Abstract
Background
Physiologic adaptations occurring across successive pregnancies may increase the risk of adverse cardiovascular health outcomes in later life.
Methods and Results
The association between parity and metabolic syndrome (MetS) was examined among 7,467 Hispanic/Latina women of diverse backgrounds, aged 18–74 years, who participated in the Hispanic Community Health Study/Study of Latinos (HCHS/SOL) from 2008–2011. MetS components were defined according to AHA/NHLBI criteria and included abdominal obesity, elevated triglycerides, low HDL cholesterol, high blood pressure, and elevated fasting glucose. Logistic regression models estimated odds ratios adjusting for socio-demographic, behavioral, and reproductive characteristics. At HCHS/SOL baseline, women reported none (21.1%), one (19.9%), two (25.7%), three (18.6%), four (8.8%), and five or more (5.9%) live births. Compared to women with one birth, those with four births had the highest odds of abdominal obesity (OR=2.0, 95%CI 1.5, 2.8) and overall MetS (OR=1.4, 95%CI 1.0, 2.0) and those with five or more births had the highest odds of low HDL cholesterol (OR=1.5, 95%CI 1.2, 2.0) and elevated fasting glucose (OR=1.6, 95%CI 1.1, 2.4), after adjusting for age, background, education, marital status, income, nativity, smoking, physical activity, menopause, oral contraceptive use, hormone therapy, and field center. Further adjustment for percent body fat attenuated these associations. No associations were observed between parity and elevated triglycerides or high blood pressure.
Conclusions
Higher parity is associated with an increased prevalence of selected components of the MetS among Hispanic/Latina women in the U.S. High parity among Hispanics/Latinas with a high prevalence of abdominal obesity suggests high risk for metabolic dysregulation.
Keywords: parity, pregnancy, metabolic syndrome, Hispanic women, Latina, cohort
Cardiovascular disease (CVD) is a leading cause of morbidity and mortality among women in the United States. In 2013, approximately 365,000 U.S. women died from heart disease and stroke.1 Metabolic risk factors have been identified for CVD, including abdominal obesity, elevated triglycerides, low high-density lipoprotein (HDL) cholesterol, high blood pressure, and elevated fasting glucose; a combination of three or more of these risk factors is known as the “metabolic syndrome” (MetS).2 The MetS is associated with an increased risk of adverse cardiovascular health outcomes, particularly among women.3,4
Lactation, hormonal contraceptive use, and polycystic ovary syndrome (PCOS) are factors unique to women that are associated with the MetS.4 Menopause and pregnancy can also impact the prevalence and characteristics of the MetS.4 Pregnancy, in particular, is a time when women experience physiological changes and are at risk of pregnancy-related complications, some of which are associated with a higher risk of adverse cardiovascular health outcomes in later life.5–8 Physiologic adaptations and complications occurring across successive pregnancies may be associated with an even higher risk of adverse cardiovascular outcomes.8 Previous studies have examined the association between parity and the MetS, but they have been limited by small sample sizes9–11 and study populations that were predominantly of non-Hispanic background.10,12–17 To our knowledge, no studies have examined the association between parity and the MetS in a U.S. Hispanic/Latina population.
Hispanic/Latina women have a higher prevalence of the MetS than non-Hispanic women.18 Between 2003 and 2006, the prevalence of the MetS was approximately 41% among U.S. Mexican American women compared to 32% among non-Hispanic white women.18 A more recent estimate of the age-standardized prevalence of the MetS among Hispanic/Latina women from four US cities was 36% (34.6%–37.4%).19 Latinos are also the fastest-growing minority population in the U.S. and Hispanic/Latina women report higher fertility and birth rates than their non-Hispanic counterparts.20 Thus, understanding the impact of parity on the MetS is important for informing preventive efforts to decrease the prevalence of metabolic and cardiovascular disorders in this population.
Our objective was to examine the association between parity and the prevalence of the five components of the MetS among a cohort of Hispanic/Latina women enrolled in the Hispanic Community Health Study/Study of Latinos (HCHS/SOL). We hypothesized that nulliparous (no prior live births) and multiparous (multiple live births) women would have a higher prevalence of each of the five components of the MetS as compared to primiparous (one live birth) women, with a J-shaped association expected.
METHODS
Study Population
The HCHS/SOL is a prospective, population-based cohort study of Hispanics/Latinos of diverse backgrounds, including individuals self-identifying as Cuban, Dominican, Mexican, Puerto Rican, Central American, and South American. The HCHS/SOL cohort was selected through a stratified multistage area probability sample in four U.S. field centers (Bronx, Chicago, Miami, and San Diego). Census block groups were randomly selected from specified areas within each community, and households were randomly selected from each block group. At both stages, the study oversampled areas with a high concentration of Hispanics/Latinos, households with a Hispanic/Latino surname, and individuals aged 45 to 74 years. Individuals were excluded from the study if they were planning to move from the area within six months, unable to travel to the study site, or unable to complete the questionnaires. Pregnant women were asked to reschedule their visit after delivery. More details about the study design and methods have been previously described.21,22 This study was approved by the Institutional Review Boards at the Albert Einstein College of Medicine, Northwestern University, San Diego State University, University of Miami, and the University of North Carolina at Chapel Hill. Informed consent was obtained for all study participants.
Between 2008 and 2011, 16,415 men and women, aged 18 to 74 years, were recruited for participation. For this analysis, we excluded males (n=6,580). We also excluded 2,368 women who did not meet at least one of the inclusion criteria, including those who were reportedly pregnant at baseline (n=14); those with missing (n=207) or implausible (n=5) data for parity or missing data for any of the MetS components (n=133); and those with self-reported or diagnosed diabetes at baseline (n=2,102). Diabetics were excluded to assess the relationship between parity and MetS in an otherwise healthy population. The final sample included 7,467 women.
