Abstract
We evaluated the prevalence and correlates of intimate partner violence in the past year by a regular male partner in HIV-positive female sex workers in Mombasa, Kenya. This cross-sectional study included HIV-positive women ≥ 18 years old who reported engagement in transactional sex at the time of enrolment in the parent cohort. We asked 13 questions adapted from the World Health Organization survey on violence against women about physical, sexual, or emotional violence in the past year by the current or most recent emotional partner (index partner). We used standardised instruments to assess socio-demographic and behavioural characteristics as possible correlates of intimate partner violence. Associations between intimate partner violence and these correlates were evaluated using univariate and multivariate logistic regression. Overall, 286/357 women (80.4%) had an index partner, and 52/357 (14.6%, 95% confidence interval 10.9%–18.2%) reported intimate partner violence by that partner in the past year. In multivariate analysis, women with severe alcohol problems (adjusted odds ratio 4.39, 1.16–16.61) and those experiencing controlling behaviours by the index partner (adjusted odds ratio 4.98, 2.31–10.74) were significantly more likely to report recent intimate partner violence. Recent intimate partner violence was common in HIV-positive female sex workers. Interventions targeting risk factors for intimate partner violence, including alcohol problems and partner controlling behaviours, could help to reduce recurrent violence and negative health outcomes in this key population.
Keywords: Intimate partner violence, HIV-positive women, transactional sex, Africa
Introduction
An estimated one in three women report ever experiencing intimate partner violence (IPV).1,2 There are several negative outcomes associated with experiencing IPV, including depression,3 unwanted pregnancy,4 sexually transmitted infections (STIs), including HIV5,6 and suicide.7 In Africa, IPV in women is common.2,5,8 According to the 2008/9 Kenya Demographic and Health Survey, 48% of ever married women reported lifetime IPV, and 41% reported IPV in the past year.9 Previous studies of correlates of IPV in African women have found that inequitable gender norms,10,11 alcohol use by either partner,12 women having multiple sex partners,13 prior abuse as a child or adult,10 lower education12 and HIV-positive status14 are associated with greater frequency of IPV.15 There may be unique correlates of IPV in HIV-positive women, including HIV status disclosure and initiation of HIV care.16–18
An estimated 1–4% of all women in Africa are female sex workers (FSWs), a particularly stigmatised population that experiences high rates of violence.19,20 This population has an estimated 14-fold higher likelihood of HIV-infection compared to women not engaged in sex work.21 Quantitative and qualitative studies reveal that most FSWs maintain intimate partners (i.e. boyfriends or husbands), for emotional and financial support.16,22,23 FSWs may also experience a high frequency of IPV, which may affect their overall health and ongoing risk of unintended pregnancy and HIV transmission.16,22,24 One cohort study of HIV-negative FSWs in Kenya reported that 55.0% of women had experienced any physical or sexual violence by an ‘emotional’ partner in the past year.24 Limitations to the existing literature in African FSWs include a focus on violence by clients and police rather than IPV, lack of standard definitions of IPV in this population and lack of studies on the correlates of IPV in HIV-positive FSWs.23,25 Improved understanding of the prevalence and correlates of IPV in HIV-positive FSWs using standardised tools will help to identify potentially modifiable intervention targets to help reduce IPV, and potentially strengthen more comprehensive HIV care for this key population.26 To address these knowledge gaps, we conducted a cross-sectional study to evaluate the prevalence and correlates of IPV in the past year among HIV-positive FSWs in Mombasa, Kenya.
Methods
This study was a cross-sectional analysis of enrolment data from women participating in a cohort study on the relationship between reproductive lifecourse events and HIV treatment and prevention-related outcomes at our HIV/STI research clinic. Most women were already participating in a long-term open cohort on risk factors for HIV acquisition and transmission (parent cohort). Eligible women were laboratory-confirmed HIV-positive, age 18 or older, and reported exchanging sex for cash or in-kind payment at the time of enrolment in the parent cohort. Women completed a standardised face-to-face interview in their preferred language (Kiswahili or English) with a trained Kenyan study nurse to collect socio-demographic, health, and behavioural data. All interviews were conducted in a private room. A study clinician conducted a physical examination including a speculum-assisted pelvic examination for collection of genital swabs for laboratory testing. Participants received free outpatient care at our research clinic, including comprehensive risk reduction counselling, antiretroviral therapy (ART) according to Kenyan National Guidelines and STI treatment. Study staff received additional training on conducting research on violence against women (VAW), emphasising objective and non-judgmental interviewing techniques. Women who reported experiencing violence were offered counselling on site or referral. This study was approved by the ethics committees of Kenyatta National Hospital and the University of Washington. All participants provided written informed consent.
Measures
The main outcome, ‘any IPV’ in the last year, was defined as responding yes to at least 1 of 13 questions about acts of IPV in the past 12 months committed by an emotional partner. Questions were adapted from the WHO survey on VAW (WHO VAW), which has high internal consistency in different settings.27 These questions were pilot tested in our target population to ensure understanding prior to initiating the study. All women were asked whether they had a regular emotional partner, defined as a boyfriend or husband, who they did not consider to be a client or a casual partner. If they did not have an emotional partner at the time of the interview, they were asked about their most recent emotional partner. That man was identified as the ‘index partner’. Only participants who had an index partner were asked the IPV questions. When responding to the IPV questions, women were asked to think about behaviours by that index partner. If a participant reported any lifetime IPV by that index partner, she was then asked whether that act occurred in the past 12 months. There were six questions on physical violence (slapped, pushed, hit, kicked, choked, or threatened with a weapon); four on emotional violence (insulted, belittled, intimidated, threatened to hurt someone you care about) and three on sexual violence (forced sex, coerced sex or degrading sexual behaviour). We measured how closely related these 13 items were in our sample using Cronbach’s alpha. Internal consistency was high (α = 0.88). Women who reported no index partner were classified as having no IPV.
