Abstract
Intravenous (IV) administration of iodinated contrast agents (ICAs) is frequently employed for image enhancement while performing radiographic studies such as computed tomography and angiography. Complications related to IV administration of ICAs such as immediate hypersensitivity reactions and nephrotoxicity are well-known. However, severe skin and soft tissue injuries and acute compartment syndrome resulting from contrast extravasation are rare. This is especially so with small volume extravasation of a low osmolar, nonionic ICA such as iohexol. Here, we report a 63-year-old woman who developed acute compartment syndrome of left hand following iohexol extravasation and had swelling, blistering, cutaneous and soft tissue necrosis. She underwent fasciotomy for acute compartment syndrome of hand and later surgical debridement of necrotic skin and soft tissues was carried out. Clinical pharmacology of ICAs, extravasation injuries following their IV administration, their management and measures to reduce them are discussed in brief.
Keywords: Compartment syndrome, complication, contrast agent, extravasation, skin necrosis
INTRODUCTION
Intravenous (IV) administration of iodinated contrast agents (ICAs) is frequently employed for image enhancement while performing computed tomography (CT), angiography and other radiographic studies. Adverse effects reported following IV administration of ICAs include nausea, vomiting, pain after injection, cutaneous hypersensitivity reactions, nephrotoxicity, hypotension and severe systemic hypersensitivity reactions such as anaphylaxis.[1] However, acute compartment syndrome of hand and severe skin and soft tissue injuries resulting from extravasation of ICAs are rare. Here, we report a 63-year-old woman who developed acute compartment syndrome of left hand following iohexol extravasation and had swelling, blistering, cutaneous and soft tissue necrosis.
CASE REPORT
A 63-year-old woman, without significant medical past, was admitted to emergency department with worsening breathlessness for 2 days. She had intermittent cough, mucoid expectoration, and breathlessness for the prior 3 years. There was no history of chest pain, fever and worsening of cough or expectoration. Electrocardiogram showed sinus tachycardia, right axis deviation and right ventricular strain pattern. Echocardiography revealed dilated right atrium and ventricle, with a paradoxical ventricular septal motion. With a high clinical suspicion of acute pulmonary embolism, CT-pulmonary angiography was planned. Injection of 100 ml of radiocontrast OPTISCAN™-300, containing iohexol (organic iodine content: 300 mg/ml, osmolarity: 465 mOsm/l, manufactured by Genetek Biosciences, Nagpur, India) was started through a 20 gauge venous cannula placed on the dorsum of left hand, with a mechanical bolus injector at a rate of 4.5 ml/s. After starting injection, patient complained of swelling and pain in the left hand. Further injection of contrast was stopped and extravasation of about 20 ml iohexol was noted.
Over next 12 h, there was progressive swelling, skin erythema, blistering and early cutaneous gangrenous changes were noted at the extravasation site [Figure 1]. She was initially managed conservatively, by elevation of left upper limb above heart level, local cold compresses and analgesics. She complained of paraesthesias and had severe pain on passive extension of fingers, with a slow capillary refill in fingers. With suspicion of acute compartment syndrome of hand, surgical consultation was sought. Fifteen hours after extravasation, longitudinal incisions were made through the second and fourth metacarpal ridges on the dorsum of left hand, to relieve pressure in the dorsal interosseous compartments. CT-pulmonary angiography done subsequently revealed emphysematous changes of lungs and ruled out pulmonary embolism. She was treated for acute exacerbation of chronic obstructive pulmonary disease. Necrotic changes of skin and soft tissues [Figure 2] were noted 60 h after the extravasation and empiric antibiotic coverage with co-amoxiclav (1.2 g IV 8 hourly) and levofloxacin (500 mg IV once daily) was started. Surgical debridement of gangrenous skin and soft tissues was carried out 80 h after extravasation. At 3 months follow-up, the wound on dorsum of left hand has healed by secondary intention.
Figure 1.
