Abstract
Background
Over 550,000 sinus surgeries are performed annually in the United States on patients with chronic rhinosinusitis (CRS). Although the results of sinus surgery vary widely, no known genetic factor has been identified to predict surgical outcomes. The bitter taste receptor T2R38 has recently been demonstrated to regulate upper airway innate defense and may affect patient responses to therapy. Our goal was to determine whether TAS2R38 genetics predicts outcomes in CRS patients following sinus surgery.
Methods
A prospective study of patients undergoing sinus surgery evaluating postoperative outcomes through the 22-item Sino-Nasal Outcome Test (SNOT-22). Patients were genotyped for TAS2R38.
Results
A total of 123 patients with CRS were initially analyzed; 82 patients showed nasal polyps (CRSwNP) and 41 patients were without nasal polyps (CRSsNP). Six months a er surgery, the overall SNOT-22 improvement was 25 ± 23 points. The TAS2R38 genotype was found to significantly correlate with surgical outcomes in patients without polyps; homozygotes for the functional receptor had a mean improvement of 38 ± 21, whereas heterozygotes or homozygotes for the nonfunctional receptor had a mean improvement of 12 ± 22 (p = 0.006). This result was confirmed with a multivariate regression that incorporated further patients with 1-month and 3-month scores (n = 207).
Conclusion
In patients undergoing sinus surgery for CRS, we have identified a genetic polymorphism that predicts variability in quality of life improvement following surgery at 6 months in nonpolypoid CRS. This is the first genetic polymorphism identified that has demonstrated to predict surgical outcome for a select group of CRS patients.
Keywords: sinusitis, FESS, SNOT-22, biofilm, biomarker, quality of life, sinus surgery, taste buds, polymorphism, genetic
Chronic rhinosinusitis (CRS) affects more than 35 million Americans, with annual direct costs in excess of $8 billion in the United States alone, and accounts for 1 in 5 antibiotic prescriptions in adults.1–5 Patients with CRS have significant decrements in quality of life (QOL) both in disease-specific areas and in general health. In fact, patients requiring sinus surgery demonstrate worse scores for physical pain and social functioning than those suffering from chronic obstructive pulmonary disease, congestive heart failure, or angina.6
Over 550,000 CRS patients who do not respond to medical therapy choose functional endoscopic sinus surgery (FESS) for treatment. Although most patients show considerable postoperative improvement following FESS, approximately 25% of patients continue to suffer from CRS symptoms.7 Currently, we do not understand why, nor can we predict which patients will have persistent symptoms. Thus, if biomarkers can be identified that correlate with surgical success rates, they could be used to counsel patients toward improvements in outcomes.
We have recently demonstrated that the bitter taste receptor T2R38 is expressed in ciliated cells of the human upper airway and is activated by acyl-homoserine lactones (AHLs): quorum-sensing molecules secreted by Pseudomonas aeruginosa and other gram-negative bacteria.8 Furthermore, we found that T2R38 regulates human upper airway innate defenses through nitric oxide (NO) production, which stimulates mucociliary clearance and has direct antibacterial effects.8 Moreover, common polymorphisms of the TAS2R38 gene, correlating with taste sensitivity to the bitter molecule phenylthiocarbamide (PTC), are linked to significant differences in the ability of upper respiratory cells to clear and kill bacteria in response to AHLs.8 There are 2 common forms of T2R38 protein depending on the amino acid residues at positions 49, 262, and 296; the functional form of the receptor contains a proline, alanine, and valine (PAV), whereas the nonfunctional form of the receptor contains alanine, valine and isoleucine (AVI) at these respective positions. Thus, the active haplotype in this context is called PAV, and the inactive haplotype is called AVI. These 2 common haplotypes generate 3 common genotypes (PAV/PAV, PAV/AVI, and AVI/AVI), which follow near classic Mendelian genetics with a respective 20%, 50%, 30% population distribution.9 Further supporting the contribution of T2R38 to upper airway innate immunity, 2 recent clinical reports show that patients homozygous for the functional TAS2R38 allele (PAV) are less likely to develop CRS necessitating FESS.10,11
CRS patients are often characterized on the presence or absence of nasal polyps. Although the etiology of nasal polyps has not been determined, they tend to appear in patients with asthma, allergies, aspirin sensitivity syndrome, and eosinophilia, and may affect surgical outcomes, although the literature on this is conflicted.7,12,13
To date, no prior studies have showed a compelling genetic linkage to sinus surgery outcomes. We investigated whether the TAS2R38 genotype and/or phenotype (assessed by a PTC taste test) correlated with clinical outcomes after FESS.
Patients and methods
Study population
We performed a prospective cohort study of adults (age > 18 years) undergoing sinus surgery at the Hospital of the University of Pennsylvania. Based on our in vitro studies using primary human sinonasal epithelial cells, which demonstrated a robust respiratory innate immune response in PAV/PAV cells but not PAV/AVI or AVI/AVI cells,8 patients for this study were divided into PAV/PAV and non–PAV/PAV cohorts. As a secondary analysis to examine the feasibility of phenotypic testing, the T2R38 gustatory phenotype was determined by a PTC taste sensitivity test, and patients were also divided into 2 cohorts based on taste-test score. There is no common classification scheme for phenotypic expression of PTC; thus, patients were divided into high-sensitivity and low-sensitivity groups with PTC taste-test scores either above or below the median.