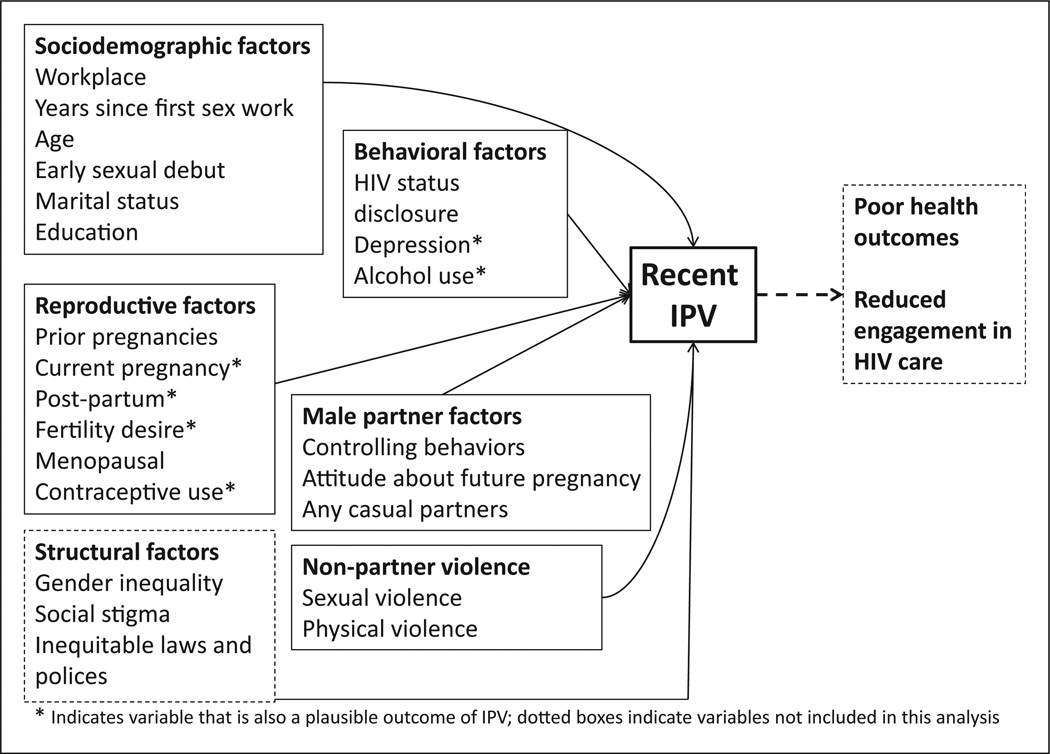
Socio-demographic, behavioural and clinical characteristics were evaluated as correlates of IPV in the past 12 months, based on a literature review and our conceptual model (Figure 1). Socio-demographic characteristics included age (continuous); marital status (ever married); years since first sex work (<5, 5–9, ≥10); early sexual debut (first sex ≤ 15 years); education level (<8 years versus 8 or more); and workplace (bar, nightclub, home/other). Reproductive characteristics included pregnancy history; fertility desire; use of modern contraceptive methods (none/condoms only, oral or injectable hormonal contraceptives, intrauterine device, tubal ligation, or hysterectomy); laboratory-confirmed pregnancy; post-partum status (within nine months of last delivery); and menopausal status.28 Women were asked about their index partner’s reaction to a possible pregnancy (excited, neutral, upset). They were also asked whether they had a casual partner in the last three months. The number of sexual partners in the past week (any, including the index partner) was dichotomised at the median (≥2 vs.<2) because the distribution of these data was highly skewed.
Figure 1.
Conceptual model of individual- and relationship-level correlates of intimate partner violence in the past year in HIV-positive female sex workers.
We evaluated depressive symptoms, alcohol use, HIV disclosure and male controlling behaviours with tools used previously in similar populations in Africa.29–31 Recent depressive symptoms were assessed with the Patient Health Questionnaire-9 (PHQ-9).30 Scores were categorised as 0–4 (minimal), 5–9 (mild), 10 or higher (consistent with a major depressive disorder).32 Alcohol use in the past year was evaluated with the alcohol use disorders identification test (AUDIT).33 Scores were categorised as non-drinkers (zero), minimal (1–6), moderate (7–15) and severe problem or possible alcohol use disorder (AUD) (≥16).34 Disclosure of HIV status was assessed by asking whether women had ever shared their results with someone.35 Exposure to controlling behaviours was defined as responding yes to at least one of seven statements about behaviours ever committed by her index partner (e.g. requires permission to get health care). In addition, all women were asked about history of sexual or physical violence, since age 15, by someone besides an emotional partner (i.e. not the index partner, former boyfriend, or former husband). Sexual violence was assessed by asking whether women had been forced to have sex or perform a sexual act. Physical violence was assessed by asking women whether they had been beaten or physically mistreated.31 Prevalent STIs (Neisseria gonorrhoeae, Chlamydia trachomatis, or Trichomonas vaginalis) was assessed by nucleic acid amplification testing (APTIMA;Hologic/Gen Probe, San Diego, CA). Baseline CD4 count was dichotomised as ≤350 versus >350 cells/µl. Current antiretroviral (ART) use was measured by self-report. For women receiving ART through our research clinic, we confirmed that they were taking ART with our pharmacy records.
Statistical analysis
We estimated the prevalence of IPV in the past year (recent IPV) and conducted an exploratory analysis of the correlates of IPV that included all women in the sample with complete data. We evaluated variables that were plausible correlates of recent IPV. These variables included socio-demographic characteristics,13 early age of first sex,36 reproductive characteristics (pregnancy, post-partum, menopausal, fertility desire, non-condom contraceptive use),8,37 disclosure of HIV status,38 controlling behaviours,39 alcohol use23 and depression.40 Univariate logistic regression was used to estimate the association between each correlate and recent IPV. Variables associated with any recent IPV in univariate analysis (p < 0.10) were included simultaneously in the multivariate model. We decided a priori to evaluate variables that could be both correlates and outcomes of IPV (depressive symptoms, alcohol use, and reproductive characteristics), as illustrated in the conceptual model (Figure 1).3,8,41–43 Sexual behaviours and STIs were considered primarily outcomes of IPV and were not included in the correlates analysis.44 We conducted a sensitivity analyses restricted to women who reported an index partner. Because this analysis was exploratory, we did not adjust α = 0.05 level for multiple comparisons. With a sample of 360 women, we estimated that we would have at least 80% power to detect an Odds Ratio (OR) ≥ 1.7 for common correlates (>30%) and an OR ≥ 2.0 for less frequent correlates (10–30%), assuming 20% prevalence of IPV in unexposed women. All associations were reported as ORs with 95% confidence intervals (CI). Models used robust standard errors. Analyses were conducted in STATA 13.0 (StataCorp, College Station, TX).
