Abstract
Originally formulated to understand the recurrence of depressive disorders, the stress generation hypothesis has recently been applied in research on anxiety and externalizing disorders. Results from these investigations, in combination with findings of extensive comorbidity between depression and other mental disorders, suggest the need for an expansion of stress generation models to include the stress generating effects of transdiagnostic pathology as well as those of specific syndromes. Employing latent variable modeling techniques to parse the general and specific elements of commonly co-occurring Axis I syndromes, the current study examined the associations of transdiagnostic internalizing and externalizing dimensions with stressful life events over time. Analyses revealed that, after adjusting for the covariation between the dimensions, internalizing was a significant predictor of interpersonal dependent stress, whereas externalizing was a significant predictor of noninterpersonal dependent stress. Neither latent dimension was associated with the occurrence of independent, or fateful, stressful life events. At the syndrome level, once variance due to the internalizing factor was partialled out, unipolar depression contributed incrementally to the generation of interpersonal dependent stress. In contrast, the presence of panic disorder produced a “stress inhibition” effect, predicting reduced exposure to interpersonal dependent stress. Additionally, dysthymia was associated with an excess of noninterpersonal dependent stress. The latent variable modeling framework used here is discussed in terms of its potential as an integrative model for stress generation research.
Keywords: stress generation, internalizing disorders, externalizing disorders, comorbidity, young adulthood
According to the original formulation of the stress generation hypothesis (Hammen, 1991), individuals with a history of depression, relative to their never-depressed counterparts, encounter a higher rate of stressful life events that are dependent, at least in part, on their own actions. An extensive body of longitudinal research over the past two decades has consistently supported this hypothesis (Liu & Alloy, 2010). However, one facet of stress generation theory that remains relatively unexplored is the role of other disorders in the stress generation phenomenon (see Hammen, 2006). In fact, the specificity of stress generation to depression has been challenged by recent data demonstrating that a pattern of stress generation is associated with a variety of other clinical syndromes (e.g., Allen & Rapee, 2009; Connolly, Eberhart, Hammen, & Brennan, 2010; Rudolph, 2008).
It is explicit in modern diagnostic criteria that all psychological disorders involve impaired functioning in typical roles. Thus, it is inherent in the conceptualization of psychopathology that symptoms cause disruptions in domains such as relationships, work, and financial stability, and it may be assumed that such disruptions represent acute and chronic stressors. Further, functional disabilities likely stem not just from symptoms, but also from underlying vulnerabilities for disorders, such as neurocognitive, information-processing, emotion regulation, neuroendocrine, and personality factors. In short, individuals who are diagnosed with any disorder, or are at risk for disorder, likely behave in ways that contribute to stressors in their lives.
At the same time, an abundant literature on the stress-depression association gives some reason to believe that depression plays a uniquely important role in the generation of stressors. Therefore, the purpose of the present study is to expand stress generation models to apply both to depression and broadband dimensions of psychopathology that cut across traditional diagnostic boundaries. The questions are approached with a methodology designed specifically to take into account the problems associated with comorbidity inherent in current nosological systems. Specifically, we use a hierarchical-spectrum model of mental disorders (Krueger & Piasecki, 2002) to evaluate the influences of (a) transdiagnostic internalizing and externalizing dimensions of pathology and (b) specific clinical syndromes on the stress generation effect.
Specificity of the Stress Generation Effect
Hammen (1991) initially observed that women with a history of unipolar depression, as compared to women with chronic medical conditions, bipolar disorder, and no disorder, experienced an excess of stressful events that were at least partly caused by their own personality traits or behavioral characteristics (i.e., dependent stress). This group difference was most pronounced in the domain of conflict stress, a subset of dependent stress characterized by disturbances in interpersonal relationships. Unipolar depressed women did not, however, experience higher rates of independent, or fateful, events. This stress generation pattern has been replicated across clinical (Chun, Cronkite, & Moos, 2004; Harkness, Monroe, Simons, & Thase, 1999) and community (Harkness & Luther, 2001) samples of depressed men and women. Prior work in samples of depressed children and adolescents (Rudolph & Hammen, 1999; Rudolph et al., 2000), as well as in samples of college students endorsing elevated depressive symptom levels (Hankin, Kassel, & Abela, 2005), also supports the stress generation hypothesis.
Although Hammen (1999; 2006) has theorized that stress generation is not a direct result of the depression syndrome per se, and various studies have documented that stress generation occurs even during remission from a depressive episode (Daley et al., 1997; Hammen, 1991), the majority of previous research has conceptualized stress generation as a feature of depression. However, emerging evidence suggests that other forms of psychopathology may produce a stress generation effect. For example, anxiety disorders have been linked with elevated levels of dependent stress (e.g., Allen & Rapee, 2009; Connolly et al., 2010) and the personality trait of anxiety sensitivity, theorized to be a diathesis for various anxiety disorders (Reiss, Peterson, Gursky, & McNally, 1986), has been found to predict the occurrence of dependent stressors (Riskind, Black, & Shahar, 2010). Moreover, research has shown neuroticism, a nonspecific vulnerability factor for depressive and anxiety disorders (Clark & Watson, 1991), to confer risk for increased dependent stress exposure (Ellenbogen & Hodgins, 2004; Kercher, Rapee, & Schniering, 2009).
Several developmental psychopathology studies suggest that higher levels of externalizing psychopathology may also lead to increases in dependent stress over time (Carter, Garber, Ciesla, & Cole, 2006; Rudolph, 2008; Rudolph et al., 2000). For example, in a high risk sample of young adolescents followed over four years, Carter and colleagues (2006) found that maternal reports of adolescents’ externalizing symptoms predicted frequencies of subsequent peer and academic hassles. Additionally, Rudolph (2008) reported a robust stress generation effect for adolescent externalizing symptoms, but not depressive symptoms, with respect to noninterpersonal dependent stress. Conversely, depressive symptoms, but not externalizing symptoms, were longitudinally associated with interpersonal dependent stress in this study. These findings suggest that both depression and externalizing symptoms contribute to the generation of dependent stress, although event content (i.e., interpersonal, noninterpersonal) may differ for depression versus externalizing pathology.
Further highlighting the complex roles of internalizing and externalizing psychopathology in stress generation, comorbidity of depression with other syndromes has been found to augment the stress generation effect (Connolly et al., 2010; Daley et al., 1997; Harkness & Luther, 2001). Daley and colleagues (1997) initially reported that interpersonal stress levels were higher among individuals with comorbid, relative to pure, depression. Harkness and Luther (2001) subsequently demonstrated that comorbid anxiety and dysthymia intensified stress generation among a clinical sample of individuals diagnosed with depression. Specifically, the stress generation effect was most evident for the group with both anxiety and dysthymia diagnoses (in addition to depression), relative to individuals with only comorbid anxiety or dysthymia.
In sum, these data indicate that stress generation may be a consequence of multiple forms of psychopathology. However, previous studies have been heterogeneous with respect to sample composition, stress assessment instruments, and symptom- versus diagnosis-based conceptualizations of psychopathology. These inconsistencies make it difficult to draw definitive conclusions about the pattern of stress generation across various syndromes. The present study provides a comprehensive examination of stress generation effects in common Axis I syndromes using psychometrically-sound stress assessment interviews. Further, we expand on previous research by investigating the stress generating effects of core psychopathological processes that account for comorbidity among internalizing and externalizing disorders. The next sections review the origins and current theoretical status of a structural model of comorbidity among mental disorders and the possibility of using it to examine the independent and joint contributions of various Axis I syndromes to stress generation.
Hierarchical-Spectrum Model (HSM) of Mental Disorders
Coinciding with the increasing recognition of the roles of anxiety and externalizing disorders in the stress generation literature, advances in latent variable modeling theory have promoted the development of quantitative models of comorbidity. These efforts were originally stimulated by the observation that certain sets of syndromes tend to co-occur at particularly high rates. For instance, according to the National Comorbidity Survey Replication, respondents endorsing major depression in the past year are also commonly diagnosed with anxiety disorders (57.5%), as compared to substantially lower rates of comorbidity with substance use (8.5%) or impulse control (16.6%) disorders (Kessler et al., 2003). Acknowledging these reliable constellations of diagnostic co-occurrence, Clark et al. (1995) argued that “comorbidity, while rampant, is not random” (p. 129).
This realization inspired researchers to develop explanatory models to elucidate the origins of comorbidity patterns. While some of these theories focused on how comorbidity may be explained by limitations in diagnostic assessment tools or study recruitment methods (e.g., Caron & Rutter, 1991), a preponderance of evidence indicated that comorbidity is not an artifactual phenomenon (Angold, Costello, & Erkanli, 1999). Thus, the majority of recent work has focused on common cause models, in which highly comorbid syndromes are posited to be indicators of a single latent vulnerability factor in much the same way that vocabulary and comprehension scales on intelligence tests are considered to be indicators of a higher-order verbal index.
In a landmark study, Krueger and colleagues (1998) used confirmatory factor analysis (CFA) to delineate the number and nature of latent factors underlying 10 common mental disorders assessed in the longitudinal Dunedin, New Zealand, birth cohort study (Silva, 1990). These authors found support for a two-factor model in which major depression (MDD), dysthymia (DYS), generalized anxiety disorder (GAD), agoraphobia (AGO), social phobia (SOP), specific phobia (SPP), and obsessive-compulsive disorder (OCD) loaded on a latent internalizing spectrum, whereas conduct disorder (CD), marijuana dependence, and alcohol dependence loaded on a latent externalizing spectrum. Following Krueger and colleagues (e.g., Krueger & Piasecki, 2002), we label this theoretical model the hierarchical-spectrum model (HSM) of mental disorders, where hierarchical refers to the distinction between the superordinate latent variable level and the subordinate observed syndrome level of the model, and spectrum refers to the continuous scale of the liability factors.
