Abstract
Introduction:
This study examined the effect of duration electronic cigarette (e-cigarette) use on e-cigarette dependence, frequency of use, and strength of nicotine solution as well as number of cigarettes smoked per day.
Methods:
Individuals were recruited at e-cigarette retail locations in a large Midwestern metropolitan city of the United States in July 2013. A total of 159 participants completed a brief 29-item self-report measure that assessed behaviors and perceptions of use. The mean age of the participants was 35.8 years; 84.4% were White, and 53.7% were male.
Results:
Increased duration of e-cigarette use was associated with fewer cigarettes smoked per day and differing patterns of dependence to e-cigarettes contingent upon smoking history. Additionally, increased duration of e-cigarette use was associated with increased frequency of use; however, this finding became nonsignificant when current tobacco cigarette use was accounted for, suggesting that individuals may increase e-cigarette use frequency as they decrease cigarette use. Overall, e-cigarette users tended to decrease the strength of nicotine in their e-cigarette products regardless of duration of use.
Conclusions:
Although preliminary in nature, this study identifies several factors that are important to consider when examining the effects of prolonged e-cigarette use. The implications of the current results should be informative to future studies that examine these variables in longitudinal designs.
Introduction
Sales, awareness, and public debate regarding electronic cigarette (e-cigarette) use have increased sharply and steadily since their advent in 2003 (Etter & Bullen, 2011; Herzog & Pokhrel, 2012; Pearson, Richardson, Niaura, Vallone, & Abrams, 2012; Wagener, Siegel, & Borrelli, 2012). E-cigarettes, which deliver nicotine through inhaled vapor, have been viewed as both a threat (Cobb & Abrams, 2012) and a potential benefit (Wagener et al., 2012) to public health. An examination of the evidence supporting these opposing views reveals several important lines of future research necessary to expand our understanding of these products.
To date, the literature includes several promising aspects of e-cigarettes. Large survey studies indicate that 67%–92% of e-cigarette users successfully reduce cigarette consumption and that 49%–96% are successful in quitting traditional cigarette use completely (Dawkins, Turner, & Crowe, 2013; Etter & Bullen, 2011; Siegel et al., 2012). Moreover, individuals who use e-cigarettes to quit smoking traditional cigarettes report improved breathing and decreased coughing (Dawkins et al., 2013). Clinical and crossover trials support these findings demonstrating that e-cigarettes appear to reduce craving for cigarettes and number of cigarettes smoked (Bullen et al., 2010; Vansickel, Cobb, Weaver, & Eissenberg, 2010); however, randomized clinical trials of smoking cessation demonstrate more modest effects (Polosa et al., 2011). Lastly, ex-smokers reported that their time to first daily cigarette (when they were active smokers) was significantly shorter than their time to first daily “vape” (use of e-cigarette), suggesting that e-cigarettes may be less addictive than traditional cigarettes (Dawkins et al., 2013).
Conversely, many potential concerns regarding e-cigarette use have been documented including data demonstrating that e-cigarettes may contain varying levels of toxins; from levels lower than that of traditional cigarettes (Cahn & Siegel, 2011; “FDA Warns of Health Risks Posed by E-Cigarettes,” 2009; Goniewicz et al., 2013; Laugesen, 2008), to levels equal to and exceeding those found in traditional cigarettes (Williams, Villarreal, Bozhilov, Lin, & Talbot, 2013). Furthermore, one study reported that individuals who used a state tobacco quitline and reported using or trying e-cigarettes in the past were significantly less likely to be tobacco abstinent at seven-month follow up than those who had never tried e-cigarettes (Vickerman, Carpenter, Altman, Nash, & Zbikowski, 2013). Several studies have also demonstrated that individuals often continue to use traditional cigarettes, albeit at a reduced level, after initiating e-cigarette use (e.g., Bullen et al., 2013; Caponnetto et al., 2013; Lee, Grana, Glantz, 2013; Popova & Ling, 2013; Vickerman et al., 2013). Lastly, there have been several unfortunate injuries related to e-cigarette use including e-cigarettes exploding as well as other safety issues surrounding the use of these products (e.g., Chen, 2013).
