Abstract
Objective
The objective of the current study was to examine the feasibility of telemedicine vs. telephone for the delivery of a multidisciplinary weekly family based behavioral group intervention to treat pediatric obesity delivered to families living in rural areas using a randomized controlled trial methodology.
Methods
103 rural children and their families were recruited. Feasibility measures included participant satisfaction, session attendance and retention. Treatment outcome measures included child BMIz, Parent BMI, 24-hour dietary recalls, accelerometer data, Child Behavior Checklist and the Behavioral Pediatrics Feeding Assessment Scale.
Results
Participants were highly satisfied with the intervention both via telemedicine and via telephone. Completion rates were much higher than for other pediatric obesity intervention programs, and both methodologies were highly feasible. There were no differences in telemedicine and telephone groups on primary outcomes.
Conclusion
Both telemedicine and telephone intervention appear to be feasible and acceptable methods of delivering pediatric obesity treatment to rural children.
Keywords: obesity, randomized controlled trial, weight management
Introduction
The prevalence and incidence of obesity in the United States remain a significant public health concern. Data from the National Health and Nutrition Examination Survey (NHANES) from 2009 to 2010 indicate that 16.9% of US children and adolescents are classified as obese (BMI ≥ 95th percentile of the BMI-for-age growth charts) and 31.8% of youth are either overweight or obese (BMI ≥ 85th percentile).1 These prevalence rates are particularly alarming given that pediatric obesity confers significant risk on the current and future health of children.2, 3
As a result, there has been an increasing emphasis on the treatment of pediatric obesity. One well-established treatment model recommended for the treatment of pediatric obesity and overweight is family-based, behavioral group programs.4 These programs have been developed in an attempt to promote healthy weight and alter the trajectory of weight gain, especially among overweight youth. They focus on parents and families as agents and models of behavior change and target improvements in diet, physical activity, and sedentary behavior.5, 6 Although these programs have been effective at improving health outcomes among urban and suburban youth, few programs have been developed for rural youth, and rates of pediatric obesity among this underserved group are disproportionately high.
Rural youth face unique barriers to healthy living7, 8 and our own analyses indicate they have higher rates of pediatric obesity.9 Some of these barriers include lack of nutrition education, poor access to nutritionists and other healthcare providers, limited resources, and fewer opportunities for physical exercise contribute to a higher rate of obesity in this population compared to their urban counterparts.10 Therefore, obesity treatment programs for obesity are needed which specifically target rural youth and address factors which are unique to this group.
Interventions targeting pediatric obesity specifically among rural children are generally sparse. Some studies have been published on medical/clinical rural obesity services delivered by primary care physicians or other medical providers11, 12 or on the perspectives of rural healthcare providers who are faced with the pediatric obesity epidemic.13 Therefore, a major weakness of the current obesity literature is a lack of focus on treatment outcome among rural children.
To address this need, our team has conducted a line of research assessing the effectiveness of the use of telemedicine (i.e. interactive synchronous video telemedicine) in delivering family based behavioral groups to rural families for the treatment of pediatric obesity.14, 15 Although telemedicine is an extremely common method of providing distance learning in rural areas, there are still some communities that do not have this technology, or find its use cost prohibitive, leaving a portion of rural children and their families with no access to these services. However, all schools in the state of Kansas do have access to a telephone, making this technology widely available. There are no studies, however, comparing telemedicine to telephone in terms of effectiveness, satisfaction or feasibility of treatment delivery, and only our own studies focus on the use of telemedicine for the delivery of group programs, rather than individual treatment.
Therefore, the objective of the current study was to examine the feasibility of telemedicine vs. telephone for the delivery of a multidisciplinary weekly family based behavioral group intervention to treat pediatric obesity delivered to families living in rural areas using a randomized controlled trial methodology. We also examined treatment effects on child BMIz, nutrition, physical activity and quality of life indicators.
Methods
School recruitment
Recruitment flyers were sent to all rural elementary schools in the state of Kansas. Interested schools contacted researchers via a toll free number and their eligibility for the rural status was confirmed (city and/or county with a population of < 20,000). The qualified schools identified an on-site representative for the project, who completed training in Human Subjects Research, Conflict of Interest, and HIPAA. The first eleven schools to complete these steps were recruited for the study and randomly assigned to telemedicine or telephone. Schools were provided with measurement equipment (scales, stadiometers) specifically for this project (see Measures). Randomization occurred at the school level, such that all participants from each school were assigned to a single modality. Randomization was completed by the statistician using a random numbers table. All study procedures were approved by the relevant Institutional Review Board.
Training of on-site representatives
After being recruited, each school identified an on-site representative to be the lead of the study at that particular school. These staff members were typically a nurse, gym teacher, or computer teacher. They received project specific training regarding recruitment, consent, and intervention procedures. They were also given an intervention manual and all necessary forms, and were trained regarding the anthropometric measurement protocol, including calibration techniques and the importance of taking measurements in triplicate.
Recruitment of participants
Each school then sent recruitment letters home to their elementary students. Recruitment letters were sent home with children by school personnel to determine which families were interested in participation, and interested families signed consent forms and completed baseline measures. Inclusion criteria were: children with BMI of > 85th for age/gender, family living in a rural area (city and/or county population < 20,000), child attending a school with phone and Internet capabilities, and the family having access to a phone. Exclusion criteria were family moving to a non-rural area, child having physical limitation or receiving an injury which significantly limited physical mobility, child having a significant medical issue, or child and parents having significant developmental delay or cognitive impairment that was known to the school. No children who met the inclusion criteria had to be excluded.
