Introduction
The landscape of surgical resident education at most institutions has changed substantially over the last few decades, due to a myriad of factors including work-hour restrictions, attending responsibilities, patient expectations, curriculum oversight and accreditation guidelines. Ward teaching, apprenticeship modeling, and grand rounds have historically been the building blocks of the surgical curriculum. The Accreditation Council for Graduate Medical Education (ACGME) now mandates that programs have a “comprehensive, effective and well-organized educational curriculum; ensure that conferences be scheduled to permit resident attendance on a regular basis, and resident time must be protected from interruption by routine clinical duties1.” Constraints on faculty time, including requirements for relative value units (RVUs), increased documentation, and in the case of academic faculty, research productivity, have severely limited the amount of faculty time that can be devoted to resident education. These evolving pressures have put a strain on the educational environment of modern surgical residency programs, necessitating change. Many institutions have addressed these demands by relying on ancillary staff and nonclinical educators who receive salary support to provide resident education. We present a model for academic institutions without salaried professional nonclinical educators.
The “resident as educator” model (RAE) was introduced at Vanderbilt University in 2008, empowering residents to serve as the organizers and, often, the teachers of the educational curriculum. Peer-assisted learning is defined as individuals of similar training levels who are not professional teachers who help each other learn and as a result learn by teaching2–5. The model that follows was presented in 2012 as a workshop at the annual meeting for the Association for Program Directors in Surgery (APDS)6. As surgery residencies at academic centers are often seven years in length, considerably longer than other specialties, many of these years in training are at the equivalent of attending status in some specialties. Prior work has shown that both faculty and students have indicated that residents are highly valuable for clinical and surgical education7,8. Also, many residents come to training with significant teaching exposure or experience, having served as teaching assistants for anatomy or other courses while in medical school, some having even participated in formal students-as-teachers training programs9,10. There have been limited formal studies investigating the use of peer learning in resident education11,12. However, these studies confirmed that peer teaching, as in the RAE model, can be effective in the resident population4,11,12. Residents provide a unique and beneficial perspective on effective education given their shared proximity to the learners training level. Therefore, surgical residents at academic institutions are a strong, sustainable, and often already well-trained option to bridge the gap in faculty availability.
From an administrative perspective, promoting residents as educators leads to an overall total benefit for the program and department, increases efficiency in curriculum, and is both cost-effective and time-efficient. We will outline these aspects below as they pertain to intern and junior resident education.
Background
Resident education has historically been based on a large lecture-teaching model or clinical teaching. Accordingly, resident education at Vanderbilt prior to a curriculum revision in 2007–2008 was largely centered on weekly Grand Rounds conferences. Other educational opportunities included a faculty-led teaching session following grand rounds and educational discussions centered on cases presented at weekly morbidity and mortality conferences (personal communication, JLT). No organized curricula were in place other than intermittent, industry-sponsored events. In 2007, a group of residents attended the American College of Surgeons (ACS) sponsored Residents as Teachers and Leaders conference, a course designed for mid-to senior-level surgery residents to address “the skills necessary to be more effective teachers and more successful leaders13.” Following the conference and the resident discussion that ensued, the educational curriculum at Vanderbilt transitioned to a resident-organized model.
The RAE model is built on a culture of commitment to education, skill development and team building. Several modules were initially implemented, all designed at a level to address intern or junior level residents. These included (1) intern boot camp, (2) summer school, (3) technical skill sessions, (4) trauma orientation, and (5) additional weekly teaching conferences. Later, a fourth year medical student surgical preparation course was added to the curriculum. RAE acted as a focus group, reflected on learning deficiencies in their progression to that point, and designed initial curricula set forth on specific components. The modules designed for interns in their current form are organized throughout the academic year, and a timeline is shown in Figure 1.
Figure 1.
