Abstract
IMPORTANCE
Racial disparities in use of analgesia in emergency departments have been previously documented. Further work to understand the causes of these disparities must be undertaken, which can then help inform the development of interventions to reduce and eradicate racial disparities in health care provision.
OBJECTIVE
To evaluate racial differences in analgesia administration, and particularly opioid administration, among children diagnosed as having appendicitis.
DESIGN, SETTING, AND PARTICIPANTS
Repeated cross-sectional study of patients aged 21 years or younger evaluated in the emergency department who had an International Classification of Diseases, Ninth Revision diagnosis of appendicitis, using the National Hospital Ambulatory Medical Care Survey from 2003 to 2010. We calculated the frequency of both opioid and nonopioid analgesia administration using complex survey weighting. We then performed multivariable logistic regression to examine racial differences in overall administration of analgesia, and specifically opioid analgesia, after adjusting for important demographic and visit covariates, including ethnicity and pain score.
MAIN OUTCOMES AND MEASURES
Receipt of analgesia administration (any and opioid) by race.
RESULTS
An estimated 0.94 (95% CI, 0.78–1.10) million children were diagnosed as having appendicitis. Of those, 56.8% (95% CI, 49.8%–63.9%) received analgesia of any type; 41.3% (95% CI, 33.7%–48.9%) received opioid analgesia (20.7% [95% CI, 5.3%–36.0%] of black patients vs 43.1% [95% CI, 34.6%–51.4%] of white patients). When stratified by pain score and adjusted for ethnicity, black patients with moderate pain were less likely to receive any analgesia than white patients (adjusted odds ratio = 0.1 [95% CI, 0.02–0.8]). Among those with severe pain, black patients were less likely to receive opioids than white patients (adjusted odds ratio = 0.2 [95% CI, 0.06–0.9]). In a multivariable model, there were no significant differences in the overall rate of analgesia administration by race. However, black patients received opioid analgesia significantly less frequently than white patients (12.2% [95% CI, 0.1%–35.2%] vs 33.9% [95% CI, 0.6%–74.9%], respectively; adjusted odds ratio = 0.2 [95% CI, 0.06–0.8]).
CONCLUSIONS AND RELEVANCE
Appendicitis pain is undertreated in pediatrics, and racial disparities with respect to analgesia administration exist. Black children are less likely to receive any pain medication for moderate pain and less likely to receive opioids for severe pain, suggesting a different threshold for treatment.
Racial disparities in health care have been well documented in both adults and children.1–3 In the emergency department (ED), racial and ethnic differences have been demonstrated with respect to ED wait times to see a physician,4,5 hospital admission rates,6 and management of closed head trauma.7 Racial and ethnic differences in the ED management of pain have also been described, with lower rates of opioid prescription for black and Hispanic patients than for white patients.8–12 There are fewer studies in children, however, that verify these findings.8,13,14
Previous studies have noted racial and ethnic differences in the ED management of abdominal pain in both adult and pediatric populations.14,15 However, these studies may be affected by different biases, including spectrum bias, as under-represented minorities are more likely to identify the ED as their usual source of health care16–19 and use the ED for nonurgent care.20 Therefore, among other reasons, these differences may be more of a reflection of racial and ethnic differences in ED use rather than ED management, as minorities may be more likely to present to the ED for nonsurgical or less intense causes of abdominal pain.21 Appendicitis is the most common surgical cause of abdominal pain in the ED and the provision of analgesia to patients with appendicitis is now accepted and encouraged.22,23 Therefore, the investigation of pain management among children diagnosed as having appendicitis provides a more appropriate paradigm in which to evaluate racial differences in the administration of analgesia. We hypothesized that black patients would be less likely to receive opioid analgesia than white patients.
Methods
Study Design
We conducted a repeated cross-sectional analysis of the National Hospital Ambulatory Medical Care Survey (NHAMCS) from 2003 to 2010. This study was considered exempt from review by the Children’s National Health System Institutional Review Board. Informed consent was not required because the study used deidentified data from a national database.
Data Source and Study Population
The NHAMCS is a multistage national probability sample survey of visits to the EDs and outpatient departments of hospitals, exclusive of federal, military, and Veterans Affairs hospitals in the 50 states and the District of Columbia. The survey is conducted by the Centers for Disease Control and Prevention, National Center for Health Statistics during a randomly assigned 4-week data period annually. The survey uses a 4-stage probability design with samples of primary sampling units, hospitals within primary sampling units, clinical and emergency service areas within hospitals, and patient visits within clinics and emergency service areas. The patient visit is the basic sampling unit. Each patient visit represents a larger number of visits. A weight is assigned to each observation and allows for the generation of nationally representative estimates. For the purposes of this study, we limited our analysis to emergency service areas or EDs only.
