ABSTRACT
A spontaneous cervical epidural hematoma (SCEH) is a rare condition, which usually requires urgent treatment. However, unusual manifestations, such as hemiparesis, may lead to a misdiagnosis. We herein report a case of SCEH that presented with pure motor hemiparesis to discuss the appropriate and prompt diagnosis and treatment of such cases. An 84-year-old female was brought to our emergency department complaining of nuchal pain, followed by right hemiparesis. A contrast-enhanced computed tomography (CT) scan of the neck demonstrated a spinal epidural hematoma right posterolateral to the spinal cord, extending from C2 to C3. She was managed conservatively and her symptoms improved significantly. The authors emphasize that cervical spinal lesions should be considered in the differential diagnosis for patients with acute onset of hemiparesis, when they are associated with neck pain. Even though magnetic resonance imaging is the gold standard, a CT scan is also useful for quick screening for SCEH.
Key words: spinal epidural hematoma, hemiparesis, cerebrovascular stroke, diagnosis, spontaneous remission
INTRODUCTION
A spontaneous cervical epidural hematoma (SCEH) is a rare disease entity. It is usually manifested by neurological syndromes such as tetraparesis, paraparesis or Brown-Sequard syndrome. SCEH presenting with pure motor hemiparesis is extremely rare, and may be mistaken for cerebrovascular stroke.1,2,3) Although magnetic resonance imaging (MRI) is generally considered to be the most reliable diagnostic tool, it may not be available in certain situations. For example, it can take a long time, especially when an extended area of the central nervous system must be examined quickly. We herein report a case of SCEH with pure motor hemiparesis in which a cervical computed tomography (CT) scan was obtained on admission and led to the rapid and correct diagnosis. This patient was treated without surgery, and her neurological symptoms resolved completely. The appropriate diagnosis and management of SCEH is also discussed.
CASE REPORT
An 84-year-old female was brought to the emergency department after the sudden onset of neck pain, followed by right motor weakness. The pain started while she was washing her back. She had no remarkable past medical history and was not regularly taking any medication. On neurologic examination, the motor strength of her right extremities was classified as one out of five, while there was no motor weakness of right facial muscles. Her sensory function was totally preserved. Her deep tendon reflexes were hyperactive on the right side. Her mental status, cognitive function, speech and facial movements were normal. However, her blood pressure was 185/105 mmHg. Routine laboratory and diagnostic studies, including coagulation parameters, were all within normal limits. A brain CT scan showed no hemorrhagic lesion, but a small cavernous angioma in the left postcentral gyrus was present, which was considered irrelevant to the present condition.
The paresis improved to some extent, and a cerebral ischemic accident was strongly suspected. However, the patient complained of persistent neck pain. Therefore, a contrast enhanced CT was performed to rule out cervical lesions. The scan revealed a slightly high-density mass posterolateral to the spinal cord extending from C2 to C3, compatible with an epidural hematoma (Fig. 1). No apparent extravasation or abnormal accumulation of the contrast medium was observed. She was administered nitroglycerin for hypertension. A cervical MRI obtained two days after onset was also compatible with an epidural hematoma (Fig. 2). No neoplasms or vascular malformations were suspected as a causative factor. Angiography was non-contributory.
Fig. 1.
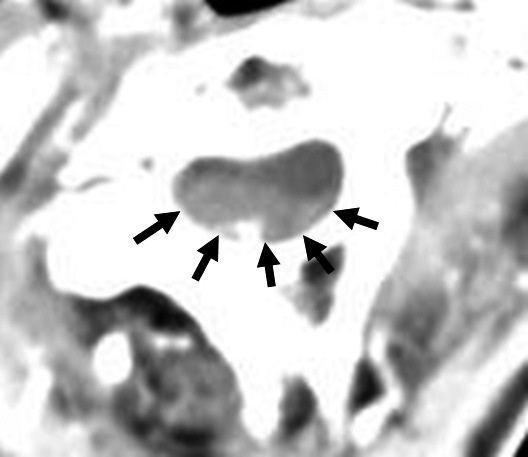
An axial section of computed tomography of the cervical spine. A hematoma at C2–3 compressed the spinal cord (arrows).