Baseline Examination
Participants completed a baseline clinical examination for which they were asked to fast, abstain from smoking for at least 12 hours, and abstain from vigorous physical activity the morning of the visit.22 This examination included assessments of anthropometrics, blood pressure, oral glucose tolerance, and several other biological measures. Weight (measured to the nearest 0.1kg) and height (recorded to the nearest centimeter) were obtained and waist circumference (recorded to the nearest centimeter) was measured. Weight and body composition were measured using the Tanita scale and percent body fat was provided by a bioelectrical impedance method. After a 5-minute rest period, three seated blood pressure measurements were obtained with an automatic sphygmomanometer; the second and third readings were averaged and used in this analysis.
Study participants provided blood samples according to standardized protocols and samples were shipped to the HCHS/SOL Central Laboratory for processing. High-density lipoprotein cholesterol (HDL-C) was measured using a direct magnesium/dextran sulfate method and fasting plasma glucose was measured using a hexokinase enzymatic method (Roche Diagnostics, Indianapolis, Indiana). Serum triglycerides were measured on a Roche Modular P chemistry analyzer using a glycerol blanking enzymatic method (Roche Diagnostics). The assay methodologies are described in HCHS/SOL Manual 7a (available at: https://www2.cscc.unc.edu/hchs/system/files/protocols-manuals/UNLICOMMManual07AddendumCentralLaboratoryProceduresv1006222011.pdf).
Participants completed interviewer-administered questionnaires with information collected about demographics, health behaviors, and medical history. They were also asked to report all prescription and nonprescription medications and supplements. To overcome language barriers, all questionnaires were offered in English or Spanish based on the participant’s preference by bilingual staff who were centrally trained. All questionnaires were translated by a certified service using culturally sensitive translation to ensure the use of language that could be interpreted correctly by all Hispanic/Latino backgrounds, and pilot tested at all sites. Among the 7467 women included in our analysis, 80.3% (n=5,999) preferred Spanish questionnaires.
Measures
Parity
Parity was defined as the number of prior live births as reported by women on the interviewer-administered questionnaire. For this analysis, parity was categorized as: none (nulliparity), one, two, three, four, and five or more (grand-multiparity) prior live births. For secondary analyses, parity was modeled as a continuous measure.
Components of the metabolic syndrome
The components of the metabolic syndrome were classified according to the American Heart Association/National Heart, Lung, and Blood Institute 2009 Joint Scientific Statement2 and included: 1) abdominal obesity (waist circumference ≥88cm); 2) elevated triglycerides (≥150 mg/dL); 3) low HDL-C (<50 mg/dL); 4) high blood pressure (≥130 mmHg systolic or ≥85 mmHg diastolic or use of anti-hypertension medications); and 5) elevated fasting glucose (≥100 mg/dL or use of anti-diabetic medications). A combination of three or more of these factors comprised the overall MetS.
Covariates
Women reported their age, Hispanic/Latino background, years of education (categorized as <12 years, 12 years, or greater than 12 years), marital status, annual household income (categorized as <$20,000, $20,000–$40,000, $40,000–$75,000, >$75,000), and country of birth on the interviewer-administered questionnaire. Participants also reported current smoking status, physical activity (minutes per hour categorized as meeting the U.S. Department of Health and Human Services guidelines23 if they participated in the equivalent of ≥150 minutes of moderate-intensity activity or ≥75 minutes of vigorous-intensity activity), and reproductive history (menopausal status, history of oral contraceptive use, current hormone therapy).
Statistical Analysis
Descriptive analyses were conducted to examine participant characteristics by categories of parity at baseline. All reported means and prevalence estimates were weighted to account for the probability of selection and to partially adjust for differential nonresponse bias. Prevalence estimates of overall MetS and its components were estimated by parity using predicted marginals from logistic regression models and adjusted for weighted mean age in the analytic sample. Odds ratios (OR) and 95% confidence intervals (CI) were estimated from logistic regression models to assess the association between parity and MetS. Separate models were examined for each component of MetS and for overall MetS with several adjustments considered, including Model 1 (unadjusted), Model 2 (age), Model 3 (age, Hispanic/Latino background, education, marital status, income, nativity, smoking, physical activity, menopausal status, oral contraceptive use, hormone therapy, and field center), and Model 4 (covariates from Model 3 plus percent body fat). Model 4 was conducted to estimate the direct effect of parity on MetS independent of body fat because obesity is hypothesized to drive this association. Several coding strategies were used to assess the shape of the association between age and MetS. The effect of age was found to be linear for each component of the MetS and overall MetS, thus age was treated as a continuous variable for all adjusted analyses.
One prior live birth was chosen as the reference group to assess the hypothesis that there is a J-shaped association between parity and MetS. Women with no prior live births include those with a history of infertility or other reproductive issues as well as those who did not intend to have children. Conditions that contribute to infertility may be associated with risk factors for MetS, thus potentially increasing the prevalence of MetS among nulliparous women. Analyses were performed using SAS 9.3 software (SAS Institute, Cary, NC) or SUDAAN software Release 11 (RTI International, Research Triangle Park, NC).
