INTRODUCTION
Acute kidney injury (AKI) is a common clinical syndrome characterized by an abrupt decline of renal function and has been recognized as a major healthcare problem affecting millions of patients worldwide. AKI is strongly associated with increased resource utilization, mortality, and risk for the development of chronic kidney disease (CKD).[1,2,3] In the past decade, a number of definitions regarding AKI (including Risk Injury Failure Loss End-Stage Renal Disease [RIFLE], Acute Kidney Injury Network [AKIN], Kidney Disease Improving Global Outcomes [KIDGO]) have been published, which greatly stimulated the epidemiologic and clinical study of AKI throughout the world. With 1.3 billion people, China is the largest developing country in the world. Although the nationwide community-based survey on the incidence rate of AKI in China is still not available, a number of studies for specific patient groups (such as hospitalized patients, Intensive Care Unit [ICU] patients or children) have been conducted. The present study will evaluate the epidemiology, etiology, and current status of the diagnosis and treatment of AKI in China.
EPIDEMIOLOGY
The incidence of AKI varies widely in China ranging from 0.32% to 44.30% due to the difference of study design and definitions. In a large retrospective study by Fang et al.[4] conducted at Shanghai ZhongShan Hospital, a tertiary comprehensive university hospital, it was found that among 176,155 hospitalized patients, 3.19% of patients experienced an episode of AKI according to the AKIN criteria. Similarly, 2.41% (934/38734) of hospitalized patients were diagnosed with AKI (AKIN criteria) in another retrospective study performed by Lu et al.[5] at Shanghai Renji Hospital. Interestingly, when we looked at the data by Wang et al. at the University of Alabama, the incidence rate of AKI (AKIN criteria) reached 22.7% among 19,249 hospitalized patients.[6] The similar result was also recently reported from Brigham and Women's Hospital of Harvard University, with an AKI incidence rate of 16.6% among 25,859 hospitalized patients (AKIN criteria).[7] Furthermore, in a meta-analysis, Susantitaphong et al.[8] analyzed data from over 3.6 million patients in 154 studies published in the last 10 years and found that the pooled incidence rate of AKI in hospitalized patients was 23.2% (KDIGO criteria). Most of the data collected in this study is from developed countries, it clearly indicated that the incidence rates of hospital-acquired AKI in developed countries is much higher than that reported in China. Such discrepancy might stem from the differences of awareness of AKI between China and developed countries. Due to the lack of awareness of AKI, many hospitalized patients in China failed to receive a continuous monitoring of kidney function and such under-measurement would lead to the underestimation of incidence of AKI in hospitalized patients in China. The differences in the distribution of the patients’ admissions may also contribute to such discrepancy in AKI.
The incidence of AKI is greatly influenced by the specific population, such as patients in different clinical settings. In a multi-center prospective study, patients from 22 ICUs in China, it was found that the incidence rate of AKI was 30.7% (RIFLE criteria).[9] A similar result was also found in a single center retrospective study at West China Hospital[10] in which AKI occurred in 34.1% (353/1036) of critically ill patients in the ICU (AKIN criteria). Patients with heart failure are also a high-risk group to experience AKI. In a retrospective study, among 1230 patients with acute decompensated heart failure in the Cardiac Critical Unit at Nanfang Hospital, the incidence rate of AKI (RIFLE criteria) was shown to be as high as 44.3%, which suggested that this specific group of patients is at high-risk of acquiring AKI and that more attention should be focused on this patient group.[11] The incidence rate of AKI varies greatly with age. In a retrospective study, Fang et al.[4] found that the incidence rate of AKI increased with age from 1.62% to 6.17%. A similar result was observed in the study at Renji Hospital[5] [Figure 1]. In another retrospective study with 4781 elderly patients (≥65 years) at Beijing PLA General Hospital, the overall incidence of AKI (AKIN criteria) was as high as 10.8%, and even 17.4% of the patients aged over 85 years developed AKI.[12] Children, on the other hand, also comprised a patient group that is vulnerable to AKI, specifically those children aged <1-year. In a large multi-center prospective study of 388,736 pediatric patients enrolled from 27 hospitals in China, the general incidence of AKI (AKIN criteria) was as low as 0.32%, whereas patients aged <1-year accounted for almost half of all AKI patients[13] [Figure 2].
Figure 1.