Krueger (1999) followed up the initial study by examining the latent structure of a similar set of 10 mental disorders in the National Comorbidity Survey (NCS). Model fit indices suggested that a three-factor model, in which the internalizing factor bifurcated into anxious-misery (defined by MDD, DYS, and GAD) and fear (defined by panic disorder [PAN], AGO, SOP and SPP) subfactors, offered the best approximation of the observed diagnostic correlations in the complete NCS sample. However, the two internalizing subfactors were highly correlated, and in the treatment-seeking subsample of NCS respondents, the two-factor (correlated internalizing and externalizing dimensions) model provided the best fit.
Subsequent research has replicated the basic two-factor HSM configuration across a variety of cultures and age ranges (see Krueger & Markon, 2006). Supporting the traitlike nature of the latent dimensions, longitudinal studies of the HSM have reported considerable rank-order stability of HSM dimensions over time, with some indication that standing on externalizing is especially stable (Fergusson, Horwood, & Boden, 2006; Vollebergh et al., 2001). For example, over a three year interval in the Dunedin study, standardized autocorrelation effects were 0.69 for internalizing and 0.86 for externalizing (Krueger et al., 1998). Moreover, quantitative genetics studies have shown these phenotypically coherent liability spectra to also be genotypically coherent. Two separate investigations have now identified distinct genetic components underlying risk for internalizing and externalizing syndromes (Kendler et al., 2003; Wolf et al., 2010). Taken together, these data suggest that the internalizing and externalizing dimensions are traitlike, etiologically-distinct vulnerability factors that have the potential to serve as useful explanatory constructs in research on psychopathology.
The HSM as an Integrative Model for Stress Generation Research
With only a few notable exceptions (Kramer, Krueger, & Hicks, 2008; Patrick et al., 2006), the HSM has been used for descriptive purposes and not to evaluate theories of psychopathology. Yet, the HSM framework offers a powerful method for elucidating the general and specific causes and consequences of mental disorders (Krueger & Piasecki, 2002). That is, the associations of a particular psychopathological construct (e.g., dependent stress) with (a) transdiagnostic dimensions and (b) specific syndromes can be simultaneously ascertained. For example, it is possible that the stress generation effect documented previously in the depression literature is in large part a result of individual differences on the internalizing dimension, of which depression is a strong marker (e.g., Krueger, 1999). An alternative, and complementary, hypothesis is that depression contributes to the occurrence of dependent stress even after adjusting for the variance it shares with the internalizing dimension, which would suggest that depression plays a unique role in stress generation.
There are two reasons to hypothesize a unique association between depression and the generation of interpersonal stress. First, while stress generation broadly refers to the elevated rates of events that are dependent on the person’s actions and characteristics, the initial stress generation research found particularly strong evidence that unipolar depressed women, compared to those with other disorders, had higher rates of interpersonal conflict events. Second, various vulnerability factors implicated in depression are particularly likely to affect interpersonal functioning, such as excessive reassurance seeking, negative feedback seeking, co-rumination, anxious attachment style, and high levels of sociotropy (Blatt & Zuroff, 1992; Joiner, 1995; Prinstein, Borelli, Chea, Simon, & Aikins; Rose, 2002; Reinecke & Rogers, 2001). Indeed, there is empirical evidence to support the notion that such interpersonal styles lead to higher rates of interpersonal impairment. For instance, a number of studies have demonstrated that excessive reassurance seeking serves as a risk factor for interpersonal, but not noninterpersonal or independent, stress exposure (Eberhart & Hammen, 2009; Shih, Abela, & Starrs, 2009). Similarly, Shih (2006) reported that a sociotropic personality style was associated with elevated levels of exposure to interpersonal, but not achievement, stress in women. Further, adult avoidant and anxious attachment styles have been linked to higher rates of interpersonal stress (Hankin et al., 2005). While research has shown that several of these vulnerability factors are correlated with other disorders besides depression—for example, anxious attachment increases risk for multiple clinical syndromes (Mickelson, Kessler, & Shaver, 1997)—many of them are theorized to be particularly central to the psychopathology of depression and have been most robustly linked to depression, relative to other diagnostic categories, in empirical studies (e.g., Coyne, 1976; Joiner, 1995; Rose, 2002). Finally, several cognitive styles theorized to be proximal risk factors for depression (i.e., hopelessness, rumination) have been prospectively associated with increases in interpersonal stress (Joiner, Wingate, & Otamendi, 2005; Kercher & Rapee, 2009). Based on this body of evidence, it is predicted that a specific association between depression and stress generation will be observed even after accounting for the associations between broadband internalizing and externalizing dimensions and stress generation.
The current study has two primary objectives. First, the stress generation approach is expanded to include tests of the impact of the latent internalizing and externalizing dimensions of the HSM on the generation of stressful life events, using structural equation modeling to parse the variance shared among syndromes from variance specific to each syndrome. In the HSM framework, the internalizing factor represents the variance shared among depressive and anxiety disorders. Likewise, the externalizing factor represents the variance shared among substance use and disruptive behavior disorders.
Second, the present study examines the effects of the specific components of each syndrome on stress generation. The specific component of major depression, for example, represents the variance in depression that is statistically independent (i.e., unique) from the variance it shares with all other syndromes. Significant associations between syndrome-specific components and stress would indicate that diagnostic categories capture unique clinical features relevant to stress generation.
This study was carried out in a community sample of behaviorally high-risk young adults oversampled for maternal depression. Semi-structured interviews were administered to assess the contextual threat associated with stressful life events (e.g., Hammen, 1991), and structured diagnostic protocols were used to determine the presence of Axis I syndromes. Based on prior work associating stress generation with a diversity of internalizing and externalizing problems (see Liu & Alloy, 2010), we hypothesize that elevations on the internalizing and externalizing dimensions will predict increased levels of dependent, but not independent, stress. In view of evidence that externalizing symptoms may eventuate in more noninterpersonal dependent stress (such as academic or other achievement domains; Rudolph, 2008), it is anticipated that the externalizing dimension will be related to noninterpersonal dependent stress only, while the internalizing dimension will be linked specifically with interpersonal dependent stress, after adjusting for the covariation between these dimensions. As noted previously, it is also expected that the specific component of major depression will predict interpersonal dependent stress levels, even after accounting for the influence of the internalizing factor.
Method
Participants
A sample of 815 15-year-old youth was selected from the Mater-University Study of Pregnancy (MUSP) in Brisbane, Australia (Keeping et al., 1989), which followed a birth cohort of over 7,000 mothers and their offspring born between 1981 and 1984 at the Mater Misericordiae Mother’s Hospital to study children’s health and development. This sample was selected to include youth with mothers who endorsed a wide range of experiences with depression based on perinatal evaluations of the severity and chronicity of maternal depressive symptoms. As detailed below, diagnostic assessments of mothers at offspring age 15 revealed that 318 (45.1%) had a lifetime history of major depression or dysthymia. Complete details of the sampling procedures have been published elsewhere (Hammen, Shih, Altman, & Brennan, 2003).
When youth reached age 20, all families were recontacted regarding participation in a second assessment, with 705 youth (363 [51.4%] females) and mothers consenting to complete further interviews and questionnaires (2 were deceased, 51 refused, 52 could not be located or scheduled, 1 withdrew after data collection). The sample was 92% Caucasian and 8% minority (Asian, Pacific Islander, and Aboriginal), with median family income falling in the lower middle class and mothers’ median education level at grade 10. Youth participating at age 20 did not differ from those participating at age 15 but not 20 in terms of family income at age 15 (t(782) = −1.49, p = .14), maternal depression history by age 15 (χ2(1, 815) = 0.18, p = .67), or history of any depressive, anxiety, or externalizing disorder by age 15 (χ2 s < 1, ps > .10). Youth not participating at age 20 were more likely to be male (χ2(1, 815) = 11.08, p < .01).
Procedures
Interviews assessing stress exposure and Axis I diagnoses were administered independently to youth and mothers in their homes at youth age 15 and again to youth when they reached age 20. Interviewers were advanced graduate students in psychology and were blind to maternal depression status and youth prior psychiatric history. All participants gave their written informed consent (or assent), and were compensated for their time. All procedures were approved by the UCLA Institutional Review Board, Emory University Investigations Committee, and the University of Queensland Ethics Review Committee.
Measures
Lifetime Axis I Diagnoses
The Schedule for Affective Disorders and Schizophrenia in School-Aged Children (K-SADS-E; Orvaschel, 1995) was administered during age 15 data collection to determine offspring current and lifetime diagnoses of Axis I psychiatric disorders. The K-SADS-E is a widely used and validated semi-structured interview for assigning Axis I diagnoses in children and adolescents. Trained clinicians interviewed adolescents and their mothers separately and privately during the age 15 assessment. Diagnoses were assigned if either the adolescent or maternal interview indicated that the adolescent qualified for a given syndrome. Interrater reliability was assessed using a random sample of 75 K-SADS-E interview recordings evaluated by clinicians blind to the original diagnostic ratings. Weighted kappas were in the acceptable range (i.e., greater than 0.75) for all internalizing and externalizing disorders.
The Structured Clinical Interview for DSM-IV (SCID; First, Spitzer, Gibbon, & Williams, 1995) was administered at offspring age 20 to assess for onsets of Axis I syndromes since the age 15 assessment. Diagnostic information from the K-SADS-E and SCID interviews was combined to determine the lifetime presence of internalizing and externalizing diagnoses. However, for the current analyses diagnoses with onsets occurring in the 12 months prior to the age 20 assessment were omitted in order to ensure that the onsets of all diagnoses preceded the occurrence of acute stressors. Therefore, although diagnosis onsets always preceded stress exposure, the amount of time elapsed between disorder onset and stress occurrence was variable across participants and across disorders within participants. To determine interrater reliabilities for SCID diagnoses, a sample of 55 interviews were selected and reviewed by a second trained clinician blind to the original diagnoses. Weighted kappas for internalizing and externalizing disorders were all above 0.79.
