Abstract
Introduction:
Percutaneous nephrolithotomy (PCNL) has witnessed rapid advancements, the latest being ultra-mini-percutaneous nephrolithotomy (UMP), which makes the use of 11–13F sheaths as compared to 24–30F sizes used in conventional PCNL. This miniaturization aims to reduce morbidity and improve patient outcomes. We evaluated the safety and efficacy of UMP and report our ourtcomes.
Patients and Methods:
A total of 120 patients underwent UMP from July 2012 to March 2014. These patients had a single unilateral renal stone measuring between 8 and 20 mm. All patients underwent UMP using a 3F nephroscope, 7.5F inner sheath, and 11F or 13F outer metallic cannula, which served as the Amplatz sheath. Stone fragmentation and clearance were achieved with holmium laser. No nephrostomy or stent was used routinely.
Results:
Complete stone fragmentation was achieved in 114 out of 120 patients (95%) using UMP; whereas the remaining 6 were converted into mini-PCNL using a 12.5F nephroscope and 15F Amplatz sheath. The mean operative time was 39.7 ± 15.4 min, and the mean postoperative hospital stay was 22.3 ± 2.2 h. Postoperatively, 6 (5%) patients had residual fragments measuring ≤4 mm. At the 2 weeks follow-up, the stone-free status was >99% (119/120). There were no significant postoperative complications.
Conclusion:
This study shows UMP to be an effective and safe procedure for managing stones up to 20 mm. This procedure offers an attractive alternative to shock wave lithotripsy and retrograde intrarenal surgery for managing small stones.
Keywords: Nephrolithiasis, percutaneous nephrolithotomy, ultra-mini-percutaneous nephrolithotomy
INTRODUCTION
The management of nephrolithiasis has undergone the complete transformation since the 1980s following the introduction of extracorporeal shock wave lithotripsy (SWL), and endourological procedures such as percutaneous nephrolithotomy (PCNL), ureterorenoscopy (URS), and retrograde intrarenal surgery (RIRS).[1,2] The success of these minimally-invasive therapies has made open surgery for urinary stone disease rare. However, the choice of appropriate treatment from among these minimally-invasive options continues to remain a debatable issue. The desired approach to a certain technique depends on ensuring a fine balance between the success rate in terms of stone clearance versus complications and morbidity associated with it.
SWL is a low-risk procedure, but has high re-treatment rate and continues to have a high incidence of residual fragments despite many advancements in technology.[1,2,3] RIRS is a popular procedure for small volume nephrolithiasis, especially as the risk of injury to the viscera and bleeding is much lower when compared to PCNL.[4,5] However, flexible ureteroscopy often requires the placement of a Double J stent before and/or after the procedure, and requires a second procedure in the form of re-look or stent removal in a large percentage of cases. In addition, the overall stone-free rates and the duration of time required to achieve a stone-free status, are only marginally different from SWL.[3,5,6]
PCNL has established itself as an effective and safe technique that delivers high stone-free rate as well as a shorter overall treatment time.[7,8,9] However, the biggest limitation of PCNL is its relatively higher morbidity, including trauma and bleeding. With growing evidence that a reduced tract size leads to a reduction in morbidity from PCNL,[10,11] recent developments in PCNL have been targeted toward creating a reduced tract size in the attempt to reduce complications. This advancement has led to the development of various minimally-invasive percutaneous approaches (“Minimally-invasive PCNL” [MIP]).[12,13]
“Mini-PCNL” makes use of 12–14F size nephroscope and 15–18F Amplatz sheath, as compared to the normally used 24–30F sized sheaths used in conventional PCNL, in an attempt to bring down the morbidity of the procedure. At the farthest end of the spectrum aiming to miniaturize PCNL, is a 4.85F “all-seeing” needle called the “Micro-perc,” which does not even make use of a working sheath.[14,15] However, as Micro-perc does not employ an Amplatz sheath, irrigation fluid does not have an outlet, and neither can stone fragments and debris be cleared during the procedure as in conventional PCNL.
