Abstract
Background
High salt intake may be associated with pro-inflammatory changes in the immune response, and increased clinical and MRI activity in adults with relapsing-remitting multiple sclerosis.
Objective
We sought to determine if dietary salt intake is associated with pediatric-onset MS risk in a multicenter, case-control study.
Methods
Pediatric-onset CIS/MS cases within four years of onset and controls less than 22 years old recruited from 14 pediatric-MS centers were studied. Dietary sodium intake was assessed using the validated Block Kids Food Screener (NutritionQuest). Sodium intake, excess sodium, and sodium terciles were compared between cases and controls. Logistic regression models were adjusted for age, gender, ethnicity, body mass index, and socioeconomic status.
Results
Among 170 cases (mean age=15.2±3.5) and 331 controls (mean age=14.0±3.7), no significant difference in unadjusted mean sodium intake was found between cases (2044 mg/d) and controls (2030 mg/d, p=0.99). The proportion of subjects consuming excess sodium, based on the adequate intake for age and gender, was similar between cases and controls (65% versus 69%, p=0.34). There were no increased odds of higher sodium intake among cases as compared to controls (for each 100 mg/d increase in sodium, OR=1.00, 95% CI 0.98, 1.02; p=0.93, for excess sodium intake, OR=1.05, 95% CI 0.67, 1.64; p=0.84).
Conclusions
Our results show no strong association between dietary salt intake and pediatric-onset MS risk, suggesting that salt intake may not play a prominent role in susceptibility to MS in children.
Keywords: Pediatric, Multiple sclerosis, Epidemiology, Salt, Dietary factors, Susceptibility
1. Introduction
Between 3.0% and 10.5% of multiple sclerosis (MS) patients have disease onset in childhood (Yeh et al., 2011; Simone et al., 2002). Compared to adults, pediatric patients tend to experience more frequent and severe exacerbations in the early stages of the disease (Gorman et al., 2009; Fay et al., 2012) and transition to secondary progressive (SP) MS after a longer disease duration but at a younger age (Simone et al., 2002; Renoux et al., 2007).
An association between obesity in childhood and the development of MS has been consistently reported (Munger et al., 2013; Langer-Gould et al., 2013). Epidemiologic studies have explored the role of dietary factors and MS susceptibility with conflicting results (Ascherio and Munger, 2007). Vitamin D deficiency is associated with higher MS risk in adults, and an increased relapse rate in both pediatric and adult MS patients (Munger et al., 2006; Mowry et al., 2010). No association was found between vitamins C, E and carotenoids and MS risk in women (Zhang et al., 2001). Studies of high-energy diet and saturated fat consumption have reported conflicting results (Zhang et al., 2000; Ghadirian et al., 1998).
There is limited, but suggestive, evidence for the role of dietary salt intake in MS susceptibility. An observational study of adult relapsing-remitting (RR) MS noted an increased rate of clinical exacerbations and MRI activity in subjects with high versus moderate or low salt intake (Farez et al., 2015). These findings support research in the animal model of MS, experimental allergic encephalomyelitis (EAE), for which a high salt diet was associated with earlier disease onset and progression (Wu et al., 2013; Kleinewietfeld et al., 2013). These studies also suggested that salt was associated with pro-inflammatory changes. Taken together, available data suggest that dietary salt intake might play a role in disease activity via its pro-inflammatory effect but additional research is needed to ascertain the role of dietary salt intake on MS susceptibility.
Pediatric-onset MS offers a unique opportunity to study such factors, due to temporal proximity at the time of diagnosis to exposure, thereby minimizing recall bias. In this multi-center project (R01NS071463, PI Waubant), data from a dietary screener for children (NutritionQuest) were collected to determine whether dietary salt intake was associated with pediatric-onset MS risk.
2. Methods
2.1. Participating sites
This case-control study was carried out as part of a larger investigation on pediatric MS conducted at 14 pediatric MS centers, including University of California San Francisco, State University of New York at Buffalo, Massachusetts General Hospital for Children, Mayo Clinic Rochester, Stony Brook University Medical Center, Texas Children’s Hospital Baylor, Loma Linda University, Children’s Hospital of Philadelphia, Ann & Robert H. Lurie Children’s Hospital of Chicago, Children’s Hospital of Colorado, University of Texas Southwestern/Children’s Medical Center Dallas, Boston Children’s Hospital, University of Alabama, and Washington University School of Medicine in St. Louis. Each center recruited study participants and collected data on pediatric-onset MS cases and controls. Data, including demographic, developmental, environmental exposure and medical history information, were then merged into a collaborative database. Participants were recruited between November 2011 and June 2014. Approval was obtained by the institutional review board at each participating institution. All participants and one of their parents signed assent and consent forms, as required by each center’s institutional review board, prior to enrollment.
