Abstract
Over the past fifty years Medicaid has taken divergent paths in financing mental health and addiction treatment. In mental health, Medicaid became the dominant source of funding and had a profound impact on the organization and delivery of services. But it played a much more modest role in addiction treatment. This is poised to change, as the Affordable Care Act is expected to dramatically expand Medicaid’s role in financing addiction services. In this article we consider the different paths these two treatment systems have taken since 1965 and identify strategic lessons that the addiction treatment system might take from mental health’s experience under Medicaid. These lessons include leveraging optional coverage categories to tailor Medicaid to the unique needs of the addiction treatment system, providing incentives to addiction treatment programs to create and deliver high-quality alternatives to inpatient treatment, and using targeted Medicaid licensure standards to increase the quality of addiction services.
Medicaid has played an important role during the past fifty years for low-income Americans needing mental health or addiction treatment. The mental health care and addiction treatment systems rely on Medicaid as a crucial financier of care. Nevertheless, Medicaid’s coverage for treatment of mental health and addictive disorders has diverged in important ways. Whereas Medicaid began as a small player in financing services for both types of disorders, it eventually grew to become the dominant source of funding for mental health treatment but has yet to reach that dominance in addiction treatment.1
Much has been written about Medicaid’s growing role in financing mental health treatment. Less considered is the broader effect of these financing changes on the organization and quality of the mental health treatment system for low-income people in the United States.2 Stakeholders in mental health treatment have been deliberate not only in using Medicaid to leverage new funds for treatment but also in using the program to increase the comprehensiveness of mental health services, elevate standards for mental health providers, and create meaningful alternatives to inpatient treatment.
The Affordable Care Act (ACA) gives states the option to expand Medicaid eligibility to people younger than age sixty-five whose family incomes are at or below 138 percent of the federal poverty level. In doing so, it creates an opportunity for the addiction treatment system to improve service access and quality. As a result of the ACA’s Medicaid eligibility expansion, along with the law’s mandate to provide addiction treatment coverage for newly eligible enrollees, Medicaid is expected to soon become the largest payer of addiction treatment.1 As such, Medicaid will obtain principal market power over major segments of the addiction treatment system in the United States and, therefore, have the ability to influence addiction treatment practices on a broader scale than ever before.
In this article we provide a brief history of financing for mental health and addiction treatment, and we highlight Medicaid’s contrasting role in paying for these services. We then show how Medicaid influenced reforms in the mental health delivery system, and we draw strategic lessons for addiction treatment in three main areas: leveraging optional coverage categories to tailor Medicaid to the unique needs of the addiction treatment system, providing incentives for addiction treatment programs to create and deliver high-quality alternatives to inpatient treatment, and using targeted Medicaid licensure standards to increase the quality of addiction services. These three strategies are consistent with the broader goal of integration of behavioral health services with mainstream medical care in the United States.
A Tale Of Two Systems
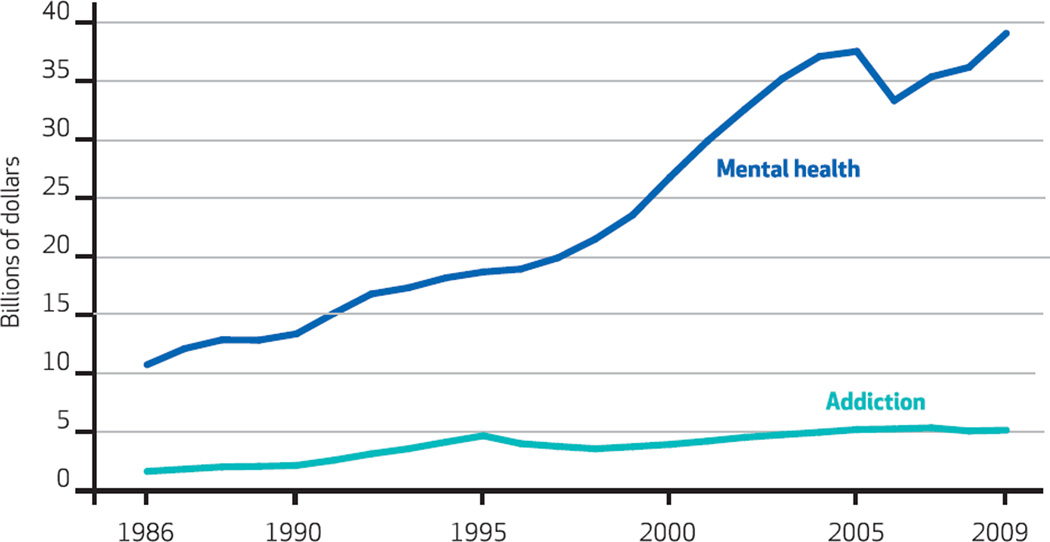
Medicaid has played a very different role in financing mental health versus addiction treatment for low-income individuals over the past thirty years. Both systems initially received little revenue from Medicaid.1 However, Medicaid’s role in financing mental health treatment has grown dramatically, while its role in financing addiction treatment has been more modest and constrained (Exhibit 1).
