hyperplasia. Alveolar and arteriolar endothelial cells and pulmonary arteriolar smooth muscle cells demonstrated diffuse viral antigen by IHC staining (Fig. 4). Most animals (three of four) in the partially protected rVSV-ZEBOV-GP-NiVN group developed pneumonia similar to that found in controls. These hamsters had rare and weak multifocal viral antigen staining, primarily within mononuclear cells in areas of pneumonia. All animals in the completely protected groups (rVSV-ZEBOV-GP-NiVF and rVSV-ZEBOV-GP-NiVG) showed no lesions and were negative for viral antigen by IHC staining (Fig. 4).
3.5. Passive serum transfer protects naïve animals from Nipah virus infection
To test whether antibodies elicited by the rVSV vectors alone can afford protection against NiV challenge, we performed a passive transfer experiment. Groups of 18 hamsters were vaccinated with 105 PFU i.p. of one of the rVSV vectors. After 28 days, sera were collected and pooled for each group. Pooled sera from rVSV-ZEBOV-GP-NiVF and rVSV-ZEBOV-GP-NiVG had neutralization titers of 200 and 400, respectively, whereas sera collected from the rVSV-ZEBOV-GP and rVSV-ZEBOV-GP-NiVN vaccinated groups were negative. Groups of six naïve hamsters were administered i.p. 1 mL of pooled serum the day prior to and the day following NiV challenge (1000 LD50). All animals, except one, that received serum without neutralizing activity (rVSV-ZEBOV-GP and rVSV-ZEBOV-GP-NiVN) had to be euthanized according to protocol (Fig. 5). All animals that received serum displaying neutralizing activity (rVSV-ZEBOV-GP-NiVF- or rVSV-ZEBOV-GP-NiVG) were completely protected from NiV challenge with no signs of disease.
Fig. 5. Passive serum transfer protects naïve hamsters from Nipah virus challenge.
Serum was collected from groups of 18 hamsters 28 days after vaccination with 105 PFU of the specific vaccine vectors. One day prior to, and 1 day post challenge with 1000 LD50 of NiV, groups of six naïve hamsters were given 1 mL of sera from immunized animals and monitored for 42 days for signs of disease.
4. Discussion
Over the past decade, multiple distinct NiV vaccine approaches have been developed and evaluated in different animal models, including DNA vaccines, subunit vaccines (virus-like particles, soluble G protein), replication-deficient vectors as well as replication-competent vectors. Several of these approaches have only been evaluated for their ability to elicit immune responses, whereas others have been used to evaluate protective efficacy against NiV challenge in different animal models [8-16,18-23].
With the exception of three recent studies, all vaccine approaches thus far have required a boosting immunization scheme for immunogenicity and/or efficacy and are therefore less likely to be useful for ring vaccination approaches in an outbreak situation. The three new studies include an adenovirus-associated virus vector expressing NiV G [20], replication-incompetent VSV pseudotypes expressing NiV G or F proteins [22] and a VSV virion with F and G that can undergo a single round of replication that was produced by co-infection of two VSV pseudotypes, one expressing F and one expressing G [38]. The adenovirus-associated virus vector approach used relatively high vaccine doses, and the VSV approaches are based on replication-deficient pseudotype particles produced by plasmid transfections, both of which may be challenging in regards to vaccine production.
Our goal was to develop a fast-acting, single-dose NiV vaccine suitable for use as a ring vaccination approach during outbreaks as they currently occur in Bangladesh. We chose live-attenuated rVSV vectors as our platform due to their ease of genetic modification and their subsequent efficient and cost-effective manufacturing. We preferred a replication-competent vaccine as those generally provide better durability when compared to a replication-incompetent vaccine approaches, eliciting faster and more effective innate and adaptive immune responses [39]. Replication-competent vaccine approaches, however, are commonly associated with safety concerns, but all of our previous vaccine work using the rVSV platform, including immunization of several immune-compromised animal species, has assigned this approach a good safety record [26,40]. Noteworthy, a live-attenuated rVSV-based vaccine vector was approved for use in a human laboratory exposure to Ebola virus [41]. Among commonly used replicating vaccine vectors, VSV provides advantages over similar platforms, such as the limited pre-existing immunity against VSV in the human population and the only rare and mild human disease caused by VSV, which is largely an animal pathogen [42,43]. To further limit VSV immunity and pathogenicity, we removed VSV-G, the major target for neutralizing antibodies and a key VSV virulence factor [43]. VSV-G was replaced in the vaccine vector by ZEBOV-GP to overcome the lack of a functional surface protein for virus entry. Virus entry cannot be achieved by any of the chosen NiV antigens, because henipavirus cell entry is dependent on the presence of both G and F proteins [44]. The ZEBOV-GP was particularly chosen for its known targeting of important immune cells, such as mononuclear phagocytotic and antigen presenting cells [27,33,45]. Targeting of these cells allows for their strong stimulation and better antigen presentation by MHC class I and II pathways, and thus leads to more potent innate and adaptive immune responses [46,47].