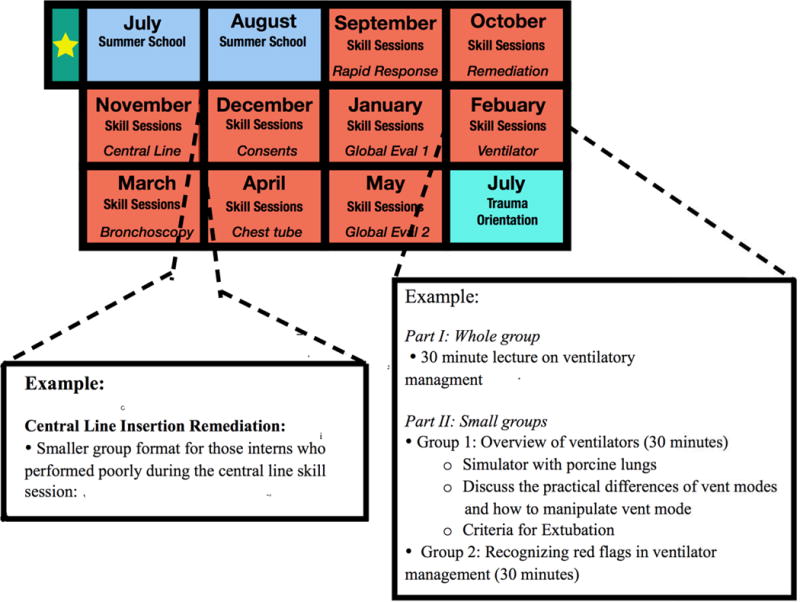
Curriculum schedule for the academic year with detailed overview of the central line insertion remediation session and the ventilator management skill session
Two residents in research or in some instances, senior residents, are designated for each module of the intern curriculum. The following outlines each of these modules:
1. Intern Boot Camp
Prior to the start of the academic year, incoming interns are immersed in small group sessions, simulation scenarios, and hands-on practice with partial task trainers, collectively referred to as “Intern Boot Camp” (Table 1). Faculty and residents in anesthesia, surgery, and interventional radiology teach these sessions. By focusing on the management of common conditions and the initial management of unstable patients, these training sessions are designed to refresh interns and ease anxiety as they enter the wards.
Table 1.
Topics covered in Intern Boot Camp
| Intern Boot Camp |
|---|
1. The unstable patient education:
|
2. The stable patient curriculum:
|
2. Intern Summer School
During the first two months of the academic year, the RAE direct Summer School, a series of conferences held from 7 to 9 am each Friday morning for a total of 16 hours of instruction. These are centered around “TED” talk style lectures (15 minutes)14 and emphasize important management strategies for high yield topics with the goal to prepare new residents for the successful management of common clinical scenarios (Table 2). Surgical Olympics, a skills competition, is incorporated into the curriculum to mark the end of Summer School.
Table 2.
Intern Summer School
| Intern Summer School [RAE Commitment time: 4 hours/week for 2 months] |
|---|
1.Learning format includes:
|
2. Lectures focus on:
|
3. Breakout sessions involving smaller groups:
|
| 4. Suturing and knot tying skill sessions |
3. Intern Skills Sessions
Intern skills sessions are held every Thursday afternoon throughout the year for 2 hours, and each intern is required to attend one session a month, as the topic changes monthly (Table 3). This forum allows interns to learn in a smaller group setting with attention to outcomes and performance. The curriculum focuses on surgical technique, surgical knowledge, and critical care management. Although the curriculum is designed and managed by RAE, attendings are asked to deliver the topics in order to reinforce the topic importance, convey nuances that come with additional experience, and to expose the interns to the faculty in a small group setting. Each session is followed by a written evaluation to assess how the interns processed the information that was discussed, and time is provided between sessions for remediation if needed.
Table 3.
Topics covered in Intern Skill Sessions
| Intern Skills Sessions [RAE Commitment time: 4 hours/week for 8 months] |
|---|
1. Case based simulation
|
2. Standardized patient simulation
|
3. Procedure simulation
|
4. Surgical technique and anatomy
|
At the end of the Intern Skill Sessions curriculum, a global assessment evaluates interns by requiring each one to obtain a consent form for a central line, place a central line in a partial task trainer, read a post-procedure chest x-ray, identify acute pathology (i.e. tension pneumothorax or hemothorax), and subsequently place a chest tube in a simulation model. The assessment also requires the intern to then communicate the complication to the family (“breaking bad news”). The consent and breaking bad news components of the assessment are performed using standardized patients and are evaluated by upper level residents and attendings in real time through a video feed. The interns are evaluated using a standardized rubric and given feedback that emphasizes high yield points during a debriefing session. This exercise is designed to combine communication skills, procedural skills, and clinical decision-making. Senior residents and attendings provide the assessment and debriefing in real time.