The eligible study population included all sampled ED visits by patients aged 21 years or younger with an International Classification of Diseases, Ninth Revision diagnosis of appendicitis (codes 540, 541).
Variables
Our outcome measure was receipt of analgesic medication (overall, nonopioid, and opioid) by race. The NHAMCS codes up to 8 medications per patient visit. All medications were categorized as the following: opioid analgesia, nonopioid analgesia, or nonanalgesia. Each visit was categorized as no analgesia prescribed or analgesia prescribed. We further categorized the group with analgesia prescribed as nonopioid analgesia if at least 1 nonopioid analgesic and no opioid analgesic were administered and as opioid analgesia if at least 1 opioid analgesic was administered.
Independent Variables
The NHAMCS captures race as the following: white, black/African American, Asian, Native Hawaiian/other Pacific Islander, American Indian/Alaska Native, or more than 1 race reported. The NHAMCS then recategorizes race as white, black, or other. We used the recategorized race variable for our analyses. The following covariates were included in our analyses to adjust for potential confounding: ethnicity, age, sex, insurance status, triage acuity level, pain score, geographic region, ED type, and survey year. Ethnicity is coded in the NHAMCS as Hispanic/Latino or as not Hispanic/Latino. We analyzed age as a continuous variable. We categorized insurance status as private insurance, public insurance (Medicare, Medicaid/State Children’s Health Insurance Program, workers’ compensation), or no insurance (self-pay, no charge/charity). The NHAMCS captures triage acuity level using the 5-level Emergency Severity Index. For our analyses, we collapsed the 2 most acute categories, immediate and emergent, into a singular immediate/emergent category as very few visits were categorized as immediate. Therefore, we categorized triage level as immediate/emergent, urgent, semiurgent, and nonurgent. In 2009, the NHAMCS began recording pain on a 10-point scale. Prior to 2009, pain scores were captured in 4 categories. Using the Stanford Comparative Pain Scale,24 2009 and 2010 pain data were reclassified into the 4 categories of no pain, mild pain, moderate pain, and severe pain. Geographic region is categorized in the NHAMCS as Northeast, Midwest, South, and West. Finally, we categorized ED type as general ED or pediatric ED. We categorized visits as occurring at a pediatric ED if more than 75% of visits to the particular ED were by patients aged 21 years or younger.
Statistical Analysis
We used the survey sample suite of programs implemented in Stata version 12.1 statistical software (StataCorp LP) for all analyses to account for the multistage cluster sampling design of the NHAMCS. We performed bivariable logistic regression to identify the strength of association of race on overall administration of analgesia and on opioid administration specifically. We then performed multivariable logistic regression to adjust for confounding by specified covariates for which there was biological or epidemiological plausibility. Variables with P < .10 in any of the bivariable analyses and any variables that were a priori felt to have a potential relationship with overall analgesia or opioid administration were retained in our multivariable model. Furthermore, we performed tests of interaction between sex and pain score. Estimates derived from the multivariable model included adjusted odds ratios (ORs) with 95% confidence intervals and predicted probabilities. We estimated the predicted probabilities of analgesia and opioid administration by means of predictive margins as implemented in the “margins” command in Stata.25
Results
During the study period, there were an estimated 0.94 (95% CI, 0.78–1.10) million ED visits for appendicitis among patients aged 21 years or younger. The mean age of the study population was 13.5 years and most participants were male (64.8%) (Table 1). Most visits were by white patients (86.6%).
Table 1.