Results
Sample characteristics
Overall, 359 women enrolled between October 2012 and December 2013, of whom, 357 had complete data on the IPV questions. Baseline characteristics are shown in Table 1. The median age was 39 years (interquartile range [IQR] 33, 44; range 20–61). Many reported first engaging in transactional sex at least 10 years earlier (173/355, 48.5%), and more than half reported engagement in sex work in the last year (193, 54.3%). Only 24 (8%) women reported being currently married. The majority of women (286, 80.1%) reported having an index partner. About one-fifth of women (73, 20.5%) reported ever experiencing physical abuse since age 15 by someone other than an emotional partner. A lower proportion of women (36/355, 10.1%) reported experiencing any sexual abuse since age 15 by someone other than an emotional partner. Nearly half of the women reported any alcohol use in the past year (174, 48.7%). Among women who were alcohol users, 103/174 (59.1%) reported drinking behaviour consistent with minimal alcohol use problems, 57/174 (32.8%) with moderate problems and 14/174 (8.0%) with severe alcohol problems or possible AUD. The prevalence of symptoms consistent with mild (scores 5–9; 66, 18.5%) and moderate (scores ≥ 10; 23/357, 6.4%) depression by PHQ-9 in the past two weeks was relatively low. Nearly half of the women experienced at least one controlling behaviour by the index partner 167 (46.8%). Less than one-third reported more than one sexual partner in the past week (98/356, 27.5%). Of 228 women who reported taking ART, 116 (50.8%) were receiving ART from our research clinic, while others received medications elsewhere.
Table 1.
Enrollment characteristics of 357 HIV-positive women who reported current or past engagement in transactional sex.
| Characteristic | Median (IQR) or n(%) |
|---|---|
| Age | 39 (33,44) |
| Highest education level ≥ 8 years Workplace |
144 (40.3) |
| Bar/restaurant | 210 (58.8) |
| Nightclub | 83 (23.3) |
| Home/other | 64 (17.9) |
| Early sexual debut (age 15 or younger) | 101 (28.9) |
| Years since first sex work (n = 355) | |
| Less than 5 | 72 (20.2) |
| 5–9 | 110 (30.8) |
| 10 or more | 173 (48.5) |
| Ever married | 276 (77.3) |
| Had only a casual partner in the past 3 months |
27 (7.6) |
| Has an index partner | 286 (80.1) |
| Index partner in the past 3 months | 160 (44.9) |
| Index partner in the past 3 months, no casual partner |
99 (27.7) |
| Has both an index and casual partner in the past 3 months |
132 (37.0) |
|
Reproductive health characteristics |
|
| Number of previous pregnancies (n = 356) |
3 (2,4) |
| Pregnant by urine hCG test (n = 356) | 3 (0.8) |
| Fertility desire (n = 355) | 87 (24.3) |
| Post-partum (n=350) | 6 (1.7) |
| Post-menopausal (n=354)a | 57 (16.0) |
| Contraceptive use category (n = 355) | |
| None or condoms only | 249 (69.8) |
| DMPA or OCP (short/medium acting hormonal methods) |
72 (20.2) |
| IUD, TL, Norplant, hysterectomy (long acting methods) |
34 (9.5) |
|
Partner attitude about pregnancy (n=286)b |
|
| Excited | 165 (58.3) |
| Neutral | 71 (24.9) |
| Upset | 47 (16.8) |
| Depressive symptoms by PHQ-9 | |
| Minimal (0–4) | 268 (75.1) |
| Mild (5–9) | 66 (18.5) |
| Mod/severe (10 or higher) | 23 (6.4) |
| Alcohol use problems by AUDIT | |
| Non drinkers | 183 (51.0) |
| Minimal (1–6) | 103 (28.9) |
| Moderate (7–15) | 57 (15.9) |
| Severe (16 or higher) | 14 (3.9) |
| Disclosed HIV status to anyone in the Past (n=356) |
228 (68.9) |
|
History of violence and controlling behaviours |
|
| History of sexual abuse since age 15 (n=355)c |
36 (10.1) |
| Any sexual abuse in the past 12 months (n=352)c |
18 (5.1) |
| History of physical abuse since age 15c | 73 (20.5) |
| Any physical abuse in the past 12 months (n = 355)c |
23 (6.5) |
| Ever had controlling behaviours by the index partner |
167 (46.8) |
| HIV-related clinical variables | |
| CD4 lymphocyte count ≤ 350 cells/ µl (n = 355) |
93 (26.1) |
| On ART by self-report (n = 356)d | 228 (64.0) |
| Any GC, CT, or TV by APTIMA (n=348) |
38 (10.9) |
ART: anti-retroviral therapy; AUDIT: alcohol use disorders identification test; CT: Chlamydia tracomatis; DMPA: depot medroxyprogesterone acetate; GC: Neisseria gonorrhoeae; IPV: intimate partner violence; hCG: human chorionic gonadotropin; OCP: oral contraceptive pills; PHQ-9: Patient health questionnaire 9; TV: Trichomonas vaginalis.
Post-menopausal status based on clinical algorithm was defined as >40 years old, reported ≥ 12 months of amenorrhea from the time of their last menstrual period, and not taking unopposed progesterone contraception such as depot medroxyprogesterone acetate or progesterone only oral contraceptive pills.
Among women who had an index partner.
Refers to anyone besides the index partner, former boyfriend, or former husband.
Of 228 women who reported taking ART at enrollment, 116 (50.9%) were receiving this medication at our clinic and 107 (46.9%) reported getting ART at another clinic (five missing responses).
