Abstract
Previous study findings of psychotherapy’s effect on suicide prevention have been inconsistent. The present study reports the results of secondary analyses of outcome data from a short-term depression treatment on reducing death/suicidal ideation among 158 low-income homebound adults aged 50+. The treatment, in-person or telehealth problem-solving therapy (PST), compared to telephone support call, has been found effective in reducing depressive symptoms and disability among participants. Compared to support call participants, tele-PST participants, but not in-person PST participants, exhibited lower ideation ratings across the follow-up period. Effect sizes at 36 weeks were 0.31 for tele-PST and 0.17 for in-person PST. Hopelessness mediated the effect of tele-PST but not in-person PST; however, in-person PST also alleviated hopelessness, which led to lower ideation. Clinical implications of the findings are discussed.
Keywords: Homebound older adults, tele-delivered problem-solving therapy, hopelessness
Death by suicide among late middle-aged and older adults is a significant public health problem. In 2010, suicide was the fourth and eighth leading cause of death in the 45–54 and 55–64 age groups, respectively, and the 65+ age group who made up 13% of the U.S. population accounted for 16% of all suicides (National Center for Health Statistics, 2014). Individual-level risk factors are poor predictors of who will die by suicide, but depression severity and diagnosis of major depressive disorder (MDD), hopelessness, poor physical and functional health, pain, and lack of social support/social isolation have been identified as significant correlates of death or suicidal ideation among older adults (Conwell, Van Orden, & Caine, 2011; Cukrowicz, Jahn, Graham, Poindexter, & Williams, 2013; De Leo, Draper, Snowdon, & Kõlves, 2013; Kim, Bogner, Brown, & Gallo, 2006; Rowe, Conwell, Schulberg, & Bruce, 2006; Sachs-Ericsson et al., 2014).
Some previous studies found that pharmacotherapy and/or psychotherapy for depression reduced suicidal ideation among high-risk older adults (Lapierre et al., 2011). An evaluation of short-term (12-week) effectiveness of pharmacotherapy, with or without interpersonal psychotherapy, for MDD found that suicidal ideation rapidly resolved in all treated patients, although the time to resolution was longer in the high-risk group (those with a recent suicide attempt or current suicidal ideation) than in the moderate (those with recurrent thoughts of death) or low-risk groups (those with no suicidal ideation/thoughts of death or who reported questioning whether life is empty or not worth living) (Szanto, Mulsant, Houck, Dew, & Reynolds, 2003). The Improving Mood-Promoting Access to Collaborative Treatment (IMPACT; Unützer et al., 2002, 2006) for depression in primary care settings also found that tailored collaborative care and personalized treatment for older patients significantly reduced both depressive symptoms and suicidal ideation among the intervention group compared to the usual care group throughout the 24-month follow-up period.
The effect of depression treatment on suicidal ideation was less clear in other studies. The PROSPECT study that provided depression care manager interventions for older primary care patients found that after 24 months, reduction in suicidal ideation among the intervention group members with MDD was 2.1 times greater than that of the usual care group, but the difference was not statistically significant (Alexopoulos et al., 2009). No benefits were detected among those with minor depression. A systematic review and meta-analysis also concluded that psychotherapy of depression may have small positive effect on adult suicidal ideation and cannot be considered to be a sufficient treatment for suicidal ideation, although the effects on hopelessness were probably higher (Cuijpers, de Beurs, van Spijker, Berking, Andersson, & Kerkhof, 2013). Hopelessness has been identified as a stronger indicator of suicide risk than depression and a central mediating factor between depression and suicidal intent and behavior (Abramson et al., 2000; Beck, 1986; Beck, Brown, Berchick, Stewart, & Steer, 1990; Beck, Brown, & Steer, 1989; Kovacs, Beck, & Weissman, 1975; Weishaar & Beck, 1992). More research is needed to examine the effect of psychotherapy on alleviating hopelessness and suicidal ideation among depressed older adults.
Due to their disability and social isolation, homebound older adults are at especially higher risk for depression and death/suicidal ideation than their mobile age peers. An earlier study of homecare older patients found that 13.5% had MDD, a majority of whom suffered from late-onset depression (Bruce et al., 2002). Other studies of homecare patients or home-delivered meal recipients found that 9–12% had clinically significant depressive symptoms (Ell, Unützer, Aranda, Sanchez, & Lee, 2005; Sirey et al., 2008). The point-in-time rates of death/suicidal ideation among these older adults were 12–13%, with as many as 1.1% in one study reporting current active suicidal ideation (thoughts about harming oneself, suicidal ideation with poor impulse control, or a suicide plan) (Raue, Meyers, Rowe, Heo, & Bruce, 2007; Rowe, Bruce, & Conwell, 2006; Sirey et al., 2008). A study of older adults who received care management services from aging-service network agencies also found that 14% endorsed current death or suicidal ideation (O’Riley, Van Orden, He, Richardson, Podgorski, & Conwell, 2014). Little research has been done, however, on the effectiveness of psychotherapy on reducing death/suicidal ideation and hopelessness among depressed, homebound older adults.
Previous research emphasized the critical role of inability to identify problems and corresponding solutions and resultant feelings of being overwhelmed and hopeless in suicidal ideation and behavior (Neuringer, 1974; Rudd, Rajab, & Dahm, 1994). While suicidal behavior has been attributed to an individual’s desire to escape from an “insolvable” problem and hopelessness (Beck, 1986), those with problem-solving skills enabling them to generate productive alternatives would be less likely to feel hopeless (Ruud et al., 1994). Problem-solving therapy (PST), an evidence-based, short-term depression treatment, posits that people with deficits in problem-solving skills become vulnerable to depression and teaches problem-solving coping skills (Cuijipers, Karyotaki, Pot, Park, & Reynolds, 2014; D’Zurilla & Nezu, 2007; Nezu, Nezu, & D’Zurilla, 2012). PST’s orientation that problems are solvable and its focus on systematic problem-solving skills training have been effective in treating depression in all age groups (Nezu, Nezu, & D’Zurilla, 2012). Because depression, hopelessness, and suicidal ideation are interrelated, PST has potential to concomitantly reduce hopelessness and suicidal ideation along with depression. A study of middle-aged breast cancer patients with MDD found that PST reduced suicidal ideation and increased hopefulness (Hopko et al., 2013). However, no previous PST outcome trials with depressed older adults systematically examined its effect on their hopelessness and death/suicidal ideation.