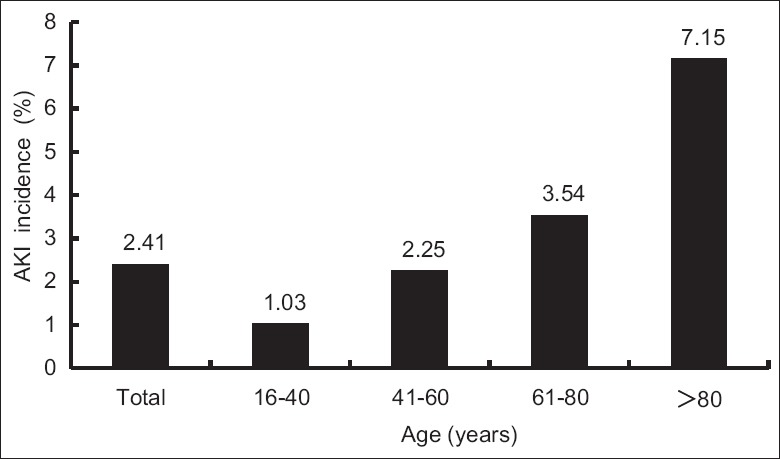
Age-specific incidence of acute kidney injury in a retrospective study of 38,734 patients hospitalized at Shanghai Renji Hospital.
Figure 2.
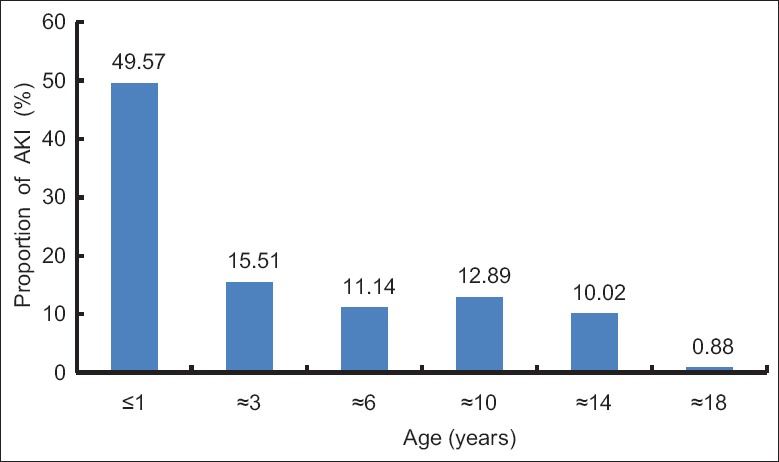
A multi-center study of 388,736 pediatric patients performed in China; patients aged <1-year accounted for almost half of all acute kidney injury patients.
ETIOLOGY
Etiology is also a key issue in AKI research. Clinically, the causes of AKI can be classified into three disease categories: Prerenal, renal and postrenal. The etiology of AKI varies markedly depending on the location of the patient population. In a single center retrospective study at Shanghai Renji Hospital, the most common cause of AKI in hospitalized patients was shown to be prerenal, which accounted for 52% of all cases, followed by renal parenchymal AKI (44.7%) and postrenal AKI (3.3%). The most common cause of AKI was acute tubular necrosis (37.5%), followed by absolute (33.6%) and relative inadequacy of blood volume (13.4%).[14] In another study on hospitalized patients, it was found that the three leading causes of AKI among hospitalized patients were diseases of the circulatory system, urogenital system, and neoplasms.[4] In a retrospective study from the USA, Zeng et al.[7] demonstrated that the American clinical settings with the highest incidence of AKI were sepsis (68.4%), mechanical ventilation (63.9%), critical care (60.3%), hematopoietic stem cell transplantation (55.9%), cardiac surgery (52.2%), and vascular surgery (50.2%).
However, infection might be the most common cause of AKI in a specific group of patients. In a retrospective study, 232 very elderly patients with an average age over 85 years were investigated, with infection accounting for 43.1% of all causes, followed by hypovolemia (19.0%) and use of nephrotoxic drugs (16.8%).[15] Nevertheless, a large prospective study of pediatric patients (388,736) demonstrated that the most common cause of AKI in children is parenchymal disease, which accounts for 57.5%.[13] Urolithiasis induced by melamine-contaminated milk powder accounted for 14% in this large cohort study. In another retrospective study, infectious and autoimmune disease (39.4%), renal vascular disease (27.1%), and circulatory disorder (11.9%) were shown to be the most common causes of AKI among pediatric patients.[16] This finding is quite different from the situation in other developing countries such as India. In a study from South India, infection was found to be the most common cause of pediatric AKI, accounting for 55% of pediatric AKI while acute glomerular diseases accounted for only 17%.[17] Such differences might be associated with the improvement of healthcare infrastructure in China.