Prevalence of IPV in the past year and ever by the index partner
Fifty-two women (14.6%, 95% CI 10.9%–18.2%) reported IPV in the past year. The prevalence of IPV in the past year restricted to women who reported an index partner was 52/286 (18.2%, 13.7%–22.7%).
The most common type of recent IPV was physical violence (38, 10.6%), followed by emotional violence (36, 10.1%) and sexual violence (13, 3.6%). Nearly 40% of women reported ever experiencing IPV by an index partner (137/357, 38.2%, 33.2%–43.3%).
In univariate analysis, reporting alcohol problems (minimal OR 2.06, 0.99–4.29; moderate OR 3.08, 1.38–6.90; severe OR 7.83, 2.41–25.42), and controlling behaviours by the index partner (OR 6.05, 2.92–12.51) were associated with a significantly greater likelihood of IPV in the past year (Table 2). Compared to women who reported first engaging in sex work less than five years ago, those who reported first engaging in sex work 10 or more years earlier had a lower likelihood of recent IPV (OR 0.51, 0.24–1.09).
Table 2.
Correlates of any IPV in the past 12 months by the index partner.
| Variable | IPV (n = 52) |
No IPV (n = 305) |
OR (95% CI) |
p-value | AOR (95% CI)* |
p-value |
|---|---|---|---|---|---|---|
| Age | 37 (32, 44) | 40 (33, 44) | 0.98 (0.94–1.00) | 0.16 | -- | |
| Early sexual debut (≤ 15 years) |
18 (34.6) | 83 (27.2) | 1.42 (0.76–2.64) | 0.28 | -- | |
| Years since first sex work | ||||||
| <5 (ref) | 14 (26.9) | 58 (19.1) | 1.0 | 1.0 | ||
| 5–9 | 19 (36.5) | 91 (30.0) | 0.86 (0.40–1.86) | 0.71 | 1.11 (0.48, 2.58) | 0.80 |
| 10 or more | 19 (36.5) | 154 (50.8) | 0.51 (0.24–1.09) | 0.08 | 0.87 (0.37, 2.05) | 0.75 |
| Number of pregnancies (n=356) |
3 (2, 4) | 2 (2, 4) | 1.08 (0.93–1.23) | 0.36 | -- | |
| Number of births (n=355) | 3 (1, 4) | 2 (1, 3) | 1.07 (0.90–1.27) | 0.43 | -- | |
| Work place | ||||||
| Bar (ref) | 33 (63.5) | 177 (58.0) | 1.0 | -- | ||
| Nightclub | 11 (21.2) | 72 (23.6) | 0.82 (0.39–1.71) | 0.60 | ||
| Home, Other | 8 (15.4) | 56 (18.4) | 0.73 (0.33–1.76) | 0.53 | ||
| Ever married | 44 (84.6) | 232 (76.1) | 1.73 (0.78–3.84) | 0.18 | -- | |
| 8 or more years education | 25 (48.1) | 119 (39.0) | 1.45 (0.80–2.61) | 0.22 | -- | |
| Fertility desire (n = 355) | 13 (25.5) | 74 (24.3) | 1.06 (0.54–2.11) | 0.86 | -- | |
| Contraception (n = 355)a | ||||||
| None/condoms (ref) | 35 (67.3) | 214 (70.6) | 1.0 | |||
| OCP or DMPA | 11 (21.2) | 61 (20.1) | 1.10 (0.53–2.30) | 0.80 | -- | |
| Long-acting methods | 6 (11.5) | 28 (9.2) | 1.31 (0.51–3.40) | 0.58 | -- | |
| Pregnant (urine hCG) | 2 (3.9) | 1 (0.3) | 1.68 (0.48–5.90) | 0.42 | -- | |
| Post-partum (n = 350) | 1 (1.9) | 5 (1.7) | 1.15 (0.13–10.10) | 0.90 | -- | |
| Post-menopausal (n = 354) | 7 (13.7) | 50 (16.5) | 0.81 (0.34–1.89) | 0.62 | -- | |
| How would your partner feel if you became pregnant? b |
||||||
| Excited (ref) | 33 (66.0) | 132 (56.7) | 1.0 | |||
| Neutral | 12 (24.0) | 59 (25.3) | 0.81 (0.39–1.69) | 0.58 | -- | |
| Upset | 5 (10.0) | 42 (17.8) | 0.48 (0.17–1.30) | 0.15 | -- | |
| Controlling behaviours by index partner |
42 (80.8) | 125 (41.0) | 6.05 (2.92–12.51) | <0.001 | 4.98 (2.31–10.74) | <0.001 |
| Physical abuse since age 15c | 15 (28.9) | 58 (19.0) | 1.73 (0.89–3.35) | 0.11 | -- | |
| Physical abuse, past yearc (n = 355) |
4 (7.7) | 19 (6.3) | 1.25 (0.41–3.83) | 0.70 | -- | |
| Sexual abuse since age 15c (n = 355) |
5 (9.6) | 31 (10.2) | 0.93 (0.34–2.53) | 0.89 | -- | |
| Sexual abuse, past yearc (n = 352) |
3 (5.8) | 15 (5.0) | 1.17 (0.33, 4.20) | 0.81 | -- | |
| Ever disclosed HIV status | 33 (63.5) | 195 (64.1) | 0.97 (0.53–1.79) | 0.93 | -- | |
| Depressive symptoms by PHQ-9 categories |
||||||
| Min 0–4 (ref) | 35 (67.3) | 233 (76.4) | 1.0 | |||
| Mild 5–9 | 12 (23.1) | 54 (17.7) | 1.48 (0.72–3.04) | 0.29 | -- | |
| Mod/Sev (10 or higher) | 5 (9.6) | 18 (5.9) | 1.85 (0.64–3.51) | 0.25 | ||
| Alcohol problems by AUDIT | ||||||
| Non-drinkers (ref) | 16 (30.8) | 167 (54.8) | 1.0 | 1.0 | ||
| Min 1–6 | 17 (32.7) | 86 (28.2) | 2.06 (0.99–4.29) | 0.05 | 1.95 (0.89–4.27) | 0.09 |
| Mod 7–15 | 13 (25.0) | 44 (14.4) | 3.08 (1.38–6.90) | 0.006 | 2.09 (0.87–5.00) | 0.10 |
| Sev 16+ | 6 (11.5) | 8 (2.6) | 7.83 (2.41–25.42) | 0.001 | 4.39 (1.16–16.63) | 0.03 |
| CD4 count <350 cells/µl (n = 355) |
12 (23.5) | 81 (26.6) | 0.85 (0.42–1.70) | 0.61 | -- | |
| On ART (n=356) | 32 (61.5) | 196 (64.2) | 0.86 (0.58–1.53) | 0.61 | -- |
ART: anti-retroviral therapy; AUDIT: alcohol use disorders identification test; DMPA: depot medroxyprogesterone acetate; hCG: human chorionic gonadotropin; IPV: intimate partner violence; OCP: oral contraceptive pills; OR: Odds Ratio; AOR: adjusted Odds Ratio; PHQ-9, patient health questionnaire 9.
