Abstract
This study evaluated the implications of the 2008 increase in age for sexual consent in Canada using a population health survey of Canadian adolescents. Government rationales for the increase asserted younger adolescents were more likely to experience sexual exploitation and engage in risky sexual behaviour than adolescents 16 and older. Using data from sexually experienced adolescents in the 2008 British Columbia Adolescent Health Survey (BC AHS, N=6,262; age range 12 – 19; 52% female), analyses documented the scope of first intercourse partners who were not within the ‘close in age’ exemptions, then compared sexual behaviours of younger teens (14 and 15 years) with older teens (16 and 17) navigating their first year of sexual activity. Comparisons included: forced sex, sex under the influence of alcohol or drugs, multiple partners, condom use, effective contraception use, self-reported sexually transmitted infections, and pregnancy involvement. Results showed very few 14- and 15-year-olds had first intercourse partners who were not within the ‘close in age’ exemptions based on age (boys: <2%, girls: 3–5%). In contrast, among 12- and 13-year-olds (a group unaffected by the law’s change) between 25% and 50% had first intercourse partners who were not within the ‘close in age’ exemptions, and almost 40% of teens who first had sex before age 12 reported a first partner age 20 years or more. In their first year of intercourse, 14- and 15-year-olds were slightly more likely to report forced sex and 3 or more partners than older teens, but otherwise made similarly healthy decisions. This study demonstrates the feasibility of evaluating policy using population health data and shows that better strategies are needed to protect children 13 and under from sexual abuse.
It is important that public policy be grounded in empirical evidence. Although ideally this takes place before laws or policies are enacted, it is not always possible; however, it is just as important to evaluate existing policy based on the best available information. Evidence-based policy analysis has been used over the years to evaluate a variety of health-related laws, including graduated driver licensing (Fohr, Layde & Guse, 2005; Wiggins, 2006), firearm restrictions, (Niederkrotenthaler et al, 2009; Shah, Hoffman, Wake & Marine, 2000), tobacco control (Luke, Stamatakis & Brownson, 2000), helmet laws (Robinson, 2006; Rodgers, 2002), and sexual health policy (Joyce, Kaestner & Colman, 2006). The effectiveness of a law or policy can be measured by the health outcomes of the population. This paper provides an evidence-based policy analysis of the 2008 change in Canada’s age of sexual consent law, using the federal government’s rationale to frame the evaluation.
The New Age of Sexual Consent
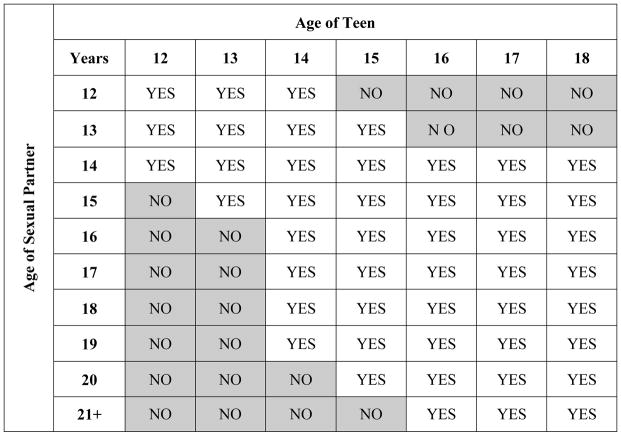
For more than 100 years, from 1892 to 2008, the legal age of sexual consent in Canada was 14. Consent in this context is the capacity to understand and agree to engage in partnered sexual activity (Sexuality Information and Education Council of Canada [SIECCAN], 2010). In 2006, Bill C-22 was put forward in Parliament, to take effect January 1, 2008, which raised the legal age of consent for non-exploitative sexual activity to 16. Eighteen remains the age of consent for anal intercourse and exploitative sexual activity, which includes prostitution, pornography, and situations where one individual is in a position of authority over the other individual. Bill C-22 outlined a “close in age” exception for younger adolescents, permitting 14-and 15-years-olds to be able to consent to non-exploitative sexual activity with individuals not more than 5 years older, and 12- and 13-year-olds to consent to non-exploitative sexual activity with adolescents not more than 2 years older (see Figure 1). In addition, neither partner can be under the influence of drugs or alcohol, as this impairs judgement and affects an individual’s ability to consent to sexual activity.
Figure 1.
Age of sexual consent in Canada as outlined in Bill C-22.
Note: Shaded areas show the ages in which older partners would be outside the range for “close in age” exemption; i.e., illegal.
The federal government passed Bill C-22 based on two key rationales: that younger adolescents are at greater risk of exploitation than older adolescents, especially when it comes to internet predators, and that younger adolescents lack the maturity needed to handle the responsibility of becoming sexually active, including making safe sexual health decisions (MacKay & Bédard, 2007). Lawmakers and law enforcers believed Bill C-22 would send a strong message to sex offenders, especially to internet predators from the U.S. who may persuade young adolescents to meet across the border. Lawmakers also suggested this law would have the positive outcome of not allowing 14- and 15-year-olds to be cross-examined during sexual assault trials, a process which can cause considerable distress (MacKay & Bédard, 2007). Section 151 of the Criminal Code of Canada now reads: “Every person who, for a sexual purpose, touches, directly or indirectly, with a part of the body or with an object, any part of the body of a person under the age of 16 years is guilty of an indictable offence…” (Criminal Code of Canada, 2008), indicating that adult offenders are the targets of this law, not consenting adolescents. The code also provides an additional clarification that “No person aged 12 or 13 years shall be tried for an offense under section 151 or 152.” (Section 150.1, Criminal Code of Canada).
Bill C-22 has been controversial. Most adolescents are not aware of legal issues, and may not understand what Bill C-22 means (Pearce, 2008). Critics suggested that this law is difficult to understand because of the “close in age” exceptions, which vary by age. Others asserted that “Age of Consent” is a misnomer for Bill C-22, as it implies all sexual intercourse under age 16 is illegal. Sexual health organizations and other groups who opposed raising the age of consent claimed this confusion might prevent adolescents from accessing information or resources on safer sex and sexual health (Black, 2006). Adolescents, believing they are breaking the law by engaging in sexual activity “below the age of consent,” may be reluctant to admit to this “illegal” activity by visiting sexual health clinics, and so may not get needed tests for sexually transmitted infections (STI) or pregnancy. Most adolescents do not know that they have the right to request and receive these services without disclosing the age of their partner (Wong, 2006).