The study protocol and inclusion/exclusion criteria have been published.11 In brief, participants met the guidelines for CRS outlined by the clinical practice guideline for adult sinusitis set forth by the Academy of Otolaryngology–Head and Neck Surgery14 who had failed medical therapy and were undergoing surgical intervention for the management of their disease. Exclusion criteria included overt altered sinonasal immunity, ie, known autoimmune dysfunction, immunodeficiency, or cystic fibrosis, as well as prior sinonasal trauma. The Institutional Committee on Research Involving Human Subjects approved the study protocol. All surgical procedures were performed by 4 fellowship-trained rhinologists.
The study was initially designed to incorporate patients who had outcomes scores available at 6 months. Our primary analysis was conducted with this patient population. However, data was also available for patients who did not show up to their 6-month follow-up visit, but had usable outcomes scores at 1 or 3 months. Although these patients lost to follow-up tended to have better 1-month and 3-month outcomes, neither genotype nor phenotype was a significant predictor of whether a patient would be lost. In order to increase the sample size and utilize all data available, all patients with usable outcomes scores at 1, 3, or 6 months were subsequently incorporated into our multivariate regression model. The analysis was conducted both with and without these patients. These could be incorporated seamlessly because a mixed-effects model designed for time-series data had been chosen.
Data collection
The preoperative evaluation included an in-person interview, a physical examination, and a chart review, all of which were conducted by rhinologists or trained researchers. Coexisting conditions were self-reported. Rhinologists conducted preoperative nasal endoscopy to document nasal polyp status. Preoperative computed tomography (CT) scans were used to assess disease severity, which was quantified by a Lund-Mackay score.15 The extent of surgery was tailored to an individual's disease by the surgeon's judgment.
Genotype/phenotype variables
Genomic DNA was isolated from sinonasal tissue removed during routine sinus surgery to determine the T2R38 genotype.8 For the secondary analysis, the T2R38 gustatory phenotype was determined by a taste test. During the preoperative assessment, consenting patients were asked to rate the bitterness intensity of PTC (180 mM) (a taste ligand of the T2R38 receptor), as well as other bitter agonists (denatonium benzoate [1.8 mM] and quinine HCL [56 mM]), and 2 compounds unrelated to bitter perception (sucrose [0.35 M] and sodium chloride [0.25M]). The latter solutions were included to establish that these patients did not have poorer overall taste function than the general population (also see Cowart et al.16). Taste intensity for each solution was rated on a 13-point Likert scale with all compounds being presented twice and the mean rating determined. Patients were unaware of the composition of each solution, and were not told their T2R38 phenotype and genotype. Physicians were not present for the taste test, and were blind to all genotypes and phenotypes. Because polyps were a potential confounder, patients were subdivided into CRSwNP and CRSsNP groups for analysis.
Outcome variables
The primary outcome was subjective improvement in symptoms from sinonasal disease at 6 months, measured with the 22-item Sino-Nasal Outcome Test (SNOT-22), a validated QOL survey of the severity of nasal disease symptoms that patients have experienced over the preceding 2 weeks.17 Each of the 22 questions about sinonasal symptoms was rated 0 to 5 on a Likert scale, for a total score between 0 and 110. Improvement in QOL at 6 months has been shown to correlate with long-term success from sinus surgery.18 The SNOT-22 score was also obtained at 1 and 3 months post-surgery.
Statistical analysis
Descriptive statistics were used to analyze baseline characteristics. Effects of T2R38 phenotype and genotype on SNOT-22 score are presented as the total improvement at 6 months. Student t tests were used to compare the improvement between groups. Because CRS symptoms and, therefore, the SNOT-22 scores, are prone to fluctuation, a mixed-effects, generalized-least-squares multivariate regression model was also constructed to determine change between preoperative scores and all available postoperative scores at 1, 3, and 6 months. All patients with a SNOT-22 score were incorporated into this model; it was not limited to patients with scores at 6 months. Genotype, age, gender, race, and any significant variables (p < 0.05) on analysis of outcomes were also incorporated into the model. The model finally allowed for interaction between genotype and polyp status. All statistical analysis was performed using STATA/IC 13.0 software (Stata Corporation, College Station, TX).
Results
Patients
A total of 123 patients with outcomes available at 6 months were initially enrolled in the study. After genetic analysis (after surgery was complete) 27 of these were PAV/PAV diplotypes, and the remaining 96 had other diplotypes, including PAV/AVI, AVI/AVI, and genotypes containing rare haplotypes (such as AAV and PVI).
Eighty-three patients that had been lost to follow-up for their 6-month visit, yet had data from their 1-month or 3-month postoperative visit, were subsequently incorporated to make a total of 207 patients. This population was used in our final multivariate regression. Forty of these were PAV/PAV diplotypes, and the remaining 167 had other diplotypes.
Phenotype (taste testing) was available for 147 patients; the median PTC score was 5.5 (standard deviation [SD], 3.8; range, 0–12). The high-sensitivity cohort contained 70 patients, and the low-sensitivity contained 77 patients.