At the age 15 assessment, the SCID was also used to evaluate mothers’ lifetime history of depression, which served as a covariate in supplementary stress generation analyses described below. Based on a sample of 33 interviews reviewed by multiple raters, a kappa value of 0.79 was computed for ratings of maternal depression history, indicating adequate interrater reliability.
Acute Stressful Life Events
At age 20, participants were administered the semi-structured UCLA Life Stress Interview (LSI; Hammen, Henry, & Daley, 2000). Modeled after the contextual threat assessment methods of George Brown and colleagues (e.g., Brown & Harris, 1978), the interview uses standard general probes to elicit specific life events in the past 12 months and follow-up queries to establish the dating of each event and circumstances surrounding its occurrence. Written narratives of each event were then presented to a rating team that was blind to youths’ actual response to the event. For each event, the team then assigned a severity rating representing the impact this event would be expected to have on an average person in identical circumstances. Severity ratings ranged from 1 (no impact) to 5 (extremely severe). Each event was also rated in terms of its dependence (i.e., the extent to which it was caused by the participant’s behavior or characteristics) on a 1 (fateful or completely independent) to 5 (completely dependent) scale; events with a rating greater than or equal to 3 (partly dependent) are considered to be dependent, as previously reported by Hammen and colleagues (2000). The rating team also determined whether or not each event was interpersonal in nature, based on identification of the primary content. For instance, dependent interpersonal events focused on a relationship with another person and included disputes, losses, or separations due at least in part to the participant’s behaviors, whereas noninterpersonal dependent events were commonly related to work or school performance, person-determined injuries, or financial challenges. For each participant, a cumulative objective stress score was created for each class of event (i.e., independent, noninterpersonal dependent, interpersonal dependent) by summing the objective threat ratings across all events. The number of stressful life events reported per participant ranged from 0 to 11 (M = 3.22, SD = 1.95). Reliability and validity data for the UCLA Life Stress Interview have been reported in other studies of adolescents and young adults (e.g., Hammen et al., 1995). In the present sample, the interrater reliability analyses for 89 cases yielded intraclass correlations of 0.95 and 0.97 for severity and dependence ratings, respectively, and a kappa of 0.89 for the interpersonal (versus noninterpersonal) rating.
Chronic Stress
The LSI was also used at the age 15 assessment to gather information about the ongoing difficulties in at least the prior 6 months in several domains: best friendship, romantic relationship, relationships with family members, finances, health (self), health of family members, academic performance, and school behavior. Interviewers assigned a rating to each domain according to a set of behaviorally-specific anchors. Ratings ranged from 1 (no stress; superior circumstances) to 5 (severe stress; major difficulties). The chronic stress interview attempts to ascertain an objective assessment of ongoing stressful conditions that is independent of the individual’s subjective experience of stress. The stability of the LSI chronic stress ratings has been established in previous longitudinal investigations (e.g., Daley, Hammen, & Rao, 2000; Hammen, Kim, Eberhart, & Brennan, 2009), and its convergent validity—in terms of significant agreement with other measures of functioning in typical roles such as academic performance, successful peer relations, and quality of parent-child relationships—has been documented consistently (Hammen, 2005; Hammen et al., 2009). In the present study, reliability analyses using independent raters yielded intraclass correlations of 0.77 and higher for each chronic stress domain. The chronic stress score used in the present analyses was computed by summing interviewer ratings across all domains.
Data Analytic Plan
Data analyses using structural equation modeling proceeded in three parts. First, the fit of the two-factor (internalizing and externalizing) and three-factor (in which the internalizing factor is divisible into anxious-misery and fear subfactors) models was compared. In the two-factor model, the internalizing factor was defined by MDD, DYS, GAD, PAN, SOP, SPP, and post-traumatic stress disorder (PTSD) diagnoses, and the externalizing factor was defined by CD, oppositional defiant disorder (ODD), alcohol abuse or dependence (AAD), and drug abuse or dependence (DAD) diagnoses. In the three-factor model, the anxious-misery subfactor was defined by MDD, DYS, GAD, and PTSD, whereas the fear subfactor was defined by PAN, SOP, and SPP (see Watson, 2005)1. These models were evaluated and compared on the basis of the likelihood ratio chi-square test, the comparative fit index (CFI; Bentler, 1990), the root-mean-square error of approximation (RMSEA; Browne & Cudeck, 1993), and the weighted root-mean-square residual (WRMR).
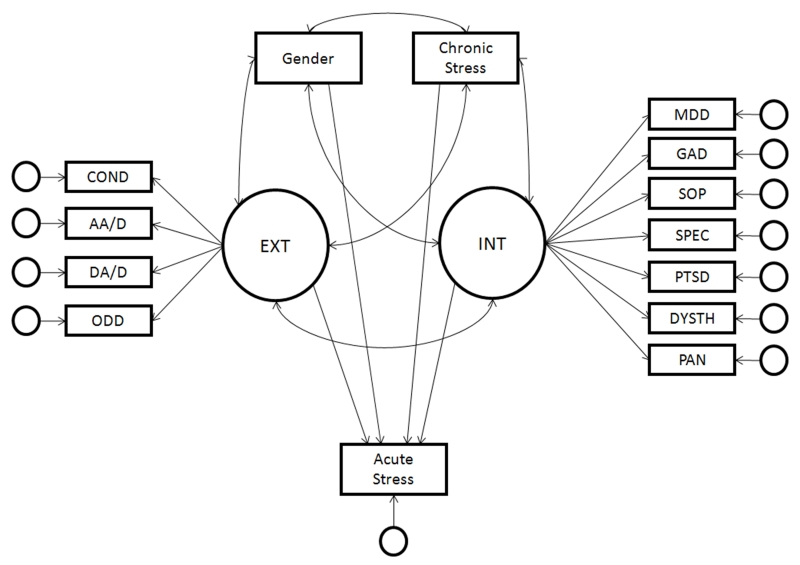
Second, the predictive associations between the latent dimensions and all three classes of stress (i.e., independent, noninterpersonal dependent, and interpersonal dependent) were examined in three separate models. That is, the sum of contextual threat ratings within a particular class of stress was regressed on the factors from the best fitting factor model (see Figure 1). Importantly, in these regressions, the effect of the factors on stress occurrence above and beyond the effects of other factors was estimated (e.g., shared variance between internalizing and externalizing factors was partialled out in the regression of stress on the internalizing factor).
Figure 1.
Path diagram of the stress generating effects of the internalizing and externalizing dimensions. INT = internalizing; EXT = externalizing; COND = conduct disorder; AA/D = alcohol abuse or dependence; DA/D = drug abuse or dependence; ODD = oppositional defiant disorder; MDD = major depressive disorder; GAD = generalized anxiety disorder; SOP = social phobia; SPEC = specific phobia; PTSD = post-traumatic stress disorder; DYSTH = dysthymia; PAN = panic disorder. Unlabeled circles represent residual variances.
Multiple group structural equation modeling was carried out to examine gender as a moderator of the stress generating effects of the internalizing and externalizing dimensions given previous research reporting gender differences in rates of exposure to dependent stressors (Rudolph & Hammen, 1999; Shih, 2006). Two models were compared in tests of moderation. In one, the regression of acute stress on the latent dimensions was constrained to be equal across gender. In the other, these parameters were allowed to vary for males and females. A likelihood ratio test (LRT) was used to compare the fit of these two models (Chou & Bentler, 2002). Significant LRT values would indicate that constraining the structural paths to equality across gender degrades model fit, reflecting statistically significant moderation. LRTs for gender moderation revealed no significant differences for males and females for any of the 3 types of stress (all χ2s < 1, ps > .10). As such, all results presented below reflect analyses conducted in the full sample. However, gender was included as a covariate in all stress generation models in light of prior research in young adult (e.g., Achenbach, 1997) and epidemiological samples (Kessler et al., 2003) demonstrating prominent gender differences in susceptibility to both internalizing and externalizing pathology.
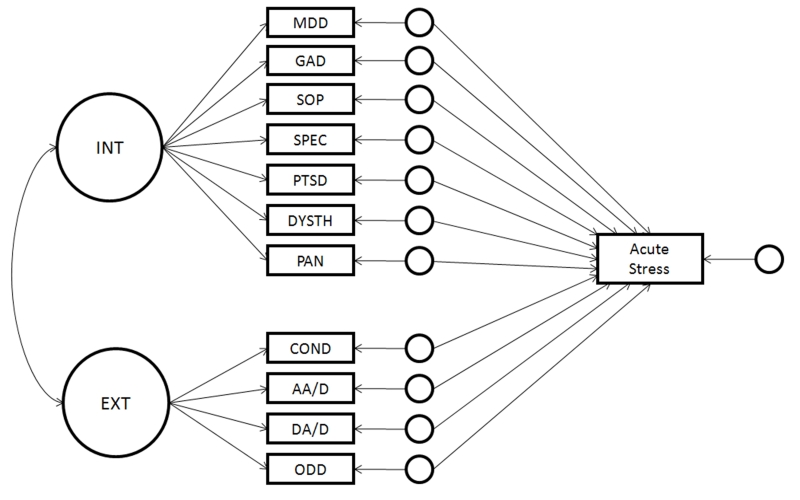
Third, each class of stress was regressed on the residual variances of all observed syndromes (see Figure 2). Again, separate models were estimated to evaluate the residual associations of diagnoses with independent, noninterpersonal dependent, and interpersonal dependent stress. These analyses were carried out to determine whether the unique portions of the various manifest syndromes (i.e., variance not shared with other disorders) predicted stress occurrence. It is useful to reiterate here that only diagnoses with onsets that preceded the 12 month period prior to the age 20 data collection point were included in the present analyses in order to establish the appropriate temporal ordering between syndrome and stress occurrence.