2.2. Study participants
Cases included children with clinically isolated syndromes (CIS) or RRMS with onset before 18 years of age and less than four years of disease duration (Polman et al., 2011). All cases were confirmed by a review committee (LK, TL, and EW). Eligibility for controls included age less than 22 years, absence of autoimmune disorders except for asthma or eczema, no history of treatment with immunosuppressive therapy nor history of severe health conditions. Parents of controls could not have MS. Eligible controls were invited to participate by recruitment in general or specialty pediatric clinics at the same participating institutions.
Race and ethnicity were self-reported according to NIH categories. Socioeconomic status (SES) was defined by self-report as the highest level of education attained by the participants’ mother.
2.3. Sodium intake assessment using block kids food screener (BKFS)
Dietary sodium intake (mg/d) estimates were obtained using the 2007 BKFS, a 41-item diet screener that focuses on fruit and fruit juices, vegetables, processed foods such as potatoes (including French fries) and processed meats, as well as other meat/poultry/fish, whole grains, dairy, legumes and saturated fat (NutritionQuest., 2014). The questionnaire is designed for children aged 2–17 years old and available in English and Spanish and evaluates the frequency and portion of foods and beverages consumed during the past week. The subject or his/her caregiver completed the questionnaire after receiving instructions from a member of the research staff. The BKFS is a simple method of dietary assessment that has been validated against three, 24-hour dietary recalls in children aged 10–17 for servings of fruits, vegetables, meats, grains and other food groups (Hunsberger et al., 2015). Subjects were instructed to select the frequency (none last week, 1 day, 2 days, 3–4 days, 5–6 days, everyday) and then the food-specific portion size (e.g. 1 slice, 2 slices, 3+ slices) that most closely matched their intake in the preceding week.
Daily nutrient values, including sodium, were obtained by first quantifying the nutrient in each of the 41-items, the averages of which were then summed to provide the daily nutrient intake. The amount of nutrient in each item was determined by multiplying the frequency of consumption (as a decimal fraction from 0=never to 1=everyday) by the sex- and gender-specific portion size consumed (which is then divided by 100), and then multiplied by the amount of nutrient-per-100 g. Nutrient values are based on the Food and Nutrient Database for Dietary Surveys (FNDSS), a database developed by the United States Department of Agriculture. Six age-sex categories were used to provide dietary estimates based on differing caloric intake patterns by age and sex: males and females 2–3 years old, males and females 4–8 years old, males 9–13 years old, males 14–17 years old, females 9–15 years old and females 16–17 years old. For this study, participants between 18–19 years old (20 cases and 45 controls) were calculated according to norms for 16–17 year olds. Subjects were excluded if >15/41 food items, were missing to questions, or if reported estimates reflected biologically implausible daily energy intakes (<500 or >5000 kcal/day) based on NutritionQuest food screener analysis.
2.4. Statistics
All analyses were performed using SAS Version 9.3 (SAS Institute, Cary, NC). To compare dietary sodium intake between pediatric-onset MS cases and controls, sodium was assessed as a continuous variable, using the Mann–Whitney U test, and as a categorical variable (yes/no) based on whether a subject consumed excess sodium using chi-squared test. Excess sodium was defined by the adequate intake, the recommended daily average intake (AI) level of sodium, for each age group (1000 mg/d 1–3 years old, 1200 mg/d 4–8 years old, and 1500 mg/d 9–19 year olds) (Institute of Medicine, 2005).
Logistic regression was performed to determine the effect of daily sodium intake on disease risk, with models adjusted for age, gender, BMI, and SES. Sodium was included as a continuous predictor (100 mg/day), as a categorical predictor comparing excess sodium (based on AI) versus non-excess sodium and as a categorical variable based on terciles (mg/d of sodium) for the entire sample of cases and controls. We also looked at log transformation of sodium.