PAV/PAV patients had similar baseline characteristics to other patients (Table 1), except that in the full sample of 207 patients, PAV/PAV patients were significantly less likely to be undergoing primary surgery (15% vs 34%; p = 0.02), as previously reported,10 and had higher baseline SNOT scores (51 ± 22 vs 42 ± 20; p = 0.01). Not surprisingly, PAV/PAV patients also had significantly higher PTC taste scores (8.0 vs 4.5; p < 0.0001); there were no associations with control taste tests. In addition, a higher percentage of PAV/PAV patients had allergic fungal sinusitis (AFS) (28% of PAV/PAV patients vs 14% of non–PAV/PAV, p = 0.06).
TABLE 1.
Baseline characteristics of patients based on TAS2R38 genotype*
| PAV/AVI or AVI/AVI (n = 167) | PAV/PAV (n = 40) | p | |
|---|---|---|---|
| Gender | |||
| Male, n (%) | 98 (59) | 22 (55) | 0.72 |
| Age | |||
| Age at surgery (years) | 49 ±13 | 51 ± 12 | 0.35 |
| Ethnicitya | |||
| White, n (%) | 151 (90) | 33 (83) | 0.17 |
| Hispanic, n (%) | 2 (1) | 0 (0) | |
| Asian, n (%) | 0 (0) | 1 (3) | |
| Black, n (%) | 14 (8) | 6 (15) | |
| Preoperative characteristics | |||
| Current or former smoker, n (%) | 59 (37) | 14 (37) | 1.00 |
| Polyps, n (%) | 112 (67) | 30 (75) | 0.45 |
| Asthma, n (%) | 90 (54) | 25 (63) | 0.38 |
| Allergies, n (%) | 26 (65) | 113 (67) | 0.85 |
| Aspirin sensitivity, n (%) | 21 (13) | 8 (20) | 0.22 |
| Diabetes, n (%) | 17 (10) | 2 (5) | 0.54 |
| Allergic fungal sinusitis, n (%) | 23 (14) | 11 (28) | 0.06 |
| Primary surgery, n (%) | 56 (34) | 6 (15) | 0.02 |
| Lund-Mackay score | 13 ± 6 | 14 ± 5 | 0.48 |
| Initial SNOT score | 42 ± 20 | 51 ± 22 | 0.01 |
| Taste sensitivityb | |||
| PTC | 5 ± 4 | 8 ± 3 | <0.0001 |
| Quinine | 4 ± 3 | 3 ± 2 | 0.23 |
| Denatonium | 5 ± 3 | 4 ± 3 | 0.90 |
| Sucrose | 6 ± 2 | 6 ± 2 | 0.41 |
Results are shown for all 207 patients used in the study. There were no significant differences in the baseline characteristics of the initial 123 patients used for the study when analyzed by genotype (data not shown; p = 0.21 for primary surgery; p = 0.17 for initial SNOT score). Plus-minus values are means ± SD. Values of p are for the overall comparisons.
Ethnicity is self-reported; p value is for white vs non-white.
For taste tests, participants rated the taste intensity of solutions of the bitter agonists PTC, quinine, and denatonium, as well as sucrose.
AVI = nonfunctional receptor haplotype containing alanine, valine and isoleucine; PAV = functional receptor haplotype containing proline, alanine, and valine; PTC = phenylthiocarbamide; SD = standard deviation; SNOT = Sino-Nasal Outcome Test.
Primary outcome
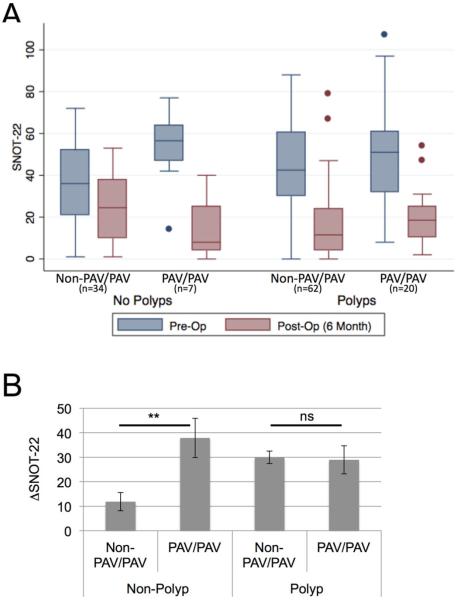
Among patients with 6-month outcomes, PAV/PAV patients (n = 27) demonstrated a mean QOL improvement of 31 ± 25, whereas the other patients (PAV/AVI, AVI/AVI, and other rare genotypes) (n = 96) had mean improvement of 24 ± 22 (p = 0.13). When patients were divided by the presence or absence of nasal polyps, nonpolypoid PAV/PAV patients (n = 7) had significantly better outcomes, with a mean improvement of 38 ± 21 vs a mean improvement of 12 ± 22 for the nonpolypoid non–PAV/PAV patients (n = 34) (p = 0.006) (Table 2, Fig. 1). However, in the patients with nasal polyps, the mean improvement was roughly equivalent in PAV/PAV (n = 20) and non–PAV/PAV (n = 62) patients (Fig. 1). The 1-month and 3-month SNOT-22 scores showed similar improvements from baseline to the 6-month scores (p = 0.0002 and 0.07, respectively). Nasal polyposis patients also had more favorable outcomes than nonpolypoid patients (p = 0.002); however, no other variables examined, including asthma, preoperative CT score and demographic variables, significantly predicted favorable outcomes in the full cohort, the polyposis cohort, or the nonpolypoid cohort.
TABLE 2.