In order to characterize the mechanism of protection afforded by the rVSV-based vaccine vectors, we examined the importance of the humoral immune responses. Previously it has been demonstrated that protection against NiV challenge can be afforded by passive serum transfer that contains neutralizing antibodies [8]. Additionally, m102.4, a human neutralizing monoclonal antibody, can protect against NiV and Hendra virus in several animal models [13,48]. The rVSV vaccine vectors expressing NiV F or G both induced glycoprotein-specific antibody responses that conferred complete protection against NiV challenge in a serum transfer study. Neutralizing antibody responses are most likely key for protection, as serum transfer of N-specific antibodies did not show any protective effect, even though the role of non-neutralizing glycoprotein-specific antibodies for protection cannot be excluded. VSV is known to also elicit strong cellular immune responses [39,49,50]. The role of cellular immune responses mediated through rVSV vectors is supported here by the partial protection achieved through vaccination with the rVSV vector expressing NiV N as well as the lack of protection in serum transfer experiments using sera with N-specific non-neutralizing antibodies. Therefore, these new rVSV vectors might be stronger vaccine candidates than vaccine platforms that more selectively trigger humoral immune responses, such as subunit protein vaccines [9,12,18].
5. Conclusions
Here we describe a vaccine approach and mechanism of protection that could be used to control NiV infections and spread in outbreak situation if used in a ring vaccination approach. Recent outbreaks have involved increased human-to-human transmission events, most often seen in family members or healthcare workers [7]. Due to the ease in identifying high-risk individuals, those in close contact with patients, fast-acting, single-dose vaccines, like the rVSV vectors here, would be advantageous for targeted use during outbreaks over vaccines that need multiple injections and thus require more time between vaccination and protection. Another advantage of replication-competent rVSVs has been its efficacy upon use peri-exposure, allowing for simultaneous vaccination and treatment in outbreak situations [26,27,33,51,52]. Future studies are aimed to assess time to immunity and peri-exposure treatment efficacy of these new rVSV NiV vectors as well as efficacy studies in a second animal model to fulfill FDA requirements for licensing.
Acknowledgments
This work was supported by the Division of Intramural Research (DIR), National Institutes of Allergy and Infection Diseases (NIAID), National Institutes of Health (NIH). The authors would like to thank Dan Long, Rebecca Rosenke, and Tina Thomas (Rocky Mountain Veterinary Branch, DIR, NIAID, NIH) for histopathology work, Elaine Haddock (DIR, NIAID, NIH) for BSL4 technical assistance and Anita Mora (DIR, NIAID, NIH) for graphics.
Footnotes
Conflict of interest
All authors declare no conflict of interest.
References
- 1.Goh KJ, Tan CT, Chew NK, Tan PS, Kamarulzaman A, Sarji SA, et al. Clinical features of Nipah virus encephalitis among pig farmers in Malaysia. N Engl J Med. 2000;342:1229–35. doi: 10.1056/NEJM200004273421701. [DOI] [PubMed] [Google Scholar]
- 2.Luby SP, Gurley ES. Epidemiology of henipavirus disease in humans. Curr Top Microbiol Immunol. 2012;359:25–40. doi: 10.1007/82_2012_207. [DOI] [PubMed] [Google Scholar]
- 3.Hooper P, Zaki S, Daniels P, Middleton D. Comparative pathology of the diseases caused by Hendra and Nipah viruses. Microb Infect. 2001;3:315–22. doi: 10.1016/s1286-4579(01)01385-5. [DOI] [PubMed] [Google Scholar]
- 4.Chong HT, Hossain MJ, Tan CT. Differences in epidemiologic and clinical features of Nipah virus encephalitis between the Malaysian and Bangladesh outbreaks. Neurol Asia. 2008;13:23–6. [Google Scholar]
