Abstract
BACKGROUND:
Endotracheal tube security is a critical safety issue. We compared the mobility of an in situ endotracheal tube secured with adhesive tape to the one secured with a new commercially available purpose-designed endotracheal tube-holder device (Haider Tube-Guard®). We also observed for the incidence of oropharyngeal or facial trauma associated with the 2 tube fixation methods.
METHODS:
Thirty adult patients undergoing general anesthesia with neuromuscular blockade were prospectively enrolled. Immediately after intubation, a single study author positioned the endotracheal tube tip in the distal trachea using a bronchoscope. Anesthesiologists caring for patients secured the tube in their normal fashion (always with adhesive tape). A force transducer was used to apply linear force, increasing to 15 N or until the principal investigator deemed that the force be aborted for safety reasons. The displacement of the endotracheal tube was measured with the bronchoscope. Any tape was then removed and the endotracheal tube secured with the Haider Tube-Guard device. The linear force was reapplied and the displacement of the endotracheal tube measured. The Haider Tube-Guard device was left in place for the duration of the case. The patient’s face and oropharynx were examined for any evidence of trauma during surgery and in the recovery room. On discharge from the postanesthesia care unit, the patient answered a brief survey assessing for any subjective evidence of minor facial or oropharyngeal trauma.
RESULTS:
Under standardized tension, the endotracheal tube withdrew a mean distance of 3.4 cm when secured with adhesive tape versus 0.3 cm when secured with the Haider Tube-Guard (P <0.001). Ninety-seven percent of patients (29/30) experienced clinically significant endotracheal tube movement (>1 cm) when adhesive tape was used to secure the tube versus 3% (1/30) when the Haider Tube-Guard was used (P <0.001). Thirty percent of patients (9/30) were potentially deemed a high extubation risk (endotracheal tube movement >4 cm) when the endotracheal tube was secured with tape versus 0% (0/30) when secured with the Haider Tube-Guard (P = 0.004). Six patients with taped endotracheal tubes required the traction to be aborted before 15 N of force was achieved to prevent potential extubation as the tape either separated from the face or stretched to allow excessive endotracheal tube movement. None of the patients appeared to sustain any injury from the Haider Tube-Guard device.
CONCLUSIONS:
The Haider Tube-Guard significantly reduced the mobility of the endotracheal tube when compared with adhesive tape and was well tolerated in our observations.
Endotracheal intubation is a common procedure performed in both the operating room and the intensive care unit. The inadvertent movement of the endotracheal tube (ETT) is potentially life-threatening. For this reason, the American Heart Association’s 2005 Advanced Cardiac Life Support guidelines recommend securing the ETT with either a tape or a commercial device.1 In current clinical practice, there is wide variability of methods used to secure the ETT including (1) adhesive tape, (2) cloth tape ties, and (3) commercial ETT holders. Prior studies have demonstrated diverging expert opinions on the optimum method for securing an ETT.2–8 The ideal method would minimize movement of the ETT, be quick and easy to apply, and have a low risk of injury to the oropharyngeal structures.
The Haider Tube-Guard® is a new, commercially available device designed to optimally secure an ETT. The device is composed of a “clamshell”-like silicone body that wraps around and attaches onto the ETT via an adjustable, one-size-fits-all plastic clamp (Fig. 1A). The device plus ETT combination rests between the upper and the lower teeth, using the immobility of the maxilla for rigid fixation of the ETT to the patient (Fig. 1B). A Velcro neck strap (Posey foam/Velcro tie, Arcadia CA) is then attached for extra security. The Haider Tube-Guard device also incorporates a built-in soft bite block and, according to the company, is engineered to be gentle on the oropharyngeal and facial soft tissues during clinical use.
Figure 1.