EXHIBIT 1. Medicaid Expenditures For Mental Health And Addiction Treatment Services For Selected Populations, 1986–2009.
SOURCE Substance Abuse and Mental Health Services Administration. National expenditures for mental health services and substance abuse treatment, 1986–2009 (see Note 5 in text). NOTE Estimates are inflation-adjusted (2009).
Before 1965 the vast majority of mental health treatment services were paid for by states and administered under the authority of state mental health agencies. Medicaid changed this arrangement.3 In 1981 Medicaid represented only 16 percent of revenues received by state mental health agencies, the major providers of mental health treatment to low-income individuals. The vast majority of funding—73 percent—came from state general revenue and special funds. By 2010 Medicaid accounted for half of state mental health agency–controlled revenues and was responsible for nearly two-thirds of all new state mental health agency spending between 2001 and 2010.4 Medicaid is now the largest purchaser of mental health treatment, accounting for nearly half of all public dollars and more than a quarter of all mental health spending (public and private combined).5
A principal driver of this growth has been expanded eligibility for people with mental health disorders. The creation of the Supplemental Security Income (SSI) program in 1972 and its linkage with Medicaid eligibility resulted in a major change in Medicaid’s role in covering people with mental health disorders severe enough to qualify as a disabling condition. Since the late 1980s mental health disorders have represented one of the fastest-growing categories of SSI eligibility. In 2009, 41 percent of all SSI beneficiaries younger than age sixty-five qualified because of a mental disorder.6
A significant expansion in the scope of mental health treatment services covered by Medicaid has also increased its role. The addition of targeted case management in 1986 and the expansion of psychosocial rehabilitation under Medicaid’s rehabilitation option in the early 1990s gave states important new options for providing intensive community-based supports to people with serious mental health disorders. Currently, almost all states have adopted these options. By 2005 targeted case management accounted for $2.9 billion in Medicaid expenditures, while services provided under the rehabilitative services option accounted for another $6.4 billion.7 People with mental health disorders constitute close to three-quarters of service recipients under the rehabilitative services option and account for almost 80 percent of expenditures.8 These options have enabled states to provide evidence-based practices such as assertive community treatment, medication management, and family psychoeducation.7
Medicaid has traditionally played a more modest role in financing addiction treatment. National spending for addiction treatment increased by roughly $15 billion between 1986 and 2009, representing an average annual rate of growth in nominal dollars of 4.4 percent.9 Medicaid spending on addiction treatment services also grew substantially during this period, from less than $1 billion to $5 billion. However, because other funding sources for addiction treatment also increased during this time, Medicaid’s share of spending remained steady at approximately 20 percent of total addiction outlays. In contrast, state and local government funds for addiction treatment increased from $2.5 billion in 1986 to $7.5 billion in 2009 and continued to increase, albeit modestly, as a percentage of overall spending.9 Unlike the financing of mental health treatment, these state and local funds have remained the backbone of the publicly funded addiction treatment system.
Medicaid’s coverage for treatment of mental health and addictive disorders has diverged in important ways.
Before 1996 it seemed likely that Medicaid’s financing of addiction treatment would follow the same path that the program has taken in funding for mental health. Between 1990 and 1995 the number of people qualifying for SSI through an addiction-related disability increased by more than 500 percent. However, concerns emerged about rapid growth in the number of people enrolling in Medicaid as a result of addiction-related disability, which were rooted in a longer-standing controversy as to whether addiction should even be characterized as a disabling condition for the purpose of receiving public aid.10
These concerns were embodied in the Contract with America Advancement Act of 1996, under which addiction became disallowed as a qualifying condition for federal disability programs. Consequently, the number of people with addiction disorders who qualified for Medicaid was greatly circumscribed. Although only about 200,000 recipients were immediately affected by this policy, because the new law restricted states’ ability to use Medicaid as a vehicle to cover and treat the majority of people with addiction disorders, its significance was, of course, much broader over time. When the ACA passed in 2010, for example, only about 20 percent of patients entering publically funded addiction treatment programs were covered by Medicaid.11
Moreover, coverage for addiction treatment within state Medicaid programs has been less comprehensive than mental health coverage. As recently as 2013 several states did not provide any coverage for addiction treatment, apart from federally mandated detoxification and short-term inpatient treatment. States can use the same options for addiction treatment that were used to establish expanded coverage for mental health treatment, including the rehabilitative services, case management, and the community-based services options. However, states’ take-up of optional coverage for addiction services has been highly variable. In 2003, the most recent year in which state Medicaid coverage for addiction was systematically reviewed, thirty states covered outpatient group counseling for substance abuse.12 Twenty-five states covered methadone maintenance. Twenty covered day treatment, and only seventeen covered buprenorphine and naltrexone—evidence-based treatments for opioid addiction.