- 5.Yob JM, Field H, Rashdi AM, Morrissy C, van der Heide B, Rota P, et al. Nipah virus infection in bats (order Chiroptera) in peninsular Malaysia. Emerg Infect Dis. 2001;7:439–41. doi: 10.3201/eid0703.010312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Luby SP, Gurley ES, Hossain MJ. Transmission of human infection with Nipah virus. Clin Infect Dis. 2009;49:1743–8. doi: 10.1086/647951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gurley ES, Montgomery JM, Hossain MJ, Bell M, Azad AK, Islam MR, et al. Person-to-person transmission of Nipah virus in a Bangladeshi community. Emerg Infect Dis. 2007;13:1031–7. doi: 10.3201/eid1307.061128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Guillaume V, Contamin H, Loth P, Georges-Courbot M-C, Lefeuvre A, Marianneau P, et al. Nipah virus: vaccination and passive protection studies in a hamster model. J Virol. 2004;78:834–40. doi: 10.1128/JVI.78.2.834-840.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mungall BA, Middleton D, Crameri G, Bingham J, Halpin K, Russell G, et al. Feline model of acute Nipah virus infection and protection with a soluble glycoprotein-based subunit vaccine. J Virol. 2006;80:12293–302. doi: 10.1128/JVI.01619-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wang X, Ge J, Hu S, Wang Q, Wen Z, Chen H, et al. Efficacy of DNA immunization with F and G protein genes of Nipah virus. Ann NY Acad Sci. 2006;1081:243–5. doi: 10.1196/annals.1373.029. [DOI] [PubMed] [Google Scholar]
- 11.Weingartl HM, Berhane Y, Caswell JL, Loosmore S, Audonnet J-C, Roth JA, et al. Recombinant nipah virus vaccines protect pigs against challenge. J Virol. 2006;80:7929–38. doi: 10.1128/JVI.00263-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.McEachern JA, Bingham J, Crameri G, Green DJ, Hancock TJ, Middleton D, et al. A recombinant subunit vaccine formulation protects against lethal Nipah virus challenge in cats. Vaccine. 2008;26:3842–52. doi: 10.1016/j.vaccine.2008.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bossart KN, Zhu Z, Middleton D, Klippel J, Crameri G, Bingham J, et al. A neutralizing human monoclonal antibody protects against lethal disease in a new ferret model of acute nipah virus infection. PLoS Pathog. 2009;5:e1000642. doi: 10.1371/journal.ppat.1000642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Defang GN, Khetawat D, Broder CC, Quinnan GV. Induction of neutralizing antibodies to Hendra and Nipah glycoproteins using a Venezuelan equine encephalitis virus in vivo expression system. Vaccine. 2010;29:212–20. doi: 10.1016/j.vaccine.2010.10.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chattopadhyay A, Rose JK. Complementing defective viruses that express separate paramyxovirus glycoproteins provide a new vaccine vector approach. J Virol. 2011;85:2004–11. doi: 10.1128/JVI.01852-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Walpita P, Barr J, Sherman M, Basler CF, Wang L. Vaccine potential of Nipah virus-like particles. PLoS One. 2011;6:e18437. doi: 10.1371/journal.pone.0018437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pallister JA, Klein R, Arkinstall R, Haining J, Long F, White JR, et al. Vaccination of ferrets with a recombinant G glycoprotein subunit vaccine provides protection against Nipah virus disease for over 12 months. Virol J. 2013;10:237. doi: 10.1186/1743-422X-10-237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bossart KN, Rockx B, Feldmann F, Brining D, Scott D, LaCasse R, et al. A Hendra virus G glycoprotein subunit vaccine protects African green monkeys from Nipah virus challenge. Sci Transl Med. 2012;4:146ra107. doi: 10.1126/scitranslmed.3004241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kong D, Wen Z, Su H, Ge J, Chen W, Wang X, et al. Newcastle disease virus-vectored Nipah encephalitis vaccines induce B and T cell responses in mice and long-lasting neutralizing antibodies in pigs. Virology. 2012;432:327–35. doi: 10.1016/j.virol.2012.06.001. [DOI] [PubMed] [Google Scholar]