Despite some advancements made in researching e-cigarettes over the last several years, many questions remain. It is still unclear how the prolonged use of e-cigarettes influences important factors that could affect the users’ health, such as frequency of e-cigarette use and e-cigarette dependence. In fact, only one study to our knowledge has examined the effects of duration of e-cigarette use (Dawkins et al., 2013) and reporting on this variable was limited. Dawkins and colleagues (2013) reported that duration of e-cigarette use was significantly higher in current than ex-smokers, which suggests that dual use of both e-cigarettes and traditional cigarettes is the typical result of prolonged e-cigarette use. This is particularly noteworthy considering that approximately 76% of individuals in the same study reported the intention to use e-cigarettes as a complete alternative to smoking (Dawkins et al., 2013). In light of the substantial proliferation of e-cigarettes, the dearth of information regarding the long-term effects of their use on smoking behavior, nicotine dependence, and frequency of use is cause for concern.
Therefore, the purpose of this study was to examine the effects of duration of e-cigarette use on several factors including current cigarette use, dependence to e-cigarettes, frequency of e-cigarette use, and the strength of nicotine solution used in e-cigarettes. Previous studies suggest that e-cigarette users often reduce or quit smoking; therefore, we hypothesized that increased duration of e-cigarette use would be associated with decreased smoking. Considering the lack of information regarding dependence, changes in nicotine levels, and frequency of use, no a-priori hypotheses were made for these variables. Examining these associations will provide much needed preliminary data on the effects of long-term e-cigarette use and will be helpful in identifying important relationships to consider in longitudinal studies.
Methods
All measures and procedures were approved by the universities’ institutional review board. Individuals were recruited at e-cigarette retail locations often referred to as “vape stores/vape shops” in a large metropolitan city in the Midwestern United States. Customers were asked to participate in the study prior to exiting the retail store. The managers of all retail “vape stores” in the metropolitan area were contacted and asked to participate in serving as a data collection site for the study; 8 out of 10 stores contacted agreed to participate. Participants completed a brief (29-item) self-report measure assessing behaviors and perceptions regarding e-cigarette and traditional cigarette use as well as demographic information. Specifically, participants were asked to report the average number of cigarettes they smoked daily prior to initiating e-cigarette use as well as the average number of cigarettes they smoke currently. Past heavy and past light smoking groups were defined as ≥10 cigarettes daily or <9 cigarettes daily; a cutpoint previously used in several studies (Coady et al., 2012; Fagerström, Russ, Yu, Yunis, & Foulds, 2012; Kotz, Fidler, & West, 2012; Okuyemi et al., 2002). Current cigarette and e-cigarette dependence was measured via the Fagerström Test for Nicotine Dependence time to first cigarette (FTND TTFC) (Baker et al., 2007; Heatherton, Kozlowski, Frecker, & Fagerström, 1991), which assesses the time from waking until first daily cigarette or e-cigarette. Duration of e-cigarette use was measured in days of reported e-cigarette use. Frequency of e-cigarette use was measured by asking participants to estimate their daily number of “puffs.” A puff was defined as each time the participant inhaled from the e-cigarette. Strength of nicotine in milligrams (mg) was assessed retrospectively at initiation of e-cigarette use as well as currently at the time of data collection.
