Abstract
Background. Repairing aged composite resin is a challenging process. Many surface treatment options have been proposed to this end. This study evaluated the effect of different surface treatments on the shear bond strength (SBS) of nano-filled composite resin repairs.
Methods. Seventy-five cylindrical specimens of a Filtek Z350XT composite resin were fabricated and stored in 37°C distilled water for 24 hours. After thermocycling, the specimens were divided into 5 groups according to the following surface treatments: no treatment (group 1); air abrasion with 50-μm aluminum oxide particles (group 2); irradiation with Er:YAG laser beams (group 3); roughening with coarse-grit diamond bur + 35% phosphoric acid (group 4); and etching with 9% hydrofluoric acid for 120 s (group 5). Another group of Filtek Z350XT composite resin samples (4×6 mm) was fabricated for the measurement of cohesive strength (group 6). A silane coupling agent and an adhesive system were applied after each surface treatment. The specimens were restored with the same composite resin and thermocycled again. A shearing force was applied to the interface in a universal testing machine. Data were analyzed using one-way ANOVA and post hoc Tukey tests (P < 0.05).
Results. One-way ANOVA indicated significant differences between the groups (P < 0.05). SBS of controls was significantly lower than the other groups; differences between groups 2, 3, 4, 5 and 6 were not significant. Surface treatment with diamond bur + 35% phosphoric acid resulted in the highest bond strength.
Conclusion. All the surface treatments used in this study improved the shear bond strength of nanofilled composite resin used.
Keywords: Composite resin, dental air abrasion, dental restoration repair, Er:YAG lasers
Introduction
Composite resins have significantly improved over the last decades; however, failures may occur as a result of discoloration, secondary caries, margin ditching or simply fractures.1-4 Treatment choices are repairing or replacing the whole restoration.1,5-9 Replacing a deficient restoration completely results in overextension of the preparation,10 loss of sound tooth structure and increased risk of pulpal exposure.3,7-9,11 According to several clinical studies, repairing the pre-existing restoration is a more conservative alternative that can increase the longevity of the restoration, preserve the sound tooth structure and reduce operative trauma.4,5,12
In clinical practice, bonding between two composite layers is accomplished by the presence of an oxygen-enriched surface layer that remains unpolymerized.3,5,7,13 This layer contains unreacted C=C bonds, allowing the monomers of the new composite resin to bond to it.7,13,14In an aged composite resin the adhesion to a new one reduces 25% to 80% of its original cohesive strength due to a diminished amount of unreacted double bonds.1,12,15 The success of new composite-to- old composite resin adhesion depends on the chemical composition of the surface, roughness, wetting and the surface conditioning methods applied.7,12,13 Therefore, different surface treatment modalities have been used to enhance the repair bond strength of composite resins,1,2,4,7-9,16including bur roughening, etching with hydrofluoric or phosphoric acids, air abrasion, silica coating and silanization.4,6-9,15,16 In recent years there has been more focus on the efficiency of lasers for composite repair bond strength, including Er:YAG laser.4,8,9,17
Studies have shown that Er:YAG laser can influence the surface of composite resins in addition to tooth surfaces.4,8,9,17 The wavelength of Er:YAG laser is 2940 nm and it is absorbed by the water and hydroxyapatite of the tooth. In the laser ablation process the produced heat releases hydroxyl groups from hydroxyapatite,18 causing the water surrounding the apatite crystals to evaporate suddenly. This evaporation results in an increase in the internal tissue pressure and subsequently micro-explosions happen.19,20 Most of the energy is used during the ablation process and the rest diffuses into the adjacent tissues, without an extreme increase in temperature.21,22 Additionally, the use of laser on enamel and dentin results in micro-retentions on the enamel and opening of the dentinal tubules.19
In an attempt to achieve long-lasting composite restorations, the composition of composite resins has been modified in recent years. Major modifications include changes in the size and distribution of fillers with reduced filler particle sizes and increased loading. This has led to the development of nanofilled composite resins.7,13 The range of the filler size in nanofilled composite is between 5 and 100 nm and the particles are in clusters or dispersed forms.13 The repair of nanofilled composite resins has not been yet investigated in detail and there is no consensus on the results obtained with the different surface treatments.1,11-13
Therefore, the aim of this study was to evaluate the effect of different mechanical and chemical surface treatment procedures on shear bond strength of repaired nanofilled composite resin and to characterize changes in surface topography following each treatment. The null hypothesis tested was that different surface treatments would not affect the shear bond strength.