- 20.Ploquin A, Szécsi J, Mathieu C, Guillaume V, Barateau V, Ong KC, et al. Protection against henipavirus infection by use of recombinant adeno-associated virus-vector vaccines. J Infect Dis. 2013;207:469–78. doi: 10.1093/infdis/jis699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Prescott J, de Wit E, Feldmann H, Munster VJ. The immune response to Nipah virus infection. Arch Virol. 2012;157:1635–41. doi: 10.1007/s00705-012-1352-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lo MK, Bird BH, Chattopadhyay A, Drew CP, Martin BE, Coleman JD, et al. Single-dose replication-defective VSV-based Nipah virus vaccines provide protection from lethal challenge in Syrian hamsters. Antiviral Res. 2013;101:26–9. doi: 10.1016/j.antiviral.2013.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yoneda M, Georges-Courbot M-C, Ikeda F, Ishii M, Nagata N, Jacquot F, et al. Recombinant measles virus vaccine expressing the Nipah virus glycoprotein protects against lethal Nipah virus challenge. PLoS One. 2013;8:e58414. doi: 10.1371/journal.pone.0058414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lawson ND, Stillman EA, Whitt MA, Rose JK. Recombinant vesicular stomatitis viruses from DNA. PNAS. 1995;92:4477–81. doi: 10.1073/pnas.92.10.4477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cobleigh MA, Wei X, Robek MD. A vesicular stomatitis virus-based therapeutic vaccine generates a functional CD8 T cell response to hepatitis B virus in transgenic mice. J Virol. 2013;87:2969–73. doi: 10.1128/JVI.02111-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Geisbert TW, Feldmann H. Recombinant vesicular stomatitis virus-based vaccines against Ebola and Marburg virus infections. J Infect Dis. 2011;204(Suppl):S1075–81. doi: 10.1093/infdis/jir349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Brown KS, Safronetz D, Marzi A, Ebihara H, Feldmann H. Vesicular stomatitis virus-based vaccine protects hamsters against lethal challenge with Andes virus. J Virol. 2011;85:12781–91. doi: 10.1128/JVI.00794-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Roberts A, Kretzschmar E, Perkins AS, Forman J, Price R, et al. Vaccination with a recombinant vesicular stomatitis virus expressing an influenza virus hemagglutinin provides complete protection from influenza virus challenge. J Virol. 1998;72:4704–11. doi: 10.1128/jvi.72.6.4704-4711.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wilson SR, Wilson JH, Buonocore L, Palin A, Rose JK, Reuter JD. Intranasal immunization with recombinant vesicular stomatitis virus expressing murine cytomegalovirus glycoprotein B induces humoral and cellular immunity. Comp Med. 2008;58:129. [PMC free article] [PubMed] [Google Scholar]
- 30.Ito N, Takayama-Ito M, Yamada K, Hosokawa J, Sugiyama M, Minamoto N. Improved recovery of rabies virus from cloned cDNA using a vaccinia virus-free reverse genetics system. Microbiol Immunol. 2003;47:613–7. doi: 10.1111/j.1348-0421.2003.tb03424.x. [DOI] [PubMed] [Google Scholar]
- 31.DeBuysscher BL, de Wit E, Munster VJ, Scott D, Feldmann H, Prescott J. Comparison of the pathogenicity of Nipah virus isolates from Bangladesh and Malaysia in the Syrian hamster. PLoS Negl Trop Dis. 2013;7:e2024. doi: 10.1371/journal.pntd.0002024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Garbutt M, Liebscher R, Wahl-Jensen V, Jones S, Möller P, Wagner R, et al. Properties of replication-competent vesicular stomatitis virus vectors expressing glycoproteins of filoviruses and arenaviruses. J Virol. 2004:78, 5458–65. doi: 10.1128/JVI.78.10.5458-5465.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tsuda Y, Safronetz D, Brown K, LaCasse R, Marzi A, Ebihara H, et al. Protective efficacy of a bivalent recombinant vesicular stomatitis virus vaccine in the Syrian hamster model of lethal Ebola virus infection. J Infect Dis. 2011;204(Suppl):S1090–7. doi: 10.1093/infdis/jir379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Biering SB, Huang A, Vu AT, Robinson LR, Bradel-Tretheway B, Choi E, et al. N-Glycans on the Nipah virus attachment glycoprotein modulate fusion and viral entry as they protect against antibody neutralization. J Virol. 2012;86:11991–2002. doi: 10.1128/JVI.01304-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.De Wit E, Bushmaker T, Scott D, Feldmann H, Munster VJ. Nipah virus transmission in a hamster model. PLoS Negl Trop Dis. 2011;5:e1432. doi: 10.1371/journal.pntd.0001432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wong KT, Grosjean I, Brisson C, Blanquier B, Fevre-Montange M, Bernard A, et al. A golden hamster model for human acute Nipah virus infection. Am J Pathol. 