Another issue is the inconsistency of the law compared to other laws. For example, a 14-year-old can be given an adult sentence in youth court for committing a theft, based on the belief that a 14-year-old can appreciate the consequences of his or her actions (Black, 2006), so these young adolescents legally have the maturity necessary to take responsibility for their actions in the case of theft, but not in the case of sex. Bill C-22 was also not in line with the age of consent for anal intercourse, which is 18. Some sexual health organizations argue this is discriminatory toward gay, lesbian and bisexual adolescents (Weber, 2006). In addition, laws already exist to protect adolescents from exploitative and/or non-consensual sexual activity (Picard, 2008) although these laws are only partially effective: sexual exploitation and sexual abuse still exist despite laws against them (MacKay & Bédard, 2007).
Was this Change Necessary? Evidence from Existing Literature
Age of sexual debut, sexual coercion, and sexual health decision-making of adolescents have received considerable attention in the research literature, although the strength of the evidence, especially in Canada, is limited. Some of the strongest evidence is from population studies in other countries. A longitudinal population-based study of Australian females, for example, found a strong association between early age at first intercourse, defined as younger than 16 years of age, and experiences of violence by young adulthood, even after controlling for socioeconomic status (Watson, Taft & Lee, 2007). This association was strongest for females who debuted earliest: adolescents initiating sexual activity at age 14 or younger were up to seven times more likely to have experienced partner violence than women who first had sex at a later age. Watson and colleagues hypothesized this may be in part because of the link between sexual abuse and re-victimization; in a New Zealand birth cohort, Dickson, Paul, Herbison & Silva (1998) found that younger debut was associated with abuse or coercion at first sexual intercourse.
Early sexual debut has been associated with a number of sexual health risks, including higher number of sexual partners, alcohol and drug use, lack of condom use, pregnancy, and STIs, although these results have been mixed, and drawn from correlational studies. For example, a cross-sectional survey of American adolescents found that adolescents who debuted younger than age 13 were at least nine times more likely to have had four or more lifetime sexual partners compared with adolescents debuting at 15 or older, with rates differing by gender and race (Coker, Richter, Valois, McKeown, Garrison & Vincent, 1994); these findings were replicated more recently in the U.S. by Sneed (2009). In Canada, however, the 2003 British Columbia Adolescent Health Survey (BC AHS) showed no difference across adolescent age groups for multiple partners in the past year (Saewyc, Homma, Taylor & Ogilvie, 2008). U.S. adolescents who reported early debut were also more likely to report having had alcohol or drugs prior to their last sexual intercourse (Coker et al., 1994; Sneed, 2009). In Canada, Saewyc et al. (2008) found gender differences in sex after alcohol or drug use: adolescent females age 12 to 14 years were more likely than adolescent females 17 and older to have had alcohol or drugs prior to their last sexual intercourse, but males demonstrated the opposite age effect.
Protective sexual health behaviours have also been explored in light of age of first sex, with mixed results. Coker et al. (1994) found that U.S. teens who debuted before age 13 years were half as likely to use condoms as adolescents who debuted at an older age. Manlove and colleagues (2005) found that males and females who first had sex younger than age 15 with an older partner were less likely than other sexually experienced adolescents to report having used contraceptives. However, Sneed (2009) found that 18-year-olds were less likely to report using a condom at latest intercourse compared to 16-year-olds, regardless of age at sexual debut. In the 2003 BC AHS, among females, condom use was highest among sexually active adolescents aged 12 to 14, and lowest among sexually active adolescents 17 and older, but this was complemented by a corresponding increase by age group of females reporting the use of birth control pills (Saewyc et al., 2008).
Potentially due to this lower condom use, American adolescents who first had sex before 13 years of age were more likely to report pregnancy involvement, and females (but not males) were more likely to report contracting an STI (Coker et al., 1994). Similarly, almost half of adolescent females who had sex before age 15 with an older male reported a teen birth compared with one quarter of other sexually experienced adolescent females (Manlove et al., 2005). In a US longitudinal study that included STI testing, earlier age of sexual debut was consistently associated with STI prevalence among adolescent males and females, but by young adulthood, the age at first intercourse no longer had an effect on STI prevalence (Kaestle, Halpern, Miller & Ford, 2005). This suggests that maturation eventually attenuates any effects of early sexual experience.
Limitations of Current Evidence in the Literature
Not only does the literature contain mixed findings around the impact of early sexual debut, with the greatest differences found between U.S. and Canadian studies, but there are additional limitations to the design of the studies. Most of the research does not control for a history of childhood sexual abuse, or sexual initiation that was a result of force or coercion, when evaluating the relationship between early sexual debut and negative outcomes; yet several studies have documented the link between childhood or adolescent sexual abuse and higher rates of risky sexual behaviours (see for example, Noll, Shank & Putnam, 2008; Saewyc, Pettingell & Magee, 2004; Saewyc et al., 2006). Studies which have taken pre-debut characteristics such as coercion or childhood maltreatment into account have found these attenuated the link between early debut and outcome variables (for example, Spriggs & Halpern, 2008). Likewise, while there is a considerable amount of research on females, there is not much evidence of the effect of early sexual debut on young men.
Another challenge is that research groups have defined “early sexual debut” differently. Cut offs range from 12 to 16 years of age, and may be based on law, a community’s mean age of sexual initiation, or biological maturity; however, it is far more common for researchers to provide no justification for the age chosen. The most common “early age of debut” is 13, which was illegal in Canada both before and after Bill C-22. Even more problematic is that, depending on types of sampling and analyses, the comparison of earlier and later age of first sex may actually conflate multiple reasons for the differences in behaviour. If one is comparing older and younger sexually active teens at the present moment, differences could be based on cohort effects, i.e., different norms among the groups at the time they are first starting to have sex, since older teens may have started at an earlier time when norms were slightly different. Alternately, those differences could be based on experiential effects, i.e., people with more experience have developed more skill to negotiate healthier choices. Analyses with such samples cannot differentiate these influences from maturational effects, i.e., that older teens have better judgment developmentally and make more mature decisions. Such a study requires comparing teens of different ages but similar time-spans and levels of experience since sexual debut, for example, assessing teens who have started having sex during the same time period, preferably recently. To our knowledge, no previous studies exploring the link between early debut and sexual health behaviours have focused on recently debuted adolescents only, despite indications that this could be useful (Kaestle et al., 2005).
Purpose of this Study
Given the limitations and mixed results of the evidence to date, especially the limited data from Canada, an updated, focused analysis of Canadian-based evidence to inform this change in the law is warranted. The purpose of this study was to test the rationales provided by the government for raising the age of consent, using population-based data from British Columbia. The specific aims included identifying the scope of the problem addressed, i.e., how many adolescents are potentially affected by this change in the law, and are younger teens developmentally less capable than older adolescents to navigate riskier and safer sexual behaviours, after controlling for the potential confounder of experience?
The rationales for the law guided our hypotheses.