Methods
No ethical approval was obtained because this in vitro study only involved non-invasive procedures on composite resin samples. The brands, manufacturers and chemical compositions of the materials used in this study are listed in Table 1.
Table 1. List of brands, manufacturers and chemical compositions of the materials used.
| Material | Manufacture | Chemical composition |
|
Filtek Z350 XT Universal Restorative
(shades A2 and A4) |
3M ESPE, St. Paul, MN, USA | Bis-GMA, UDMA, TEGDMA, PEGDMA, Bis-EMA, non-aggregated 4 to 10nm zirconia, non-aggregated 20 nm silica and aggregated zirconia/silica cluster filler (63.3 vol%) |
| Swiss TEC SL Etchant Gel | Coltene Whaledent AG, Altstätten Switzerland | 35% phosphoric acid |
| Porcelain Etch Gel | PULPDENT Corp, Watertown, MA , USA | 9% Hydrofluoric Acid |
| Adper Single Bond2 | 3M ESPE, St. Paul, MN, USA | Dimethacrylate, HEMA, polyalcenoic acid copolymer, silane treated colloidal silica, ethanol, water, photoinitiator |
| Silane Bond Enhancer | PULPDENT Corp, Watertown, MA , USA | 3-methacryloxypropyltrimethoxysilane |
| Diamond Bur | FGS110012, DIA-ITALY, ITALY | Grit:100µm |
Sample preparation
Seventy-five cylindrical specimens, 4 mm in height and 4 mm in diameter, were prepared by the layering technique with 2-mm-thick increments of a nanofilled composite resin (Filtek Z350 XT, shade A2) using plastic molds. Each layer was light-cured for 20 s with an LED light-curing unit (Valo, Ultradent Products, Inc. UT, USA) according to the manufacturer’s instructions. The intensity of the light-curing unit was 1000 mW/cm2 and verified by a radiometer after every 5 specimens. The last increment was covered with a Mylar strip (KerrHawe SA, Bioggio, Switzerland) and a glass slide in order to create a smooth surface and to prevent the formation of an oxygen-inhibited layer. After polymerization, the molds were gently removed and the specimens were cured from each side for 20 s in order to ensure uniform and complete polymerization. Fifteen additional specimens, 6 mm in height and 4 mm in diameter, were prepared in the same manner in order to evaluate the cohesive strength. To age the composite resin, the substrates were placed in distilled water at 37°C for 24 hrs and then thermocycled for 500 cycles at 5 ± 2/55 ± 2°C with a dwell time of 30 s and transfer time of 10 s.23
Except for the samples of the cohesive group (group 6), the other specimens were randomly divided into five groups (N=15) according to the surface treatment applied.
In group 1 (control), no surface treatment was performed on the specimens.
In group 2, the samples were air-abraded at a pressure of 60 PSI using an air abrasion device (AEROETCHER, D670, PARKELL Farmingdale, NY, USA) for 5 s with 50-µm aluminum oxide particles. The tip was positioned 5 mm away from the target and perpendicular to the specimen surface. Subsequently, the specimens were rinsed under tap water and air-dried.
In group 3, composite resin surfaces were irradiated with Er:YAG laser beams (Doctor Smile, LAEDL001.1, LAMBDA Scientifica S.p.A, Italy). A H6/12-type laser tip was used for surface treatment. Laser energy was delivered in pulse mode at a wavelength of 2.94 µm, a duration of 75 µs and a repetition rate of 25 Hz. The output power was 1.5 W at 60% air level and 30% water level. The beam was perpendicular to the target area, with a distance of 1 mm between the laser tip and the composite resin surface. Subsequently, the specimens were rinsed and air-dried.
In group 4, composite resin surfaces were roughened in three strokes with a coarse diamond bur using a high-speed handpiece with water spray. A new diamond bur was used for each 5 samples. Then 35% phosphoric acid was applied for 15 s and washed with water and dried.