2003;163:2127–37. doi: 10.1016/S0002-9440(10)63569-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rockx B, Brining D, Kramer J, Callison J, Ebihara H, Mansfield K, et al. Clinical outcome of henipavirus infection in hamsters is determined by the route and dose of infection. J Virol. 2011;85:7658–71. doi: 10.1128/JVI.00473-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mire CE, Versteeg KM, Cross RW, Agans KN, Fenton KA, Whitt MA, et al. Single injection recombinant vesicular stomatitis virus vaccines protect ferrets against lethal Nipah virus disease. Virol J. 2013;10:353. doi: 10.1186/1743-422X-10-353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kapadia SU, Rose JK, Lamirande E, Vogel L, Subbarao K, Roberts A. Long-term protection from SARS coronavirus infection conferred by a single immunization with an attenuated VSV-based vaccine. Virology. 2005;340:174–82. doi: 10.1016/j.virol.2005.06.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mire CE, Miller AD, Carville A, Westmoreland SV, Geisbert JB, Mansfield KG, et al. Recombinant vesicular stomatitis virus vaccine vectors expressing filovirus glycoproteins lack neurovirulence in nonhuman primates. PLoS Negl Trop Dis. 2012;6:e1567. doi: 10.1371/journal.pntd.0001567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Günther S, Feldmann H, Geisbert TW, Hensley LE, Rollin PE, Nichol ST, et al. Management of accidental exposure to Ebola virus in the biosafety level 4 laboratory, Hamburg, Germany. J Infect Dis. 2011;204(Suppl):S785–90. doi: 10.1093/infdis/jir298. [DOI] [PubMed] [Google Scholar]
- 42.Brody JA, Fischer GF, Peralta PH. Vesicular stomatitis virus in Panama. Human serologic patterns in a cattle raising area. Am J Epidemiol. 1967;86:158–61. doi: 10.1093/oxfordjournals.aje.a120721. [DOI] [PubMed] [Google Scholar]
- 43.Lyles DS, Rupprecht CE. Rhabdoviridae. In: Knipe DM, editor. Fields virology. Philadelphia, PA: Lippincott Williams & Wilkins; 2007. pp. 1364–409. [Google Scholar]
- 44.Aguilar HC, Iorio RM. Henipavirus membrane fusion and viral entry. Curr Top Microbiol Immunol. 2012;359:79–94. doi: 10.1007/82_2012_200. [DOI] [PubMed] [Google Scholar]
- 45.Feldmann H, Geisbert TW. Ebola haemorrhagic fever. Lancet. 2011;377:849–62. doi: 10.1016/S0140-6736(10)60667-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Yewdell JW, Norbury CC, Bennink JR. Mechanisms of exogenous antigen presentation by MHC class I molecules in vitro and in vivo: implications for generating CD8+ T cell responses to infectious agents, tumors, transplants, and vaccines. Adv Immunol. 1999;73:1–77. doi: 10.1016/s0065-2776(08)60785-3. [DOI] [PubMed] [Google Scholar]
- 47.Banchereau J, Steinman RM. Dendritic cells and the control of immunity. Nature. 1998;392:245–52. doi: 10.1038/32588. [DOI] [PubMed] [Google Scholar]
- 48.Bossart KN, Geisbert TW, Feldmann H, Zhu Z, Feldmann F, Geisbert JB, et al. A neutralizing human monoclonal antibody protects African green monkeys from Hendra virus challenge. Sci Transl Med. 2011;3:105ra103. doi: 10.1126/scitranslmed.3002901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Palin A, Chattopadhyay A, Park S, Delmas G, Suresh R, Senina S, et al. An optimized vaccine vector based on recombinant vesicular stomatitis virus gives high-level, long-term protection against Yersinia pestis challenge. Vaccine. 2007;25:741–50. doi: 10.1016/j.vaccine.2006.08.010. [DOI] [PubMed] [Google Scholar]
- 50.Schwartz JA, Buonocore L, Suguitan AL, Silaghi A, Kobasa D, Kobinger G, et al. Potent vesicular stomatitis virus-based avian influenza vaccines provide long-term sterilizing immunity against heterologous challenge. J Virol. 2010;84:4611–8. doi: 10.1128/JVI.02637-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Feldmann H, Jones SM, Daddario-DiCaprio KM, Geisbert JB, Ströher U, Grolla A, et al. Effective post-exposure treatment of Ebola infection. PLoS Pathog. 2007;3:e2. doi: 10.1371/journal.ppat.0030002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Geisbert TW, Hensley LE, Geisbert JB, Leung A, Johnson JC, Grolla A, et al. Postexposure treatment of Marburg virus infection. Emerg Infect Dis. 2010;16:1119–22. doi: 10.3201/eid1607.100159. [DOI] [PMC free article] [PubMed] [Google Scholar]


