Abstract
This study aimed to assess the frequency of Klebsiella pneumoniae in food samples and to detect antibiotic resistance phenotypes, antimicrobial resistance genes and the molecular subtypes of the recovered isolates. A total of 998 food samples were collected, and 99 (9.9%) K. pneumoniae strains were isolated; the frequencies were 8.2% (4/49) in fresh raw seafood, 13.8% (26/188) in fresh raw chicken, 11.4% (34/297) in frozen raw food and 7.5% (35/464) in cooked food samples. Antimicrobial resistance was observed against 16 antimicrobials. The highest resistance rate was observed for ampicillin (92.3%), followed by tetracycline (31.3%), trimethoprim-sulfamethoxazole (18.2%), and chloramphenicol (10.1%). Two K. pneumoniae strains were identified as extended-spectrum β-lactamase (ESBL)–one strain had three beta-lactamases genes (blaSHV, blaCTX-M-1, and blaCTX-M-10) and one had only the blaSHV gene. Nineteen multidrug-resistant (MDR) strains were detected; the percentage of MDR strains in fresh raw chicken samples was significantly higher than in other sample types (P<0.05). Six of the 18 trimethoprim-sulfamethoxazole-resistant strains carried the folate pathway inhibitor gene (dhfr). Four isolates were screened by PCR for quinolone resistance genes; aac(6’)-Ib-cr, qnrB, qnrA and qnrS were detected. In addition, gyrA gene mutations such as T247A (Ser83Ile), C248T (Ser83Phe), and A260C (Asp87Ala) and a parC C240T (Ser80Ile) mutation were identified. Five isolates were screened for aminoglycosides resistance genes; aacA4, aacC2, and aadA1 were detected. Pulsed-field gel electrophoresis-based subtyping identified 91 different patterns. Our results indicate that food, especially fresh raw chicken, is a reservoir of antimicrobial-resistant K. pneumoniae, and the potential health risks posed by such strains should not be underestimated. Our results demonstrated high prevalence, antibiotic resistance rate and genetic diversity of K. pneumoniae in food in China. Improved control and prevention strategies are urgently needed.
Introduction
Klebsiella pneumoniae is a common opportunistic pathogen that causes human infections. It can be widely distributed not only in the respiratory and intestinal tracts of humans and animals but also in a variety of environments and vectors. This pathogen can cause pneumonia, respiratory tract infections, urinary system infections, septicemia and other diseases [1,2]. Antimicrobials have been widely used to treat K. pneumoniae infections in humans. However, increasing antimicrobial resistance, especially that mediated by extended-spectrum β-lactamases (ESBL), plasmid-borne AmpCs, and carbapenemases, has been reported in recent years and has become a serious problem [3–5].
Foodborne diseases caused by pathogenic bacteria constitute a serious threat to public health worldwide [6,7]. Until now, most investigations on foodborne bacteria focused on common foodborne pathogens, such as Salmonella, Campylobacter, Escherichia coli, Shigella, Listeria monocytogenes, Staphylococcus aureus, and Vibrio parahaemolyticus. In contrast, little information was obtained on foodborne K. pneumoniae as K. pneumoniae is generally not recognized as a foodborne pathogen. However, antimicrobial-resistant K. pneumoniae strains have been isolated from marketed fresh vegetables [8], shrimp in international trade [9], and farm-raised chicken [10]. A recent report showed that foodborne K. pneumoniae could cause a nosocomial outbreak [11]. Furthermore, several resistance genes in K. pneumoniae are located in transferable genetic elements that may be transferred to other bacteria. Thus, the potential contribution of K. pneumoniae to the resistance of clinically relevant bacteria is cause for concern.
The presence of antimicrobial-resistant K. pneumoniae strains in the food supply is alarming. Our objective was to assess the frequency of K. pneumoniae in food samples. We focused on the contamination rate in foods and on the characteristics of K. pneumoniae isolates. We characterized their antimicrobial resistance phenotypes, identified their antimicrobial resistance genes and analyzed their molecular subtypes.
Materials and Methods
Sample collection
A total of 998 food samples were collected in Shijiazhuang, a city of approximately 10 million inhabitants in eastern China, between April 2013 and July 2014. Those samples were used to isolate K. pneumoniae strains. The samples included 49 fresh raw seafood (fish, shellfish, shrimp) samples, 188 fresh raw chicken samples, 297 frozen raw food (meat, vegetables, flour and rice products) samples and 464 cooked food samples (meat, vegetables, flour and rice products). These samples were collected from different farms, supermarkets and restaurants distributed throughout the city. None of the samples were duplicated.
