Abstract
Objective
A dissociative subtype of posttraumatic stress disorder (PTSD) was recently added to the Diagnostic and Statistical Manual-5 (American Psychiatric Association, 2013) and is thought to be associated with poor PTSD treatment response.
Method
We used latent growth curve modeling to examine data from a randomized controlled trial of Prolonged Exposure and Present-Centered Therapy for PTSD in a sample of 284 female veterans and active duty service members with PTSD to test the association between the dissociative subtype and treatment response.
Results
Individuals with the dissociative subtype (defined using latent profile analysis) had a flatter slope (p = .008) compared to those with high PTSD symptoms and no dissociation such that the former group showed, on average, a 9.75 (95% CI = -16.94 to -2.57) lesser decrease in PTSD severity scores on the Clinician Administered PTSD Scale (Blake et al., 1995) over the course of the trial. However, this effect was small in magnitude. Dissociative symptoms decreased markedly among those with the subtype, though neither treatment explicitly addressed such symptoms. There were no differences as a function of treatment type.
Conclusions
Results raise doubt about the common clinical perception that exposure therapy is not effective or appropriate for individuals who have PTSD and dissociation and provide empirical support for the use of exposure treatment for individuals with the dissociative subtype of PTSD.
Public Health Significance
. This study found that female veterans and active duty service members with the dissociative subtype of posttraumatic stress disorder (PTSD) did not respond as well to PTSD treatment with Prolonged Exposure or Present-Centered Therapy as did those without the subtype. However, both PTSD and dissociation symptoms did improve markedly in the dissociative group, suggesting that the dissociative subtype is not a contraindication for the use of empirically supported treatments for PTSD.
Keywords: Dissociative subtype, PTSD, latent growth curve, treatment response
The Influence of the Dissociative Subtype of Posttraumatic Stress Disorder on Treatment Efficacy in Female Veterans and Active Duty Service Members
The dissociative subtype (DS) of posttraumatic stress disorder (PTSD) was newly added to the 5th edition of the Diagnostic and Statistical Manual (DSM-5, American Psychiatric Association [APA], 2013) and is defined as meeting full criteria for PTSD and showing comorbid “persistent or recurrent” symptoms of derealization (i.e., experiencing the world as unreal or dreamlike) and/or depersonalization (i.e., feeling as if one's physical body is disconnected from the self). Psychometric research, primarily using latent profile analysis (LPA), has provided consistent evidence across populations that approximately 15-30% of those with PTSD manifest the DS (e.g., Armour, Elklit, Lauterbach, & Elhai, 2014; Stein et al., 2013; Steuwe et al., 2012; Wolf, Lunney et al., 2012; Wolf, Miller et al., 2012).
The inclusion of the DS in the DSM may yield new insight into the pathophysiology and treatment of PTSD. Dissociation is thought to negatively influence the efficacy of exposure-based PTSD therapies (Lanius et al., 2010), such as Prolonged Exposure (PE), because it may prevent activation of the fear network (i.e., processing of trauma-related emotions; van Minnen, Harned, Zoellner, & Mills, 2012). Further, research suggests that clinicians consider dissociation a contraindication for exposure therapy for PTSD (Becker, Zayfert, & Anderson, 2004). Despite this, no studies have found that dissociation negatively influences response to exposure therapy (Hagenaars, van Minnen, & Hoogduin, 2010; Halvorsen, Stenmark, Neuner, & Nordahl, 2014; Price, Kearns, Houry, & Rothbaum, 2014).