We hypothesized that adolescents who first had sex at younger ages (before age 16) would be more likely to report an older sexual partner than older teens, especially one aged 20 or older.
We also expected that younger sexually experienced adolescents (those aged 14 and 15 years) when navigating their first year of sexual activity would be more likely than similarly-experienced older adolescents (aged 16 and 17) to report sexual abuse or coercion.
In terms of risky sexual behaviours and negative outcomes, we expected younger teens to be more likely than older teens to have had sex under the influence of alcohol or drugs, to have more sexual partners, to report an STI, and to be involved in a pregnancy.
When it comes to safer sexual behaviours, we hypothesized that younger adolescents would be less likely than older adolescents to use condoms or other barrier methods, or effective contraception the last time they had sexual intercourse.
Methods
This analysis draws on data from the British Columbia Adolescent Health Survey of 2008 (BC AHS) conducted by the McCreary Centre Society (Saewyc & Green, 2008; Smith, Stewart, Peled, Poon & Saewyc, 2009). The BC AHS is a cluster-stratified random survey of adolescent health and risk behaviours. Public school classrooms were randomly selected within each grade and region from participating school districts in BC (50 of 59 districts) to provide a provincially and regionally representative sample of grade 7 to 12 students (age 12 – 19). The survey consists of 147 items covering demographics, perceptions of current physical and emotional health, risky behaviours and experiences, and positive health behaviours. The anonymous surveys were administered by public health nurses and other trained personnel external to the school.
In the spring of 2008, more than 29,000 adolescents across BC completed the BC AHS. Participating school districts comprised 92% of high school students enrolled in BC, and the response rate averaged 67%. Data were weighted to adjust for the differential probability of sampling within regions and response rates, to ensure its representativeness. Further details about the methodology of the 2008 BC AHS are available elsewhere (Saewyc & Green, 2008).
Samples for this Study
We selected two subsets of students from the BC AHS for testing the aims of the policy analysis. First, we selected all sexually experienced adolescents (age 12 – 19), regardless of age or length of time they have been sexually active, who indicated their age at first sexual intercourse, and the age of their sexual partner (N=6,262; 52% female). This sample was used to test the hypotheses about the scope of adolescents affected, and age differences between partners at first intercourse.
Then we selected those adolescents who were 14 through 17 and who reported first sex at their same age, to compare younger adolescents (14- and 15-year-olds) with older adolescents (16- and 17-year-olds) who were within their first year of sexual intercourse. Adolescents were included regardless of sexual orientation, although the number of teens who identify as gay, lesbian, or bisexual is only 3% (Smith, et al., 2009). By focusing on recently experienced teens, we could rule out explanations for disparities in behaviours as due to increased experience or skills, as well as relationship length; healthy sexual decision-making, like most skills, can become easier with familiarity and practice. There were 321 younger and 362 older adolescent females, and 296 younger and 307 older adolescent males who were at the same age as when they reported first having sexual intercourse. Thus, each of the four groups of adolescents who were within their first year of sexual intercourse had approximately 300 adolescents.
Measures
Beyond questions about ever having sexual intercourse, age at first sexual intercourse, and the age of first sexual partner, the BC AHS asks several questions about both risky and safer sexual behaviours. These included lifetime experiences of forced intercourse by adults or by other youth, having unwanted sex in the past year because of alcohol or drug use, using alcohol or drugs before the latest episode of sexual intercourse, the number of sexual partners in the past year, as well as condom use or other contraceptive use at last intercourse, ever being diagnosed with an STI, or ever being pregnant or having caused a pregnancy. Most variables were dichotomous or were recoded to be dichotomous measures, based on the literature; for example, number of sexual partners in the past year was re-coded as 1 or 2 vs. 3 or more. Similarly, among the list of options for contraception at last intercourse, “effective” contraception included condoms, birth control pills, depo provera, the patch, the ring, diaphragm/contraceptive sponge, or IUD, vs. no methods, those that suggest lack of prior planning (emergency contraception), much less effective strategies (withdrawal), and “not sure.” It should be noted that sexual intercourse was not defined in the survey, so teens might be indicating either penile-vaginal intercourse or anal intercourse.
Analyses
Because differences in patterns of sexual behaviour between adolescent males and females have been extensively documented in research, analyses were conducted separately by gender. Analyses used SPSS Complex Samples version 18.0 to adjust for the complex stratified sampling, In order to examine the rates of illegal sexual activity as defined by Bill C-22, we characterized the first sexual experiences of students as “legal” or “illegal” based on student’s age and age of sexual partner at first intercourse. “Legal” was categorized as first sex which occurred at age 16 or older, or which occurred at age 14 or 15 with a partner less than 5 years older or less than 2 years younger, or which occurred at age 12 or 13 with a partner less than 2 years older. All other first sexual experiences were identified as “illegal,” except sexual debut before age 12 with a partner under age 13, as the law indicates no teens of these ages should be charged under the criminal sexual conduct sections (Section 150.1, Criminal Code of Canada).
The second set of analyses compared risky and safer sexual behaviours between younger and older groups. Rao-Scott chi-square tests, which are version of the Pearson chi-square test adjusted for complex sampling designs (Rao & Scott, 1981), and 95% confidence intervals were calculated.
Results
Fewer than 25% of adolescents in the 2008 BC AHS reported ever having sexual intercourse, with relatively equal rates of males and females. As would be expected, the number of adolescents who reported being sexually experienced increased with age for both genders (see Table 1 for estimated prevalence by age).
Table 1.
Estimated number of sexually experienced teens in British Columbia public schools by age, BC AHS 2008
| Age in Years | Percent Ever Had Sexual Intercourse | Estimated # Sexually Experienced Students* |
|---|---|---|
| 12 | 2.9% | 711 |
| 13 | 5.0% | 2,208 |
| 14 | 10.5% | 4,677 |
| 15 | 17.9% | 8,224 |
| 16 | 31.0% | 15,331 |
| 17 | 42.5% | 19,058 |
| 18 | 48.9% | 9,804 |
| 19+ | 44.3% | 668 |
Data weighted and scaled to 2008 enrollment in BC public schools grades 7–12, ~ 274,812 total
Prevalence of First Intercourse Partners outside the “Close in Age” Range by First Partner’s Age
Tables 2 and 3 report the percentage of individuals in each age group who would be potentially affected by Bill C-22, based on the age discrepancies of sexual partners at first intercourse. Before focusing on the adolescents most affected by the change in law (14 and 15 year olds) it is worth examining the experiences of those whose sexual debut was under age 14, so “illegal” to have sex with both before and after the law changed. Of those who had sexual intercourse under 12 years of age, 42.9% of males (Table 2) and 34.3% (Table 3) of females reported that their partner was also less than 13 years of age (according to the law, these teens would not be charged); however, 38.2% of adolescent boys and 39.4% of adolescent girls in this youngest age category reported that their partner was 20 or more years old. Of the students who reported first intercourse at age 12, 49.2% of girls (Table 3) and 25.3% of boys (Table 2) had a partner more than two years older (so outside the “close in age” exception under the change in law). Of the students who had first had sexual intercourse at 13 years of age, 15.7% of males (Table 2) and 35.9% of females (Table 3) had a partner who was more than 2 years older than them. However, contrary to our first hypothesis, i.e., that adolescents who first had sex at younger ages (before age 16) would be more likely to report a much older sexual partner, we found that more than 98% of 14- and 15-year-old males (Table 2) and more than 95% of 14- and 15-year-old females (Table 3) had engaged in sexual intercourse with “close-in-age” peers. Like their older counterparts, the majority of 14 and 15-year-olds first had sex with another teen who was within three years of their age.