Height and/or weight were missing for a number of participants (17 cases, 72 controls), making it impossible to calculate BMI. Using CDC stature-for-age and weight-for-age growth charts, we approximated the age- and gender-specific z-scores of height and weight for cases and controls. We then applied the Markov chain Monte Carlo method of multiple imputation to obtain 5 imputed sets of z-scores for height and weight from case-control status, race, ethnicity, SES, average daily calories, grams of fat, sodium intake and fiber intake (Schafer., 1997). Imputed sets of BMI were calculated by back-transforming the z-scores for heights and weights.
3. Results
At the time BKFS were analyzed, 631 subjects had been enrolled into the case-control study. Among them, 103 had not yet provided the completed BKFS form. These subjects did not differ from the 501 who completed the form and remained in the final analysis (see Supplemental table). Out of 557 BKFS collected, 501 questionnaires were included in the final analysis. Subjects were excluded due to incorrect subject identification numbers noted on the questionnaire (n=5), presence of autoimmune disease (n=2), family member already enrolled (n=11), ineligibility after adjudication review (n=2), failure to meet inclusion criteria for MS/CIS (n=1), energy intake <500 kcal (n=21), mismatch between age and gender (n=5), age less than three years (n=6), incomplete questionnaires (n=2), and missing gender data (n=1) (see Supplemental Fig. 1).
3.1. Patient characteristics
Among 170 cases and 331 controls, the mean age at the time of BKFS completion was 14.4 years (±3.7 years) (Table 1). Cases were older on average compared to controls (p<0.01). There were significantly more females (63% versus 49%) and Hispanic/Latino (29% versus 18%) cases compared to controls; however, the proportions of cases and controls were similar in terms of race. Baseline nutritional estimates, including total energy intake (kcal/d), total fat (g/d), and percent energy intake from fat (%) were similar between groups. Cases consumed 1334 (±596) kcal/d on average compared to 1330 (±625) kcal/d for controls (p=0.94). Total fat consumption was likewise similar between cases (54.2 g/d) and controls (54.2 g/d) (p=0.99). BMI was higher in cases (24.7 kg/m2) compared to controls (22.2 kg/m2) (p<0.01). Forty-three percent of controls’ mothers reported receiving a Bachelor’s or graduate degree compared to 29% such degrees among the mothers of cases (p<0.01). At enrollment in the study, 159/170 cases had a diagnosis of MS and 11/170 CIS. Of the 11 CIS cases at enrollment, 6 have been diagnosed with MS, 4 remain CIS, and 1 became NMO.
Table 1.
Baseline characteristics between cases and controls.
| Cases | Controls | All | p-value | |
|---|---|---|---|---|
| N | 170 | 331 | 501 | |
| Age at enrollment | 15.2 (3.5) | 14.0 (3.7) | 14.4 (3.7) | <0.01 |
| Years since MS onset | 1.0 (1.2) | |||
| BMI (mean (sd) [n]) | 24.6 (6.0) [153] | 22.2 (6.1) [259] | 23.1 (6.2) [412] | |
| Imputed BMI (mean (sd)) | 24.7 (6.1) | 22.2 (6.1) | 23.1 (6.2) | <0.01 |
| Energy (kcal/d) | 1334 (596) | 1330 (625) | 1331 (615) | 0.94 |
| Total fat (g) | 54.2 (28.0) | 54.2 (28.2) | 54.2 (28.1) | 0.99 |
| Gender | <0.01 | |||
| Female | 107 (62.94%) | 161 (48.64%) | 268 (53.49%) | |
| Race | 0.11 | |||
| American Indian or Alaska Native | 4 (2.35%) | 5 (1.51%) | 9 (1.80%) | |
| Asian | 6 (3.53%) | 18 (5.44%) | 24 (4.79%) | |
| Black or African American | 34 (20.00%) | 52 (15.71%) | 86 (17.17%) | |
| Native Hawaiian or Other Pacific Islander | 1 (0.59%) | 0 (0.00%) | 1 (0.20%) | |
| White | 98 (57.65%) | 227 (68.58%) | 325 (64.87%) | |
| Mixed | 15 (8.82%) | 17 (5.14%) | 32 (6.39%) | |
| Unknown/missing | 12 (7.06%) | 12 (3.63%) | 24 (4.79%) | |
| Ethnicity | <0.01 | |||
| Hispanic or Latino | 49 (28.82%) | 59 (17.82%) | 108 (21.56%) | |
| Not Hispanic or Latino | 117 (68.82%) | 263 (79.46%) | 380 (75.85%) | |
| Ethnicity unknown/missing | 4 (2.35%) | 9 (2.72%) | 13 (2.59%) | |
| Mother highest education | <0.01 | |||
| None | 20 (11.76%) | 16 (4.83%) | 36 (7.19%) | |
| High school diploma | 95 (55.88%) | 136 (41.09%) | 231 (46.11%) | |
| Bachelor or graduate degree | 49 (28.82%) | 141 (42.60%) | 190 (37.92%) | |
| Other | 0 (0.00%) | 11 (3.32%) | 11 (2.20%) | |
| Unknown/missing | 6 (3.53%) | 27 (8.16%) | 33 (6.59%) |
SD=standard deviation.