The latest advancement in the MIP methods is “Ultra-Mini-PCNL (UMP).”[16] “UMP,” as the name suggests, is an attempt to miniaturize the tract size further than Mini-PCNL. UMP makes use of a 1 mm (3F) telescope with a specially designed 7.5F nephroscope that allows the surgeon to carry out PCNL with 11–13F sized sheaths [Figure 1]. The reduction in the size of the tract from 30F to 11F ultimately provides a reduction in the cross-sectional surface area to nearly one-eighth of the original tract size compared to conventional PCNL [Figure 2]. This major reduction in the invasiveness of the procedure may help reduce bleeding and tissue trauma. The objective of this study is to present our initial experience with the first 120 patients with moderate-sized (8–20 mm) kidney stones, who underwent UMP at our center.
Figure 1.
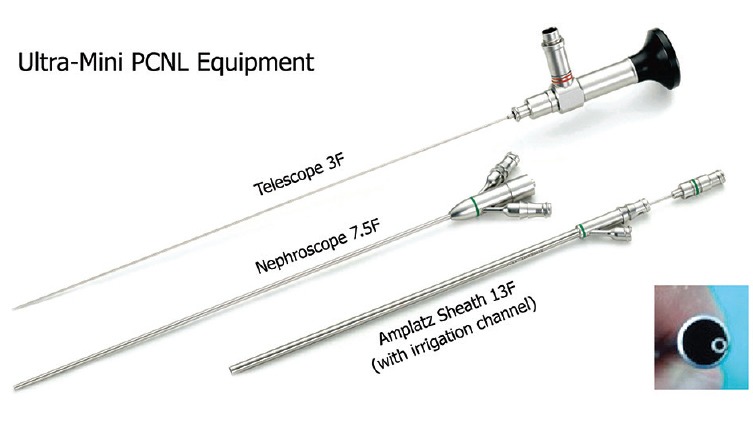
Ultra-mini-percutaneous nephrolithotomy equipment
Figure 2.
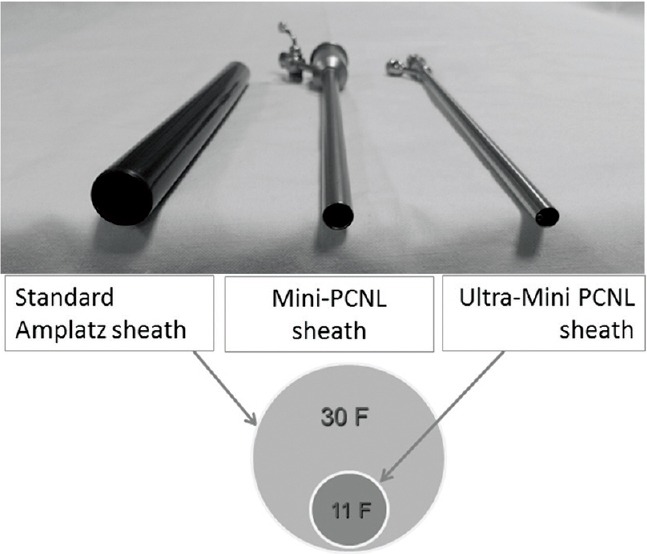
Ultra-mini-percutaneous nephrolithotomy comparison of sheath sizes
PATIENTS AND METHODS
This prospective study was undertaken from July 2012 to June 2014. Institutional Review Board approvaland written informed consent was obtained from all patients before recruitment. Within this period, 628 patients underwent PCNL at our hospital, of which 120 patients were sub-selected who met the inclusion criteria and were recruited to undergo UMP. The remaining 508 patients underwent conventional PCNL (n = 302) or mini-PCNL using 12F nephroscope with 15–18F sheaths (n = 206). During the same period, the number of patients undergoing ureteroscopy and SWL was 456 and 147, respectively.