Figure 2.
Path diagram of the stress generating effects of the unique components of Axis I syndromes. For clarity of presentation, the effects of covariates (i.e., gender, chronic stress) are omitted from this diagram. INT = internalizing; EXT = externalizing; COND = conduct disorder; AA/D = alcohol abuse or dependence; DA/D = drug abuse or dependence; ODD = oppositional defiant disorder; MDD = major depressive disorder; GAD = generalized anxiety disorder; SOP = social phobia; SPEC = specific phobia; PTSD = post-traumatic stress disorder; DYSTH = dysthymia; PAN = panic disorder. Unlabeled circles represent residual variances.
Chronic stress assessed at age 15 was included as a covariate in all stress generation analyses given its associations with both acute stress (Hammen et al., 2009) and psychopathology (Paykel & Cooper, 1992). That is, we wanted to isolate the portion of the relationship between psychopathology and acute stress exposure that was independent of the effects of chronic stress. All analyses were performed in Mplus 5.0 using the WLSMV estimator (Muthén & Muthén, 2007).
Results
Structure of the HSM
Table 1 displays the frequencies of Axis I diagnoses in the current sample as well as a tetrachoric correlation matrix for all diagnoses. A visual inspection of Table 1 reveals that the externalizing disorders tended to co-occur more often with each other than with internalizing disorders, providing a preliminary indication of the distinction between internalizing and externalizing spectra.
Table 1. Correlations and Descriptive Statistics for Study Variables.
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Major Depression | — | ||||||||||||||
| 2. Dysthymia | .36 | — | |||||||||||||
| 3. Generalized Anxiety Disorder | .57 | .32 | — | ||||||||||||
| 4. Panic Disorder | .53 | .51 | .47 | — | |||||||||||
| 5. Social Phobia | .21 | .24 | .41 | .10 | — | ||||||||||
| 6. Specific Phobia | .16 | .20 | .28 | .19 | .23 | — | |||||||||
| 7. Post-Traumatic Stress Disorder | .54 | .32 | .46 | .25 | .08 | .24 | — | ||||||||
| 8. Obsessive-Compulsive Disorder | .04 | −.06 | .33 | .08 | −.05 | .15 | .33 | — | |||||||
| 9. Conduct Disorder | .11 | .26 | .01 | .39 | .24 | .19 | .01 | .03 | — | ||||||
| 10. Oppositional Defiant Disorder | .25 | .07 | .30 | .06 | .39 | −.15 | .30 | .37 | .15 | — | |||||
| 11. Alcohol Abuse/Dependence | .28 | .02 | .25 | .21 | .17 | .03 | .25 | .30 | .40 | .53 | — | ||||
| 12. Drug Abuse/Dependence | .24 | .21 | .23 | .19 | .27 | .06 | .31 | .29 | .54 | .36 | .59 | — | |||
| 13. Interpersonal Stress | .28 | .16 | .18 | .03 | .04 | .15 | .24 | .17 | −.03 | .08 | .15 | .14 | — | ||
| 14. Noninterpersonal Stress | .03 | .15 | .11 | .11 | .07 | .02 | −.01 | −.08 | .20 | .13 | .08 | .23 | .07 | — | |
| 15. Independent Stress | .15 | .15 | .03 | −.08 | .04 | .07 | .08 | .18 | .02 | .06 | .12 | .06 | .25 | .01 | — |
| 16. Gender | −.26 | −.14 | −.18 | −.11 | .09 | −.24 | −.34 | −.15 | .23 | .16 | .09 | .18 | −.12 | .10 | −.10 |
| N (% of sample) | 204 (28.6) | 63 (8.9) | 37 (5.2) | 14 (2.0) | 112 (15.8) | 79 (11.2) | 39 (5.5) | 16 (2.3) | 22 (3.1) | 22 (3.1) | 139 (19.7) | 146 (20.6) | — | — | — |
| Mean (SD) | — | — | — | — | — | — | — | — | — | — | — | — | 3.05 (3.02) | 1.74 (2.16) | 3.06 (2.91) |
All correlations among diagnoses are tetrachoric correlations. Correlations greater than |.07| are significant at the .05 level; correlations greater than |.10| are significant at the .01 level. For gender, 0 = female, 1 = male. N = number of participants qualifying for a diagnosis.
The two-factor model provided an excellent fit to the data (χ2(24) = 28.24, p = .35; CFI = .99; RMSEA = .01; WRMR = .86). The factor loadings from the two-factor configuration are presented in Table 2. A correlation between the internalizing and externalizing factors of .46 indicated moderate overlap between the two latent constructs. All factor loadings on both dimensions were significant at an alpha level of .01.
Table 2. Factor Loadings of Axis I Syndromes on the Internalizing and Externalizing Factors of the Hierarchical-Spectrum Model.
| Internalizing |
Externalizing |
|
|---|---|---|
| Major Depression | .73 | — |
| Dysthymia | .52 | — |
| Generalized Anxiety Disorder | .76 | — |
| Panic Disorder | .61 | — |
| Social Phobia | .43 | — |
| Specific Phobia | .31 | — |
| Post-Traumatic Stress Disorder | .65 | — |
| Alcohol Abuse/Dependence | — | .75 |
| Drug Abuse/Dependence | — | .80 |
| Conduct Disorder | — | .60 |
| Oppositional Defiant Disorder | — | .57 |
All factor loadings are significant at the .01 alpha level.
The attempt to fit the three-factor model resulted in a Heywood case (i.e., out of range parameter estimate). Specifically, the factor loading of the fear dimension on the superordinate internalizing dimension was found to be greater than 1.0. Exploratory analyses omitting the higher-order internalizing dimension revealed that the correlation between the fear and anxious-misery dimensions was extremely high (r = .97). A LRT indicated that this factor correlation did not significantly differ from unity (χ2(1) = 0.56, p = .45). Given that the two internalizing subfactors in the three-factor model could not be reliably differentiated in the current sample, the two-factor model was used in subsequent analyses to test stress generation hypotheses.
HSM Dimensions, Syndrome-Specific Components, and Stress Generation
Independent Stress
In the baseline model, independent stress load was regressed on internalizing, externalizing, gender, and chronic stress. This model fit the data extremely well (χ2(32) = 32.48, p = .44; CFI = .99; RMSEA = .01; WRMR = .82)2. Gender was significantly related to internalizing (r = −.30) and externalizing (r = .19) in expected directions, with males averaging higher scores on externalizing and lower scores on internalizing. In addition, chronic stress was strongly associated with both the internalizing (r = .35) and externalizing (r = .49) dimensions. As summarized in Table 3, the internalizing and externalizing dimensions were not significantly related to independent stress occurrence in the past 12 months. Next, independent stress was regressed on the residual variances of each of the syndromes of the HSM. This model also provided a good fit to the observed data (χ2(26) = 26.14, p = .45; CFI = .99; RMSEA = .01; WRMR = .75)2. Analyses revealed that none of the residual associations with independent stress were significant (ps > .05).
Table 3. Regression of Stress on Latent Internalizing and Externalizing Dimensions and Specific Syndromes.
| Interpersonal Dependent Stress |
Noninterpersonal Dependent Stress |
Independent Stress |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Predictors | b | SE | β | b | SE | β | b | SE | β |
| Latent Dimensions | |||||||||
| Internalizing | 0.76 | 0.25 | .29** | −0.07 | 0.13 | −.03 | 0.17 | 0.23 | .06 |
| Externalizing | 0.32 | 0.34 | .09 | 0.43 | 0.21 | .17* | 0.37 | 0.33 | .10 |
| Syndrome-Specific Components | |||||||||
| Major Depression | 0.49 | 0.16 | .24** | −0.10 | 0.14 | −.07 | 0.31 | 0.23 | .15 |
| Dysthymia | 0.18 | 0.17 | .07 | 0.25 | 0.10 | .13* | 0.32 | 0.19 | .11 |
| Generalized Anxiety Disorder | 0.06 | 0.21 | .03 | 0.13 | 0.19 | .09 | −0.14 | 0.24 | −.07 |
| Panic Disorder | −0.76 | 0.34 | −.21* | 0.13 | 0.27 | .07 | −0.43 | 0.30 | −.16 |
| Social Phobia | −0.25 | 0.18 | −.09 | −0.07 | 0.12 | −.04 | 0.03 | 0.18 | .01 |
| Specific Phobia | 0.23 | 0.17 | .08 | 0.01 | 0.14 | .01 | 0.04 | 0.17 | .01 |
| Post-Traumatic Stress Disorder | 0.36 | 0.21 | .15 | −0.09 | 0.17 | −.05 | 0.03 | 0.22 | .01 |
| Alcohol Abuse/Dependence | 0.16 | 0.15 | .08 | 0.04 | 0.26 | .01 | 0.23 | 0.14 | .12 |
| Drug Abuse/Dependence | 0.14 | 0.16 | .07 | 0.46 | 0.28 | .15 | −0.01 | 0.15 | −.01 |
| Conduct Disorder | −0.30 | 0.43 | −.11 | 0.09 | 0.23 | .04 | −0.02 | 0.26 | −.01 |
| Oppositional Defiant Disorder | 0.08 | 0.31 | .03 | 0.02 | 0.12 | .01 | 0.02 | 0.39 | .02 |
| Gender | −0.24 | 0.31 | −.04 | 0.38 | 0.23 | .09 | −0.59 | 0.32 | −.10 |
| Chronic Stress | −0.10 | 0.07 | −.07 | 0.14 | 0.04 | .14** | 0.07 | 0.05 | .07 |
For gender, female = 0, male = 1.
p < .05.
p < .01.
