Abstract
Background
p16INK4A expression has been used as a surrogate marker for human papillomavirus (HPV) infection in cervical cancer and head and neck cancer. p53 has also been reported as a feasible marker to identify HPV-positive oropharyngeal carcinoma and penile lesions. This study aimed to investigate p16INK4A and p53 expression levels and their correlation with HPV status and clinical parameters in Kazakh patients with esophageal squamous cell carcinoma.
Methods
Immunohistochemical expression of p16INK4A and p53 were evaluated in 163 cases of esophageal squamous cell carcinoma in Kazakh patients. The presence of HPV DNA was detected by polymerase chain reaction.
Results
p16INK4A-positive expression was detected in 19.0 % of patients, and its expression was significantly correlated with a lower frequency of lymph node metastasis (p = 0.038). By contrast no significant association was found between p16INK4A-positive expression and HPV status (correlation coefficient = -0.062, p = 0.499). p16INK4A-positive expression did not affect the odds of tumors being HPV positive (odds ratio [OR] = 0.727 with 95 % confidence interval [CI] = 0.288–1.836). The sensitivity of p16INK4A-positive expression as an HPV marker was 0.164, with a specificity of 0.788 and a positive predictive value of 0.391. p53-positive expression was present in 88.3 % of all cases. Although no significant correlation with available clinical parameters was found, a significantly inverse correlation was observed between p53 expression and HPV status (correlation coefficient = -0.186, p = 0.039). Moreover, p53-positive expression decreased the odds of tumors being HPV positive (OR = 0.292 with 95 % CI = 0.086–0.990). The sensitivity of p53-negative expression as an HPV marker was 0.179, with a specificity of 0.940 and a positive predictive value of 0.714. The overall HPV prevalence was high (45.5 %) in Kazakh patients, with no significant association between HPV positivity and available clinical parameters or combined p16INK4A/p53 expression.
Conclusions
p16INK4A-positive expression was associated with lymph node metastasis. Results indicate that p53-negative expression and not p16INK4A-positive expression may be used as a marker for HPV status in ESCC; however, this finding requires further studies for validation.
Keywords: p16INK4A, p53, Human papillomavirus, Esophageal squamous cell carcinoma, Kazakh
Background
Esophageal cancer (EC), is one of the most common malignancies and the sixth most frequent cause of cancer-related death worldwide with a global number of 400,000 deaths in 2012 (http://globocan.iarc.fr/Default.aspx). China is one of the geographical regions with the highest incidence of esophageal cancer. Of the two main histological types, the squamous cell carcinoma (ESCC) and the adenocarcinoma (EAC), the former is the predominant type in China accounting for more than 80 % of cases [1]. The Kazakh population, which is a nomadic tribe and mainly residing in Xinjiang, Northwestern China, shows higher ESCC incidence and mortality compared with other ethnic groups in China [2]. A better understanding of ESCC pathogenesis for early diagnosis is crucial considering the present difficulties in detecting early symptoms, identifying unfavourable prognosis, and low 5-year survival rate.
Human papillomavirus (HPV) are small circular non-enveloped double-stranded DNA viruses exhibiting strict epithelial tropism and infecting either mucosa (α-papillomaviruses) or skin (β- and γ-papillomaviruses) [3]. Several studies have demonstrated that HPV infection is the main cause of cervical cancer and head and neck cancer [4, 5]. HPV infection in esophageal cancer was first reported in 1982 based on histological observations [6]. The HPV16 and HPV18 were the viral genotypes most frequently identified in the majority of the studies [7, 8]. Few studies searched for mucosal as well as cutaneous HPV sequences in esophageal lesions [9]. Recently it has been reported that the HPV prevalence in ESCC of Kazakh patients ranged from 30 % to 66.67 % [10–12]. For such reason the identification of HPV status in the ESCC lesions is important to establish their etiology and prognostic significance [13].
HPV E6 and E7 oncoproteins are able to inactivate p53 and pRb oncosuppressors, respectively, interfering with cell cycle control. The oncosuppressor pRB is a negative regulator of the cyclin-dependent kinase inhibitor p16INK4A and its degradation mediated by HPV E7 causes the abnormal p16INK4A and p53 expression. Surrogate markers of HPV infection are essential for cancer screening given the low cost and high sensitivity of immunohistochemistry (IHC). Studies have shown that p16INK4A expression measured by IHC correlates with the presence of HPV DNA and thus can be used as a surrogate marker of HPV infection in squamous cell carcinoma (SCC) of the cervix, vagina, and oropharynx [14–17]. p53 has also been reported as a useful marker for identifying HPV-positive oropharyngeal carcinoma [18] and penile lesions [19]. However, the biomarkers of HPV status in ESCC should be further validated to improve their use for diagnosis and treatment.
This study aimed to investigate p16INK4A and p53 expression levels and their correlation with HPV status and clinical parameters in Kazakh patients to raise the possibility of using them as surrogate markers of HPV infection in ESCC.
Methods
Patients and samples
All formalin-fixed paraffin-embedded tissue (FFPE) blocks from 163 Kazakh patients who underwent esophagectomy without prior chemotherapy or radiotherapy were obtained from the First Affiliated Hospital of Shihezi University School of Medicine, the People’s Hospital of Xinjiang Uyghur Autonomous Region, and Xinjiang Yili Prefecture Friendship Hospital in Northwestern China from 1984 to 2013. Detailed clinical data [17] of all the patients, including gender, age, differentiation, invasion depth, lymph node metastasis, and UICC stage (TNM stage), were also collected. The ESCC patients were staged according to the Cancer Staging Manual of the American Joint Committee on Cancer. The research protocol used in this study was in accordance with the medical ethics and human clinical trial committee of the Shihezi University School of Medicine, and all recruited subjects were enrolled with written informed consent.