Multivariate analysis sample was 355.
Long-term methods include Norplant, IUD, tubal ligation, hysterectomy.
Among 286 women with an index partner.
Violence by any person besides the index partner, former boyfriend, or former husband.
In multivariate analysis, compared to women who did not drink, women with higher alcohol use scores had a greater likelihood of IPV in the past year, although only the severe alcohol use category remained statistically significant (≥16 aOR 4.39, 1.16–16.61). The partner’s controlling behaviours also remained significantly associated with a greater likelihood of IPV in the past year (aOR 4.98, 2.31–10.74). Results from the sensitivity analyses restricted to women who reported an index partner were similar to the results in the primary analysis (data not shown).
Discussion
IPV in the past year was common in this sample of HIV-positive FSWs in Kenya. Male controlling behaviours and women having more severe alcohol use problems were significantly associated with experiencing recent IPV.
The 15% prevalence of IPV in the past year by the index partner fell within the range of previous studies among African women,15,31,45–47 including those at-risk for HIV acquisition and transmission.48,49 We found a lower prevalence of recent IPV compared to prior studies of Kenyan sex workers.23,42 Differences in the reported prevalence of IPV are partly due to differences in study instruments, violence definitions and prevalence of risk factors for violence across samples.31,50 In addition, other studies in FSWs have included both regular sex partners and clients in the definition of ‘intimate partner,’ which likely explains the higher prevalence of reported IPV. Both earlier studies included higher proportions of women with alcohol use problems, and one study was conducted with women receiving an alcohol use intervention.20,51 As a result, those women may have been at higher risk of violence generally. In our sample, most women were taking ART and had been counselled that alcohol use can impair adherence, which can decrease medication effectiveness. Our study adds to the limited literature in HIV-positive FSWs. Specifically, this research highlights the important role of intimate partners as perpetrators of violence in HIV-positive women with past or present involvement in transactional sex.
Our finding that alcohol use problems were associated with a greater likelihood of IPV also parallels results from previous studies in Africa.42 The relationship between alcohol use and IPV is complex and likely bidirectional.41 Women who consume higher quantities of alcohol may be more likely to get into conflict that culminates in IPV, and have intimate partners who commit IPV while intoxicated.52 Alternatively, women may drink to cope with IPV or other life stress. Longitudinal studies are needed to determine how each of these pathways may contribute to the observed association between IPV and alcohol use, and to inform future interventions to address high-risk alcohol use and IPV.42,51
The association between male partner controlling behaviours and experiencing IPV is consistent with results from other samples of African women.12,39,53 Surveys conducted among men have found that controlling behaviours are associated with a greater likelihood of male perpetration of IPV.54 Controlling behaviours like suspiciousness or requiring permission to get health care indicate unequal power dynamics in a relationship.10,55,56 A woman’s failure to act within in a designated role may trigger IPV because her partner feels that his power is threatened.56,57 In-depth interviews of pregnant women, men, and health care providers in Western Kenya found that one of the triggers of IPV was a woman’s failure to consult her husband before getting HIV testing.58 Related themes emerged in a qualitative study of South African men.56 In that study, improved communication with a partner and a reduced sense of sexual entitlement were identified as ways to help men to resolve relationship conflict without resorting to IPV. These findings provide support for interventions that target relationship factors to improve power balance and communication skills, to reduce IPV.20
The strengths of this study include using a standardised instrument to measure IPV. The WHO VAW survey has been used successfully in studies in other populations of women in Africa.5,8 Using this tool will enable us to interpret and compare findings across studies. Similarly, we measured potential correlates of IPV, including alcohol use and depressive symptoms, with tools that have been validated in similar populations.24,30 We also considered directionality of associations, and aimed only to test variables as correlates of IPV that were plausible risk factors.
This study also had limitations. First, the cross-sectional design limited inferences about temporal sequence or causality. Second, this analysis was exploratory and should be replicated in other samples. We would have had lower power to detect associations between infrequent correlates and IPV. Future studies should also evaluate HIV disclosure to an emotional partner, the partner’s alcohol use, and community-level factors including inequitable gender norms.54,59 Third, IPV was measured by self-report and is subject to underreporting due to recall bias and sensitivity of the topic.31 We tried to minimise underreporting of IPV by asking behaviourally specific questions, which have been shown to facilitate disclosure.31 Fourth, we did not conduct a partner-level analysis to evaluate the frequency of IPV with different partners, including more than one index partner.16,23 Asking about IPV committed by the current or most recent emotional partner is consistent with use of the WHO VAW tool, but could underestimate the true prevalence of IPV in the past year if women have more than one emotional partner. While our results may not be generalisable to all other populations, our findings are likely applicable to other women engaged in transactional sex.44,60,61 Studies from diverse settings and risk groups are important for providing a more comprehensive understanding of IPV among HIV-positive women.
Conclusion
VAW with past or current involvement in sex work is a key health and human rights problem. There are several important health outcomes at stake, including the risk of depression, unintended pregnancy, STI and HIV transmission. Our study extends knowledge about this key population by highlighting the problem of IPV and providing evidence for potentially modifiable intervention targets.62 A brief empowerment-based behavioural intervention has been shown to be efficacious at reducing IPV, substance use and unprotected sex in randomised trials in HIV-positive and HIV-negative women in South Africa.20 Similar interventions should be evaluated in FSWs in other African settings to help reduce IPV and improve women’s quality of life.