Drug-induced AKI is another common renal cause of AKI among Chinese hospitalized patients. Based on an AKI registry originating from 17 hospitals in Shanghai, drug-induced AKI accounted for 28.9% of 1200 cases. Antibiotics are the leading cause (47.8%), followed by diuretics (22.2%) and contrast media (13.3%).[18] In another single center retrospective study in Shanghai, contrast media and chemotherapeutics were the most common medications implicated in drug-induced AKI.[4] The increasing significance of antimicrobials and contrast media in drug-induced AKI is probably associated with the abuse of antibiotics and the development of interventional techniques.
Seismic trauma is also an important cause for AKI. On May 12, 2008, a devastating earthquake hit Wenchuan County of Sichuan province. In a cross-sectional study, among the 1827 hospitalized patients due to seismic trauma, 41% of patients with crush syndrome developed AKI, whereas among the patients without crush syndrome, the incidence of AKI was only 1.6%.[19] In another study, Zhang et al. found that elderly crash victims (age ≥65 years) developed AKI more frequently (19.7% vs. 7.6%) compared to younger victims (age, 15–64 years) in Wenchuan earthquake.[20]
DIAGNOSTIC BIOMARKERS
Serum creatinine (SCr) is a classical useful biomarker for diagnosis of AKI. However, its shortcoming is insensibility to find the early decline of GFR. It is therefore urgently needed to find a biomarker for early detection of AKI.
In a retrospective study, Zhu et al. investigated the diagnostic value of urine neutrophil gelatinase apolipoprotein (NGAL) and kidney injury molecule-1 (KIM-1) on AKI after using contrast for percutaneous coronary intervention.[21] It was shown that both NGAL and KIM-1 are sensitive and specific indicators for the early detection of AKI induced by contrast medium. In another study of hospitalized patients in China, urinary KIM-1, interleukin 18 (IL-18), and cystatin C were all shown to be early predictive biomarkers of gadolinium-based contrast-induced nephropathy in the elderly patients.[22] More recently, a meta-analysis comprising 2979 patients from 11 eligible studies investigated the value of KIM-1 on diagnosis of AKI.[23] The estimated sensitivity of urinary KIM-1 for the diagnosis of AKI was 74.0% (95% confidence interval [CI], 61.0%–84.0%), and specificity was 86.0% (95% CI, 74.0%–93.0%). The authors concluded that urinary KIM-1 might be a promising biomarker with considerable predictive value for the early detection of AKI, especially for cardiac surgery patients. Another meta-analysis incorporated data from 23 studies involving 4,512 patients.[24] Those investigators found the diagnostic odds ratio for urinary IL-18 level to predict AKI was 4.22 (95% CI, 2.90–6.14), with sensitivity and specificity of 58% and 75%, respectively. The investigators concluded that urinary IL-18 might be a useful biomarker with moderate predictive value in all clinical settings.
Although the availability of new biomarkers of kidney damage and functional change offers an unprecedented opportunity in diagnosing AKI, the current evidence based for AKI biomarkers is limited. Many previous studies focused on establishing the performance of various damage markers relative to creatinine. And this would strongly constrain the verification of the diagnostic value of various damage markers in subclinical AKI and restrict their use in the early detection of AKI in clinical settings.
THERAPY
As in the rest of the world, the treatment of AKI remains a challenging issue in China. Because most hospital-acquired AKI in China is due to prerenal reasons, AKI is treatable and largely preventable. Special care should be given to the high-risk of patients to prevent renal hypoperfusion, avoid nephrotoxic medications, and provide adequate fluid therapy.