Finally, in group 5 the substrates were etched with 9% hydrofluoric acid (HF) (Porcelain Etch Gel) for 120 s, rinsed and dried.
After surface treatments, silane coupling agent (Silane Bond Enhancer) was applied to all the specimens in a thin layer, the solvent was gently removed under compressed air. Thereafter, Single Bond 2 bonding agent was applied on sample surfaces according to the manufacturer’s instructions and light-polymerized for 20 s using a Valo LED light-curing unit at a light intensity of 1000 mW/cm2.
Then cylindrical molds (2×2 mm) were placed at the center of the specimens and filled with the A4 shade of Filtek Z350XT composite resin by the same operator and light-cured for 20 s. The molds were then removed and additional curing was carried out for 20 s from each side.
All the specimens were stored in 37°C distilled water for 24 hrs and additionally thermocycled for 500 cycles at 5±2/55±2°C with a dwell time of 30 s and a transfer time of 10 s.
The specimens were mounted in acrylic resin and placed in a universal testing machine (Zwick ROELL Z050, Germany) and a shear force was applied using a shearing blade parallel to the adhesive interface. The load was applied to the interface at a cross-head speed of 1 mm/min until failure and the stress-strain curve was analyzed with the machine’s software program. The same technique was used to measure the cohesive strength of the samples in group 6.
In order to visualize the topography of samples after the surface treatment, one specimen from each group was selected and gold-sputtered by a 150-A° thin gold layer; the surface topography was then evaluated under a scanning electron microscope (Tescan Vega-II; Tescan, S.RO. LibusiniaTrida, CZ) at ×1000 magnification and kVp=15.
The failure modes of the specimens were determined at ×40 under a stereomicroscope (Motic Smz-143 SERIES, Micro-optic industrial group Co, Xiamen, China) and recorded as ‘cohesive in aged or new composite’, ‘adhesive at the interface’, or ‘mixed adhesive-cohesive’.
Statistical analysis
Data were collected and analyzed with SPSS V.20. Analyses were performed by one-way ANOVA and post hoc Tukey tests. Statistical significance was defined at α = 0.05.
Results
The means and standard deviations of repair shear bond strengths in the study groups are presented in Table 2. The highest shear bond strength was found in group 4 (diamond bur + phosphoric acid) and the lowest in group 1 (control). One-way ANOVA indicated significant differences between the study groups (P < 0.001). Two-by-two comparisons of the groups revealed significant differences in repair bond strength between group 1 and the other five study groups; however, there were no statistically significant differences between groups 2, 3, 4, 5 and 6. The percentages of fracture modes of the samples are illustrated in Figure 1. The mode of failure was predominantly cohesive for all the groups. Only a few fractures were adhesive and there were no mixed failures.
Table 2. Means and standard deviations of shear bond strengths in the studied groups (in MPa).
| Groups | N | Mean (MPa) | Std. Deviation | Min (MPa) | Max (MPa) |
| 1 | 15 | 20.22 a | 5.12 | 11.96 | 31.68 |
| 2 | 15 | 32.29 b | 5.42 | 25.39 | 44.09 |
| 3 | 15 | 29.14 b | 3.43 | 22.13 | 35.47 |
| 4 | 15 | 35.51 b | 4.41 | 25.49 | 44.56 |
| 5 | 15 | 33.77 b | 4.67 | 26.63 | 42.22 |
| 6 | 15 | 27.79 b | 5.70 | 18.37 | 37.88 |
Group 1: control; group 2: air abrasion; group 3: Er:YAG laser; group 4::diamond bur + phosphoric acid; group 5: HF acid; group 6: bulk. Different letters in a column indicate the statistically significant differences at α=0.001 between the two groups.
Figure 1.
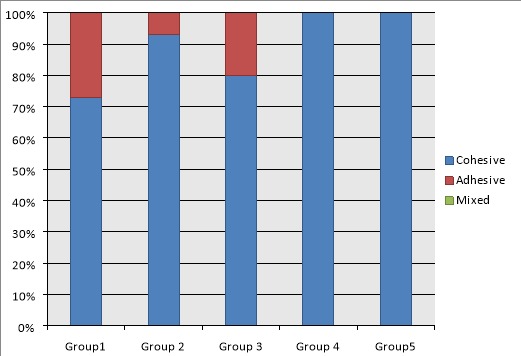
Percentages of fracture modes evaluated under a stereomicroscope after shear bond strength testing of each group (Group 1: control, group 2: air abrasion, group 3: Er:YAG Laser, group 4: diamond bur + phosphoric acid, group 5: HF acid).