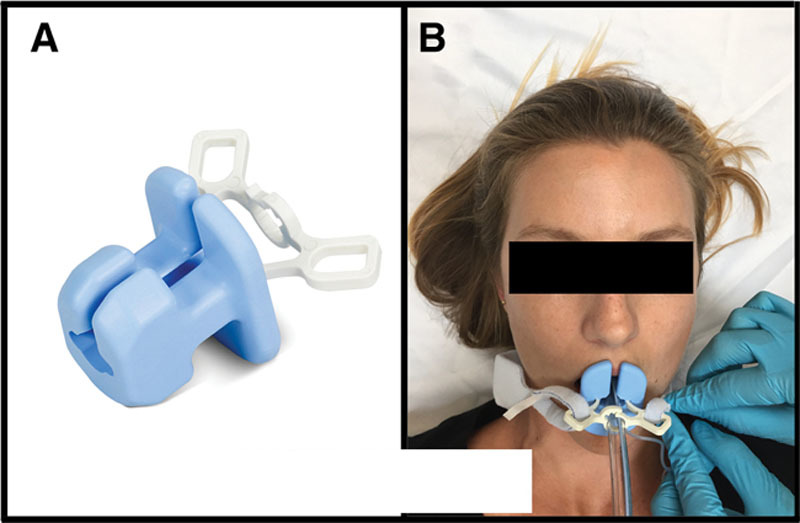
Haider Tube-Guard device. A, Photograph of the Haider Tube-Guard device. The blue silicone portion wraps around and grips the endotracheal tube while also acting as a bite block. The white adjustable clamp maximizes grip and enables fixation to a Velcro neck strap. The device fits all adult-sized endotracheal tubes (size 6.0–8.5 mm ID). B, Photograph of the Haider Tube-Guard shown in situ with the Velcro neck strap being applied.
The goal of this study was to compare ETT mobility when securing the ETT with the Haider Tube-Guard versus adhesive tapes, our current standard of practice. We hypothesized that the Haider Tube-Guard would provide more secure ETT attachment in adults undergoing general endotracheal anesthesia when compared with tapes and adhesives. The primary objective of the study was to quantify the movement of the ETT caused by a standardized force of dislodgement, comparing the Haider Tube-Guard with adhesive tape. The secondary objective of the study was to determine whether the Haider Tube-Guard device was well tolerated during routine clinical use.
METHODS
After approval by our institutional review board and obtaining written informed consent, 30 adult patients undergoing general anesthesia with endotracheal intubation and neuromuscular blockade were prospectively enrolled in this study. The trial was registered with the clinicatrials.gov registry (NCT02347488; PI: Nir N. Hoftman, January 8, 2015). A careful history and physical examination were performed preoperatively; patients with loose or missing teeth, temporomandibular joint disease, severe asthma, and immunosuppression and patients undergoing surgery of the oropharynx or surgery who required the prone position were excluded from the trial.
Immediately after endotracheal intubation with a standard adult (6.5–8.0 mm ID) ETT (Mallinckrodt™; Covidien, Mansfield, OH), a single-study author with >10 years’ experience in thoracic anesthesia positioned the ETT tip in the distal one-third of the trachea using a bronchoscope. The exact distance from the carina to the ETT tip was measured and recorded, and the ETT was then secured at the discretion of the anesthesiologist caring for the patient. A force transducer (IWS V2-30, Jennings, Vancouver, BC, Canada) accurate to within 0.1 N was then attached to the ETT assembly and linear force applied parallel to the ETT such that it would pull the tube from the trachea if the tube was not adequately secured. While securing the head in a neutral position to prevent unwanted movement, we increased the force over approximately 5 seconds until the target of 15 N was reached or until the principal investigator deemed that the force be aborted to prevent possible tracheal extubation. Based on our previous mannequin testing, we selected a 15-N force because it could reliably displace inadequately secured ETTs. This force was at least an order of magnitude less than that generated during routine mastication and less than half the force routinely used during the application of cricoid pressure.9,10 We thus thought that this force would be safe in all patients, but as a precaution, we excluded any patients with actual or perceived loose teeth or any temporomandibular joint pain or disease. The change in ETT tip position caused by this force was then measured with the indwelling bronchoscope, rounded up to the nearest 5 mm, and recorded. After removal of the adhesive tape, the ETT was repositioned in the distal trachea, and the Haider Tube-Guard device was inserted and used to secure the ETT as recommended by the manufacturer. The linear force was reapplied as before, and the change in ETT tip position caused by the force was recorded. Linear force was aborted at the discretion of the investigators if tracheal extubation was deemed likely to occur without intervention. In such cases, the greatest achievable force was recorded along with the ETT displacement distance at the time of force abort. The bronchoscope was then removed and the Haider Tube-Guard device left in place for the duration of the case. Any conditions that would interfere with tape adhesion such as facial hair, sweating, and oily or flaky skin were documented. During the intraoperative portion as well as at admission and discharge from the postanesthesia care unit, an anesthesiologist who was part of the study team thoroughly examined the patient’s face and oropharynx for any evidence of minor tissue trauma. On discharge from the postanesthesia care unit, the patient also answered a brief survey assessing any subjective evidence of minor facial or oropharyngeal tissue trauma.
