ABSTRACT
The aim of this pilot study was to evaluate whether sleep was improved by a 1-day sleep education program in an occupational setting and whether stopping alcohol intake at bedtime might influence sleep. Subjects were 40 high school employees. The sleep education program lasted 4.5 hours and consisted of sleep science information, and sleep hygiene education including the risk of sleep related breathing disorder resulting from alcohol intake. Sleep conditions were evaluated by self-administered questionnaires at baseline and approximately 1 month later. The mean the Epworth Sleepiness Scale (ESS) score was significantly decreased by 1.2 points (P = 0.04), while the mean sleep duration was significantly decreased by 10 minutes (P = 0.02). Shortened sleep duration coincided with a decrease in sleepiness. This may indicate an improvement in sleep quality. The percentage of habitual alcohol intake at bedtime was significantly decreased (from 38.5% (15/39) to 20.5% (8/39), P = 0.04). Subjects who stopped alcohol intake at bedtime (n = 8) received the most benefit, with decreased scores of ESS and Insomnia Severity Index (ISI), although the reductions were not significant. This education program offers the possibility of improving sleep conditions among the general population, especially in those who cease habitual alcohol intake at bedtime. Further larger, randomized, controlled studies are warranted.
Key Words: Sleep hygiene education, sleep apnea, alcohol intake at bedtime, occupational group
INTRODUCTION
Sleep disturbance is a major health issue in Japan. Sleep disturbance is one of the risk factors for depression and suicide1-3). A national survey in 1997 showed that the prevalence of insomnia, including difficulty initiating sleep, difficultly of maintaining sleep and early morning awakening, was 21.4% in the general population4). It has been also reported that short sleep duration is associated with mortality, cardiovascular disease and diabetes5-9). Sleep duration in Japan was reported to be shorter than in other countries10).
Being able to inform people of the features of sleep and to provide methods that could improve their sleep, might be a way to contribute to preventing health problems related to poor sleep. A study in an occupational setting in Japan reported that a 1-hour sleep hygiene program reduced afternoon sleepiness at work, but did not improve sleep at night11). However, sleep hygiene education is not widely conducted in Japan. The aim of this pilot study was therefore to evaluate whether sleep was improved by a 1-day sleep education program in an occupational setting, including stopping habitual alcohol intake at bedtime, which may contribute to poor sleep conditions.
METHODS
Participants and procedures
Subjects were participants attending a 1-day sleep education program in December 2010. The program was arranged by school boards in Shiga prefecture, Japan, to improve the mental health of employees in public high schools. Participants attending the program were principals, vice-principals, teachers, school nurses, and office workers in public high schools.
Sleep and health conditions were evaluated by a self-administered questionnaire. Subjects were required to complete a questionnaire at baseline and 1 month later. The baseline survey was conducted on the program day. The second questionnaire was collected by mail. Among 66 participants, 54 participated in this study. One withdrew by the end of December 2010, and 40 completed and returned the second questionnaire and were included in the analysis (24 males and 16 females, mean age ± SD: 49.1 ± 8.9 years). Informed consent was obtained from all subjects. This study was approved by the ethics committee of Shiga University of Medical Science.
Sleep education program
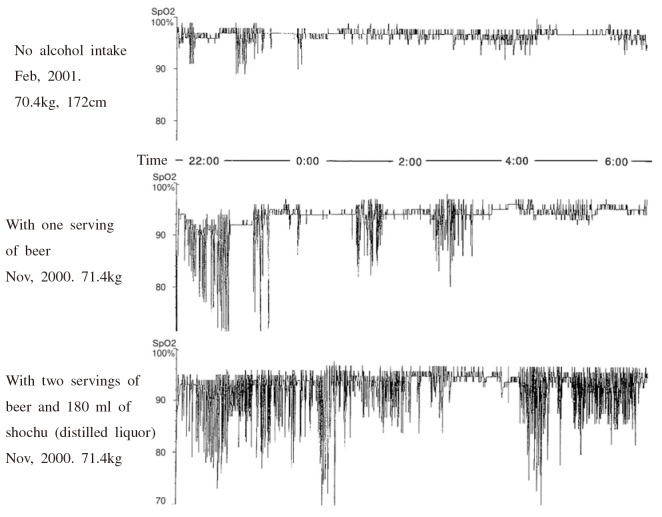
The program was created by three professors from sleep medicine disciplines of physiology and sleep-disordered breathing, and environmental physiology. The program took about 4.5 hours in total. Speakers explained using slides and a video presentation to explain basic sleep science information, including the role of sleep in people’s health and the sleep mechanisms involved, features of sleep in adolescence for high school students, sleep hygiene education including the risks of low arterial oxygen saturation during sleep resulting from alcohol intake (see Appendix 1)12), and methods to evaluate sleep.