Isolation and identification
A 25-g portion of each sample was suspended in 225 mL of buffered peptone water (BPW). The sample suspensions were incubated overnight at 36°C. A 1-mL aliquot of the pre-enrichment culture was added to 10 mL of selenite cystine broth (SC) and incubated overnight at 36°C. A loopful (10 μL) of SC was streaked directly onto Salmonella Shigella (SS) agar plates and incubated for 24 h at 36°C. Colorless, medium-sized, smooth and moist colonies were transferred to triple-sugar iron (TSI) agar plates. All the suspected K. pneumoniae isolates were identified using a BD Phoenix™-100 Automated Microbiology System (Becton, Dickinson and Company, Sparks, Maryland, USA).
Antimicrobial susceptibility testing
Antimicrobial susceptibility testing for the K. pneumoniae strains was performed using a BD Phoenix NMIC/ID-4 system according to the manufacturer’s instructions. The following 21 antimicrobials were tested: amikacin (AMI), gentamicin (GEN), imipenem (IPM), meropenem (MEM), cefazolin (CZO), ceftazidime (CAZ), cefotaxime (CTX), cefepime (FEP), aztreonam (ATM), ampicillin (AMP), piperacillin (PRL), amoxicillin-clavulanate (AMC), ampicillin-sulbactam (SAM), piperacillin-tazobactam (TZP), colistin (CL), trimethoprim-sulfamethoxazole (SXT), chloramphenicol (C), ciprofloxacin (CIP), levofloxacin (LVX), moxifloxacin (MXF), and tetracycline (TE). The minimum inhibitory concentrations (MICs) were interpreted by the standards of Clinical and Laboratory Standards Institute (CLSI) document M100-S24:2014 [12]. The presence of ESBLs was detected with the BD Phoneix NMIC/ID-4 test and was further confirmed by the double-disk diffusion method [12]. Escherichia coli strain ATCC 25922 and K. pneumoniae strain ATCC 700603 were used as quality-control strains for the antimicrobial susceptibility testing.
A standardized international definition was used to define multidrug-resistant (MDR) bacteria [13]. MDR was defined as acquired non-susceptibility to at least 1 agent in 3 or more antimicrobial categories.
PCR amplification and sequencing
Genomic DNA was extracted using a QIAamp DNA minikit (Qiagen, Dusseldorf, Germany) or prepared by the boiling method. Antimicrobial resistance-associated genes were detected by PCR and sequenced using the primers listed in Table 1. The PCR was performed in a 50-μL reaction volume that contained 25 μL of Premix Taq TM (Takara, Dalian, China), 10 μM of each primer and 1 μL of sample DNA. The PCR conditions for the β-lactamase genes consisted of an initial denaturation at 95°C for 5 min, 35 cycles of denaturation at 95°C for 50 s, annealing at 56°C, 50°C or 60°C for 40 s and elongation at 72°C for 1 min, followed by a final extension at 72°C for 5 min, in a thermocycler (Labcycler, Senso, Germany). The PCR conditions for other resistance genes consisted of an initial denaturation at 95°C for 5 min, 30 cycles of denaturation at 94°C for 1 min, annealing at 55°C for 1 min and elongation at 72°C for 2 min, followed by a final extension at 72°C for 5 min, in a thermocycler. The PCR products were detected in a 1% agarose gel. Positive amplicons were sequenced on a PE Applied Biosystems ABI Prism 3730 instrument. The DNA sequences were annotated using the BLAST program (http://blast.ncbi.nlm.nih.gov) to identify the gene subtypes. Mutations in the gyrA and parC sequences of K. pneumoniae (reference GenBank accession numbers DQ673325 and NC009648 for gyrA and parC, respectively) were detected.
Table 1. Primers Used for PCR Amplification and Resistance Gene Sequencing.