The intervention
Groups were scheduled according to the convenience of the participating families and the on-site school representative (typically in the evenings). Each group session had specific objectives outlined in a treatment manual and began with a short introduction and review of weekly goals and progress led by both the offsite leader and the on-site school representative. Then, the off-site leader (a clinician member of the research team) met with the parents via the randomized modality (telemedicine, telephone), and simultaneously the on-site school representative met with the children in the next room to cover their manualized topics. All group meetings lasted approximately one hour. The parent and child groups covered the same topics, but the parent group was more didactic and the child group more activity based.
The intervention was based upon cognitive behavioral theory and was family based, covering behavioral, nutrition and physical activity topics. The existing intervention15 was tailored to better meet the needs of rural families based upon previous qualitative work7 and has been studied previously.14 The intervention consists of eight weekly meetings followed by six monthly meetings, for a total intervention period of eight months, which was designed to coincide with a typical school year. Topics included Goal Setting, Stop-Light Diet,16 Sedentary Activity, Praising and Ignoring, Calorie Counting, Portion Size, Self-Esteem, and dressing tips for the large body types, among others (see Table 1 for a list of topics by session).
Table 1.
Session topics.
| Session Number | Topics |
|---|---|
| 1 | Overview of Program and Expectations; Goal Setting |
| 2 | Use of Goal Charts; Reinforcement and Incentives |
| 3 | Stop Light Diet & Nutrition Recommendations |
| 4 | Screen Time & Sedentary Activity; The Importance of Tracking; Activity Monitor Results |
| 5 | Praising & Ignoring: Role Play & Homework |
| 6 | Diet Recall Results; Calorie Counting; Healthy Substitutions |
| 7 | Portion Sizes: Lesson, Demonstration & Quiz |
| 8 | Self-Esteem; Dressing for Larger Body Sizes; Adult Modeling: What I Like About Myself |
| 9 | Reading Food Labels & Vitamins/Minerals |
| 10 | The Concept of Nutrient Density |
| 11 | Potlucks, BBQs, and Other Events: How To Be Smart |
| 12 | Exercising as a Family |
| 13 | The Application of Energy Balance |
| 14 | The Use of Privileges & Maintenance |
Modality 1: Phone
Parents and children sat around a speakerphone to communicate with the research team for all group meetings. If the school did not have an adequate speakerphone, one was provided to them.
Modality 2: Telemedicine
Telemedicine (or interactive synchronous video telemedicine) allows for real time communication of audio and video. Parents and children sat around a large TV screen to communicate in real time with the research team for all group meetings. All schools were already outfitted with this technology due to their involvement with a state wide distance learning program, which is common in rural areas/states.
Measures
All measures were completed just prior to the start of the intervention (baseline) and immediately following the eight-month intervention (post-intervention), with the exception of demographics, which were only collected at baseline. Also, child BMIz and parent BMI were collected at the eight-week time point in addition to baseline and eight months. Demographic information was self-report and included the target child’s birth date, gender, grade level, and ethnicity as well as maternal and paternal age, marital status, education, occupation, and income level.
Feasibility measures
Several measures of feasibility were collected, including attendance/retention, and satisfaction (via a paper and pencil measure). For satisfaction, five items were on a scale of 1 (low) and 10 (high) and covered satisfaction with different aspects of the program. One items was yes/no (overall, do you think this project helped your child to be healthier), and three items were open ended.
Child BMIz
Height and weight were measured by school nurses via a Harpenden Holtain stadiometer, Model 603 (Holtain, Crymych, UK) and a portable SECA digital scale (SECA, Hamburg, Germany). Height and weight were calculated as the average of three independent measurements and used (along with age and gender) to determine BMIz, which was used for primary outcome based upon previous similar research,17, 18 and BMI percentile for children (which was used for educational purposes) based on the Center for Disease Control’s growth charts.19
Parent BMI
Parent height and weight were measured on identical equipment using standardized procedures as mentioned above at both baseline and eight months. Parent Body Mass Index was calculated based upon the standard CDC formula.19
24-hour dietary recall
The 24-hour diet recall is a standardized three-pass method, developed by the US Department of Agriculture for use in national dietary surveillance. This measure has been shown to be a valid and reliable representation of a child’s overall diet.20 Dietary recall data were gathered over the phone by trained Master’s and PhD level researchers who were deemed reliable in diet recall procedures by a registered dietician. Prior to the phone call, parents were asked to sit with their child and write down information regarding their child’s food intake regarding two weekdays and one weekend day at each time point. All dietary data were analyzed using NDSR software version 2005 developed by the Nutrition Coordinating Center, University of Minnesota, Minneapolis, MN, USA. Daily intake of calories, percent calories from fat, fruit and vegetable servings, sugar-sweetened beverage servings, and servings of “red” foods [foods with more than 12 grams of sugar and/or 7 grams of fat16] were assessed.
Accelerometers
The ActiGraph (Actigraph LLC, Pensacola, FL) is a small, light-weight device worn on an adjustable belt over the non-dominant hip that measures physical activity duration and intensity. The ActiGraph has been shown to provide valid assessments of physical activity for adults and children during daily-living activities.21 Participants were asked to wear the activity monitor for at least six hours a day for a minimum of three days during a one-week period. All data were run through Santech MeterPlus software, which accounts for age and gender cut-offs when determining moderate or vigorous activity. [For specific cut-offs, see22.] Data are reported as average minutes of moderate to vigorous activity per day.