Demographic Characteristics of Study Population
| Characteristic | Value (95% CI) |
|---|---|
| Age, mean, y | 13.5 (12.9–14.1) |
| Male, % | 64.8 (58.1–71.5) |
| Race, % | |
| White | 86.6 (82.0–91.1) |
| Black | 8.8 (4.9–12.6) |
| Asian | 3.1 (0.9–5.3) |
| Other | 1.5 (0.1–2.9) |
| Ethnicity, % | |
| Hispanic | 22.4 (15.8–28.9) |
| Non-Hispanic | 77.6 (71.1–84.2) |
| Insurance status, % | |
| Private | 60.6 (52.8–68.3) |
| Public | 27.0 (19.4–34.6) |
| None | 12.4 (7.3–17.7) |
| Triage acuity level, % | |
| Immediate/emergent | 18.2 (10.9–25.5) |
| Urgent | 49.2 (41.1–57.4) |
| Semiurgent | 26.1 (18.4–33.8) |
| Nonurgent | 6.5 (3.1–9.9) |
| Pain score, % | |
| None | 2.6 (0.1–6.0) |
| Mild | 6.4 (2.8–9.9) |
| Moderate | 40.9 (33.4–48.3) |
| Severe | 50.1 (42.9–57.2) |
| Geographic region, % | |
| Northeast | 20.5 (13.8–27.2) |
| Midwest | 24.2 (16.6–31.9) |
| South | 30.5 (22.4–38.6) |
| West | 24.8 (17.7–31.9) |
| Emergency department type, % | |
| General | 91.7 (86.8–96.6) |
| Pediatric | 8.3 (3.4–13.2) |
Overall, 56.8% (95% CI, 49.8%–63.9%) of patients received some form of analgesia, and 41.3% (95% CI, 33.7%–48.9%) received at least 1 opioid analgesic. Fewer than 1% of patients received ketorolac, and of those who did, 90% received opioid analgesia in conjunction with ketorolac. Table 2 describes the distribution of analgesia administration by race. In bivariable analysis, there were no statistically significant differences in administration of any analgesia by race; however, black patients were less likely to receive opioid analgesia than white patients (20.7% [95% CI, 5.3%–36.0%] vs 43.1% [95% CI, 34.6%–51.4%], respectively; OR = 0.3 [95% CI, 0.1–0.9]).
Table 2.
Unadjusted Analgesia Administration and Opioid Administration by Race
| Race | Proportion Receiving, % (95% CI) | ||
|---|---|---|---|
| Any Analgesia | Type of Analgesia | ||
| Nonopioid | Opioid | ||
| White | 57.0 (49.2–64.8) | 13.9 (13.4–14.6) | 43.1 (34.6–51.4) |
| Black | 54.8 (34.3–75.3) | 34.1 (29.0–39.3) | 20.7 (5.3–36.0) |
In bivariable analysis, we also found that older age (P = .01) and higher pain score (P = .007) were significantly associated with administration of any analgesia. With respect to opioid administration, we found statistically significant differences in administration with higher pain score (P = .01) only. There were no statistically significant differences by ethnicity in any analgesia administration (52.9% for Hispanic patients vs 58.0% for non-Hispanic patients; P = .58) or opioid administration (36.5% for Hispanic patients vs 42.8% for non-Hispanic patients; P = .47). Furthermore, there were no statistically significant differences in any analgesia administration or opioid administration by sex, insurance status, triage level, geographic region, or ED type. Additionally, there was no statistically significant difference in trends of analgesia administration or opioid administration by year during the period studied. Moreover, there was no significant interaction between sex and pain score.
When stratified by pain score and adjusted for ethnicity (Figure 1), black patients with moderate pain were less likely to receive any analgesia than white patients (15.7% [95% CI, 0.1%–39.5%] vs 58.5% [95% CI, 45.8%–71.1%], respectively; adjusted OR = 0.1 [95% CI, 0.02–0.8]). Among those with severe pain, black patients were less likely to receive opioids than white patients (24.5% [95% CI, 1.1%–48.0%] vs 58.3% [95% CI, 46.1%–70.4%], respectively; adjusted OR = 0.2 [95% CI, 0.06–0.9]).
Figure 1.
Predicted Probabilities for Analgesic and Opioid Administration by Race Stratified by Pain Score and Adjusted for Ethnicity
A, Moderate pain. B, Severe pain.
a Statistically significant difference in administration (P < .05).