RESULTS
Study Population
At HCHS/SOL baseline, the mean number of prior live births per woman was 1.97 (standard error, SE, 0.03) and ranged from 0 to 22. Women reported none (21.1%), one (19.9%), two (25.7%), three (18.6%), four (8.8%), and five or more (5.9%) prior live births. High percentages of women with five or more live births (i.e., grand multiparous women) did not complete high school, had a low family income, were overweight or obese, not born in the U.S., postmenopausal, and ever used oral contraceptives (Table). More than half of these women were of Mexican background (55.2%). Conversely, high percentages of women with one live birth completed some college, had a higher income, were normal weight, U.S. born, and premenopausal. Less than a third of these women were of Mexican background (31.0%). On average, women with five or more live births were the oldest and those with no prior live births were the youngest. Percent body fat, on average, was highest among those with four and five or more live births and lowest among those with no prior live births.
Table.
Characteristics of Hispanic/Latina women by parity (N=7,467), HCHS/SOL Study, 2008–2011.
| No prior live births (n=1103) |
One prior live birth (n=1205) |
Two prior live births (n=1968) |
Three prior live births (n=1685) |
Four prior live births (n=825) |
Five or more prior live births (n=681) |
|
|---|---|---|---|---|---|---|
| Overall, % | 21.1 | 19.9 | 25.7 | 18.6 | 8.8 | 5.9 |
| Age in years, mean (SE) | 27.3 (0.4) | 36.1 (0.5) | 42.7 (0.5) | 45.6 (0.6) | 46.1 (0.9) | 52.1 (0.8) |
| Hispanic/Latino background, % | ||||||
| Central American | 9.6 | 10.3 | 11.3 | 10.9 | 12.9 | 12.2 |
| Cuban | 12.6 | 23.6 | 18.8 | 7.4 | 3.9 | 3.8 |
| Dominican | 9.4 | 9.5 | 8.9 | 12.9 | 10.3 | 6.2 |
| Mexican | 40.7 | 31.0 | 37.3 | 45.3 | 50.1 | 55.2 |
| Puerto Rican | 11.5 | 12.5 | 14.7 | 15.3 | 15.9 | 14.4 |
| South American | 9.5 | 9.2 | 7.2 | 5.4 | 5.3 | 5.3 |
| Mixed | 6.6 | 3.9 | 1.9 | 2.9 | 1.7 | 2.9 |
| Education, % (SE) | ||||||
| Less than high school | 14.5 (1.4) | 22.5 (2.0) | 27.8 (1.7) | 39.0 (2.2) | 46.7 (3.1) | 71.4 (2.5) |
| High school graduate | 28.5 (1.7) | 28.9 (2.2) | 28.3 (1.6) | 23.5 (1.5) | 28.8 (3.3) | 13.5 (1.8) |
| At least some college | 57.1 (1.9) | 48.5 (2.2) | 43.9 (1.9) | 37.5 (2.2) | 24.4 (2.4) | 15.1 (1.9) |
| Married, % (SE) | 22.4 (1.8) | 51.0 (2.2) | 56.8 (1.7) | 57.5 (2.0) | 54.6 (3.0) | 51.5 (2.7) |
| U.S. Born, % (SE) | 42.8 (2.2) | 21.8 (1.9) | 16.8 (1.5) | 13.1 (1.2) | 17.9 (3.4) | 12.2 (1.8) |
| Annual family income, % (SE) | ||||||
| <$20,000 | 30.3 (1.8) | 47.3 (2.0) | 46.3 (1.8) | 48.9 (2.2) | 49.6 (3.0) | 55.9 (2.8) |
| $20,000–$40,000 | 31.6 (2.0) | 29.4 (2.1) | 29.1 (1.5) | 30.1 (2.0) | 29.3 (2.5) | 24.4 (2.6) |
| $40,000–$75,000 | 17.8 (2.0) | 9.8 (1.2) | 12.2 (1.0) | 10.2 (1.0) | 8.2 (1.4) | 4.5 (1.1) |
| >$75,000 | 5.3 (0.8) | 4.1 (0.8) | 4.0 (0.8) | 4.1 (1.6) | 2.0 (1.0) | 0.7 (0.4) |
| Not reported | 15.1 (1.4) | 9.4 (1.2) | 8.5 (0.9) | 6.8 (0.8) | 10.9 (1.8) | 14.5 (1.9) |
| Smoker, % (SE) | 16.1 (1.7) | 17.3(1.8) | 15.8 (1.2) | 15.2 (1.2) | 21.4 (3.4) | 14.4 (1.9) |
| Body mass index, % (SE) | ||||||
| Underweight | 4.6 (1.0) | 1.6 (0.4) | 0.6 (0.3) | 0.3 (0.2) | 0.2 (0.1) | 1.8 (1.3) |
| Normal weight | 39.7 (2.1) | 27.5 (2.0) | 21.5 (1.4) | 18.2 (1.3) | 11.2 (1.7) | 12.5 (1.9) |
| Overweight | 25.7 (1.8) | 35.0 (2.2) | 39.4 (1.7) | 38.5 (2.0) | 37.1 (2.9) | 37.3 (2.7) |
| Obese | 30.0 (2.0) | 35.9 (2.3) | 38.6 (2.0) | 43.0 (2.0) | 51.6 (3.1) | 48.4 (2.8) |
| Percent body fat, mean (SE) | 33.2 (0.5) | 36.9 (0.4) | 38.1 (0.3) | 38.7 (0.3) | 40.3 (0.5) | 39.6 (0.4) |
| Meets 2008 HHS PA guidelines, % (SE) | 68.2 (1.9) | 61.3 (2.1) | 57.4 (1.7) | 60.2 (2.0) | 61.3 (2.7) | 52.9 (2.6) |
| Postmenopausal, % (SE) | 6.4 (0.8) | 17.8 (1.4) | 27.7 (1.7) | 36.1 (2.0) | 34.5 (2.8) | 50.6 (2.9) |
| Hysterectomy, % (SE) | 2.6 (0.5) | 7.2 (1.4) | 9.9 (0.9) | 13.6 (1.3) | 15.5 (1.9) | 15.4 (1.9) |
| Ever used oral contraceptives, % (SE) | 42.7 (2.1) | 63.5 (2.1) | 65.7 (1.6) | 65.8 (2.0) | 68.6 (2.7) | 61.9 (2.7) |
| Current hormone therapy use, % (SE) | 2.3 (0.8) | 1.7 (0.5) | 3.0 (0.5) | 2.3 (0.4) | 2.5 (0.7) | 2.6 (0.7) |
Abbreviations: SE, standard error; PA, self-reported physical activity
NOTE: All values are percentages (SE) except age and percent body fat which are reported as mean (SE); all percentages (with the exception of Hispanic/Latino background) and means are weighted for study design and non-response
Age-Adjusted Prevalence of MetS Components by Parity
Among women at HCHS/SOL baseline, abdominal obesity was the most prevalent MetS component with age-adjusted prevalence estimates ranging from 61% (standard error, SE, 2.3) among those with no live births to 84% (SE=2.0) among those with four or more live births (Figure 1). Elevated fasting glucose was the least prevalent component with age-adjusted prevalence estimates ranging from 12% (SE=1.3) among women with one live birth to 21% (SE=2.4) among those with five or more live births. Among the parity groups, women with no live births had the lowest prevalence and those with five or more live births had the highest prevalence of abdominal obesity, elevated triglycerides, and low HDL-C while adjusting for age. Similar patterns were observed for the overall MetS.