Acknowledgments
We are grateful to the study participants and our research, clinical, laboratory, outreach, and administrative staff for making this study possible.
Funding
This study was funded by a grant from the National Institutes of Health (R01HD072617). KSW was supported by the University of Washington Center for STD and AIDS (grant T32 AI07140). Infrastructure and logistics support for the Mombasa research site was provided by the University of Washington’s Center for AIDS Research (CFAR), an NIH funded programme (P30 AI027757) which is supported by the following centres: NIAID, NCI, NIMH, NIDA, NICHD, NHLBI, NCCAM. No abstracts were published.
Footnotes
Authors’ contributions
KSW and RSM designed the study. KSW analysed the data and drafted the manuscript. RSM, LM, RD, JMS, JPH, JS, WJ and AV reviewed drafts of the manuscript. RD, LM, and JS provided oversight of study procedures and data collection at our research clinic. Access to research materials for this study is available by request.
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Data were presented previously at the Annual Meeting of the University of Nairobi Collaborative Centre for Research and Training in HIV/AIDS/STIs on 28 January 2014.
References
- 1.UNAIDS. Getting to zero: 2011–2015 strategy joint united nations programme on HIV/AIDS (UNAIDS) Geneva: UNAIDS Publication; 2010. [Google Scholar]
- 2.Devries KM, Mak JY, Garcia-Moreno C, et al. Global health. The global prevalence of intimate partner violence against women. Science. 2013;340:1527–1528. doi: 10.1126/science.1240937. [DOI] [PubMed] [Google Scholar]
- 3.Ellsberg M, Jansen HAFM, Heise L, et al. Intimate partner violence and women’s physical and mental health in the WHO multi-country study on women’s health and domestic violence: an observational study. Lancet. 2008;371:1165–1172. doi: 10.1016/S0140-6736(08)60522-X. [DOI] [PubMed] [Google Scholar]
- 4.Pallitto CC, Garcia-Moreno C, Jansen HA, et al. Intimate partner violence, abortion, and unintended pregnancy: results from the WHO multi-country study on women’s health and domestic violence. Int J Gynaecol Obstet. 2013;120:3–9. doi: 10.1016/j.ijgo.2012.07.003. [DOI] [PubMed] [Google Scholar]
- 5.Jewkes RK, Dunkle K, Nduna M, et al. Intimate partner violence, relationship power inequity, and incidence of HIV infection in young women in South Africa: a cohort study. Lancet. 2010;376:41–48. doi: 10.1016/S0140-6736(10)60548-X. [DOI] [PubMed] [Google Scholar]
- 6.Kouyoumdjian FG, Calzavara LM, Bondy SJ, et al. Intimate partner violence is associated with incident HIV infection in women in Uganda. AIDS. 2013;27:1331–1318. doi: 10.1097/QAD.0b013e32835fd851. [DOI] [PubMed] [Google Scholar]
- 7.Devries K, Watts C, Yoshihama M, et al. Violence against women is strongly associated with suicide attempts: evidence from the WHO multi-country study on women’s health and domestic violence against women. Soc Sci Med. 2011;73:79–86. doi: 10.1016/j.socscimed.2011.05.006. [DOI] [PubMed] [Google Scholar]
- 8.Shamu S, Abrahams N, Zarowsky C, et al. Intimate partner violence during pregnancy in Zimbabwe: a cross-sectional study of prevalence, predictors and associations with HIV. Trop Med Int Health. 2013;18:696–711. doi: 10.1111/tmi.12078. [DOI] [PubMed] [Google Scholar]
- 9.Kenya National Bureau of Statistics (KNBS) and ICF Macro. Kenya Demographic and Health Survey 2008–09. Calverton, Maryland: KNBS and ICF Macro; 2010. [Google Scholar]
- 10.Gass JD, Stein DJ, Williams DR, et al. Gender differences in risk for intimate partner violence among South African adults. J Interpers Violence. 2011;26:2764–2789. doi: 10.1177/0886260510390960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shannon K, Leiter K, Phaladze N, et al. Gender inequity norms are associated with increased male-perpetrated rape and sexual risks for HIV infection in Botswana and Swaziland. PLoS One. 2012;7:e28739. doi: 10.1371/journal.pone.0028739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mandal M, Hindin MJ. Men’s controlling behaviors and women’s experiences of physical violence in Malawi. Matern Child Health J. 2013;17:1332–1338. doi: 10.1007/s10995-012-1137-1. [DOI] [PubMed] [Google Scholar]
- 13.Dunkle KL, Jewkes RK, Brown HC, et al. Prevalence and patterns of gender-based violence and revictimization among women attending antenatal clinics in Soweto, South Africa. Am J Epidemiol. 2004;160:230–239. doi: 10.1093/aje/kwh194. [DOI] [PubMed] [Google Scholar]
- 14.Were E, Curran K, Delany-Moretlwe S, et al. A prospective study of frequency and correlates of intimate partner violence among African heterosexual HIV serodiscordant couples. AIDS. 2011;25:2009–2018. doi: 10.1097/QAD.0b013e32834b005d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chersich MF, Luchters SM, Malonza IM, et al. Heavy episodic drinking among Kenyan female sex workers is associated with unsafe sex, sexual violence and sexually transmitted infections. Int J STD AIDS. 2007;18:764–769. doi: 10.1258/095646207782212342. [DOI] [PubMed] [Google Scholar]
- 16.Benoit C, Roth E, Hallgrimsdottir H, et al. Benefits and constraints of intimate partnerships for HIV positive sex workers in Kibera, Kenya. Int J Equity Health. 2013;12:76. doi: 10.1186/1475-9276-12-76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Skovdal M, Campbell C, Nyamukapa C, et al. When masculinity interferes with women’s treatment of HIV infection: a qualitative study about adherence to antiretroviral therapy in Zimbabwe. J Int AIDS Soc. 2011;14:29. doi: 10.1186/1758-2652-14-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cowan FM, Mtetwa S, Davey C, et al. Engagement with HIV prevention treatment and care among female sex workers in Zimbabwe: a respondent driven sampling survey. PLoS One. 2013;8:e77080. doi: 10.1371/journal.pone.0077080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Vandepitte J, Lyerla R, Dallabetta G, et al. Estimates of the number of female sex workers in different regions of the world. Sex Transm Infect. 2006;82(Suppl 3):ii18–ii25. doi: 10.1136/sti.2006.020081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wechsberg WM, Luseno WK, Lam WK, et al. Substance use, sexual risk, and violence: HIV prevention intervention with sex workers in Pretoria. AIDS Behav. 2006;10:131–137. doi: 10.1007/s10461-005-9036-8. [DOI] [PubMed] [Google Scholar]