ETT movements >1 cm were defined as clinically significant because they could lead to patients’ coughing or moving. Furthermore, specialty ETTs such as double-lumen endobronchial tubes or electromyography tubes could become dislodged and malfunction with such movements. ETT movements >4 cm were defined as “potentially high risk for extubation” based on the dimensions of standard ETT cuffs and presumed positioning of the tube cuff in the proximal third of the trachea. Given that the average human trachea is 10 to 12 cm in length, movements >4 cm in such a positioned ETT would be highly likely to displace the majority of the balloon cuff beyond the vocal cords, risking imminent tracheal extubation. Our protocol was designed with safety nets in place to eliminate any chance of extubation during the study period. First, the ETT was positioned in the distal trachea to increase the margin of safety. Second, the principal investigator continuously ensured in real time that the ETT was well within the trachea during the data collection period using the indwelling bronchoscope. Third, a second study anesthesiologist and the clinical provider anesthesiologist not participating in the study were both constantly observing the patient to ensure proper ETT placement. Any of those providers had overriding power to request that the force be aborted should safety concerns arise. Finally, the bronchoscope was left in the trachea during the entire data collection period to act as a guide for reintubation in the extremely unlikely event that the ETT was pulled out of the trachea.
A power analysis performed before patient enrollment determined that 17 patients would need to be enrolled to show a difference of 1 SD from the mean between the 2 fixation techniques at 80% power. We chose to enroll 30 patients to increase the power of our results and include a larger variety of patients undergoing different surgical procedures. The comparison of average ETT movement during maximal force was first performed using the paired t test. Given that the order of securing the ETT (tape versus Haider-Tube Guard) was not randomized, we also ran an analysis of covariance (ANCOVA) model to confirm our findings from the paired t test. The ANCOVA model was constructed with the pairwise difference between methods of securement as the dependent variable and tape movement (centered) for each patient as the covariate. The intercept from this model represents the average difference between methods, and the slope represents the expected difference for each 1-cm increase in tape movement. The slope from this model was estimated to be 0.98 (95% confidence interval [CI], 0.86–1.11; P <0.001), indicating that for each 1-cm increase in tape movement, the expected difference between methods of securement increased by 0.98 cm.
The absolute movement values were then dichotomized into clinically relevant thresholds (>1 cm and >4 cm). The rate of patients exceeding these thresholds was compared between the 2 ETT securing methods using the McNemar test for paired proportions. P values <0.05 were considered statistically significant. All statistical analyses were performed using SAS 9.4 (Cary, NC).
RESULTS
Thirty patients successfully completed the protocol, and no patients had to be excluded once they were recruited. Surgical case mix included neurological, vascular, gynecological, colorectal, thoracic, and oncological surgery. The mean surgical time and, therefore, dwell time of the Haider Tube-Guard was 189 minutes (range 65–410 minutes). All patients were positioned supine for the duration of surgery.
The Haider Tube-Guard significantly reduced the mobility of the ETT when compared with adhesive tape. Under standardized traction, the ETT withdrew a mean distance of 3.4 cm (SD ±1.8) when secured with adhesive tape versus 0.3 cm (SD ±0.6) when secured with the Haider Tube-Guard (average difference = 3.1 [SD ±1.8; 95% CI, 2.88–3.32; P <0.001; ANCOVA]). The paired t test results were similar to the ANCOVA with the average difference of 3.1 (95% CI, 2.41–3.79; P <0.001). The ETT displacement distances measured with each of the securing methods for every patient are shown graphically in Figure 2.