Tissue microarray construction
All tissues were sectioned and stained with hematoxylin and eosin. Furthermore, the morphologically representative tissue areas of each sample identified from these stained slides were marked. Subsequently, the fields corresponding to these selected regions were located in the paraffin block for tissue microarray (TMA) construction. 1.0 mm diameter tissue cylinders were punched from these areas of each donor tissue block and brought into a recipient paraffin block using a homemade semi-automated tissue arrayer (Alphelys, Plaisir, France). The region of each tissue cylinder was reviewed to guarantee that at least 70 % represented the typical region of interest in that sample. Finally, 5 μm-thick serial sections were prepared from the TMA blocks for immunohistochemical staining.
Immunohistochemistry
Immunohistochemical staining of p16INK4A and p53 were performed using an automated immunostainer (BOND-MAX, Leica). Slides were de-paraffinized using a bond dewax solution (29490, Leica) and rehydrated in absolute alcohol. Afterward, bond epitope retrieval solution 2 (ER20134, Leica) was used for epitope retrieval, and the slides were incubated for 20 min at 100 °C and 12 min at room temperature. The slides were washed with bond wash solution (W0080, Leica) for 3 min. Endogenous peroxidase activity was abolished by incubating the slides for 5 min in a peroxidase-blocking solution. A total of 150 μl of the primary antibody against p16INK4A (ZM-0205, dilution 1:500, ZSGQ-BIO) or p53 (DO-7, dilution 1:600, Gene Tech) was dropped onto each slide, followed by incubation for 15 min. After posting primary and polymery for 8 min each, the slides were incubated in DAB buffer for 5 min and then washed with distilled water. Subsequently, hematoxylin was added onto each slide followed by incubation for 5 min. The slides were dehydrated in graded alcohol to xylene and mounted on an anti-fade mounting medium with mounting glass. p16INK4A-positive cervical cancer and p53-positive esophageal cancer tissues were used as positive controls. The data of p16INK4A immunohistochemistry were available in 158 patients, whereas p53 expression was evaluable in 163 patients. Other samples were not evaluated because of the lack of carcinoma in the residual tissue material.
All the immunostained slides were independently evaluated by two experienced pathologists. Cases in which the two pathologists disagreed on the immunostaining results, a third pathologist was consulted to analyze the staining. The expressions of these two markers were scored based on cytoplasmic/nuclear staining intensity and percentage of positively stained cells. The staining intensity was categorized as follows: 0, negative; 1, buff; 2, yellow; and 3, brown. The percentages of positive stained cells were scored as follows: 0 (<5 % positive cells), 1 (6 %–25 % positive cells), 2 (26 %–50 % positive cells), 3 (51 %–75 % positive cells), or 4 (≥76 % positive cells). p16INK4A was considered positive if strong and diffuse staining was present in >50 % of the tumor cells [20, 21].
The percentages of positive stained cells and the staining intensities were further multiplied to generate the immunoreactivity score for each case and evaluate p53 expression. Four categories of expression were listed as follow: − (a score of 0–1), + (a score of 2–4), ++ (a score of 5–8), and +++ (a score of 9–12) [22]. p53 was considered negative when the score was between + and ++ categories, whereas the +++ score and null expression category were considered p53 positive [18].
DNA preparation and quality control
The FFPE samples were collected in 5 μm thick sections with 10–15 slides per sample for genomic DNA extraction using QIAamp DNA FFPE Tissue Kit (Qiagen, Hilden, Germany) according to the manufacturer’s instructions. The methods used were as previously described [23] to minimize the possibility of cross-contamination. Subsequently, 75 % medicinal alcohol was used to disinfect the blade before sectioning each sample, and paraffin-only samples were cut to act as no contamination control for every five samples. DNA extraction, polymerase chain reaction (PCR) amplification, and PCR product detection were performed in separate spaces. As an internal control, the quality of the prepared DNA was validated through PCR with a human β-globin (forward: 5′-CAGACACCATGGTGCACCTGAC-3′ and reverse: 5′-CCAATAGGCAGAGAGAGTCAGTG-3′). The DNA with sufficient quality was chosen for further study.
HPV detection
HPV DNA was detected as previously described [12]. Non-degenerate primer sets GP5+/6+ (forward: TTGGATCCTTTGTACTGTGGTAGATACTAC and reverse: TTGGATCCGAAAAATAAACTGTAAATCATATTC) amplifying a 150 bp fragment within L1 gene of a wide range of HPV types were used. HPV16 E7 gene was amplified with forward primer GATGAAATAGATGGTCCAGC and reverse primer GCTTTGTACGCACAACCGAGC. A total of 5 μL of extracted DNA was amplified in a final volume of 25 μL for each PCR reaction. The reaction was performed on Life technology under the following conditions: at 95 °C for 10 min, followed by 40 cycles of denaturation at 94 °C for 30 s, annealing at 42 °C for 90 s, and extension at 72 °C for 30 s, with a final extension at 72 °C for 5 min. The assays of the samples were run in triplicate with positive and negative controls. Subsequently, the 10 % DNA sequence of the positive products was identified using NCBI Blast (www.ncbi.nlm.nih.gov/BLAST) to confirm the HPV type detected by PCR.
Statistical analysis
All statistical analyses were performed using SPSS Statistics 17.0 software. Associations among p16INK4A, p53 expression, HPV status, and clinical parameters were analyzed using χ2-test or Fisher’s exact test. Spearman’s rank correlation coefficients were analyzed to investigate the possible correlations between HPV status and p16INK4A and p53 expression levels. All statistical tests were two-sided and p-values considered significant when p < 0.05.
Results
Immunohistochemical expression of p16INK4A in correlation with clinical parameters and HPV status in Kazakh patients with ESCC
A total of 158 ESCC samples were analyzed for p16INK4A expression through immunohistochemistry, with 30 (19.0 %) and 128 (81.0 %) showing positive and negative expressions, respectively (Fig. 1). A significant inverse correlation was observed between p16INK4A expression and lymph node invasion (p = 0.038). Patients with p16INK4A-positive expression had significantly less lymph node metastasis (35.7 % versus 57.5 %) and were diagnosed at less advanced TNM stage, although the difference was not significant (p = 0.147). No correlation was found between p16INK4A expression and gender, age at diagnosis, histopathological grade, and invasion depth (Table 1).