Although the controversy continues regarding the effectiveness of modality of renal replacement therapy (RRT) in AKI, RRT including continuous RRT (CRRT) is still the cornerstone therapy for the treatment of patients with severe AKI. In a large retrospective study performed by Jinling Hospital, 1692 critically ill patients received CRRT, with continuous high-volume hemofiltration and continuous veno-venous hemofiltration (CVVH) as the main modalities. It was found that 47% of patients were cured, and 27% improved, with a total effective rate of 74%. The outcome of critically ill patients was significantly improved by CRRT.[25] More recently, a retrospective analysis of 145 patients with septic AKI who underwent RRT was conducted by Sun et al.[26] Sixty-five and 80 patients were treated with CVVH and extended daily hemofiltration (EDHF), respectively. Patients in the CVVH group experienced significantly higher recovery of renal function (50.77% of CVVH group vs. 32.50% in the EDHF group, P = 0.026) and shorter median time to renal recovery (17.26 days for CVVHF group vs. 25.46 days for EDHF group, P = 0.039). CVVH is more effective than EDHF for septic AKI in terms of its effect on renal function recovery independent of clinically relevant variables.
The optimal timing for CRRT initiation is a critical issue in the treatment of AKI. A retrospective analysis was conducted on critically ill patients treated with CRRT.[27] The results indicated that the time of initiation of CRRT has no effect on the 28-, 90-, 180-day survival rate. However, in another retrospective analysis of 106 critically ill patients with AKI, starting CRRT prior to RIFLE-F stage was associated with a higher 90-day survival rate and a better renal outcome.[28]
PROGNOSIS
Acute kidney injury is a risk factor for de-novo chronic or end-stage kidney disease in patients without preceding chronic disease and in whom kidney function seemed to completely recover after hospital-associated AKI.[17] A long-term follow-up study of 941 patients after cardiac surgery was conducted at Shanghai Renji Hospital.[29] At the end of the follow-up, patients with AKI had statistically higher Scr than nonAKI patients (107.6 μmol/L vs. 83.0 μmol/L, P = 0.014), and among those AKI patients, 34.0% progressed into CKD stages 3 through 5. Furthermore, the 6-year survival rate is closely correlated with the severity of AKI [Figure 3], and even if complete recovery, the survival rate in the AKI group is lower than in those without AKI (69.6% vs. 85.6%, P < 0.01). These results indicated the need for long-term follow-up of survivors of AKI even after complete recovery.
Figure 3.
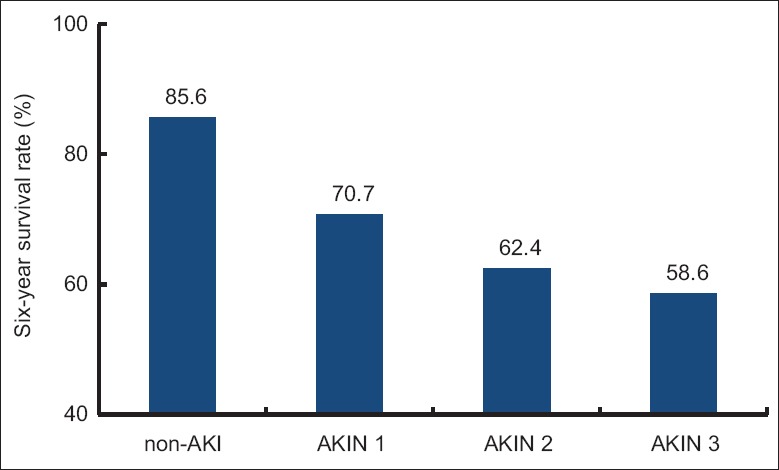
A long-term follow-up study of 941 patients after cardiac surgery at Shanghai Renji hospital; the 6-year survival rate is closely related with the severity of acute kidney injury.
In conclusion, acute kidney injury is a common clinical syndrome in China. Although many advances have been made in the past decade, significant challenges remain existence for Chinese nephrologists. We need to determine the incidence rate of AKI on the basis of the national community surveys. Meanwhile, identifying how to reduce the incidence of hospital-acquired AKI is also an important issue. In addition, the development of rational strategies for initiation, dosing, and effective delivery modality of CRRT for critical ill patients with AKI requires clarification. Furthermore, as the largest developing country in the world, China's resources and facilities for treating the AKI patients are still limited especially in many remote regions. Indeed, the solution to these challenges will rely on technological progress, academic investment, and establishment of perfect health care system.
Footnotes
Edited by: Yi Cui
Source of Support: This work was supported by grants from the National Natural Science Foundation of China (Key Program, No. 81130010 81370919) and the Natural Science Foundation of Jiangsu Province (No. BK2011603, BL2014080).
Conflict of Interest: None declared.