Child behavior checklist (CBCL)
Previous data have indicated that children with overweight/obesity are more likely to have psychological issues.23 As the current study examined two modalities with the same intervention, we were interested in comparing outcomes on a measure of global behavioral issues, such as the Child Behavior Checklist (CBCL). The CBCL24 is a standardized measure that assesses parental report of child competencies and behavioral or emotional problems. Values for total score, internalizing behavior, and externalizing behavior were assessed.
Behavioral pediatrics feeding assessment scale
Previous data indicate that children with overweight/obesity have higher rates of mealtime behavior problems,25 such as those measured by the Behavioral Pediatrics Feeding Assessment Scale (BPFAS). As the current study compared a behavioral intervention delivered via telemedicine or telephone, we were interested in comparing outcomes on a measure of mealtime behavior problems, such as the BPFAS. The measure is composed of 35 items: 25 describe the child’s feeding behavior and 10 describe parent’s feelings about or strategies for dealing with eating problems. Parents are also asked to rate on a scale from 1–5 how much they agree or disagree with each statement, as well as whether or not each of the 35 items are a problem. Thus, the measure results in a child frequency score, child problem score, parent frequency score and parent problem score. Higher scores are suggestive of more problematic feeding behaviors. Previous research has shown the BPFAS to be a valid and reliable representation of a child’s and parent’s mealtime behavior.26
Obesity related quality of life
Obesity related related quality of life was assessed via child self-report (Sizing Me Up, SMU) and parent-proxy report (Sizing Them Up, STU). Both measures were composed of 22 items each, used a 4-point Liker scale, and have acceptable reliability and validity in previous studies.27, 28
Results
Overview of analyses
Group comparison analyses were planned a priori and conducted by an independent statistician. To assess differences in primary outcome (BMIz) between intervention groups, the adjusted two sample t-test was used. This statistical analysis is consistent with recommendations for the analysis of cluster randomization trials in health research29. To assess changes in anthropometric outcomes (child BMIz, parent BMI) by group from pre- to post-intervention, adjusted t-test for matched pairs was used. Results are presented as Mean (Standard Deviation) unless otherwise indicated.
Participants
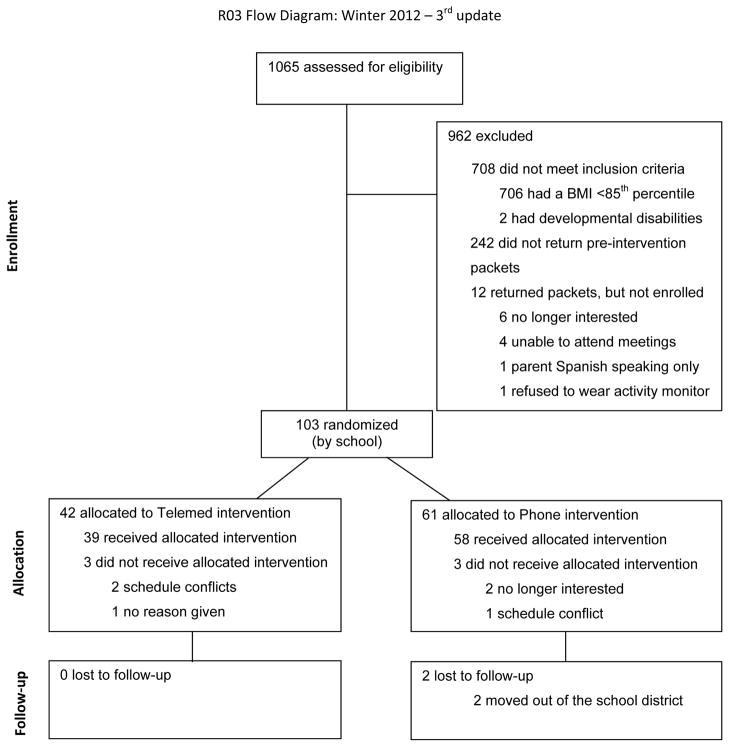
Approximately 1065 children attended the 11 elementary schools in the current project. Of these, 708 were not overweight or obese, 242 did not return interest forms, or 12 returned incomplete packets. Of the 103 participants who qualified for the study, 42 attended a school assigned to telemedicine and 61 attended a school assigned to telephone (see CONSORT diagram in Figure 1). Participant characteristics are shown in Table 2. There were no significant differences across groups at baseline on any demographic factors or outcome measures. The children ranged in age from 5 to 12 years (M = 9.14, SD = 1.86) and most of the participants were Caucasian (88.24%), consistent with the region from which they were drawn. Overall, 46 participants were male (44.66%) and approximately one-third (40.2%) of the children were eligible for free or reduced lunch. At study entry, children had a mean BMIz of 1.73 (SD = .46) and a mean BMI percentile of 94.30 (SD = 4.43) with 57.28% (n = 59) of the sample falling in the overweight (85th ≤ BMI percentile ≤95th) category and 42.72% (n = 44) in the obese (BMI percentile ≥ 95th) category. Parents/caregivers had a baseline mean BMI of 31.81 (SD = 7.33) with 10.67% falling in the overweight category (n = 11) and 42.72% falling in the obese category (n = 44).
Figure 1.
CONSORT diagram.
Table 2.
Demographics of randomized sample.
| Variable | Full Sample (N = 103) | Telemedicine (n = 42) | Telephone (n = 61) |
|---|---|---|---|
| Age in years M (SD) | 9.14 (1.86) | 9.39 (1.70) | 8.97 (1.96) |
| % Male (N)* | 44.66 (46) | 40.48 (17) | 47.54 (29) |
| % Caucasian (N)* | 88.24 (90) | 92.68 (38) | 85.25 (52) |
| Eligible for free/reduced lunch (N)* | 40.20 (41) | 33.33 (14) | 45.00 (27) |
| Child BMIz M (SD) | 1.73 (0.46) | 1.66 (0.39) | 1.78 (0.50) |
| Child BMI%ile M (SD) | 94.30 (4.43) | 94.02 (4.12) | 94.49 (4.66) |
| Parent BMI M (SD) | 31.81 (7.33) | 33.43 (6.63) | 30.88 (7.62) |
Note. No differences were statistically significant at baseline.