Fig. 1.
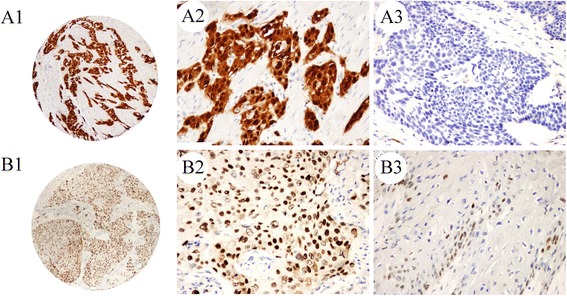
Immunohistochemical staining of p16 and p53 in Kazakh ESCC tissues. High p16 and p53 expression levels in ESCC (A1, p16; B1, p53; original magnification 40×). High power view (original magnification 200×) shows positive staining for p16 and p53 in the nucleus/cytoplasm and nucleus staining of cancer cells, respectively (A2, p16; B2, p53) and p16- and p53-negative expression (A3, p16; B3, p53; original magnification 200×)
Table 1.
p16INK4A expression in correlation with clinical parameters and HPV status in Kazakh patients with ESCC
| Clinical properties | Total | p16 expression (n/%) | ||
|---|---|---|---|---|
| Negative (%) | Positive (%) | P value | ||
| Gender | ||||
| Male | 103 | 85(66.4 %) | 18(60.0 %) | 0.507 |
| Female | 55 | 43(33.6 %) | 12(40.0 %) | |
| Age (mean) | ||||
| < 58 | 85 | 60(48.0 %) | 13(50.0 %) | 0.853 |
| ≥ 58 | 67 | 65(52.0 %) | 13(50.0 %) | |
| Histopathological grade | ||||
| Well | 38 | 34(27.2 %) | 4(13.3 %) | 0.268 |
| Moderate | 97 | 76(60.8 %) | 21(70.0 %) | |
| Poor | 20 | 15(12.0 %) | 5(16.7 %) | |
| Invasion depth | ||||
| T1-T2 | 78 | 63(53.8 %) | 15(51.7 %) | 0.838 |
| T3-T4 | 68 | 54(46.2 %) | 14(48.3 %) | |
| Lymphatic invasion | ||||
| N0 | 66 | 48(42.5 %) | 18(64.3 %) | 0.038 |
| N1-N3 | 75 | 65(57.5 %) | 10(35.7 %) | |
| TNM Staging | ||||
| I/II | 76 | 59(60.8 %) | 17(77.3 %) | 0.147 |
| III/IV | 43 | 38(39.2 %) | 5(22.7 %) | |
| HPV infection | ||||
| Negative | 66 | 52(53.1 %) | 14(60.9 %) | 0.499 |
| Positive | 55 | 46(46.9 %) | 9(39.1 %) | |
P < 0.05 indicates a significant association among the variables
Although p16INK4A is used as a surrogate marker for HPV-associated cervical cancer and head and neck cancer, the prevalence of HPV infection in p16INK4A-positive and p16INK4A-negative specimens demonstrated no statistically significant difference (correlation coefficient = -0.062, p = 0.499). p16INK4A-positive expression did not affect the odds of tumors being HPV positive (odds ratio [OR] = 0.727 with 95 % confidence interval [CI] 0.288–1.836). The sensitivity of p16INK4A-positive expression as an HPV marker was 0.164, with specificity of 0.788 and positive predictive value of 0.391.
Immunohistochemical expression of p53 in correlation with clinical parameters and HPV status in Kazakh patients with ESCC
A total of 163 ESCC cases were included in this analysis, of which 144 (88.3 %) and 19 (11.7 %) exhibited p53 positive and negative expression, respectively (Fig. 1). Patients with p53 positive expression were diagnosed at a younger age (53.6 % versus 36.8 %) and with moderate to poor histopathological grade (77.1 % versus 57.9 %), although the difference was not significant (p = 0.171 and 0.070, respectively). No correlation was detected between p53 expression and other clinical parameters (Table 2).
Table 2.
p53 expression in relation to clinical parameters and HPV status in Kazakh patients with ESCC
| Clinical properties | Total | p53 expression (n/%) | ||
|---|---|---|---|---|
| Negative (%) | Positive (%) | P value | ||
| Gender | ||||
| Male | 106 | 10(52.6 %) | 96(66.7 %) | 0.228 |
| Female | 57 | 9(47.4 %) | 48(33.3 %) | |
| Age (mean) | ||||
| < 58 | 82 | 7(36.8 %) | 75(53.6 %) | 0.171 |
| ≥ 58 | 77 | 12(63.2 %) | 65(46.4 %) | |
| Histopathological gradea | ||||
| Well | 40 | 8(42.1 %) | 32(22.9 %) | 0.070 |
| Moderate | 98 | 8(42.1 %) | 91(65.0 %) | |
| Poor | 20 | 3(15.8 %) | 17(12.1 %) | |
| Invasion depth | ||||
| T1-T2 | 76 | 8(47.1 %) | 68(51.1 %) | 0.752 |
| T3-T4 | 74 | 9(52.9 %) | 65(48.9 %) | |
| Lymphatic invasion | ||||
| N0 | 68 | 6(33.3 %) | 62(49.2 %) | 0.207 |
| N1-N3 | 76 | 12(66.7 %) | 64(50.8 %) | |
| TNM Staging | ||||
| I/II | 79 | 9(60.0 %) | 70(64.2 %) | 0.750 |
| III/IV | 45 | 6(40.0 %) | 39(35.8 %) | |
| HPV infection | ||||
| Negative | 67 | 4(28.6 %) | 63(57.8 %) | 0.039 |
| Positive | 56 | 10(71.4 %) | 46(42.2 %) | |
P < 0.05 indicates a significant association among the variables
a Well differentiation vs. moderate + poor differentiation
A significantly inverse correlation between p53 expression and HPV status was found (correlation coefficient = -0.186, p = 0.039). The prevalence of HPV DNA in p53-negative specimens was significantly increased compared with that in p53-positive tumors (71.4 % versus 42.2 %). p53-positive expression decreased the odds of tumors being HPV positive (OR = 0.292 with 95 % CI = 0.086–0.990). The sensitivity of p53-negative expression as an HPV marker was 0.179, with specificity of 0.940 and positive predictive value of 0.714.