The inclusion criteria consisted of patients with a single unilateral kidney stone measuring between 8 and 20 mm, normal renal function tests, American Society of Anaesthesiologists score of 1 or 2, lack of any congenital abnormalities, and patient preference for percutaneous stone removal. The other indications were the presence of narrow infundibulum in a caliceal calculus, diverticular renal stones, stones refractory to SWL, and failed flexible ureteroscopy. Patients with multiple stones, anatomical defects, bleeding diathesis, or history of previous open surgery were excluded. A plain abdominal X-ray and renal ultrasonography were done in all patients as the initial screening procedure, followed by computed tomography (CT). Patients who had positive urine cultures were treated with appropriate antibiotics preoperatively.
The “UMP” system (LUT, Germany) consists of a 1 mm (3F) telescope, 7.5F nephroscope inner sheath with three ports (one each for telescope, saline irrigation inlet, and laser fiber), and 11 or 13F metallic outer cannula which serves as the Amplatz sheath [Figure 1]. The basic steps of UMP were the same as conventional PCNL. The procedure was done under epidural (n = 76) or spinal (n = 44) anesthesia. After retrograde ureteric catheterization with a 5F open-ended ureteric catheter, the patient was placed in prone position under a C-arm image intensifier. An 18-gauge trocar tip two-part puncture needle (Cook Urological, USA) was used for puncture through the flank and into the chosen calyx of the kidney. The puncture was performed under combined fluoroscopic and ultrasonic guidance. A hydrophilic nitinol (Terumo, USA), guide wire of size 0.035 in was passed through the needle and the tract was dilated by passing a Teflon dilator over the guide wire. Unlike conventional PCNL, only a single-step dilatation was required. Dilatation was done under fluoroscopic control and the 11F or 13F metal Amplatz cannula was passed with the obturator to provide direct access to the collecting system. The 7.5F nephroscope was then passed through the cannula to visualize the collecting system.
Stones were fragmented under direct visualization using Holmium: YAG laser (Lumenis, USA) using a 365 μ end-firing optical fiber, using power up to 40 W (2.0 J/20 Hz). Stone fragments were washed out using the “water-jet” effect using saline with an irrigation pump. An additional feature of this technique is spontaneous expulsion of stone fragments through the sheath under the influence of the turbulence produced by the irrigation fluid as they are broken up, as opposed to conventional PCNL, where each fragment requires to be manually extracted. The LUT Amplatz cannula is also equipped with an irrigation channel which runs through the whole length of the cannula and allows irrigation or “washing-out” of the pelvi-caliceal system of all the debris at the end of the procedure using a hand-held syringe. This helps in clearing out the kidney of all fragments and achieving a stone-free status on the table.
At the end of the procedure, clearance was confirmed by direct visualization of the collecting system accessible to the telescope, combined with fluoroscopy. As a matter of routine, all procedures were carried out using a “tubeless” approach, leaving only a ureteric catheter and Foley's catheter indwelling overnight. No nephrostomy tube was routinely placed. A Double J stent was not routinely used, except for patients with edema or obstruction at the pelvi-ureteric junction. This was required in 3 patients out of 120. Intravenous paracetamol and tramadol were used for analgesia in all patients postoperatively. Patients were routinely discharged from the hospital the day after the procedure. If a Double J ureteral stent was inserted, it was removed 2 weeks after the procedure at the follow-up visit.
The outcomes that were assessed included operating time, stone clearance rates, postoperative analgesia requirement, morbidity, hospital stay, and time to convalescence. Hemoglobin levels were measured, and a kidney, ureter, and bladder (KUB) X-ray was done in all patients on postoperative day 1 before discharge from the hospital. A noncontrast CT (NCCT) scan was done in all patients at the follow-up visit at 2 weeks to assess the stone-free status of the patients. A later follow-up was arranged for all patients 3 months postoperatively.