SEM analysis
Figure 2 illustrates SEM micrographs of Filtek Z350XT composite resin surfaces treated with various techniques. As determined from the SEM micrographs, the control sample had a relatively smooth surface. The bur-treated and acid-etched sample exhibited a rougher surface and more area for micromechanical retention compared to other treatments. In the laser-treated samples, a homogeneous micro-retentive feature was noticeable. In HF-etched surfaces, the specimen exhibited a moderate amount of surface relief along with pores. In sand-blasted samples, a rough pattern was visible along with grooves.
Figure 2.
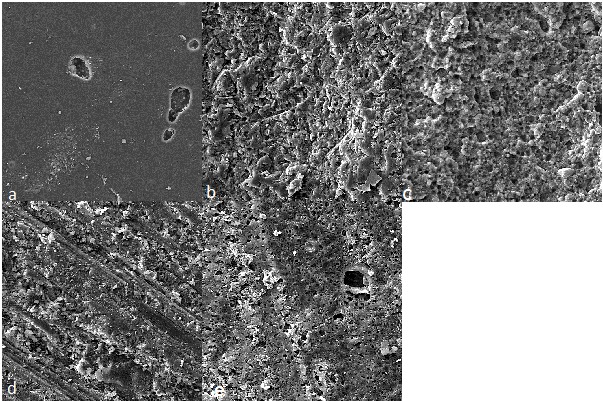
Scanning electron micrographs of the aged resin composite. (a) control sample with no surface treatment; (b) air abraded sample; (c) Er:YAG laser-treated sample; (d) bur + acid etched sample; (e) HF-treated sample.
Discussion
Adhesion of a new composite resin to an aged one is challenging because of the absence of oxygen-inhibited layer and reduction of unsaturated C=C bonds.3,11,15 A variety of surface treatments have been used to improve the repair bond strength of composite resins.1,2,4,7 In the present study, four different surface treatment methods were evaluated to achieve optimal repair bond strength. According to the results, the lowest repair bond strength was recorded in the control group, which was expected due to smooth surface visible in scanning electron micrograph of the sample in this group. This is in consistent with the results of other studies,6,13,17and indicates the importance of surface roughening in improving the repair bond strength of nanofilled composite resins. All the surface treatments applied in this study reached the cohesive strength of the en bloc samples and the repair bond strengths were significantly higher than those of the controls. Inclusion of both the control and cohesive groups in the present study defines the influence of different methods on repair bond strength and the repair potential compared to the cohesive strength of the material.10
Based on our results, roughening the aged composite resin with a coarse bur and subsequent acid etching formed the highest repair bond strength, followed by hydrofluoric acid etching, air abrasion and Er:YAG laser, although no significant differences were observed between the groups. This indicates that all the four surface treatment modalities were effective in bonding the aged composite resin to the fresh one. Thus, the null hypothesis was rejected.
In the present study, after surface treatments and prior to the bonding with all the specimens, a silane solution was applied. Composite materials roughly have 50 vol% filler; therefore, 50% of the roughened composite surface should consist of fillers.3 Silane molecules have two main functional groups; the silanol bonds to the silica particles of a composite resin and at the same time the organofunctional group of this compound bonds to the methacrylate of the bonding agent.3,10,15 Silane also assists the infiltration of bonding agent by increasing the wettability of the surface.5,7,10,13-16,23,24
Application of a diamond bur and subsequent phosphoric acid etching in the present study yielded the highest repair bond strength. This finding is supported by a study of Tabatabaei et al.23 This method of surface treatment creates macro-retentive as well as micro-retentive features and this may differentially expose filler particles.23 This finding is supported by the SEM image which shows a more retentive linear patterns and courser surface. Moreover, acid etching removes the smear debris and exposes the underlying surface and fillers. This results in an increased surface area which can help stress distribution along the interface of the two bonded substrates.11Additionally acid etching might also set off the reaction between a silane coupling agent and silica surface.10 A combination of bur roughening, phosphoric acid etching and silane application can be suggested to achieve higher repair bond strength in Filtek Z350XT composite resin.