- 21.Baral S, Beyrer C, Muessig K, et al. Burden of HIV among female sex workers in low-income and middle-income countries: a systematic review and meta-analysis. Lancet Infect Dis. 2012;12:538–549. doi: 10.1016/S1473-3099(12)70066-X. [DOI] [PubMed] [Google Scholar]
- 22.Voeten HA, Egesah OB, Varkevisser CM, et al. Female sex workers and unsafe sex in urban and rural Nyanza, Kenya: regular partners may contribute more to HIV transmission than clients. Trop Med Int Health. 2007;12:174–182. doi: 10.1111/j.1365-3156.2006.01776.x. [DOI] [PubMed] [Google Scholar]
- 23.Pack AP, L’Engle K, Mwarogo P, et al. Intimate partner violence against female sex workers in Mombasa, Kenya. Cult Health Sex. 2014;16:217–230. doi: 10.1080/13691058.2013.857046. [DOI] [PubMed] [Google Scholar]
- 24.Luchters S, Richter ML, Bosire W, et al. The contribution of emotional partners to sexual risk taking and violence among female sex workers in Mombasa, Kenya: a cohort study. PLoS One. 2013;8:e68855. doi: 10.1371/journal.pone.0068855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Decker MR, Wirtz AL, Pretorius C, et al. Estimating the impact of reducing violence against female sex workers on HIV epidemics in Kenya and Ukraine: a policy modeling exercise. Am J Reprod Immunol. 2013;69(Suppl 1):122–132. doi: 10.1111/aji.12063. [DOI] [PubMed] [Google Scholar]
- 26.Wechsberg WM, Jewkes R, Novak SP, et al. A brief intervention for drug use, sexual risk behaviours and violence prevention with vulnerable women in South Africa: a randomised trial of the women’s health CoOp. BMJ Open. 2013;3:e002622. doi: 10.1136/bmjopen-2013-002622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Schraiber LB, Latorre Mdo R, Franca I, Jr, et al. Validity of the WHO VAW study instrument for estimating gender-based violence against women. Rev Saude Publica. 2010;44:658–666. doi: 10.1590/s0034-89102010000400009. [DOI] [PubMed] [Google Scholar]
- 28.Casper RF. [accessed 19 August 2015];Clinical manifestations and diagnosis of menopause. Available at: http://www.uptodate.com/contents/clinical-manifestations-and-diagnosis-of-menopause?source=see_link.
- 29.Luchters S, Geibel S, Syengo M, et al. Use of AUDIT, and measures of drinking frequency and patterns to detect associations between alcohol and sexual behaviour in male sex workers in Kenya. BMC Public Health. 2011;11:384. doi: 10.1186/1471-2458-11-384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Monahan PO, Shacham E, Reece M, et al. Validity/reliability of PHQ-9 and PHQ-2 depression scales among adults living with HIV/AIDS in western Kenya. J Gen Intern Med. 2009;24:189–197. doi: 10.1007/s11606-008-0846-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Garcia-Moreno C, Jansen HA, Ellsberg M, et al. Prevalence of intimate partner violence: findings from the WHO multi-country study on women’s health and domestic violence. Lancet. 2006;368:1260–1269. doi: 10.1016/S0140-6736(06)69523-8. [DOI] [PubMed] [Google Scholar]
- 32.Gelaye B, Williams MA, Lemma S, et al. Validity of the Patient Health Questionnaire-9 for depression screening and diagnosis in East Africa. Psychiatry Res. 2013;210:653–661. doi: 10.1016/j.psychres.2013.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Saunders JB, Aasland OG, Babor TF, et al. Development of the alcohol use disorders identification test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption-II. Addiction. 1993;88:791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- 34.Babor TFH-BJ, Saunders J, Monteiro M. The alcohol use disorders identification test: guidelines for use in primary care. 2nd. Geneva, Switzerland: World Health Organization; 2001. pp. 1–39. [Google Scholar]
- 35.Peltzer K, Chao LW, Dana P. Family planning among HIV positive and negative prevention of mother to child transmission (PMTCT) clients in a resource poor setting in South Africa. AIDS Behav. 2009;13:973–979. doi: 10.1007/s10461-008-9365-5. [DOI] [PubMed] [Google Scholar]
- 36.Shuaib FM, Ehiri JE, Jolly P, et al. Sexual violence and associated factors among women in HIV discordant and concordant relationships in Uganda. Int J Adolesce Med Health. 2012;24:125–133. doi: 10.1515/ijamh.2012.019. [DOI] [PubMed] [Google Scholar]
- 37.Duff P, Lee ML, Hillier SL, et al. Amoxicillin treatment of bacterial vaginosis during pregnancy. Obstet Gynecol. 1991;77:431–435. [PubMed] [Google Scholar]
- 38.Tabana H, Doherty T, Rubenson B, et al. ‘Testing Together Challenges the Relationship’: consequences of HIV testing as a couple in a High HIV prevalence setting in rural South Africa. PLoS One. 2013;8:e66390. doi: 10.1371/journal.pone.0066390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zacarias AE, Macassa G, Svanstrom L, et al. Intimate partner violence against women in Maputo city, Mozambique. BMC Int Health Hum Rights. 2012;12:35. doi: 10.1186/1472-698X-12-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Nduna M, Jewkes RK, Dunkle KL, et al. Associations between depressive symptoms, sexual behaviour and relationship characteristics: a prospective cohort study of young women and men in the Eastern Cape, South Africa. J Int AIDS Soc. 2010;13:44. doi: 10.1186/1758-2652-13-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Devries KM, Child JC, Bacchus LJ, et al. Intimate partner violence victimization and alcohol consumption in women: a systematic review and meta-analysis. Addiction. 2014;109:379–391. doi: 10.1111/add.12393. [DOI] [PubMed] [Google Scholar]