We recently completed a randomized controlled trial of in-person and telehealth problem-solving therapy (PST), compared to telephone support (support call), for depressed, low-income homebound older adults. The trial found that both PST modalities were more effective than support calls in reducing depressive symptoms at both 12 and 24 weeks, but only telehealth PST (tele-PST) was more effective than support call at 36 weeks (Choi, Marti, Bruce, Hegel, Wilson, & Kunik, 2014). In this paper, we report the results of secondary analyses of the PST outcome data focusing on (1) PST’s potential effects on death/suicidal ideation during the 36-week follow-up period, and (2) mediating role of hopelessness. We hypothesized that (1) both in-person PST and tele-PST, compared to support call, would reduce death/suicidal ideation; and (2) the PST’s effect on death/suicidal ideation will be mediated by hopelessness. Examination of hopelessness is likely to lend a greater insight into the mechanism of PST that may alleviate death/suicidal ideation among low-income, homebound older adults. This study contributes to building knowledge base on PST’s effect on death/suicidal ideation and hopelessness among low-income homebound older adults who had been underexposed in previous depression and suicide research.
METHODS
Data Source and Sample
Participants were 158 English-speaking, non-Hispanic White, Black, or Hispanic homebound adults aged 50+ with moderately severe-to-severe depressive symptoms (a score of 15+ on the 24-item Hamilton Rating Scale for Depression [HAMD]; Depression Rating Scale Standardization Team, 2003). Case managers of a large home-delivered meal (HDM) program and four other aging-service agencies in Central Texas referred potential participants (those with scores≥10 on the PHQ-9 [Kroenke & Spitzer, 2002] or those who showed symptoms of depression when a lack of privacy prevented administration of the PHQ-9). In-person screening at individuals’ homes excluded those with HAMD<15, possible dementia (assessed with the Mini-Cog [Borson, Scanlan, Brush, Vitaliano, & Dokmak, 2000]), bipolar disorder and other mental illness, and active alcohol/other substance abuse. Active suicidal ideation was also a criterion for study exclusion to allow immediate comprehensive evaluation and preventive intervention, but none of the referred individuals had active suicidal ideation at the time of screening. Those taking antidepressant medication for more than 8 weeks but having HAMD≥15 were included. Those who passed the screening proceeded to a comprehensive assessment that included the DSM-IV-TR depression module. Although 164 of the 238 persons referred by their case managers during the 30-month recruitment period met the inclusion criteria and provided baseline data, six declined further participation. Thus, 158 were randomly assigned (based on HAMD score, the primary outcome) to the study’s three arms using simple random assignment (63 to in-person PST, 56 to tele-PST, and 39 to support calls) and enrolled in the study. Of the enrollees, 139 (54 in-person PST, 49 tele-PST, and 36 support calls) completed all six intervention sessions and provided 12-week follow-up data; 125 (52 in-person PST, 41 tele-PST, and 32 support call) provided 24-week follow-up data; and 116 (45 in-person PST, 40 tele-PST, and 31 support calls) provided 36-week follow-up data. Attrition was due mostly to hospitalization, nursing home placement, and death; however, the baseline demographic and clinical characteristics of the nonparticipants (n=6) and dropouts did not significantly differ from those of the participants who completed all assessments. The primary author’s institutional review board approved the study protocol.
Intervention
Two master’s-level therapists delivered both modalities of PST and two master’s-level research associates who did not receive PST training made the support calls, while receiving ongoing clinical supervision. In-person PST participants received all six face-to-face PST sessions at their residence. The tele-PST participants received in-person PST for the first session at their residence, at the end of which the therapist provided each of them a locked down laptop computer that allowed Skype video calls only from the therapist and demonstrated its use. The laptops were removed following five tele-sessions. In each PST session that lasted 60 minutes, the therapist and participant used a worksheet to progress through the seven steps of PST-Primary Care (Hegel & Areán, 2002), focusing on participants’ appraisal of specific problems, identification of the best possible solutions, and the practical implementation of those solutions. PST sessions also included behavioral activation to help participants schedule and engage in pleasant daily events to address anhedonia and psychomotor retardation. The support calls, each lasting up to 30 minutes, were intended to provide unspecified support and empathy and to monitor participants’ depressive symptoms to ensure their safety.
Measures
Depressive symptoms
The 24-item HAMD consists of the GRID-HAMD-21 structured interview guide augmented with three additional items assessing feelings of hopelessness, helplessness, and worthlessness (Depression Rating Scale Standardization Team, 2003; Moberg et al., 2001). Scoring of the majority of HAMD items, including the suicide and hopelessness items, are based on the four levels of symptom frequency and the five levels of symptom intensity grids. Four frequency levels are: absent/not occurring or clinically insignificant; occasional/infrequent (less than 3 days; up to 30% of the week); much of the time/often (3–5 days; 31%–75% of the week); almost all the time/persistent (6–7 days; more than 75% of the week). Five levels of intensity are absent, mild, moderate, severe, and very severe, with qualifying descriptions for each symptom item. Assessors trained and supervised by a PhD-level geropsychologist administered the HAMD to measure each participant’s depressive symptoms “during the past week.”
Death/suicidal ideation rating
(0–4; ideation rating hereafter) was determined from the “suicide” item in the GRID-HAMD. Frequency levels are as described above. Intensity levels are: absent; mild (feels life is not worth living, but expresses no wish to die); moderate (wishes to be dead; thoughts of dying, but no specific plan or intent); severe (clear suicidal plan or intent; suicidal gesture); and very severe (attempts at suicide). The 0–4 ideation ratings represent gradations of severity: 0 (absent) when both frequency and intensity were absent or when intensity was mild at clinically insignificant frequency; 1 (mild-occasional, mild-much of the time, or moderate-occasional); 2 (mild-persistent or moderate-much of the time); 3 (moderate-persistent, severe-occasional, or severe-much of the time); and 4 (very severe at any frequency).