According to our results, air abrasion with 50-μm aluminum oxide particles produced favorable repair bond strength in the aged composite resin. Following air abrasion, some of the resin matrix is removed and the surface fillers are exposed resulting in an increased surface roughness of the composite resin.8,23Several previous studies have reported contradictory findings about air abrasion. In some studies, sandblasting promoted the best repair bond strength,1,25,26 while a reduction in repair strength after surface abrasion was found in a few studies.8,27,28 This reduction has been ascribed to the exposure of filler particles, and hence decreased amount of available resin for bonding.8,23 It seems that the application of a silane coupling agent following sandblasting in the present study enhanced the bond to the exposed filler particles and thus, increased the repair bond strength. In the present study, evaluation of scanning electron microscope images of the air-abraded samples revealed an increase in surface roughness in a pattern different from other treatment modalities. It has been reported that the surface characteristics following air abrasion depends on the microstructure and composition of the material. In nanofilled composite resins, breaking off of the clusters occurs when they are subjected to abrasion.14 Thus the loss of fillers might reduce the interaction with silane compared to diamond bur-treated groups. Moreover after air abrasion the smear debris is not removed and this may reduce the surface area available for bonding, hence reducing the bond strength compared to the acid etching group.
In the present study, hydrofluoric acid treatment resulted in significantly higher SBSs than the control group, which is consistent with the findings of other studies.10,29 HF acid dissolves the glass particles of the composite, leaving micro-mechanical pores that allow adequate bonding agent infiltration.29 SEM analysis of samples etched with HF revealed a moderate amount of surface relief with partial removal of filler particles and the presence of pores. The fillers of Filtek Z350 XT are a combination of silica fillers, zirconia fillers and zirconia/silica cluster fillers. It seems that subsequent to etching with HF, silica-containing fillers are partially dissolved and the remaining fillers react with silane agent, promoting the bond, in addition to micro-mechanical retention. However, other composite repair studies have reported that the HF etching of the composite surface decreased the repair bond strength.1,30,31 This difference can be due to differences in the type of composite resins used in these studies. The effect of HF is related to the percentage, size and type of the inorganic filler of composite resin.1 HF etching can be an effective surface treatment but necessitates extreme care when used for intraoral repairs due to the risk for acid burns and soft tissue necrosis.10
The results of this study showed that SBS of samples in the laser group was significantly higher than that of the controls, but in comparison to diamond bur, air abrasion and HF groups lower bond strengths were achieved, although the difference was not significant. This finding is consistent with that of Rosatto et al,9 in which the Er:YAG laser yielded results similar to diamond bur and sandblasting. Likewise, Bektas et al4 concluded that repair bond strength of laser-treated surfaces was comparable to that of bur-treated surfaces. However, in the study of Alizadeh et al32 with Er,Cr:YSGG laser, and Hasan8 with Er:YAG laser, higher repair bond strength was reported for the laser groups compared to other surface treatments. The differences might be related to the type, structure and chemical composition of composites used as well as laser parameters that affected the efficacy of mechanical surface treatments.4
Electron microscope images in the present study revealed that laser irradiation resulted in formation of a micro-retentive pitting feature, without smear layer formation, which increases the bonding surface, resulting in a higher repair bond strength compared to the controls. However, the micro-retentive feature was less prominent compared to other treatment modalities. Lizarelli et al33 reported that the micromorphology of the laser-irradiated surface depends on the chemical composition and structure of composite resin. Composite resins with greater filler-matrix bond energy and cohesion are more resistant to laser ablation. Under laser ablation the polymeric matrix is abraded first and subsequently the filler particles are released. It seems that in Filtek Z350XT nanofilled composite resin, presence of nanoparticles and nanoclusters increases the filler loadings and leads to less matrix exposed for ablation.