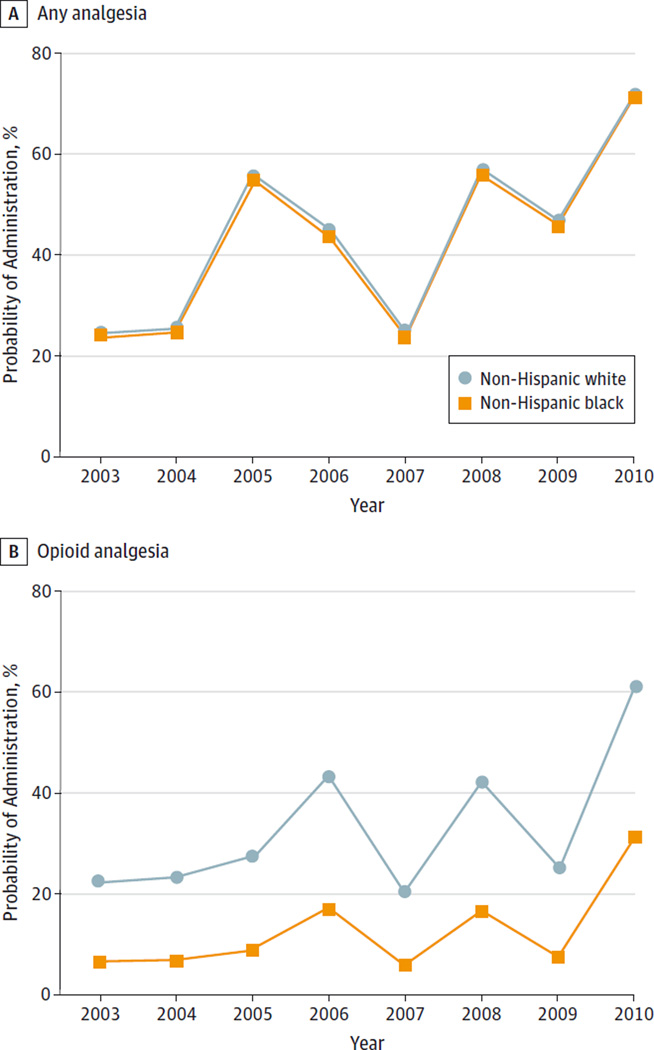
Table 3 displays the results of our multivariable analysis, which included ethnicity, age, sex, insurance status, triage level, and pain score as covariates. There was no statistically significant difference in overall analgesia administration by race, but there was a statistically significant difference in opioid administration by race. Black children with appendicitis were less likely to receive opioid analgesia than white children (12.2% [95% CI, 0.1%–35.2%] vs 33.9% [95% CI, 0.6%–74.9%], respectively; adjusted OR = 0.2 [95% CI, 0.06–0.8]). No other covariates achieved statistical significance in the multivariable model. Figure 2 illustrates trends in overall analgesia administration and opioid administration by race over time, adjusted for ethnicity, age, sex, insurance status, triage level, and pain score. When adjusted for covariates and time trend, the differences between white and black race in opioid administration remained stable and statistically significant (P = .03), although the time trend variable was not (P = .72).
Table 3.
Multivariable Analysis of Overall Analgesia and Opioid Administration by Racea
| Any Analgesia Administration | Opioid Administration | |||
|---|---|---|---|---|
| Race | Predicted Probability, % (95% CI) |
AOR (95% CI) | Predicted Probability, % (95% CI) |
AOR (95% CI) |
| White | 48.3 (12.2–84.4) | 1 [Reference] | 33.9 (0.6–74.9) | 1 [Reference] |
| Black | 42.0 (2.9–81.0) | 0.7 (0.3–1.8) | 12.2 (0.1–35.2) | 0.2 (0.06–0.8) |
Abbreviation: AOR, adjusted odds ratio.
Adjusted for ethnicity, age, sex, insurance status, triage level, and pain score.
Figure 2.
Adjusted Predicted Probabilities for Analgesia and Opioid Administration by Race Over Time
A, Any analgesia. B, Opioid analgesia. Adjusted for ethnicity, age, sex, insurance status, triage level, and pain score.
Discussion
In this nationally representative cross-sectional analysis of ED visits of children diagnosed as having appendicitis, we found low rates of analgesia and opioid administration overall and marked racial differences in opioid administration. Black children had one-fifth the odds of receiving opioid analgesia than white children, even after adjustment for potential confounders.
Overall, the rate of administration of analgesia to children diagnosed as having appendicitis in the ED was low. Only 56.8% of our study population received any analgesia, and only 41.3% received any opioid analgesia. These findings are consistent with other studies that have demonstrated low rates of administration of analgesia to patients with appendicitis.21, 26, 27 Such low rates of administration may be due to the persistent perceptions among clinicians that analgesia may lead to diagnostic delays by masking disease. However, several randomized trials have demonstrated that opioid analgesia in the management of acute abdominal pain is safe and does not have a negative impact on diagnosis or treatment.28–32 Regardless, this phenomenon would not explain the racial disparity we observed in the administration of opioid analgesia.
Oligoanalgesia may be further exaggerated in the care of children, as clinicians may be concerned about adverse outcomes with administration of opioids. One study found that children with histologically proven appendicitis were less likely to receive opioids than adults,33 and similar trends have been found in the management of pain from sickle cell vasoocclusive crises,34 fractures,34, 35 and burns34 with children being much less likely to receive analgesia than adults. Furthermore, despite pain management becoming a quality indicator by The Joint Commission in 2000, we did not see a significant increase in analgesia use over time. Additionally, racial disparities with respect to opioid administration remained constant during the period as well.