Participants
A sample of 159 current e-cigarette users was recruited. The majority of the sample (78.7%) reported using refillable “tank” systems. Participants had a mean age of 35.7 (SD = 12.6), the majority were male (53.7%), employed full-time (72.0%), and reported an average household income of $30,000–$39,999. The sample primarily identified as Caucasian (84.8%), followed by African American (3.7%), Hispanic (1.2%), Asian (0.6 %), American Indian/Alaskan Native (4.3%), and other (3.0%), and most participants had obtained a high school/GED or higher education level (93.9%). Prior to using e-cigarettes, participants reported smoking an average of 19.8 (SD = 12.8) tobacco cigarettes per day; after initiating e-cigarette use, participants reported smoking an average of 2.87 (SD = 5.53) tobacco cigarettes per day. The mean number of previous quit attempts was 4.05 (SD = 4.78), and the majority of participants utilized nicotine gum (64.3%) or a nicotine patch (61.3) to aid in their previous quit attempts (all percentages listed in Table 1). Average duration of e-cigarette use was 210 days or (6.8 months), with time to first daily use of e-cigarette ranging from 6 to 30min. Additional descriptives regarding demographics, traditional cigarette use, and e-cigarette use are reported in Table 1.
Table 1.
Participant Demographics
| Variable | M | SD | Frequency | % |
|---|---|---|---|---|
| Age | 35.7 | 12.6 | ||
| Duration of e-cigarette use (days) | 285 | 321.3 | ||
| Daily cigarettes prior to e-cigarette use | 19.8 | 12.9 | ||
| Daily cigarettes current | 2.87 | 5.53 | ||
| Lifetime quit attempts | 4.05 | 4.78 | ||
| Mean FTND TTFC e-cigarettes | 2.14 | .9 | ||
| Method of previous quit attempt | ||||
| Nicotine gum | 64.3 | |||
| Nicotine lozenge | 24.3 | |||
| Nicotine inhaler | 7.8 | |||
| Nicotine nasal spray | 2.6 | |||
| Nicotine patch | 61.3 | |||
| Chantix | 29.6 | |||
| Zyban | 16.5 | |||
| Gender | ||||
| Female | 88 | 56.1 | ||
| Male | 69 | 43.9 | ||
| Ethnicity | ||||
| White | 139 | 86.3 | ||
| Black | 6 | 3.7 | ||
| Hispanic | 2 | 1.2 | ||
| Asian | 1 | .6 | ||
| Native American | 7 | 4.3 | ||
| Other | 5 | 3.1 | ||
| Declined | 1 | .6 | ||
| Education | ||||
| Grade 9–11 | 10 | 6.3 | ||
| High school/GED | 40 | 25.0 | ||
| Technical school | 12 | 7.5 | ||
| Some college | 50 | 31.3 | ||
| College graduate | 38 | 23.8 | ||
| Graduate school | 10 | 6.3 | ||
| Employment | ||||
| Employed full-time | 118 | 74.7 | ||
| Employed part-time | 12 | 7.6 | ||
| Unemployed | 11 | 7.0 | ||
| Homemaker | 6 | 3.8 | ||
| Retired | 8 | 5.1 | ||
| Student | 3 | 1.9 | ||
FTND TTFC = Fagerström Test for Nicotine Dependence time to first cigarette.
Analytic Strategy
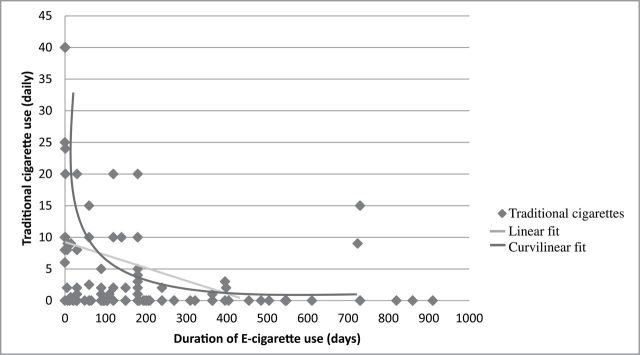
We conducted linear regression analyses to examine the effects of duration of e-cigarette use on current number of cigarettes smoked per day, dependence to e-cigarettes (FTND score), change in strength of nicotine (mg of nicotine), and estimated e-cigarette “puffs.” No issues with skewness or kurtosis were observed in the data. Visual examination of plotted residuals revealed linearity. Visual examination of the data for current number of cigarettes smoked per day by days of e-cigarettes use revealed a curvilinear rather than linear pattern. Therefore, post-hoc analyses of the curvilinear effects of traditional cigarette use were modeled using nonlinear regression to examine if this estimation provided a better fit of the data for this variable. Baron and Kenny’s (1986) moderation analysis was utilized to examine potential interactions between duration of use and smoking history. No issues with multicollinearity were observed, VIF = 1.04. Significant interactions were followed using analysis of simple slopes (Aiken & West, 1991). We also conducted repeated measures analysis of variance to examine change in nicotine level over time, and logistic regression to examine participants smoking status (i.e., ex-smoker vs. smoker). Linearity of the logit was assessed and confirmed via the Box–Tidwell approach. Measures of effect size (pr 2 for linear regression, η2 for repeated measures analysis of variance, and odds ratio for logistic regression) are listed for all analyses.