4. Trauma Orientation
Residents as educators orchestrate trauma orientation for the rising second year residents in a daylong session. Attendings and senior residents give lectures and work through simulated trauma scenarios (Table 4). This introduction also exposes the residents to the clinically demanding trauma rotation in a controlled setting, emphasizing information collection, patient triage, and time management and organization skills.
Table 4.
Topics covered in Trauma Orientation
| Trauma Orientation [RAE Commitment time: 8 hours total] |
|---|
1. Trauma resuscitation is reviewed in detail
|
| 2. “Survival Tips” are communicated |
5. Resident Teaching Conferences
Resident teaching conferences are scheduled twice a week for all residents (Table 5). These didactic lectures provide an opportunity for the presenting residents to hone their public speaking skills before a large audience and allow other residents to benefit from patient scenarios to which they otherwise would not be exposed. Evaluations are obtained by electronic survey after each session and returned to the resident lecturer.
Table 5.
Format of Resident Teaching Conferences
| Weekly Educational Conferences [RAE Commitment time: 3 hours/week for 8 months] |
|---|
Conference 1 (30 min weekly):
|
Conference 2 (1 hour weekly):
|
6. Med Student Prep Course
In the spring, a resident co-directed course is offered to fourth year medical students who are planning to enter a surgical residency, as a pilot course using the ACS/APDS/ASE Resident Prep Curriculum15. The month long course focuses on necessary skills needed to function as a safe and efficient surgical intern. Resident leaders, in conjunction with a faculty member, spend time coordinating the schedule, developing the curriculum, giving lectures, and leading simulation sessions.
Operational Details
The education curriculum is run, organized, developed, and executed by residents. The Resident Education Committee (REC) is the group that holds ownership for allocating responsibility and promoting the culture of sustainability and includes all residents in research. Residents responsible for different modules are expected to attend, as this committee reviews each module and explores avenues for improvements each year (Figure 2). The ownership is divided among the non-clinical residents in research with some direction from the chief residents. The curriculum of each module is passed down each year with a focus on annual improvement and continuity. Two non-clinical research residents oversee each piece of the curriculum, with each team including a 1st year and 2nd year lab resident. This structure allows the experience, organization, and execution of the curriculum to be passed down from senior resident to junior resident each year for continuity. In addition, this organization promotes creativity, innovation, and rapid iteration, as new residents must take the lead each year, often suggesting and implementing changes in the module that they have themselves recently experienced.
Figure 2.
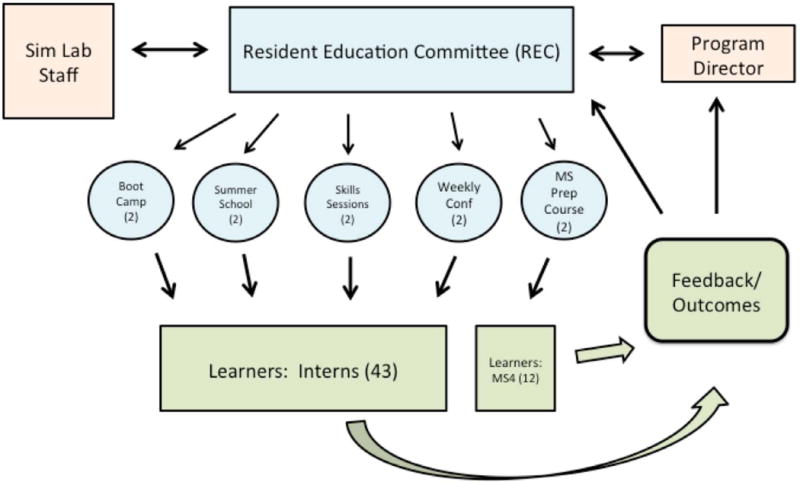
Organization of the stakeholders involved in the RAE model. The Resident Education Committee (REC) oversees the various teaching groups of two residents with associated feedback from the learners to the program director and education committee.