Appendix 1:
A slide used in the sleep education program: low arterial oxygen saturation during sleep caused by alcohol intake in an obstructive sleep apnea patient12).
Educational materials, consisting of two pamphlets and a paperback pocket edition written by the speakers, were distributed to the participants. These included information on obstructive sleep apnea, basic sleep science and specific methods for improving sleep.
Questionnaires
The questionnaire comprised the Japanese version of the Pittsburgh Sleep Quality Index (PSQI)13, 14), the Japanese version of the Epworth Sleepiness Scale (ESS)15, 16), the Japanese version of the Insomnia Severity Index (ISI)17, 18), and a question on alcohol intake at bedtime (times per week). In PSQI, ESS and ISI, higher scores indicate worse conditions.
Statistical analysis
Continuous variables in the two groups were compared using the Student t-test. Continuous variables at baseline and 1 month later were compared using the paired t-test. Proportions in the two groups were compared using the chi-squared test. The proportions before and after the program were compared using McNemar’s test. Interaction between groups (‘continued no alcohol intake’, ‘stopped intake’ and ‘continued intake’) and time (at baseline vs. 1 month later) was tested by mixed model analysis of variance (ANOVA). The significance level was set at 5%. IBM SPSS Statistics 19 was used for statistical analysis.
RESULTS
The percentage of habitual alcohol intake at bedtime at baseline and approximately 1 month after the program is presented in Table 1. The percentage of subjects with habitual alcohol intake at bedtime was significantly decreased (38.5% (15 of 39) to 20.5% (8 of 39), p=0.04). Among the 15 subjects who habitually consumed alcohol at bedtime at baseline (12 of 23 men (52.2%), three of 16 women (18.8%)), eight (53.3%) stopped alcohol intake at bedtime after the sleep education program. However, one subject started to intake alcohol at bedtime after the program.
Table 1.
Proportion with habitual alcohol intake at bedtime and sleep conditions at baseline and 1 month after the program
| n | Baseline | 1 month later | Pa | |
|---|---|---|---|---|
| Habitual alcohol intake at bedtime, n (%) | 39 | 15 (38.5%) | 8 (20.5%) | 0.04a |
| PSQI (score, mean ± SD) | 34 | 5.3 ± 2.4 | 5.1 ± 2.9 | 0.42b |
| ESS (score, mean ± SD) | 39 | 8.3 ± 3.2 | 7.1 ± 4.1 | 0.04b |
| ISI (score, mean ± SD) | 39 | 6.9 ± 4.2 | 5.9 ± 4.3 | 0.07b |
| Sleep duration (min, mean ± SD) | 40 | 389.3 ± 48.7 | 379.1 ± 57.8 | 0.02b |
a: McNemar test, b: paired Student t-test
PSQI: Pittsburgh Sleep Quality Index; ESS: Epworth Sleepiness Scale; ISI: Insomnia Severity Index; SD: standard deviation.
The self-rated sleep conditions from the first questionnaire and the one approximately a month later are shown in Table 1. The mean ESS score was significantly decreased by 1.2 points (p=0.04), while the mean sleep duration was significantly decreased by 10 minutes (p=0.02). The mean ISI score was decreased, but not significantly.
The characteristics of the participants and sleep conditions at baseline by alcohol intake at bedtime are presented in Table 2. Mean age was not significantly different between the group which stopped alcohol intake and the group which continued. The percentage of men in the ‘continued intake’ group was higher than in the ‘stopped intake’ group, although not significantly. All three women and five of 12 men (41.7 %) stopped. The number of times alcohol was taken at bedtime per week at baseline and the proportion taking alcohol at bedtime 5 times or more per week at baseline in the ‘continued intake’ group were significantly higher than in the ‘stopped intake’ group. The PSQI score at baseline in the ‘stopped intake’ group was significantly higher than that in the ‘continued intake’ group. Although not significant, the ESS and the ISI scores at baseline in the ‘stopped intake’ group were higher than those in the ‘continued intake’ group.