3.2. Sodium intake and pediatric-onset MS risk
Unadjusted analyses comparing mean sodium intake (mg/d) demonstrated no significant difference between cases (2044 mg/d) and controls (2030 mg/d) (p=0.99) (Table 2). Sex-specific analyses revealed no difference in sodium intake for males or females between cases and controls. Male subjects consumed significantly higher sodium (2393 mg/d) compared to females (1723 mg/d) (p<0.01). The mean intake for male cases (2483 mg/d) exceeded the tolerable upper limit of 2300 mg/d. In line with these results, 81% of male cases and 79% of male controls consumed excess sodium (p=0.72). For males and females combined, 65% of cases and 69% of controls consumed excess sodium (p=0.34). Analyses of sodium by terciles showed no difference between sodium tercile and case-control status (males, p=0.96; females, p=0.44). Fig. 1 shows the distribution of sodium intake for cases and controls.
Table 2.
Dietary intake of sodium by whole group and gender.
| Sodium intake | Gender | Cases | Controls | All | p-value |
|---|---|---|---|---|---|
| Sodium (mg/d±SD) | ALL | 2044 (1086) | 2030 (1088) | 2035 (1086) | 0.99 |
| Male | 2483 (1248) | 2360 (1277) | 2393 (1268) | 0.43 | |
| Female | 1785 (887) | 1681 (692) | 1723 (776) | 0.58 | |
| Excess sodium | ALL | 110/170 (65%) | 228/331 (69%) | 338/501 (67%) | 0.34 |
| Male | 51/63 (81%) | 134/170 (79%) | 185/233 (79%) | 0.72 | |
| Female | 59/107 (55%) | 94/161 (58%) | 153/268 (57%) | 0.6 | |
| Sodium terciles | ALL | 0.71 | |||
| Male | 0.96 | ||||
| Female | 0.44 | ||||
| 1st | ALL | 58/170 (34%) | 102/331 (31%) | 160/501 (32%) | |
| Male | 13/63 (21%) | 36/170 (21%) | 49/233 (21%) | ||
| Female | 45/107 (42%) | 66/161 (41%) | 111/268 (41%) | ||
| 2nd | ALL | 55/170 (32%) | 117/331 (35%) | 172/501 (34%) | |
| Male | 18/63 (29%) | 51/170 (30%) | 69/233 (30%) | ||
| Female | 37/107 (35%) | 66/161 (41%) | 103/268 (38%) | ||
| 3rd | ALL | 57/170 (34%) | 112/331 (34%) | 169/501 (34%) | |
| Male | 32/63 (51%) | 83/170 (49%) | 115/233 (49%) | ||
| Female | 25/107 (23%) | 29/161 (18%) | 54/268 (20%) | ||
| Log(Sodium) | ALL | 7.50 (0.49) | 7.50 (0.47) | 7.50 (0.47) | 0.99 |
| Male | 7.71 (0.47) | 7.64 (0.49) | 7.66 (0.49) | 0.43 | |
| Female | 7.38 (0.45) | 7.35 (0.39) | 7.36 (0.42) | 0.58 |
SD=standard deviation.
Fig. 1.