Bond strength between 15 MPa to 25 MPa is suggested for composite resin repairs in some studies. These values are typical of the bond strength of composite resin to dentin,23,34 which could be clinically accepted. In our study, all the repair groups reached these values, with even the control group. It seems that high repair bond strength in Filtek Z350XT nanofilled composite resin is achievable by any of the treatment modalities. This could be explained by the fact that Filtek Z350XT composite resin consists of nano-sized silica particles (20 nm) and clusters of Si/Zr. Small filler particles expose a higher surface area and increase the bonding substrate. It is also believed that the nanoclusters may present a reinforcing mechanism and that the silane infiltration within the intimacy of the nanoclusters modifies the response to loading stresses, thus providing an improved clinical performance.35
A general repair technique cannot be suggested for nanofilled composite resins since all the surface treatments showed higher SBS than the cohesive controls and can be considered appropriate. However, there is a limitation in utilizing these methods clinically; for example HF is corrosive for intraoral use, aerosols in air abrasion can be harmful for respiratory system and Er:YAG laser needs special equipment and proficiency. Bur roughening and acid etching on the other hand can be a safe and cost-effective alternative and should be recommended to be used clinically for repairing nanofilled composite resins. Our study was carried out in vitro; therefore, it is difficult to extend the results to clinical situations. It is suggested that in future studies the repair bond strength of nanofilled composites be evaluated in vivo where they are exposed to the effects of pH and temperature changes, salivary enzymes and the oral environment.
Conclusion
Within the limitations of this study, it was concluded that composite resin surface treatment with bur and acid etching, air abrasion, HF acid and Er:YAG laser resulted in similar bond strength and can be recommended to obtain optimal repair bond strength.
Acknowledgments
The authors thank Babol University of Medical Sciences for supporting this research. The authors are grateful to Dr. Evangeline Foronda for the English proofreading.
Authors’ contributions
The study was planned by GA, BE and AT. AT carried out the laboratory procedures and shear bond testing process. The statistical analyses and interpretation of data were carried out by SK. GA, BE, AT and TJ were responsible for manuscript preparation. ZJ, TJ, and FAD critically revised the manuscript for intellectual content. All authors contributed to the final draft, and have read and approved the final manuscript.
Funding
This study was a part of a thesis and research project (Grant No: 1710) supported and funded by Babol University of Medical Sciences.
Competing interests
The authors declare that they have no competing interests with regards to the authorship and/or publication of this article.
Ethics approval
Not applicable.
References
- 1.Lucena-Martín C, González-López S, Navajas-Rodríguez de Mondelo JM. The effect of various surface treatments and bonding agents on the repaired strength of heat-treated composites. J Prosthet Dent. 2001;86:481–8. doi: 10.1067/mpr.2001.116775. [DOI] [PubMed] [Google Scholar]
- 2.Cavalcanti AN, Lavigne C, Fontes CM, Mathias P. Microleakage at the composite-repair interface: effect of different adhesive systems. J Appl Oral Sci. 2004;12:219–22. doi: 10.1590/s1678-77572004000300011. [DOI] [PubMed] [Google Scholar]
- 3.Hamano N, Chiang YC, Nyamaa I, Yamaguchi H, Ino S, Hickel R, Kunzelmann KH. Effect of different surface treatments on the repair strength of a nanofilled resin-based composite. Dent Mater J. 2011;30:537–45. doi: 10.4012/dmj.2010-202. [DOI] [PubMed] [Google Scholar]