Eliminating racial health disparities has been one of the overarching goals of the Healthy People initiative.36 Although there are many complex factors for these health disparities, there is growing evidence that the quality of care delivered to minority patients is less than that received by white patients. In fact, the 2003 Institute of Medicine report found evidence that “stereotyping, biases, and uncertainty on the part of healthcare providers can all contribute to unequal treatment”37 of racial and ethnic minorities. Our study and documentation of racial disparities in children with acute abdominal pain associated with appendicitis allow for future efforts, including electronic health record–embedded clinical pathways, to work toward minimizing these disparities.
Opioid administration remains a cornerstone in the management of abdominal pain associated with appendicitis.23 The racial disparities we identified with respect to opioid administration were striking. It was surprising that although there were no differences in overall analgesia administration by race, black patients were much less likely to receive opioid analgesia than white patients even after adjustment for potential confounders, including pain score. Our findings suggest that although clinicians may recognize pain equally across racial groups, they may be reacting to the pain differently by treating black patients with nonopioid analgesia, such as ibuprofen and acetaminophen, while treating white patients with opioid analgesia for similar pain.
A prior study evaluating racial disparities in ED analgesia prescription for all conditions found trends similar to ours. That is, even though there were no racial differences in overall analgesia prescriptions, black patients were less likely than white patients to receive opioid analgesia.11 The authors of that study postulated that the greater disparities noted for opioid prescriptions than for nonopioid prescriptions may be because prescribing an opioid requires more trust of the patient by the physician.11 However, in our study, we evaluated medications administered in the ED (and not prescriptions). No patients with appendicitis were discharged home from the ED. Alternatively, a similar study using NHAMCS data to evaluate pain management of children undergoing ED management for isolated long-bone fractures found no such racial differences in analgesia administration.38 It is unclear why such a striking racial disparity was found with respect to pain management in childhood appendicitis but not in long-bone fractures. Furthermore, a recent single-center study at a pediatric ED did not find racial differences in opioid administration among children diagnosed as having appendicitis.21 However, this study was underpowered to detect such differences with only a total of 404 children with appendicitis, of whom fewer than 10% were black patients.
Not surprisingly, as pain scores increased, the use of any analgesia (including opioid analgesia) increased overall. However, there appeared to be a threshold effect with respect to administration of analgesia by race. Black patients with moderate pain were less likely to receive any analgesia, and black patients with severe pain were less likely to be treated with opioids. This analysis by pain strata suggests that there may be a higher threshold of pain score for administering analgesia to black patients with appendicitis.
Although we found disparities with respect to opioid administration by race, unlike other studies,11 we found no differences in opioid administration by ethnicity. This may be partially explained by the observations that Hispanic children are more likely to present with appendiceal perforation rather than uncomplicated appendicitis39, 40 and therefore may be more ill appearing and in worse pain on presentation. However, we found no differences in triage acuity level or pain score by race or ethnicity.
There are several potential limitations to this study. First, it is possible that patients declined analgesia despite having pain, and this phenomenon could be different between races. Unfortunately, the database we used and the study design do not allow us to test this hypothesis. Second, there is the possibility of misclassification errors in abstracting medication data. However, unless there were a systematic bias in abstracting medication databased on patient race, this should occur randomly and would not affect our results. Third, pain score was abstracted only at triage, whereas analgesia administration was abstracted from the entire visit. Therefore, it is possible that as a patient’s pain level increased, analgesia was administered. However, this should not have been different between racial groups. Furthermore, we are unable to account for any analgesia patients may have received prior to ED arrival (eg, via emergency medical services or in another ED prior to transfer). However, given that we adjusted for pain score and that we found no racial differences in pain scores, prior treatment of pain should not affect our results. Moreover, pain medications are uncommonly provided during emergency medical services transport. It is important to note that NHAMCS data are available only through 2010. Therefore, it is possible that there have been improvements in analgesia administration and a reduction in racial differences in analgesia administration in more recent years. However, to our knowledge, there has not been any published literature with more recent data. Finally, race and ethnicity, as reported in the NHAMCS, were determined by someone other than the patient. This may have led to some patients being categorized differently than their self-identified racial and ethnic group. However, in the context of studying disparities, the perception of patients’ race and ethnicity may be more important than patients’ self-classification.