Correlation of HPV status with clinical characteristics and p16INK4A and p53 expression levels
Among the 123 Kazakh patients with ESCC evaluated for HPV status 56 (45.5 %) were found HPV-positive and 67 (54.5 %) HPV-negative (Table 3). No significant differences were observed between HPV positivity and gender, patient age, tumor differentiation, invasion depth, lymph node metastasis, or TNM stage.
Table 3.
Correlation between HPV status and clinical parameters in Kazakh patients with ESCC
| Clinical properties | Total | HPV status (n/%) | ||
|---|---|---|---|---|
| Negative (%) | Positive (%) | P value | ||
| Gender | ||||
| Male | 78 | 42(62.7 %) | 36(64.3 %) | 0.855 |
| Female | 45 | 25(37.3 %) | 20(35.7 %) | |
| Age (mean) | ||||
| <57 | 55 | 29(43.9 %) | 26(47.3 %) | 0.714 |
| ≥57 | 66 | 37(56.1 %) | 29(52.7 %) | |
| Histopathological gradea | ||||
| Well | 28 | 15(22.4 %) | 13(23.6 %) | 0.937 |
| Moderate | 77 | 42(62.7 %) | 35(63.6 %) | |
| Poor | 17 | 10(14.9) | 7(12.7 %) | |
| Invasion depth | ||||
| T1-T2 | 59 | 37(55.2 %) | 22(40.0 %) | 0.094 |
| T3-T4 | 63 | 30(44.8 %) | 33(60.0 %) | |
| Lymphatic invasion | ||||
| N0 | 55 | 28(43.8 %) | 27(50.9 %) | 0.438 |
| N1-N3 | 62 | 36(56.2 %) | 26(49.1 %) | |
| TNM Staging | ||||
| I/II | 74 | 40(61.5 %) | 34(65.4 %) | 0.668 |
| III/IV | 43 | 25(38.5 %) | 18(34.6 %) | |
a Well differentiation vs. moderate + poor differentiation
The relationship between HPV status and p16INK4A or p53 expression levels has been analyzed in order to identify possible associations. Previous studies reported that high-risk HPV16 was the predominant genotype in patients with ESCC among the Kazakh populations [24, 25], therefore we stratified the results in HPV16 positive cases to see if there was any association with the expression of p16INK4A and p53. Results showed that HPV16 infection was associated with p53 (p = 0.012) but not with p16INK4A expression (p = 0.987). Similar results were obtained considering all HPV infections. p16INK4A and p53 expression patterns exhibited a slight inverse correlation, but this correlation was not statistically significant (correlation coefficient = -0.061, p = 0.455, Table 4). Furthermore, the combined p16INK4A/p53 expression was not significantly correlated with HPV status in Kazakh patients with ESCC (correlation coefficient = -0.077, p = 0.420, Table 5).
Table 4.
Correlation between p16INK4A and p53 expression in Kazakh patients with ESCC
| p16- | p16+ | Correlation coefficient | P value | |
|---|---|---|---|---|
| p53- | 14 | 5 | -0.061 | 0.455 |
| p53+ | 107 | 25 |
Table 5.
Correlation between p16INK4A/p53 expression and HPV status in Kazakh patients with ESCC
| HPV status | Correlation coefficient | P value | ||
|---|---|---|---|---|
| Negative | Positive | |||
| p16+ p53+ | 12 | 7 | -0.077 | 0.420 |
| p16- p53- | 2 | 8 | ||
| p16+ p53- | 2 | 2 | ||
| p16- p53+ | 48 | 32 | ||
Discussion
We have evaluated the HPV status and p16INK4A and p53 expression levels in ESCC from Kazakh patients. One limitation of our study is the relative small sample size. Nevertheless, this is among the largest studies addressing p16INK4A and/or p53 expression and HPV infection in ESCC of Kazakh population [26, 27].
The use of p16INK4A immunohistochemical analysis as a surrogate marker of HPV infection in squamous cell carcinoma of the cervix, vagina, and oropharynx has been supported by many studies in recent years [15, 17, 28–30]. The p16INK4A expression is indicative of high risk HPV infection in cancers of squamous cell origin [31]. In our study, patients with p16INK4A overexpression have a better prognosis, are correlated with less lymph node metastasis (p = 0.038), and are frequently associated with lower-grade TNM stage (p = 0.147), which are in accordance with previous studies [21, 26, 32]. Furthermore, p16INK4A positivity has been detected in 16.4 % of HPV-positive patients with ESCC, which is lower than previously published data reporting a range of prevalence between 20 % and 86.2 % [26, 33, 34]. In addition, a correlation between p16INK4A overexpression and HPV DNA positivity was previously found in HPV-related oropharynx carcinoma [28, 29, 35]. This association has also been previously reported in ESCC [26, 36]. However, in the present study the p16INK4A over expression is not associated with HPV status (p = 0.499, OR = 0.727 with 95 % CI = 0.288–1.836). This finding is consistent which data described in a meta-analysis [37] and recent study [34]. The inconsistency may be explained by the limited number of patients included in these studies and the lack of uniformity in cut-off values (different criteria ranged from >0 % to >70 % of tumor cells displaying moderate to strong staining) to define p16INK4A overexpression. In the present study, a cut-off value of 50 %, which has been validated to correlate with the presence of HPV in oropharyngeal SCC [16, 21], was utilized to evaluate p16INK4A staining. The discrepant results may also be attributed to the variation in HPV prevalence because of different geographic areas and ethnicity of patients [38, 39]. In addition to previously described factors, which may influence the accuracy of p16INK4A staining for HPV status, an aberrant p16INK4A expression such as p16INK4A (+)/HPV(–) and p16INK4A (–)/HPV(+) cases in various cancers exists [15, 17, 40, 41]. Many of tumors with high p16INK4A expression were HPV-negative indicating that non-HPV factors also lead to p16 overexpression in ESCC. The diametrical expression of p16INK4A may be caused by different genetic alterations. For example, 11q is frequently detected to be gained in HPV-negative oropharyngeal SCC, wherein Ets (a protein that can raise the p16INK4A level) is located [15, 42]. Rb1 alterations and subsequent p16 INK4A overexpression have also been described in non-HPV-driven tumors [43]. Therefore, the p16INK4A expression in HPV-negative tumors needs to be further investigated to obtain additional information in ESCC etiology, especially in low-incidence HPV geographic regions.