Hopelessness (0–4)
The 0–4 hopelessness ratings also represent the severity gradation, with 0 representing the lowest level (absence) of frequency and intensity. Intensity levels were: absent; mild/trivial (doubts that “things will improve,” but can be reassured.); moderate (feels “hopeless” but accepts reassurance); severe (expresses feelings of discouragement, despair, pessimism about future, which cannot be dispelled); and very severe (spontaneously and inappropriately perseverates, “I’ll never get well,” or its equivalent).
Potential covariates
These included demographics (age, gender, race/ethnicity, living arrangement, and family income), health status (numbers of diagnosed chronic illnesses and instrumental/activities of daily living [IADL/ADL] impairments), and antidepressant medication intake.
Analysis
Descriptive analysis of participants’ baseline characteristics (one-way ANOVA, with Bonferroni-corrected post-hoc tests, χ2 tests, and t tests) were performed with SPSS v.21 (IBM Corp., Armonk, NY). Treatment effects on ideation ratings, as a continuous dependent variable, were tested from an intent-to-treat approach using mixed models with random intercepts (Raudenbush & Bryk, 2001) with the R lmer function in the lme4 package (Bates, Maechler, & Bolker, 2014). Treatment group was coded using two dummy variables for tele-PST and in-person PST. Mixed models were constructed following Singer and Willett’s (2003) recommendations to first fit unconditional means, linear, and nonlinear growth models to determine the best model prior to adding independent variables. We tested whether time in weeks was better represented as no-change, linear, or quadratic trajectory. Based on Akaike Information Criterion (AIC) values (Burnham & Anderson, 2002), we determined that an unconditional means (i.e., an intercept-only model in which ideation ratings remained stable throughout the three follow-up assessment points) was the best growth model. Thus, main effects in the growth models represent the effect of a putative variable throughout the entire follow-up period. Two growth models, with the 12-, 24- and 36-week ideation ratings as the outcomes, were fit; one with baseline HAMD scores (minus the suicide item) as a covariate, and the other with baseline hopelessness and time-varying hopelessness (i.e., at 12, 24, and 36 weeks) as covariates. Because there were baseline differences in ideation ratings by treatment group (reported in the Results section), baseline ideation ratings, along with gender, was also included as a covariate in both growth models. Following recommendations from Feingold (2009), effect sizes at 36 weeks were estimated by dividing the difference between the estimated means of treatment groups by the baseline standard deviation. The formula generates an effect size (dGMA-raw) in a growth model context that is equivalent to traditional effect sizes (e.g., Cohen’s d).
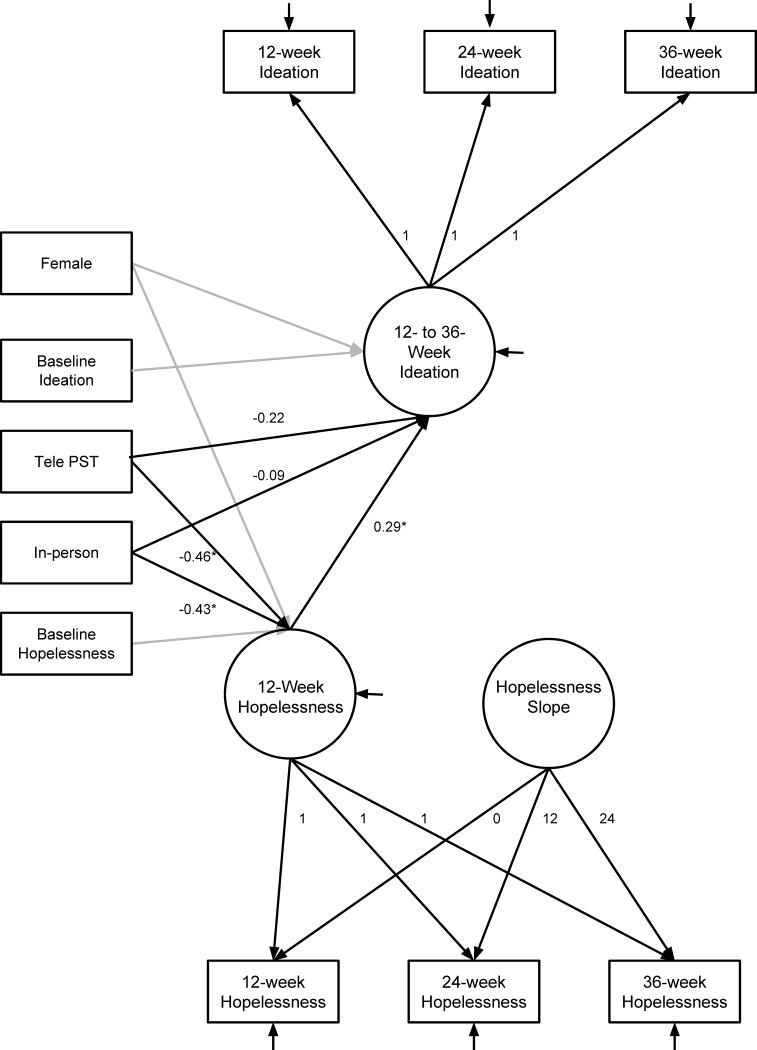
Mediation effect of hopelessness was assessed in a latent growth curve (LGC) model framework implemented using Mplus (Muthén & Muthén, 1998–2012) and with the following steps from MacKinnon (2008): (1) treatment predicts change in the outcome (i.e., ideation ratings), (2) treatment predicts change in the mediator (i.e., hopelessness), and (3) the change in the mediator predicts the change in the outcome. The mediation model was constructed by first individually fitting LGC models for ideation ratings and hopelessness. The LGC model for ideation ratings was fit as described above (i.e., unconditional means). The hopelessness LGC was fit as a linear change model in which hopelessness decreased across time (z=−2.29, p=.022) and was thus fit with an intercept (i.e., 12-week follow-up estimate adjusted for treatment conditions) and a slope (i.e., change across the follow-up period). The hopelessness intercept was treated as the mediator as it represents a single point in time and thus largely precedes the ideation intercept, which represents the entire follow-up period. Significance of the indirect effect (i.e., mediation) was assessed using bias-corrected bootstrapped confidence intervals (Preacher & Hays, 2008) with 10,000 bootstrap draws in a parallel growth curve model that included the hopelessness and ideation growth curves as well as the treatment effects. Gender was included as a covariate for both the ideation growth models and the LGCs; baseline ideation rating was included as a covariate for the ideation LGC; and baseline hopelessness was included as a covariate for the hopelessness LGC. Model fit was assessed using the two-index presentation strategy (Hu & Bentler, 1999) in which the maximum standardized root mean squared residual (SRMR) is supplemented with an additional fit index, for which we selected root mean squared error of approximation (RMSEA). The following cutoff values were used: a SRMR value less than .08 and RMSEA values of .01, .05, and .08 respectively indicate excellent, good, and mediocre fit (Hu & Bentler, 1999; MacCallum, Browne, & Sugawara, 1996).