Table 2.
Characteristics of groups according to alcohol intake at bedtime
| Continued no alcohol intake at bedtime (n= 23) | Habitual alcohol intake at bedtime at baseline | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Stopped intake(n= 8) | Continued intake (n= 7) |
P (stopped vs. continued) |
|||||||
| n | Baseline | n | Baseline | n | Baseline | ||||
| Age (years, mean ± SD) | 48.0 ± 9.3 | 50.9 ± 6.3 | 49.3 ± 11.2 | 0.74a | |||||
| Men, n (%) | 10 (43.5%) | 5 (62.5%) | 7 (100.0%) | 0.07b | |||||
| Number of times of alcohol intake at bedtime per week at program end (mean ± SD) | – | 3.2 ± 2.4 | 6.9 ± 0.4 | 0.004a | |||||
| Alcohol intake at bedtime 5 times or more per week (%) | – | 2 (25.0%) | 7 (100.0%) | 0.003b | |||||
| PSQI (score, mean ± SD) | 20 | 5.1 ± 2.9 | 7 | 6.3 ± 0.8 | 6 | 4.3 ± 1.5 | 0.01a | ||
| ESS (score, mean ± SD) | 23 | 8.3 ± 3.2 | 7 | 9.4 ± 3.3 | 7 | 7.0 ± 3.4 | 0.20a | ||
| ISI (score, mean ± SD) | 22 | 6.0 ± 4.2 | 8 | 8.9 ± 2.7 | 7 | 5.6 ± 3.5 | 0.06a | ||
| Sleep duration(min, mean ± SD) | 23 | 383.0 ± 56.4 | 8 | 402.5 ± 21.9 | 7 | 402.9 ± 34.0 | 0.98a | ||
a: Student t-test, b: chi-square test, SD: standard deviation.
The sleep conditions at baseline and approximately 1 month after the program in the ‘continued no alcohol intake at bedtime’ group, in the ‘stopped intake’ group and in the ‘continued alcohol intake’ group are shown in Table 3. Although interactions between time (at baseline vs. 1 month later) and alcohol intake at bedtime (‘stopped intake’, ‘continued intake’ and ‘continued no alcohol intake’) were not significant on any sleep parameters owing to the relatively small number of subjects, ESS scores, ISI scores and sleep duration in the ‘stopped alcohol intake’ group decreased more than in the ‘continued’ group and in the ‘continued no alcohol intake’ group.
Table 3.
Change in sleep conditons by groups according to alcohol intake at bedtime
| Continued no alcohol intake (n= 23) | Stopped intake (n= 8) | Continued intake (n= 7) | Pfor | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | Baseline | 1 month later | Pa | n | Baseline | 1 month later | Pa | n | Baseline | 1 month later | Pa | interactionb | |||
| PSQI (score, mean± SD) | 20 | 5.1 ± 2.9 | 4.9 ± 3.4 | 0.65 | 7 | 6.3 ± 0.8 | 6.0 ± 1.8 | 0.63 | 6 | 4.3 ± 1.5 | 4.2 ± 2.1 | 0.77 | 0.99 | ||
| ESS (score, mean± SD) | 23 | 8.3 ± 3.2 | 7.2 ± 3.7 | 0.14 | 7 | 9.4 ± 3.3 | 6.9 ± 4.7 | 0.18 | 7 | 7.0 ± 3.4 | 5.9 ± 3.8 | 0.20 | 0.63 | ||
| ISI (score, mean± SD) | 22 | 6.0 ± 4.2 | 5.6 ± 4.6 | 0.47 | 8 | 8.9 ± 2.7 | 6.8 ± 3.8 | 0.33 | 7 | 5.6 ± 3.5 | 4.7 ± 4.4 | 0.47 | 0.51 | ||
| Sleep duration (min, mean± SD) | 23 | 383.0 ± 56.4 | 372.6 ± 64.8 | 0.09 | 8 | 402.5 ± 21.9 | 380.0 ± 50.1 | 0.08 | 7 | 402.9 ± 34.0 | 405.0 ± 33.5 | 0.77 | 0.24 | ||
a: Student paired t-test; b: mixed model analysis of variance; SD: standard deviation.