Results
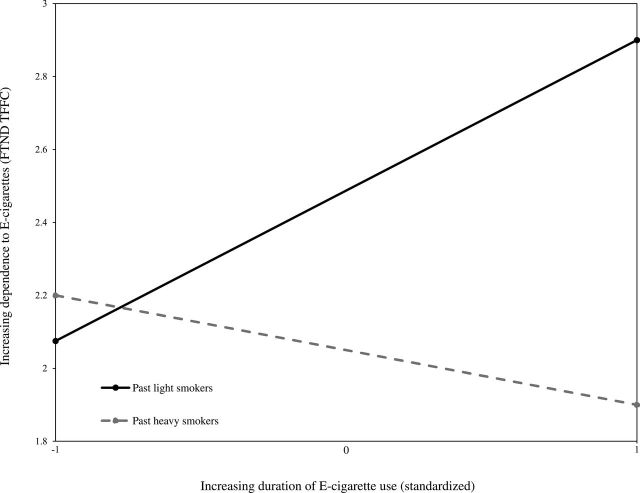
Nonlinear regression analysis revealed that increased duration of e-cigarette use was associated with fewer cigarettes currently smoked (F(1, 146) = 102.559, p < .001); the data were better characterized by an inverse curve than by a linear relationship (see Figure 1). Increased duration of e-cigarette use increased the likelihood of being an ex-smoker as compared to being a dual user of cigarettes and e-cigarettes (β = .003, SE = .001, Wald = 6.729, p = .012, odds ratio = 1.003). Duration of e-cigarette use was not associated with addiction to e-cigarettes as measured by the FTND TTFC (β = −.118, t[149] = −.145, p = .149, pr 2 = .118). However, when smoking history was considered, a significant interaction between past heavy smoking status (≥10 cigarettes/day) and past light smoking status (<9 cigarettes/day) suggested that these groups may evince different patterns of addiction to e-cigarettes over time (β = −.548, t[152] = −2.20, p = .029, pr 2 = .174). The pattern of the simple slope analysis for past heavy smokers suggested small decreases in dependence over time, while the pattern for past light smokers suggested small increases in dependence over time. However, neither slope was significantly different than zero, meaning that neither of the slopes represented significant change (see Figure 2). Duration of e-cigarette use did not predict change in the strength (mg of nicotine) of e-cigarettes used at initiation compared to strength of e-cigarettes currently used (β = −.058, t[106] = −.598, p = .551, pr 2 = .058), and no significant interaction between smoking history and duration of use was observed (β = .568, t[105] = 1.843, p = .07, pr 2 = .179). Overall, the reported strength of e-cigarettes decreased from initiation to current use, F(1, 108) = 32.686, p < .001, η2 = .232, and neither duration of use, F(1, 103) = .460, p = .499, η2 = .004, nor smoking history affected this change, F(1, 103) = .460, p = .760, η2 = .007. Conversely, duration of e-cigarette use was associated with estimated “puffs” on an e-cigarette per day, with increasing duration predicting more puffs (β = .186, t[120] = 2.068, p = .041, pr 2 = .186), again no interaction of smoking history and duration of use was observed (β = .159, t[120] = .666, p = .507, pr 2 = .060). However, when current traditional cigarette use was entered as a covariate, duration of e-cigarette use did not significantly predict puffs per day (β = .174, t[120] = 1.810, p = .073, pr 2 = .162).