RESULTS
Participant Baseline Characteristics
Of the participants, 79% were female; 58% were Black or Hispanic; 84% had income at or below $25,000; 64% lived alone; 65% had MDD; and 47% were taking antidepressant medications. They had, on average, three chronic medical conditions and four IADL/ADL impairments (Table 1). The three treatment groups did not differ in any of these characteristics. The mean HAMD score and the mean hopelessness score were 23.89±6.52 and 1.53±1.49, respectively, without any significant difference by treatment group (Table 2). With respect to ideation ratings, 50% (n=79) had 0; 24% (n=38) had 1; 12% (n=19) had 2; 14% (n=22) had 3; and none had 4. All 22 participants with a rating of 3 had death/passive suicidal ideation, i.e., they were at moderate risk without a clear suicidal plan or intent. Most study participants stated that despite their wishes to be dead, they would not attempt suicide because such an act would be against their religious faith and cause their families’ suffering. The distribution of ratings, when treated as a categorical variable, did not significantly differ by treatment group (χ2=9.78, p=.134); however, significant group difference was found in mean ratings (F[2, 155]=4.82, p=.009). In-person-PST group had significantly lower ratings than support call group (0.62± 0.91 vs. 1.28±1.17; t=−3.21, df=100, p=.002), while tele-PST group did not differ from support call group (0.95±1.14 vs. 1.28±1.17; t=−1.40, df=93, p=.165). Ideation ratings were also significantly associated with HAMD (minus the suicide item) (r=.22, p=.005) and hopelessness (r=.34, p<.001) and marginally significantly associated with gender (1.18±1.29 for men vs. 0.82±1.01 for women; t=1.70, df=156, p=.092); 26.5% of men versus 10.5% of women had a rating of 3. Ideation ratings were not significantly associated with the other demographic and health variables, antidepressant intake, and depression diagnosis.
TABLE 1.
Study Participants’ Baseline Demographic and Health Characteristics (n=158)
| Age (M±SD) | 64.80±9.18 |
| Age group (n, %) | |
| 50–59 | 44 (27.8) |
| 60–69 | 71 (44.9) |
| 70–79 | 29 (18.4) |
| 80+ | 14 (8.9) |
| Gender (n, %) | |
| Female | 124 (78.5) |
| Male | 34 (21.5) |
| Race/ethnicity (n, %) | |
| Non-Hispanic White | 67 (42.4) |
| African American/Black | 52 (32.9) |
| Hispanic | 39 (24.7) |
| Family income (n, %) | |
| Up to $25,000 | 133 (84.2) |
| $25,001–$35,000 | 11 (7.0) |
| $35,001 + | 7 (4.4) |
| Refused | 7 (4.4) |
| Living arrangement (n, %) | |
| Living alone | 101 (64.3) |
| Living with spouse and/or other | 57 (35.7) |
| No. of diagnosed chronic illness1 (M±SD) | 3.06±1.54 |
| No. of IADL/ADL impairment2 (M±SD) | 4.12±2.37 |
| Antidepressant medication intake (n, %) | 74 (46.8) |
| DSM-IV-TR diagnosis of depression (n, %) | |
| Major depressive disorder | 103 (65.2) |
| Depressive disorder, NOS | 47 (29.7) |
| Dysthymia | 8 (5.1) |
Arthritis/rheumatism; hypertension; diabetes; heart disease; stroke; emphysema/chronic bronchitis/other lung problems; cancer/malignant tumor; kidney disease; and liver disease were included if they were still problems at time of the interview.
IADLs: Preparing and cooking meals; using the telephone; grocery shopping; doing housework or handyman work; taking medications; and managing money; and ADLs: Bathing or taking a shower; toileting; getting dressed or putting on outdoor clothing by oneself; combing or brushing hair; getting into and out of bed; and feeding oneself.
TABLE 2.