For an example of the advantage of this model in terms of incremental improvement, note the changes implemented yearly as demonstrated in Figure 3 as the residents rotated through leadership of the Intern Skills Sessions. This figure demonstrates how each resident pair started with an infrastructure and improved the system each year, avoiding stagnation. What is not shown is the added benefit that the resident educators return to the clinical stream as senior residents after RAE, remaining invested.
Figure 3.
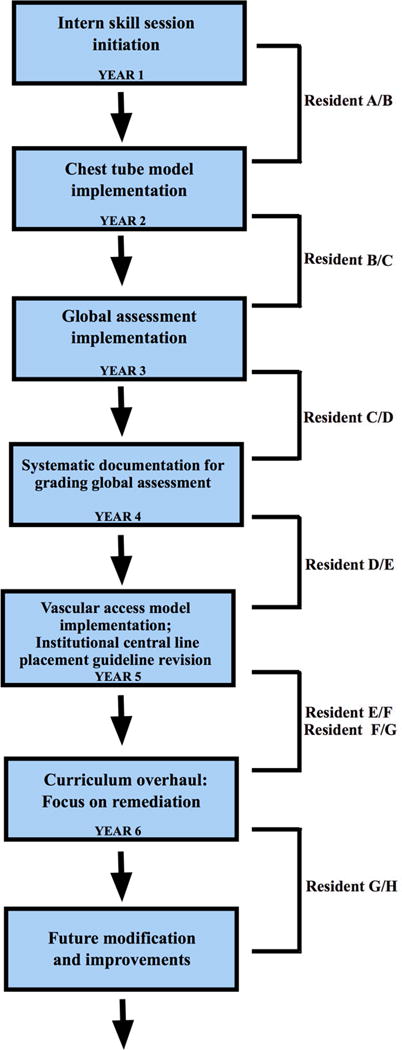
The intern surgical skill sessions have under gone several iterations since the curriculum was introduced. The education curriculum is re-evaluated and adjustments are made each year as a new resident team takes over responsibility. This process leads to innovation over time that improves the education environment for the learner.
The success of integrating the RAE model is largely based on establishing a strong culture dedicated to education by starting small, with invested residents, within the infrastructure of the residency program. However, there are formal efforts to develop residents as educators. First year residents in research who are involved in major components of RAE are expected (and supported) to attend the ACS sponsored Residents as Teachers and Leaders program. Since the beginning of RAE, three residents have entered the Surgical Education Research Fellowship (Association for Surgical Education). Additionally, residents are encouraged to participate locally in educator development programs sponsored by the Office of Health Sciences Education at Vanderbilt. As expected with any shift in culture, there was some initial resistance to change; however, sustainability quickly outweighed the disadvantages from both a resident development and faculty productivity perspective.
Implementing a RAE model requires oversight to ensure a high quality educational program. An associate program director or program director has always been primarily involved in oversight as a whole. Additionally, there is always an attending present at lectures given by residents. The faculty presence ensures both high quality content and appropriate feedback regarding teaching style and effectiveness of the resident lecture.
There are both formal and informal evaluations provided by residents as well. Electronic surveys are distributed at the end of each didactic (in the case of resident teaching conference) or at the end of each curriculum component (in the case of intern summer school or intern skills sessions).
Advantages and Disadvantages
An important byproduct of the RAE model is promoting a culture of education within the residency. Resident teaching demands that the instructor master the topic covered, and the adage that one learns best when he or she teaches is at the centerpiece of the philosophy behind the RAE model. Upper level surgical residents are often at the same training level as attendings in other specialties with shorter training requirements; therefore, early teaching should be part of any surgery resident’s academic development. Applicants during the interview season are now introduced to the fact that they are entering a program where teaching junior residents will be part of their expectations in an academic environment.
An important advantage for the learners is that, compared to attendings far removed from surgical training, residents are closer to the age and experience level of the learner. This increases the chance of “filling in the missing gaps” in educational development. Residents commit to this teaching model because the comprehensive education of junior residents ensures higher quality patient care for their teams in the future. In addition to teaching, upper-level residents play a large role in assessment of junior residents, honing the skills needed to provide appropriate feedback and constructive criticism. In fact, in a study of the assessment skills when residents and attendings assessed interns in our global assessment after intern skills session (consent, line placement, breaking bad news, chest tube placement), residents and attendings gave statistically similar scores using a checklist but residents gave significantly more critical feedback in some tasks to junior residents regarding their global skills such as economy of motion and handling of instruments (unpublished results, KT).