Figure 1.
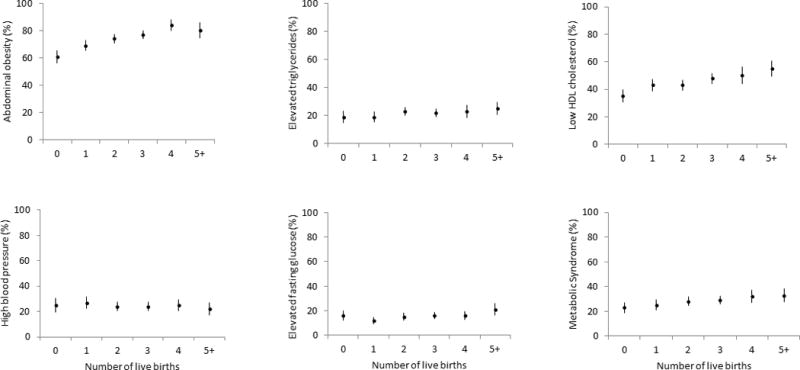
Age-adjusted prevalence (95% CI) of MetS components by parity (N=7,467), HCHS/SOL Study 2008–2011. Age adjusted at 39.6 years (weighted mean age in the analytic sample). Abdominal obesity (waist circumference ≥88cm), elevated triglycerides (≥150 mg/dL), low HDL cholesterol (<50 mg/dL), high blood pressure (≥130 mmHg systolic or ≥85 mmHg diastolic or use of anti-hypertension medications), elevated fasting glucose (≥100 mg/dL or use of anti-diabetic medications), overall metabolic syndrome (a combination of 3 or more components).
Parity and MetS Components
Compared to women with one live birth, those with four live births had the highest odds of abdominal obesity (OR=2.0, 95% CI 1.5, 2.8) and overall MetS (OR=1.4, 95% CI 1.0, 2.0) and those with five or more live births had the highest odds of low HDL-C (OR=1.5, 95% CI 1.2, 2.0) and elevated glucose (OR=1.6, 95% CI 1.1, 2.4), after adjusting for age, Hispanic/Latino background, education, marital status, income, nativity, smoking, physical activity, menopausal status, oral contraceptive use, hormone therapy, and field center (Figure 2; specific ORs and 95% CI for all models are located in Supplemental Table 1). Women with no live births had the lowest odds of abdominal obesity (OR=0.7; 95% CI 0.5, 0.9). Further adjustment for percent body fat attenuated the associations, including low HDL-C (OR=1.5; 95% CI 1.1, 2.0) and elevated fasting glucose (OR=1.5, 95% CI 1.0, 2.2), and the associations of parity with abdominal obesity and overall MetS were no longer statistically significant. No associations were observed between parity and elevated triglycerides or high blood pressure.
Figure 2.