Baseline Depressive Symptom, Suicidal Ideation and Hopelessness by Treatment Group (n=158)
| All | In-person PST | Tele-PST | Support call | p | |
|---|---|---|---|---|---|
| HAMD1 score (M±SD) | 23.89±6.52 | 23.75±6.58 | 23.54±6.43 | 24.64±6.67 | .703 |
| HAMD1 score w/o suicide item (M±SD) | 22.98±6.22 | 23.13±6.47 | 22.55±5.98 | 23.36±6.26 | .803 |
| Death/suicidal ideation rating2,3 (M±SD) | 0.90±1.08 | 0.62±0.91a | 0.95±1.14b | 1.20±1.17c | .009 |
| Death/suicidal ideation rating2 (%) | .134 | ||||
| 0 | 50.0 | 60.3 | 50.0 | 33.3 | |
| 1 | 24.1 | 23.8 | 21.4 | 28.2 | |
| 2 | 12.0 | 9.5 | 12.5 | 15.4 | |
| 3 | 13.9 | 6.3 | 16.1 | 23.1 | |
| Hopelessness (M±SD) | 1.53±1.49 | 1.43±1.39 | 1.66±1.62 | 1.51±1.49 | .698 |
Hamilton rating Scale for depression
0=Absent; 1=Mild frequent or moderate infrequent; 2=Mild persistent or moderate frequent; and 3=Moderate persistent or severe frequent
Bonferronni-corrected ANOVA: a<c; a=b; b=c
Effects of PST on Death/Suicidal Ideation
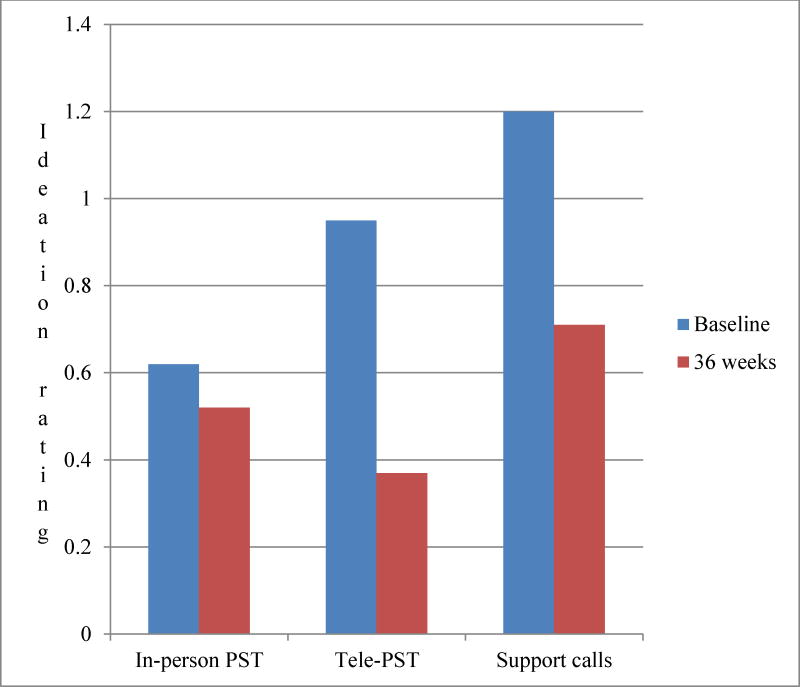
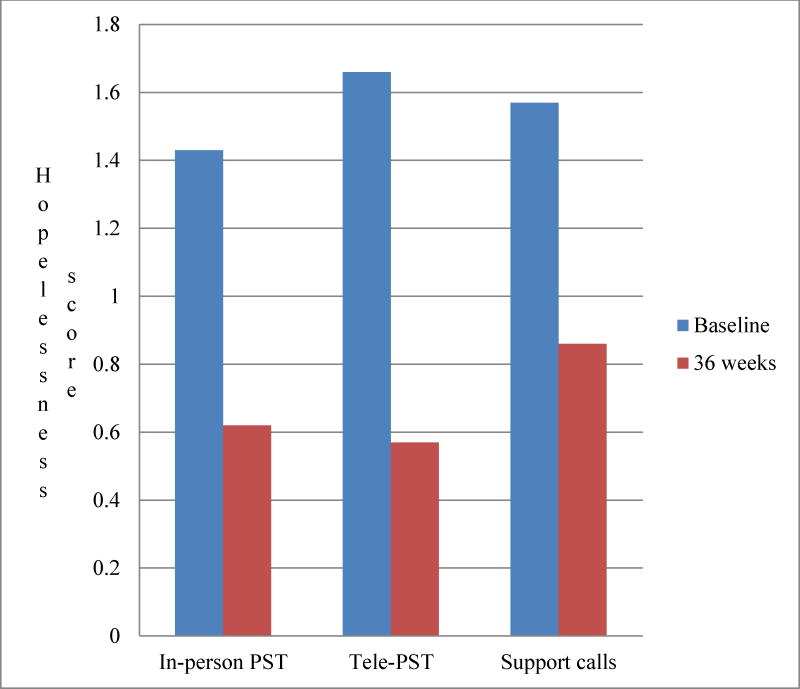
Table 3 shows that in both growth models, compared to support call participants, tele-PST participants, but not in-person PST participants, exhibited significantly lower ideation ratings across the follow-up period, indicating that tele-PST was more effective than in-person PST in reducing them over time. Baseline ideation rating and hopelessness scores since baseline (i.e., at 12, 24, and 36 weeks) were significantly positively associated with ideation ratings, while gender and baseline HAMD (minus suicide item) and hopelessness scores were not significant factors. Figure 1 shows changes in ideation ratings among treatment groups between baseline (raw means as shown in Table 2) and 36 weeks (predicted means: 0.52±0.09 for in-person PST; 0.37±0.09 for tele-PST; and 0.71±0.11 for support call). Effect sizes (compared to support call) at 36 weeks were 0.17 for in-person PST and 0.31 for tele-PST. Figure 2 shows changes in hopelessness scores among treatment groups: from 1.43±1.39 at baseline to 0.62±0.18 at 36 weeks for in-person PST; from 1.66±1.62 to 0.57±0.20 for tele-PST; and from 1.51±1.49 to 0.86±0.22 for support calls.
TABLE 3.
Effect of Intervention and Time on Death/Suicidal Ideation Ratings (N= 158)
| Model 1 | Model 2 | |||||||
|---|---|---|---|---|---|---|---|---|
| B (SE) | df | t | p | B (SE) | df | t | p | |
| Intercept | .53 (.24) | 133 | 2.07 | .029 | .45 (.15) | 138 | 2.92 | .004 |
| In-person PST | −.19 (.13) | 137 | −1.46 | .148 | −.16 (.13) | 137 | −1.24 | .216 |
| Tele-PST (Support call) |
−.33 (.13) | 139 | −2.57 | .011 | −.29 (.13) | 140 | −2.34 | .021 |
| Female (Male) |
−.21 (.12) | 137 | −1.70 | .092 | −.19 (.12) | 136 | −1.65 | .101 |
| Baseline ideation ratings | .25 (.05) | 138 | 5.18 | <.001 | .22 (.05) | 136 | 4.41 | <.001 |
| Baseline HAMD scores (minus suicide item) | .003 (.01) | 135 | 0.31 | .761 | ||||
| Baseline hopelessness score | .03 (.04) | 144 | 0.81 | .418 | ||||
| Hopelessness since baseline | .12 (.03) | 375 | 3.85 | <.001 | ||||
Note: Reference categories are denoted in parentheses.
FIGURE 1.
Ideation Ratings by Treatment Group
FIGURE 2.