Dissociation is also thought to impair the ability to generate, attend to, and retain restructured trauma-related cognitions (a key component of cognitive therapies for PTSD) and to limit access to trauma-related memories (necessary for narrative therapies). But, to date, the data support only subtle effects of dissociation on response to cognitive and narrative therapies. Specifically, Resick, Suvak, Johnides, Mitchell, and Iverson (2012) reported no overall effect of dissociation on PTSD symptom decline in response to Cognitive Processing Therapy (CPT), however, individuals with high levels of dissociation undergoing the full course of CPT showed faster PTSD symptom improvement relative to those undergoing only cognitive therapy (CPT-C). Similarly, Cloitre, Petkova, Wang, and Lu (2012) reported no overall effect of baseline dissociation on change in PTSD in a randomized controlled trial of Skills Training in Affective and Interpersonal Regulation (STAIR) and Narrative Story Telling (NST). However, participants with high post-treatment dissociation who completed the combined STAIR/NST arm showed greater PTSD symptom decline at 3 and 6-month follow-ups than did individuals with high post-treatment dissociation in the other treatment conditions. In both Resick et al. and Clotire et al., the differences that emerged in PTSD response were within the groups with relatively high levels of dissociation and not between those with high versus low levels of dissociation.
Aims and Hypotheses
The primary aim of this study was to examine if the DS was associated with differential PTSD symptom response to treatment in a sample of female service members and Veterans. A second aim was to evaluate how dissociative symptoms changed among those with the DS in response to PTSD treatment. We evaluated these aims in a dataset that we have previously employed to test the latent structure of dissociation and PTSD. Specifically, using data from a large, randomized clinical trial of PE versus Present-Centered Therapy (PCT) for the treatment of PTSD among military women (reference masked for review), we previously conducted LPAs of the 17 DSM-IV (APA, 1994) PTSD symptoms and four items indexing derealization and depersonalization, as measured at the baseline assessment (reference masked for review). Approximately 30% of the sample was assigned to the dissociative class. To extend this, we retained class assignment (the moderate PTSD, high PTSD, or high PTSD and high dissociation groups) as a predictor of PTSD symptoms and symptom change using latent growth curve modeling. We hypothesized that the DS would be associated with poorer response to treatment as defined by less PTSD symptom improvement relative to the moderate and high PTSD groups and that dissociative symptoms would improve among those with the DS.
Method
Participants and Measures
Participants were 284 female veterans (n = 277) and active-duty service members (n = 7) with PTSD who participated in a multi-site (n = 12) randomized clinical trial of PE for PTSD (reference masked for review). Mean age of participants was 44.79 (SD = 9.44, range 22–78). Almost half (45.4%, n = 129) self-identified as a non-White minority. The majority of the sample had been exposed to sexual assault (93.0%). Data were available from 235 participants at immediate post-treatment, 232 participants at 3-month follow-up and from 229 participants at six-month follow-up. Participants were not removed from the study if they missed an assessment. PTSD was assessed using the Clinician-Administered PTSD Scale (CAPS; Blake et al., 1995). Dissociation was measured using four self-report derealization and depersonalization items from the Dissociation scale of the Trauma Symptom Inventory (Briere, 1995).1
Procedure
Institutional review boards approved the protocol. A master's- or doctoral-level assessor, blinded to condition, performed assessments before and after treatment and at 3- and 6-month follow-ups. All sessions were videotaped and reviewed by supervisors who provided weekly phone supervision; group calls with master supervisors were employed to maintain treatment fidelity. Participants were randomly assigned to 10 weekly 90-minute sessions of PE (n = 141) or PCT (n = 143). PE included psychoeducation, imaginal exposure, homework, and discussion of thoughts and feelings related to exposures. PCT focused on current life problems as manifestations of PTSD and on general daily difficulties, accomplishments made during therapy, and future plans. There were no significant trauma or demographic differences among the treatment groups and no site or therapist treatment effects (reference masked for review).