The ACA And Addiction Treatment
The ACA is expected to dramatically change the historic contrast between Medicaid’s role in financing mental health and in financing addiction treatment for low-income Americans.1,13,14 The law mandates Medicaid coverage for addiction treatment and prohibits limits on the provision of addiction treatment services that is more restrictive than those for other medical services. The ACA also enables states to expand eligibility to all citizens with incomes at or below 138 percent of the federal poverty level. It therefore removes categorical federal restrictions on eligibility that have historically limited Medicaid enrollment to children, parents, elderly, and individuals with disabilities. Millions of low-income Americans who experience either of these disorders have become Medicaid-eligible in states that have embraced this eligibility expansion, and more are expected to do so in the years ahead.15 Now active in twenty-nine states and the District of Columbia, the Medicaid expansion will increase enrollment by 10.7 million people.15 Medicaid spending for addiction treatment is projected to double from $5 billion to $12 billion by 2020, quickly making Medicaid the largest payer of addiction treatment in the country.1
Lessons For Medicaid’s Future In Addiction Treatment
Because Medicaid has been the dominant funder in mental health treatment, reforms to the program have had wide-reaching implications for the entire system of mental health care. Below we discuss three broad lessons that the addiction treatment system can learn from the successes and challenges of the mental health treatment system’s expansion within Medicaid. We do not mean to suggest that the mental health treatment system is without challenges or that the challenges facing the addiction treatment system are the same as those facing mental health treatment. Instead, we seek to point out strategies and successes of the mental health treatment system that may inform efforts to improve access and quality in addiction treatment, particularly for low-income individuals, who make up the majority of Medicaid enrollees.
REGULATORY FLEXIBILITY
The first lesson from the experience of the mental health treatment system highlights the importance of regulatory flexibility around Medicaid’s optional coverage categories. Since the 1980s, stakeholders in the mental health treatment system have skillfully crafted more responsive systems of care for mental health disorders. As noted, Medicaid’s optional benefits—targeted case management and rehabilitation—allow states to use Medicaid to finance a variety of community support programs for people with serious mental health disorders, including intensive case management, crisis intervention, family psychosocial education, life skills training and social supports, assertive community treatment, community residential services, education and employment related supports, and peer services.16,17 This flexibility was enormously important for expanding access to a range of services,18,19 and states’take-up grew substantially over time. In 1988 only nine states covered psychosocial rehabilitation or targeted case management for people with mental health disorders; today nearly every state has adopted these options.
More recently, states have sought to expand options for mental health treatment under Medicaid’s 1915(c) home and community-based services (HCBS) waiver program. In the past, the HCBS waiver program was constrained in its ability to rebalance institutional care for people with severe mental illnesses toward more home and community-based models by Medicaid’s Institutions for Mental Disease (IMD) exclusion. This exclusion prohibits Medicaid coverage of working-age adults in IMDs, defined as nursing homes, hospitals, or other institutions of more than sixteen beds that are primarily engaged in the treatment of mental disorders.
6 States In 2012 only six states required addiction treatment providers to possess a bachelor’s degree, and only one required a master’s degree.
The IMD exclusion made it difficult for states to meet the cost-neutrality requirements of the HCBS waiver program for adults with severe mental illnesses. However, recent policy clarifications have expanded this option. Four states—Colorado, Connecticut, Montana, and Wisconsin—currently have HCBS waivers for adults with severe mental illnesses. Demonstration projects, such as the Money Follows the Person Rebalancing Demonstration, have also played an important role in expanding Medicaid’s role in mental health care, as have new options for home and community-based services authorized under the Deficit Reduction Act of 2005 and the ACA.7,20,21
A growing body of evidence suggests that inpatient addiction treatment is no more effective than outpatient treatment for many patients.