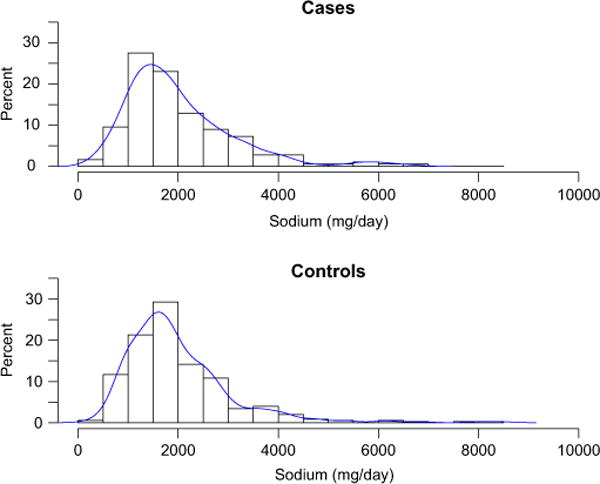
Histograms for cases and controls in order to depict the distribution of sodium intake (mg/d) between groups.
There was no increased odds of MS for higher sodium intake (for each 100 mg/d increase in sodium OR=1.00, 95% CI 0.98, 1.02; p=0.93) or for excess sodium intake (OR=1.05, 95% CI 0.67, 1.64; p=0.84) in multivariate analyses adjusted for age, gender, BMI, ethnicity, and SES. There were no increased odds when comparing subjects in the second versus first tercile of sodium intake (OR=1.00, 95% CI 0.60, 1.66; p=1.00) or in the third versus first tercile (OR=1.14, CI=0.67, 1.95; p=0.62). Analyses using log transformation of sodium did not show any association (data not shown).
4. Discussion
This study assessed the association between dietary salt intake and pediatric-onset MS risk using data from a large well-characterized data set of children. Our findings do not support a strong association between dietary sodium intake, as measured by the BKFS, and pediatric-onset MS risk in both unadjusted analyses and multivariable logistic regression models. It is remarkable that despite the tendency of food frequency screeners to underestimate the consumption of various nutrients, including sodium and caloric intake in general, our subjects had sodium intake above recommended while they had relatively low estimated caloric intake (Bentley, 2006; Espeland et al., 2001).
While the BKFS has been validated against three, 24-h food frequency questionnaires for major food groups, it has yet to be validated for sodium intake and does not assess the contribution of table salt to daily sodium intake, which may have differed between groups. It is noteworthy, however, that no salt-specific food screener for children has been validated at this time. 24 h Urine collections represent the gold standard to measure sodium intake, however, urine collection was not feasible in the present study. Dietary recall, including food frequency questionnaires, has been used to estimate sodium intake in children when urine measurements were lacking. Sodium intake measured by dietary recall tends to yield estimates lower than urine collections and available food frequency questionnaires are only moderately correlated to salt intake measured by 24 h-urine collection (Mercado et al., 2015). There is no clear consensus on which method of dietary recall is best, though dietary recalls that capture >1 day of intake, such as the BKFS that assess consumption over a 1-week period, better reflect usual intake (Bentley, 2006). Therefore, while our findings do not support an association between sodium intake and pediatric-onset MS risk, further evaluation of sodium intake using more objective measures, such as urine collection, would be useful to replicate our findings.
Although study findings did not support our hypothesis of higher dietary salt intake in children with MS compared to controls, this does not exclude the possibility that salt intake is related to relapses or disease activity. A recent observational study in adult RRMS highlighted salt as a potential player in disease activity wherein an association was found between high salt intake, estimated using early morning urinary sodium excretion, and the development of clinical exacerbations and new lesions on MRI (Farez et al., 2015).
The relationship between salt intake and MS pathogenesis has been supported in the animal model of MS, EAE, and a mechanism through which salt mediates the disease process has been proposed (Wu et al., 2013; Kleinewietfeld et al., 2013). Prior studies have shown that Th17 cells produce pro-inflammatory cytokines, including IL-17 and IL-22, which disrupt the blood-brain barrier and are probably critical for MS processes (Jadidi-Niaragh and Mirshafiey, 2011). Wu et al.’s study proposes a mechanism by which salt may promote the Th17 pathway and the development of autoimmunity. In particular, an increase in dietary salt promotes a serine/threonine kinase (SGK1) that plays a role in salt homeostasis and IL-23 signaling. This signaling pathway enhances pathogenic Th17 cells and their pro-inflammatory effects. Moreover, their study found that mice fed a high salt diet had more severe disease activity than those fed a normal diet.