Data Analyses
We created two dummy-coded variables to reflect LPA class assignment with the dissociative class as the reference group (Moderate PTSD versus the High PTSD and Dissociative class; High PTSD versus the High PTSD and Dissociative class) and specified them as predictors of the latent intercept and slope factors in a latent growth curve model. As the shape of change over time was not a focus of this research and because we did not expect the shape of change to be equivalent across all time points, we fixed the first and last slope loadings (baseline and Month 6) and freely estimated those for Months 0 and 3. To obtain estimated means at Months 0 and 3, we fixed the baseline and Month 0 (and, separately, the baseline and Month 3) slope loadings in follow-up analyses. We also examined treatment type X class as a predictor of the slope and intercept factors. Analyses were conducted separately for the CAPS scores and the derealization/depersonalization item means. We examined if the groups differed in terms of loss of PTSD diagnosis over time using logistic regression and in the amount of treatment received as a function of class (and class X treatment type) using chi-square and ANOVAs. For all analyses, we compared the dissociative class to the moderate and high PTSD classes, though the primary comparison of interest was that between the dissociative and the high PTSD classes because differences between these groups can be attributed to dissociation. In contrast, the dissociative class differed from the moderate PTSD group on both dissociation and PTSD severity, making it impossible to determine the source of treatment trajectory differences. Latent variable analyses were conducted in Mplus 7.0 (Muthén & Muthén, 2012) using maximum likelihood estimation. Missing data were modeled directly (maximum amount of missingness was 20.1%).
Results
Descriptive statistics for each class at each time point as a function of treatment type are listed in Table 1. An initial latent growth curve model which included treatment type by class interaction terms as predictors of the intercept and slope factors fit the data well, χ2 (13, n = 284) = 10.33, p = .67, RMSEA < .001, 90% CI for RMSEA: < .001 = .05, CFI = 1.0, TLI = 1.01, SRMR = .02, but revealed no significant interactions between treatment type and class (smallest p = .29). Therefore, growth models collapsed across treatment type.
Table 1. Observed Mean CAPS Severity Scores (and SDs) by Group and Treatment Type at Each Assessment.
| Class | Baseline | Month 0 | Month 3 | Month 6 | ||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| PCT | PE | PCT | PE | PCT | PE | PCT | PE | |
|
| ||||||||
| M (SD) | ||||||||
| Moderate PTSD | 64.75 (9.20) | 64.44 (10.06) | 51.25 (19.69) | 36.72 (25.16) | 47.59 (20.61) | 37.00 (23.03) | 45.63 (23.01) | 36.91 (22.88) |
| High PTSD | 91.03 (12.00) | 89.21 (9.00) | 64.26 (25.27) | 67.93 (27.26) | 62.33 (27.38) | 60.90 (27.70) | 61.06 (27.53) | 63.57 (28.11) |
| High PTSD & Dissociation | 83.98 (15.29) | 86.21 (17.65) | 70.62 (23.53) | 66.83 (27.72) | 65.25 (25.62) | 65.69 (26.47) | 65.00 (30.13) | 64.40 (29.49) |
Note. PCT = Present-Centered Therapy; PE = Prolonged Exposure; PTSD = posttraumatic stress disorder; M = mean; SD = standard deviation.
The second model, which included the effects of group membership on the slope and intercept factors, yielded a good fitting model, χ2 (7, n = 284) = 3.78, p = .80, RMSEA < .001, 90% CI for RMSEA: < .001 = .05, CFI = 1.0, TLI = 1.01, SRMR = .01, with the moderate and high PTSD groups, relative to the dissociative group, predicting the latent intercept. The high PTSD group's baseline CAPS score was, on average, 5.05 points greater than that of the dissociative class, 95% CI [1.29, 8.81], p = .009, and the moderate PTSD group's baseline CAPS score was, on average, 20.49 points below that of the dissociative class, 95% CI [-23.89, -17.10], p < .001. There was also an effect of the high PTSD class (versus the dissociative class) on the slope factor: on average, CAPS scores decreased 9.75 points more from the first to the last assessments in the high PTSD class relative to the dissociative class, 95% CI [-16.94, -2.57], p = .008 (see Figure 1).2 There was no slope effect comparing the moderate PTSD group to the dissociative one (unstandardized [unst] γ = -3.69, p = .26) nor was the baseline CAPS score associated with the rate of change (unst γ = 24.74, p = .76). The mean baseline CAPS score for the High PTSD and Dissociative class was estimated as 85.09, 95% CI [82.49, 87.69], p < .001, and the mean rate of change for this group from the first to last assessment was -18.71, 95% CI [-23.75, -13.68,] p < .001. The residual variance for the slope was significant (p < .001), suggesting variables other than class assignment contributed to individual differences in rate of change; residual variance in the intercept was not significant (p = .08).