RESULTS
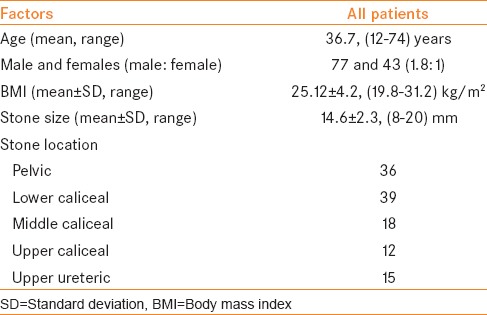
The baseline demographics of the 120 patients included in the study are outlined in Table 1. All patients were operated with a single tract. In 34 patients, access was obtained via a supra-costal (11th inter-costal space) puncture; while in the remaining 86 patients, access was achieved via an infra-costal puncture.
Table 1.
Patient demographics at baseline
The outcomes are outlined in Table 2. Complete fragmentation of stone was achieved with the “UMP” in 114 out of 120 (95%) patients, whereas conversion to “mini-PCNL” (12.5F nephroscope and 15F Amplatz sheath) was required in 6 patients (5%), mainly due to the presence of bleeding and blood clots leading to problems in visualization. The mean operative time, defined as time taken from puncture to Amplatz sheath removal, was 39.7 ± 15.4 min (24.3–68.0) min, whereas the mean time for complete stone fragmentation using laser was 28.5 ± 9.6 (16.7–45.8) min. The mean reduction in levels of hemoglobin postoperatively was 0.4 g/L, and no patient required a blood transfusion. All patients were discharged from the hospital on postoperative day 1; mean hospital stay being 22.3 ± 2.2 h (range 20.3–28.0 h).
Table 2.
Results of patient outcomes
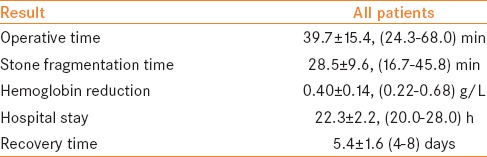
On postoperative KUB X-ray on the 1st postoperative day, 6 (5%) had residual fragments measuring ≤ 4 mm. On the CT scan done at the 2 weeks follow-up, stone-free status of > 99% (119/120) was achieved; whereas one patient had a < 4 mm asymptomatic calculus fragment in lower pole calyx, which was kept on expectant treatment. The mean time to recovery, defined as patients reporting back to work, was 5.4 ± 1.6 (4–8) days.
Mild postoperative fever (>38°C) occurred in 10 patients (Clavien-Dindo grade II), which was treated successfully by antibiotics (amoxicillin-clavulanic acid) for 5–7 days. There were no episodes of uro-sepsis. In two patients, there were episodes of minor secondary hemorrhage between 7th and 10th postoperative days (Clavein-Dindo grade II). These patients presented with mild hematuria, which settled with conservative treatment using antibiotics and hemostatic agents (tranexamic acid) for 2–3 days. Follow-up of patients consisted of out-patients visit to the clinic 2 weeks postoperatively, during which the NCCT scan was performed. No long-term complications were noted in any patient at the 3-month follow-up visit.
DISCUSSION
PCNL has undergone the major changes since it was first described over three decades ago with higher success rates and reduced morbidity. One of the significant changes brought about in recent times has been the reduction of tract size in an attempt to reduce bleeding and tissue trauma, from conventional PCNL using Amplatz sheaths of 24–30F, to “mini-perc” involving 15–18F sheaths and now the UMP at 11–13F.