- 42.Chersich MF, Bosire W, King’ola N, et al. Effects of hazardous and harmful alcohol use on HIV incidence and sexual behaviour: a cohort study of Kenyan female sex workers. Global Health. 2014;10:22. doi: 10.1186/1744-8603-10-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Duff P, Shoveller J, Feng C, et al. Pregnancy intentions among female sex workers: recognising their rights and wants as mothers. J Fam Plann Reprod Health Care. 2015;41:102–108. doi: 10.1136/jfprhc-2012-100532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kacanek D, Bostrom A, Montgomery ET, et al. Intimate partner violence and condom and diaphragm nonadherence among women in an HIV prevention trial in southern Africa. J Acquir Immune Defic Syndr. 2013;64:400–408. doi: 10.1097/QAI.0b013e3182a6b0be. [DOI] [PubMed] [Google Scholar]
- 45.Dude AM. Spousal intimate partner violence is associated with HIV and Other STIs among married Rwandan women. AIDS Behav. 2011;15:142–152. doi: 10.1007/s10461-009-9526-1. [DOI] [PubMed] [Google Scholar]
- 46.Tegang SP, Abdallah S, Emukule G, et al. Concurrent sexual and substance-use risk behaviours among female sex workers in Kenya’s Coast Province: findings from a behavioural monitoring survey. SAHARA J. 2010;7:10–16. doi: 10.1080/17290376.2010.9724972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Adudans MK, Montandon M, Kwena Z, et al. Prevalence of forced sex and associated factors among women and men in Kisumu, Kenya. Afr J Reprod Health. 2011;15:87–97. [PubMed] [Google Scholar]
- 48.Fonck K, Leye E, Kidula N, et al. Increased risk of HIV in women experiencing physical partner violence in Nairobi, Kenya. AIDS Behav. 2005;9:335–339. doi: 10.1007/s10461-005-9007-0. [DOI] [PubMed] [Google Scholar]
- 49.Peltzer K, Jones D, Weiss SM, et al. Sexual risk, serostatus and intimate partner violence among couples during pregnancy in rural South Africa. AIDS Behav. 2013;17:508–516. doi: 10.1007/s10461-012-0185-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Groves AK, Moodley D, McNaughton-Reyes L, et al. Prevalence, rates and correlates of intimate partner violence among south african women during pregnancy and the postpartum period. Matern Child Health J. 2014;19:487–495. doi: 10.1007/s10995-014-1528-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Watt MH, Sikkema KJ, Abler L, et al. Experiences of forced sex among female patrons of alcohol-serving venues in a South African township. J Interpers Violence. 2015;30:1533–1552. doi: 10.1177/0886260514540807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Gonzalez JM, Connell NM, Businelle MS, et al. Characteristics of adults involved in alcohol-related intimate partner violence: results from a nationally representative sample. BMC Public Health. 2014;14:466. doi: 10.1186/1471-2458-14-466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Dunkle KL, Jewkes RK, Brown HC, et al. Gender-based violence, relationship power, and risk of HIV infection in women attending antenatal clinics in South Africa. Lancet. 2004;363:1415–1421. doi: 10.1016/S0140-6736(04)16098-4. [DOI] [PubMed] [Google Scholar]
- 54.Fulu E, Jewkes R, Roselli T, et al. Prevalence of and factors associated with male perpetration of intimate partner violence: findings from the UN multi-country cross-sectional study on men and violence in Asia and the Pacific. The Lancet Global health. 2013;1:e187–e207. doi: 10.1016/S2214-109X(13)70074-3. [DOI] [PubMed] [Google Scholar]
- 55.Jewkes R, Sikweyiya Y, Morrell R, et al. Gender inequitable masculinity and sexual entitlement in rape perpetration South Africa: findings of a cross-sectional study. PloS One. 2011;6:e29590. doi: 10.1371/journal.pone.0029590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Hatcher AM, Colvin CJ, Ndlovu N, et al. Intimate partner violence among rural South African men: alcohol use, sexual decision-making, and partner communication. Cult Health Sex. 2014;16:1–17. doi: 10.1080/13691058.2014.924558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Jewkes R, Morrell R. Gender and sexuality: emerging perspectives from the heterosexual epidemic in South Africa and implications for HIV risk and prevention. J Int AIDS Soc. 2010;13:6. doi: 10.1186/1758-2652-13-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Hatcher AM, Romito P, Odero M, et al. Social context and drivers of intimate partner violence in rural Kenya: implications for the health of pregnant women. Cult Health Sex. 2013;15:404–419. doi: 10.1080/13691058.2012.760205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Shai NJ, Jewkes R, Nduna M, et al. Masculinities and condom use patterns among young rural South Africa men: a cross-sectional baseline survey. BMC Public Health. 2012;12:462. doi: 10.1186/1471-2458-12-462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.El-Bassel N, Gilbert L, Wu E, et al. HIV and intimate partner violence among methadone-maintained women in New York City. Soc Sci Med. 2005;61:171–183. doi: 10.1016/j.socscimed.2004.11.035. [DOI] [PubMed] [Google Scholar]
- 61.Pitpitan EV, Kalichman SC, Eaton LA, et al. Gender-based violence, alcohol use, and sexual risk among female patrons of drinking venues in Cape Town, South Africa. J Behav Med. 2013;36:295–304. doi: 10.1007/s10865-012-9423-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Bekker LG, Johnson L, Cowan F, et al. Combination HIV prevention for female sex workers: what is the evidence? Lancet. 2015;385:72–87. doi: 10.1016/S0140-6736(14)60974-0. [DOI] [PMC free article] [PubMed] [Google Scholar]