Table 2.
Prevalence of partnered sexual intercourse by age among BC adolescent males (illegal pairings highlighted), BC AHS 2008
| Age at first intercourse | Age of partner at first intercourse | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Less than 13 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | 20 + | |
| Less than 12 | 42.9% | 2.8% | 3.1% | 3.8% | 3.4% | 3.0% | 2.1% | 0.4% | 38.2% |
| 12 years | 27.6% | 32.9% | 13.8% | 6.0% | 5.1% | 2.7% | 1.2% | 2.8% | 7.5% |
| 13 years | 1.4% | 48.2% | 22.8% | 11.9% | 6.0% | 3.1% | 2.1% | 1.1% | 3.4% |
| 14 years | 0.7% | 6.3% | 53.1% | 21.5% | 10.0% | 4.9% | 1.0% | 0.8% | 1.3% |
| 15 years | 0.3% | 0.9% | 12.6% | 54.4% | 19.8% | 6.3% | 2.4% | 1.6% | 1.6% |
| 16 years | 0.4% | 0.1% | 4.5% | 25.2% | 47.9% | 13.4% | 4.6% | 1.5% | 2.1% |
| 17 or more | 1.9% | 0.6% | 0.4% | 2.9% | 27.5% | 48.1% | 11.6% | 3.5% | 3.3% |
Table 3.
Prevalence of partnered sexual intercourse by age among BC adolescent females (illegal pairings highlighted), BC AHS 2008
| Age at first intercourse | Age of partner at first intercourse | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Less than 13 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | 20 + | |
| Less than 12 | 34.3% | 10.2% | 3.6% | 5.2% | 2.9% | 1.3% | 2.5% | 0.5% | 39.4% |
| 12 years | 10.8% | 24.4% | 15.7% | 14.0% | 12.4% | 7.0% | 3.7% | 3.2% | 8.9% |
| 13 years | 0.9% | 18.5% | 22.6% | 22.2% | 14.0% | 12.1% | 3.0% | 2.5% | 4.3% |
| 14 years | 0 | 1.1% | 16.9% | 24.7% | 23.2% | 20.5% | 7.1% | 3.7% | 2.8% |
| 15 years | 0 | 0.1% | 1.7% | 25.5% | 28.5% | 22.3% | 12.9% | 5.0% | 4.1% |
| 16 years | 0.1% | 0 | 0.1% | 5.2% | 32.2% | 28.8% | 16.8% | 7.7% | 8.8% |
| 17 or more | 0.5% | 0 | 0 | 0.8% | 5.8% | 40.0% | 19.5% | 15.3% | 18.1% |
With Bill C-22’s close in age stipulations, it is also possible for older teens to be engaging in sexual intercourse with teens who are younger than the law allows. Of those who first had sex at age 16, fewer than 1% of either males or females reported sexual intercourse with a partner too young for the “close-in-age” exemption. Among adolescents who debuted at 17 years of age and older, just under 3% of males and fewer than 1% of females had inappropriately younger sexual partners.
Are Younger Adolescents Developmentally at Greater Risk? Comparing Teens Within Their First Year of Sexual Intercourse
Comparisons of younger teens (14 and 15) who were within their first year of sexual intercourse with similarly-experienced older teens (16 and 17) on both sexual risk and health behaviours are reported for males and females in Tables 4 and 5.
Table 4.
Sexual health and risk behaviours among adolescent males, BC AHS 2008
| Sexual Behaviour | Younger males (14 & 15 years old) | Older males (16 & 17 years old) | p value* | ||
|---|---|---|---|---|---|
| % | 95% CI | % | 95% CI | ||
| Forced sex by another youth | 3.8 | 1.9 – 7.4 | 1.3 | 0.4 – 3.7 | p = .025 |
| Forced sex by an adult | 1.7 | 0.7 – 4.0 | 0.2 | 0 – 1.6 | |
| Unwanted sex in past year because of alcohol or drugs | 9.1 | 6.0 – 13.7 | 4.9 | 2.8 – 8.5 | p =.077 |
| Alcohol/drug use before last sex | 24.4 | 19.2 – 30.3 | 24.5 | 20.1 – 29.5 | p =.479 |
| 3 + sexual partners in past year | 17.9 | 13.7 – 23.0 | 8.6 | 5.7 – 12.7 | p =.02 |
| Condom used at last sex | 83.1 | 77.5 – 87.5 | 74.2 | 68.5 – 79.1 | p =.018 |
| Effective birth control at last sex** | 89.3 | 84.3 – 92.8 | 90.1 | 85.4 – 93.4 | p =.781 |
| Pregnancy involvement | 5.5 | 3.3 – 9.1 | 4.1 | 2.2 – 7.6 | p =.863 |
| Told had an STI | 2.3 | 1.0 – 5.1 | 0.2 | 0 – 1.6 | p =.009 |
The p-value is calculated from a variant of the second-order Rao-Scott adjusted chi-square test statistic, an adjusted F, and its degrees of freedom.
Among the 89.3% of younger males who reported effective birth control at last sex, 61.7% used condoms only, 5.2% used hormonal methods only, and 33.1% used dual methods; among the 90.1% of older males who reported effective birth control at last sex, 46.4% used condoms only, 19.6% used hormonal methods only, and 34.1% used dual methods.
Table 5.