Figure 1.
Traditional cigarettes smoked by duration of e-cigarette use.
Figure 2.
Interaction of smoking history and duration of e-cigarette use on dependence to e-cigarettes.
Discussion
This study examined duration of e-cigarette use in terms of several factors that may influence the health of the user, including current cigarette use, dependence to e-cigarettes, strength of nicotine used, and e-cigarette puffs per day. To our knowledge, this is the first study to focus directly on duration of e-cigarette use as a predictor of several tobacco-related outcomes.
Results revealed that reported daily consumption of traditional cigarettes decreased with increasing duration of e-cigarette use. Although this information is distinct from previous studies, it supports the notion that individuals are often able to reduce or quit cigarette use by using e-cigarettes (Dawkins et al., 2013; Etter & Bullen, 2011; Siegel et al., 2012). Furthermore, post-hoc analysis revealed that traditional cigarette use decreased with increasing duration of use in a pattern more consistent with an inverse curve rather than a linear relationship (see Figure 1). This suggests that individuals reduce cigarette use acutely after initiating e-cigarette use. It should be noted that reducing cigarette use alone may not be enough to prevent smoking-related illness; results from previous studies suggest that light and intermediate smokers still carry significantly increased risk for a host of negative health outcomes (Bjartveit & Tverdal, 2005; Schane, Ling, & Glantz, 2010). Our analyses also revealed that with increasing duration of e-cigarette use, the likelihood of being an ex-smoker (e-cigarette only user) increased modestly as compared to being a dual user of traditional cigarettes and e-cigarettes. Although the odds ratio for this finding was modest, the results contrast Dawkins and colleagues (2013) finding that current smokers (dual users) evinced a longer duration of e-cigarette use as compared to ex-smokers in their sample (Dawkins et al., 2013). The results reported by Dawkins and colleagues (2013) is a potentially troubling finding in that it suggests that dual use is more likely with increased duration of e-cigarette use. The current results suggest that there may be a period of time when individuals are transferring from traditional cigarettes to e-cigarettes. During this transition period, individuals use both products, but with continued use, eventually transfer to e-cigarette use only.
Overall, we observed no main effect between dependence to e-cigarettes and duration of e-cigarette use. However, past heavy smokers and past light smokers showed a significantly different pattern of dependence to e-cigarettes over time. Past heavy smokers demonstrated a pattern of slightly decreased dependence over time, while past light smokers demonstrated a pattern of slightly increased dependence over time. However, neither slope was significantly different from no change in dependence over time. The effect size for this interaction (pr 2 = .179) was medium by convention (Cohen, 1988). If this significant interaction is replicated in future studies and the slopes differ significantly from no change in dependence, treatment recommendations regarding e-cigarettes may differ for heavy versus light past smokers.
Additionally, we observed that duration of e-cigarette use did not predict change in the strength (mg of nicotine) of e-cigarettes used at initiation compared to strength of e-cigarette use currently reported. However, the reported strength of e-cigarettes did decrease from initiation to current use, regardless of duration of use or severity of smoking history. These findings suggest that individuals decrease the strength of nicotine in their e-cigarettes from initiation to current use, but that this change is not dependent on duration of use. That is, some individuals decreased nicotine strength very quickly, while others decreased strength after a longer period of e-cigarette use. It is important to note that previous studies have reported variations in levels of labeled nicotine concentrations (e.g., Goniewicz et al., 2013). Thus, the most meaningful information garnered from this result may be that individuals requested reduced nicotine concentrations in their nicotine liquid over time. Conversely, duration of e-cigarette use was associated with increased puffs on an e-cigarette per day, with increasing duration predicting more puffs, regardless of smoking history. However, individuals often report using both traditional cigarettes and e-cigarettes while transitioning to using e-cigarettes exclusively (Dawkins et al., 2013). The increase in e-cigarette puffs per day observed in the current results may be confounded by this transition. After controlling for number of cigarettes currently smoked daily, the finding was no longer significant. This suggests that individuals report more puffs per day as they decrease traditional cigarette use and increase e-cigarette use over time.