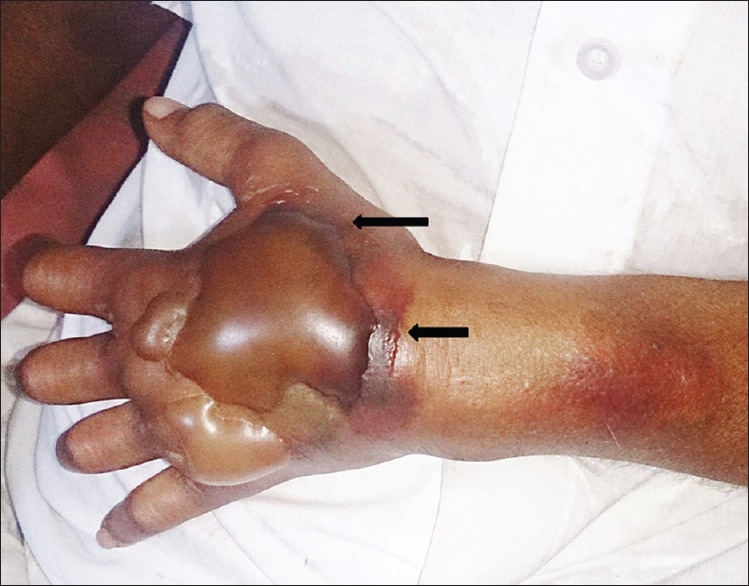
Extensive swelling, cutaneous erythema, blistering and gangrenous changes of the skin (arrows) over dorsum of left hand, noted 12 h after extravasation
Figure 2.

Necrotic changes of the skin and soft tissues (arrow), ulceration and exposure of underlying muscles and tendons noticed 60 h after extravasation
DISCUSSION
ICAs are broadly categorized into ionic and nonionic compounds and each group has monomeric and dimeric agents, with one and two tri-iodinated benzene rings respectively.[1] The charged ionic agents have a carboxylate functional group (-COO-) on an organic side chain. They tend to disrupt the electrical potential of cell membranes and hence, carry increased toxicity. Ionic monomers are hyperosmolar (approximate osmolarity = 1500–2000 mOsm/l) compared to plasma. Low osmolarity ICAs (ionic dimers and nonionic monomers, approximate osmolarity = 290–860 mOsm/l) and agents iso-osmolar with plasma (nonionic dimers) are much less toxic compared to hyperosmolar agents.[1]
Extravasation involving ICAs is an infrequent complication and the usual consequences include swelling or tightness and mild burning or stinging pain at the injection site. Extravasation can occur both during hand injection and mechanical bolus injection of ICA. Reported incidence of contrast extravasation related to IV mechanical bolus injection of ICAs for CT scans ranges from 0.1% to 0.9%.[2] Most extravasations involve skin and subcutaneous tissues and are clinically inconsequential. Infrequently extravasation elicits a brisk local inflammatory response, which peaks in 24–48 h.
The severity of extravasation injury depends on the volume of ICA extravasated and its osmolarity. ICAs with high osmolarity are more likely to cause severe extravasation injuries.[2] Severe complications following extravasation of nonionic, low-osmolar ICAs are rare and reported to occur with large volume (>100 ml) extravasation.[3] Apart from skin toxicity manifested by swelling, cutaneous erythema, blistering and gangrenous changes, other reported severe complications include acute compartment syndrome and brachial plexopathy.[3] The frequency of extravasation after mechanical bolus injection is higher than that reported with hand-injection or drip-infusion techniques.[4] Employing high flow rates during contrast injection, use of smaller caliber peripheral venous cannulae such as 22 gauge cannula for injection and location of the cannula on hand increase the risk of extravasation.[5] Apart from hand, other high-risk sites include wrist, foot and ankle.[2] Patient-related factors that increase the risk of extravasation include altered consciousness, elderly, infants and children, who cannot communicate properly, severely ill and debilitated patients, malnourishment with poor muscle mass and subcutaneous tissue atrophy, presence of peripheral arterial disease, venous thrombosis or insufficiency and prior chemotherapy. Surgery and radiation therapy to the limb to be injected increase the risk of extravasation, by compromising lymphatic drainage.[2,4] Acute compartment syndrome of hand and severe skin and soft tissue injuries occurred in the index patient despite low volume extravasation of iohexol, a nonionic low osmolar monomeric ICA.[1] Injection over the dorsum of hand might have contributed to severe extravasation injury in the index case.