Fig. 2.
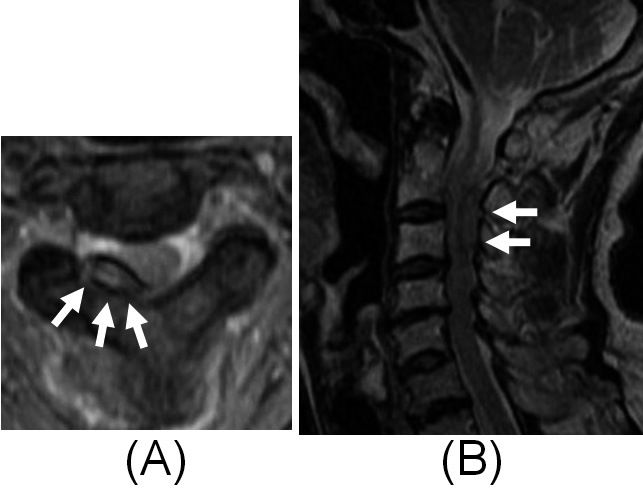
Magnetic resonance images of the cervical spine which were obtained on the third day after the onset. Axial (A) and sagittal (B) T2WIs show an extradural mass with hyperintensity that compressed the spinal cord (arrows).
Her symptoms improved gradually after hospitalization and she began ambulation on the following day with improved motor strength to 4+/5 on the right. A repeated MRI on the 7th day showed that the hematoma was in the process of absorption. She was discharged with a normal neurological function on the 9th day after onset. She had no recurrence of the symptom during one year of follow up period.
DISCUSSION
Spinal epidural hematoma is a rare disease; its incidence is estimated to be only 0.1 per 100,000 patients per year.4) It has characteristic symptoms, such as paraparesis or tetraparesis with radiating neck or back pain and sensory deficit. To our knowledge, only 3 cases of SCEH presenting with pure motor hemiparesis have been reported.1,3,5) All of the reported cases were misdiagnosed as cerebral ischemia and erroneously treated with anticoagulant therapy. The absence of facial weakness or cranial signs suggested that hemiparesis was due to a lesion in the cervical spinal cord.1,3) The present case developed sudden hemiparesis after neck pain and was brought to our hospital 40 minutes after the onset. A CT scan of the head and neck was performed within 30 minutes after arrival, which eventually revealed SCEH. Even though the enhancement of contrast medium is limited to the arterial phase, it often provides valuable diagnostic information.
Many previous authors have reported that a CT scan could elucidate cervical spinal hematomas. However, Börm et al. reported that CT failed to make the diagnosis in one case. A plain CT scan was reported to be helpful in detecting the location of a cervical subdural hematoma.6) Nevertheless, the possibility of misdiagnosis still remains. This risk is higher when the thoracic and lumbar region are affect, probably because of air artifacts within the thoracic and peritoneal cavity.7,8) Therefore, MRI has been suggested to be the procedure of choice because of its capabilities for tissue differentiation. Nevertheless, when limited to the cervical spine, CT also yields acceptable results. Considering the short period of time for the optimal treatment of acute brain ischemia, cervical CT should be chosen to exclude a spinal hematoma prior to administering potentially harmful anti-coagulant therapy, especially if the patient complains of neck pain.
The mechanism underlying the development of SCEH remains unclear. The majority of cases have been reported as spontaneous, while coagulation disorders or anticoagulation therapy have also been implied as predisposing conditions.4,7) In addition, the previous papers have pointed out other causative backgrounds, such as a vascular malformation, tumor, trauma, lumbar puncture and spinal anesthesia. Groen et al. reported that the posterior internal vertebral venous plexus plays an important role in spinal epidural hematoma, by investigating clinical cases and human cadavers.9,10) Holtas et al. reported that SCEH was located predominantly in the anterior epidural space.4)
In the current case, the location of the SCEH was dorsolateral to the spinal cord. These findings supported the hypothesis that the posterior internal vertebral venous plexus was the bleeding source. The network of the epidural venous plexus is thought to be especially vulnerable to venous pressure because it lacks valves. It is speculated that increased venous pressure induced by physical activity can result in the rupture of the vessels.11) The neck pain in the present case began when the patient raised her arms to wash herself. This could have caused such an increase in the venous pressure.