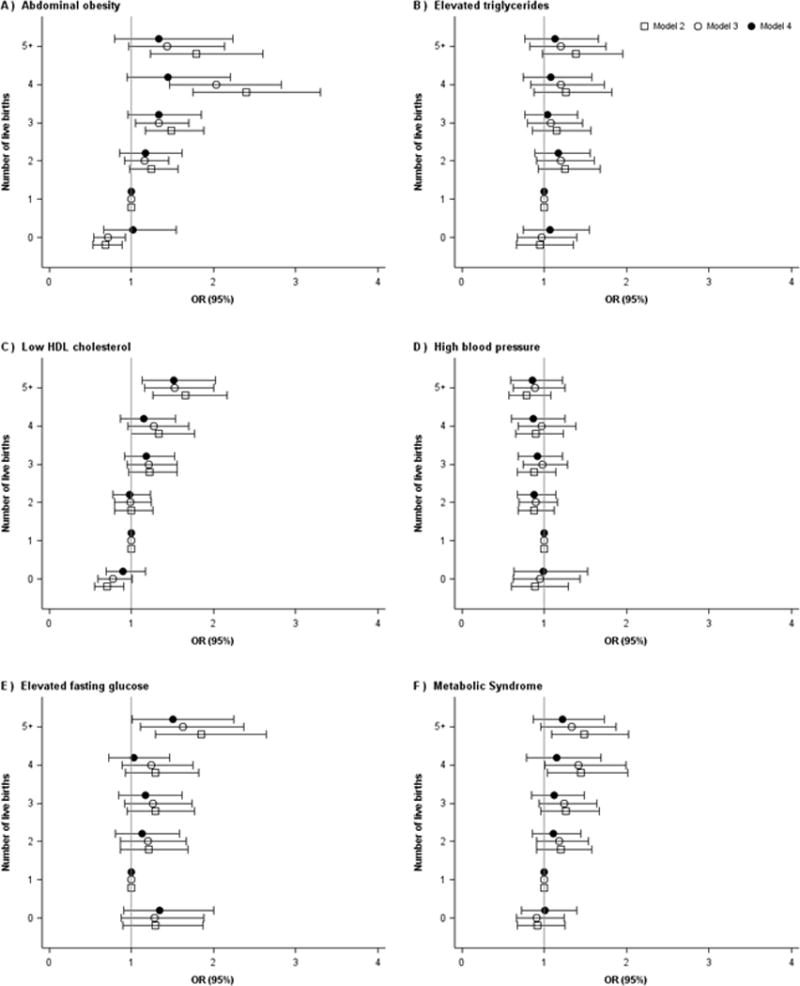
Adjusted odds ratios for the association between parity and components of the MetS (N=7,467), HCHS/SOL Study, 2008–2011. Model 2 (adjusted for age), Model 3 (adjusted for age, Hispanic/Latino background, education, marital status, income, nativity, smoking, physical activity, menopausal status, oral contraceptive use, hormone therapy, and field center), and Model 4 (adjusted for covariates from Model 3 plus percent body fat). Abdominal obesity (waist circumference ≥88cm), elevated triglycerides (≥150 mg/dL), low HDL cholesterol (<50 mg/dL), high blood pressure (≥130 mmHg systolic or ≥85 mmHg diastolic or use of anti-hypertension medications), elevated fasting glucose (≥100 mg/dL or use of anti-diabetic medications), overall metabolic syndrome (a combination of 3 or more components).
When assessing parity as a continuous measure, a dose-response effect was observed between increasing number of live births and both abdominal obesity and low HDL-C. For each additional birth (i.e., an increase of one birth in the exposure measure), the estimated ORs of both abdominal obesity and low HDL-C were 1.1 (95% CI 1.0, 1.2) after adjusting for all covariates in Model 4. A dose-response effect was not observed between number of live births and the prevalence of elevated triglycerides, high blood pressure, elevated fasting glucose, or overall MetS.
To further rule out confounding by age, we conducted a sensitivity analysis restricted to women aged 50 years and older. The results were similar, with the exception of low HDL cholesterol, fasting glucose, and abdominal obesity. Women with five or more live births had even higher odds of low HDL cholesterol compared to those with no prior live births (OR=2.2; 95% CI 1.4, 3.2) and the associations between parity and fasting glucose were attenuated and no longer statistically significant (Supplemental Table 2). Additionally, after adjustment for socio-demographic, behavioral, and reproductive characteristics, women with no live births had higher odds of abdominal obesity than those with one live birth (OR=1.8; 5% CI 0.9, 3.4), but the results were not statistically significant. Adjustment for percent body fat further attenuated this association (OR=1.3; 95% CI 0.6, 2.8).
DISCUSSION
To our knowledge, this is the first study to examine the association between parity and MetS in a U.S. Hispanic/Latina population. Multi-parity was associated with an increased prevalence of selected components of the MetS, particularly abdominal obesity, low HDL-C and elevated fasting glucose, after adjustment for socio-demographic, behavioral, and reproductive characteristics. In contrast to our hypothesis, a linear association was observed between parity and both abdominal obesity and low HDL-C such that each additional live birth increased the odds of these MetS components by 10%. With the exception of abdominal obesity, these associations persisted after further adjustment for percent body fat.
Prior studies of the association between parity and individual components of the metabolic syndrome have conflicting results. While our results are similar to those from studies among Chinese and U.S. populations that found a linear association between increasing parity and both higher waist circumference13 and an increased prevalence of abdominal obesity (waist circumference >88cm),12 respectively, they are in contrast to studies of Bangladeshi17 and Iranian15 women where no association was observed between parity and waist circumference, after adjustment for similar socio-demographic, lifestyle, and reproductive factors. Similarly, a few prior studies also noted a linear association between increasing parity and lower HDL-C12,13,15 while others found no association.16,17 In contrast to our findings, most prior studies did not find an association between parity and elevated fasting glucose,12,13,17 and a few studies observed a linear association between increasing parity and elevated triglycerides.12,15,16 The most consistent finding across studies, including the present study, was the lack of association observed between parity and blood pressure.12,13,15,16 Overall, these results suggest that parity may alter women’s metabolic profiles. However, the differences in results across prior studies indicates that specific MetS components may be more or less susceptible to change depending on the population.
Multi-parity of four or more live births was associated with a higher prevalence of the overall MetS in this population of Hispanic/Latina women; as expected, this association was attenuated and no longer statistically significant after adjustment for percent body fat. This finding is consistent with prior studies among other racial and ethnic groups that observed significant relationships between increasing parity and overall MetS,12,13,15,16 including statistically significant variations by history of gestational diabetes.14 Adjustment for BMI attenuated these earlier findings and the associations were no longer statistically significant for some.12,15 These results suggest that the relationship between parity and MetS may not be independent of obesity, thus adiposity or weight may mediate this association.