Figure 1.
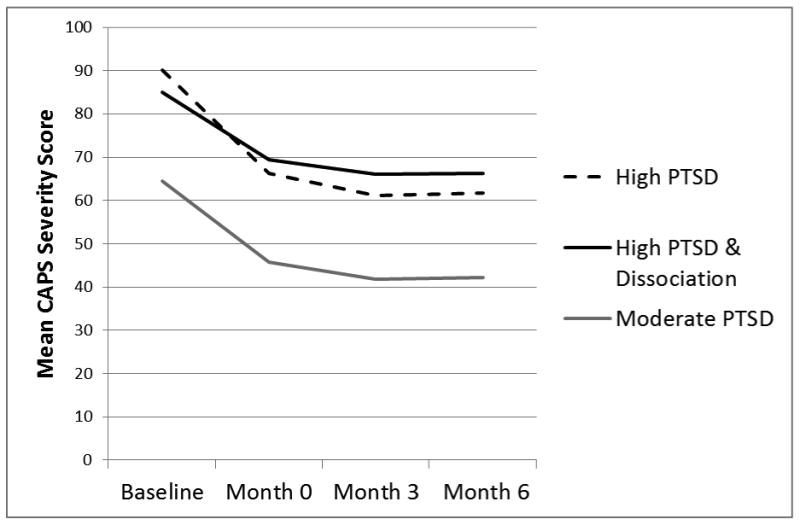
The figure shows the estimated mean CAPS severity scores at pre-treatment and follow-up assessments as a function of class assignment. PTSD = posttraumatic stress disorder; CAPS = Clinician Administered PTSD Scale.
Logistic regressions revealed an omnibus significant group difference in the percentage of women who no longer met criteria for PTSD at any post-treatment assessment, χ2 (2, n = 235) = 18.19, p = .0001 (see Table 2). However, follow-up pairwise testing showed that this was due to differences between the moderate versus the high PTSD group, χ2 (1, n = 235) = 10.34, p = .0013, and versus the dissociative group, χ2 (1, n = 235) = 12.20, p = .0005. There were no differences between the dissociative and high PTSD classes, Wald χ2 (1, n = 235) = 0.02, p = .89. This pattern held at both 3- and 6-months. There were no differences in the number of completed treatment sessions as a function of group membership (moderate PTSD group: M = 7.91, SD = 3.53; high PTSD group: M = 8.50, SD = 2.94; dissociative group: M = 8.04, SD = 3.33); F (2, 281) = 0.78, p = .46, and there was no difference in the number of completed sessions as a function of group membership by treatment type; F (2, 278) = 0.04, p = .96. There was no difference in the proportion of participants who received any treatment (i.e., 1 or more sessions) as a function of class membership (moderate group: 93.4%; high group: 94.9%; dissociative group: 94.1%); χ2 (2, 284) = 0.19, p = .91. Nor was there a class membership by treatment type effect on receiving any treatment; χ2 (2, 284) = 0.95, p = .62. There were no group differences in the proportion of participants who completed treatment (moderate group: 70.3%; high group: 74.4%; dissociative group: 68.2%); χ2 (2, 284) = 0.77, p = .68, and no interaction between group membership and treatment type on therapy completion; χ2 (2, 284) = 0.03, p = .99.