Acting as a transcription factor in cell cycle regulation, genomic stability and apoptosis, p53 protein displays the highest correlation with a number of cancers [44, 45]. p53 expression may be regarded as an indicator of p53 gene mutation. p53 levels are generally low or even undetectable under normal conditions [46]. However, p53 shows nuclear staining because of the accumulation of mutant p53, which is resistant to degradation. Although accumulation of p53 identified by IHC does not necessarily indicate gene mutation, p53 overexpression in most cases (85 %) implies an underlying mutation [47]. p53 has also been reported as a feasible marker for identifying HPV-positive oropharyngeal carcinoma and penile lesions [18, 19]. In the present study, patients with p53-positive expression were younger (p = 0.171) and had poorer differentiation levels (p = 0.070) than those with p53-negative expression, although these differences were not significant. Similar to previously reported data, [27, 48], these results indicate that p53 may serve as an unfavourable prognostic marker in ESCC. Moreover, p53 expression exhibited a significantly inverse correlation with HPV status (p = 0.039, OR = 0.292 with 95 % CI = 0.086–0.990), which is in accordance with a previous study [49]. HPV-associated oropharyngeal SCCs generally show a low level of p53 protein because of degradation through viral E6 protein [18], whereas HPV-negative tumors show absent or high p53 protein level because of nonsense or missense p53 mutations [50]. Thus, p53 IHC may be used as a rapid, easy, and inexpensive screening test with high specificity (0.940) and high positive predictive value (0.714) for HPV in ESCC. However, p53 IHC should be evaluated in larger studies given the small number of p53-negative patients.
HPV positivity was detected in 45.5 % of ESCC patients in this study, which is similar with previously reported data in Kazakhs [10–12], with a prevalence ranging from 30 % to 66.67 %. No correlation was observed between HPV positivity and clinicopathological characteristics, which is in agreement with previous studies on ESCC [51]. However this finding is not in agreement with results obtained in cervical and head and neck cancer patients [17, 52]. Nevertheless, several studies have suggested that HPV mRNA detection may differentiate active HPV infections from inactive viruses and transient HPV contamination [53, 54]. In addition, the correlation between HPV infection and p16INK4A and p53 co-expression did not statistically differ. Likewise, p16INK4A and p53 expression levels have been analyzed in primary adenocarcinoma of the urinary bladder on 36 samples. A slight inverse correlation between p16INK4A and p53 expression was observed but without statistical significance [31], which is consistent with the present results.
Conclusions
In summary, p16INK4A-positive expression should not be interpreted as a reliable surrogate marker for HPV infection in Kazakhs with ESCC but can indicate lower risk of lymph node metastasis. Our findings show that p53 expression may be a useful biomarker for diagnosis and prognosis of HPV-positive ESCC. Nonetheless, further studies should be performed to investigate toinvestigate the molecular alterations of these cell-cycle related proteins to elucidate ESCC pathogenesis.
Acknowledgements
We thank Dr. Louise T. Chow (University of Alabama at Birmingham) for her helpful suggestions. This work was supported by grants from the National Natural Science Foundation of China (No. 81460416, 81560399, 81260301), the Ministry of Science and Technology of China (2012AA02A503), and the Scientific Research Start-up Capital for High-level Talents of Shihezi University (RCZX201444, RCZX201229).
Footnotes
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
LW, JL, and JH performed the experiment and drafted the manuscript. ML, XC, SL, XY, ZZ, WL, HL, LP, YC and JZ participated in patients’ recruitment, materials collection and data interpretation. LW and FL participated in the design of the study and revision of the manuscript. All authors read and approved the final manuscript.
Contributor Information
Jin Zhao, Email: zhaojin7736@126.com.
Feng Li, Email: lifeng7855@126.com.