Mean change between preoperative and postoperative (6-month) SNOT-22 scores*
| All patients (n = 123) | Polyp patients (n = 82) | Nonpolypoid patients (n = 41) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| n | Mean ± SD change | p | n | Mean ± SD change | p | n | Mean ± SD change | p | |
| All patients | 123 | 25 ± 23 | 82 | 30 ± 21 | 0.002 | 41 | 16 ± 24 | 0.002 | |
| Genotype | |||||||||
| Non-PAV | 96 | 24 ± 22 | 0.13 | 62 | 30 ± 20 | 0.85 | 34 | 12 ± 22 | 0.006 |
| PAV/PAV | 27 | 31 ± 25 | 20 | 29 ± 26 | 7 | 38 ± 21 | |||
| Taste sensitivitya | |||||||||
| PTC <5.5 | 41 | 25 ± 24 | 0.53 | 29 | 33 ± 19 | 0.80 | 12 | 4 ± 21 | 0.03 |
| PTC ≥5.5 | 54 | 28 ± 23 | 34 | 31 ± 24 | 20 | 21 ± 20 | |||
| Denatonium <4 | 34 | 27 ± 25 | 0.97 | 28 | 31 ± 23 | 0.76 | 6 | 5 ± 22 | 0.20 |
| Denatonium ≥4 | 62 | 26 ± 22 | 36 | 33 ± 21 | 26 | 17 ± 21 | |||
| Quinine <3 | 42 | 28 ± 25 | 0.45 | 29 | 34 ± 24 | 0.68 | 13 | 16 ± 23 | 0.89 |
| Quinine ≥3 | 54 | 25 ± 22 | 35 | 31 ± 20 | 19 | 14 ± 21 | |||
| Sucrose <6 | 43 | 25 ± 24 | 0.46 | 30 | 29 ± 23 | 0.27 | 13 | 14 ± 25 | 0.86 |
| Sucrose ≥6 | 53 | 28 ± 22 | 34 | 35 ± 20 | 19 | 16 ± 20 | |||
| Other variables | |||||||||
| Female gender | 50 | 24 ± 24 | 0.6 | 26 | 34 ± 23 | 0.20 | 12.9 | 19.9 ± 13 | 0.272 |
| Male gender | 73 | 26 ± 22 | 56 | 28 ± 20 | 21.2 | 28 ± 21 | |||
| White | 111 | 24 ± 23 | 0.09 | 71 | 29 ± 22 | 0.25 | 16.0 | 24 ± 16 | |
| Non-white | 12 | 36 ± 20 | 11 | 37 ± 21 | |||||
| Age less than 50 years | 45 | 30 ± 21 | 0.07 | 35 | 33 ± 21 | 0.22 | 20.1 | 20 ± 20 | 0.566 |
| Age 50 years or greater | 78 | 22 ± 24 | 47 | 27 ± 22 | 15.1 | 25 ± 15 | |||
| Never smoked | 76 | 24 ± 20 | 0.35 | 54 | 28 ± 18 | 0.33 | 13.5 | 22.0 ± 14 | 0.368 |
| Current or former smoker | 43 | 28 ± 26 | 26 | 34 ± 27 | 20.2 | 24 ± 20 | |||
| Asthma | 72 | 27 ± 20 | 0.39 | 58 | 29 ± 19 | 0.60 | 17.9 | 21 ± 18 | 0.757 |
| No asthma | 51 | 23 ± 27 | 24 | 32 ± 27 | 15.5 | 25 ± 16 | |||
| ASA | 18 | 35 ± 20 | 0.06 | 18 | 35 ± 20 | 0.28 | 16.3 | ||
| No ASA | 105 | 23.6 ± 23 | 64 | 28 ± 22 | |||||
| Diabetes | 15 | 26 ± 18 | 0.79 | 10 | 31 ± 18 | 0.89 | 19.0 | 17 ± 19 | 0.790 |
| No diabetes | 108 | 25 ± 24 | 72 | 30 ± 22 | 15.9 | 25 ± 16 | |||
| No AFS | 98 | 25 ± 23 | 0.91 | 58 | 31 ± 22 | 0.60 | |||
| AFS | 25 | 26 ± 23 | 24 | 28 ± 21 | |||||
| Primary surgery | 32 | 22 ± 25 | 0.42 | 17 | 24 ± 25 | 0.18 | 21.3 | 26 ± 21 | 0.314 |
| Revision surgery | 91 | 26 ± 22 | 65 | 31 ± 20 | 13.5 | 22 ± 14 | </TB> | ||
Values of p show whether each variable affects the difference between the preoperative and postoperative 6-month SNOT-22 scores.
For each taste sensitivity test, patients were categorized as having a taste intensity above or below the median score for the overall population (5.5, 4, 3, and 6, respectively, for PTC, denatonium, quinine, and sucrose).
AFS = allergic fungal sinusitis; ASA = acetylsalicylic acid; PAV = functional receptor haplotype containing proline, alanine, and valine; PTC = phenylthiocarbamide; SD = standard deviation; SNOT = Sino-Nasal Outcome Test.
FIGURE 1.