As the severity of extravasation injury may not be evident immediately, observation for several hours is required. There is no consensus regarding best approach for the management of extravasation. Elevation of the limb involved is useful to reduce edema. Although there is dearth of evidence, both cooling the injection site with ice packs to limit inflammation and application of warm compresses to hasten the redistribution and absorption of the contrast and to improve the blood flow distal to the site of extravasation have been tried.[2] Injection of steroids and hyaluronidase locally has been employed to limit the inflammation and enable rapid redistribution and absorption of the contrast respectively, although their efficacy is yet to be proven.[2,4] Immediate aspiration of extravasated hyperosmolar contrast agents through a needle or angiocatheter and saline washout has been reported to prevent skin and soft tissue necrosis associated with extravasation.[6]
Management is mainly conservative. Surgical consultation is indicated when there are extensive cutaneous blistering and gangrenous changes, diminished sensations or paraesthesias, motor deficits and evidence of compromised perfusion such as slow capillary refilling distal to extravasation site.[2] The latter features suggest acute compartment syndrome and should prompt urgent consideration of fasciotomy. Stellate ganglion block and intra-arterial nitroglycerin have been employed to counteract vasospasm provoked by extravasation in upper limb and to limit injury.[7] There have been only a few reported cases of acute compartment syndrome of hand resulting from ICA extravasation.[3,8,9]
Extravasation injuries can be reduced by preferring freshly placed larger IV accesses at the antecubital fossa, meticulous supervision of injection, preferring nonionic low osmolar ICAs and using mechanical bolus injectors fitted with an extravasation detection accessory[10] capable of detecting extravasation early. The latter detects extravasation based on the changes of skin electrical impedance at the extravasation site.
CONCLUSION
To conclude, extravasation of ICAs, although largely inconsequential, can rarely produce severe skin and soft tissue injuries and acute compartment syndrome of hand. Careful supervision of injection procedure, opting for a freshly placed large bore peripheral venous access in the antecubital fossa and preference to nonionic low osmolar ICAs can reduce this complication.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Pasternak JJ, Williamson EE. Clinical pharmacology, uses, and adverse reactions of iodinated contrast agents: A primer for the non-radiologist. Mayo Clin Proc. 2012;87:390–402. doi: 10.1016/j.mayocp.2012.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Reston, Virginia, USA: The American College of Radiology; 2015. American College of Radiology Committee on Drugs and Contrast Media. ACR manual on contrast media. Ver. 10.1; pp. 17–20. [Google Scholar]
- 3.Wang CL, Cohan RH, Ellis JH, Adusumilli S, Dunnick NR. Frequency, management, and outcome of extravasation of nonionic iodinated contrast medium in 69,657 intravenous injections. Radiology. 2007;243:80–7. doi: 10.1148/radiol.2431060554. [DOI] [PubMed] [Google Scholar]
- 4.Federle MP, Chang PJ, Confer S, Ozgun B. Frequency and effects of extravasation of ionic and nonionic CT contrast media during rapid bolus injection. Radiology. 1998;206:637–40. doi: 10.1148/radiology.206.3.9494479. [DOI] [PubMed] [Google Scholar]
- 5.Wienbeck S, Fischbach R, Kloska SP, Seidensticker P, Osada N, Heindel W, et al. Prospective study of access site complications of automated contrast injection with peripheral venous access in MDCT. AJR Am J Roentgenol. 2010;195:825–9. doi: 10.2214/AJR.09.3739. [DOI] [PubMed] [Google Scholar]
- 6.Vandeweyer E, Heymans O, Deraemaecker R. Extravasation injuries and emergency suction as treatment. Plast Reconstr Surg. 2000;105:109–10. doi: 10.1097/00006534-200001000-00019. [DOI] [PubMed] [Google Scholar]
- 7.Lee CC, Chuang CC, Liou JY, Hsieh YC, Tsou MY, Chen KH. Successful management of contrast medium extravasation injury through stellate ganglion block and intra-arterial nitroglycerin. Acta Anaesthesiol Taiwan. 2011;49:116–8. doi: 10.1016/j.aat.2011.07.003. [DOI] [PubMed] [Google Scholar]
- 8.Belzunegui T, Louis CJ, Torrededia L, Oteiza J. Extravasation of radiographic contrast material and compartment syndrome in the hand: A case report. Scand J Trauma Resusc Emerg Med. 2011;19:9. doi: 10.1186/1757-7241-19-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Selek H, Ozer H, Aygencel G, Turanli S. Compartment syndrome in the hand due to extravasation of contrast material. Arch Orthop Trauma Surg. 2007;127:425–7. doi: 10.1007/s00402-006-0238-y. [DOI] [PubMed] [Google Scholar]
- 10.Birnbaum BA, Nelson RC, Chezmar JL, Glick SN. Extravasation detection accessory: Clinical evaluation in 500 patients. Radiology. 1999;212:431–8. doi: 10.1148/radiology.212.2.r99au14431. [DOI] [PubMed] [Google Scholar]