Finally, another important outcome is the professional development of residents involved in RAE. Educational research and publications have increased at this institution since the beginning of RAE, promoting professional development of resident educators. Since 2008, twenty publications16–35 focusing on education have been authored or co-authored by residents compared to only five publications36–40 prior to the implantation of the RAE curriculum. In addition, the emphasis on education within the surgery residency has resulted in multiple institutional teaching awards (from medical students as well as residents), and two national teaching awards, all given to residents heavily involved in the RAE curriculum.
It is difficult to quantify the opportunity cost of attending time; an hour less of lecture preparation or lecturing, for example, does not necessarily translate into an hour more of RUV-generating activities, clinic time, or available time for other clinical or research activities. However, the average amount of money a surgeon makes per hour can be used as a surrogate. According to the Medical Group Management Association 2013 report, the median total compensation for an academic general surgeon (>67% clinical activity) in the US is $299,40441. Assuming that a surgeon works 60 hours a week and 45 weeks per year, he or she makes $111 per hour. Faculty at Vanderbilt value resident education, but their involvement is not necessary or cost effective for many of the activities described above. Intern summer school, for example, is used to teach intern-level skills to incoming residents and requires a time commitment of 4 hours per week. Using average pay-per-hour, a faculty member would be compensated $444 a week for lecturing in summer school, a relatively low value activity relative to faculty skill level. Economic principles suggest that assets should be utilized at their highest-value; therefore, faculty should be compensated and utilized for activities like board preparation with senior residents, operative education, generating RVUs, and research productivity. Overall, residents spend 32 hours/year teaching intern summer school, 128 hours/year teaching intern skill sessions, 8 hours/year leading a trauma orientation, and 64 hours/year prepping for weekly discussions, for a total of 232 hours/year of activities that do not require attending instruction. Based on an average hourly rate of $111, utilizing residents as teachers saves $25,752/year.
Disadvantages include a perceived decreased quality of teaching; however, with appropriate faculty oversight, these potential shortcomings can be avoided. Another potential disadvantage of the RAE model is the added resident responsibilities and time commitment, potentially detracting from clinical duties. As previously stated, the major stakeholders each year at this institution are the non-clinical residents, mitigating this potential disadvantage. Also, as there is a framework in place from the year prior, much of the work is already complete and residents each year can focus on changes in which they are invested. Finally, there is worth in acquiring the time-management skills needed to balance these increased educational responsibilities, adding to the development of the future academic surgeon.
Conclusion
We present a potential education model for an academic surgery program to improve junior level curriculum, as well as promote mid-level residents in their professional development. In addition, RAE is aimed to improve the efficient use of faculty time. Even in academic surgery programs that have robust non-clinician educator support, allowing residents to be responsible for curriculum design and change (especially with oversight) may lead to a more applicable and adaptable educational program. Mid-level residents, many of whom would be at attending level in any other specialty, and many of whom enter residency with significant teaching experience, are already capable of designing sound educational programs. Ownership of the educational process allows residents to strive for improvement and sustainability while improving their own clinical knowledge by preparing lectures, honing teaching skills, learning to critically evaluate younger residents, and fostering career development. Improved resident interactions and camaraderie within the program as a whole are added benefits for both the learners and educators. Importantly, our model does not eliminate teaching by attending surgeons. The content is largely maintained at the faculty level while the best method to learn and teach for this generation of surgical trainees is overseen by resident educators.
Table 6.
Format of Medical Student Prep Course
| Medical Student Prep Course [Commitment time: 15–20 hours/week for 5 weeks] |
|---|
| 1. Didactic Lectures given by residents, attendings, and fellows |
2. Standardized patient scenarios
|
| 3. Cadaver lab training and basic surgical skill sessions |
Acknowledgments
Dr. Clark Kensinger received salary support from the Renal Biology and Disease Training Program grant: NIH/NIDDK 5T32DK007569. We would to graciously thank Dr. John Tarpley (JLT) and Mrs. Margaret Tarpley for providing information that contributed to the manuscript. In addition, we would like to thank Dr. Julia Shelton and Dr. Felicitas Koller for their contributions to the initial presentation of this material at the APDS annual conference in 2012.