References
- 1.Kamangar F, Dores GM, Anderson WF. Patterns of cancer incidence, mortality, and prevalence across five continents: defining priorities to reduce cancer disparities in different geographic regions of the world. J Clin Oncol. 2006;24:2137–2150. doi: 10.1200/JCO.2005.05.2308. [DOI] [PubMed] [Google Scholar]
- 2.Zheng S, Vuitton L, Sheyhidin I, Vuitton DA, Zhang Y, Lu X. Northwestern China: a place to learn more on oesophageal cancer. Part one: behavioural and environmental risk factors. Eur J Gastroenterol Hepatol. 2010;22:917–925. doi: 10.1097/MEG.0b013e3283313d8b. [DOI] [PubMed] [Google Scholar]
- 3.Doorbar J, Quint W, Banks L, Bravo IG, Stoler M, Broker TR, Stanley MA. The biology and life-cycle of human papillomaviruses. Vaccine. 2012;30(Suppl 5):F55–70. doi: 10.1016/j.vaccine.2012.06.083. [DOI] [PubMed] [Google Scholar]
- 4.Hansson BG, Rosenquist K, Antonsson A, Wennerberg J, Schildt EB, Bladstrom A, Andersson G. Strong association between infection with human papillomavirus and oral and oropharyngeal squamous cell carcinoma: a population-based case-control study in southern Sweden. Acta Otolaryngol. 2005;125:1337–1344. doi: 10.1080/00016480510043945. [DOI] [PubMed] [Google Scholar]
- 5.Abate E, Aseffa A, El-Tayeb M, El-Hassan I, Yamuah L, Mihret W, Bekele L, Ashenafi S, El-Dawi N, Belayneh M, et al. Genotyping of human papillomavirus in paraffin embedded cervical tissue samples from women in Ethiopia and the Sudan. J Med Virol. 2013;85:282–287. doi: 10.1002/jmv.23437. [DOI] [PubMed] [Google Scholar]
- 6.Syrjanen K, Pyrhönen S, Aukee S, Koskela E. Squamous cell papilloma of the esophagus: a tumour probably caused by human papilloma virus (HPV) Diagn Histopathol. 1982;5:291–296. [PubMed] [Google Scholar]
- 7.Lavergne D, de Villiers EM. Papillomavirus in esophageal papillomas and carcinomas. Int J Cancer. 1999;80:681–684. doi: 10.1002/(SICI)1097-0215(19990301)80:5<681::AID-IJC8>3.0.CO;2-A. [DOI] [PubMed] [Google Scholar]
- 8.Halec G, Schmitt M, Egger S, Abnet CC, Babb C, Dawsey SM, Flechtenmacher C, Gheit T, Hale M, Holzinger D, et al. Mucosal Alpha-Papillomaviruses are not associated with Esophageal Squamous Cell Carcinomas: Lack of Mechanistic Evidence from South Africa, China and Iran and from a World-Wide Meta-Analysis. Int J Cancer. 2015. doi:10.1002/ijc.29911. http://www.ncbi.nlm.nih.gov/pubmed/26529033. [DOI] [PMC free article] [PubMed]
- 9.Tornesello ML, Monaco R, Nappi O, Buonaguro L, Buonaguro FM. Detection of mucosal and cutaneous human papillomaviruses in oesophagitis, squamous cell carcinoma and adenocarcinoma of the oesophagus. J Clin Virol. 2009;45:28–33. doi: 10.1016/j.jcv.2009.02.004. [DOI] [PubMed] [Google Scholar]
- 10.Lu XM, Monnier-Benoit S, Mo LZ, Xu SY, Pretet JL, Liu Z, Vuitton DA, Mougin C. Human papillomavirus in esophageal squamous cell carcinoma of the high-risk Kazakh ethnic group in Xinjiang, China. Eur J Surg Oncol. 2008;34:765–770. doi: 10.1016/j.ejso.2007.11.007. [DOI] [PubMed] [Google Scholar]
- 11.Chen WG, Yang CM, Xu LH, Zhang N, Liu XY, Ma YG, Huo XL, Han YS, Tian DA, Zheng Y. Gene chip technology used in the detection of HPV infection in esophageal cancer of Kazakh Chinese in Xinjiang Province. J Huazhong Univ Sci Technolog Med Sci. 2014;34:343–347. doi: 10.1007/s11596-014-1280-6. [DOI] [PubMed] [Google Scholar]
- 12.Zou N, Yang L, Chen L, Li T, Jin T, Peng H, Zhang S, Wang D, Li R, Liu C, et al. Heterozygote of TAP1 Codon637 decreases susceptibility to HPV infection but increases susceptibility to esophageal cancer among the Kazakh populations. J Exp Clin Cancer Res. 2015;34:70. doi: 10.1186/s13046-015-0185-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cao F, Han H, Zhang F, Wang B, Ma W, Wang Y, Sun G, Shi M, Ren Y, Cheng Y. HPV infection in esophageal squamous cell carcinoma and its relationship to the prognosis of patients in northern China. Sci World J. 2014;2014:804738. doi: 10.1155/2014/804738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bergeron C, Ronco G, Reuschenbach M, Wentzensen N, Arbyn M, Stoler M, von Knebel DM. The clinical impact of using p16(INK4a) immunochemistry in cervical histopathology and cytology: an update of recent developments. Int J Cancer. 2015;136:2741–2751. doi: 10.1002/ijc.28900. [DOI] [PubMed] [Google Scholar]
- 15.Wang H, Sun R, Lin H, Hu WH. P16INK4A as a surrogate biomarker for human papillomavirus-associated oropharyngeal carcinoma: consideration of some aspects. Cancer Sci. 2013;104:1553–1559. doi: 10.1111/cas.12287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Liu SZ, Zandberg DP, Schumaker LM, Papadimitriou JC, Cullen KJ. Correlation of p16 expression and HPV type with survival in oropharyngeal squamous cell cancer. Oral Oncol. 2015;51:862–869. doi: 10.1016/j.oraloncology.2015.06.014. [DOI] [PubMed] [Google Scholar]
- 17.Hellman K, Lindquist D, Ranhem C, Wilander E, Andersson S. Human papillomavirus, p16(INK4A), and Ki-67 in relation to clinicopathological variables and survival in primary carcinoma of the vagina. Br J Cancer. 2014;110:1561–1570. doi: 10.1038/bjc.2014.32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Holzinger D, Flechtenmacher C, Henfling N, Kaden I, Grabe N, Lahrmann B, Schmitt M, Hess J, Pawlita M, Bosch FX. Identification of oropharyngeal squamous cell carcinomas with active HPV16 involvement by immunohistochemical analysis of the retinoblastoma protein pathway. Int J Cancer. 2013;133:1389–1399. doi: 10.1002/ijc.28142. [DOI] [PubMed] [Google Scholar]