Hopelessness Scores by Treatment Group
Mediation Effect of Hopelessness
The results show that the first mediation criterion, treatment predicts change in the outcome, was met for tele-PST (z=−2.573, p=.010), but not in-person PST (z=−31.446, p=.148). The second mediation criterion, treatment predicts change in the mediator, was met for both in-person PST (z=−2.308, p=.021) and tele-PST (z=−2.378, p=.017). The third mediation criterion, mediator change predicts change in the outcome, was met (z=3.276, p=.001). The indirect effect was significant for both in-person PST (95% CI=−0.306, −0.017) and tele PST (95% CI=−0.369, −0.012). All three mediation requirements were met for tele-PST. On the other hand, because the direct effect of in-person PST on ideation ratings was not significant, significant indirect effect for this group alone was not sufficient to establish the mediation effect. The mediation model exhibited good fit as assessed by SRMR (0.070) and adequate fit as assessed by the RMSEA (.077). Figure 3 presents the LGC model with meditation paths and coefficients.
FIGURE 3.
Mediation Effect of Hopelessness: Latent Growth Curve Model
DISCUSSION
Depression and wishes to die among older adults are important steps on the path to suicide (Conwell et al., 2011). This study was a follow-up of our original study that examined effectiveness of short-term tele- and in-person PST for depression as the direct/primary target in 158 low-income, depressed homebound individuals aged 50+ years. The depression outcomes showed longer-term effectiveness of tele-PST compared to in-person PST (Choi et al., 2014). Our secondary analyses of the PST’s outcome data with respect to death/suicidal ideation and hopelessness found the following: (1) 12% of the participants had mild-persistent or moderate-frequent death ideation and 14% had moderate-persistent death ideation/passive suicidal ideation at baseline; (2) short-term tele-PST, but not in-person PST, was more effective than telephone support calls in reducing death/suicidal ideation throughout the follow-up period; (3) hopelessness was a significant mediator of tele-PST’s effect on reduced ideation ratings; (5) in-person PST was still effective in alleviating hopelessness; and (5) hopelessness was significantly associated with ideation ratings throughout the follow-up period. The nonsignificant reduction in in-person PST participants’ ideation ratings may have been attributable to their lower baseline ratings than those of support call participants to begin with (a likely result of randomization based on depressive symptoms, not suicidal ideation specifically). However, almost 60% reduction in tele-PST participants’ ideation ratings between baseline and 36 weeks is notable. Although the study participants who were randomized to tele-PST expressed their preference for in-person sessions, almost all of them embraced tele-sessions once they began participating and had more positive treatment evaluation ratings than in-person PST participants (Choi et al., 2014). These higher levels of satisfaction and sense of self-efficacy related to technology use (first time for many participants) may have contributed to better depression, hopelessness, and ideation outcomes.
The key findings of the study are the confirmation of the significant association between hopelessness and ideation and the support for PST, either tele-delivered or in-person, as an effective approach to alleviating hopelessness (along with depression) in these vulnerable older adults with multiple medical conditions and other life stressors. PST’s training in positive, goal-oriented problem-solving skills is likely a contributor to increasing hopefulness and fostering a sense of self-efficacy, which further provides positive reinforcement. Through these mechanisms, hopelessness, death/suicidal ideations, as well as depressive symptoms, may have been attenuated.
Although it was less effective than tele-PST, support calls nevertheless also appear to have helped reduce participants’ ideation ratings. Previous studies suggested that telephone counseling outreach programs providing emergency/crisis support, regular check-ins, and information and referral services may reduce depressive symptoms and/or prevent suicide as well (Lapierre et al., 2011). Interactions with a caller are likely to increase a sense of social connectedness, which protects against suicide (Centers for Disease Control and Prevention, 2008; Lapierre et al., 2011; Szanto et al., 2013).
The study had a few limitations. First, death/suicidal ideation and hopelessness were not PST’s primary targets in the original trial. Thus, death/suicidal ideation and hopelessness were measured with a single HAMD item for each. Although some previous studies (Hopko et al., 2013; Nelson, Delucci, & Schneider, 2007) used the same measure, future research calls for more comprehensive measures. Future research should also examine PST’s effect on suicidal ideation as a primary target. Second, the sample size, especially the number of men, was small. Future research with more men is needed. Third, because active suicidal ideation, cognitive impairment, and substance use were study-exclusion criteria, the findings likely underestimate actual death/suicidal ideation among these vulnerable older adults, and PST’s effect on hopelessness and active suicidal ideation among these high-risk groups was not examined. One study of older adults who received outpatient depression treatment found that hopelessness remained significantly higher in the suicide attempter group than among ideators or nonsuicidal patients (Szanto, Reynolds, Conwell, Begley, & Houck, 1998). Further research is needed to examine PST’s effect on hopelessness among higher risk group, including suicide attempters. Fourth, compared to 60-minute PST sessions, each telephone support call lasted up to 30 minutes. Although treatment was neither intended nor provided during support calls, 60 minutes, rather than 30 minutes of interaction may have increased support calls’ effectiveness.
Despite these limitations, this study has the following practice implications: (1) Given the effectiveness of tele-sessions and increasing Internet use among older adults, tele-delivery of psychotherapy and suicide-prevention interventions for homebound older adults should be more widely implemented because they can increase access and reduce delivery (transportation) costs. (2) Tele-PST or other psychotherapy that includes systematic, creative, and realistic problem-solving approaches specifically targeting hopelessness may be promising as both therapeutic interventions for and prevention of suicidal ideation in vulnerable older adults. (3) Further research is called for to test the effectiveness of telephone support calls as a suicide prevention strategy for depressed, low-income homebound older adults. Since low-income homebound older adults have limited access to professional mental health services, training aging-service providers to identify at-risk clients, increase their social connectedness via telephone, and provide ongoing monitoring may be a feasible and sustainable approach.
Acknowledgments
The study was supported by grants from the National Institute of Mental Health and St. David’s Foundation to the first author and the Centers for Disease Control and Prevention to the third author.
Funding Sources: National Institute of Mental Health (R34 MH083872), Centers for Disease Control and Prevention (U01 CE001942), and St. David’s Foundation
Footnotes
Conflicts of interest
None declared.
Contributor Information
C. Nathan Marti, Email: nate78701@gmail.com.
Yeates Conwell, Email: Yeates_Conwell@URMC.Rochester.edu.