In the contrasting case of addiction disorders, some states have made great progress toward using Medicaid options to expand coverage for these disorders. However, the overall national impact of these efforts has been limited. A minority of states have actively pursued this strategy, in part because the largest group of people receiving addiction treatment in the United States prior to 2014 were uninsured. Yet many of the existing options within Medicaid can be used to expand addiction coverage, including the rehabilitative services, case management, and HCBS options, and the 1115 waiver, which enables states to implement five-year demonstration projects that incorporate coverage and eligibility expansions or service delivery model innovations.
Learning from the experience of mental health coverage, stakeholders in addiction treatment can leverage the flexibility built into Medicaid’s optional benefit policies to advocate for coverage across the service continuum—from intensive outpatient treatment and crisis management to recovery-oriented services—to effectively manage addiction as a chronic illness. Moreover, a substantial body of research supports the efficacy and cost-effectiveness of medication-assisted addiction treatments.22,23 Especially since current adoption of such programs is sparse,24 Medicaid coverage flexibility should include room for them. Relatedly, most states do not provide reimbursement for wraparound services associated with opioid treatment programs such as initial assessments, brief counseling, and follow-up with patients who are receiving these drugs.
The mental health and addiction treatment systems now face a common challenge to integrate with each other.
ALTERNATIVES TO INPATIENT TREATMENT
The second lesson to be drawn from the mental health system relates to Medicaid’s capacity to promote broad-scale delivery system changes, particularly in spurring the creation of a high-quality alternative to treatment in inpatient and other institutionalized settings. Medicaid’s role in promoting community-based services for mental health was initially inadvertent. Medicaid’s IMD exclusion strengthened incentives for states to shift patient care (and costs) from state-financed mental hospitals into Medicaid-reimbursable settings—such as nursing homes, community mental health centers, and general hospitals. Between 1955 and 1980 the resident census in state mental hospitals dropped by 75 percent. This early history played a critical role in making Medicaid the primary driver of mental health systems change.19
Medicaid also played a complementary role in helping states comply with a series of court decisions requiring greater emphasis on home and community-based services. Medicaid’s support for efforts such as Money Follows the Person and Balanced Incentives Program—policies expanded and supported by the ACA—is an important tool for many states seeking to meet their legal responsibilities to expand or improve their alternatives to institution-based care.25,26 Programs such as assertive community treatment, covered by a number of state Medicaid programs, provide intensive supports for people with severe mental illnesses, to enable them to manage their illnesses while remaining in the community.27
In crafting Medicaid addiction treatment coverage, states should consider how coverage design can be used to promote high-quality, community-based alternatives to inpatient addiction treatment for people with more severe addictive disorders. There will always be a need for inpatient addiction treatment services for people who require medically risky detoxification, are in crisis, or are experiencing severe symptoms. However, a growing body of evidence suggests that inpatient addiction treatment is no more effective than outpatient treatment for many patients. Also, inpatient treatment is more costly, restrictive, and stigmatized than community-based addiction treatment.28 Nonetheless, despite this evidence, a large proportion of people receive addiction treatment in inpatient settings. In 2013 roughly 45 percent of people who received addiction treatment reported receiving it in a residential or inpatient setting.29
EXPANDING TREATMENT OPTIONS
The third lesson concerns the power of public purchasers, namely Medicaid, to expand the supply of qualified treatment providers, and consequently, elevate the quality of services provided. As late as 1970 staffing in state mental hospitals consisted of a small number of professional mental health workers and a large number of less skilled custodial workers.3 However, as more institutional forms entered the mental health market, professional staffing ratios increased.30 As community mental health centers emerged in response to deinstitutionalization and Medicaid dollars funded care in such centers, a whole new cadre of mental health professionals responded to this supply. These growing mental health professions exerted political pressure on politicians to establish state licensing laws. By 1990 forty-two states had passed such laws, and eventually most states passed mandates that required insurers to cover mental health services provided by these professionals.3
Medicaid regulations for staff providing mental health treatment have also increased substantially. Under the rehabilitative services option, for example, the Centers for Medicare and Medicaid Services requires that mental health treatment services be authorized by “licensed practitioners of the healing arts.” Most state Medicaid programs define licensed practitioners of the healing arts as a licensed psychiatrist, psychologist, clinical social worker, or registered or advanced practice nurse. States also define the qualifications of service providers under Medicaid, and most require that mental health providers possess state board licensure as well as a master’s or doctoral degree from an accredited university in a relevant area of practice. States that cover paraprofessionals have also established minimal qualifications for this role.31
The evolution of licensing standards in the mental health treatment system differs markedly from that governing addiction treatment. Many commentators and researchers express concerns about the overall quality of addiction treatment providers in the United States.13,14 While the number and type of addiction treatment providers have similarly increased, fewer than half of addiction treatment providers have professional degrees and any formal training or credentialing in addiction treatment.32 Most states have no or low licensure standards for addiction treatment providers. In 2012 only six states required addiction treatment providers to possess a bachelor’s degree, and only one state required a master’s degree.33 Fourteen states had no educational attainment requirements for licensure whatsoever.