(A) Pre-Op and Post-Op (6 months) quality of life assessment of patients undergoing functional endoscopic sinus surgery as a function of polyp status and TAS2R38 genotype. Patients were classified based on the presence or absence of nasal polyps and subsequently genotyped for the TAS2R38. Patients were divided into PAV/PAV or non–PAV/PAV diplotype (AVI/AVI, PAV/AVI or rare haplotypes). (B) Pre-Op and Post-Op (6 months) quality of life assessment of patients undergoing functional endoscopic sinus surgery as a function of polyp status and TAS2R38 genotype. Surgical outcomes as measured by the change in quality of life (SNOT-22: pre-post). In nonpolypoid patients TAS2R38 genotype significantly correlates with favorable vs suboptimal outcomes (**p < 0.01). AVI = nonfunctional receptor haplotype containing alanine, valine and isoleucine; ns = not significant; PAV = functional receptor haplotype containing proline, alanine, and valine; Post-Op = postoperative; Pre-Op = preoperative; SNOT-22 = 22-item Sino-Nasal Outcome Test.
The mixed-model multivariate regression examined predictors of improvement for all scores at 1, 3, and 6 months (n = 207). This model allowed us to examine all 207 patients that met inclusion criteria, instead of only the 123 patients with outcomes available at 6 months. All variables that were found to significantly affect outcomes were included in the model, as well as age, gender, and race. A significant interaction term was included to account for the observed interaction between polyp status and genotype (p = 0.007). Nonpolypoid PAV/PAV patients had a mean improvement 20 points greater on average than nonpolypoid non–PAV/PAV patients (95% confidence interval [CI], 8 to 32) (Table 3). In addition, patients with polyps improved 14 points more on average than patients without polyps (95% CI, 8 to 20). Age, gender, and race were also included in the model but were not found to significantly associate with surgical outcomes.
TABLE 3.
Multivariate mixed model regression of factors associated with increased SNOT improvement in all patients undergoing sinus surgery for CRS*
| Analysis by genotype (n = 207) | SNOT improvementa | 95% CI | P |
|---|---|---|---|
| PAV genotype | 20 | 8 to 32 | 0.001 |
| Polyps | 14 | 8 to 20 | <0.001 |
| Interaction: genotype/polyps | 0.007 | ||
| Male gender | 1 | −4 to 7 | 0.65 |
| White | −4 | −12 to 5 | 0.36 |
| Age ≥50 years | −3 | −8 to 2 | 0.23 |
Results were likewise significant for the 123 initial patients in the study (p < 0.001 For a difference based on PAV genotype, polyps, and the interaction term). Bole values of p are significant.
Mixed-effects, generalized-least-squares multivariate regression model for change between preoperative SNOT-22 score and postoperative scores at 1, 3, and 6 months. Genotype, age, gender, race/ethnicity, and any significant variables (p < 0.05) on analysis of outcomes were incorporated, as well as an interaction term between genotype and polyp status.
CI = confidence interval; CRS = chronic rhinosinusitis; PAV = functional receptor naplotype containing proline, alanine, and valine; SNOT-22 = 22-item Sino-Nasal Outcome Test.
Secondary analysis
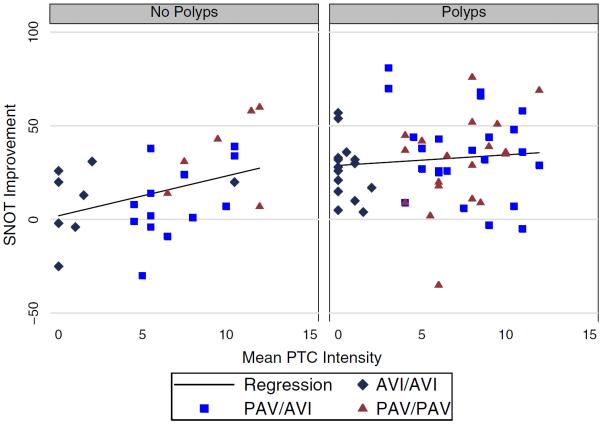
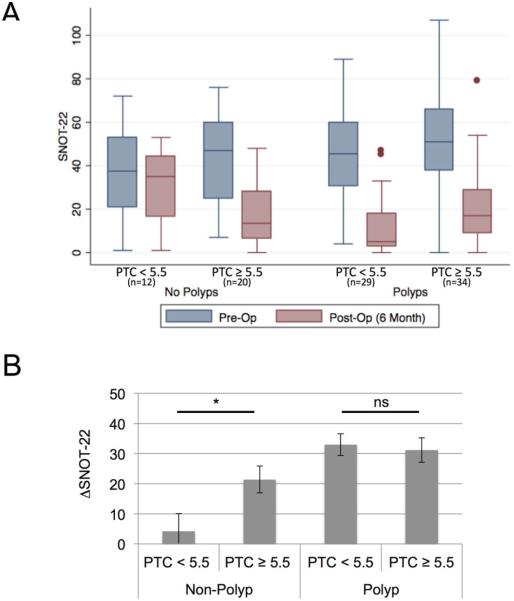
Among nonpolypoid patients, taste sensitivity to PTC was found to significantly correlate with outcomes, with a significant correlation evinced between higher taste scores and greater improvement (p = 0.03, R2 = 0.15) (Fig. 2). The more bitter PTC was perceived, the more favorable the surgical outcome (Fig. 2). In the context of a diagnostic measure, we divided patients into PTC high sensitivity (PTC score ≥5.5) or low sensitivity (<5.5). In the nonpolypoid CRS group the PTC high-sensitivity patients (n = 12) had a mean QOL improvement of 21 ± 20, whereas patients with low PTC sensitivity (n = 21) had a mean improvement of 4 ± 21 (p = 0.03) (Table 2, Figs. 2 and 3). In addition, sensitivity to the 2 bitter taste controls, as well as the other taste controls, had no association with outcomes (Table 2). Outcomes at 1 and 3 months by phenotype were again similar to those at 6 months (p = 0.02 and 0.13, respectively).