Abbreviations
- ACGME
Accreditation Council for Graduate Medical Education
- ACLS
Advanced Cardiac Life Support
- APDS
Association for Program Directors in Surgery
- ATLS
Advanced Trauma Life Support
- ASE
Association of Surgical Education
- CXR
Chest x-ray
- MS
Medical student
- RAE
Resident as educator
- REC
Resident Education Committee
- RTC
Resident Teaching Conference
- RVUs
Relative value units
Contributor Information
Clark D. Kensinger, Email: clark.d.kensinger@vanderbilt.edu.
William G. McMaster, Email: william.g.mcmaster@Vanderbilt.Edu.
Michael A. Vella, Email: michael.a.vella@Vanderbilt.Edu.
Kevin W. Sexton, Email: kevin.sexton@vanderbilt.edu.
Rebecca A. Snyder, Email: rebecca.snyder@Vanderbilt.Edu.
Kyla P. Terhune, Email: kyla.terhune@Vanderbilt.Edu.
References
- 1.ACGME. Program Requirements for Graduate Medical Education in General Surgery. http://www.acgme.org/acgmeweb/Portals/0/PFAssets/ProgramRequirements/440_general_surgery_07012014.pdf. [Accessed 3/30/15]
- 2.Topping K. The effectiveness of peer tutoring in further and higher education: a typology and review of the literature. Higher Education. 1996;32:321–345. [Google Scholar]
- 3.Yu TC, Wilson NC, Singh PP, Lemanu DP, Hawken SJ, Hill AG. Medical students-as-teachers: a systematic review of peer-assisted teaching during medical school. Adv Med Educ Pract. 2011;2:157–172. doi: 10.2147/AMEP.S14383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schuller MC, DaRosa DA, Crandall ML. Using Just-in-Time Teaching and Peer Instruction in a Residency Program’s Core Curriculum: Enhancing Satisfaction, Engagement, and Retention. Acad Med. 2015 Mar;90(3):384–391. doi: 10.1097/ACM.0000000000000578. [DOI] [PubMed] [Google Scholar]
- 5.Crouch C, W J, Fagen A, Mazur E. Peer Instruction: Engaging Students One-on-One, All At Once. Research-Based Reform of University Physics. 2007;1 [Google Scholar]
- 6.Shelton JMA, Sexton K, Synder R, Koller F, Terhune K. Assocition for Program Directors in Surgery. San Diego, CA: 2012. Residents as Teachers? Get Serious. [Google Scholar]
- 7.Rotenberg BW, Woodhouse RA, Gilbart M, Hutchison CR. A needs assessment of surgical residents as teachers. Can J Surg. 2000 Aug;43(4):295–300. [PMC free article] [PubMed] [Google Scholar]
- 8.Dunnington GL, DaRosa D. A prospective randomized trial of a residents-as-teachers training program. Acad Med Jun. 1998;73(6):696–700. doi: 10.1097/00001888-199806000-00017. [DOI] [PubMed] [Google Scholar]
- 9.Soriano RP, Blatt B, Coplit L, et al. Teaching medical students how to teach: a national survey of students-as-teachers programs in U.S. medical schools. Acad Med. 2010 Nov;85(11):1725–1731. doi: 10.1097/ACM.0b013e3181f53273. [DOI] [PubMed] [Google Scholar]
- 10.Pasquinelli LM, Greenberg LW. A review of medical school programs that train medical students as teachers (MED-SATS) Teach Learn Med. 2008 Jan-Mar;20(1):73–81. doi: 10.1080/10401330701798337. [DOI] [PubMed] [Google Scholar]
- 11.Duran-Nelson A, Baum KD, Weber-Main AM, Menk J. Efficacy of peer-assisted learning across residencies for procedural training in dermatology. J Grad Med Educ. 2011 Sep;3(3):391–394. doi: 10.4300/JGME-D-10-00218.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dyc NG, Pena ME, Shemes SP, Rey JE, Szpunar SM, Fakih MG. The effect of resident peer-to-peer education on compliance with urinary catheter placement indications in the emergency department. Postgrad Med J. 2011 Dec;87(1034):814–818. doi: 10.1136/postgradmedj-2011-130287. [DOI] [PubMed] [Google Scholar]