- 4.ÖzelBektas Ö, Eren D, HergunerSiso S, Akin GE. Effect of thermocycling on the bond strength of composite resin to bur and laser treated composite resin. Lasers Med Sci. 2012;27:723–8. doi: 10.1007/s10103-011-0958-2. [DOI] [PubMed] [Google Scholar]
- 5.JafarzadehKashi TS, Erfan M, Rakhshan V, Aghabaigi N, Tabatabaei FS. An in vitro assessment of the effects of three surface treatments on repair bond strength of aged composites. Oper Dent. 2011;36:608–17. doi: 10.2341/10-386-l. [DOI] [PubMed] [Google Scholar]
- 6.da Costa TR, Serrano AM, Atman AP, Loguercio AD, Reis A. Durability of composite repair using different surface treatments. J Dent. 2012;40:513–21. doi: 10.1016/j.jdent.2012.03.001. [DOI] [PubMed] [Google Scholar]
- 7.Özcan M, Pekkan G. Effect of different adhesion strategies on bond strength of resin composite to composite-dentin complex. Oper Dent. 2013;38:63–72. doi: 10.2341/11-482-l. [DOI] [PubMed] [Google Scholar]
- 8.Hasan NH. The Influence of Er: YAG Laser, Aluminum oxide and diamond bur on surface treatmentof Aged Composite Resin to Repair Restoration. Al–Rafidain Dent J. 2012;12:257–65. [Google Scholar]
- 9.Rossato DM, Bandeca MC, Saade EG, Lizarelli RFZ, Bagnato VS, Saad JRC. Influence of Er:YAG laser on surface treatment of aged composite resin to repair restoration. Laser Phys. 2009;19:2144–9. doi: 10.1134/s1054660x09210105. [DOI] [Google Scholar]
- 10.Loomans BA, Cardoso MV, Roeters FJ, Opdam NJ, De Munck J, Huysmans MC, Van Meerbeek B. Is there one optimal repair technique for all composites? Dent Mater. 2011;27:701–9. doi: 10.1016/j.dental.2011.03.013. [DOI] [PubMed] [Google Scholar]
- 11.Fawzy AS, El-Askary FS, Amer MA. Effect of surface treatments on the tensile bond strength of repaired water-aged anterior restorative micro-fine hybrid resin composite. J Dent. 2008;36:969–76. doi: 10.1016/j.jdent.2008.07.014. [DOI] [PubMed] [Google Scholar]
- 12.Özcan M, Corazza PH, Marocho SM, Barbosa SH, Bottino MA. Repair bond strength of microhybrid, nanohybrid and nanofilled resin composite: effect of substrate resin type, surface conditioning and aging. Clin Oral Invest. 2013;17:1751–8. doi: 10.1007/s00784-012-0863-5. [DOI] [PubMed] [Google Scholar]
- 13.Rinastiti M, Ozcan M, Siswomihardjo W, Busscher HJ. Immediate repair bond strengths of microhybrid, nanohybrid and nanofilled composites after different surface treatments. J Dent. 2010;3:29–38. doi: 10.1016/j.jdent.2009.08.009. [DOI] [PubMed] [Google Scholar]
- 14.Rodrigues SA Jr, Ferracane JL, Della Bona A. Influence of surface treatments on the bond strength of repaired resin composite restorative materials. Dent Mater. 2009;25:442–51. doi: 10.1016/j.dental.2008.09.009. [DOI] [PubMed] [Google Scholar]
- 15.Ozcan M, Barbosa SH, Melo RM, Galhano GA, Bottino MA. Effect of surface conditioning methods on the microtensile bond strength of resin composite to composite after aging conditions. Dent Mater. 2007;23:1276–82. doi: 10.1016/j.dental.2006.11.007. [DOI] [PubMed] [Google Scholar]
- 16.Rinastiti M, Özcan M, Siswomihardjo W, Busscher HJ. Effects of surface conditioning on repair bond strengths of non-aged and aged microhybrid, nanohybrid, and nanofilled composite resins. Clin Oral Invest. 2011;15:625–33. doi: 10.1007/s00784-010-0426-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kimyai S, Mohammadi N, Navimipour EJ, Rikhtegaran S. Comparison of the effect of three mechanical surface treatments on the repair bond strength of a laboratory composite. Photomed Laser Surg. 2010;28:S25–30. doi: 10.1089/pho.2009.2598. [DOI] [PubMed] [Google Scholar]
- 18.Malta DAMP, Kreidler MAM, Villa GE, de Andrade MF, Fontana CR, Lizarelli RFZ. Bond strength of adhesive restorations to Er:YAG laser-treated dentin. Laser Phys Lett. 2006;4:153–6. doi: 10.1002/lapl.200610085. [DOI] [Google Scholar]