A combination of biological changes and lifestyle factors associated with childbearing may explain the associations that were observed. During pregnancy, women experience physiological changes, such as insulin resistance, dyslipidemia, fat accumulation, inflammation, and weight gain.24,25 While most of these alterations revert back to the non-pregnant state after delivery, some changes could persist and even accumulate across successive pregnancies.24,26,27 Additionally, changes in lifestyle risk factors (e.g., physical activity and stress) and the cumulative burden of caring for a larger family may impact the prevalence of the MetS and its components. In our study, adjustment for behavioral factors simultaneously with other socio-demographic and reproductive factors attenuated the results slightly. Additional assessment of the association between parity and MetS among HCHS/SOL men could provide further insight into the role of lifestyle factors in the prevalence of the MetS in this population.
Etiologic mechanisms of the MetS likely differ across racial and ethnic subgroups.28 In the U.S., Hispanic women are disproportionately affected by the MetS18 and have a higher prevalence of overweight and obesity than non-Hispanic white women.29 They also have more children and larger families than non-Hispanics.20 Among Hispanic/Latina women in the HCHS/SOL Study, abdominal obesity was the most prevalent MetS component and was highest among women with at least four prior live births, while elevated fasting glucose was the least prevalent MetS component across all parity categories. High parity and a high prevalence of abdominal obesity among these women may suggest a context of high risk for metabolic dysregulation. A better characterization of the links between pregnancy, adiposity, and body fat distribution is needed to further assess these associations.
Strengths and limitations
Overall, this study expands upon prior studies by examining parity and MetS in a large Hispanic/Latina population, while also assessing this association independent of body fat. The strengths of this study include the large, diverse cohort recruited from HCHS/SOL field centers that are located in cities with large Hispanic/Latino populations, thus allowing for a good representation of various backgrounds among participants. This study also measured anthropometrics and collected detailed information on a number of biological and behavioral measures, including percent body fat, which to our knowledge was not collected or assessed in prior studies.
This study has limitations. Like most prior studies of parity and MetS, the cross-sectional design limits the ability to establish temporality and assess changes in biological and lifestyle risk factors over time. The HCHS/SOL study lacked information on pregnancy-related complications, including diabetes and preeclampsia, which have been found to be associated with adverse cardiovascular health outcomes in later life7,30 and may contribute to the associations that were observed. Information on breastfeeding history was not collected in HCHS/SOL; however, breastfeeding rates among Latina women are higher than among other racial and ethnic groups.31 Lactation may reverse cardiometabolic adaptations occurring during pregnancy and fat accumulation,32,33 thus lowering the risk of metabolic syndrome12,34 and attenuating the association between parity and MetS.15 This study also lacked information on age at first live birth, which has been found to be associated with a decreased risk of MetS.10 There also may be additional unmeasured risk factors associated with multi-parity and MetS (e.g., stress). Residual confounding by these factors may have weakened the associations that were observed. Additionally, the generalizability of this study to other racial and ethnic groups may be limited.
CONCLUSION
Given the expected growth of the Hispanic/Latino population in the U.S., preventive action is needed to reduce metabolic and cardiovascular disease risks in this population, particularly women. Our study highlights the importance of multi-parity as a potential risk factor for developing selected components of the MetS that can ultimately impact the risk of CVD in later life. The 2011 American Heart Association’s Guidelines for CVD Prevention in Women35 recommend obtaining information on pregnancy history when evaluating cardiovascular risk for women. While these guidelines highlight the importance of capturing a detailed history of pregnancy complications, information on the number of prior live births may also be informative. Early identification of high-risk women based on their pregnancy history provides an opportunity for both primordial and primary prevention of CVD.
Supplementary Material
What is Known
Prior studies have conflicting results, with some suggesting a linear association between increasing parity and an increased prevalence of abdominal obesity and lower HDL cholesterol, and others suggesting no association between parity and waist circumference or HDL cholesterol.
Several prior studies found no association between parity and elevated fasting glucose.
What the Study Adds
Among Hispanic/Latina women, multi-parity is associated with an increased prevalence of abdominal obesity, low HDL cholesterol, and elevated fasting glucose, after adjustment for socio-demographic, behavioral, and reproductive characteristics.
Higher parity is not associated with an increased prevalence of elevated triglycerides or high blood pressure.
Multi-parity is associated with an increased prevalence of the overall MetS, but the association may not be independent of percent body fat.
Acknowledgments
The authors thank the staff and participants of the HCHS/SOL for their important contributions. A complete list of staff and investigators has been provided by Sorlie et al. in Ann Epidemiol. 2010; 20:642–649 and is also available on the study website: http://www.cscc.unc.edu/hchs
SOURCES OF FUNDING: CJV received financial support from grant T32-HL007055 from the National Heart, Lung, and Blood Institute (NHLBI), National Institutes of Health. The Hispanic Community Health Study/Study of Latinos was carried out as a collaborative study supported by contracts from the NHLBI to the University of North Carolina (N01-HC6533), University of Miami (N01-HC65234), Albert Einstein College of Medicine (N01-HC65235), Northwestern University (N01-HC65236), and San Diego State University (N01-HC65237). The following Institutes/Centers/Offices contribute to the HCHS/SOL through a transfer of funds to the NHLBI: National Center on Minority Health and Health Disparities, the National Institute of Deafness and Other Communications Disorders, the National Institute of Dental and Craniofacial Research, the National Institute of Diabetes and Digestive and Kidney Diseases, the National Institute of Neurological Disorders and Stroke, and the Office of Dietary Supplements.
Footnotes
DISCLOSURES
Drs. Ni, Sotres-Alvarez, and Vladutiu had full access to the study data and take responsibility for the integrity of the data and accuracy of analyses. All authors have reviewed and approved the final manuscript. None of the authors had any financial or other conflicts of interest
References
- 1.Centers for Disease Control and Prevention. Web-based Injury Statistics Query and Reporting System (WISQARS) [online] www.cdc.gov/ncipc/wisqars; Accessed October 5, 2015.