Conclusions
Our findings suggest that there are racial disparities in opioid administration to children with appendicitis, even after adjustment for potential confounders. More research is needed to understand why such disparities exist. This could help inform the design of interventions to address and eliminate these disparities and to improve pain management for all youths.
At a Glance.
The purpose was to identify racial disparities in administration of analgesia, specifically opioid analgesia, to children diagnosed as having appendicitis in the emergency department using a large national database (the National Hospital Ambulatory Medical Care Survey).
Only 56.8% of almost 1 million children evaluated in EDs who were diagnosed as having appendicitis received any analgesia, and only 41.3% received at least 1 dose of opioid analgesia.
In a multivariable model with adjustment for age, ethnicity, sex, insurance status, triage level, and pain score, black patients were significantly less likely to receive opioid analgesia than white patients (12.2% [95% CI, 0.1%–35.2%] vs 33.9% [95% CI, 0.6%–74.9%], respectively; adjusted odds ratio = 0.2 [95% CI, 0.06–0.8]).
Acknowledgments
Funding/Support: This work was supported by grant K23 HD070910 from the National Institutes of Health (Dr Goyal).
Role of the Funder/Sponsor: The National Institutes of Health had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Footnotes
Author Contributions: Dr Goyal had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Goyal, Kuppermann, Teach, Chamberlain.
Acquisition, analysis, or interpretation of data: All authors.
Drafting of the manuscript: Goyal, Chamberlain.
Critical revision of the manuscript for important intellectual content: Kuppermann, Cleary, Teach, Chamberlain.
Statistical analysis: Goyal, Cleary, Chamberlain.
Obtained funding: Goyal.
Study supervision: Kuppermann, Teach, Chamberlain.
Conflict of Interest Disclosures: None reported.
REFERENCES
- 1.Groman R, Ginsburg J. American College of Physicians. Racial and ethnic disparities in health care: a position paper of the American College of Physicians. Ann Intern Med. 2004;141(3):226–232. doi: 10.7326/0003-4819-141-3-200408030-00015. [DOI] [PubMed] [Google Scholar]
- 2.Fiscella K, Franks P, Gold MR, Clancy CM. Inequality in quality: addressing socioeconomic, racial, and ethnic disparities in health care. JAMA. 2000;283(19):2579–2584. doi: 10.1001/jama.283.19.2579. [DOI] [PubMed] [Google Scholar]
- 3.Cheng TL, Goodman E Committee on Pediatric Research. Race, ethnicity, and socioeconomic status in research on child health. Pediatrics. 2015;135(1):e225–e237. doi: 10.1542/peds.2014-3109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wilper AP, Woolhandler S, Lasser KE, et al. Waits to see an emergency department physician: US trends and predictors, 1997–2004. Health Aff (Millwood) 2008;27(2):w84–w95. doi: 10.1377/hlthaff.27.2.w84. [DOI] [PubMed] [Google Scholar]
- 5.James CA, Bourgeois FT, Shannon MW. Association of race/ethnicity with emergency department wait times. Pediatrics. 2005;115(3):e310–e315. doi: 10.1542/peds.2004-1541. [DOI] [PubMed] [Google Scholar]
- 6.Chamberlain JM, Joseph JG, Patel KM, Pollack MM. Differences in severity-adjusted pediatric hospitalization rates are associated with race/ethnicity. Pediatrics. 2007;119(6):e1319–e1324. doi: 10.1542/peds.2006-2309. [DOI] [PubMed] [Google Scholar]
- 7.Natale JE, Joseph JG, Rogers AJ, et al. PECARN (Pediatric Emergency Care Applied Research Network) Cranial computed tomography use among children with minor blunt head trauma: association with race/ethnicity. Arch Pediatr Adolesc Med. 2012;166(8):732–737. doi: 10.1001/archpediatrics.2012.307. [DOI] [PubMed] [Google Scholar]
- 8.Pletcher MJ, Kertesz SG, Kohn MA, Gonzales R. Trends in opioid prescribing by race/ethnicity for patients seeking care in US emergency departments. JAMA. 2008;299(1):70–78. doi: 10.1001/jama.2007.64. [DOI] [PubMed] [Google Scholar]