REFERENCES
- 1.Chang JW, Jeng MJ, Yang LY, Chen TJ, Chiang SC, Soong WJ, et al. The epidemiology and prognostic factors of mortality in critically ill children with acute kidney injury in Taiwan. Kidney Int. 2015;87:632–9. doi: 10.1038/ki.2014.299. [DOI] [PubMed] [Google Scholar]
- 2.Lu R, Muciño-Bermejo MJ, Armignacco P, Fang Y, Cai H, Zhang M, et al. Survey of acute kidney injury and related risk factors of mortality in hospitalized patients in a third-level urban hospital of Shanghai. Blood Purif. 2014;38:140–8. doi: 10.1159/000366127. [DOI] [PubMed] [Google Scholar]
- 3.Stevens PE, Levin A. Kidney Disease: Improving Global Outcomes Chronic Kidney Disease Guideline Development Work Group Members. Evaluation and management of chronic kidney disease: Synopsis of the kidney disease: Improving global outcomes 2012 clinical practice guideline. Ann Intern Med. 2013;158:825–30. doi: 10.7326/0003-4819-158-11-201306040-00007. [DOI] [PubMed] [Google Scholar]
- 4.Fang Y, Ding X, Zhong Y, Zou J, Teng J, Tang Y, et al. Acute kidney injury in a Chinese hospitalized population. Blood Purif. 2010;30:120–6. doi: 10.1159/000319972. [DOI] [PubMed] [Google Scholar]
- 5.Lu RH, Fang Y, Gao J, Cai H, Zhu ML, Zhang MF, et al. The incidence and risk factors associated with prognosis of acute kidney injury in hospitalized patients. Chin J Nephrol. 2012;28:194–200. [Google Scholar]
- 6.Wang HE, Muntner P, Chertow GM, Warnock DG. Acute kidney injury and mortality in hospitalized patients. Am J Nephrol. 2012;35:349–55. doi: 10.1159/000337487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zeng X, McMahon GM, Brunelli SM, Bates DW, Waikar SS. Incidence, outcomes, and comparisons across definitions of AKI in hospitalized individuals. Clin J Am Soc Nephrol. 2014;9:12–20. doi: 10.2215/CJN.02730313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Susantitaphong P, Cruz DN, Cerda J, Abulfaraj M, Alqahtani F, Koulouridis I, et al. World incidence of AKI: A meta-analysis. Clin J Am Soc Nephrol. 2013;8:1482–93. doi: 10.2215/CJN.00710113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Du B, An Y, Kang Y, Yu X, Zhao M, Ma X, et al. Characteristics of critically ill patients in ICUs in mainland China. Crit Care Med. 2013;41:84–92. doi: 10.1097/CCM.0b013e31826a4082. [DOI] [PubMed] [Google Scholar]
- 10.Zhou J, Yang L, Zhang K, Liu Y, Fu P. Risk factors for the prognosis of acute kidney injury under the Acute Kidney Injury Network definition: A retrospective, multicenter study in critically ill patients. Nephrology (Carlton) 2012;17:330–7. doi: 10.1111/j.1440-1797.2012.01577.x. [DOI] [PubMed] [Google Scholar]
- 11.Zhou Q, Zhao C, Xie D, Xu D, Bin J, Chen P, et al. Acute and acute-on-chronic kidney injury of patients with decompensated heart failure: Impact on outcomes. BMC Nephrol. 2012;13:51. doi: 10.1186/1471-2369-13-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wen J, Cheng Q, Zhao J, Ma Q, Song T, Liu S, et al. Clinical analysis of acute kidney injury in the hospitalized elderly patients. Chin J Geriatr. 2012;31:386–9. [Google Scholar]
- 13.Cao Y, Yi ZW, Zhang H, Dang XQ, Wu XC, Huang AW. Etiology and outcomes of acute kidney injury in Chinese children: A prospective multicentre investigation. BMC Urol. 2013;13:41. doi: 10.1186/1471-2490-13-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lu RH, Fang Y, Gao JY, Cai H, Zhu ML, Zhang MF, et al. Analysis of incidence and risk factor in hospitalized patients with acute kidney injury (in Chinese) Chin Crit Care Med. 2011;23:413–7. [PubMed] [Google Scholar]