DISCUSSION
The ESS score was significantly decreased after the program, while sleep duration was significantly shortened. Shortened sleep duration coincided with a decrease in sleepiness. This may indicate an improvement in sleep quality. The most marked effect of the sleep education program was to stop alcohol intake at bedtime. Approximately half of the subjects who had habitual alcohol intake at bedtime stopped taking alcohol at bedtime after the program. Although a 1-day sleep education program promoted a reduction in sleepiness and symptoms related to sleep problems according to the ESS (1.2-point average reduction) and the ISI (1.1-point average reduction) in all subjects, subjects who stopped alcohol intake at bedtime received the most benefit, with a greater decrease in sleepiness and symptoms related to sleep problems as evaluated by ESS (2.6-point average reduction) and ISI (2.1-point average reduction).
The risks of sleep related breathing disorder resulting from alcohol intake at bedtime were explained in the program. In the education program, a slide showing low arterial oxygen saturation during sleep caused by alcohol intake in an obstructive sleep apnea patient was presented (Appendix 1). We believe that this data in a clinical setting may promote stopping alcohol intake, by providing a better understanding of the risk of alcohol intake, although data why the participants stopped alcohol intake at bedtime was not available.
Alcohol consumption is one of the risk factors for sleep apnea19, 20) and is associated with difficulty in maintaining sleep and early morning awakening21). The proportion of alcohol use as a sleep aid one or more times per week is 48.3% among men and 18.3% among women in the general Japanese population22), similar to the proportions of alcohol intake at bedtime in the subjects in this study. If a sleep education program similar to that used in this study was to be widely conducted in future, half of those with habitual alcohol intake at bedtime in the general population could conceivably stop alcohol intake at bedtime. Thus sleep education might contribute to a reduction in the general population of sleep problems and health problems resulting from alcohol intake at bedtime in future.
Bedtime alcohol drinkers who continued alcohol intake after the program tended to take alcohol every night, many were men, and they had relative low PSQI, ESS, and ISI scores. They might not want to stop alcohol intake at bedtime because they might consider it unnecessary to improve sleep by self-rated good sleep. In contrast, bedtime alcohol drinkers who stopped alcohol intake after the intervention tended not to take alcohol every night, many were women, and they had relative high PSQI, ESS, and ISI scores. If these populations who are conscious of their poor sleep with alcohol intake at bedtime could be targeted in future programs, there might be easily gained benefits in these populations.
This study had some limitations. First, the study design had some flaws. The preliminary study did not have a control group and selection bias of subjects might have occurred. Second, the number of subjects was small, especially in the sub-analysis by alcohol intake at bedtime. Third, the subjects knew the aim of the study. The subjects might have reported more effects, because of using a self-administered questionnaire. Objective measurement such as actigraphy could be included in future studies.
In conclusion, the 1-day sleep education program contributed to stopping alcohol intake at bedtime which may lead to improved sleep conditions. Therefore, this program offers the possibility of improving sleep conditions among the general population, especially those with habitual alcohol intake at bedtime. Further larger, randomized, controlled studies are warranted.