Sexual health and risk behaviours among adolescent females, BC AHS 2008
| Sexual Behaviour | Younger females (14 & 15 years old) | Older females (16 & 17 years old) | p value* | ||
|---|---|---|---|---|---|
|
| |||||
| % | 95% CI | % | 95% CI | ||
| Forced sex by another youth
|
11.9 | 8.7 – 16.1 | 6.2 | 3.8 – 9.8 | p = .007 |
| Forced sex by an adult
|
3.9 | 2.1 – 7.1 | 1.1 | 0.4 – 3.5 | |
| Forced by both youth & adult | 0.3 | 0 – 1.8 | 0 | 0 | |
|
| |||||
| Unwanted sex in past year because of alcohol or drugs | 18.3 | 14.3 – 23.1 | 11.3 | 8.2 – 15.4 | p =.016 |
|
| |||||
| Alcohol/drug use before last sex | 27.3 | 22.4 – 32.9 | 22.6 | 18.4 – 27.4 | p =.311 |
|
| |||||
| 3 + sexual partners in past year | 8.5 | 5.8 – 12.3 | 3.8 | 2.4 – 6.0 | p =.007 |
|
| |||||
| Condom used at last sex | 70.4 | 64.7 – 75.5 | 74.9 | 69.0 – 80.1 | p =.248 |
|
| |||||
| Effective birth control at last sex** | 82.9 | 77.7 – 87.0 | 89.8 | 85.4 – 93.0 | p =.026 |
|
| |||||
| Pregnancy involvement | 5.3 | 3.1 – 9.0 | 0.9 | 0.2 – 3.6 | p =.032 |
|
| |||||
| Told had an STI | 2.1 | 0.9 – 4.9 | 1.9 | 0.9 – 4.1 | p =.846 |
The p-value is calculated from a variant of the second-order Rao-Scott adjusted chi-square test statistic, an adjusted F, and its degrees of freedom.
Among the 82.9% of younger females who reported effective birth control at last sex, 55.8% used condoms only, 12.3% used hormonal methods only, and 31.9% used dual methods; among the 90.1% of older females who reported effective birth control at last sex, 42.2% used condoms only, 15.8% used hormonal methods only, and 42.0% used dual methods.
Forced sex
Younger males were slightly more likely (5.5%) to report forced sexual intercourse in their lifetime than older males (1.5%) (Table 4), and younger females were more than twice as likely (16.1%) to report forced sex in their lifetime than older females (7.3%) (Table 5). While teens in each group were more likely to be forced by another youth rather than an adult, there was no significant difference between older or younger teens in whether they were forced by an adult or by another youth. A small percentage of females, but not males, reported having been forced by both a youth and an adult (Table 5).
Unwanted sex under the influence
There was no statistical differences between younger and older males in the percent who reported they had sex in the past year when they didn’t want to because of alcohol or drug use. However, younger females were significantly more likely to report having had unwanted sexual intercourse because of drug or alcohol use than were older females (18.3% vs. 11.3%), although the 95% confidence intervals of the estimates overlapped (Table 5).
Sex after alcohol or drug use
There was no significant difference between older and younger teens in the prevalence of sex under the influence of alcohol or drugs (Tables 4 and 5). One-quarter of both older and younger adolescents reported using alcohol or drugs before their most recent episode of sexual intercourse.
Number of sexual partners
The large majority of adolescent males and females had only one or two sexual partners in the past year. However, for both males and females, younger adolescents were significantly more likely to have had three or more sexual partners in the past year (17.9% males, 8.5% females) than older adolescents (8.6% males, 3.8% females).
As it was unclear whether the reason for younger teens’ greater number of partners could be due to their increased likelihood of forced intercourse, we re-ran analyses controlling for sexual abuse or forced intercourse. Among non-abused teens, younger males and females were still significantly more likely to have had multiple partners than their older peers (data not shown).
Condom use and effective contraception
Younger males were significantly more likely than older males to report using condoms at last intercourse (83.1% younger vs. 74.2% older, Table 4), however there were no differences for females. While the overwhelming majority of sexually active teens of either gender reported using effective contraceptive methods at last intercourse (89.3% & 90.1% males, 82.9% & 89.8% females), around 10% of both older and younger males as well as older females reported much less effective strategies or no method, while a significantly higher percent of younger females (17%) did not use effective birth control at last intercourse.
In order to determine whether these patterns in condom and contraceptive use might be because older adolescents relied on the use of hormonal birth control, additional analyses were conducted to compare the use of only condoms, only hormonal birth control (including the pill, the ring, the patch, depo provera, and IUDs), or dual method use (both condoms and hormonal contraception). Older males were almost four times more likely to report having used only hormonal birth control than younger males (19.6% older vs. 5.2% of younger males), but were equally likely to report having used dual methods (34.1% older vs. 33.1% younger males). Among females, examination of the 95% confidence intervals suggested there were no differences between older and younger teens in hormonal or dual method use, but younger females were significantly more likely to use condoms (55.8% younger vs. 42.2% older females).
Pregnancy Involvement
Just 5% or fewer adolescents of either gender or age category within their first year of sexual intercourse were involved in pregnancy (Tables 4 and 5). However, younger adolescent females were slightly more likely to report a pregnancy than older females, although the 95% confidence intervals overlapped (Table 5).
Sexually Transmitted Infections (STIs)
Very few adolescents of either gender or age category reported a health care provider told them they had a sexually transmitted infection within their first year of sexual intercourse. Younger males were statistically more likely to report an STI than older peers, but the rates were very low (2.5% vs. 0.2%) and the confidence intervals overlapped (Table 4). There was no statistical difference between older and younger females.
Discussion
According to population health data collected from BC adolescents in public high schools in 2008, very few of the 14- and 15-year-olds that Bill C-22 aimed to protect actually experienced first intercourse with partners outside of the legal age range. Adolescents 13 years of age and younger were the most likely to have sexual partners outside of the legal age range, and the most vulnerable group was those who first had sex under 12 years of age, which has been illegal since 1892. Of concern, among both girls and boys who first had intercourse younger than 12 years of age, nearly 40% reported that their partner was 20 or more years of age. Unfortunately, Bill C-22 did not provide any additional legal measures to further protect these adolescents beyond laws that were already in place.
The prevalence rates reported in this study and much of the literature reviewed lead us to the conclusion that the most vulnerable group of sexually active adolescents are those aged 13 and younger. This study did not examine the sexual risk behaviours of adolescents aged 13 and younger because Bill C-22 did not change the laws for this age group. However, since all sexual intercourse with an individual less than 12 years old is illegal, and adolescents 12 and 13 years of age frequently reported that their first partner was outside of the legal “close in age” exception range, it suggests further strategies are needed to prevent sexual abuse of these very young teens.