- 9.Tsai CL, Sullivan AF, Gordon JA, et al. Racial/ethnic differences in emergency care for joint dislocation in 53 US EDs. Am J Emerg Med. 2012;30(9):1970–1980. doi: 10.1016/j.ajem.2012.04.023. [DOI] [PubMed] [Google Scholar]
- 10.Quazi S, Eberhart M, Jacoby J, Heller M. Are racial disparities in ED analgesia improving? evidence from a national database. Am J Emerg Med. 2008;26(4):462–464. doi: 10.1016/j.ajem.2007.05.007. [DOI] [PubMed] [Google Scholar]
- 11.Tamayo-Sarver JH, Hinze SW, Cydulka RK, Baker DW. Racial and ethnic disparities in emergency department analgesic prescription. Am J Public Health. 2003;93(12):2067–2073. doi: 10.2105/ajph.93.12.2067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Young MF, Hern HG, Alter HJ, Barger J, Vahidnia F. Racial differences in receiving morphine among prehospital patients with blunt trauma. J Emerg Med. 2013;45(1):46–52. doi: 10.1016/j.jemermed.2012.07.088. [DOI] [PubMed] [Google Scholar]
- 13.Hostetler MA, Auinger P, Szilagyi PG. Parenteral analgesic and sedative use among ED patients in the United States: combined results from the National Hospital Ambulatory Medical Care Survey (NHAMCS) 1992–1997. Am J Emerg Med. 2002;20(3):139–143. doi: 10.1053/ajem.2002.33002. [DOI] [PubMed] [Google Scholar]
- 14.Johnson TJ, Weaver MD, Borrero S, et al. Association of race and ethnicity with management of abdominal pain in the emergency department. Pediatrics. 2013;132(4):e851–e858. doi: 10.1542/peds.2012-3127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mills AM, Shofer FS, Boulis AK, Holena DN, Abbuhl SB. Racial disparity in analgesic treatment for ED patients with abdominal or back pain. Am J Emerg Med. 2011;29(7):752–756. doi: 10.1016/j.ajem.2010.02.023. [DOI] [PubMed] [Google Scholar]
- 16.Heron SL, Stettner E, Haley LL., Jr Racial and ethnic disparities in the emergency department: a public health perspective. Emerg Med Clin North Am. 2006;24(4):905–923. doi: 10.1016/j.emc.2006.06.009. [DOI] [PubMed] [Google Scholar]
- 17.Brown LE, Burton R, Hixon B, et al. Factors influencing emergency department preference for access to healthcare. West J Emerg Med. 2012;13(5):410–415. doi: 10.5811/westjem.2011.11.6820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Blanchard JC, Haywood YC, Scott C. Racial and ethnic disparities in health: an emergency medicine perspective. Acad Emerg Med. 2003;10(11):1289–1293. doi: 10.1111/j.1553-2712.2003.tb00615.x. [DOI] [PubMed] [Google Scholar]
- 19.Baker DW, Stevens CD, Brook RH. Determinants of emergency department use: are race and ethnicity important? Ann Emerg Med. 1996;28(6):677–682. doi: 10.1016/s0196-0644(96)70093-8. [DOI] [PubMed] [Google Scholar]
- 20.Zimmer KP, Walker A, Minkovitz CS. Epidemiology of pediatric emergency department use at an urban medical center. Pediatr Emerg Care. 2005;21(2):84–89. doi: 10.1097/01.pec.0000159050.19188.23. [DOI] [PubMed] [Google Scholar]
- 21.Caperell K, Pitetti R, Cross KP. Race and acute abdominal pain in a pediatric emergency department. Pediatrics. 2013;131(6):1098–1106. doi: 10.1542/peds.2012-3672. [DOI] [PubMed] [Google Scholar]
- 22.Fein JA, Zempsky WT, Cravero JP Committee on Pediatric Emergency Medicine and Section on Anesthesiology and Pain Medicine, American Academy of Pediatrics. Relief of pain and anxiety in pediatric patients in emergency medical systems. Pediatrics. 2012;130(5):e1391–e1405. doi: 10.1542/peds.2012-2536. [DOI] [PubMed] [Google Scholar]
- 23.Cole MA, Maldonado N. Evidence-based management of suspected appendicitis in the emergency department. Emerg Med Pract. 2011;13(10):1–29. [PubMed] [Google Scholar]
- 24.Rich A. Comparative Pain Scale. [Accessed November 12, 2013]; https://lane.stanford.edu/portals/cvicu/HCP_Neuro_Tab_4/0-10_Pain_Scale.pdf. [Google Scholar]