Following its introduction by Jackman et al., the safety and efficacy of “Mini-PCNL” has been well established in reducing morbidity as compared to conventional PCNL.[17,18,19] Reduction the diameter of the Amplatz sheath not only provides the surgeon adequate working access, but also significantly aids in reducing injury to the renal parenchyma. This has proven to be an effective and safe procedure, and has been shown to allow decreased overall time spent in the hospital, reduced pain, and lesser complications.[20,21]
“UMP” is the latest addition to the armamentarium in the ever-evolving PCNL techniques. The initial results of our cohort of 120 patients undergoing UMP are promising. UMP is technically feasible and appears to be a safe and efficacious alternative for small volume renal calculus disease with an advantage of high immediate and final stone-free rates and low complication rates. The indications for UMP are small and moderate-sized stones, preferably under 20 mm, as an alternative to SWL or RIRS, including lower pole stones which are not amenable to RIRS, diverticular renal stones, and stones refractory to SWL.[22]
The equipment provided clear visualization due to excellent optics with a high-resolution 1-mm diameter telescope. The “water-jet” effect allowed for easy retrieval of stone fragments by spontaneous expulsion, without the need of any graspers or baskets. This expulsion of the fragments occurs secondary to the turbulence created by the sheath and the high-flow plus low-pressure irrigation system. Following stone fragmentation by laser, the nephroscope is withdrawn, and saline is injected through the irrigation port provided in the outer cannula, leading up to the calyx. This leads to an eddy-current phenomenon, which occurs when fluid flows past the stone fragments, and forms a reverse swirling of fluid, causing the fragments to move in the direction of the source of the fluid, out of the calyx, and toward the cannula. This provides for a very effective method of stone expulsion without the need of instrumentation.
UMP is a relatively new procedure, with limited experience worldwide. We started performing UMP in July 2012 and our initial results were presented in the World Congress of Endourology and SWL in 2013.[23] We are a high-volume tertiary care centre and our large experience with PCNL may be contributory to our success with this procedure. The use of laser energy for intra-corporeal lithotripsy in PCNL is also relatively new for most urologists. Whereas higher power with low frequency results in disintegration of stones in large fragments, choosing lower power settings with high-frequency results in the production of fine fragments or a “dusting” effect. Since fragments are cleared spontaneously as they are fragmented under the water-jet effect, the procedure is not unduly time-consuming as would be expected.
The small size of the tract results in lower morbidity in terms of less tissue trauma, less bleeding, and postoperative pain. UMP has the added advantage of being “tubeless” and “stent-free,” that is, a truly “totally tubeless” procedure. Most of the patients are discharged from the hospital on the first postoperative day, the hospital stay being <24 h in the majority of cases. For smaller upper tract stones, as compared with SWL and RIRS, UMP has the promise of providing higher stone-free status in terms of both immediate on-table stone clearance as well as long-term stone-free rates. The additional benefit of avoiding stent-related symptoms or need for a secondary procedure would make it a further attractive proposition. While being equally effective as the alternatives, this technique may have the added advantage of being less expensive than URS, a factor that plays a significant role in developing countries.[24]
The limitation of UMP, however, is the operative time taken to fragment and completely clear stones larger than 2 cm through 11–13F sheaths. Similarly, for larger stone burden, multiple or branched calculi, especially in a significantly dilated pelvi-caliceal system, UMP is unlikely to be able to replace standard PCNL. Thus, the role of this technique appears to be more suitable for low-volume upper tract urolithiasis only. This study is our initial experience with the technique and suffers from the limitation of being a nonrandomized study. Since this was not a blinded controlled trial, nor were these consecutive patients, selection bias in this study cannot be ruled out. Obviously, many of these stones could also have been treated by other modalities including flexible ureteroscopy and SWL. However, the study does point to the feasibility of this technique, and the potential advantages of achieving excellent stone clearance without significant morbidity. This initial promise needs to be validated by randomized prospective trials, which are ongoing, comparing UMP with flexible ureteroscopy and Mini-PCNL.