Study strengths include a case-control design with a large catchment area across the United States and diverse patient population. Compared to food diaries and 24-h dietary recalls, the validated BKFS is a simple method ideally suited for the pediatric population and takes approximately 10–12 min to complete in one sitting. The BKFS was not specifically designed to assess sodium intake and has not been evaluated for its validity for dietary sodium intake; however, the questionnaire assessed consumption of foods typically high in sodium, including pizza, lunchmeat, snack chips and bread rolls. Multivariable analyses were appropriately adjusted for factors associated with both MS risk and diet, including age, race, gender, ethnicity, and BMI. Although there are no clear guidelines on how dietary salt intake should be analyzed, we employed standard statistical methods of analyzing salt as a continuous variable, categorized based on the Institute of Medicine recommendations for children, and by terciles, this latter method typical of nutrient analyses.
While all cases completed the BKFS within a mean of 1.0 years of MS onset, we cannot be sure that their dietary patterns reflect their usual intake prior to disease onset. However, at this time there are no specific dietary recommendations for patients once MS is established, decreasing the likelihood of reduction in dietary salt content as a result of diagnosis. Self-report dietary assessment can be influenced by subject recall, the limited categories of foods listed, and ability to estimate intake over the past week, which may have differed between groups. We cannot exclude that those subjects or caregivers who consented to participate had eating habits that differed from those who did not wish to participate, which may have impacted results. Finally, at this time we cannot exclude that salt in the diet may be associated with MS risk in a sub-group of individuals with specific genotypes or other unidentified risk factors.
4.1. Conclusion
In summary, in this multi-center case-control study, we found no evidence that dietary salt intake is strongly associated with MS susceptibility in children. The use of food frequency questionnaires completed shortly after disease onset to evaluate the association of various nutrients with MS risk, although not perfect, is probably the best attempt at deciphering associations between diet and MS risk despite questionnaires limitations. The Pediatric MS Network has the unique ability to collect data on children with MS and controls that will facilitate ongoing research on the potential role of dietary factors as mediators of MS risk and disease progression.
Supplementary Material
Acknowledgments
We acknowledge the commitment of MS patients and controls and family members to this study and thank them for the time they invested in providing answers to the environmental and food frequency questionnaires.
Participating centers (with collaborators) are listed below in alphabetical order: Ann & Robert H. Lurie Children’s Hospital of Chicago (J. Rubin, L. Webb), Children’s Hospital of Alabama (J. Ness, Y. Harris), Boston Children’s Hospital (M. Gorman, L. Benson, S. Camposano), Children’s Hospital of Philadelphia (A. Waldman, G. Liu), Children’s Hospital Denver (T. Schreiner, K. Connelly), Children’s Hospital Salt Lake City (M. Candee, J. Narus), Loma Linda University Children’s Hospital (G. Aaen, M. Rundquist), Massa-chusetts General Hospital for Children (T. Chitnis, C. Crooks), Mayo Clinic (J. Tillema, J. M. Rodriguez, D. Weiss, J. Sorum), State University of New York at Stony Brook (L. Krupp, A. Belman, N. Oquendo), Texas Children’s Hospital (T. Lotze, M. Stocic), University of Buffalo (B. Weinstock-Guttman, M. Karpinski), University of California at San Francisco (E. Waubant, J. Graves, S. Lulu, J. Hart, M. Lee, J. McDonald), University of Texas Southwestern (B. Greenberg, P. Plumb), University of Utah Data Coordinating and Analysis Center (T. C. Casper, J. Rose, S. Roalstad, T. Hunt, C. Olsen, T. Simmons, W. Weber, B. Brown, E. Roan), Washington University School of Medicine in St. Louis (S. Mar, L. Grayson).
Study funding
This study was funded by NIH-Grant R01NS071463-04 (PI: E. Waubant). Dr. Waubant is also funded by the Race to Erase MS. A grant from the National Multiple Sclerosis Society HC 0165 (PI: T.C. Casper) also supported this study.
Appendix A. Supplementary material
Supplementary data associated with this article can be found in the online version at http://dx.doi.org/10.1016/j.msard.2016.02.011.
Footnotes
Disclosures
Jamie McDonald has no disclosures.
Dr. Graves was supported by the Foundation for Consortium of Multiple Sclerosis Centers and the NIH Bridging Interdisciplinary Research Careers in Women’s Health programs during this work. She has been a one-time consultant for EMD-Serono.
Dr. Waldman is supported by the NIH and previously received support from the National MS Society, American Brain Foundation, and The Calliope Joy Foundation. She received a one-time honorarium from Teva.