- 25.Korn EL, Graubard EL. Analysis of Health Surveys. New York, NY: John Wiley & Sons; 1999. [Google Scholar]
- 26.Goldman RD, Crum D, Bromberg R, Rogovik A, Langer JC. Analgesia administration for acute abdominal pain in the pediatric emergency department. Pediatr Emerg Care. 2006;22(1):18–21. doi: 10.1097/01.pec.0000195761.97199.37. [DOI] [PubMed] [Google Scholar]
- 27.Tsze DS, Asnis LM, Merchant RC, Amanullah S, Linakis JG. Increasing computed tomography use for patients with appendicitis and discrepancies in pain management between adults and children: an analysis of the NHAMCS. Ann Emerg Med. 2012;59(5):395–403. doi: 10.1016/j.annemergmed.2011.06.010. [DOI] [PubMed] [Google Scholar]
- 28.Green R, Bulloch B, Kabani A, Hancock BJ, Tenenbein M. Early analgesia for children with acute abdominal pain. Pediatrics. 2005;116(4):978–983. doi: 10.1542/peds.2005-0273. [DOI] [PubMed] [Google Scholar]
- 29.Ciarrocchi A, Amicucci G. Safety and impact on diagnostic accuracy of early analgesia in suspected acute appendicitis: a meta-analysis. Int J Surg. 2013;11(9):847–852. doi: 10.1016/j.ijsu.2013.08.005. [DOI] [PubMed] [Google Scholar]
- 30.Amoli HA, Golozar A, Keshavarzi S, Tavakoli H, Yaghoobi A. Morphine analgesia in patients with acute appendicitis: a randomised double-blind clinical trial. Emerg Med J. 2008;25(9):586–589. doi: 10.1136/emj.2007.050914. [DOI] [PubMed] [Google Scholar]
- 31.Bailey B, Bergeron S, Gravel J, Bussières JF, Bensoussan A. Efficacy and impact of intravenous morphine before surgical consultation in children with right lower quadrant pain suggestive of appendicitis: a randomized controlled trial. Ann Emerg Med. 2007;50(4):371–378. doi: 10.1016/j.annemergmed.2007.04.018. [DOI] [PubMed] [Google Scholar]
- 32.Kokki H, Lintula H, Vanamo K, Heiskanen M, Eskelinen M. Oxycodone vs placebo in children with undifferentiated abdominal pain: a randomized, double-blind clinical trial of the effect of analgesia on diagnostic accuracy. Arch Pediatr Adolesc Med. 2005;159(4):320–325. doi: 10.1001/archpedi.159.4.320. [DOI] [PubMed] [Google Scholar]
- 33.Furyk J, Sumner M. Pain score documentation and analgesia: a comparison of children and adults with appendicitis. Emerg Med Australas. 2008;20(6):482–487. doi: 10.1111/j.1742-6723.2008.01133.x. [DOI] [PubMed] [Google Scholar]
- 34.Selbst SM, Clark M. Analgesic use in the emergency department. Ann Emerg Med. 1990;19(9):1010–1013. doi: 10.1016/s0196-0644(05)82565-x. [DOI] [PubMed] [Google Scholar]
- 35.Brown JC, Klein EJ, Lewis CW, Johnston BD, Cummings P. Emergency department analgesia for fracture pain. Ann Emerg Med. 2003;42(2):197–205. doi: 10.1067/mem.2003.275. [DOI] [PubMed] [Google Scholar]
- 36.US Department of Health and Human Services. Healthy People 2020. [Accessed September 13, 2012]; http://www.healthypeople.gov/2020/about/foundation-health-measures/Disparities.
- 37.Smedley BD, Stith AY, Nelson AR, editors. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: Institute of Medicine, National Academies Press; 2003. pp. 285–383. [PubMed] [Google Scholar]
- 38.Yen K, Kim M, Stremski ES, Gorelick MH. Effect of ethnicity and race on the use of pain medications in children with long bone fractures in the emergency department. Ann Emerg Med. 2003;42(1):41–47. doi: 10.1067/mem.2003.230. [DOI] [PubMed] [Google Scholar]
- 39.Zwintscher NP, Steele SR, Martin MJ, Newton CR. The effect of race on outcomes for appendicitis in children: a nationwide analysis. Am J Surg. 2014;207(5):748–753. doi: 10.1016/j.amjsurg.2013.12.020. [DOI] [PubMed] [Google Scholar]
- 40.Levas MN, Dayan PS, Mittal MK, et al. Pediatric Emergency Medicine Collaborative Research Committee of the American Academy of Pediatrics. Effect of Hispanic ethnicity and language barriers on appendiceal perforation rates and imaging in children. J Pediatr. 2014;164(6):1286–1291. e2. doi: 10.1016/j.jpeds.2014.01.006. [DOI] [PubMed] [Google Scholar]