Figure 2.
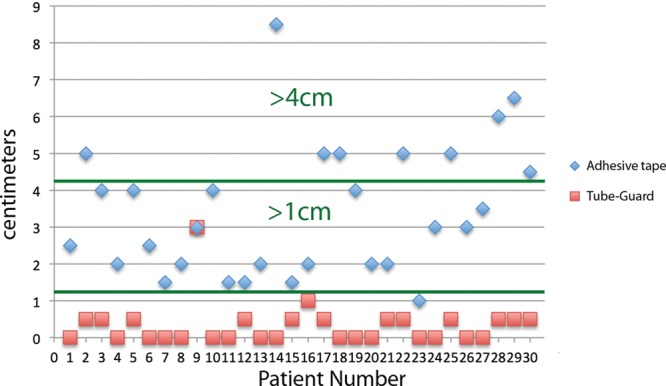
Results summary. This graph highlights the study results. Every patient is represented by a number and plotted on the x-axis. Endotracheal tube (ETT) movement during applied traction is plotted for each patient on the y-axis in centimeters. Movement distance is denoted by blue diamonds during fixation with adhesive tape and red squares during fixation with the Haider Tube-Guard. Individual patients have both symbols shown because each patient served as his or her own control. Horizontal green lines highlight 2 clinically relevant categories: (1) >1-cm ETT movement and (2) >4 cm of ETT movement.
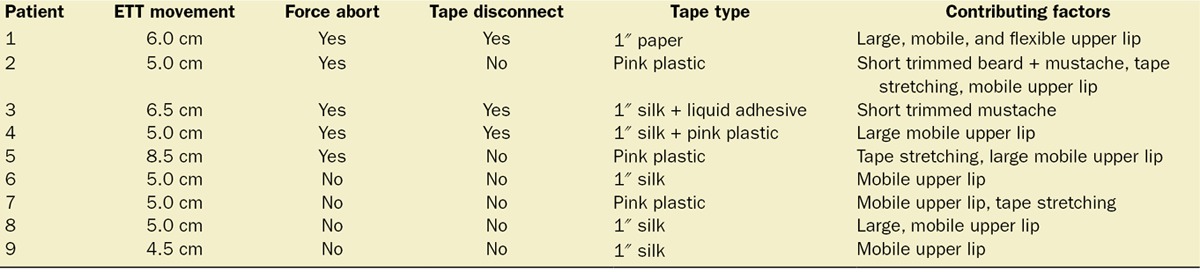
Ninety-seven percent of patients (29/30) experienced clinically significant ETT movement (>1 cm) when adhesive tape was used to secure the tube versus 3% (1/30) when the Haider Tube-Guard was used (P < 0.001). Thirty percent of patients (9/30) experienced ETT movement >4 cm (potential high extubation risk) when the ETT was secured with tape versus 0% (0/30) when secured with the Haider Tube-Guard (P = 0.004). Six patients required that traction be aborted before 15 N of force was achieved to prevent extubation because the tape either completely separated from the face or stretched enough to allow for significant ETT excursion. Three of these 6 patients had short facial hair, and despite significant efforts to tape and glue the ETT, in 2 cases, the tape disconnected under load. Five of the 6 patients with tape disconnects experienced ETT movement >4 cm and were categorized into the high extubation risk group, whereas the sixth (who had a short mustache) was not because the ETT excursion was only 4.0 cm at the time the force was aborted. The details of the patients deemed potentially high extubation risk are summarized in Table 1.
Table 1.