Spontaneous resolution of SCEH has been reported in only a few cases; each occurred within the setting of unilateral hemiparesis and dysesthesia.2,12) SCEH cases with acute neurological deficits usually require immediate surgical decompression.13) However, if the neurological symptoms are minimal or improving rapidly, conservative management is an alternative choice.
CONCLUSION
SCEH may manifest as pure motor paresis with sudden neck pain. Even in the MRI era, a cervical CT scan is still a reasonable choice for making a quick differential diagnosis of SCEH, when considering the therapeutic time window available for the treatment of brain ischemia.
REFERENCES
- 1).Hsieh CF, Lin HJ, Chen KT, Foo NP, Te AL. Acute spontaneous cervical spinal epidural hematoma with hemiparesis as the initial presentation. Eur J Emerg Med, 2006; 13: 36. 38. [DOI] [PubMed]
- 2).Marinella MA, Barsan WG. Spontaneously resolving cervical epidural hematoma presenting with hemiparesis. Ann Emerg Med, 1996; 27: 514. 517. [PubMed]
- 3).Wang CC, Chang CH, Lin HJ, Lin KC, Kuo JR. Misdiagnosis of spontaneous cervical epidural haemorrhage. Eur Spine J, 2009; 18 (Suppl 2): 210. 212. [DOI] [PMC free article] [PubMed]
- 4).Holtås S, Heiling M, Lönntoft M. Spontaneous spinal epidural hematoma: findings at MR imaging and clinical correlation. Radiology, 1996; 199: 409. 413. [DOI] [PubMed]
- 5).Oh SH, Han IB, Koo YH, Kim OJ. Acute spinal subdural hematoma presenting with spontaneously resolving hemiplegia. Journal of Korean Neurosurgical Society, 2009; 45: 390. 393. [DOI] [PMC free article] [PubMed]
- 6).Post MJ, Becerra JL, Madsen PW, Puckett W, Quencer RM, Bunge RP, Sklar EM. Acute spinal subdural hematoma: MR and CT findings with pathologic correlates. AJNR Am J Neuroradiol, 1994; 15: 1895. 1905. [PMC free article] [PubMed]
- 7).Börm W, Mohr K, Hassepass U, Richter HP, Kast E. Spinal hematoma unrelated to previous surgery: analysis of 15 consecutive cases treated in a single institution within a 10-year period. Spine, 2004; 29: E555. 561. [DOI] [PubMed]
- 8).Boye S, Schumacher J. Diagnosis of vertebral canal haematoma by myelography and spiral computer tomography in a patient with an implantable cardioverter-defibrillator contraindicating magnetic resonance imaging. Br J Anaesth, 2009; 103: 137. 138. [DOI] [PubMed]
- 9).Groen RJ, Grobbelaar M, Muller CJ, van Solinge G, Verhoof O, du Toit DF, Hoogland PV. Morphology of the human internal vertebral venous plexus: a cadaver study after latex injection in the 21–25-week fetus. Clin Anat, 2005; 18: 397. 403. [DOI] [PubMed]
- 10).Groen RJ, Groenewegen HJ, van Alphen HA, Hoogland PV. Morphology of the human internal vertebral venous plexus: a cadaver study after intravenous Araldite CY 221 injection. Anat Rec, 1997; 249: 285. 94. [DOI] [PubMed]
- 11).Groen RJ, Ponssen H. The spontaneous spinal epidural hematoma. A study of the etiology. J Neurol Sci, 1990; 98: 121. 138. [DOI] [PubMed]
- 12).Kim IY, Kim SH, Kim JH, Lee JK. Rapid spontaneous resolution of a traumatic cervical epidural haematoma. Br J Neurosurg, 2005; 19: 451–452. [DOI] [PubMed]
- 13).Liao CC, Hsieh PC, Lin TK, Lin CL, Lo YL, Lee SC. Surgical treatment of spontaneous spinal epidural hematoma: a 5-year experience. J Neurosurg Spine, 2009; 11: 480. 486. [DOI] [PubMed]