Column percentage
Feasibility measures
Satisfaction
Satisfaction was rated on a 10-point scale with 10 being highest. There were no significant group differences in level of satisfaction following completion of treatment. Mean satisfaction score for the overall intervention at post-treatment was 7.77 (1.58) for the telephone group and 8.33 (1.63) for the telemedicine group. Regarding whether they found the program helpful in facilitating the improved health in their child, 95.74% of participating parents in the telephone group responded “yes” and 93.55% of the parents in the telemedicine group responded “yes.” Across both groups, parents were extremely satisfied with the group leaders (M = 8.93, SD = 1.55), with the handouts (M = 8.63, SD = 1.39), with the topics covered (M = 8.31, SD = 1.74) and with the degree of feedback they received during the program (M = 8.13, SD = 1.81). When asked what parts of the program helped the most, some representative quotes include “(He is) more aware… being active and has a better understanding of why we don’t let him have lots of candy and sugary/fatty snacks and foods” and “keeping track of what he ate, going through and seeing how much exercise it would take to burn off calories.” When asked what parts of the project they liked the most, they consistently stated the activity monitors (“liked the activity monitors”), the dietary tracking devices suggested (“resources for tracking dietary habits”), and the group meetings (“getting together with others with the same problem”). When asked what could be done to improve the program, parents had many ideas, including increased contact (“continue with the kids maybe once a month or once a quarter during school”), and increased content on certain topics (“give more recipes”). Interestingly, several parents in the telephone group wrote spontaneous comments requesting at least one face-to-face meeting (“have real person instead of phone call”; “video conferencing or at least 1 personal visit”; “have a real person instead of a call”, “make at least one face-to-face visit to make the program more meaningful” and “I think for my kids anyway it would have worked better if it wasn’t all done on the phone.”)
Attendance
The overall attendance rate for the sample was 89.40%. No significant differences in attendance or sessions completed were found. Participants in the telephone group completed 88.41% of sessions and participants in the telemedicine group completed 90.82% of sessions.
BMI/z, diet, and physical activity measures
Data on child BMIz indicated no significant differences by group from pre-treatment to immediate post-treatment (8-week; t =.91, p> .05) and from pre-treatment to post-treatment (8-month; t = −.13, p> .05; Table 3). For parent BMI, data indicated no significant differences in change in parent BMI by group from pre-treatment to immediate post-treatment (8-week; t = −.47, p> .05) and from pre-treatment to post-treatment (8-month; t = −1.81, p> .05; Table 3). Results from adjusted two-sample t-tests indicate no significant differences in groups by time (p > .05) for any diet or nutrition variables (Table 4) or for physical activity (t = 2.28, p = 0.05; Table 4).
Table 3.
Changes in child BMIz.
| Child BMIz |
|||
|---|---|---|---|
| Pre M (SD) |
BMIz M Δ at 8 weeks |
BMIz M Δ at 8 months* |
|
| Telemedicine Group | 1.68 (0.39) | −.01 (0.16) | .00 (.22) |
| Telephone Group | 1.77 (0.51) | −.07 (.19) | .00 (.18) |
change from pre to 8 months.
Table 4.
Child diet and physical activity change by group over time.
| Telemedicine Group |
Telephone Group |
|||
|---|---|---|---|---|
| Pre M (SD) |
Post M (SD) |
Pre M (SD) |
Post M (SD) |
|
| Dietary Behaviors/day | ||||
| Kilocalories | 1871.79 (394.29) | 1777.67 (362.46) | 1802.63 (354.98) | 1726.10 (370.82) |
| Fruit and Vegetable Servings | 3.52 (1.37) | 3.98 (1.39) | 3.63 (1.64) | 3.47 (1.34) |
| Sugar Sweetened Beverage Servings | 1.18 (1.20) | 1.23 (1.43) | 1.26 (0.92) | 1.50 (1.02) |
| Physical Activity Behaviors | ||||
| Minutes of M/V* Activity | 69.79 (54.93) | 61.87 (39.38) | 81.62 (53.37) | 62.88 (43.27) |
Note.
M/V = moderate to vigorous. Only children with pre and post measures were included.
Psychological, feeding and quality of life measures
There were no group by time changes from pre-treatment post-treatment for the Child Behavior Checklist, the Behavioral Pediatrics Feeding Assessment Scale, or the two measures of quality of life (Sizing Me Up and Sizing Them Up; Table 4).
Discussion
The objective of the current study was to examine the feasibility of telemedicine vs. telephone for the delivery of a multidisciplinary weekly family based behavioral group intervention to treat pediatric obesity delivered to families living in rural areas using a randomized controlled trial methodology. Results overwhelmingly indicate that both modalities were feasible for the delivery of family based behavioral group treatment to rural areas. Satisfaction was extremely high and approximately equivalent across both modalities. Parents were positive about all aspects of the program, especially their group leaders. Open ended questions did reveal that many parents in the telephone group desired some face-to-face contact and felt that it would likely improve outcomes for their children. In terms of attrition, another of our measures of feasibility, there was slightly higher attrition in the telephone group compared to the telemedicine group, but in general, attrition from both groups was extremely low. Attrition in prior pediatric weight-management interventions has ranged from 0–42% at six months post baseline and at 12–52% at 12 months.30 Our low attrition rates (10%) could be attributed to the fact that our intervention was designed to be accessible and convenient for a rural population who often has poor access to health related resources.10 Even so, it is remarkable that an intervention that is only slightly effective with lowering child BMI had such low attrition, which clearly speaks to the high need for treatment programs in these rural communities. This fits with the observations of our team members, who all reported that families were extremely grateful to be receiving such an extensive treatment program at such a convenient location. Similar to prior studies utilizing telemedicine for pediatric weight management,15, 31 no significant technological problems were noted in the telemedicine or the telephone groups.