As Medicaid’s role in addiction treatment expands in the years ahead, there is an important opportunity to use the program to improve quality. Medicaid can require formal training and licensure standards for staff who provide addiction treatment as a condition of Medicaid certification. Because Medicaid is poised to become the largest payer of addiction treatment, most addiction treatment programs will need to remain or become Medicaid certified to access this increasingly important revenue source.34
Such requirements could also help speed implementation of evidence-based addiction therapies, given evidence that licensed professionals are more likely than nonlicensed providers to endorse and use such therapies.33 For this strategy to be effective, many existing addiction treatment providers will need technical assistance and, ideally, additional financial resources to meet new Medicaid staffing requirements.
The Common Challenge Of Integration
The mental health and addiction treatment systems have evolved into two different and largely separate systems over the past fifty years. These systems now face a common challenge to integrate with each other. Stakeholders across both systems recognize the high prevalence of co-occurring mental health and addiction disorders. The field has advanced treatment strategies that address both disorders in tandem. Unfortunately, funding regulations often conflict with integrated delivery approaches and have played a major role in hindering their proliferation.35 As Medicaid plays a greater role in financing addiction treatment, there will be new opportunities to improve access to integrated treatment for people who are newly eligible for Medicaid, as well as Medicaid enrollees in states that have expanded coverage for addiction treatment.
Medicaid health homes provide a major new option with the potential to address long-standing problems of segmentation in physical and behavioral health—including mental health and addiction treatment. At an enhanced federal matching rate for the first two years, state Medicaid programs have the option to create health homes, which deliver coordinated care to enrollees with multiple chronic health conditions, including mental health and addiction disorders. The health home model has the potential to significantly improve coordination and integration of care and may become the primary model of treatment for people who have mental health or addiction treatment needs but require less intensive services.36
Medicaid agencies must develop strategies to support a continuum of care that responds to people with diverse addiction-related needs.
Both systems also face the challenge to integrate their services within primary care settings, where the vast majority of health care services to people with mental health or addiction use disorders will actually be provided or initiated. Integrating mental health and addiction treatment into primary care can improve quality and reduce overall health care costs.37–39 Primary care providers have made greater strides in integrating mental health treatment into their repertoire of services. General physicians provide an increasing share of mental health services.3 By the 1990s, 34 percent of mental health diagnoses came from general physicians, and prescribing of psychotropic medications in primary care has increased substantially. Assessment and treatment of addiction treatment has been less well integrated into primary care, in part as a result of restrictions on prescribing of addiction medications.40
Conclusion
Under the ACA Medicaid expansion, Medicaid agencies will become increasingly important purchasers of addiction treatment services. As such, they will now play a regulatory role analogous to the one they have played with the mental health treatment system.
While Medicaid agencies consider how to optimally allocate resources for addiction treatment, differences in the severity of need, as illustrated in mental health, will complicate these financing and regulatory decisions. Medicaid agencies must develop strategies to support a continuum of care that effectively responds to people with diverse addiction-related needs. State Medicaid programs will need to create regulatory policies that set clear rules to improve quality while remaining flexible and nimble to adjust to different patient needs.
Any major purchaser such as Medicaid will be able to create important incentives to develop new innovative delivery model reforms. It is hoped that states will consider the power of this leverage prospectively to provide efficient, high-quality addiction treatment services instead of responding retrospectively to unintended problems that so often arise with the infusion of new funding.
Acknowledgments
The authors acknowledge support from the National Institute on Drug Abuse (Grant No. R01 DA034634-01) for its project, “The impact of health reform on outpatient substance abuse treatment programs,” although the recommendations and responsibility for any errors rest solely with the authors. The authors also acknowledge helpful feedback from the editors of Health Affairs and two anonymous reviewers.
Contributor Information
Christina Andrews, College of Social Work, University of South Carolina, in Columbia.
Colleen M. Grogan, Email: cgrogan@uchicago.edu, School of Social Service Administration, University of Chicago, in Illinois.
Marianne Brennan, School of Social Service Administration, University of Chicago.