CONCLUSION
Our study shows UMP to be a safe and effective procedure for the management of urolithiasis, in particular, stones under 20 mm. Initial results are promising enough to suggest this procedure as an alternative to SWL and RIRS for low-volume stone disease, with high stone-free rates and low complications.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Albala DM, Assimos DG, Clayman RV, Denstedt JD, Grasso M, Gutierrez-Aceves J, et al. Lower pole I: A prospective randomized trial of extracorporeal shock wave lithotripsy and percutaneous nephrostolithotomy for lower pole nephrolithiasis-initial results. J Urol. 2001;166:2072–80. doi: 10.1016/s0022-5347(05)65508-5. [DOI] [PubMed] [Google Scholar]
- 2.Muslumanoglu AY, Tefekli A, Sarilar O, Binbay M, Altunrende F, Ozkuvanci U. Extracorporeal shock wave lithotripsy as first line treatment alternative for urinary tract stones in children: A large scale retrospective analysis. J Urol. 2003;170(6 Pt 1):2405–8. doi: 10.1097/01.ju.0000096422.72846.80. [DOI] [PubMed] [Google Scholar]
- 3.Srisubat A, Potisat S, Lojanapiwat B, Setthawong V, Laopaiboon M. Extracorporeal shock wave lithotripsy (ESWL) versus percutaneous nephrolithotomy (PCNL) or retrograde intrarenal surgery (RIRS) for kidney stones. Cochrane Database Syst Rev. 2009;11 doi: 10.1002/14651858.CD007044.pub2. CD007044. [DOI] [PubMed] [Google Scholar]
- 4.Akman T, Binbay M, Ugurlu M, Kaba M, Akcay M, Yazici O, et al. Outcomes of retrograde intrarenal surgery compared with percutaneous nephrolithotomy in elderly patients with moderate-size kidney stones: A matched-pair analysis. J Endourol. 2012;26:625–9. doi: 10.1089/end.2011.0526. [DOI] [PubMed] [Google Scholar]
- 5.Bozkurt OF, Resorlu B, Yildiz Y, Can CE, Unsal A. Retrograde intrarenal surgery versus percutaneous nephrolithotomy in the management of lower-pole renal stones with a diameter of 15 to 20 mm. J Endourol. 2011;25:1131–5. doi: 10.1089/end.2010.0737. [DOI] [PubMed] [Google Scholar]
- 6.Bryniarski P, Paradysz A, Zyczkowski M, Kupilas A, Nowakowski K, Bogacki R. A randomized controlled study to analyze the safety and efficacy of percutaneous nephrolithotripsy and retrograde intrarenal surgery in the management of renal stones more than 2cm in diameter. J Endourol. 2012;26:52–7. doi: 10.1089/end.2011.0235. [DOI] [PubMed] [Google Scholar]
- 7.Agrawal MS, Sharma M, Agarwal K. Tubeless percutaneous nephrolithotomy using antegrade tether: A randomized study. J Endourol. 2014;28:644–8. doi: 10.1089/end.2013.0693. [DOI] [PubMed] [Google Scholar]
- 8.Feng MI, Tamaddon K, Mikhail A, Kaptein JS, Bellman GC. Prospective randomized study of various techniques of percutaneous nephrolithotomy. Urology. 2001;58:345–50. doi: 10.1016/s0090-4295(01)01225-0. [DOI] [PubMed] [Google Scholar]
- 9.Kumar R, Anand A, Saxena V, Seth A, Dogra PN, Gupta NP. Safety and efficacy of PCNL for management of staghorn calculi in pediatric patients. J Pediatr Urol. 2011;7:248–51. doi: 10.1016/j.jpurol.2011.02.016. [DOI] [PubMed] [Google Scholar]
- 10.Kukreja R, Desai M, Patel S, Bapat S, Desai M. Factors affecting blood loss during percutaneous nephrolithotomy: Prospective study. J Endourol. 2004;18:715–22. doi: 10.1089/end.2004.18.715. [DOI] [PubMed] [Google Scholar]