- 2.Alberti KG, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, Fruchart JC, james WP, Loria CM, Smith SC, Jr, International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation. 2009;120:1640–1645. doi: 10.1161/CIRCULATIONAHA.109.192644. [DOI] [PubMed] [Google Scholar]
- 3.Sarafidis PA, McFarlane SI, Bakris GL. Gender disparity in outcomes of care and management for diabetes and the metabolic syndrome. Curr Diab Rep. 2006;6:219–224. doi: 10.1007/s11892-006-0038-3. [DOI] [PubMed] [Google Scholar]
- 4.Bentley-Lewis R, Koruda K, Seely EW. The metabolic syndrome in women. Nature clinical practice. Endocrinol Metab. 2007;3:696–704. doi: 10.1038/ncpendmet0616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McDonald SD, Malinowski A, Zhou Q, Yusuf S, Devereaux PJ. Cardiovascular sequelae of preeclampsia/eclampsia: a systematic review and meta-analyses. Am Heart J. 2008;156:918–930. doi: 10.1016/j.ahj.2008.06.042. [DOI] [PubMed] [Google Scholar]
- 6.Bellamy L, Casas JP, Hingorani AD, Williams DJ. Pre-eclampsia and risk of cardiovascular disease and cancer in later life: systematic review and meta-analysis. BMJ. 2007;335:974. doi: 10.1136/bmj.39335.385301.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fraser A, Nelson SM, Macdonald-Wallis C, Cherry L, Butler E, Sattar N, Lawlor DA. Associations of pregnancy complications with calculated cardiovascular disease risk and cardiovascular risk factors in middle age: the Avon Longitudinal Study of Parents and Children. Circulation. 2012;125:1367–1380. doi: 10.1161/CIRCULATIONAHA.111.044784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Parikh NI, Cnattingius S, Dickman PW, Mittleman MA, Ludvigsson JF, Ingelsson E. Parity and risk of later-life maternal cardiovascular disease. Am Heart J. 2010;159:215–221. e216. doi: 10.1016/j.ahj.2009.11.017. [DOI] [PubMed] [Google Scholar]
- 9.Ortiz AP, Suarez E, Beauchamp G, Romaguera J, Soto-Salgado M, Perez CM. Correlates of the metabolic syndrome among a sample of women in the San Juan Metropolitan area of Puerto Rico. Metab Syndr Rel Disord. 2010;8:235–242. doi: 10.1089/met.2009.0076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cho GJ, Park HT, Shin JH, Kim T, Hur JY, Kim YT, Lee W, Kim SH. The relationship between reproductive factors and metabolic syndrome in Korean postmenopausal women: Korea National Health and Nutrition Survey 2005. Menopause. 2009;16:998–1003. doi: 10.1097/gme.0b013e3181a03807. [DOI] [PubMed] [Google Scholar]
- 11.Rodrigues AD, Theodoro H, Mendes KG, Paniz VM, de Lorenzi D, Anselmo Olinto MT. Factors associated with metabolic syndrome in climacteric women of southern Brazil. Climact. 2013;16:96–103. doi: 10.3109/13697137.2012.659099. [DOI] [PubMed] [Google Scholar]
- 12.Cohen A, Pieper CF, Brown AJ, Bastian LA. Number of children and risk of metabolic syndrome in women. J Women’s Health. 2006;15:763–773. doi: 10.1089/jwh.2006.15.763. [DOI] [PubMed] [Google Scholar]
- 13.Wu J, Xu G, Shen L, Zhang Y, Song L, Yang S, Yang H, Yuan J, Liang Y, Wang Y, Wu T. Parity and risk of metabolic syndrome among Chinese women. J Women’s Health. 2015;24:602–607. doi: 10.1089/jwh.2014.5134. [DOI] [PubMed] [Google Scholar]
- 14.Gunderson EP, Jacobs DR, Jr, Chiang V, Lewis CE, Tsai A, Quesenberry CP, Jr, Sidney S. Childbearing is associated with higher incidence of the metabolic syndrome among women of reproductive age controlling for measurements before pregnancy: the CARDIA study. Am J Obstet Gynecol. 2009;201:177, e171–179. doi: 10.1016/j.ajog.2009.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mousavi E, Gharipour M, Tavassoli A, Sadri GH, Sarrafzadegan N. Multiparity and risk of metabolic syndrome: Isfahan Healthy Heart Program. Metab Syndr Rel Disord. 2009;7:519–524. doi: 10.1089/met.2008.0076. [DOI] [PubMed] [Google Scholar]
- 16.Lao XQ, Thomas GN, Jiang CQ, Zhang WS, Yin P, Schooling M, Heys M, Leung GM, Adab P, Cheng KK, Lam TH. Parity and the metabolic syndrome in older Chinese women: the Guangzhou Biobank Cohort Study. Clin Endocrinol. 2006;65:460–469. doi: 10.1111/j.1365-2265.2006.02615.x. [DOI] [PubMed] [Google Scholar]
- 17.Akter S, Jesmin S, Rahman MM, Islam MM, Khatun MT, Yamaguchi N, Akashi H, Mizutani T. Higher gravidity and parity are associated with increased prevalence of metabolic syndrome among rural Bangladeshi women. PloS One. 2013;8:e68319. doi: 10.1371/journal.pone.0068319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ervin R. Prevalence of Metabolic Syndrome Among Adults 20 Years of Age and Over, by Sex, Age, Race and Ethnicity, and Body Mass Index: United States, 2003–2006. Nat Health Stat Rep. 2009;13:1–8. [PubMed] [Google Scholar]