Although this study has potential to provide valuable information to the field, it must be considered in light of several noteworthy limitations. First, our data were collected at retail e-cigarette stores and included a sample of individuals who primarily used refillable “tank” systems. These results may differ from individuals using primarily disposable e-cigarettes or buying their products online or at alternative store fronts. Second, the design of the study was cross-sectional, precluding causal interpretations. Third, some of the current results relied on retrospective reporting of behaviors. Although this is standard practice for assessing smoking history, it can be problematic (Bernard, Killworth, Kronenfeld, & Sailer, 1984). Fourth, the current results are self-reported and therefore must be considered in light of the limitations associated with self-reported data (Schuler, Lechner, Malcolm, & Carter, 2009). A biologic marker such as cotinine would have been an ideal addition to the self-reported data. However, biologic specimens were not collected due to a lack of funds necessary to conduct the necessary analyses and concern that specimen collection would limit recruitment, especially because compensation was not provided for participation. Our interest in generalizability outweighed any reliability issues associated with unintentional or intentional errors in self-reported data. We believe the motivation for individuals to intentionally misrepresent self-reported data was low. Furthermore, we have no reason to believe that this motivation would differ systematically based on our main predictor (duration of e-cigarette use), which we believe limits any substantial confounding effects. Additionally, we conducted several statistical tests in this study, which increases the likelihood of type 1 error. Lastly, the results reported regarding a reduction in the nicotine concentration of nicotine liquid over time must be interpreted in light of findings that suggest that the nicotine concentration in nicotine liquid reported by retailers may fluctuate (e.g., Goniewicz, et al., 2013).
Future studies would improve upon this study by utilizing an experimental design. As mentioned previously, biologic markers of nicotine may increase the reliability of results. Additionally, the significant interaction of duration of use and past smoking status in terms of dependence to e-cigarettes should be tested in a longitudinal study. If the current results are replicated, treatment recommendation regarding e-cigarettes as a tool for quitting may differ for heavy versus light smokers. Lastly, there appears to be a trend for tank systems to outperform traditional e-cigarettes in a number of consumer preferences (Dawkins et al., 2013). Studies comparing these two forms of e-cigarettes in terms of the variables within this study will likely provide valuable information.
Funding
WL and AT were supported by the Oklahoma Tobacco Research Center during data collection. NT and LD were supported by NCI R21CA164521 to TW.
Declaration of Interests
None declared.
References
- Aiken L. S., West S. G. (1991). Multiple regression: Testing and interpreting interactions. Thousand Oaks, CA: Sage Publications. [Google Scholar]
- Baker T. B., Piper M. E., McCarthy D. E., Bolt D. M., Smith S. S., Kim S., Toll B. A. (2007). Time to first cigarette in the morning as an index of ability to quit smoking: Implications for nicotine dependence. Nicotine & Tobacco Research, 9(4), S555–S570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baron R. M., Kenny D. A. (1986). The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology, 51, 1173–1182. [DOI] [PubMed] [Google Scholar]
- Bernard R., Killworth P., Kronenfeld D., Sailer L. (1984). The problem of informant accuracy: The validity of retrospective data. Annual Review of Anthropology, 13, 495–517. [Google Scholar]