- 11.Ferakis N, Stavropoulos M. Mini percutaneous nephrolithotomy in the treatment of renal and upper ureteral stones: Lessons learned from a review of the literature. Urol Ann. 2015;7:141–8. doi: 10.4103/0974-7796.152927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cheng F, Yu W, Zhang X, Yang S, Xia Y, Ruan Y. Minimally invasive tract in percutaneous nephrolithotomy for renal stones. J Endourol. 2010;24:1579–82. doi: 10.1089/end.2009.0581. [DOI] [PubMed] [Google Scholar]
- 13.Mishra S, Sharma R, Garg C, Kurien A, Sabnis R, Desai M. Prospective comparative study of miniperc and standard PNL for treatment of 1 to 2 cm size renal stone. BJU Int. 2011;108:896–9. doi: 10.1111/j.1464-410X.2010.09936.x. [DOI] [PubMed] [Google Scholar]
- 14.Desai MR, Sharma R, Mishra S, Sabnis RB, Stief C, Bader M. Single-step percutaneous nephrolithotomy (microperc): The initial clinical report. J Urol. 2011;186:140–5. doi: 10.1016/j.juro.2011.03.029. [DOI] [PubMed] [Google Scholar]
- 15.Tepeler A, Armagan A, Sancaktutar AA, Silay MS, Penbegul N, Akman T, et al. The role of microperc in the treatment of symptomatic lower pole renal calculi. J Endourol. 2013;27:13–8. doi: 10.1089/end.2012.0422. [DOI] [PubMed] [Google Scholar]
- 16.Desai J, Solanki R. Ultra-mini percutaneous nephrolithotomy (UMP): One more armamentarium. BJU Int. 2013;112:1046–9. doi: 10.1111/bju.12193. [DOI] [PubMed] [Google Scholar]
- 17.Helal M, Black T, Lockhart J, Figueroa TE. The Hickman peel-away sheath: Alternative for pediatric percutaneous nephrolithotomy. J Endourol. 1997;11:171–2. doi: 10.1089/end.1997.11.171. [DOI] [PubMed] [Google Scholar]
- 18.Jackman SV, Docimo SG, Cadeddu JA, Bishoff JT, Kavoussi LR, Jarrett TW. The “mini-perc” technique: A less invasive alternative to percutaneous nephrolithotomy. World J Urol. 1998;16:371–4. doi: 10.1007/s003450050083. [DOI] [PubMed] [Google Scholar]
- 19.Monga M, Oglevie S. Minipercutaneous nephorlithotomy. J Endourol. 2000;14:419–21. doi: 10.1089/end.2000.14.419. [DOI] [PubMed] [Google Scholar]
- 20.Armagan A, Tepeler A, Silay MS, Ersoz C, Akcay M, Akman T, et al. Micropercutaneous nephrolithotomy in the treatment of moderate-size renal calculi. J Endourol. 2013;27:177–81. doi: 10.1089/end.2012.0517. [DOI] [PubMed] [Google Scholar]
- 21.Chan DY, Jarrett TW. Mini-percutaneous nephrolithotomy. J Endourol. 2000;14:269–72. doi: 10.1089/end.2000.14.269. [DOI] [PubMed] [Google Scholar]
- 22.Desai J, Zeng G, Zhao Z, Zhong W, Chen W, Wu W. A novel technique of ultra-mini-percutaneous nephrolithotomy: Introduction and an initial experience for treatment of upper urinary calculi less than 2 cm. Biomed Res Int 2013. 2013 doi: 10.1155/2013/490793. 490793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Agrawal MS. Experience with ‘ULTRA-MINI’ PCNL. Scientific program for 31 st world congress of endourology and SWL program book. J Endourol. 2013;27(Suppl 1):A87–8. [Google Scholar]
- 24.Schoenthaler M, Wilhelm K, Hein S, Adams F, Schlager D, Wetterauer U, et al. Ultra-mini PCNL versus flexible ureteroscopy: A matched analysis of treatment costs (endoscopes and disposables) in patients with renal stones 10-20 mm. World J Urol. 2015:1–5. doi: 10.1007/s00345-015-1489-4. Epub ahead of print. [DOI] [PubMed] [Google Scholar]