FIGURE 2.
Correlation between improvement in quality of life and score on bitter taste test. There is a signification correlation only in nonpolypoid patients (p = 0.03, R2 = 0.15; for polyp patients, p = 0.45 and R2 = 0.01). Only subjects with both a taste test and T2R38 genotype are included in the graphic. AVI = nonfunctional receptor haplotype containing alanine, valine and isoleucine; ns = not significant; PAV = functional receptor haplotype containing proline, alanine, and valine; PTC = phenylthiocarbamide; SNOT-22 = 22-item Sino-Nasal Outcome Test.
FIGURE 3.
(A) Pre-Op and Post-Op (6 months) quality of life assessment of patients undergoing functional endoscopic sinus surgery as a function of polyp status and PTC taste sensitivity. Patients were classified based on the presence or absence of nasal polyps and were asked to rate the bitterness of the PTC with a taste test on a scale of 0 to 12. Patients were characterized as sensitive to PTC (≥5) or insensitive (<5). (B) Pre-Op and Post-Op (6 months) quality of life assessment of patients undergoing functional endoscopic sinus surgery as a function of polyp status and PTC taste sensitivity. Surgical outcomes as measured by the change in quality of life assessment (SNOT-22: pre-post) based on PTC sensitivity and polyp status. In nonpolypoid patients TAS2R38 taste sensitivity to PTC significantly correlates with favorable vs suboptimal outcomes (*p < 0.05). ns = not significant; PAV = functional receptor haplotype containing proline, alanine, and valine; Post-Op = postoperative; Pre-Op = preoperative; PTC = phenylthiocarbamide; SNOT-22 = 22-item Sino-Nasal Outcome Test.
Discussion
CRS is a complex disease process estimated to affect 14% to 16% of the population. Patients are typically treated with 4 to 6 weeks of medical therapy that consists of topical and/or systemic steroids, sinonasal lavage, and culture-directed antibiotics.19 Those patients with persistent symptoms are offered FESS with the goal of ventilating the sinuses, which often restores normal mucociliary clearance and has positive QOL outcomes.7 There are certain well-known characteristics that minimize postsurgical improvement, including history of sinonasal autoimmune disease, diseases affecting ciliary function (primary ciliary dyskinesia, cystic fibrosis), Samter's triad, and AFS. Aside from these comorbid risk factors, there are as yet no known genetic associations contributing to disease manifestation and outcomes. Our data demonstrate that in patients with CRSsNP, TAS2R38 genotype is predictive of surgical outcomes. Nonpolypoid patients who are PAV/PAV (and have a higher sensitivity to a known ligand for T2R38) show superior QOL outcomes. It should be stressed that all patient groups, regardless of T2R38 genotype, demonstrated improved outcomes, but the nonpolypoid PAV/PAV group had the greatest improvement.
Lee et al.,8 utilizing a primary human sinonasal epithelial cell culture model, demonstrated a novel pathway in which the bitter taste receptor T2R38, when activated by bacterial quorum sensing molecules, stimulates production of epithelial NO, which results in acceleration of mucociliary clearance as well as has direct bactericidal activity against organisms in the airway mucus. These defensive responses were further shown to be governed by genotype, with the PAV/PAV receptor yielding robust generation of NO whereas the PAV/AVI or AVI/AVI forms yielded minimal NO production.
Recent studies by Adappa et al.10,11 showed that the prevalence of homozygotes for the functional T2R38 receptor (PAV/PAV) in CRS patients undergoing primary FESS was significantly lower than its prevalence in the general population, suggesting that individuals homozygous for the functional T2R38 receptor variant may have a lower incidence of CRS failing medical therapy and require less frequent sinus surgery.
Although this prior work demonstrated a skewed population distribution, with fewer than expected PAV/PAV patients failing medical therapy and progressing to surgical intervention, the correlation of the T2R38 genotype with surgical outcomes has not been previously investigated. For the vast majority of CRS patients (>75%), FESS provides improved QOL.7 The challenge for clinicians is to set realistic expectations for patients and discuss the degree of improvement likely to be experienced following standard sinus surgery.
This study shows a statistically significant association of TAS2R38 genotype and phenotype with surgical outcomes as measured by symptom improvement using the SNOT-22 in CRSsNP patients at their 6-month follow-up appointment. Prior work has demonstrated that improvement at 6 months following surgery is predictive of long-term outcomes.20 By identification of a genotype and, even more so, a phenotype (taste sensitivity to PTC), we are able to provide physicians and patients preoperative expectations of long-term outcomes from standard FESS. Our study of 207 CRS surgical patients demonstrates that by using the conventional polyp/nonpolypoid categorization and further dividing patients based on TAS2R38 genotype, we can stratify the degree of QOL improvement following standard FESS. Furthermore, because the taste test may more accurately reflect the functional receptor in the heterozygote population, taste testing may prove to be more informative than genotyping.