Dr. Greenberg has received grant support from NIH, PCORI, Biogen Idec, Guthy Jackson Charitable Foundation, Accorda Therapeutics, Chugai and Medimmune. He has received consultingfees from DioGenix, Novartis and Biogen. He has equity in Amplimmune.
Dr. Weinstock-Guttman received honoraria for serving in advisory boards and educational programs from Teva Pharmaceuticals, Biogen Idec, Novartis, Accorda, EMD Serono, Novartis, Genzyme and Sanofi. She also received support for research activities from the National Institutes of Health, National Multiple Sclerosis Society, National Science Foundation, Department of Defense, EMD Serono, Biogen Idec, Teva Neuroscience, Novartis, Accorda, Genzyme and the Jog for the Jake Foundation.
Yolanda Harris is supported by the National MS Society.
Dr. Krupp is supported by the National MS Society, NIH, Robert and Lisa Lourie Foundation, Department of Defense. She has received honoraria, consulting payments, grant support or royalties from Biogen, Medimmune, Novartis, Teva Neuroscience, Sanofi-Aventis, and EMD Serono.
Dr. Benson has research funding from Boston Children’s Hospital Office of Faculty Development Career Development grant.
Dr. Chitnis has served as a consultant for Biogen-Idec, Teva Neurosciences, Novartis, Sanofi-Aventis, and has received grant support from NIH, National MS Society, Guthy-Jackson Charitable Foundation, CMSC and Merck-Serono and Novartis.
Dr. Rose has research funding from Teva Neuroscience and Biogen. He is a member of the Medical Advisory Board for the DECIDE trial which is funded by Biogen and AbbVie.
Dr. Casper has been supported by the National MS Society and the NIH (R01NS071463). He is an ad-hoc consultant for Biovest International, Inc.
Dr. Waubant is funded by the National MS Society, the NIH and the Race to Erase MS. She has received honorarium from Roche for an educational lecture. She volunteers on an advisory board for a clinical trial of Novartis.
Drs. Belman, Schreiner, Tillema, Rubin, Candee, Ness, Gorman, Lotze, Rodriguez, Mar, Aaen, James, Lulu, Barcellos and Laraia have no disclosures. Janace Hart, Shelly Roalstad and Timothy Simmons have no disclosures.
References
- Ascherio A, Munger KL. Environmental risk factors for multiple sclerosis. Part II: Noninfectious factors. Ann Neurol. 2007;61:504–513. doi: 10.1002/ana.21141. [DOI] [PubMed] [Google Scholar]
- Bentley B. A review of methods to measure dietary sodium intake. J Cardiovasc Nurs. 2006;21:63–67. doi: 10.1097/00005082-200601000-00012. [DOI] [PubMed] [Google Scholar]
- Espeland MA, Kumanyika S, Wilson AC, et al. Statistical issues in analyzing 24-h dietary recall and 24-h urine collection data for sodium and potassium intakes. Am J Epidemiol. 2001;153:996–1006. doi: 10.1093/aje/153.10.996. [DOI] [PubMed] [Google Scholar]
- Farez MF, Fiol MP, Gaitan MI, Quintana FJ, Correale J. Sodium intake is associated with increased disease activity in multiple sclerosis. J Neurol, Neurosurg Psychiatry. 2015;86:26–31. doi: 10.1136/jnnp-2014-307928. [DOI] [PubMed] [Google Scholar]
- Fay AJ, Mowry EM, Strober J, Waubant E. Relapse severity and recovery in early pediatric multiple sclerosis. Mult Scler. 2012;18:1008–1012. doi: 10.1177/1352458511431725. [DOI] [PubMed] [Google Scholar]
- Ghadirian P, Jain M, Ducic S, Shatenstein B, Morisset R. Nutritional factors in the aetiology of multiple sclerosis: a case-control study in Montreal, Canada. Int J Epidemiol. 1998;27:845–852. doi: 10.1093/ije/27.5.845. [DOI] [PubMed] [Google Scholar]
- Gorman MP, Healy BC, Polgar-Turcsanyi M, Chitnis T. Increased relapse rate in pediatric-onset compared with adult-onset multiple sclerosis. Arch Neurol. 2009;66:54–59. doi: 10.1001/archneurol.2008.505. [DOI] [PubMed] [Google Scholar]