Regarding outcome measures, there were no statistically significant differences between the two groups on any of the outcome measures. This suggests that there were no differences between the two modalities (telemedicine and telephone) on these measures. This is important because although a great number of schools have access to interactive synchronous video telemedicine equipment, there are still a significant proportion of schools that do not have access to this technology. Because the current study demonstrated that the two methodologies are approximately equivalent, future intervention dissemination efforts can use both technologies when trying to reach children in rural areas.
For both modalities, our results indicate that mean child BMIz decreased slightly (but not significantly) during active treatment (from baseline to eight weeks) and that baseline levels were maintained at eight months. These are small but meaningful changes, as research indicates that children slowing of weight gain, weight maintenance, and/or weight loss should all be considered “successful” outcomes in pediatric weight management.32
It is interesting to note that parents were obese (BMI≥30) at baseline, despite the fact that only child BMI percentile was an inclusion criteria. These findings corroborate previous research which indicates that parents of obese children are often obese themselves.33–36 Prior research indicates that interventions with an emphasis on parent and/or family involvement are effective for treating pediatric overweight/obesity,30, 37 and may be more effective than programs that target the child alone.37 Parents serve as important role models for health behaviors for their children38–40 and parent weight-loss has been shown to predict child weight loss in family-based interventions.41, 42
Regarding dietary outcome, our results indicated that overall number of kilocalories decreased in both intervention groups by about 100 kilocalories per day. This degree of calorie deficit is equivalent to approximately one pound per month of weight loss. Also of note, children were exceeding national recommendations (USDA) for 30% of calories from fat both before and after the interventions. These results are unsurprising as data indicate that for most American children approximately 30% of total energy intake comes from foods with high levels of fat and sugar.43 Children were consuming over 6 red foods per day at baseline, and this only decreased slightly post intervention. The traditional Stop Light Diet recommends no more than 4 red foods per week.16 Although the average number of red foods decreased in both groups on average between baseline and follow-up, the average number of sugar sweetened beverages increased in both groups. Prior research has indicated a connection between daily servings of sugar sweetened beverages and BMI, particularly in girls.44–46 Children were also far below the national recommendation of five servings of fruits and vegetables a day both before and after the interventions.47 Although several of our nutrition related behaviors trended in the expected direction, results clearly indicate the need for more effective intervention components related to nutrition behavior change that would enable participants to meet the national nutritional guidelines.
Our results regarding physical activity indicated that the child participants were quite active on average both pre- and post-intervention. Children in both groups met the national recommendation of 60 minutes of moderate to vigorous physical activity at all time points.48 Considering that prior research has indicated that only 42% of children age 6–11 meet the recommendations for 60 minutes of moderate to vigorous physical activity,22 the children in our study were quite active.
Results from the CBCL indicate that children were psychologically healthy at baseline in both groups, and remained psychologically healthy at post, with no significant differences in outcomes by group. CBCL scores obtained in the current study were lower (more healthy) than those obtained from other studies of urban and suburban children with higher degrees of obesity.49, 50 Overall, prior research has indicated that children who are obese are significantly more likely than typical weight peers to have psychosocial problems, such as low self-esteem, depression, body dissatisfaction, loss-of-control eating, dissatisfaction, and decreased health-related quality of life.51 Thus, future research should assess why findings between rural and urban overweight and obese children seem to differ with regard to child psychopathology.
Results from the BPFAS, which is designed to assess mealtime behaviors, indicate that the children and parents in both groups did demonstrate some mealtime behavior difficulties at baseline, and that these problems decreased slightly in both intervention groups, suggesting that our interventions may improve mealtime behaviors in this population. Prospective studies have indicated that problematic eating behaviors early in life may be a risk factor for overweight and obesity in childhood.25, 52 One cross-sectional study found that parents of overweight and obese children are more likely to report problematic mealtime behaviors than parents of children with a normal weight.53 Overall, there is a lack of research investigating mealtime behaviors in children with overweight/obesity using measures that have been validated for use with this population.
Results for quality of life indicated that our sample had high (healthy) quality of life at baseline, and that this value remained high at post. This was true for both parent reported and child self-reported of quality of life. Previous research on these measures with treatment seeking overweight and obese pediatric populations indicates scores ranging from the mid- 50’s to the mid 70’s on the 5 subscales across both the parent report and child report forms.54 For the current study, however, our mean scores were primarily in the 80’s for both parent and child report, indicating that rural status may somehow protect weight-related quality of life among treatment seeking overweight and obese youth. However, a relatively recent study assessing the reliability and the validity of Sizing Me Up (the child self-report measure) with a community based non-treatment seeking sample found scores very similar to our own.55
The clinical implications of this study are many. First, for rural families facing the issue of pediatric obesity, both the telemedicine and telephone methods appear to be feasible for the delivery of empirically supported interventions. Both of these intervention modalities are highly scalable and would allow for the treatment of a large number of families without the inconveniences of travel time or cost – an important clinical implication. Families from rural areas who commit to this type of intervention are likely to show up for treatment, be satisfied with the treatment, and to encounter few technical difficulties. Children who participate are also likely to improve at least some of their health behaviors and to maintain their body mass, as are parents (which argues for including them in the intervention program). However, data also clearly indicate that the rural intervention needs to be improved if it is going to result in meaningful body mass changes for children. Potential strategies to do this could include increased monitoring accountability between the family and the group leader. In our face-to-face programs with urban children56 we spend a great deal of time reviewing monitoring forms kept by the families each week. However, doing this remotely proved to be a challenge.