This study has several broad implications. First, from an investigational standpoint, these results demonstrate a discrete genetic polymorphism that contributes to QOL improvement following sinus surgery. Second, from a clinical standpoint, knowledge of a patient's TAS2R38 genotype, or the more easily assessed phenotype, may help stratify expectations regarding degree of QOL improvement following standard sinus surgery. Despite these implications, questions still exist as to optimal management; ie, will the non–PAV/PAV nonpolypoid patients benefit from more aggressive surgery (modified Lothrop, endoscopic medial maxillectomy, etc.)? Based on our investigation, T2R38 does not appear to play a role in outcomes in CRS patients with nasal polyps because all groups independent of T2R38 genotype demonstrated similar robust QOL improvement. However, in the nonpolypoid CRS group, although both the PAV/PAV and the non–PAV/PAV cohorts demonstrate clinically significant QOL improvement (which has been defined as a change of ≥0.50 of a SD of the baseline score; in our case, this was >10.5 points for all patients and >9.5 points for non–PAV/PAV nonpolypoid patients),20 the PAV/PAV cohort demonstrate a statistically significant greater QOL improvement (mean improvement of 38 points) compared to the nonpolypoid non–PAV/PAV cohort (mean improvement of 12 points) (p = 0.006).
This study further supports the notion that CRSwNP and CRSsNP are 2 distinct pathophysiologic entities. Additionally, it is interesting to note that in the nonpolypoid disease, the PAV/PAV patients had worse preoperative QOL scores. This may reflect that these patients have an additional defect in innate immunity which when exploited by the disease process may present with more severe symptoms.
One interesting finding was the higher percentage of PAV/PAV patients with AFS. We are unsure of the etiology; it is possible that the mechanism for AFS may override any protective benefit of the PAV/PAV phenotype, and so a higher percentage of the PAV/PAV patients requiring surgery have AFS, or conversely PAV/PAV may be protective for some forms of CRS but leave the individual vulnerable in other forms of CRS (such as AFS) because the haplotype is a balanced polymorphism, which argues for some evolutionary protection resulting from both forms of the allele.
The main limitations of this study are sample size and duration of follow-up. We have included 123 patients with only 41 being CRSsNP for whom we have 6-month outcomes data. To account for the reduced sample size, as well as to account for fluctuations in the SNOT-22 score, we included patients with outcomes scores at 1 and 3 months but not at 6 months in the mixed-methods regression (n = 84 patients with 24 being CRSsNP). The generalized-least-squares, mixed-model multivariate model allowed us to make this calculation in time-series data. Patient follow-up was also an issue because our institution is a tertiary care center and patients often travel a great distance for surgical intervention: in general we are subject to bias in our sample in that those who do well tend to “drop off” in follow-up. Despite this, we have obtained 6-month follow-up data that has been shown to correlate with long-term data.21
Additionally, surgical outcomes are highly multifactorial; it is inherently difficult to isolate the effect of 1 variable. We have attempted to address this limitation by including as many possible confounders in our statistical analysis. Nonetheless, it is important to note that other potential modifiers of this effect, such as the microbiology present in the sinuses at the time of surgery, and variability in the technique of individual surgeons, were not addressed in this study.
Moreover, PAV/PAV patients did have a higher preoperative SNOT-22 scores, and were more often revision patients. Although the higher starting score may give the patients more room for improvement on their SNOT-22 score, we believe it does not change the overall conclusion of the study: that nonpolypoid PAV/PAV patients showed a greater QOL improvement than non–PAV/PAV nonpolypoid patients. Further multi-institutional studies focusing on CRSsNP patients are necessary to corroborate our findings. Future studies on this finding will include other metrics for sinonasal surgery besides the SNOT-22, such as endoscopy scores and medication use, as well as other possible confounders of this affect, such as the bacterial culture present.
Conclusion
The T2R38 bitter taste receptor genotype predicts surgical outcomes in CRSsNP after FESS. Although all patients demonstrate postsurgical improvement, the PAV/PAV genotype appears to confer a protective mechanism that correlates with improved 6-month QOL outcomes compared to the other T2R38 genotypes (PAV/AVI and AVI/AVI) in nonpolypoid disease. Furthermore, PTC sensitivity shows an even greater correlation with standard FESS outcomes in this select population (nonpolypoid). T2R38 does not appear to correlate with outcomes in CRSwNP because both groups showed similar QOL improvement.
Acknowledgments
N.D.A. and N.A.C. from the University of Pennsylvania had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. D.F. from the University of Pennsylvania performed the data analysis.
Funding sources for the study: Grant from a philanthropic contribution from the RLG Foundation, Inc. (to N.A.C.); U.S. Public Health Service (R01DC013588 to N.A.C.; P30DC011735 to D.R.R.; R01DC004698 to D.R.R.).
Footnotes
Additional Supporting Information may be found in the online version of this article.
Potential conflict of interest: None provided.