Characteristics and Details of Patients with Endotracheal Tube (ETT) Movements >4.0 cm
The study team examined the oropharynx of all 30 patients postoperatively, and all but one patient completed the study questionnaire (one patient was aphasic postoperatively). None of the patients suffered any significant injury from the Haider Tube-Guard device. Sixty-five percent of patients reported a mild sore throat deemed to be secondary to tracheal intubation. One patient reported mild discomfort of the gum near a rear molar thought to be unrelated to the Haider Tube-Guard. Another patient had a minor abrasion of the tongue frenulum possibly because of a difficult nasogastric and orogastric tube insertion, although the Haider Tube-Guard could not be excluded as a causative agent.
DISCUSSION
The Haider Tube-Guard significantly outperformed all types and combinations of adhesive tape because it affixes to the patient in a far more secure fashion. Whereas adhesive tape attaches to the facial surface, the Haider Tube-Guard anchors to the maxilla and mandible. Forces applied to a taped ETT distort and pull on mobile facial tissues, allowing for significant ETT movements to occur even in the absence of an adhesive failure. An ETT secured with the Haider Tube-Guard on the contrary is pinned between rigid bony structures that do not move under such loads. This lack of reliance on a tape–skin interface explains why the Haider Tube-Guard functioned well in notoriously difficult settings such as in patients with facial hair.
The Haider Tube-Guard all but eliminated ETT movements >1 cm under maximal load, in contrast to adhesive tapes, which failed to prevent such movements in all but 1 patient. The Haider Tube-Guard may prove especially useful in cases using specialty ETTs such as double-lumen endobronchial tubes or electromyography tubes, where small movements can dislodge the bronchial balloon or electrode interface, respectively. Further studies should be conducted in such scenarios as well as in patients not undergoing neuromuscular blockade to determine whether in fact the Haider Tube-Guard reduces unwanted intraoperative coughing by eliminating such small ETT movements. Of note, in one patient with a very large mouth opening, the Haider Tube-Guard separated from the teeth under load, but the Velcro neck strap served as a backup and kept the ETT from moving beyond 3 cm. The control method of taping in this patient, which included 5 different tapes and adhesives, faired no better by allowing 3 cm of movement under load.
Nearly one-third (n = 9) of the study population experienced ETT movement >4 cm when adhesive tape was used to affix the ETT and could have been highly vulnerable to extubation under normal, uncontrolled circumstances. In a tenth patient (with a mustache), whose force was aborted at 4 cm, ETT movement because of tape disconnect could have been included in the high extubation risk category; we chose not to include this patient to stay true to our original definition in the protocol. In all 10 of these patients, securing the ETT with the Haider Tube-Guard mitigated this extubation vulnerability by eliminating excessive ETT movement. Our definition of high extubation risk (movement >4 cm) was quite conservative, and the actual population at risk in this study may have been higher.2–8 Reported rates of unintentional extubation range from 0.03% to 2.5% depending on the clinical setting.11–14 Undeniably, unintentional extubation can lead to increased patient morbidity and even mortality.15–17 In fact, 12% of all airway cases in the anesthesia closed claims analysis were caused by unintentional extubation.18 Several commercial devices have been introduced into clinical practice over the years with the aim of mitigating this risk. Clinical trials comparing various commercial ETT holders to traditional adhesive tape have shown mixed results; traditional tape was found to be superior to these devices in some but not all trials.2–8 These findings, combined with the perceived extra cost of the commercial devices, have slowed their adoption into clinical practice. The Haider Tube-Guard’s superior and unequivocal performance versus traditional tape may indicate improved design compared with other available commercial devices, although head-to-head testing should be performed to determine any such benefit. The Haider Tube-Guard may prove beneficial in clinical settings prone to ETT motion including (1) emergency transport (civilian and military) of trauma patients, (2) prone and lateral positioning, and (3) extensive head and neck surgery. Blood, sweating, oral and facial secretions, and burns can make securing the ETT in these cases even more challenging, and further studies using the Haider Tube-Guard in such scenarios are warranted.
This clinical study had several methodological advantages when compared with previous ETT-holding device trials. We conducted the trial in the operating room on patients undergoing surgery with each patient serving as his or her own control for a true comparison of the Haider Tube-Guard versus adhesive tape. Many previous studies were performed on human cadavers or plastic simulation mannequins, limiting the generalizability of the results.2–5 Also, our protocol used bronchoscopy to measure the distance between the ETT tip and the carina, thus defining the actual ETT movement within the airway. Other studies used only indirect surrogates of ETT airway movement such as distance from the incisor or lip.3,5 Finally, all patients in the study received neuromuscular blockade during data collection to eliminate any baseline intrinsic jaw muscle tone, ensuring that only the device’s inherent grip was being measured.