Table 2. Percentage of Individuals who no Longer Met Criteria for PTSD at Follow-up as a Function of Class Assignment.
| % No Longer Meeting Criteria for PTSD | ||||
|---|---|---|---|---|
|
|
||||
| Follow-up Point | 1. Moderate PTSD (n = 98) | 2. High PTSD (n = 64) | 3. High PTSD & Dissociative (n = 73) | Omnibus Comparison χ2 (df = 2) |
| Month 0 | 43.88a | 18.75b | 17.81b | 18.19*** |
| Month 3 | 45.92a | 24.19b | 20.83b | 14.50*** |
| Month 6 | 50.53a | 26.15b | 26.09b | 14.30*** |
Note. Sample size listed in the second row reflects the baseline sample size for each group. Sample size at the immediate follow-up assessment (Month 0) was n = 98, 64, and 73 for groups 1,2, and 3, respectively. Sample size at Month 3 was n = 98, 62, and 72 for groups 1, 2, and 3, respectively. Sample size Month 6 was n = 95, 65, and 69 for groups 1, 2, and 3, respectively. For each follow-up, percentages sharing the same subscript are not significantly different from each other (p > .05). PTSD = posttraumatic stress disorder.
p < .001.
We next tested if the severity of derealization and depersonalization changed in response to PTSD treatment. Descriptive statistics for each class at each time point as a function of treatment type are listed in Table 3. As with the model for the CAPS, the initial model with the treatment type by class assignment term yielded good fit, χ2 (13, n = 284) = 16.00, p = .25 (RMSEA = .03, 90% CI for RMSEA: < .001 = .07, CFI = 1.0, TLI = .99, SRMR = .02), but the interaction did not predict the slope or intercept factors (smallest p = .10). Given this, we again collapsed across treatment type and re-ran the latent growth curve model. This model fit the data well, χ2 (7, n = 284) = 12.40, p = .09 (RMSEA = .05, 90% CI for RMSEA: < .001 = .10, CFI = .99, TLI = .99, SRMR = .03), and revealed significant effects of the moderate and high PTSD classes (versus the dissociative class) on the intercept factor (unst γs = -1.66 and -1.45, respectively, both ps < .001, 95% CIs: -1.77 to -1.55 and -1.57 to -1.32, respectively; see Figure 2). As expected, the former two groups had lower baseline mean scores on dissociation relative to the dissociative class. In addition, both group variables predicted the slope factor such that the moderate and high PTSD groups had more positive slopes (unst γs = 0.67 and 0.71, respectively, both ps < .001, 95% CIs: 0.46 to 0.89 and 0.48 to 0.94, respectively) relative to the dissociative class, indicating less dissociative symptom decline in these two groups.3 The baseline conditional intercept estimate for the dissociative group was 1.95, 95% CI [1.86, 2.03], p < .001, and the average rate of symptom decline for this group was estimated at -0.52, 95% CI [-0.69, -0.36], p < .001, across the first to last assessment points. The slope and intercept factors were not related to each other (r = -.04, p = .69). The residual variance for the slope factor was significant (p = .005); the residual variance for the intercept factor was not (p = .213).
Table 3. Observed Mean Dissociation Severity Scores (and SDs) by Group and Treatment Type at Each Assessment.
| Class | Baseline | Month 0 | Month 3 | Month 6 | |||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| PCT | PE | PCT | PE | PCT | PE | PCT | PE | ||
|
| |||||||||
| M (SD) | |||||||||
| Moderate PTSD | 0.30 (0.33) | 0.27 (0.36) | 0.47 (0.49) | 0.30 (0.43) | 0.48 (0.61) | 0.38 (0.48) | 0.55 (0.71) | 0.31 (0.56) | |
| High PTSD | 0.49 (0.36) | 0.50 (0.39) | 0.71 (0.76) | 0.78 (0.78) | 0.64 (0.62) | 0.74 (0.81) | 0.41 (0.55) | 0.75 (0.71) | |
| High PTSD & Dissociation | 1.92 (0.54) | 1.97 (0.48) | 1.53 (0.80) | 1.47 (0.88) | 1.54 (0.88) | 1.47 (0.81) | 1.42 (0.90) | 1.22 (0.97) | |
Note. PCT = Present-Centered Therapy; PE = Prolonged Exposure; PTSD = posttraumatic stress disorder.