- 15.Li QL, Cheng QL, Ma Q, Wang XD, Ao QG, Zhao JH, et al. Risk factors and short-term prognosis of acute kidney injury in elderly patients (in Chinese) Natl Med J Chin. 2013;93:2715–8. [PubMed] [Google Scholar]
- 16.Chen LZ, Chen L, Jiang X, Mo Y, Lu HY. Clinical analysis of prognostic factors in 118 children with acute kidney injury. Chin J Nephrol. 2010;26:497–502. [Google Scholar]
- 17.Lameire NH, Bagga A, Cruz D, De Maeseneer J, Endre Z, Kellum JA, et al. Acute kidney injury: An increasing global concern. Lancet. 2013;382:170–9. doi: 10.1016/S0140-6736(13)60647-9. [DOI] [PubMed] [Google Scholar]
- 18.Che ML, Yan YC, Zhang Y, Gu Y, Wang NS, Chen N, et al. Analysis of drug-induced acute renal failure in Shanghai (in Chinese) Natl Med J Chin. 2009;89:744–9. [PubMed] [Google Scholar]
- 19.He Q, Wang F, Li G, Chen X, Liao C, Zou Y, et al. Crush syndrome and acute kidney injury in the Wenchuan Earthquake. J Trauma. 2011;70:1213–7. doi: 10.1097/TA.0b013e3182117b57. [DOI] [PubMed] [Google Scholar]
- 20.Zhang L, Fu P, Wang L, Cai G, Zhang L, Chen D, et al. The clinical features and outcome of crush patients with acute kidney injury after the Wenchuan earthquake: Differences between elderly and younger adults. Injury. 2012;43:1470–5. doi: 10.1016/j.injury.2010.11.036. [DOI] [PubMed] [Google Scholar]
- 21.Zhu RZ, Hao L, Wang D, Xu BL, Wu JX. Early diagnosis of contrast-induced renal damage and the protective effect of hydration therapy (in Chinese) Chin J Nephrol. 2014;30:24–8. [Google Scholar]
- 22.Yu ZQ, Duan SB, Zhou SK, Pan P, Liu GL, Sun L, et al. Prognostic value of urinary injury molecule 1, interleukin 18, cystatin C as biomarkers for gadolinium-based contrast-induced nephropathy in the elderly patients (in Chinese) Chin J Nephrol. 2013;29:173–7. [Google Scholar]
- 23.Shao X, Tian L, Xu W, Zhang Z, Wang C, Qi C, et al. Diagnostic value of urinary kidney injury molecule 1 for acute kidney injury: A meta-analysis. PLoS One. 2014;9:e84131. doi: 10.1371/journal.pone.0084131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Liu Y, Guo W, Zhang J, Xu C, Yu S, Mao Z, et al. Urinary interleukin 18 for detection of acute kidney injury: A meta-analysis. Am J Kidney Dis. 2013;62:1058–67. doi: 10.1053/j.ajkd.2013.05.014. [DOI] [PubMed] [Google Scholar]
- 25.Xie HL, Ji DX, Gong DH, Xu B, Tao J, Chen YM, et al. Continuous blood purification in the treatment of 1692 critical patients: A retrospective study. J Nephrol Dial Transplant. 2007;16:301–7. [Google Scholar]
- 26.Sun Z, Ye H, Shen X, Chao H, Wu X, Yang J. Continuous venovenous hemofiltration versus extended daily hemofiltration in patients with septic acute kidney injury: A retrospective cohort study. Crit Care. 2014;18:R70. doi: 10.1186/cc13827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hu ZJ, Liu LX, Zhao CC. Influence of time of initiation of continuous renal replacement therapy on prognosis of critically ill patients with acute kidney injury (in Chinese) Chin Crit Care Med. 2013;25:415–9. doi: 10.3760/cma.j.issn.2095-4352.2013.07.012. [DOI] [PubMed] [Google Scholar]
- 28.Li WX, Chen HD, Wang XW, Zhao S, Chen XK, Zheng Y, et al. Predictive value of RIFLE classification on prognosis of critically ill patients with acute kidney injury treated with continuous renal replacement therapy. Chin Med J. 2009;122:1020–5. [PubMed] [Google Scholar]
- 29.Liu S, Che ML, Xie B, Xu S, Zhu ML, Qian JQ, et al. Acute kidney injury is a risk factor for the long-term prognosis of cardiac surgery (in Chinese) Chin J Nephrol. 2011;27:416–22. [Google Scholar]