REFERENCES
- 1).Ford DE, Kamerow DB. Epidemiologic study of sleep disturbances and psychiatric disorders. An opportunity for prevention? JAMA 1989; 262: 1479–84. [DOI] [PubMed]
- 2).Fujino Y, Mizoue T, Tokui N, Yoshimura T. Prospective cohort study of stress, life satisfaction, self-rated health, insomnia, and suicide death in Japan. Suicide Life Threat Behav 2005; 35: 227–37. [DOI] [PubMed]
- 3).Chang PP, Ford DE, Mead LA, Cooper-Patrick L, Klag MJ. Insomnia in young men and subsequent depression. The Johns Hopkins Precursors Study. Am J Epidemiol 1997; 146: 105–14. [DOI] [PubMed]
- 4).Kim K, Uchiyama M, Okawa M, Liu X, Ogihara R. An epidemiological study of insomnia among the Japanese general population. Sleep 2000; 23: 41–7. [PubMed]
- 5).Gallicchio L, Kalesan B. Sleep duration and mortality: a systematic review and meta-analysis. J Sleep Res 2009; 18: 148–58. [DOI] [PubMed]
- 6).Tamakoshi A, Ohno Y; JACC Study Group. Self-reported sleep duration as a predictor of all-cause mortality: results from the JACC study, Japan. Sleep 2004; 27: 51–4. [PubMed]
- 7).Nagai M, Hoshide S, Kario K. Sleep duration as a risk factor for cardiovascular disease- a review of the recent literature. Curr Cardiol Rev 2010; 6: 54–61. [DOI] [PMC free article] [PubMed]
- 8).Gottlieb DJ, Punjabi NM, Newman AB, Resnick HE, Redline S, Baldwin CM. Nieto FJ. Association of sleep time with diabetes mellitus and impaired glucose tolerance. Arch Intern Med. 2005; 165: 863–7. [DOI] [PubMed]
- 9).Heslop P, Smith GD, Metcalfe C, Macleod J, Hart C. Sleep duration and mortality: The effect of short or long sleep duration on cardiovascular and all-cause mortality in working men and women. Sleep Med. 2002; 3: 305–14. [DOI] [PubMed]
- 10).Soldatos CR, Allaert FA, Ohta T, Dikeos DG. How do individuals sleep around the world? Results from a single-day survey in ten countries. Sleep Med. 2005; 6: 5–13. [DOI] [PubMed]
- 11).Kakinuma M, Takahashi M, Kato N, Aratake Y, Watanabe M, Ishikawa Y, Kojima R, Shibaoka M, Tanaka K. Effect of brief sleep hygiene education for workers of an information technology company. Ind Health. 2010; 48: 758–65. [DOI] [PubMed]
- 12).Miyazaki S. Pathology and surgical treatment for Sleep Apnea Syndrome. Oto-Rhino-Laryngology, Tokyo 2002; 45: 10–17.
- 13).Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989; 28: 193–213. [DOI] [PubMed]
- 14).Doi Y, Minowa M, Utiyama S, Okawa M. Development of the Japanese version of the Pittsburgh Sleep Quality Index. Japanese Journal of Psychiatry Treatment. 1998; 13: 755–763. (Article in Japanese).
- 15).Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep 1991; 14: 540–5. [DOI] [PubMed]
- 16).Takegami M, Suzukamo Y, Wakita T, Noguchi H, Chin K, Kadotani H, Inoue Y, Oka Y, Nakamura T, Green J, Johns MW, Fukuhara S. Development of a Japanese version of the Epworth Sleepiness Scale (JESS) based on item response theory. Sleep Med. 2009; 10: 556–65. [DOI] [PubMed]
- 17).Bastien CH, Vallières A, Morin CM. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med. 2001; 2: 297–307. [DOI] [PubMed]
- 18).Munezawa T, Morin CM, Inoue Y, Nedate K. Development of the Japanese version of the Insomnia Severity Index (ISI-J). Japanese Journal of Psychiatry Treatment. 2009; 24: 219–225. (in Japanese)
- 19).Lam JC, Sharma SK, Lam B. Obstructive sleep apnea: definitions, epidemiology & natural history. Indian J Med Res. 2010; 131: 165–70. [PubMed]
- 20).Tsutsumi W, Miyazaki S, Itasaka Y, Togawa K. Influence of alcohol on respiratory disturbance during sleep. Psychiatry Clin Neurosci. 2000; 54: 332–3. [DOI] [PubMed]
- 21).Kaneita Y, Ohida T, Takemura S, Sone T, Suzuki K, Miyake T, Yokoyama E, Umeda T. Relation of smoking and drinking to sleep disturbance among Japanese pregnant women. Prev Med. 2005; 41: 877–82. [DOI] [PubMed]
- 22).Kaneita Y, Uchiyama M, Takemura S, Yokoyama E, Miyake T, Harano S, Asai T, Tsutsui T, Kaneko A, Nakamura H, Ohida T. Use of alcohol and hypnotic medication as aids to sleep among the Japanese general population. Sleep Med. 2007; 8: 723–32. [DOI] [PubMed]