Figure 2.
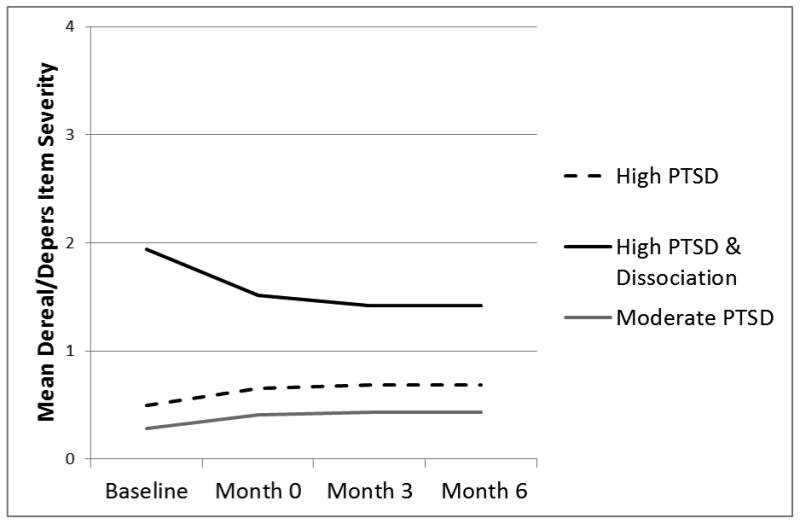
The figure shows the estimated mean dissociation item severity scores at pre-treatment and follow-up assessments as a function of class assignment. PTSD = posttraumatic stress disorder; CAPS = Clinician Administered PTSD Scale.
Discussion
To our knowledge, this is the largest study to date to evaluate the effect of the DS on PTSD treatment response and the first to use latent class assignment to the dissociative group as the moderator of treatment outcome. This was also the first time the DS has been shown to moderate overall PTSD treatment response; prior work has supported subtle effects of dissociation on cognitive and narrative therapy responses (Cloitre et al., 2012; Resick et al., 2012) but no overall dissociation X time effects. In our sample of female active duty service members and Veterans undergoing a trial of PE versus PCT, the high PTSD group demonstrated, on average, a 9.75 greater decrease in CAPS scores over the course of the study compared to the dissociative group. The high PTSD group also had higher baseline PTSD symptoms so that, by 6-months, the high PTSD group was estimated to have CAPS scores that were just 4.7 points below that of the dissociative class. Thus, although dissociation was associated with lesser treatment response relative to the high PTSD group, the magnitude of this effect was small and the clinical significance modest. The rate of change did not differ between the dissociative and moderate PTSD classes. Results also suggested that PTSD treatment yielded marked reductions in dissociative symptoms, consistent with prior work (Cloitre et al., 2012; Hagenaars et al., 2010; Resick et al., 2012). This is notable given that the treatments did not include dissociation-related content. Analyses also suggested that participants with the DS were no more likely to drop out from the trial or to otherwise receive less treatment than those without the DS, regardless of treatment type. This suggests the intervention was tolerable to those with the DS. In contrast to the prevailing clinical perception (Becker et al., 2004), these findings suggest that the DS is not a contraindication for PE as individuals with the DS can benefit from exposure therapy.
Our findings extend the literature concerning the importance of the DS in the DSM-5 diagnostic criteria. The DS may prove useful in treatment planning, case conceptualization, and tracking an individual's response to treatment. It would be reasonable to provide psychoeducation regarding dissociation to those with the DS, to ensure that symptoms of dissociation do not endanger an individual's safety, and to develop safety plans as needed. Results also suggest the importance of assessing the DS in future PTSD treatment trials. If the DS is not quantified and its variance separated from that of PTSD, then it is likely that unmeasured variability in the diagnosis will obscure the search for effective treatments.