Among BC adolescents in public high schools, younger adolescents (age 14 and 15) were more likely than older adolescents (age 16 and 17) to report higher prevalence of only a few sexual risk behaviours in their first year of sexual intercourse. The clearest differences for both males and females were in experiencing forced intercourse and number of sexual partners, while there were no differences for sex under the influence of alcohol or drugs, and somewhat marginal differences in diagnosis of an STI, or pregnancy involvement for only males or only females, respectively. As we expected in our hypothesis 2, younger teens of both genders were more likely to report forced intercourse. These results were consistent with the New Zealand birth cohort research (Dickson, et al., 1998). Contrary to the rationale provided for Bill C-22, however, younger adolescents were more likely to be forced by another youth than by an adult. Consistent with U.S. studies but not prior Canadian research, younger adolescents were more likely than older teens to have three or more sexual partners in their first year of sexual intercourse. These findings likely differ from the prior Canadian data (Saewyc et al., 2008) because of the restricted focus on adolescents within their first year of sexual intercourse. These results persist when controlling for experience of sexual abuse or force, indicating that developmental maturity does appear to affect an adolescent’s number of sexual partners (Hypothesis 3). This can be a concern, because a greater number of sexual partners can increase the chances of contracting and sharing an STI or being involved in an unintended pregnancy. However, overall, we found Hypothesis 3, that younger adolescents would be more likely to engage in riskier sexual behaviour than older peers, only partially supported.
In examining health behaviours, rather than risk exposures, however, the necessity for a change in the law, i.e., that 14 and 15-year-olds are considered less capable of healthy sexual decision-making (Hypothesis 4) seems less supported. Condom and contraceptive use in this study was similar to results reported previously by Saewyc et al. (2008) and Sneed (2009). Younger males were more likely to have used a condom than older males, but both were equally likely to report having used an effective contraceptive method at last intercourse. Younger females were somewhat less likely to have used an effective contraceptive method than older females, but were equally likely to report having used condoms, indeed, more likely to use only condoms. The reason for higher rates of hormonal contraceptive use among older teens could be that they are more easily able to obtain a prescription for a contraceptive, or in the case of males, negotiate the use of these with their partner. The overwhelming majority of teens, whether younger or older, reported using effective contraceptive methods, and one in three used dual methods—both condoms and hormonal forms of contraception. Thus, Hypothesis 4, that younger teens are less likely to engage in healthy sexual behaviours, was not supported at all.
In general, rates of STIs and pregnancy involvement were very low for both males and females in both age categories. This is quite different from findings from the U.S. (Coker et al., 1994; Kaestle, et al., 2005; Manlove et al., 2005). However, STI and pregnancy rates among Canadian teens have generally been lower than those in the U.S. (McKay & Barrett, 2010). Further, the STI measure did not take into account whether some adolescents are more likely to get tested or not; often an STI can be asymptomatic, especially among males, so teens may be unaware of a need for testing. Since these analyses focused on the first year of intercourse, the time frame may be too short to result in measurable STI or pregnancy outcomes. Without biological testing, it is impossible to confirm the reliability or accuracy of this self-report measure.
Although older adolescents in the previous literature seem to report better sexual health outcomes than younger adolescents, our research suggests that when research takes into account the likely differences in levels of sexual experience among different age groups and focuses on different ages of teens with similar levels of experience, these differences dissolve. The first year of sexual intercourse can be an important time of establishing consistent patterns of health behaviours, and it is encouraging that even younger sexually active teens often engage in healthy sexual behaviours such as condom and contraception use.
The results also appear to suggest females had more negative outcomes than males, regardless of age. This is particularly apparent regarding forced sex. This may be due to the different sexual scripts for males and females. Sexual script theory describes how females are expected to be sexually naive and self-silence their sexual needs, rights, and values; whereas males are expected to be directive and assertive (Widman, Welsh, McNulty & Little, 2006). Thus, adolescent males may not recognize force when it occurs, believing the sexual script that “real men always want sex,” or that admitting to abuse or force by another male will stigmatize them as gay among their peers. They may feel shame because they were unable to protect themselves, as a “real man” is expected to do (Edinburgh, Saewyc & Levitt, 2006). Similarly, young females’ sexual decisions may be based more on self-esteem and belonging than on preventing negative sexual health outcomes. In addition, it is more normative for females to be younger than males in a romantic relationship (Manlove et al., 2005). This can be seen in the reported age discrepancy of partners in our study: female adolescents have higher rates of adult partners and males have slightly higher rates of inappropriately young partners. This age discrepancy may create a power differential, which may make communication in these relationships even more difficult. The differences between males and females we found in the results may be due to gendered social norms that place both male and female adolescents at a disadvantage, though from very different angles.
Limitations and Strengths
One significant limitation in this analysis is the measure of “illegal” sexual activity with adolescents. The 2008 BC AHS only collected data on the age of an adolescent’s first sexual partner, with no information about age discrepancies in subsequent relationships. However, it did ask about lifetime experience of forced intercourse and sexual abuse. Thus, our measure of sexual activity outside the close in age exemptions, based on age at first intercourse alone, may underestimate its true prevalence, since this research was unable to link experience of force or abuse to the first relationship independent of age, or to any subsequent relationships. At the same time, none of the other population-based Canadian surveys of adolescents, to our knowledge, ask about age of first sex and age of first sexual partner, or age of partners after first sex, or about sexual abuse or forced sex; this includes the 2006 Health Behaviour in School Children survey (Boyce, King & Roche, 2008), the Toronto Teen Sex Survey of 2007 (Flicker et al., 2009), and the 2007 Student Drug Use Surveys of the Atlantic Provinces (Poulin & Elliott, 2007). Nor do these other surveys ask sexual behaviour questions of teens as young as age 12. The BC AHS appears to be the only population-based data source in Canada that has the ability to conduct this type of policy analysis at even a provincial level.
As with all large-scale school-based surveys, one limitation is that data rely on self-report; to the extent students did not understand the sexual behaviour questions, or perceived them as sensitive questions they did not wish to answer, their answers may not be accurate or completely honest. However, self-report is the primary way to assess sexual health behaviours, and years of evidence suggests that adolescents honestly answer anonymous surveys that have appropriate measures in place to assure confidentiality. Public health nurses administer this survey, and students are assured of the anonymity of their data; as a result, we have low missing data. We also employ careful data review and exclude surveys that have clear joking comments or highly inconsistent response patterns.
Because this research used a population health survey conducted in BC, it may not be representative of adolescent sexual behaviour throughout the rest of Canada. As the only source at present of population-based data available to evaluate the implications of the change in the law, however, the use of the BC AHS, while limited to a geographic subset of Canadians, is also a strength. The data collected by the McCreary Centre Society asked young people most of the kinds of questions needed to provide evidence to inform the law. It clearly demonstrates the importance of asking these types of sexual health questions on adolescent health surveys, especially national adolescent health surveys.