- 19.Lizarelli R, Moriyama L, Jorge J, Bagnato V. Comparative ablation rate from an Er YAG laser on enamel and dentin of primary and permanent teeth. Laser Phys. 2006;16:849–58. doi: 10.1134/s1054660x06050173. [DOI] [Google Scholar]
- 20.Hibst R, Keller U. Experimental studies of the application of the Er:YAG laser on dental hard substances: IMeasurement of the ablation rate. Lasers Surg Med. 1989;9:338–44. doi: 10.1002/lsm.1900090405. [DOI] [PubMed] [Google Scholar]
- 21.Bader C, Krejci I. Indications and limitations of Er:YAG laser applications in dentistry. Am J Dent. 2006;19:178–86. [PubMed] [Google Scholar]
- 22.Ana PA, Bachman L, Zezell DM. Lasers effect on enamel for caries prevention. Laser Phys. 2006;16:865–75. doi: 10.1134/s1054660x06050197. [DOI] [Google Scholar]
- 23.Hasani Tabatabaei M, Alizade Y, Taalim S. Effect of various surface treatment on repair strength of composite resin. J Dent TUMS. 2004;1:5–11. [Google Scholar]
- 24.Cavalcanti AN, De Lima AF, Peris AR, Mitsui FH, Marchi GM. Effect of surface treatments and bonding agents on the bond strength of repaired composites. J Esthet Restor Dent. 2007;19:90–8. doi: 10.1111/j.1708-8240.2007.00073.x. [DOI] [PubMed] [Google Scholar]
- 25.Turner CW, Meiers JC. Repair of an aged, contaminated indirect composite resin with a direct, visible-light-cured composite resin. Oper Dent. 1993;18:187–94. [PubMed] [Google Scholar]
- 26.Swift EJ, Lvalley JR, Boyer DB. Evaluation of new methods for composite repair. Dent Mater. 1992;8:362–5. doi: 10.1016/0109-5641(92)90020-d. [DOI] [PubMed] [Google Scholar]
- 27.Pounder B, Gregory WA, Powers JM. Bond strength of repaired composite resin. Oper Dent. 1987;12:127–31. [PubMed] [Google Scholar]
- 28.Boyer DB, Ehan KC, Reinhardt JW. Build up and repair of light cured composite: bond strength. J Dent Res. 1984;63:1241–4. doi: 10.1177/00220345840630101501. [DOI] [PubMed] [Google Scholar]
- 29.Yesilyurt C, Kusgoz A, Bayram M, Ulker M. Initial repair bond strength of a nano-filled hybrid resin: effect of surface treatments and bonding agents. J Esthet Restor Dent. 2009;21:251–60. doi: 10.1111/j.1708-8240.2009.00271.x. [DOI] [PubMed] [Google Scholar]
- 30.Crumpler DC, Bayne SC, Sockwell S, Brunson D, Roberson TM. Bonding to resurfaced posterior composites. Dent Mater. 1989;5:417–24. doi: 10.1016/0109-5641(89)90113-9. [DOI] [PubMed] [Google Scholar]
- 31.Brosh T, Pilo R, Bichacho N, Blutstein R. Effects of combinations of surface treatments and bonding agents on the bond strength of repaired composites. J Prosthet Dent. 1997;77:122–6. doi: 10.1016/s0022-3913(97)70224-5. [DOI] [PubMed] [Google Scholar]
- 32.Alizadeh Oskoee P, Mohammadi N, Ebrahimichaharom ME, Kimyai S, PournaghiAzar F, Rikhtegaran S, Shojaeei M. Effect of surface treatment with Er;Cr:YSSG, Nd:YAG, and CO2 lasers on repair shear bond strength of a silorane-based composite resin. J Dent Res Dent Clin Dent Prospects. 2013;7:61–6. doi: 10.5681/joddd.2013.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lizarelli R de FZ, Moriyama LT, Pelino JEP, Bagnato VS. Ablation rate and morphological aspects of composite resins exposed to Er: YAG laser. J Oral Laser App. 2005;5:151–160. [Google Scholar]
- 34.Teixeria EC, Bayne SC, Thompson JY, Ritter AV, Swift EJ. Shear bond strength of self-etching bonding systems in combination with various composites used for repairing aged composites. J Adhes Dent. 2005;7:159–64. [PubMed] [Google Scholar]
- 35.Curtis AR, Palin WM, Fleming GJ, Shortall AC, Marquis PM. The mechanical properties of nanofilled resin-based composites: the impact of dry and wet cyclic pre-loading on bi-axial flexure strength. Dent Mater. 2009;25:188–97. doi: 10.1016/j.dental.2008.06.0030. [DOI] [PubMed] [Google Scholar]