References
- Abramson LY, Alloy LB, Hogan ME, Whitehouse WG, Gibb BE, Hankin BL, Cornette MM. The hopelessness theory of suicidality. In: Joiner TE, Rudd MD, editors. Suicide science: Expanding the boundaries. Boston, MA: Kluwer Academic; 2000. pp. 17–32. [Google Scholar]
- Alexopoulos GS, Reynolds CF, 3rd, Bruce ML, Katz IR, Raue PJ, Mulsant BH, PROSPECT Group Reducing suicidal ideation and depression in older primary care patients: 24-month outcomes of the PROSPECT study. American Journal of Geratric Psychiatry. 2009;166:882–890. doi: 10.1176/appi.ajp.2009.08121779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bates D, Maechle M, Bolker B. lme4: Linear mixed-effects models using S4 classes. 2014 Available at http://CRAN.R-project.org/package=lme4.
- Beck AT. Hopelessness as a predictor of eventual suicide. Annals of the New York Academy of Sciences. 1986;487:90–96. doi: 10.1111/j.1749-6632.1986.tb27888.x. [DOI] [PubMed] [Google Scholar]
- Beck AT, Brown G, Steer RA. Prediction of eventual suicide in psychiatric inpatients by clinical ratings of hopelessness. Journal of Consulting and Clinical Psychology. 1989;57:309–310. doi: 10.1037//0022-006x.57.2.309. [DOI] [PubMed] [Google Scholar]
- Beck AT, Brown G, Berchick RJ, Stewart BL, Steer RA. Relationship between hopelessness and ultimate suicide: A replication of psychiatric outpatients. American Journal of Psychiatry. 1990;147:190–195. doi: 10.1176/ajp.147.2.190. [DOI] [PubMed] [Google Scholar]
- Borson S, Scanlan J, Brush M, Vitaliano P, Dokmak A. The mini-cog: A cognitive ‘vital signs’ measure for dementia screening in multi-lingual elderly. International Journal of Geriatric Psychiatry. 2000;15:1021–1027. doi: 10.1002/1099-1166(200011)15:11<1021::aid-gps234>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- Bruce ML, McVay J, Raue PJ, Brown EL, Meyers BS, Keohane DJ, Jagoda DR, Weber C. Major depression in elderly home health care patients. American Journal of Geratric Psychiatry. 2002;159:1367–1374. doi: 10.1176/appi.ajp.159.8.1367. [DOI] [PubMed] [Google Scholar]
- Burnham KP, Anderson D. Model selection and multi-model inference: A practical information-theoretic approach. New York: Springer; 2002. [Google Scholar]
- Centers for Disease Control and Prevention. Strategic direction for the prevention of suicidal behaviors: Promoting individual, family, and community connectedness to prevent suicidal behavior. Atlanta, GA: 2008. Available at http://www.cdc.gov/ViolencePrevention/pdf/Suicide_Strategic_Direction_Full_Version-a.pdf. [Google Scholar]
- Choi NG, Marti CN, Bruce ML, Hegel MT, Wilson NL, Kunik ME. Six-month post-intervention depression and disability outcomes of in-home telehealth problem-solving therapy for depressed, low-income homebound older adults. Depression & Anxiety. 2014;31:653–661. doi: 10.1002/da.22242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conwell Y, Van Orden K, Caine ED. Suicide in older adults. Psychiatric Clinics of North America. 2011;3:451–468. doi: 10.1016/j.psc.2011.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cuijpers P, de Beurs DP, van Spijker BA, Berking M, Andersson G, Kerkhof AJ. The effects of psychotherapy for adult depression on suicidality and hopelessness: a systematic review and meta-analysis. Journal of Affective Disorders. 2013;144:183–190. doi: 10.1016/j.jad.2012.06.025. [DOI] [PubMed] [Google Scholar]
- Cuijpers P, Karyotaki E, Pot AM, Park M, Reynolds CF., 3rd Managing depression in older age: psychological interventions. Maturitas. 2014;79:160–169. doi: 10.1016/j.maturitas.2014.05.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cukrowicz KC, Jahn DR, Graham RD, Poindexter EK, Williams RB. Suicide risk in older adults: evaluating models of risk and predicting excess zeros in a primary care sample. Journal of Abnormal Psychology. 2013;122:1021–1030. doi: 10.1037/a0034953. [DOI] [PubMed] [Google Scholar]
- De Leo D, Draper BM, Snowdon J, Kõlves K. Contacts with health professionals before suicide: Missed opportunities for prevention? Comprehensive Psychiatry. 2013;54:1117–1123. doi: 10.1016/j.comppsych.2013.05.007. [DOI] [PubMed] [Google Scholar]
- Depression Rating Scale Standardization Team. GRID-HAMD-17 GRID-HAMD-21 Structured Interview Guide. San Diego: International Society for CNS Drug Development; 2003. [Google Scholar]
- D’Zurilla TJ, Nezu AM. Problem-solving therapy: A positive approach to clinical intervention. New York: Springer; 2007. [Google Scholar]
- Ell K, Unützer J, Aranda M, Sanchez K, Lee PJ. Routine PHQ-9 depression screening in home health care: Depression prevalence, clinical and treatment characteristics, and screening implementation. Home Health Care Services Quarterly. 2005;24:1–19. doi: 10.1300/J027v24n04_01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feingold A. Effect sizes for growth-modeling analysis for controlled clinical trials in the same metric as for classical analysis. Psychological Methods. 2009;14:43–53. doi: 10.1037/a0014699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hegel MT, Areán P. PST-PC manual. 2002 Available at http://impact-uw.org/tools/pst_manual.html.