- Bjartveit K., Tverdal A. (2005). Health consequences of smoking 1-4 cigarettes per day. Tobacco Control, 14, 315–320. 10.1136/tc.2005.011932 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bullen C., Howe C., Laugesen M., McRobbie H., Parag V., Williman J., Walker N. (2013). Electronic cigarettes for smoking cessation: a randomised controlled trial. Lancet, 382(9905):1629––37. 10.1016/S0140-6736(13)61842-5 [DOI] [PubMed] [Google Scholar]
- Bullen C., Howe C., Lin R. B., Grigg M., Laugesen M., McRobbie H., Rodgers A. (2010). Pre-cessation nicotine replacement therapy: Pragmatic randomized trial. Addiction, 105, 1474–1483. 10.1111/j.1360-0443.2010.02989.x [DOI] [PubMed] [Google Scholar]
- Cahn Z., Siegel M. (2011). Electronic cigarettes as a harm reduction strategy for tobacco control: A step forward or a repeat of past mistakes? Journal of Public Health Policy, 32, 16–31. jphp201041 [pii]10.1057/jphp.2010.41 [DOI] [PubMed] [Google Scholar]
- Caponnetto P., Campagna D., Cibella F., Morjaria J. B., Caruso M., Russo C., Polosa R. (2013). EffiCiency and Safety of an eLectronic cigAreTte (ECLAT) as tobacco cigarettes substitute: a prospective 12-month randomized control design study. PLoS One, 24;8 (6):e66317. doi: 10.1371/journal.pone.0066317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen I. L. (2013). FDA Summary of Adverse Events on Electronic Cigarettes. Nicotine Tob Res 15(2): 615–616. [DOI] [PubMed] [Google Scholar]
- Coady M. H., Jasek J., Davis K., Kerker B., Kilgore E. A., Perl S. B. (2012). Changes in smoking prevalence and number of cigarettes smoked per day following the implementation of a comprehensive tobacco control plan in New York City. Journal of Urban Health, 89, 802–808. 10.1007/s11524-012-9683-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cobb N. K., Abrams D. B. (2012). Commentary on Wagener etal. (2012): Laissez-faire regulation: Turning back the clock on the Food and Drug Administration and public health. Addiction, 107, 1552–1554. 10.1111/j.1360-0443.2012.03927.x [DOI] [PubMed] [Google Scholar]
- Cohen J. (1988). Statistical power analysis for the behavioral sciences (2nd ed.). Hillsdale, NJ: Erlbaum. [Google Scholar]
- Dawkins L., Turner J., Crowe E. (2013). Nicotine derived from the electronic cigarette improves time-based prospective memory in abstinent smokers. Psychopharmacology, 227, 377–384. 10.1007/s00213-013-2983-2 [DOI] [PubMed] [Google Scholar]
- Etter J. F., Bullen C. (2011). Electronic cigarette: Users profile, utilization, satisfaction and perceived efficacy. Addiction, 106, 2017–2028. 10.1111/j.1360-0443.2011.03505.x [DOI] [PubMed] [Google Scholar]
- Fagerström K., Russ C., Yu C. R., Yunis C., Foulds J. (2012). The Fagerström Test for Nicotine Dependence as a predictor of smoking abstinence: A pooled analysis of varenicline clinical trial data. Nicotine & Tobacco Research, 14, 1467–1473. [DOI] [PubMed] [Google Scholar]
- U. S. F. a. D. Administration. (2009). FDA warns of health risks posed by e-cigarettes. FDA Consumer Health Information. [Google Scholar]
- Goniewicz M. L., Knysak J., Gawron M., Kosmider L., Sobczak A., Kurek J., Benowitz N. (2013). Levels of selected carcinogens and toxicants in vapour from electronic cigarettes. Tobacco Control, 23, 133–139. 10.1136/tobaccocontrol-2012–050859 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heatherton T. F., Kozlowski L. T., Frecker R. C., Fagerström K.-O. (1991). The Fagerström Test for Nicotine Dependence: A revision of the Fagerström Tolerance Questionnaire. British Journal of Addiction, 86, 1119–1127. [DOI] [PubMed] [Google Scholar]