Harold A. Pollack, School of Social Service Administration, University of Chicago.
NOTES
- 1.Mark TL, Levit KR, Yee T, Chow CM. Spending on mental and substance use disorders projected to grow more slowly than all health spending through 2020. Health Aff (Millwood) 2014;33(8):1407–1415. doi: 10.1377/hlthaff.2014.0163. [DOI] [PubMed] [Google Scholar]
- 2.Frank RG, Goldman HH, Hogan M. Medicaid and mental health: be careful what you ask for. Health Aff (Millwood) 2003;22(1):101–113. doi: 10.1377/hlthaff.22.1.101. [DOI] [PubMed] [Google Scholar]
- 3.Frank RG, Glied SA. Better but not well: mental health policy in the United States since 1950. Baltimore (MD): Johns Hopkins University Press; 2006. [Google Scholar]
- 4.Substance Abuse and Mental Health Services Administration. Rockville (MD): SAMHSA; 2014. [cited 2015 Jun 4]. Controlled expenditures and revenues for mental health services, state fiscal year 2009 [Internet] p. 142. Available from: http://store.samhsa.gov/product/Controlled-Expenditures-and-Revenues-for-Mental-Health-Services-State-Fiscal-Year-2009/SMA14-4843. [Google Scholar]
- 5.Substance Abuse and Mental Health Services Administration. Rockville (MD): SAMHSA; 2013. [cited 2015 Jun 4]. National expenditures for mental health services and substance abuse treatment, 1986–2009 [Internet] p. 108. Available from: http://store.samhsa.gov/product/National-Expenditures-for-Mental-Health-Services-and-Substance-Abuse-Treatment-1986–2009/SMA13-4740. [Google Scholar]
- 6.Garfield R. Washington (DC): Kaiser Commission on Medicaid and the Uninsured; 2011. Apr 1, [cited 2015 Jun 4]. Mental health financing in the United States: a primer [Internet] p. 46. Available from: http://kff.org/medicaid/report/mental-health-financing-in-the-united-states/ [Google Scholar]
- 7.Shirk C. Washington (DC): National Health Policy Forum; 2008. Oct 23, [cited 2015 Jun 4]. Medicaid and mental health services [Internet] p. 19. Available from: http://www.nhpf.org/library/background-papers/BP66_MedicaidMental-Health_10-23-08.pdf. [Google Scholar]
- 8.Crowley JS, O’Malley M. Washington (DC): Kaiser Commission on Medicaid and the Uninsured; 2007. Jul 30, [cited 2015 Jun 4]. Medicaid’s rehabilitation services option: overview and current policy issues [Internet] p. 24. Available from: http://kff.org/medicaid/issue-brief/medicaids-rehabilitation-services-option-overview-and-current/ [Google Scholar]
- 9.Levit KR, Mark TL, Coffey RM, Frankel S, Santora P, Vandivort-Warren R, et al. Federal spending on behavioral health accelerated during recession as individuals lost employer insurance. Health Aff (Millwood) 2013;32(5):952–962. doi: 10.1377/hlthaff.2012.1065. [DOI] [PubMed] [Google Scholar]
- 10.Gresenz C, Watkins K, Podus D. Supplemental security income (SSI), disability insurance (DI), and substance abusers. Community Ment Health J. 1998;34(4):337–350. doi: 10.1023/a:1018779805833. [DOI] [PubMed] [Google Scholar]
- 11.Substance Abuse and Mental Health Services Administration. Rockville (MD): SAMHSA; 2014. Feb 6, [cited 2015 Jun 4]. The TEDS report: health insurance status of adult substance abuse treatment admissions aged 26 or older: 2011 [Internet] Available from: http://www.samhsa.gov/data/sites/default/files/sr134-health-insurance-2014/sr134-health-insurance-2014/sr134-health-insurance-2014.htm. [PubMed] [Google Scholar]
- 12.Robinson G, Kaye N, Bergman D, Moreaux M, Baxter C. Rockville (MD): Substance Abuse and Mental Health Services Administration; 2005. Jan, [cited 2015 Jun 4]. State profiles of mental health and substance abuse services in Medicaid [Internet] p. 61. Available from: http://store.samhsa.gov/product/State-Profiles-of-Mental-Health-and-Substance-Abuse-Services-in-Medicaid/NMH05-0202. [Google Scholar]
- 13.Buck JA. The looming expansion and transformation of public substance abuse treatment under the Affordable Care Act. Health Aff (Millwood) 2011;30(8):1402–1410. doi: 10.1377/hlthaff.2011.0480. [DOI] [PubMed] [Google Scholar]