The large overall sample of adolescents in the BC AHS allowed us to focus on adolescents who were navigating their first year of sexual intercourse. This allowed us to rule out potential confounding due to differential experience levels, and test the evidence of developmental maturity’s role in sexual health behaviours of adolescents in Canada.
Conclusion and Implications
Using Canadian population health data, this study evaluated adolescent sexual behaviour evidence in the context of the federal government’s rationales for raising the age of sexual consent in 2008. We did not find support for the assertion that younger adolescents make unsafe sexual decisions. When focused on their first year of sexual intercourse, adolescents between 14 and 17 for the most part engaged in the same behaviours, regardless of age. The main differences found were somewhat greater number of partners for younger adolescents, lower condom use for older adolescents with more hormonal contraceptive use instead, and a slightly higher likelihood of experiences of forced intercourse (by other youth) reported by younger adolescents. The large majority of adolescents were making safe sexual health decisions.
This study did find some support for the rationale that younger adolescents are at greater risk of exploitation than older teens. However, when considering the number of adolescents affected by this legislation, the change in age of consent may not have been necessary. This is because 14- and 15-year-olds were the primary targets of the law, yet this evidence showed adolescents under 13 years were at the greatest risk of sexual abuse or force, with more than half reporting partners who are too old, and almost half reporting their partner was more than 20 years old. Unfortunately, Bill C-22 did not offer changes in the law to further protect this vulnerable group of adolescents.
This research has implications for education, policy, and future research. The findings suggest it is important to include a focus on healthy relationships in sexual health education for young people. According to Meany, Rye, Wood, and Solovieva (2009), adolescents believe it is very important to learn about self-esteem, trust, and communication in sexual relationships. Adolescents need to know how to communicate with partners and with peers about healthy romantic relationships, including how to navigate difficult sexual situations such as those involving alcohol or drugs. Given the complexities of the law’s close in age exceptions, it would be useful to provide education about age-appropriate relationships for both older and younger teens.
This evidence-based policy analysis constitutes a relatively little-used approach for research. As the results suggest, it is important to evaluate laws using the best available evidence. Although ideally this would occur prior to the enactment of a new law, it is also useful after a law has been passed. Evidence-based policy analysis creates an opportunity to make amendments to laws if needed, to prevent unintended negative effects. Health effects are a legitimate lens through which to evaluate law and policy.
This study cannot predict the actual effects of the change in the law; until enough time has passed to track changes in ages of partners or rates of abuse and risky sexual behaviours, we will not be able to measure its actual effects. Other evidence is also needed, for example, changes in teens accessing sexual health resources, or rates of convictions of adult sex offenders. These outcomes should be priorities for future research. Canada should also focus on creating a national adolescent sexual survey with detailed questions and meticulous sampling. Finally, given existing laws do not seem to be protecting the most sexually vulnerable group of children, those less than 13 years of age, future policy in Canada should focus on effective strategies to address the problem of child sexual abuse, including increasing the enforcement of existing child abuse laws.
Acknowledgments
Analyses for this paper were funded in part by grant #HOA80059 from the CIHR Institute of Gender and Health (Saewyc, PI), and by Dr. Saewyc’s Research Chair in Applied Public Health, grant #CPP86374 from the CIHR Institute of Population & Public Health, the Institute of Human Development, Child & Youth Health, and the Public Health Agency of Canada. The authors would like to acknowledge the McCreary Centre Society, www.mcs.bc.ca, as the source of the BC Adolescent Health Survey of 2008 used in this paper. The authors would also like to acknowledge Dr. Weihong Chen for her invaluable help with SPSS Complex Samples.
References
- Black D. Age of consent uproar; will law protect vulnerable kids or ‘criminalize’ teenage sex? Police welcome protection against child exploitation; youth workers see ‘criminalization’ of teen sex. Toronto Star. 2006 Jun 19;:A1. Retrieved online from http://pqasb.pqarchiver.com/thestar/access/1062406631.html.
- Boyce WF, King MA, Roche J. Healthy settings for young people in Canada. Health Behaviour in School-Age Children. Public Health Agency of Canada; 2008. [Google Scholar]
- Criminal Code of Canada. Part V: Sexual offenses, public morals, and disorderly conduct. 2008 Available at http://laws.justice.gc.ca/en/C-46?page-4.html.
- Coker AL, Richter DL, Valois RF, McKeown RE, Garrison CZ, Vincent ML. Correlates and consequences of early initiation of sexual intercourse. Journal of School Health. 1994;64(9):372–377. doi: 10.1111/j.1746-1561.1994.tb06208.x. [DOI] [PubMed] [Google Scholar]
- Dickson N, Paul C, Herbison P, Silva P. First sexual intercourse: Age, coercion, and later regrets reported by a birth cohort. British Medical Journal. 1998;316:29–33. doi: 10.1136/bmj.316.7124.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edinburgh L, Saewyc E, Levitt C. Gender differences in extrafamilial sexual abuse experiences among young teens. The Journal of School Nursing. 2006;22(5):278–284. doi: 10.1177/10598405060220050601. [DOI] [PubMed] [Google Scholar]
- Flicker S, Flynn S, Larkin J, Travers R, Guta A, et al. Sexpress: The Toronto Teen Survey Report. Toronto, ON: Planned Parenthood Toronto; 2009. [Google Scholar]
- Fohr SA, Layde PM, Guse CE. Graduated driver licensing in Wisconsin: Does it create safer drivers? Wisconsin Medical Journal. 2005;104(7):31–36. [PubMed] [Google Scholar]
- Joyce T, Kaestner R, Colman S. Changes in abortions and births and the Texas parental notification law. The New England Journal of Medicine. 2006;354(10):1031–1038. doi: 10.1056/NEJMsa054047. [DOI] [PubMed] [Google Scholar]
- Kaestle CE, Halpern CT, Miller WC, Ford CA. Young age at first sexual intercourse and sexually transmitted infections in adolescents and young adults. American Journal of Epidemiology. 2005;161(8):774–780. doi: 10.1093/aje/kwi095. [DOI] [PubMed] [Google Scholar]
- Luke DA, Stamatakis KA, Brownson RC. State youth-access tobacco control policies and youth smoking behaviour in the United States. American Journal of Preventative Medicine. 2000;19(3):180–187. doi: 10.1016/s0749-3797(00)00196-3. [DOI] [PubMed] [Google Scholar]
- MacKay A, Barrett M. Trends in teen pregnancy rates from 1996–2006: A comparison of Canada, Sweden, U.S.A. and England/Wales. Canadian Journal of Human Sexuality. 2010;19:43–52. [Google Scholar]
- MacKay R, Bédard M. Library of Parliament Legislative Summary. Ottawa, ON: 2007. Bill C-22: An act to amend the criminal code (age of protection) and to make consequential amendments to the criminal records act. [Google Scholar]
- Manlove J, Moore K, Liechty J, Ikramullah E, Cottingham S. Child Trends Research Brief. Child Trends; Washington, DC: 2005. Sex between young teens and Older individuals: a demographic portrait. [Google Scholar]
- Meany GJ, Rye BJ, Wood E, Solovieva E. Satisfaction with school-based sexual health education in a sample of university students recently graduated from Ontario high schools. The Canadian Journal of Human Sexuality. 2009;18(3):107–125. [Google Scholar]
- Niederkrotenthaler T, Till B, Herberth A, Kapusta ND, Voracek M, Dervic K, Etzersdorfer E, Sonneck G. Can media effects counteract legislation reforms? The case of adolescent firearm suicides in the wake of the Austrian firearm legislation. Journal of Adolescent Health. 2009;44:90–93. doi: 10.1016/j.jadohealth.2008.05.010. [DOI] [PubMed] [Google Scholar]
- Noll JG, Shank CE, Putnam KT. Childhood sexual abuse and adolescent pregnancy: A meta-analytic update. Journal of Pediatric Psychology. 2009;34(4):366–378. doi: 10.1093/jpepsy/jsn098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearce T. New sexual consent law may confuse teens. The Globe and Mail, 2 May 2008. 2008 Retrieved online 25 November 2009 from http://www.theglobeandmail.com/life/article683868.ece.