Separate models were estimated for each class of stress.
Interpersonal Dependent Stress
Consistent with hypotheses, the regression of dependent stress on the transdiagnostic dimensions revealed a significant effect for the internalizing dimension after partialling out its covariance with externalizing, gender, and chronic stress. Higher scores on the internalizing dimension were associated with greater generation of interpersonal dependent stress (b = 0.76, SE = 0.25, p < .01, β = 0.29). In contrast, the externalizing dimension was not significantly associated with interpersonal dependent stress.
Even after removing variance due to the internalizing dimension, both major depression and panic disorder were related to future interpersonal dependent stress (see Table 3). As hypothesized, the presence of prior depression predicted an increase in interpersonal stress during the 12 months before the age 20 assessment (b = 0.49, SE = 0.16, p < .01, β = 0.24). Interestingly, panic disorder was inversely related to interpersonal stress (b = −0.76, SE = 0.34, p < .05, β = −0.21). This is an example of a suppressor effect (Cohen & Cohen, 1983), given that the zero-order association between panic disorder and interpersonal stress was small and positive (r = .03). Thus, it appears that the variance shared between panic disorder and the other internalizing disorders obscured the moderate negative association between panic disorder and interpersonal stress occurrence.
Noninterpersonal Dependent Stress
Standing on the externalizing, but not internalizing, dimension was positively associated with noninterpersonal dependent stress (b = 0.43, SE = 0.21, p < .05, β = 0.17). In fact, after partialling out its association with externalizing, internalizing was weakly negatively related with noninterpersonal dependent stress in this model. After controlling for these effects, gender was not significantly related to stress exposure, although males tended to experience higher levels of noninterpersonal dependent stress. Chronic stress was positively associated with the occurrence of later noninterpersonal dependent stress (b = 0.14, SE = 0.04, p < .01, β = 0.14).
As presented in Table 3, analyses examining the predictive power of specific syndromes, after partialling out variance due to the transdiagnostic factors, revealed that dysthymia was associated with increased noninterpersonal dependent stress (b = 0.25, SE = 0.10, p < .05, β = 0.13). No other internalizing or externalizing syndromes demonstrated unique effects on noninterpersonal dependent stress3.
Discussion
The present study proposed to expand stress generation theory to include the complementary stress generating effects of (a) transdiagnostic internalizing and externalizing dimensions of psychopathology and (b) distinct Axis I syndromes. Even after controlling for gender and chronic stress levels, both the internalizing and externalizing dimensions were found to play a role in stress generation, supporting the hypothesis that stress generation is not a specific feature of any one diagnostic category. At the same time, after accounting for variance due to the latent dimensions, several syndromes continued to predict dependent stress levels, indicating that diagnostic boundaries in our current nosologies capture unique clinical information that may be necessary for a complete understanding of stress generation patterns.
The internalizing and externalizing dimensions were implicated in the generation of different types of stressful events. The internalizing dimension predicted levels of interpersonal, but not noninterpersonal, dependent stress. This result is consistent with separate lines of research demonstrating that neuroticism is a nonspecific vulnerability factor for depressive and anxiety disorders (Clark & Watson, 1991) and that elevated neuroticism predicts higher levels of interpersonal dependent stress (e.g., Kercher et al., 2009). Additionally, this finding is in agreement with previous life stress research that has found depression to be most strongly associated with the generation of interpersonal conflict events, as compared to noninterpersonal dependent or independent stressors (Hammen, 2006).
The observation of a stress generation effect for the internalizing dimension raises the possibility that the relationship between depression and interpersonal stress generation may simply be a marker of a more general connection between a transdiagnostic internalizing trait and interpersonal stress generation. However, results also revealed that the specific component of major depression predicted increased rates of interpersonal conflict stress above and beyond the effect of the internalizing dimension. This residual association indicates that some set of attributes unique to depression (e.g., excessive reassurance seeking [Prinstein et al., 2005], negative feedback seeking [Joiner, 1995], hopelessness [Abramson, Metalsky, & Alloy, 1989], and/or co-rumination [Rose, 2002]) promotes conflict in interpersonal relationships. Indeed, the development of depression in adolescents and adults has been linked most robustly to interpersonal disruption and loss events, as compared to noninterpersonal stressful events (see Joiner & Coyne, 1999; Rudolph et al., 2000). The current investigation extends this previous empirical work by clarifying that the transdiagnostic internalizing dimension does not completely account for interpersonal dysfunction characterizing depression; some unique vulnerability associated with the depression syndrome further increases risk for conflictual interpersonal encounters.
The unique component of panic disorder also had a significant effect on subsequent interpersonal dependent stress. Despite a non-negative zero-order correlation between panic disorder and interpersonal dependent stress, panic disorder was significantly inversely related to interpersonal dependent stress after partialling out variance due to the internalizing dimension. Thus, the covariance between panic disorder and the other internalizing syndromes masked its true role in the stress generation process (cf. Brown, Chorpita, & Barlow, 1998). Specifically, panic disorder appears to produce a “stress inhibition” effect, such that the presence of this syndrome reduces rates of interpersonal conflict events.
It is possible that the unique elements of panic disorder reflect an avoidance of autonomic arousal (Kircanski, Craske, Epstein, & Wittchen, 2009). Anxiety sensitivity, or the belief that anxiety and related physical sensations are dangerous, has been linked theoretically and empirically to panic disorder (Reiss et al., 1986) and may account in part for its relationship with interpersonal conflict stress in the current study. Due to the somatic arousal accompanying interpersonal conflict events, individuals with elevated anxiety sensitivity may experience arguments and controversy as particularly alarming and threatening. Thus, potentially due to its overlap with the anxiety sensitivity construct, the unique element of panic disorder may cause individuals to actively avoid discord within relationships and thus create a buffer from interpersonal dependent stress.
Noninterpersonal dependent stress was related to individual differences on the externalizing, but not internalizing, dimension. Higher externalizing scores predicted subsequent elevations in noninterpersonal stress levels, with no evidence that any syndrome-specific components of the substance use and disruptive behavior disorders had an incremental stress generating effect. This result supports a more extensive incorporation of externalizing disorders into stress generation theory. To date, only a limited number of studies has examined the contribution of externalizing pathology to the stress generation effect (Carter et al., 2006; Rudolph et al., 2000). Consistent with the current results, when noninterpersonal and interpersonal stressors have been distinguished in past research, externalizing symptoms have been shown to predict an excess of noninterpersonal dependent stress only (Rudolph, 2008).
Although the latent internalizing dimension did not have a significant impact on noninterpersonal dependent stress, dysthymia was associated with elevations in noninterpersonal dependent stress once variance shared with the internalizing factor was removed. Given that the specific component of dysthymia was independent of variance shared with major depression, it could be speculated that this specific component represents attributes distinctive to chronic, mild depressive conditions. In support of a unique connection between chronic depression and stress generation, recent large-scale studies have reported that chronic (i.e., duration greater than 2 years), relative to nonchronic, depressions are associated with higher rates of unemployment, medical illness, hospitalizations, and suicide attempts (Gilmer et al., 2005; Satyanarayana, Enns, Cox, & Sareen, 2009). Indicating that chronic depression may confer vulnerability to noninterpersonal stress occurrence in particular, additional studies have reported that occupational and financial functioning may be especially impaired among those with chronic depressions, relative to those experiencing a single depressive episode (e.g., DeLisio et al., 1986), possibly due to a failure to achieve key vocational milestones (Evans et al., 1996). Given that much of the prior research on the stress generating effects of depressive disorders has not distinguished between major depression and dysthymia (Liu & Alloy, 2010), our findings underscore the importance of comparing the stress generation patterns of these two disorders, especially with respect to the types of stressful life events precipitated by major depression versus dysthymia.
Implications for Stress Generation Research
By integrating the HSM and stress generation theory, the current study provides a blueprint for a hierarchical model of stress generation in which the superordinate transdiagnostic level is distinguished from the subordinate syndrome level. This hierarchical model illuminates the general and specific influences of internalizing and externalizing syndromes on exposure to diverse classes of stressful life events. It is hoped that this model may enhance the efficiency of future stress generation research, which might otherwise be difficult to design or interpret due to high rates of comorbidity among mental disorders. That is, in most representative samples, the presence of comorbidity can undercut claims that a particular disorder (e.g., major depression) caused a stress generation effect due to the possibility that stress generation was attributable, at least in part, to one or more co-occurring syndromes. On the other hand, recruiting participants who manifest only one disorder (e.g., pure cases of major depression) ensures that effects are attributable to the disorder of interest, but, owing to the relative infrequency of pure cases, the results may not generalize to the entire population of individuals qualifying for this disorder. The present model circumvents this dilemma by distinguishing the shared and specific components of mental disorders in relation to stress generation.
The validity of the hierarchical model is supported by its ability to accommodate prior theory and empirical findings in the stress generation literature. For example, recent studies have demonstrated that other internalizing syndromes besides depression produce a stress generation effect (e.g., Connolly et al., 2010). From an HSM perspective, this result is explained by the shared dependence of all internalizing syndromes on the latent internalizing dimension, which is in turn associated with interpersonal dependent stress. Moreover, the finding that comorbidity amplifies the stress generation effect (Harkness & Luther, 2001) is consistent with the hierarchical model. In this framework, the co-occurrence of multiple internalizing diagnoses within the same person indicates that this person possesses a higher level of the internalizing trait, relative to individuals with pure depression or no disorder (cf. Krueger & Finger, 2001).