- Hunsberger M, O’Malley J, Block T, Norris JC. Relative validation of Block Kids Food Screener for dietary assessment in children and adolescents. Maternal Child Nutr. 2015;11:260–270. doi: 10.1111/j.1740-8709.2012.00446.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute of Medicine. Dietary Reference Intakes for Water, Potassium, Sodium, Chloride, and Sulfate. The National Academics Press; Washington DC: 2005. [Google Scholar]
- Jadidi-Niaragh F, Mirshafiey A. Th17 cell, the new player of neuroinflammatory process in multiple sclerosis. Scand J Immunol. 2011;74:1–13. doi: 10.1111/j.1365-3083.2011.02536.x. [DOI] [PubMed] [Google Scholar]
- Kleinewietfeld M, Manzel A, Titze J, et al. Sodium chloride drives autoimmune disease by the induction of pathogenic TH17 cells. Nature. 2013;496:518–522. doi: 10.1038/nature11868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Langer-Gould A, Brara SM, Beaber BE, Koebnick C. Childhood obesity and risk of pediatric multiple sclerosis and clinically isolated syndrome. Neurology. 2013;80:548–552. doi: 10.1212/WNL.0b013e31828154f3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mercado CI, Cogswell ME, Valderrama AL, et al. Difference between 24-h diet recall and urine excretion for assessing population sodium and potassium intake in adults aged 18 39 y. Am J Clin Nutr. 2015;101:376–386. doi: 10.3945/ajcn.113.081604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mowry EM, Krupp LB, Milazzo M, et al. Vitamin D status is associated with relapse rate in pediatric-onset multiple sclerosis. Ann Neurol. 2010;67:618–624. doi: 10.1002/ana.21972. [DOI] [PubMed] [Google Scholar]
- Munger KL, Bentzen J, Laursen B, et al. Childhood body mass index and multiple sclerosis risk: a long-term cohort study. Mult Scler. 2013;19:1323–1329. doi: 10.1177/1352458513483889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Munger KL, Levin LI, Hollis BW, Howard NS, Ascherio A. Serum 25-hydroxyvitamin D levels and risk of multiple sclerosis. JAMA. 2006;296:2832–2838. doi: 10.1001/jama.296.23.2832. [DOI] [PubMed] [Google Scholar]
- NutritionQuest. Block Food Screeners for Ages 2–17. 〈 http://www.nutritionquest.com/assessment/list-of-questionnaires-and-screeners〉 (accessed 05.08.14)
- Polman CH, Reingold SC, Banwell B, et al. Diagnostic criteria for multiple sclerosis: 2010 revisions to the McDonald criteria. Ann Neurol. 2011;69:292–302. doi: 10.1002/ana.22366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Renoux C, Vukusic S, Mikaeloff Y, et al. Natural history of multiple sclerosis with childhood onset. N Engl J Mede. 2007;356:2603–2613. doi: 10.1056/NEJMoa067597. [DOI] [PubMed] [Google Scholar]
- Schafer JL. Analysis of Incomplete Multivariate Data. Chapman & Hall; New York: 1997. [Google Scholar]
- Simone IL, Carrara D, Tortorella C, et al. Course and prognosis in early-onset MS: comparison with adult-onset forms. Neurology. 2002;59:1922–1928. doi: 10.1212/01.wnl.0000036907.37650.8e. [DOI] [PubMed] [Google Scholar]
- Wu C, Yosef N, Thalhamer T, et al. Induction of pathogenic TH17 cells by inducible salt-sensing kinase SGK1. Nature. 2013;496:513–517. doi: 10.1038/nature11984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yeh EA, Waubant E, Krupp LB, et al. Multiple sclerosis therapies in pediatric patients with refractory multiple sclerosis. Arch Neurol. 2011;68:437–444. doi: 10.1001/archneurol.2010.325. [DOI] [PubMed] [Google Scholar]
- Zhang SM, Willett WC, Hernan MA, Olek MJ, Ascherio A. Dietary fat in relation to risk of multiple sclerosis among two large cohorts of women. Am J Epidemiol. 2000;152:1056–1064. doi: 10.1093/aje/152.11.1056. [DOI] [PubMed] [Google Scholar]
- Zhang SM, Hernan MA, Olek MJ, Spiegelman D, Willett WC, Ascherio A. Intakes of carotenoids, vitamin C, and vitamin E and MS risk among two large cohorts of women. Neurology. 2001;57:75–80. doi: 10.1212/wnl.57.1.75. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