Limitations
This study does have several limitations. First, our sample was relatively small, a common problem encountered in rural studies. All participants were from rural areas in only one state, so our findings may not generalize to rural areas in other states. Related to this, our sample was predominantly Caucasian, but this was reflective of the population from which the sample was drawn and therefore expected. Also, some of our measures (CBCL, BPFAS) were not obesity specific, which would likely have strengthened our study.
Conclusion
In summary, the current study addresses the key health issue of pediatric obesity among an underserved rural population, examining the effectiveness of family-based behavioral groups delivered via telemedicine or telephone. Results indicate no statistically significant differences between modality (telemedicine/telephone) and also suggest trends toward desirable changes in anthropometrics and health behaviors. The fact that our families achieved body weight/mass maintenance is important to note, as successful treatment of pediatric obesity is not necessarily measured only in terms of weight loss. Also, our high satisfaction ratings and notably low attrition indicates that a group-based, remotely-administered health behavior intervention – as opposed to individual, in-person sessions, which have limited feasibility for rural populations – allowed families to feel sufficiently “connected” that they remained committed to our eight-month program, representing an important opportunity for enhanced dissemination of similar programs. Future research will need to examine these findings with larger and more diverse samples, and to determine specific methods to increase treatment effects. Current national data indicate that 83% of all homes have Internet57 and that 58% of children ages 3 to 17 use the Internet at home58 making a home based telemedicine intervention program particularly interesting for addressing these limitations.
Acknowledgments
Funding: The authors wish to acknowledge funding from the National Institutes of Health (NIDDK 081016).
We also wish to thank all of the wonderful families who participated, and the rural schools who were excellent partners in this important work.
References
- 1.Ogden CL, Carroll MD, Kit BK, et al. Prevalence of obesity and trends in body mass index among US children and adolescents, 1999–2010. JAMA. 2012;307:483–90. doi: 10.1001/jama.2012.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Daniels SR. The consequences of childhood overweight and obesity. Future Child. 2006;16:47–67. doi: 10.1353/foc.2006.0004. [DOI] [PubMed] [Google Scholar]
- 3.Dietz WH. Health consequences of obesity in youth: childhood predictors of adult disease. Pediatrics. 1998;101:518–25. [PubMed] [Google Scholar]
- 4.Barlow SE. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics. 2007;120(Suppl 4):S164–92. doi: 10.1542/peds.2007-2329C. [DOI] [PubMed] [Google Scholar]
- 5.Epstein LH, Paluch RA, Roemmich JN, et al. Family-based obesity treatment, then and now: twenty-five years of pediatric obesity treatment. Health Psychol. 2007;26:381–91. doi: 10.1037/0278-6133.26.4.381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jelalian E, Saelens BE. Empirically supported treatments in pediatric psychology: pediatric obesity. J Pediatr Psychol. 1999;24:223–48. doi: 10.1093/jpepsy/24.3.223. [DOI] [PubMed] [Google Scholar]
- 7.Davis AM, James RL, Curtis MR, et al. Pediatric obesity attitudes, services, and information among rural parents: a qualitative study. Obesity. 2008;16:2133–40. doi: 10.1038/oby.2008.312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.McMurray RG, Harrell JS, Bangdiwala SI, Deng S. Cardiovascular disease risk factors and obesity of rural and urban elementary school children. J Rural Health. 1999;15:365–74. doi: 10.1111/j.1748-0361.1999.tb00760.x. [DOI] [PubMed] [Google Scholar]
- 9.Davis AM, Bennett KJ, Befort C, et al. Obesity and related health behaviors among urban and rural children in the United States: data from the National Health And Nutrition Examination Survey 2003–2004 and 2005–2006. J Pediatr Psychol. 2011;36:669–76. doi: 10.1093/jpepsy/jsq117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tai-Seale T, Chandler C. Rural Healthy People 2010: A companion document to Healthy People 2010. College Station, TX: The Texas A & M University System Health Science Center, School of Rural Public Health, Southwest Rural Health Research Center; 2003. Nutrition and Overweight Concerns in Rural Areas: A Literature Review. [Google Scholar]
- 11.Irby MB, Boles KA, Jordan C, et al. TeleFIT: adapting a multidisciplinary, tertiary-care pediatric obesity clinic to rural populations. Telemed J E Health. 2012;18:247–9. doi: 10.1089/tmj.2011.0117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shaikh U, Nettiksimmons J, Romano P. Pediatric obesity management in rural clinics in California and the role of telehealth in distance education. J Rural Health. 2011;27:263–9. doi: 10.1111/j.1748-0361.2010.00335.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Steele RG, Wu YP, Jensen CD, Pankey S, Davis AM, Aylward BS. School nurses’ perceived barriers to discussing weight with children and their families: a qualitative approach. J Sch Health. 2011;81:128–37. doi: 10.1111/j.1746-1561.2010.00571.x. [DOI] [PubMed] [Google Scholar]
- 14.Gallagher KS, Davis AM, Malone B, et al. Treating rural pediatric obesity through telemedicine: baseline data from a randomized controlled trial. J Pediatr Psychol. 2011;36:687–95. doi: 10.1093/jpepsy/jsr011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Davis AM, James RL, Boles RE, et al. The use of TeleMedicine in the treatment of paediatric obesity: feasibility and acceptability. Maternal & child nutrition. 2011;7:71–9. doi: 10.1111/j.1740-8709.2010.00248.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Epstein L, Squires S. The stoplight diet for children. New York, NY: Little Brown & Co; 1988. [Google Scholar]
- 17.Janicke DM, Sallinen BJ, Perri MG, et al. Comparison of parent-only vs family-based interventions for overweight children in underserved rural settings: outcomes from project STORY. Arch Pediatr Adolesc Med. 2008;162:1119–25. doi: 10.1001/archpedi.162.12.1119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Steele RG, Aylward BS, Jensen CD, et al. Comparison of a family-based group intervention for youths with obesity to a brief individual family intervention: a practical clinical trial of positively fit. J Pediatr Psychol. 2012;37:53–63. doi: 10.1093/jpepsy/jsr057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Centers for Disease Control and Prevention. [accessed 20 May 2014];CDC growth charts. 2010 http://www.cdc.gov/growthcharts.