- 19.Heiss G, Snyder ML, Teng Y, Schneiderman N, Llabre MM, Cowie C, Carnethon M, Kaplan R, Giachello A, Gallo L, Loehr L, Avilès-Santa L. Prevalence of metabolic syndrome among Hispanics/Latinos of diverse background: the Hispanic Community Health Study/Study of Latinos. Diab Care. 2014;37:2391–2399. doi: 10.2337/dc13-2505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Martin JA, Hamilton BE, Osterman MJ, Curtin SC, Matthews TJ. Births: final data for 2013. National Vital Stat Rep. 2015;64:1–65. [PubMed] [Google Scholar]
- 21.Lavange LM, Kalsbeek WD, Sorlie PD, Avilès-Santa LM, Kaplan RC, Barnhart J, Liu K, Giachello A, Lee DJ, Ryan J, Criqui MH, Elder JP. Sample design and cohort selection in the Hispanic Community Health Study/Study of Latinos. Ann Epidemiol. 2010;20:642–649. doi: 10.1016/j.annepidem.2010.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sorlie PD, Aviles-Santa LM, Wassertheil-Smoller S, Kaplan RC, Daviglus ML, Giachello AL, Schneiderman N, Raji L, Talavera G, Allison M, Lavange L, Chambless LE, Heiss G. Design and implementation of the Hispanic Community Health Study/Study of Latinos. Ann Epidemiol. 2010;20:629–641. doi: 10.1016/j.annepidem.2010.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.U.S. Department of Health & Human Services. Physical Activity Guidelines for Americans [online] 2008 http://www.health.gov/PAGUidelines/guidelines/default.aspx; Accessed January 19, 2016.
- 24.Gunderson EP, Murtaugh MA, Lewis CE, Quesenberry CP, West DS, Sidney S. Excess gains in weight and waist circumference associated with childbearing: The Coronary Artery Risk Development in Young Adults Study (CARDIA) Int J Obes Rel Metab Disord. 2004;28:525–535. doi: 10.1038/sj.ijo.0802551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Desoye G, Schweditsch MO, Pfeiffer KP, Zechner R, Kostner GM. Correlation of hormones with lipid and lipoprotein levels during normal pregnancy and postpartum. J Clin Endocrinol Metab. 1987;64:704–712. doi: 10.1210/jcem-64-4-704. [DOI] [PubMed] [Google Scholar]
- 26.Gunderson EP, Lewis CE, Murtaugh MA, Quesenberry CP, Smith West D, Sidney S. Long-term plasma lipid changes associated with a first birth: the Coronary Artery Risk Development in Young Adults study. Am J Epidemiol. 2004;159:1028–1039. doi: 10.1093/aje/kwh146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Smith D, Lewis C, Caveny J, Perkins L, Burke G, Bild D. Longitudinal changes in adiposity associated with pregnancy: The CARDIA Study. JAMA. 1994;271:1747–1751. [PubMed] [Google Scholar]
- 28.Ramos RG, Olden K. The prevalence of metabolic syndrome among US women of childbearing age. Am J Public Health. 2008;98:1122–1127. doi: 10.2105/AJPH.2007.120055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of obesity among adults: United States, 2011–2012. NCHS data brief. 2013:1–8. [PubMed] [Google Scholar]
- 30.Rich-Edwards JW, Fraser A, Lawlor DA, Catov JM. Pregnancy Characteristics and Women’s Future Cardiovascular Health: An Underused Opportunity to Improve Women’s Health? Epidemiol Rev. 2014;36:57–70. doi: 10.1093/epirev/mxt006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Scanlon KS, Grummer-Strawn LM, Chen J, Molinari N, Perrine CG. Racial and ethnic differences in breastfeeding initiation and duration by state – National Immunization Survey, United States, 2004–2008. MMWR. 2010;59:327–334. [PubMed] [Google Scholar]
- 32.Schwarz EB, Ray RM, Stuebe AM, Allison MA, Ness RB, Freiberg MS, Cauley JA. Duration of lactation and risk factors for maternal cardiovascular disease. Obstet Gynecol. 2009;113:974–982. doi: 10.1097/01.AOG.0000346884.67796.ca. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Stuebe AM, Rich-Edwards JW. The reset hypothesis: lactation and maternal metabolism. Am J Perinatol. 2009;26:81–88. doi: 10.1055/s-0028-1103034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ram KT, Bobby P, Hailpern SM, Lo JC, Schocken M, Skurnick J, Santoro N. Duration of lactation is associated with lower prevalence of the metabolic syndrome in midlife–SWAN, the study of women’s health across the nation. Am J Obstet Gynecol. 2008;198:268, e261–266. doi: 10.1016/j.ajog.2007.11.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mosca L, Benjamin EJ, Berra K, Bezanson JL, Dolor RJ, Lloyd-Jones DM, Newby LK, Pina IL, Roger VL, Shaw LJ, Zhao D, Beckie TM, Bushnell C, D’Armiento J, Kris-Etherton PM, Fang J, Ganiats TG, Gomes AS, Graca CR, Haan CK, Jackson EA, Judelson DR, Kelepouris E, Lavie CJ, Moore A, Nussmeier NA, Ofili E, Oparil S, Ouyang P, Pinn VW, Sherif K, Smith SC, Jr, Sopko G, Chandra-Strobos N, Urbina EM, Vaccarino V, Wenger NK. Effectiveness-based guidelines for the prevention of cardiovascular disease in women–2011 update: a guideline from the American Heart Association. J Am Coll Cardiol. 2011;57:1404–1423. doi: 10.1016/j.jacc.2011.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