In addition to organizing previous findings within a parsimonious theoretical framework, the hierarchical model may also elucidate new pathways to stress generation. That is, results from the current study indicate for the first time that the specific components of various internalizing syndromes may have unique effects on stress exposure. For example, after controlling for variance due to the internalizing spectrum, major depression, unlike all other disorders, predicted higher rates of interpersonal dependent stress. Further empirical work is needed to clarify the nature of the unique component of depression and identify the psychological mechanisms through which it affects stress generation. Additionally, this model revealed that the specific component of panic disorder produces a “stress inhibition” effect, whereby the presence of this diagnosis reduces exposure to interpersonal conflict.
The current findings with the HSM also suggest a number of directions for future stress generation research. First, results affirm that more empirical attention on the role of externalizing pathology in stress generation is needed. In particular, future work would benefit from a detailed investigation of potential differences in content between stressors generated primarily by internalizing versus externalizing pathology (e.g., Hammen, 2006). Second, the findings highlight the importance of differentiating between the anxiety disorders when examining patterns of stress generation. The current data suggest that panic disorder can be distinguished from other anxiety disorders with respect to the magnitude, and even direction, of its effects on stress generation. This may be a main reason that studies assessing anxiety symptoms globally (Joiner, Wingate, Gencoz, & Gencoz, 2005), or the physiological aspects of anxiety specifically (Wingate & Joiner, 2004), have failed to detect stress generation effects.
Limitations and Conclusions
A number of limitations of the current study should be borne in mind when interpreting the results. First, the coverage of Axis I diagnoses was incomplete. It is possible that when more infrequent and severe forms of pathology (e.g., bipolar and psychotic disorders) are incorporated into the HSM framework the number and/or nature of the latent dimensions may be altered. Along these lines, one previous investigation modeled the latent structure of an extensive array of Axis I and II symptoms and found evidence for internalizing and externalizing factors, in addition to factors representing thought disorder and pathological introversion (Markon, 2010).
Second, this study was conducted in a sample of young adults, who at age 20 had not completely passed through the periods of highest risk for many Axis I disorders (e.g., Kessler et al., 2003). Consequently, the prevalence of some of the diagnoses assessed in this study was likely lower than those that would be obtained from an older sample of adults. Nevertheless, model fitting procedures have identified a correlated internalizing-externalizing configuration of diagnoses in previous studies of adolescents and young adults (e.g., Griffith et al., 2010). Moreover, prior longitudinal HSM research has shown that these latent dimensions are highly stable over time (Fergusson et al., 2006; Vollebergh et al., 2001).
Third, due to the use of lifetime, as compared to current, diagnoses in these analyses, the time elapsed between disorder onset/offset and acute stress exposure varied across participants and diagnoses. Thus, while this study addresses the specificity of stress generation with regard to various Axis I syndromes, it does not address specificity with regard to the clinical course of these syndromes. In other words, the relative strength of stress generation effects in the premorbid, manifest psychopathology, and recovery/remission time periods remains unknown.
Fourth, it is acknowledged that there might be different patterns of stress generation in individuals at different stages of life (Rudolph & Hammen, 1999). For example, it is speculated that young adults may be particularly prone to stress generation as they are expected to make significant life changes by gaining geographic, emotional, and financial independence from family, establishing intimate relationships, and developing work and career paths. Individuals who are older and in more established and stable relationships, occupations, and housing situations may experience fewer life events, including those to which they have contributed (cf. Kendler et al., 2011). Further research is needed to explore differences in stress generation patterns in different life epochs.
Fifth, numerous syndrome-specific stress generation effects were estimated (see Table 3). Caution is therefore warranted in the interpretation of syndrome-specific stress generation results given the increased probability of Type I error, especially with regard to the less prevalent forms of psychopathology in this sample. Although the unique stress generating effect of MDD was highly significant, the corresponding effects for panic disorder and dysthymia were significant at the .05 alpha level and were thus more likely to be due to chance. Future replication studies in larger samples and more targeted research on the construct validity of the unique components of the syndromes studied here are recommended to evaluate the robustness of the current results.
Sixth, participants were oversampled for maternal depression. As a result, correlations among the internalizing disorders, or covariation between the latent internalizing and externalizing dimensions, may have differed from those typical of unselected samples. However, a two-factor model has been reported to provide acceptable fit to diagnostic intercorrelations in previous high-risk samples (Griffith et al., 2010; Krueger, 1999). Further, it is important to note that when the presence of maternal depression was entered into these models as a covariate, the pattern and significance of results was unaltered.
Finally, it is important to note some alternative methods for conceptualizing and quantifying stress occurrence. For instance, while stress generation analyses in the present study used total objective threat scores summed across events (Brown & Harris, 1978; Hammen, 1991), other studies have used a count of stressful events or the number of events reaching a particular threshold of severity. Further research on the most reasonable metric for characterizing acute event impact may be necessary. Additionally, although we controlled for chronic stress in all analyses, we were unable to explore the possibility that chronic stress mediates the association between disorder and acute stress. Certain chronic stressors (e.g., poor peer relationship quality) may come about as a direct result of disorder onset and, in turn, increase the likelihood of acute stress occurrence (e.g., major fights or disputes among friends). Generally, more longitudinal research is needed to disentangle the dynamic interactions between chronic stress, acute life events, and psychopathology.
In spite of these limitations, this study offers a significant contribution to theory on the relationship between stress and psychopathology. The integration of structural modeling of Axis I diagnoses with stress generation theory presents an opportunity for a hierarchical model of stress generation that has the flexibility to explain emerging findings and illuminate avenues for future stress generation research. Further empirical work is needed to evaluate the explanatory power of hierarchical models of stress generation in other samples and to examine the specific effects of clinical syndromes not studied here (e.g., eating disorders, psychotic disorders).
The present findings also have implications for the design and implementation of transdiagnostic psychotherapies (e.g., Barlow, Allen, & Choate, 2004; Mansell, Harvey, Watkins, & Shafran, 2009). The associations of the HSM dimensions with both interpersonal and noninterpersonal impairment—with standardized effect sizes in the small to medium range according to Cohen’s (1988) guidelines—support the validity of these overarching dimensions as targets of intervention. For instance, a one standard deviation increase in internalizing was associated with a 0.75 point increase on the interpersonal stress severity rating assigned by the objective rating team.
Clearly, treatments ameliorating the shared pathology of multiple disorders would be expected to enhance the efficiency of mental health service delivery (Barlow et al., 2004). At the same time, the present study provides a preliminary indication that transdiagnostic therapies may need to incorporate syndrome-specific interventions to be optimally effective in the treatment of certain disorders. For example, our results suggest that some unique pathology of MDD portends interpersonal problems. Indeed, a standard deviation increment in MDD-specific pathology predicted a full half point increase (on a 5-point scale) in the objective severity of interpersonal stress exposure. It is possible that a supplementary focus on interpersonal skills training and/or the elicitation and modification of interpersonal schemas would improve the efficacy of transdiagnostic treatments for individuals diagnosed with MDD. Statistical modeling of the HSM in future treatment outcome studies has the potential to address such hypotheses.
Acknowledgements
This research was supported by the National Health and Medical Research Council, the Mater Misericordiae Mother’s Hospital in Queensland, Australia, and the National Institute of Mental Health grant R01 MH52239. We thank Professor Jake Najman of the University of Queensland and MUSP colleagues William Bor, M.D., and Gail Williams, Ph.D. Special thanks to project coordinators Robyne LeBrocque, Cheri Dalton Comber, and Sascha Hardwicke. Finally, we appreciate the helpful feedback of Elizabeth Raposa and three anonymous reviewers on a previous version of this article.
Footnotes
Obsessive-compulsive disorder was initially included in model-fitting procedures, but because it did not load significantly on the internalizing factor (in the two-factor solution) or on either the anxious-misery or fear subfactors (in the three-factor solution) it was omitted from the final model.
Equivalent or superior levels of model fit were observed in the interpersonal dependent and noninterpersonal dependent stress models and will not be reported below. Complete fit statistics for all models are available from the first author upon request.
When maternal depression history was controlled, the pattern and significance of the findings from all three models were unaltered. Full results are available from the first author upon request.