Our study did have several limitations that should be noted. First, we introduced the force in a crescendo pattern, building to maximal force over about 5 seconds, and then held the force during bronchoscopy measurements. This was necessary to allow for accurate distance measurements and also to ensure patient safety by carefully controlling the force. Such prolonged forces may not represent all forces encountered clinically, some of which may be fast, jerking motions. Second, we applied the force in the same linear direction in all patients, whereas real-life forces encountered in clinical medicine may be multidirectional and rapidly changing. Third, we excluded edentulous patients or patients with loose teeth from the study. Further studies should be performed to assess the Haider Tube-Guard device in patients with poor dentition because this could possibly lead to reduced device grip. Fourth, our study was not blinded to the treatment group, but given the nature of the device, we thought that blinding would not be possible. Furthermore, constant observation of the ETT–face interface was required during application of force to ensure safety, making blinding impossible. Finally, although our study demonstrated that the Haider Tube-Guard was well tolerated, it was not statistically powered to determine device safety.
In conclusion, the Haider Tube-Guard was superior to adhesive tape in securing the ETT. The device significantly reduced ETT movement and may prevent unplanned patient extubation. Larger studies would need to be conducted to demonstrate utility in diverse clinical settings and to establish a patient safety record.
DISCLOSURES
Name: Jack C. Buckley, MD.
Contribution: This author helped design the study, conduct the study, analyze the data, and write the manuscript.
Attestation: Jack C. Buckley has seen the original study data, reviewed the analysis of the data, and approved the final manuscript.
Name: Adam P. Brown, MD.
Contribution: This author helped conduct the study and write the manuscript.
Attestation: Adam P. Brown approved the final manuscript.
Name: John S. Shin, MD.
Contribution: This author helped conduct the study and write the manuscript.
Attestation: John S. Shin approved the final manuscript.
Name: Kirsten M. Rogers, BA.
Contribution: This author helped conduct the study.
Attestation: Kirsten M. Rogers approved the final manuscript.
Name: Nir N. Hoftman, MD.
Contribution: This author helped design the study, conduct the study, analyze the data, and write the manuscript.
Attestation: Nir N. Hoftman has seen the original study data, reviewed the analysis of the data, approved the final manuscript, and is the author responsible for archiving the study files.
This manuscript was handled by: Sorin J. Brull, MD.
ACKNOWLEDGMENT
The authors thank Tristan Grogan, MS, for his expertise and assistance in statistical analysis.
Footnotes
Funding: All funding came from departmental research funds, with the exception of the Haider Tube-Guard devices, which were supplied by Haider Biologics free of charge.
The authors declare no conflicts of interest.
Reprints will not be available from the authors.