- Herzog T. A., Pokhrel P. (2012). Ethnic differences in smoking rate, nicotine dependence, and cessation-related variables among adult smokers in Hawaii. Journal of Community Health, 37, 1226–1233. 10.1007/s10900-012-9558-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kotz D., Fidler J., West R. (2012). Very low rate and light smokers: Smoking patterns and cessation-related behaviour in England, 2006–11. Addiction, 107, 995–1002. 10.1111/j.1360-0443.2011.03739.x [DOI] [PubMed] [Google Scholar]
- Laugesen M. (2008). Safety report on the Ruyan e-cigarette cartridge and inhaled aerosol. Christchurch, New Zealand: Health New Zealand Ltd. [Google Scholar]
- Lee S., Grana R. A., Glantz S. A. (2013). Electronic Cigarette Use Among Korean Adolescents: A Cross-Sectional Study of Market Penetration, Dual Use, and Relationship to Quit Attempts and Former Smoking. J Adolesc Health. 2013 Nov 22. pii: S1054-139X(13)00748-9. doi: 10.1016/j.jadohealth.2013.11.003 [DOI] [PMC free article] [PubMed]
- Okuyemi K. S., Harris K. J., Scheibmeir M., Choi W. S., Powell J., Ahluwalia J. S. (2002). Light smokers: Issues and recommendations. Nicotine & Tobacco Research, 4(2), S103–S112. 10.1080/1462220021000032726 [DOI] [PubMed] [Google Scholar]
- Pearson J. L., Richardson A., Niaura R. S., Vallone D. M., Abrams D. B. (2012). e-Cigarette awareness, use, and harm perceptions in US adults. American Journal of Public Health, 102, 1758–1766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polosa R., Caponnetto P., Morjaria J. B., Papale G., Campagna D., Russo C. (2011). Effect of an electronic nicotine delivery device (e-Cigarette) on smoking reduction and cessation: A prospective 6-month pilot study. BMC Public Health, 11, 786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Popova L., Ling P. M. (2013). Alternative tobacco product use and smok-ing cessation: a national study. Am J Public Health, 103(5):923–30. doi: 10.2105/AJPH.2012.301070 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schane R. E., Ling P. M., Glantz S.A. (2010). Health effects of light and intermittent smoking. Circulation, 121, 1518–1522. 10.1161/CIRCULATIONAHA.109.904235 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schuler M., Lechner W. V., Malcolm R. J., Carter R. (2009). Temporal and demographic trends in concordance of urine drug screens and self-reported use in cocaine treatment studies. Journal of Addiction Medicine, 3, 211–217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siegel A. B., Conner K., Wang S., Jacobson J. S., Hershman D. L., Hidalgo R. , … Neugut A. I. (2012). Smoking and hepatocellular carcinoma mortality. Experimental & Therapeutic Medicine, 3, 124–128. 10.3892/etm.2011.351 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vansickel A. R., Cobb C. O., Weaver M. F., Eissenberg T. E. (2010). A clinical laboratory model for evaluating the acute effects of electronic “cigarettes”: Nicotine delivery profile and cardiovascular and subjective effects. Cancer Epidemiology, Biomarkers & Prevention, 19, 1945–1953. 1055–9965.EPI-10–0288 [pii] 10.1158/1055–9965.EPI-10–0288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vickerman K. A., Carpenter K. M., Altman T., Nash C. M., Zbikowski S. M. (2013). Use of electronic cigarettes among state tobacco cessation quitline callers. Nicotine & Tobacco Research, 15, 1787–1791. 10.1093/ntr/ntt061 [DOI] [PubMed] [Google Scholar]
- Wagener T. L., Siegel M., Borrelli B. (2012). Electronic cigarettes: Achieving a balanced perspective. Addiction, 107, 1545–1548. 10.1111/j.1360-0443.2012.03826.x [DOI] [PubMed] [Google Scholar]
- Williams M., Villarreal A., Bozhilov K., Lin S., Talbot P. (2013). Metal and silicate particles including nanoparticles are present in electronic cigarette cartomizer fluid and aerosol. PLoS ONE, 8, e57987. 10.1371/journal.pone.0057987 [DOI] [PMC free article] [PubMed] [Google Scholar]