Results should be considered in light of study limitations. First, this study included only female veterans and active duty service members undergoing PE and PCT. It is unknown if results generalize to men, non-Veterans, or those engaged in other forms of PTSD treatment. Second, it is possible that excluding individuals with active self-injury and suicidal ideation from the trial may have limited the severity of dissociative symptoms in the sample. Third, analyses focused on DS by treatment type interactions on the rate of change are two-way interactions and were likely under-powered. Fourth, results are based on the DSM-IV definition of PTSD and it is unclear if they generalize to the DSM-5 definition. Finally, given inconsistent findings in the literature and the fact that our significant differences in slope from baseline to 6-month follow-up were somewhat obscured by differences in baseline symptoms between the high PTSD and dissociative groups, it is important for future work to attempt to replicate these results. Despite these limitations, results provide empirical support for the use of exposure treatment for individuals with the DS of PTSD and highlight the value of the inclusion of the DS in DSM-5.
Acknowledgments
The data reported in this article were drawn from grant CSP #494 from the VA Cooperative Studies Program with support from the Department of Defense for CSP #494. This work was also supported by a Career Development Award to Erika J. Wolf from the United States (U.S.) Department of Veterans Affairs, Clinical Sciences Research and Development Program. The contents of this manuscript do not represent the views of the U.S. Department of Veterans Affairs, the Department of Defense, or the United States Government.
Footnotes
Additional participant descriptive characteristics, and details about the measures and procedures, including inclusion/exclusion criteria, and response rates and attrition, are provided in (references masked for review).
We have previously reported (reference masked for review) that the dissociative class did not differ from the high PTSD group on demographic or trauma-related variables with the exception of race, such that the moderate and high PTSD groups included a greater percentage of women who self-reported as White (relative to identifying as a racial minority). Given this, we conducted secondary analyses in which we included race (minority or non-minority) as a covariate of group membership and re-ran the latent growth model. Results with respect to the effect of the DS on the intercept and growth factors were unchanged from the primary results reported in the text (details available from first author).
We also reexamined our latent growth curve model predicting change in dissociative symptoms with race as a covariate of group membership (as footnote # 2). We again found that results with respect to the slope and intercept effects were unchanged from that reported in the text without this covariate (details available from first author).
Contributor Information
Erika J. Wolf, National Center for PTSD at VA Boston Healthcare System, Boston, MA Boston University School of Medicine, Department of Psychiatry, Boston, MA
Carole A. Lunney, National Center for PTSD, White River Junction, VT
Paula P. Schnurr, National Center for PTSD, White River Junction, VT, Department of Psychiatry, Geisel School of Medicine at Dartmouth, Hanover, NH
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: Author; 1994. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5. Arlington, VA: Author; 2013. [Google Scholar]
- Armour C, Elklit A, Lauterbach D, Elhai J. The DSM-5 dissociative-PTSD subtype: Can levels of depression, anxiety, hostility, and sleeping difficulties differentiate between dissociative-PTSD and PTSD in rape victims? Journal of Anxiety Disorders. 2014;28:418–426. doi: 10.1016/j.janxdis.2013.12.008. [DOI] [PubMed] [Google Scholar]