- 19.Mannweiler S, Sygulla S, Winter E, Regauer S. Two major pathways of penile carcinogenesis: HPV-induced penile cancers overexpress p16ink4a, HPV-negative cancers associated with dermatoses express p53, but lack p16ink4a overexpression. J Am Acad Dermatol. 2013;69:73–81. doi: 10.1016/j.jaad.2012.12.973. [DOI] [PubMed] [Google Scholar]
- 20.Salazar CR, Anayannis N, Smith RV, Wang Y, Haigentz M, Jr, Garg M, Schiff BA, Kawachi N, Elman J, Belbin TJ, et al. Combined P16 and human papillomavirus testing predicts head and neck cancer survival. Int J Cancer. 2014;135:2404–2412. doi: 10.1002/ijc.28876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lewis JS., Jr p16 Immunohistochemistry as a standalone test for risk stratification in oropharyngeal squamous cell carcinoma. Head Neck Pathol. 2012;6(Suppl 1):S75–82. doi: 10.1007/s12105-012-0369-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Li M, Cui X, Shen Y, Dong H, Liang W, Chen Y, Hu J, Li S, Kong J, Li H, et al. ORAOV1 overexpression in esophageal squamous cell carcinoma and esophageal dysplasia: a possible biomarker of progression and poor prognosis in esophageal carcinoma. Hum Pathol. 2015;46:707–715. doi: 10.1016/j.humpath.2015.01.009. [DOI] [PubMed] [Google Scholar]
- 23.Hu J, Li L, Pang L, Chen Y, Yang L, Liu C, Zhao J, Chang B, Qi Y, Liang W, Li F. HLA-DRB1*1501 and HLA-DQB1*0301 alleles are positively associated with HPV16 infection-related Kazakh esophageal squamous cell carcinoma in Xinjiang China. Cancer Immunol Immunother. 2012;61:2135–2141. doi: 10.1007/s00262-012-1281-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dong HC, Cui XB, Wang LH, Li M, Shen YY, Zhu JB, Li CF, Hu JM, Li SG, Yang L, et al. Type-specific detection of human papillomaviruses in Kazakh esophageal squamous cell carcinoma by genotyping both E6 and L1 genes with MALDI-TOF mass spectrometry. Int J Clin Exp Pathol. 2015;8:13156–13165. [PMC free article] [PubMed] [Google Scholar]
- 25.Wang X, Tian X, Liu F, Zhao Y, Sun M, Chen D, Lu C, Wang Z, Shi X, Zhang Q, et al. Detection of HPV DNA in esophageal cancer specimens from different regions and ethnic groups: a descriptive study. BMC Cancer. 2010;10:19. doi: 10.1186/1471-2407-10-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cao F, Zhang W, Zhang F, Han H, Xu J, Cheng Y. Prognostic significance of high-risk human papillomavirus and p16(INK4A) in patients with esophageal squamous cell carcinoma. Int J Clin Exp Med. 2014;7:3430–3438. [PMC free article] [PubMed] [Google Scholar]
- 27.Huang K, Chen L, Zhang J, Wu Z, Lan L, Wang L, Lu B, Liu Y. Elevated p53 expression levels correlate with tumor progression and poor prognosis in patients exhibiting esophageal squamous cell carcinoma. Oncol Lett. 2014;8:1441–1446. doi: 10.3892/ol.2014.2343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jalaly JB, Lewis JS, Jr., Collins BT, Wu X, Ma XJ, Luo Y, Bernadt CT. Correlation of p16 immunohistochemistry in FNA biopsies with corresponding tissue specimens in HPV-related squamous cell carcinomas of the oropharynx. Cancer Cytopathol. 2015;23:723–31. [DOI] [PubMed]
- 29.Cai CY, Chernock RD, Pittman ME, El-Mofty SK, Thorstad WL, Lewis JS. Keratinizing-type squamous cell carcinoma of the oropharynx p16 overexpression is associated with positive high-risk HPV status and improved survival. Am J Surg Pathol. 2014;38:809–815. doi: 10.1097/PAS.0000000000000183. [DOI] [PubMed] [Google Scholar]
- 30.Gronhoj Larsen C, Gyldenlove M, Jensen DH, Therkildsen MH, Kiss K, Norrild B, Konge L, von Buchwald C. Correlation between human papillomavirus and p16 overexpression in oropharyngeal tumours: a systematic review. Br J Cancer. 2014;110:1587–1594. doi: 10.1038/bjc.2014.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Alexander RE, Williamson SR, Richey J, Lopez-Beltran A, Montironi R, Davidson DD, Idrees MT, Jones CL, Zhang S, Wang L, et al. The expression patterns of p53 and p16 and an analysis of a possible role of HPV in primary adenocarcinoma of the urinary bladder. PLoS One. 2014;9:e95724. doi: 10.1371/journal.pone.0095724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fischer CA, Zlobec I, Green E, Probst S, Storck C, Lugli A, Tornillo L, Wolfensberger M, Terracciano LM. Is the improved prognosis of p16 positive oropharyngeal squamous cell carcinoma dependent of the treatment modality? Int J Cancer. 2010;126:1256–1262. doi: 10.1002/ijc.24842. [DOI] [PubMed] [Google Scholar]
- 33.Lofdahl HE, Du J, Nasman A, Andersson E, Rubio CA, Lu Y, Ramqvist T, Dalianis T, Lagergren J, Dahlstrand H. Prevalence of human papillomavirus (HPV) in oesophageal squamous cell carcinoma in relation to anatomical site of the tumour. PLoS One. 2012;7:e46538. doi: 10.1371/journal.pone.0046538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Herbster S, Ferraro CT, Koff NK, Rossini A, Kruel CD, Andreollo NA, Rapozo DC, Blanco TC, Faria PA, Santos PT, et al. HPV infection in Brazilian patients with esophageal squamous cell carcinoma: interpopulational differences, lack of correlation with surrogate markers and clinicopathological parameters. Cancer Lett. 2012;326:52–58. doi: 10.1016/j.canlet.2012.07.018. [DOI] [PubMed] [Google Scholar]