- Hopko DR, Funderburk JS, Shorey RC, McIndoo CC, Ryba MM, File AA, Vitulano M. Behavioral activation and problem-solving therapy for depressed breast cancer patients: Preliminary support for decreased suicidal ideation. Behavior Modification. 2013;37:747–767. doi: 10.1177/0145445513501512. [DOI] [PubMed] [Google Scholar]
- Hu LT, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6:1–55. [Google Scholar]
- Kim YA, Bogner HR, Brown GK, Gallo JJ. Chronic medical conditions and wishes to die among older primary care patients. International Journal of Psychiatry in Medicine. 2006;36:183–198. doi: 10.2190/3QXD-UR0H-K8FH-2CU8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kovacs M, Beck AT, Weissman A. Hopelessness: An indicator of suicide risk. Suicide. 1975;5:98–103. [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL. The PHQ-9: A new depression and diagnostic severity measure. Psychiatric Annals. 2002;32:509–521. [Google Scholar]
- Lapierre S, Erlangsen A, Waern M, De Leo D, Oyama H, Scocco P, International Research Group for Suicide among the Elderly A systematic review of elderly suicide programs. Crisis. 2011;32:88–98. doi: 10.1027/0227-5910/a000076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacCallum RC, Browne MW, Sugawara HM. Power analysis and determination of sample size for covariance structure modeling. Psychological Methods. 1996;1:130–149. [Google Scholar]
- MacKinnon D. Introduction to statistical mediation analysis. New York: Routledge; 2008. [Google Scholar]
- Moberg PJ, Lazarus LW, Mesholam RI, Bilker W, Chuy IL, Neyman I, Markvart V. Comparison of the standard and structured interview guide for the Hamilton Depression Rating Scale in depressed geriatric inpatients. American Journal of Geriatric Psychiatry. 2001;9:35–40. [PubMed] [Google Scholar]
- Muthén L, Muthén B. Mplus user’s guide: Statistical analysis with latent variables. Los Angeles, CA: Muthén & Muthén; 1998–2012. [Google Scholar]
- National Center for Health Statistics. Health, United States, 2013: With special feature on prescription drugs. Hyattsville, MD: 2014. [PubMed] [Google Scholar]
- Nelson JC, Delucchi K, Schneider L. Suicidal thinking and behavior during treatment with sertraline in late-life depression. American Journal of Geriatric Psychiatry. 2007;15:573–580. doi: 10.1097/JGP.0b013e318050c9c2. [DOI] [PubMed] [Google Scholar]
- Neuringer C. Psychological assessment of suicidal risk. Springfield, IL: Charles C. Thomas; 1974. [Google Scholar]
- Nezu AM, Nezu CM, D’Zurilla T. Problem-solving therapy: A treatment manual. NewYork: Springer; 2012. [Google Scholar]
- O’Riley AA, Van Orden KA, He H, Richardson TM, Podgorski C, Conwell Y. Suicide and death ideation in older adults obtaining aging services. American Journal of Geratric Psychiatry. 2014;22:614–622. doi: 10.1016/j.jagp.2012.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods. 2008;40:879–891. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- Raudenbush SW, Bryk AS. Hierarchical linear models: applications and data analysis methods. Sage; Thousand Oaks, CA: 2001. [Google Scholar]
- Raue PJ, Meyers BS, Rowe JL, Heo M, Bruce ML. Suicidal ideation among elderly homecare patients. International Journal of Geriatric Psychiatry. 2007;22:32–37. doi: 10.1002/gps.1649. [DOI] [PubMed] [Google Scholar]
- Rowe JL, Bruce ML, Conwell Y. Correlates of suicide among home health care utilizers who died by suicide and community controls. Suicide and Life Threatening Behavior. 2006;36:65–75. doi: 10.1521/suli.2006.36.1.65. [DOI] [PubMed] [Google Scholar]
- Rowe JL, Conwell Y, Schulberg HC, Bruce ML. Social support and suicidal ideation in older adults using home healthcare services. American Journal of Geratric Psychiatry. 2006;14:758–766. doi: 10.1097/01.JGP.0000218324.78202.25. [DOI] [PubMed] [Google Scholar]
- Rudd MD, Rajab MH, Dahm PF. Problem-solving appraisal in suicide ideators and attempters. American Journal of Orthopsychiatry. 1994;64:136–149. doi: 10.1037/h0079492. [DOI] [PubMed] [Google Scholar]
- Sachs-Ericsson N, Hames JL, Joiner TE, Corsentino E, Rushing NC, Palmer E, Steffens DC. Differences between suicide attempters and nonattempters in depressed older patients: Depression severity, white-matter lesions, and cognitive functioning. American Journal of Geratric Psychiatry. 2014;22:75–85. doi: 10.1016/j.jagp.2013.01.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singer J, Willett J. Applied longitudinal data analysis: Modeling change and event occurrence. New York: Oxford University Press; 2003. [Google Scholar]
- Sirey JA, Bruce ML, Carpenter M, Booker D, Reid MC, Newell KA, Alexopoulos GS. Depressive symptoms and suicidal ideation among older adults receiving home-delivered meals. International Journal of Geriatric Psychiatry. 2008;23:1306–1311. doi: 10.1002/gps.2070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szanto K, Lenze EJ, Waem M, Duberstein P, Bruce ML, Epstein-Lubow G, Conwell Y. Research to reduce the suicide rate among older adults: Methodology roadblocks and promising paradigms. Psychiatric Services. 2013;64:586–589. doi: 10.1176/appi.ps.003582012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szanto K, Mulsant BH, Houck P, Dew MA, Reynolds CF., 3rd Occurrence and course of suicidality during short-term treatment of late-life depression. Archives of General Psychiatry. 2003;60:610–617. doi: 10.1001/archpsyc.60.6.610. [DOI] [PubMed] [Google Scholar]
- Szanto K, Reynolds CF, 3rd, Conwell Y, Begley AE, Houck P. High levels of hopelessness persist in geriatric patients with remitted depression and a history of attempted suicide. Journal of the American Geriatrics Society. 1998;46:1401–1406. doi: 10.1111/j.1532-5415.1998.tb06007.x. [DOI] [PubMed] [Google Scholar]
- Unützer J, Katon W, Callahan CM, Williams JW, Jr, Hunkeler E, Harpole L, Impact Investigators Collaborative care management of late-life depression in the primary care setting: a randomized controlled trial. JAMA. 2002;288:2836–2845. doi: 10.1001/jama.288.22.2836. [DOI] [PubMed] [Google Scholar]
- Unützer J, Tang L, Oishi S, Katon W, Williams JW, Jr, Hunkeler E, Impact Investigators Reducing suicidal ideation in depressed older primary care patients. Journal of the American Geriatrics Society. 2006;54:1550–1556. doi: 10.1111/j.1532-5415.2006.00882.x. [DOI] [PubMed] [Google Scholar]
- Weishaar ME, Beck AT. Hopelessness and suicide. International Review of Psychiatry. 1992;4:177–184. [Google Scholar]