References
- Abramson LY, Metalsky GI, Alloy LB. Hopelessness depression: A theory-based subtype of depression. Psychological Review. 1989;96:358–372. [Google Scholar]
- Achenbach TM. Manual for the Young Adult Self-Report and Young Adult Behavior Checklist. University of Vermont Department of Psychiatry; Burlington: 1997. [Google Scholar]
- Allen JL, Rapee RM. Are reported differences in life events for anxious children and controls due to comorbid disorders? Journal of Anxiety Disorders. 2009;23:511–518. doi: 10.1016/j.janxdis.2008.10.005. [DOI] [PubMed] [Google Scholar]
- Angold A, Costello EJ, Erkanli A. Comorbidity. Journal of Child Psychology and Psychiatry. 1999;40:57–87. [PubMed] [Google Scholar]
- Barlow DH, Allen LB, Choate ML. Toward a unified treatment for emotional disorders. Behavior Therapy. 2004;35:205–230. doi: 10.1016/j.beth.2016.11.005. [DOI] [PubMed] [Google Scholar]
- Bentler PM. Comparative fit indexes in structural models. Psychological Bulletin. 1990;107:238–246. doi: 10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- Blatt SJ, Zuroff DC. Interpersonal relatedness and self-definition: Two prototypes for depression. Clinical Psychology Review. 1992;12:527–562. [Google Scholar]
- Brown GW, Harris T. Social origins of depression: A Study of psychiatric disorder in women. Tavistock Publications; London, England: 1978. [Google Scholar]
- Brown TA, Chorpita BF, Barlow DH. Structural relationships among dimensions of the DSM-IV anxiety and mood disorders and dimensions of negative affect, positive affect, and autonomic arousal. Journal of Abnormal Psychology. 1998;107:179–192. doi: 10.1037//0021-843x.107.2.179. [DOI] [PubMed] [Google Scholar]
- Browne MW, Cudeck R. Alternative ways of assessing model fit. Testing Structural Equation Models. 1993;154:136–162. [Google Scholar]
- Caron C, Rutter M. Comorbidity in child psychopathology: Concepts, issues, and research strategies. Journal of Child Psychology and Psychiatry. 1991;32:1064–1080. doi: 10.1111/j.1469-7610.1991.tb00350.x. [DOI] [PubMed] [Google Scholar]
- Carter JS, Garber J, Ciesla JA, Cole DA. Modeling relations between hassles and internalizing and externalizing symptoms in adolescents: A four-year prospective study. Journal of Abnormal Psychology. 2006;115:428–442. doi: 10.1037/0021-843X.115.3.428. [DOI] [PubMed] [Google Scholar]
- Chou C-P, Bentler PM. Model modification in structural equation modeling by imposing constraints. Computational Statistics and Data Analysis. 2002;28:271–287. [Google Scholar]
- Chun CA, Cronkite RC, Moos RH. Stress generation in depressed patients and community controls. Journal of Social and Clinical Psychology. 2004;23:390–412. [Google Scholar]
- Clark LA, Watson D. Tripartite model of anxiety and depression: Psychometric evidence and taxonomic implications. Journal of Abnormal Psychology. 1991;100:316–336. doi: 10.1037//0021-843x.100.3.316. [DOI] [PubMed] [Google Scholar]
- Clark LA, Watson D, Reynolds S. Diagnosis and classification of psychopathology: Challenges to the current system and future directions. Annual Review of Psychology. 1995;46:121–153. doi: 10.1146/annurev.ps.46.020195.001005. [DOI] [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Erlbaum; Hillsdale, NJ: 1988. [Google Scholar]
- Cohen J, Cohen P. Applied multiple regression/correlation analysis for the behavioral sciences. 2nd ed. Erlbaum; Hillsdale, NI: 1983. [Google Scholar]
- Connolly NP, Eberhart NK, Hammen CL, Brennan PA. Specificity of Stress Generation: A Comparison of Adolescents with Depressive, Anxiety, and Comorbid Diagnoses. International Journal of Cognitive Therapy. 2010;3:368–379. doi: 10.1521/ijct.2010.3.4.368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coyne JC. Toward an interactional description of depression. Psychiatry: Journal for the Study of Interpersonal Processes. 1976;39:28–40. doi: 10.1080/00332747.1976.11023874. [DOI] [PubMed] [Google Scholar]
- Daley SE, Hammen C, Burge D, Davila J, Paley B, Lindberg N, Herzberg DS. Predictors of the generation of episodic stress: A longitudinal study of late adolescent women. Journal of Abnormal Psychology. 1997;106:251–259. doi: 10.1037//0021-843x.106.2.251. [DOI] [PubMed] [Google Scholar]
- Daley SE, Hammen C, Rao U. Predictors of first onset and recurrence of major depression in young women during the 5 years following high school graduation. Journal of Abnormal Psychology. 2000;109:525–533. [PubMed] [Google Scholar]
- De Lisio G, Maremmani I, Perugi G, Cassano GB, Deltito J, Akiskal HS. Impairment of work and leisure in depressed outpatients: A preliminary communication. Journal of Affective Disorders. 1986;10:79–84. doi: 10.1016/0165-0327(86)90029-7. [DOI] [PubMed] [Google Scholar]
- Eberhart N, Hammen C. Interpersonal predictors of stress generation. Personality and Social Psychology Bulletin. 2009;35:544–556. doi: 10.1177/0146167208329857. [DOI] [PubMed] [Google Scholar]
- Ellenbogen MA, Hodgins S. The impact of high neuroticism in parents of children’s psychosocial functioning in a population at high risk for major affective disorder: A family-environmental pathway of intergenerational risk. Development and Psychopathology. 2004;16:113–136. doi: 10.1017/s0954579404044438. [DOI] [PubMed] [Google Scholar]
- Evans S, Cloitre M, Kocsis JH, Keitner GI, Holzer CP, Gniwesch L. Social-vocational adjustment in unipolar mood disorders: Results of the DSM-IV field trial. Journal of Affective Disorders. 1996;2:73–80. doi: 10.1016/0165-0327(95)00045-3. [DOI] [PubMed] [Google Scholar]
- Fergusson DM, Horwood L, Boden JM. Structure of internalising symptoms in early adulthood. The British Journal of Psychiatry. 2006;189:540–546. doi: 10.1192/bjp.bp.106.022384. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders: Patient Edition (SCIDI/P. Version 2.0) New York State Psychiatric Institute; New York, NY: 1995. [Google Scholar]
- Gilmer WS, Trivedi MH, Rush AJ, Wisniewski SR, Luther J, Howland RH, Alpert J. Factors associated with chronic depressive episodes: A preliminary report from the STAR-D project. Acta Psychiatrica Scandinavica. 2005;112:425–433. doi: 10.1111/j.1600-0447.2005.00633.x. [DOI] [PubMed] [Google Scholar]
- Griffith JW, Zinbarg RE, Craske MG, Mineka S, Rose RD, Waters AM, Sutton JM. Neuroticism as a common dimension in the internalizing disorders. Psychological Medicine. 2010;40:1125–1136. doi: 10.1017/S0033291709991449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammen C. Generation of stress in the course of unipolar depression. Journal of Abnormal Psychology. 1991;100:555–561. doi: 10.1037//0021-843x.100.4.555. [DOI] [PubMed] [Google Scholar]
- Hammen C. The emergence of an interpersonal approach to depression. In: Joiner T, Coyne J, editors. The interactional nature of depression: Advances in interpersonal approaches. American Psychological Association Press; Washington, DC: 1999. pp. 21–35. [Google Scholar]
- Hammen C. Stress and depression. Annual Review of Clinical Psychology. 2005;1:293–319. doi: 10.1146/annurev.clinpsy.1.102803.143938. [DOI] [PubMed] [Google Scholar]
- Hammen C. Stress generation in depression: Reflections on origins, research, and future directions. Journal of Clinical Psychology. 2006;62:1065–1082. doi: 10.1002/jclp.20293. [DOI] [PubMed] [Google Scholar]
- Hammen CL, Burge D, Daley SE, Davila J, Paley B, Rudolph KD. Interpersonal attachment cognitions and prediction of symptomatic responses to interpersonal stress. Journal of Abnormal Psychology. 1995;104:436–443. [PubMed] [Google Scholar]
- Hammen C, Henry R, Daley SE. Depression and sensitization to stressors among young women as a function of childhood adversity. Journal of Consulting and Clinical Psychology. 2000;68:782–787. [PubMed] [Google Scholar]
- Hammen C, Kim EY, Eberhart NK, Brennan PA. Chronic and acute stress in the prediction of major depression in women. Depression and Anxiety. 2009;26:718–723. doi: 10.1002/da.20571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammen C, Shih J, Altman T, Brennan PA. Interpersonal impairment and the prediction of depressive symptoms in adolescent children of depressed and nondepressed mothers. Journal of the American Academy of Child and Adolescent Psychiatry. 2003;42:571–577. doi: 10.1097/01.CHI.0000046829.95464.E5. [DOI] [PubMed] [Google Scholar]
- Hankin BL, Kassel JD, Abela JRZ. Adult attachment dimensions and specificity of emotional distress symptoms: Prospective investigations of cognitive risk and interpersonal stress generation as mediating mechanisms. Personality and Social Psychology Bulletin. 2005;31:136–151. doi: 10.1177/0146167204271324. [DOI] [PubMed] [Google Scholar]
- Harkness KL, Luther J. Clinical risk factors for the generation of life events in major depression. Journal of Abnormal Psychology. 2001;110:564–572. doi: 10.1037//0021-843x.110.4.564. [DOI] [PubMed] [Google Scholar]
- Harkness KL, Monroe SM, Simons AD, Thase M. The generation of life events in recurrent and non-recurrent depression. Psychological Medicine. 1999;29:135–144. doi: 10.1017/s0033291798007752. [DOI] [PubMed] [Google Scholar]
- Joiner TE., Jr. The price of soliciting and receiving negative feedback: Self-verification theory as a vulnerability to depression theory. Journal of Abnormal Psychology. 1995;104:364–372. doi: 10.1037//0021-843x.104.2.364. [DOI] [PubMed] [Google Scholar]
- Joiner TE., Jr. In: The interactional nature of depression. Coyne J, editor. American Psychological Association; Washington, DC: 1999. [Google Scholar]