- 13.Residents as Teachers and Leaders. American College of Surgeons; http://www.facs.org/education/division-of-education/courses/residentsas-teachers. [Accessed 3/30/2015] [Google Scholar]
- 14.http://www.ted.com/about/programs-initiatives/ted-talks. [Accessed: 3/30/15]
- 15.Residents as Teachers and Leaders. American College of Surgeons; http://www.facs.org/education/program/resident-prep. [Accessed 3/30/15] [Google Scholar]
- 16.Kensinger CD, Merrill WH, Geevarghese SK. Surgical Mentorship From Mentee to Mentor: Lessons From the Life of Alfred Blalock, MD. JAMA Surg. 2014 Dec 17; doi: 10.1001/jamasurg.2014.2068. [DOI] [PubMed] [Google Scholar]
- 17.Julien JS, Lang R, Brown TN, et al. Minority Underrepresentation in Academia: Factors Impacting Careers of Surgery Residents. J Racial Ethn Health Disparities. 2014 Dec 1;1(4):238–246. doi: 10.1007/s40615-014-0030-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Joshua Smith J, Patel RK, Chen X, Tarpley MJ, Terhune KP. Does intentional support of degree programs in general surgery residency affect research productivity or pursuit of academic surgery? J Surg Educ. 2014 Jul-Aug;71(4):486–491. doi: 10.1016/j.jsurg.2014.01.018. [DOI] [PubMed] [Google Scholar]
- 19.Yount KW, Reames BN, Kensinger CD, et al. Resident awareness of documentation requirements and reimbursement: a multi-institutional survey. Ann Thorac Surg. 2014 Mar;97(3):858–864. doi: 10.1016/j.athoracsur.2013.09.100. discussion 864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wall AE, Kodner IJ, Keune JD. Surgical research abroad. Surgery. 2013 May;153(5):723–726. doi: 10.1016/j.surg.2013.02.015. [DOI] [PubMed] [Google Scholar]
- 21.Wall AE. Benchmarks for international surgery. Arch Surg. 2012 Sep;147(9):796–797. doi: 10.1001/archsurg.2012.696. [DOI] [PubMed] [Google Scholar]
- 22.Alamanda VK, Crosby SN, Mathis SL, Archer KR, Terhune KP, Holt GE. Influence of resident education in correctly diagnosing extremity soft tissue sarcoma. Sarcoma. 2013;2013:679323. doi: 10.1155/2013/679323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nesbitt JC, St Julien J, Absi TS, et al. Tissue-based coronary surgery simulation: medical student deliberate practice can achieve equivalency to senior surgery residents. J Thorac Cardiovasc Surg. 2013 Jun;145(6):1453–1458. doi: 10.1016/j.jtcvs.2013.02.048. discussion 1458–1459. [DOI] [PubMed] [Google Scholar]
- 24.Axt J, Nthumba PM, Mwanzia K, et al. Commentary: The role of global surgery electives during residency training: relevance, realities, and regulations. Surgery. 2013 Mar;153(3):327–332. doi: 10.1016/j.surg.2012.09.014. [DOI] [PubMed] [Google Scholar]
- 25.Dageforde LA, Kibbe M, Jackson GP. Recruiting women to vascular surgery and other surgical specialties. J Vasc Surg. 2013 Jan;57(1):262–267. doi: 10.1016/j.jvs.2012.07.029. [DOI] [PubMed] [Google Scholar]
- 26.Snyder RA, Bills JL, Phillips SE, Tarpley MJ, Tarpley JL. Specific interventions to increase women’s interest in surgery. J Am Coll Surg. 2008 Dec;207(6):942–947. 947.e941–948. doi: 10.1016/j.jamcollsurg.2008.08.017. [DOI] [PubMed] [Google Scholar]
- 27.Snyder RA, Phillips SE, Terhune KP. Impact of implementation of a pediatric surgery fellowship on general surgery resident operative volume. J Surg Educ. 2012 Nov-Dec;69(6):753–758. doi: 10.1016/j.jsurg.2012.03.007. [DOI] [PubMed] [Google Scholar]