REFERENCES
- 1.American Heart Association. Part 4: Advanced life support. Circulation. 2005;112(Suppl I):11125–54. [Google Scholar]
- 2.Carlson J, Mayrose J, Krause R, Jehle D. Extubation force: tape versus endotracheal tube holders. Ann Emerg Med. 2007;50:686–91. doi: 10.1016/j.annemergmed.2007.05.013. [DOI] [PubMed] [Google Scholar]
- 3.Owen R, Castle N, Hann H, Reeves D, Naidoo R, Naidoo S. Extubation force: a comparison of adhesive tape, non-adhesive tape and a commercial endotracheal tube holder. Resuscitation. 2009;80:1296–300. doi: 10.1016/j.resuscitation.2009.08.007. [DOI] [PubMed] [Google Scholar]
- 4.Shimizu T, Mizutani T, Yamashita S, Hagiya K, Tanaka M. Endotracheal tube extubation force: adhesive tape versus endotracheal tube holder. Respir Care. 2011;56:1825–9. doi: 10.4187/respcare.00954. [DOI] [PubMed] [Google Scholar]
- 5.Murdoch E, Holdgate A. A comparison of tape-tying versus a tube-holding device for securing endotracheal tubes in adults. Anaesth Intensive Care. 2007;35:730–5. doi: 10.1177/0310057X0703500512. [DOI] [PubMed] [Google Scholar]
- 6.Tasota FJ, Hoffman LA, Zullo TG, Jamison G. Evaluation of two methods used to stabilize oral endotracheal tubes. Heart Lung. 1987;16:140–6. [PubMed] [Google Scholar]
- 7.Kaplow R, Bookbinder M. A comparison of four endotracheal tube holders. Heart Lung. 1994;23:59–66. [PubMed] [Google Scholar]
- 8.Gardner A, Hughes D, Cook R, Henson R, Osborne S, Gardner G. Best practice in stabilisation of oral endotracheal tubes: a systematic review. Aust Crit Care. 2005;18:158, 160–5. doi: 10.1016/s1036-7314(05)80029-3. [DOI] [PubMed] [Google Scholar]
- 9.Scully C, Al-Bayaty H. Oxford Handbook of Applied Dental Sciences. Vol 156. Oxford, UK: Oxford University Press; 2002. [Google Scholar]
- 10.Herman NL, Carter B, Van Decar TK. Cricoid pressure: teaching the recommended level. Anesth Analg. 1996;83:859–63. doi: 10.1097/00000539-199610000-00036. [DOI] [PubMed] [Google Scholar]
- 11.Bouza C, Garcia E, Diaz M, Segovia E, Rodriguez I. Unplanned extubation in orally intubated medical patients in the intensive care unit: a prospective cohort study. Heart Lung. 2007;36:270–6. doi: 10.1016/j.hrtlng.2006.10.002. [DOI] [PubMed] [Google Scholar]
- 12.Boulain T. Unplanned extubations in the adult intensive care unit: a prospective multicenter study. Association des Réanimateurs du Centre-Ouest. Am J Respir Crit Care Med. 1998;157:1131–7. doi: 10.1164/ajrccm.157.4.9702083. [DOI] [PubMed] [Google Scholar]
- 13.Carrión MI, Ayuso D, Marcos M, Paz Robles M, de la Cal MA, Alía I, Esteban A. Accidental removal of endotracheal and nasogastric tubes and intravascular catheters. Crit Care Med. 2000;28:63–6. doi: 10.1097/00003246-200001000-00010. [DOI] [PubMed] [Google Scholar]
- 14.Chui I, Ohkawa S, Kakavouli A, Sun L. Incidence and causes of perioperative endotracheal reintubation in children: a review of 28 208 anesthetics. Paediatr Anaesth. 2013;23:621–6. doi: 10.1111/j.1460-9592.2012.03920.x. [DOI] [PubMed] [Google Scholar]
- 15.Atkins PM, Mion LC, Mendelson W, Palmer RM, Slomka J, Franko T. Characteristics and outcomes of patients who self-extubate from ventilatory support: a case-control study. Chest. 1997;112:1317–23. doi: 10.1378/chest.112.5.1317. [DOI] [PubMed] [Google Scholar]
- 16.Mort TC. Unplanned tracheal extubation outside the operating room: a quality improvement audit of hemodynamic and tracheal airway complications associated with emergency tracheal reintubation. Anesth Analg. 1998;86:1171–6. doi: 10.1097/00000539-199806000-00006. [DOI] [PubMed] [Google Scholar]
- 17.Epstein SK, Nevins ML, Chung J. Effect of unplanned extubation on outcome of mechanical ventilation. Am J Respir Crit Care Med. 2000;161:1912–6. doi: 10.1164/ajrccm.161.6.9908068. [DOI] [PubMed] [Google Scholar]
- 18.Cheney FW, Posner KL, Lee LA, Caplan RA, Domino KB. Trends in anesthesia-related death and brain damage: a closed claims analysis. Anesthesiology. 2006;105:1081–6. doi: 10.1097/00000542-200612000-00007. [DOI] [PubMed] [Google Scholar]