- Picard A. From 14 to 16: What does raising the age of consent accomplish? The Globe and Mail, 8 May 2008. 2008 Retrieved online 27 November 2009 from http://www.theglobeandmail.com/life/article683896.ece.
- Poulin C, Elliott D. Student drug use survey in the Atlantic Provinces. Technical Report. Halifax, NS: Dalhousie University; 2007. [Google Scholar]
- Rao JNK, Scott AJ. The analysis of categorical data from complex sample surveys: chi-square tests for goodness of fit and independence in two-way tables. Journal of the American Statistical Association. 1981;76:221–230. [Google Scholar]
- Rew L, Bowman K. Protecting youth from early and abusive sexual experiences. Pediatric Nursing. 2008;34(1):19–26. [PubMed] [Google Scholar]
- Robinson DL. Do enforced bicycle helmet laws improve public health? British Medical Journal. 2006;332:722–725. [Google Scholar]
- Rodgers GB. Effects of state helmet laws on bicycle helmet use by children and adolescents. Injury Prevention. 2002;8:42–46. doi: 10.1136/ip.8.1.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saewyc E, Green R. Survey Methodology for the 2008 BC Adolescent Health Survey IV. Vancouver, BC: McCreary Centre Society; 2009. Fact Sheet. Available at www.mcs.bc.ca. [Google Scholar]
- Saewyc EM, Magee LL, Pettingell SE. Teenage pregnancy and associated risk behaviors among sexually abused adolescents. Perspectives on Sexual and Reproductive Health. 2004;36(3):98–105. doi: 10.1363/psrh.36.98.04. [DOI] [PubMed] [Google Scholar]
- Saewyc EM, Poon CS, Homma Y, Skay CL. Stigma management? The links between enacted stigma and teen pregnancy trends among gay, lesbian, and bisexual students in British Columbia. The Canadian Journal of Human Sexuality. 2008;17(3):123–139. [PMC free article] [PubMed] [Google Scholar]
- Saewyc EM, Taylor D, Homma Y, Ogilvie G. Trends in sexual health and risk behaviours among adolescent students in British Columbia. The Canadian Journal of Human Sexuality. 2008;17:1–14. [PMC free article] [PubMed] [Google Scholar]
- Saewyc E, Richens K, Skay CL, Reis E, Poon C, Murphy A. Sexual orientation, sexual abuse, and HIV-risk behaviors among adolescents in the Pacific Northwest. American Journal of Public Health. 2006;96(6):1104–1110. doi: 10.2105/AJPH.2005.065870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shah S, Hoffman RE, Wake L, Marine WM. Adolescent suicide and household access to firearms in Colorado: Results of a case-control study. Journal of Adolescent Health. 2000;26:157–163. doi: 10.1016/s1054-139x(99)00064-6. [DOI] [PubMed] [Google Scholar]
- Sex Information and Education Council of Canada (SIECCAN) Age of consent to sexual activity: What should you know about this topic and why? Check the Research Fact Sheet, January 2010. 2010 Available at http://www.sexualityandu.ca/pdfs/CTR_AgeOfConsent.pdf.
- Smith A, Stewart D, Peled M, Poon C, Saewyc E the McCreary Centre Society. A picture of health: Highlights from the 2008 BC Adolescent Health Survey. Vancouver, BC: McCreary Centre Society; 2009. Available at http://www.mcs.bc.ca. [Google Scholar]
- Sneed CD. Sexual risk behaviour among early initiators of sexual intercourse. AIDS Care. 2009;21(11):1395–1400. doi: 10.1080/09540120902893241. [DOI] [PubMed] [Google Scholar]
- Spriggs AL, Halpern CT. Timing of sexual debut and initiation of postsecondary education by early adulthood. Perspectives on Sexual and Reproductive Health. 2008;40(3):152–161. doi: 10.1363/4015208. [DOI] [PubMed] [Google Scholar]
- Watson LF, Taft AJ, Lee C. Associations of self-reported violence with age at menarche, first intercourse, and first birth among a national population sample of young Australian women. Women’s Health Issues. 2007;17:281–289. doi: 10.1016/j.whi.2007.06.003. [DOI] [PubMed] [Google Scholar]
- Weber T. The Globe and Mail, 23 June 2006. 2006. Ottawa tables bill to raise age of sexual consent to 16. [Google Scholar]
- Widman L, Welsh DP, McNulty JK, Little KC. Sexual communication and contraceptive use in adolescent dating couples. Journal of Adolescent Health. 2006;39:893–899. doi: 10.1016/j.jadohealth.2006.06.003. [DOI] [PubMed] [Google Scholar]
- Wiggins S. Graduated licensing year six evaluation report: Short- and longer-term effects on new driver crash rates, specific component effects, and early effects of October 2003 enhancements (GLPe) 2006 http://www.icbc.com/driver-licensing/Getting-licensed/glp-6-eval.pdf#Variables._frag_. Appendices at: http://www.icbc.com/driver-licensing/Getting-licensed/glp-appendix-a.pdf#Variables._frag_ and http://www.icbc.com/driver-licensing/Getting-licensed/glp-appendix-b.pdf#Variables._frag_.
- Wong J. Age of consent to sexual activity in Canada: Background to proposed new legislation on “age of protection”. The Canadian Journal of Human Sexuality. 2006;15:163–169. [Google Scholar]