- Becker CB, Zayfert C, Anderson E. A survey of psychologists' attitudes and utilization of exposure therapy for PTSD. Behaviour Research and Therapy. 2004;42(03):277–292. 00138–4. doi: 10.1016/S0005-7967. [DOI] [PubMed] [Google Scholar]
- Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Gusman FD, Charney DS, Keane TM. The development of a clinician-administered PTSD scale. Journal of Traumatic Stress. 1995;8:75–90. doi: 10.1002/jts.2490080106. [DOI] [PubMed] [Google Scholar]
- Briere J. Trauma Symptom Inventory Professional Manual. Odessa, FL: Psychological Assessment Resources; 1995. [Google Scholar]
- Cloitre M, Petkova E, Wang J, Lu F. An examination of the influence of a sequential treatment on the course and impact of dissociation among women with PTSD related to childhood abuse. Depression and Anxiety. 2012;29:709–717. doi: 10.1002/da.21920. [DOI] [PubMed] [Google Scholar]
- Hagenaars MA, van Minnen A, Hoogduin KL. The impact of dissociation and depression on the efficacy of prolonged exposure treatment for PTSD. Behaviour Research and Therapy. 2010;48:19–27. doi: 10.1016/j.brat.2009.09.001. [DOI] [PubMed] [Google Scholar]
- Halvorsen JØ, Stenmark H, Neuner F, Nordahl HM. Does dissociation moderate treatment outcomes of narrative exposure therapy for PTSD? A secondary analysis from a randomized controlled clinical trial. Behaviour Research and Therapy. 2014;57:21–28. doi: 10.1016/j.brat.2014.03.010. [DOI] [PubMed] [Google Scholar]
- Lanius RA, Vermetten E, Loewenstein RJ, Brand B, Schmahl C, Bremner JD, Spiegel D. Emotion modulation in PTSD: clinical and neurobiological evidence for a dissociative subtype. American Journal of Psychiatry. 2010;167:640–647. doi: 10.1176/appi.ajp.2009.09081168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus user's guide. 7. Los Angeles, CA: Muthén & Muthén; 1998-2012. [Google Scholar]
- Price M, Kearns M, Houry D, Rothbaum BO. Emergency department predictors of posttraumatic stress reduction for trauma-exposed individuals with and without an early intervention. Journal of Consulting and Clinical Psychology. 2014;82:336–341. doi: 10.1037/a0035537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Resick PA, Suvak MK, Johnides BD, Mitchell KS, Iverson KM. The impact of dissociation on PTSD treatment with cognitive processing therapy. Depression and Anxiety. 2012;29:718–730. doi: 10.1002/da.21938. [DOI] [PubMed] [Google Scholar]
- Schnurr PP, Friedman M, Engel C, Foa E, Shea M, Chow B, Bernardy N. Cognitive behavioral therapy for posttraumatic stress disorder in women: A randomized controlled trial. Journal of the American Medical Association. 2007;297:820–830. doi: 10.1001/jama.297.8.820. [DOI] [PubMed] [Google Scholar]
- Stein DJ, Koenen KC, Friedman MJ, Hill E, McLaughlin KA, Petukhova M, Kessler RC. Dissociation in posttraumatic stress disorder: Evidence from the World Mental Health Surveys. Biological Psychiatry. 2013;73:302–312. doi: 10.1016/j.biopsych.2012.08.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steuwe C, Lanius RA, Frewen PA. Evidence for a dissociative subtype of PTSD by latent profile and confirmatory factor analyses in a civilian sample. Depression and Anxiety. 2012;29:689–700. doi: 10.1002/da.21944. [DOI] [PubMed] [Google Scholar]
- van Minnen A, Harned MS, Zoellner L, Mills K. Examining potential contraindications for prolonged exposure therapy for PTSD. European Journal of Psychotraumatology. 2012;3:18805. doi: 10.3402/ejpt.v3i0.18805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolf EJ, Lunney CA, Miller MW, Resick PA, Friedman MJ, Schnurr PP. The dissociative subtype of PTSD: A replication and extension. Depression and Anxiety. 2012;29:679–688. doi: 10.1002/da.21946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolf EJ, Miller MW, Reardon AF, Ryabchenko KA, Castillo D, Freund R. A latent class analysis of dissociation and PTSD: Evidence for a dissociative subtype. Archives of General Psychiatry. 2012;69:698–705. doi: 10.1001/archgenpsychiatry.2011.1574. [DOI] [PMC free article] [PubMed] [Google Scholar]