- 28.Snyder RA, Tarpley MJ, Tarpley JL, Davidson M, Brophy C, Dattilo JB. Teaching in the operating room: results of a national survey. J Surg Educ. 2012 Sep-Oct;69(5):643–649. doi: 10.1016/j.jsurg.2012.06.007. [DOI] [PubMed] [Google Scholar]
- 29.Sexton KW, Hocking KM, Wise E, et al. Women in academic surgery: the pipeline is busted. J Surg Educ. 2012 Jan-Feb;69(1):84–90. doi: 10.1016/j.jsurg.2011.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Poteet S, Tarpley M, Tarpley JL, Pearson AS. Veterans Affairs general surgery service: the last bastion of integrated specialty care. Am J Surg. 2011 Nov;202(5):507–510. doi: 10.1016/j.amjsurg.2011.06.015. [DOI] [PubMed] [Google Scholar]
- 31.Kauffmann RM, Landman MP, Shelton J, et al. The use of a multidisciplinary morbidity and mortality conference to incorporate ACGME general competencies. J Surg Educ. 2011 Jul-Aug;68(4):303–308. doi: 10.1016/j.jsurg.2011.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Landman MP, Shelton J, Kauffmann RM, Dattilo JB. Guidelines for maintaining a professional compass in the era of social networking. J Surg Educ. 2010 Nov-Dec;67(6):381–386. doi: 10.1016/j.jsurg.2010.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Terhune KP, Shelton J, Koller F. Surgical Intern Olympics: skills assessment. Med Educ. 2009 Nov;43(11):1104–1105. doi: 10.1111/j.1365-2923.2009.03482.x. [DOI] [PubMed] [Google Scholar]
- 34.Terhune KP, Zaydfudim V, Abumrad NN. International medical graduates in general surgery: increasing needs, decreasing numbers. J Am Coll Surg. 2010 Jun;210(6):990–996. doi: 10.1016/j.jamcollsurg.2010.02.021. [DOI] [PubMed] [Google Scholar]
- 35.Lomis KD, Carpenter RO, Miller BM. Moral distress in the third year of medical school; a descriptive review of student case reflections. Am J Surg. 2009 Jan;197(1):107–112. doi: 10.1016/j.amjsurg.2008.07.048. [DOI] [PubMed] [Google Scholar]
- 36.Carpenter RO, Spooner J, Arbogast PG, Tarpley JL, Griffin MR, Lomis KD. Work hours restrictions as an ethical dilemma for residents: a descriptive survey of violation types and frequency. Curr Surg. 2006 Nov-Dec;63(6):448–455. doi: 10.1016/j.cursur.2006.06.003. [DOI] [PubMed] [Google Scholar]
- 37.Carpenter RO, Austin MT, Tarpley JL, Griffin MR, Lomis KD. Work-hour restrictions as an ethical dilemma for residents. Am J Surg. 2006 Apr;191(4):527–532. doi: 10.1016/j.amjsurg.2006.01.002. [DOI] [PubMed] [Google Scholar]
- 38.Hutul OA, Carpenter RO, Tarpley JL, Lomis KD. Missed opportunities: a descriptive assessment of teaching and attitudes regarding communication skills in a surgical residency. Curr Surg. 2006 Nov-Dec;63(6):401–409. doi: 10.1016/j.cursur.2006.06.016. [DOI] [PubMed] [Google Scholar]
- 39.Poulose BK, Ray WA, Arbogast PG, et al. Resident work hour limits and patient safety. Ann Surg. 2005 Jun;241(6):847–856. doi: 10.1097/01.sla.0000164075.18748.38. discussion 856–860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Grogan EL, Stiles RA, France DJ, et al. The impact of aviation-based teamwork training on the attitudes of health-care professionals. J Am Coll Surg. 2004 Dec;199(6):843–848. doi: 10.1016/j.jamcollsurg.2004.08.021. [DOI] [PubMed] [Google Scholar]
- 41.Medical Group Management Association. http://www.mgma.com/industrydata/mgma-surveys-reports. [Accessed 3/30/15]