- 20.Crawford PB, Obarzanek E, Morrison J, et al. Comparative advantage of 3-day food records over 24-hour recall and 5-day food frequency validated by observation of 9- and 10-year-old girls. J Am Diet Assoc. 1994;94:626–30. doi: 10.1016/0002-8223(94)90158-9. [DOI] [PubMed] [Google Scholar]
- 21.Sirard JR, Melanson EL, Li L, et al. Field evaluation of the Computer Science and Applications, Inc. physical activity monitor. Med Sci Sports Exerc. 2000;32:695–700. doi: 10.1097/00005768-200003000-00022. [DOI] [PubMed] [Google Scholar]
- 22.Troiano RP, Berrigan D, Dodd KW, et al. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. 2008;40:181–8. doi: 10.1249/mss.0b013e31815a51b3. [DOI] [PubMed] [Google Scholar]
- 23.Phillips BA, Gaudette S, McCracken A, et al. Psychosocial functioning in children and adolescents with extreme obesity. J Clin Psychol Med Settings. 2012;19:277–84. doi: 10.1007/s10880-011-9293-9. [DOI] [PubMed] [Google Scholar]
- 24.Achenbach TM. Manual for the Child Behavior Checklist/4–18 and 1991 Profile. Burlington, VT: University of Vermont, Dept. of Psychiatry; 1991. p. 288. [Google Scholar]
- 25.Faith MS, Hittner JB. Infant temperament and eating style predict change in standardized weight status and obesity risk at 6 years of age. Int J Obes. 2010;34:1515–23. doi: 10.1038/ijo.2010.156. [DOI] [PubMed] [Google Scholar]
- 26.Crist W, Dobbelsteyn C, Brousseau AM, et al. Pediatric assessment scale for severe feeding problems: validity and reliability of a new scale for tube-fed children. Nutr Clin Pract. 2004;19:403–8. doi: 10.1177/0115426504019004403. [DOI] [PubMed] [Google Scholar]
- 27.Herzer M, Zeller MH, Rausch JR, et al. Perceived social support and its association with obesity-specific health-related quality of life. J Dev Behav Pediatr. 2011;32:188–95. doi: 10.1097/DBP.0b013e318208f576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Modi AC, Zeller MH. Psychosocial factors related to obesity in children and adolescents. In: Jelalian E, Steele JR, editors. Handbook of Child and Adolescent Obesity. New York, NY: Springer Science + Business Media; 2008. pp. 25–42. [Google Scholar]
- 29.Donner A, Klar N. Design and Analysis of Cluster Randomization Trials in Health Research. London, England: Arnold; 2000. p. 178. [Google Scholar]
- 30.Oude Luttikhuis H, Baur L, Jansen H, et al. Interventions for treating obesity in children. The Cochrane database of systematic reviews. 2009:CD001872. doi: 10.1002/14651858.CD001872.pub2. [DOI] [PubMed] [Google Scholar]
- 31.Davis AM, Sampilo M, Gallagher KS, et al. Treating Rural Pediatric Obesity Through Telemedicine: Outcomes From a Small Randomized Controlled Trial. J Pediatr Psychol. 2013 doi: 10.1093/jpepsy/jst005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lipana LS, Bindal D, Nettiksimmons J, et al. Telemedicine and Face-to-Face Care for Pediatric Obesity. Telemed J E Health. 2013;19:806–8. doi: 10.1089/tmj.2012.0292. [DOI] [PubMed] [Google Scholar]
- 33.Silventoinen K, Rokholm B, Kaprio J, et al. The genetic and environmental influences on childhood obesity: a systematic review of twin and adoption studies. Int J Obes. 2010;34:29–40. doi: 10.1038/ijo.2009.177. [DOI] [PubMed] [Google Scholar]
- 34.Whitaker RC, Wright JA, Pepe MS, et al. Predicting obesity in young adulthood from childhood and parental obesity. N Engl J Med. 1997;337:869–73. doi: 10.1056/NEJM199709253371301. [DOI] [PubMed] [Google Scholar]
- 35.Davis MM, McGonagle K, Schoeni RF, et al. Grandparental and parental obesity influences on childhood overweight: implications for primary care practice. J Am Board Fam Med. 2008;21:549–54. doi: 10.3122/jabfm.2008.06.070140. [DOI] [PubMed] [Google Scholar]
- 36.Price RA, Reed DR, Guido NJ. Resemblance for body mass index in families of obese African American and European American women. Obes Res. 2000;8:360–6. doi: 10.1038/oby.2000.43. [DOI] [PubMed] [Google Scholar]
- 37.McGovern L, Johnson JN, Paulo R, et al. Clinical review: treatment of pediatric obesity: a systematic review and meta-analysis of randomized trials. J Clin Endocrinol Metab. 2008;93:4600–5. doi: 10.1210/jc.2006-2409. [DOI] [PubMed] [Google Scholar]
- 38.Birch LL, Davison KK. Family environmental factors influencing the developing behavioral controls of food intake and childhood overweight. Pediatr Clin North Am. 2001;48:893–907. doi: 10.1016/s0031-3955(05)70347-3. [DOI] [PubMed] [Google Scholar]