- 35.Dayyani F, Etzel CJ, Liu M, Ho CH, Lippman SM, Tsao AS. Meta-analysis of the impact of human papillomavirus (HPV) on cancer risk and overall survival in head and neck squamous cell carcinomas (HNSCC) Head Neck Oncol. 2010;2:15. doi: 10.1186/1758-3284-2-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Castillo A, Koriyama C, Higashi M, Anwar M, Bukhari MH, Carrascal E, Mancilla L, Okumura H, Matsumoto M, Sugihara K, et al. Human papillomavirus in upper digestive tract tumors from three countries. World J Gastroenterol. 2011;17:5295–5304. doi: 10.3748/wjg.v17.i48.5295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Michaelsen SH, Larsen CG, von Buchwald C. Human papillomavirus shows highly variable prevalence in esophageal squamous cell carcinoma and no significant correlation to p16INK4a overexpression: a systematic review. J Thorac Oncol. 2014;9:865–871. doi: 10.1097/JTO.0000000000000166. [DOI] [PubMed] [Google Scholar]
- 38.Syrjanen K. Geographic origin is a significant determinant of human papillomavirus prevalence in oesophageal squamous cell carcinoma: systematic review and meta-analysis. Scand J Infect Dis. 2013;45:1–18. doi: 10.3109/00365548.2012.702281. [DOI] [PubMed] [Google Scholar]
- 39.Ludmir EB, Stephens SJ, Palta M, Willett CG, Czito BG. Human papillomavirus tumor infection in esophageal squamous cell carcinoma. J Gastrointest Oncol. 2015;6:287–295. doi: 10.3978/j.issn.2078-6891.2015.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Cui SP, Wang HL, Peng W, Liu HJ, Hou L, Zhang B. Aberrant expression and correlative analysis of P16 in breast cancers. Beijing Da Xue Xue Bao. 2012;44:755–759. [PubMed] [Google Scholar]
- 41.Yuan J, Knorr J, Altmannsberger M, Goeckenjan G, Ahr A, Scharl A, Strebhardt K. Expression of p16 and lack of pRB in primary small cell lung cancer. J Pathol. 1999;189:358–362. doi: 10.1002/(SICI)1096-9896(199911)189:3<358::AID-PATH452>3.0.CO;2-1. [DOI] [PubMed] [Google Scholar]
- 42.Rayess H, Wang MB, Srivatsan ES. Cellular senescence and tumor suppressor gene p16. Int J Cancer. 2012;130:1715–1725. doi: 10.1002/ijc.27316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Romagosa C, Simonetti S, Lopez-Vicente L, Mazo A, Lleonart ME, Castellvi J, Ramon y Cajal S. p16(Ink4a) overexpression in cancer: a tumor suppressor gene associated with senescence and high-grade tumors. Oncogene. 2011;30:2087–2097. doi: 10.1038/onc.2010.614. [DOI] [PubMed] [Google Scholar]
- 44.Soussi T. The p53 pathway and human cancer. Br J Surg. 2005;92:1331–1332. doi: 10.1002/bjs.5177. [DOI] [PubMed] [Google Scholar]
- 45.Kastan MB, Onyekwere O, Sidransky D, Vogelstein B, Craig RW. Participation of p53 protein in the cellular response to DNA damage. Cancer Res. 1991;51:6304–6311. [PubMed] [Google Scholar]
- 46.Wang X, Simpson ER, Brown KA. p53: Protection against tumor growth beyond effects on cell cycle and apoptosis. Cancer Res. 2015;75:5001–5007. doi: 10.1158/0008-5472.CAN-15-0563. [DOI] [PubMed] [Google Scholar]
- 47.Baas IO, Mulder JW, Offerhaus GJ, Vogelstein B, Hamilton SR. An evaluation of six antibodies for immunohistochemistry of mutant p53 gene product in archival colorectal neoplasms. J Pathol. 1994;172:5–12. doi: 10.1002/path.1711720104. [DOI] [PubMed] [Google Scholar]
- 48.Xu XL, Zheng WH, Tao KY, Li XX, Xu WZ, Wang Y, Zhu SM, Mao WM. p53 is an independent prognostic factor in operable esophageal squamous cell carcinoma: a large-scale study with a long follow-up. Med Oncol. 2014;31:257. doi: 10.1007/s12032-014-0257-4. [DOI] [PubMed] [Google Scholar]
- 49.Bahnassy AA, Zekri AR, Abdallah S, El-Shehaby AM, Sherif GM. Human papillomavirus infection in Egyptian esophageal carcinoma: correlation with p53, p21, mdm2, C-erbB2 and impact on survival. Pathol Int. 2005;55:53–62. doi: 10.1111/j.1440-1827.2005.01804.x. [DOI] [PubMed] [Google Scholar]
- 50.Bosch FX, Ritter D, Enders C, Flechtenmacher C, Abel U, Dietz A, Hergenhahn M, Weidauer H. Head and neck tumor sites differ in prevalence and spectrum of p53 alterations but these have limited prognostic value. Int J Cancer. 2004;111:530–538. doi: 10.1002/ijc.11698. [DOI] [PubMed] [Google Scholar]
- 51.He D, Zhang DK, Lam KY, Ma L, Ngan HY, Liu SS, Tsao SW. Prevalence of HPV infection in esophageal squamous cell carcinoma in Chinese patients and its relationship to the p53 gene mutation. Int J Cancer. 1997;72:959–964. doi: 10.1002/(SICI)1097-0215(19970917)72:6<959::AID-IJC7>3.0.CO;2-O. [DOI] [PubMed] [Google Scholar]
- 52.Lam EW, Chan JY, Chan AB, Ng CS, Lo ST, Lam VS, Chan MM, Ngai CM, Vlantis AC, Ma RK, Chan PK. Prevalence, Clinicopathological Characteristics, and Outcome of Human Papillomavirus-Associated Oropharyngeal Cancer in Southern Chinese Patients. Cancer Epidemiol Biomarkers Prev. 2016;25:165–73. [DOI] [PubMed]
- 53.Jung AC, Briolat J, Millon R, de Reynies A, Rickman D, Thomas E, Abecassis J, Clavel C, Wasylyk B. Biological and clinical relevance of transcriptionally active human papillomavirus (HPV) infection in oropharynx squamous cell carcinoma. Int J Cancer. 2010;126:1882–1894. doi: 10.1002/ijc.24911. [DOI] [PubMed] [Google Scholar]
- 54.Schache AG, Liloglou T, Risk JM, Filia A, Jones TM, Sheard J, Woolgar JA, Helliwell TR, Triantafyllou A, Robinson M, et al. Evaluation of human papilloma virus diagnostic testing in oropharyngeal squamous cell carcinoma: sensitivity, specificity, and prognostic discrimination. Clin Cancer Res. 2011;17:6262–6271. doi: 10.1158/1078-0432.CCR-11-0388. [DOI] [PMC free article] [PubMed] [Google Scholar]