- 14.Humphreys K, Frank RG. The Affordable Care Act will revolutionize care for substance use disorders in the United States. Addiction. 2014;109(12):1957–1958. doi: 10.1111/add.12606. [DOI] [PubMed] [Google Scholar]
- 15.Paradise J. Medicaid moving forward [Internet] Washington (DC): Kaiser Commission on Medicaid and the Uninsured; 2015. Mar, [cited 2015 Jun 4]. p. 12. Available from: http://files.kff.org/attachment/issue-brief-medicaid-moving-forward. [Google Scholar]
- 16.Smith G, Kennedy C, Knipper S, O’Brien J. Washington (DC): Department of Health and Human Services, Office of the Assistant Secretary for Planning and Evaluation; 2005. Jan, [cited 2015 Jun 4]. Using Medicaid to support working age adults with serious mental illnesses in the community: a handbook [Internet] p. 188. Available from: http://aspe.hhs.gov/daltcp/reports/handbook.pdf. [Google Scholar]
- 17.Koyanagi C, Semansky R. Washington (DC): Judge David L. Bazelon Center for Mental Health Law; 2001. Nov, [cited 2015 Jun 4]. Recovery in the community: funding mental health rehabilitative approaches under Medicaid [Internet] p. 92. Available from: http://www.bazelon.org/LinkClick.aspx?fileticket=S3P8OI01Rv0%3d&tabid=104. [Google Scholar]
- 18.Koyanagi C, Goldman HH. The quiet success of the national plan for the chronically mentally ill. Hosp Community Psychiatry. 1991;42(9):899–905. doi: 10.1176/ps.42.9.899. [DOI] [PubMed] [Google Scholar]
- 19.Grob GN, Goldman HH. The dilemma of federal mental health policy: radical reform or incremental change? New Brunswick (NJ): Rutgers University Press; 2006. [Google Scholar]
- 20.Buck JA. Recent changes in Medicaid policy and their possible effects on mental health services. Psychiatr Serv. 2009;60(11):1504–1509. doi: 10.1176/ps.2009.60.11.1504. [DOI] [PubMed] [Google Scholar]
- 21.Ng T, Harrington C, Musumeci MB, Reaves EL. Washington (DC): Kaiser Commission on Medicaid and the Uninsured; 2014. Dec, [cited 2015 Jun 2]. Medicaid home and community-based services programs: 2011 data update [Internet] p. 52. Available from: http://files.kff.org/attachment/report-medicaid-home-and-community-based-services-programs-2011-data-update. [Google Scholar]
- 22.Barnett PG, Zaric GS, Brandeau ML. The cost-effectiveness of buprenorphine maintenance therapy for opiate addiction in the United States. Addiction. 2001;96(9):1267–1278. doi: 10.1046/j.1360-0443.2001.96912676.x. [DOI] [PubMed] [Google Scholar]
- 23.Zaric GS, Barnett PG, Brandeau ML. HIV transmission and the cost-effectiveness of methadone maintenance. Am J Public Health. 2000;90(7):1100–1111. doi: 10.2105/ajph.90.7.1100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.American Society of Addiction Medicine. Advancing access to addiction medications: implications for opioid addiction treatment. Chevy Chase (MD): ASAM; 2013. Jun, [cited 2015 Jun 4]. p. 221. Available from: http://www.asam.org/docs/default-source/advocacy/aaam_implications-for-opioid-addiction-treatment_final. [Google Scholar]
- 25.Kaiser Commission on Medicaid and the Uninsured. Olmstead v. L. C.: the interaction of the Americans with Disabilities Act and Medicaid [Internet] Menlo Park (CA): Henry J. Kaiser Family Foundation; 2004. Jun, [cited 2015 Jun 4]. Available from: http://kff.org/medicaid/event/olmstead-v-l-c-the-interaction-of/ [Google Scholar]
- 26.Ng T, Wong A, Harrington C. Home and community-based services: introduction to Olmstead lawsuits and Olmstead plans [Internet] San Francisco (CA): University of California, San Francisco, National Center for Personal Assistance Services; 2013. May, [cited 2015 Jun 4]. Available from: http://www.americanbar.org/content/dam/aba/events/homelessness_poverty/2013_Annual_Meeting_Medicaid/intro_to_olmstead_lawsuits_and_plans.authcheckdam.pdf. [Google Scholar]
- 27.Phillip SD, Burns BJ, Edgar ER, Mueser KT, Linkins KW, Rosenheck RA, et al. Moving assertive community treatment into standard practice. Psychiatr Serv. 2001;52(6):771–779. doi: 10.1176/appi.ps.52.6.771. [DOI] [PubMed] [Google Scholar]