- 39.Wrotniak BH, Epstein LH, Paluch RA, et al. The relationship between parent and child self-reported adherence and weight loss. Obes Res. 2005;13:1089–96. doi: 10.1038/oby.2005.127. [DOI] [PubMed] [Google Scholar]
- 40.Ventura AK, Birch LL. Does parenting affect children’s eating and weight status? Int J Behav Nutr Phys Act. 2008;5:15. doi: 10.1186/1479-5868-5-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wrotniak BH, Epstein LH, Paluch RA, et al. Parent weight change as a predictor of child weight change in family-based behavioral obesity treatment. Arch Pediatr Adolesc Med. 2004;158:342–7. doi: 10.1001/archpedi.158.4.342. [DOI] [PubMed] [Google Scholar]
- 42.Boutelle KN, Cafri G, Crow SJ. Parent predictors of child weight change in family based behavioral obesity treatment. Obesity. 2012;20:1539–43. doi: 10.1038/oby.2012.48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Slining MM, Mathias KC, Popkin BM. Trends in Food and Beverage Sources among US Children and Adolescents: 1989–2010. Journal of the Academy of Nutrition and Dietetics. 2013 doi: 10.1016/j.jand.2013.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ludwig DS, Peterson KE, Gortmaker SL. Relation between consumption of sugar-sweetened drinks and childhood obesity: a prospective, observational analysis. Lancet. 2001;357:505–8. doi: 10.1016/S0140-6736(00)04041-1. [DOI] [PubMed] [Google Scholar]
- 45.Berkey CS, Rockett HR, Field AE, et al. Sugar-added beverages and adolescent weight change. Obes Res. 2004;12:778–88. doi: 10.1038/oby.2004.94. [DOI] [PubMed] [Google Scholar]
- 46.Phillips SM, Bandini LG, Naumova EN, et al. Energy-dense snack food intake in adolescence: longitudinal relationship to weight and fatness. Obes Res. 2004;12:461–72. doi: 10.1038/oby.2004.52. [DOI] [PubMed] [Google Scholar]
- 47.Office of Disease Prevention and Health Promotion. [accessed 20 May 2014];Dietary Guidelines for Americans. 2010 http://www.health.gov/dietaryguidelines.
- 48.Office of Disease Prevention and Health Promotion. [accessed 20 May 2014];Physical Activity Guidelines for Americans. 2008 http://www.health.gov/paguidelines.
- 49.Vila G, Zipper E, Dabbas M, et al. Mental disorders in obese children and adolescents. Psychosom Med. 2004;66:387–94. doi: 10.1097/01.psy.0000126201.12813.eb. [DOI] [PubMed] [Google Scholar]
- 50.Korsten-Reck U, Korsten K, Haeberle K, et al. The psychosocial situation of obese children: Psychological factors and quality of life. Psychol Res Behav Manag. 2009;2:23–9. [PMC free article] [PubMed] [Google Scholar]
- 51.Vander Wal JS, Mitchell ER. Psychological complications of pediatric obesity. Pediatr Clin North Am. 2011;58:1393–401. x. doi: 10.1016/j.pcl.2011.09.008. [DOI] [PubMed] [Google Scholar]
- 52.Agras WS, Hammer LD, McNicholas F, et al. Risk factors for childhood overweight: a prospective study from birth to 9.5 years. J Pediatr. 2004;145:20–5. doi: 10.1016/j.jpeds.2004.03.023. [DOI] [PubMed] [Google Scholar]
- 53.Zeller MH, Reiter-Purtill J, Modi AC, et al. Controlled study of critical parent and family factors in the obesigenic environment. Obesity. 2007;15:126–36. doi: 10.1038/oby.2007.517. [DOI] [PubMed] [Google Scholar]
- 54.Zeller MH, Modi AC. Development and initial validation of an obesity-specific quality-of-life measure for children: sizing me up. Obesity. 2009;17:1171–7. doi: 10.1038/oby.2009.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Cushing CC, Steele RG. Psychometric properties of sizing me up in a community sample of 4th and 5th grade students with overweight and obesity. J Pediatr Psychol. 2012;37:1012–22. doi: 10.1093/jpepsy/jss075. [DOI] [PubMed] [Google Scholar]
- 56.Davis AM, Daldalian MC, Mayfield CA, et al. Outcomes from an Urban Pediatric Obesity Program Targeting Minority Youth: The Healthy Hawks Program. Child Obes. 2013;9:492–500. doi: 10.1089/chi.2013.0053. [DOI] [PubMed] [Google Scholar]
- 57.Leichtman Research Group. [accessed 20 May 2014];Broadband access and services in the home. 2013 http://www.leichtmanresearch.com/research/bband.html.
- 58.Child Trends. [accessed 20 May 2014];Home computer access and Internet use. 2012 http://www.childtrends.org/?indicators=home-computer-access.