References
- 1.Cherry DK, Woodwell DA. National Ambulatory Medical Care Survey: 2000 summary. Adv Data. 2002;328:1–32. [PubMed] [Google Scholar]
- 2.Blackwell DL, Collins JG, Coles R. Summary health statistics for U.S. adults: National Health Interview Survey, 1997. Vital Health Stat 10. 2002;(205):1–109. [PubMed] [Google Scholar]
- 3.Ray NF, Baraniuk JN, Thamer M, et al. Healthcare expenditures for sinusitis in 1996: contributions of asthma, rhinitis, and other airway disorders. J Allergy Clin Immunol. 1999;103:408–414. doi: 10.1016/s0091-6749(99)70464-1. [DOI] [PubMed] [Google Scholar]
- 4.Ly N, McCaig LF. National Hospital Ambulatory Medical Care Survey: 2000 outpatient department summary. Adv Data. 2002;327:1–27. [PubMed] [Google Scholar]
- 5.Bhattacharyya N, Orlandi RR, Grebner J, Martinson M. Cost burden of chronic rhinosinusitis: a claims-based study. Otolaryngol Head Neck Surg. 2011;144:440–445. doi: 10.1177/0194599810391852. [DOI] [PubMed] [Google Scholar]
- 6.Gliklich RE, Metson R. The health impact of chronic sinusitis in patients seeking otolaryngologic care. Otolaryngol Head Neck Surg. 1995;113:104–109. doi: 10.1016/S0194-59989570152-4. [DOI] [PubMed] [Google Scholar]
- 7.Smith TL, Litvack JR, Hwang PH, et al. Determinants of outcomes of sinus surgery: a multi-institutional prospective cohort study. Otolaryngol Head Neck Surg. 2010;142:55–63. doi: 10.1016/j.otohns.2009.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lee RJ, Xiong G, Kofonow JM, et al. T2R38 taste receptor polymorphisms underlie susceptibility to upper respiratory infection. J Clin Invest. 2012;122:4145–4159. doi: 10.1172/JCI64240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kim UK, Jorgenson E, Coon H, Leppert M, Risch N, Drayna D. Positional cloning of the human quantitative trait locus underlying taste sensitivity to phenylthiocarbamide. Science. 2003;299:1221–1225. doi: 10.1126/science.1080190. [DOI] [PubMed] [Google Scholar]
- 10.Adappa ND, Howland TJ, Palmer JN, et al. Genetics of the taste receptor T2R38 correlates with chronic rhinosinusitis necessitating surgical intervention. Int Forum Allergy Rhinol. 2013;3:84–87. doi: 10.1002/alr.21140. [DOI] [PubMed] [Google Scholar]
- 11.Adappa ND, Zhang Z, Palmer JN, et al. The bitter taste receptor T2R38 is an independent risk factor for chronic rhinosinusitis requiring sinus surgery. Int Forum Allergy Rhinol. 2014;4:3–7. doi: 10.1002/alr.21253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Deal RT, Kountakis SE. Significance of nasal polyps in chronic rhinosinusitis: symptoms and surgical outcomes. Laryngoscope. 2004;114:1932–1935. doi: 10.1097/01.mlg.0000147922.12228.1f. [DOI] [PubMed] [Google Scholar]
- 13.Poetker DM, Mendolia-Loffredo S, Smith TL. Outcomes of endoscopic sinus surgery for chronic rhinosinusitis associated with sinonasal polyposis. Am J Rhinol. 2007;21:84–88. doi: 10.2500/ajr.2007.21.2978. [DOI] [PubMed] [Google Scholar]
- 14.Rosenfeld RM, Andes D, Bhattacharyya N, et al. Clinical practice guideline: adult sinusitis. Otolaryngol Head Neck Surg. 2007;137:S1–S31. doi: 10.1016/j.otohns.2007.06.726. [DOI] [PubMed] [Google Scholar]
- 15.Lund VJ, Mackay IS. Staging in rhinosinusitus. Rhinology. 1993;31:183–184. [PubMed] [Google Scholar]
- 16.Cowart BJ, Young IM, Feldman RS, Lowry LD. Clinical disorders of smell and taste. Occup Med. 1997;12:465–483. [PubMed] [Google Scholar]
- 17.Hopkins C, Gillett S, Slack R, Lund VJ, Browne JP. Psychometric validity of the 22-item Sinonasal Outcome Test. Clin Otolaryngol. 2009;34:447–454. doi: 10.1111/j.1749-4486.2009.01995.x. [DOI] [PubMed] [Google Scholar]
- 18.Kennedy JL, Hubbard MA, Huyett P, Patrie JT, Borish L, Payne SC. Sino-nasal outcome test (SNOT-22): a predictor of postsurgical improvement in patients with chronic sinusitis. Ann Allergy Asthma Immunol. 2013;111:246–51. e2. doi: 10.1016/j.anai.2013.06.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fokkens WJ, Lund VJ, Mullol J, et al. EPOS 2012: European position paper on rhinosinusitis and nasal polyps 2012. A summary for otorhinolaryngologists. Rhinology. 2012;50:1–12. doi: 10.4193/Rhino12.000. [DOI] [PubMed] [Google Scholar]
- 20.Norman GR, Sloan JA, Wyrwich KW. Interpretation of changes in health-related quality of life: the remarkable universality of half a standard deviation. Med Care. 2003;41:582–592. doi: 10.1097/01.MLR.0000062554.74615.4C. [DOI] [PubMed] [Google Scholar]
- 21.Soler ZM, Smith TL. Quality-of-life outcomes after endoscopic sinus surgery: how long is long enough? Otolaryngol Head Neck Surg. 2010;143:621–625. doi: 10.1016/j.otohns.2010.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]