- 28.McCarty D, Capoccia V, Chalk M. Treating alcohol and drug use disorders. Health Aff (Millwood) 2013;32(3):630. doi: 10.1377/hlthaff.2013.0093. [DOI] [PubMed] [Google Scholar]
- 29.Substance Abuse and Mental Health Services Administration. Rockville (MD): SAMHSA; 2014. Sep, [cited 2015 Jun 4]. Results from the 2013 National Survey on Drug Use and Health: summary of national findings [Internet] Available from: http://www.samhsa.gov/data/sites/default/files/NSDUHresultsPDFWHTML2013/Web/NSDUHresults2013.pdf. [Google Scholar]
- 30.Manderscheid RW, Atay JE, del R, Hernandez-Cartagena M, Edmond PY, Male A, Parker A, et al. Highlights of organized mental health services in 1998 and major national and state trends. In: Manderscheid RW, Henderson MJ, editors. Mental health, United States, 2000. Rockville (MD): Substance Abuse and Mental Health Services Administration; 2001. pp. 135–171. [Google Scholar]
- 31.O’Brien J, Lanahan P, Jackson E. Recovery in the community: volume 2: program and reimbursement strategies for mental health rehabilitative approaches under Medicaid [Internet] Washington (DC): Judge David L. Bazelon Center for Mental Health Law; 2003. Jun, [cited 2015 Jun 4]. p. 49. Available from: http://www.bazelon.org/LinkClick.aspx?fileticket=TBb6QNGK9io%3d&tabid=104. [Google Scholar]
- 32.Abraham AJ, Knudsen HK, Rieckmann T, Roman PM. Disparities in access to physicians and medications for the treatment of substance use disorders between publicly and privately funded treatment programs in the United States. J Stud Alcohol Drugs. 2013;74(2):258–265. doi: 10.15288/jsad.2013.74.258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.CASAColumbia. Addiction medicine: closing the gap between science and practice [Internet] New York (NY): CASAColumbia; 2012. Jun, [cited 2015 Jun 4]. p. 586. Available from: http://www.casacolumbia.org/addiction-research/reports/addiction-medicine. [Google Scholar]
- 34.Andrews C, Abraham A, Grogan CM, Pollack HA, Bersamira CB, Humphreys K, et al. Despite resources from the ACA, most states do little to help addiction treatment programs implement health care reform. Health Aff (Millwood) 2015;34(5):828–835. doi: 10.1377/hlthaff.2014.1330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mechanic D. More people than ever before are receiving behavioral health care in the United States, but gaps and challenges remain. Health Aff (Millwood) 2014;33(8):1416–1424. doi: 10.1377/hlthaff.2014.0504. [DOI] [PubMed] [Google Scholar]
- 36.Nardone M, Paradise J. Health homes for Medicaid beneficiaries with chronic conditions [Internet] Washington (DC): Kaiser Commission on Medicaid and the Uninsured; 2012. Aug 1, [cited 2015 Jun 4]. p. 17. Available from: http://kff.org/health-reform/issue-brief/health-homes-for-medicaid-beneficiaries-with-chronic/ [Google Scholar]
- 37.Butler M, Kane RL, McAlpine D, Kathol RG, Fu SS, Hagedorn H, et al. Rockville (MD): Agency for Healthcare Research and Quality; 2008. Oct, [cited 2015 Jun 4]. Integration of mental health/substance abuse and primary care [Internet] p. 266. Available from: http://www.ahrq.gov/research/findings/evidence-based-reports/mhsapc-evidence-report.pdf. [Google Scholar]
- 38.Friedmann PD, Zhang Z, Hendrickson J, Stein MD, Gerstein DR. Effect of primary medical care on addiction and medical severity in substance abuse treatment programs. J Gen Intern Med. 2003;18(1):1–8. doi: 10.1046/j.1525-1497.2003.10601.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Weisner C, Mertens J, Parthasarathy S, Moore C, Lu Y. Integrating primary medical care with addiction treatment: a randomized controlled trial. JAMA. 2001;286(14):1715–1723. doi: 10.1001/jama.286.14.1715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Andrews CM, D’Aunno TA, Pollack HA, Friedmann PD. Adoption of evidence-based clinical innovations: the case of buprenorphine use by opioid treatment programs. Med Care Res Rev. 2014;71(1):43–60. doi: 10.1177/1077558713503188. [DOI] [PMC free article] [PubMed] [Google Scholar]