- Joiner TE, Jr., Wingate LR, Gencoz T, Gencoz F. Stress generation in depression: Three studies on its resilience, possible mechanism, and symptom specificity. Journal of Social and Clinical Psychology. 2005;24:236–253. [Google Scholar]
- Joiner TE, Jr., Wingate LR, Otamendi A. An interpersonal addendum to the hopelessness theory of depression: Hopelessness as a stress and depression generator. Journal of Social and Clinical Psychology. 2005;24:649–664. [Google Scholar]
- Keeping JD, Najman JM, Morrison J, Western JS, Andersen MJ, Williams GM. A prospective longitudinal study of social, psychological and obstetric factors in pregnancy: response rates and demographic characteristics of the 8556 respondents. BJOG: An International Journal of Obstetrics & Gynaecology. 1989;96:289–297. doi: 10.1111/j.1471-0528.1989.tb02388.x. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Eaves LJ, Loken EK, Pedersen NL, Middeldorp CM, Reynolds C, Gardner CO. The impact of environmental experiences on symptoms of anxiety and depression across the life span. Psychological Science. 2011;22:1343–1352. doi: 10.1177/0956797611417255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendler KS, Prescott CA, Myers J, Neale MC. The structure of genetic and environmental risk factors for common psychiatric and substance use disorders in men and women. Archives of General Psychiatry. 2003;60:929–937. doi: 10.1001/archpsyc.60.9.929. [DOI] [PubMed] [Google Scholar]
- Kercher A, Rapee RM. A test of a cognitive diathesis-stress generation pathway in early adolescent depression. Journal of Abnormal Child Psychology. 2009;37:845–855. doi: 10.1007/s10802-009-9315-3. [DOI] [PubMed] [Google Scholar]
- Kercher A, Rapee RM, Schniering CA. Neuroticism, life events and negative thoughts in the development of depression in adolescent girls. Journal of Abnormal Child Psychology. 2009;37:903–915. doi: 10.1007/s10802-009-9325-1. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Koretz D, Merikangas KR, Rush AJ, Wang PS. The epidemiology of major depressive disorder. Journal of the American Medical Association. 2003;289:3095–3105. doi: 10.1001/jama.289.23.3095. [DOI] [PubMed] [Google Scholar]
- Kircanski K, Craske MG, Epstein AM, Wittchen HJ. Subtypes of panic attacks: A critical review of the empirical literature. Depression and Anxiety. 2009;26:878–887. doi: 10.1002/da.20603. [DOI] [PubMed] [Google Scholar]
- Kramer MD, Krueger RF, Hicks BM. The role of internalizing and externalizing liability factors in accounting for gender differences in the prevalence of common psychopathological syndromes. Psychological Medicine. 2008;38:51–61. doi: 10.1017/S0033291707001572. [DOI] [PubMed] [Google Scholar]
- Krueger RF. The structure of common mental disorders. Archives of General Psychiatry. 1999;56:921–926. doi: 10.1001/archpsyc.56.10.921. [DOI] [PubMed] [Google Scholar]
- Krueger RF, Caspi A, Moffitt TE, Silva PA. The structure and stability of common mental disorders (DSM-III-R): A longitudinal-epidemiological study. Journal of Abnormal Psychology. 1998;107:216–227. doi: 10.1037//0021-843x.107.2.216. [DOI] [PubMed] [Google Scholar]
- Krueger RF, Finger MS. Using item response theory to understand comorbidity among anxiety and unipolar mood disorders. Psychological Assessment. 2001;13:140–151. [PubMed] [Google Scholar]
- Krueger RF, Markon KE. Reinterpreting comorbidity: A model-based approach to understanding and classifying psychopathology. Annual Review of Clinical Psychology. 2006;2:111–133. doi: 10.1146/annurev.clinpsy.2.022305.095213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krueger RF, Markon KE, Patrick CJ, Benning SD, Kramer MD. Linking antisocial behavior, substance use, and personality: An integrative quantitative model of the adult externalizing spectrum. Journal of Abnormal Psychology. 2007;116:645–666. doi: 10.1037/0021-843X.116.4.645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krueger RF, Piasecki TM. Toward a dimensional and psychometrically-informed approach to conceptualizing psychopathology. Behaviour Research and Therapy. 2002;40:485–499. doi: 10.1016/s0005-7967(02)00016-5. [DOI] [PubMed] [Google Scholar]
- Liu RT, Alloy LB. Stress generation in depression: A systematic review of the empirical literature and recommendations for future study. Clinical Psychology Review. 2010;30:582–593. doi: 10.1016/j.cpr.2010.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mansell W, Harvey A, Watkins E, Shafran R. Conceptual foundations of the transdiagnostic approach to CBT. Journal of Cognitive Psychotherapy. 2009;23:6–19. [Google Scholar]
- Markon KE. How things fall apart: Understanding the nature of internalizing through its relationship with impairment. Journal of Abnormal Psychology. 2010;119:447–458. doi: 10.1037/a0019707. [DOI] [PubMed] [Google Scholar]
- Mickelson KD, Kessler RC, Shaver PR. Adult attachment in a nationally representative sample. Journal of Personality and Social Psychology. 1997;73:1092–1106. doi: 10.1037//0022-3514.73.5.1092. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus user’s guide. 5th ed. Author; Los Angeles, CA: 2007. [Google Scholar]
- Orvaschel H. Schedule for Affective Disorder and Schizophrenia for School-Age Children Epidemiologic version-5. Nova Southeastern University, Center for Psychological Studies; Ft. Lauderdale, FL: 1995. [Google Scholar]
- Patrick CJ, Bernat EM, Malone SM, Iacono WG, Krueger RF, McGue M. P300 amplitude as an indicator of externalizing in adolescent males. Psychophysiology. 2006;43:84–92. doi: 10.1111/j.1469-8986.2006.00376.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paykel ES, Cooper Z. Life events and social stress. In: Paykel ES, editor. Handbook of Affective Disorders. Guilford; New York: 1992. pp. 149–170. [Google Scholar]
- Prinstein MJ, Borelli JL, Cheah CSL, Simon VA, Aikins JW. Adolescent girls’ interpersonal vulnerability to depressive symptoms: A longitudinal examination of reassurance-seeking in peer relationships. Journal of Abnormal Psychology. 2005;114:676–688. doi: 10.1037/0021-843X.114.4.676. [DOI] [PubMed] [Google Scholar]
- Reinecke MA, Rogers GM. Dysfunctional attitudes and attachment style among clinically depressed adults. Behavioural & Cognitive Psychotherapy. 2001;29:129–141. [Google Scholar]
- Reiss S, Peterson RA, Gursky DM, McNally RJ. Anxiety sensitivity, anxiety frequency and the prediction of fearfulness. Behavior Research and Therapy. 1986;24:1–8. doi: 10.1016/0005-7967(86)90143-9. [DOI] [PubMed] [Google Scholar]
- Riskind JH, Black D, Shahar G. Cognitive vulnerability to anxiety in the stress generation process: Interaction between the looming cognitive style and anxiety sensitivity. Journal of Anxiety Disorders. 2010;24:124–128. doi: 10.1016/j.janxdis.2009.09.007. [DOI] [PubMed] [Google Scholar]
- Rose AJ. Co-Rumination in the friendships of girls and boys. Child Development. 2002;73:1830–1843. doi: 10.1111/1467-8624.00509. [DOI] [PubMed] [Google Scholar]
- Rudolph KD. Developmental influences on interpersonal stress generation in depressed youth. Journal of Abnormal Psychology. 2008;117:673–679. doi: 10.1037/0021-843X.117.3.673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rudolph KD, Hammen C. Age and gender as determinants of stress exposure, generation, and reactions in youngsters: A transactional perspective. Child Development. 1999;70:660–677. doi: 10.1111/1467-8624.00048. [DOI] [PubMed] [Google Scholar]
- Rudolph KD, Hammen C, Burge D, Lindberg N, Herzberg D, Daley SE. Toward an interpersonal life-stress model of depression: The developmental context of stress generation. Development and Psychopathology. 2000;12:215–234. doi: 10.1017/s0954579400002066. [DOI] [PubMed] [Google Scholar]
- Satyanarayana S, Enns MW, Cox BJ, Sareen J. Prevalence and correlates of chronic depression in the Canadian Community Health Survey: Mental health and well-being. Canadian Journal of Psychiatry. 2009;54:389–398. doi: 10.1177/070674370905400606. [DOI] [PubMed] [Google Scholar]
- Shih JH. Sex differences in stress generation: An examination of sociotropy/autonomy, stress, and depressive symptoms. Personality and Social Psychology Bulletin. 2006;32:434–446. doi: 10.1177/0146167205282739. [DOI] [PubMed] [Google Scholar]
- Shih JH, Abela JRZ, Starrs C. Cognitive and interpersonal predictors of stress generation in cihldren of affectively ill parents. Journal of Abnormal Child Psychology. 2009;37:195–208. doi: 10.1007/s10802-008-9267-z. [DOI] [PubMed] [Google Scholar]
- Silva PA. The Dunedin Multidisciplinary Health and Development Study: A fifteen year longitudinal study. Paediatric and Perinatal Epidemiology. 1990;4:96–127. doi: 10.1111/j.1365-3016.1990.tb00621.x. [DOI] [PubMed] [Google Scholar]
- Vollebergh WAM, Iedema J, Bijl RV, de Graaf R, Smit F, Ormel J. The structure and stability of common mental disorders: The NEMESIS study. Archives of General Psychiatry. 2001;58:597–603. doi: 10.1001/archpsyc.58.6.597. [DOI] [PubMed] [Google Scholar]
- Watson D. Rethinking the mood and anxiety disorders: A quantitative hierarchical model for DSM-V. Journal of Abnormal Psychology. 2005;114:522–536. doi: 10.1037/0021-843X.114.4.522. [DOI] [PubMed] [Google Scholar]
- Wingate LR, Joiner TE., Jr. Depression-related stress generation: A longitudinal study of black adolescents. Behavior Therapy. 2004;35:247–261. [Google Scholar]
- Wolf EJ, Miller MW, Krueger RF, Lyons MJ, Tsuang MT, Koenen KC. Posttraumatic stress disorder and the genetic structure of comorbidity. Journal of Abnormal Psychology. 2010;119:320–330. doi: 10.1037/a0019035. [DOI] [PMC free article] [PubMed] [Google Scholar]