| Gene | Primer Sequence (5’→3’) | Annealing Temp (°C) | Fragment (bp) | Reference | |
|---|---|---|---|---|---|
| Forward | Reverse | ||||
| β - lactamase genes | |||||
| blaTEM | TCAACATTTCCGTGTCG | CTGACAGTTACCAATGCTTA | 56 | 860 | [14] |
| blaSHV | ATGCGTTATATTCGCCTGTG | AGATAAATCACCACAATGCGC | 56 | 896 | [14] |
| blaCTX-M-1 | CCGTTTCCGCTATTACAAACCG | GGCCCATGGTTAAAAAATCACTGC | 56 | 944 | [15] |
| blaCTX-M-2 | ATGATGACTCACAGCATTCG | TCCCGACGGCTTTCCGCGTT | 56 | 833 | [16] |
| blaCTX-M-8 | TTTGCCCGTGCGATTGG | CGACTTTCTGCCTTCTGCTCT | 50 | 368 | [17] |
| blaCTX-M-9 | ATGGTGACAAAGAGAGTGCA | CCCTTCGGCGATGATTCTC | 50 | 870 | [18] |
| blaCTX-M-10 | GCAGCACCAGTAAAGTGATGG | GCGATATCGTTGGTGGTACC | 56 | 524 | [19] |
| blaCTX-M-14 | GAGAGTGCAACGGATGATG | TGCGGCTGGGTAAAATAG | 56 | 941 | [20] |
| AmpC genes | |||||
| baCMY-G1 | GCTGACAGCCTCTTTCTCCAC | CCTCGACACGGRCAGGGTTA | 56 | 1082 | [21] |
| baCMY-G2 | GGTCTGGCCCATGCAGGTGA | GGTCGAGCCGGTCTTGTTGA | 56 | 963 | [21] |
| blaDHA | AACTTTCACAGGTGTGCTGGGT | CCGTACGCATACTGGCTTTGC | 60 | 405 | [22] |
| blaACT | ATTCGTATGCTGGATCTCGCCACC | CATGACCCAGTTCGCCATATCCTG | 50 | 396 | [23] |
| blaFOX | CACCACGAGAATAACC | GCCTTGAACTCGACCG | 50 | 1184 | [23] |
| Folate pathway inhibitors | |||||
| dhfr | GCCAATCGGGTTATTGGCAA | TGGGAAGAAGGCGTCACCCTC | 55 | 357 | [24] |
| Fluoroquinolone resistance-associated genes | |||||
| qnrA | ATTTCTCACGCCAGGATTTG | GATCGGCAAAGGTTAGGTCA | 55 | 627 | [25] |
| qnrB | GATCGTGAAAGCCAGAAAGG | ACGATGCCTGGTAGTTGTCC | 55 | 469 | [25] |
| qnrC | GGGTTGTACATTTATTGAATCG | CACCTACCCATTTATTTTCA | 55 | 307 | [26] |
| qnrD | CGAGATCAATTTACGGGGAATA | AACAAGCTGAAGCGCCTG | 55 | 533 | [27] |
| qnrS | ACGACATTCGTCAACTGCAA | TAAATTGGCACCCTGTAGGC | 55 | 417 | [28] |
| aac(6’)-Ib-cr | TTGCGATGCTCTATGAGTGGCTA | CTCGAATGCCTGGCGTGTTT | 55 | 482 | [29] |
| qepA | AACTGCTTGAGCCCGTAGAT | GTCTACGCCATGGACCTCAC | 55 | 596 | [26] |
| gyrA | CGACCTTGCGAGAGAAAT | GTTCCATCAGCCCTTCAA | 55 | 626 | [30] |
| parC | TACGTCATCATGGACAGG | GCCACTTCACGCAGGTTG | 55 | 460 | [31] |
| Aminoglycoside resistance-associated genes | |||||
| aacA4 | ATGACTGA CATGACCTTGCG | TTAGGCATCACTGCGTGTTCG | 55 | 540 | [32] |
| aacC1 | ATGGGCATCATTCGCACATGTAGG | TTAGGTGGCGGTACTTGGGTC | 55 | 873 | [32] |
| aacC2 | ATGCATACGCGGAAGGCAATAAC | CTAACCGGAAGGCTCGCAAG | 55 | 861 | [32] |
| aadA1 | ATGAGGGAAGCGGTGATCG | TTATTTGCCGACTACCTTGGTG | 55 | 792 | [32] |
| aadB | ATGGACACAACGCAGGTCGC | TTAGGCCGCATATCGCGACC | 55 | 534 | [32] |
| aphA6 | ATGGAATTGCCCAATATTATTC | TCAATTCAATTCATCAAGTTTTA | 55 | 781 | [32] |
| armA | AGGTTGTTTCCATTTCTGAG | TCTCTTCATTCCCTTCTCC | 55 | 591 | [33] |
| rmtB | CCCAAACAGACCGTAGAGGC | CTCAAACTCGGCGGGCAAGC | 55 | 585 | [33] |
| Integron I | GGCATCCAAGCACAAG | AAGCAGACTTGACCTGA | 55 | Variable | [34] |
Pulsed-field gel electrophoresis (PFGE)
We used the 1-day, standardized PFGE protocol for K. pneumoniae [35]. Cell suspensions were placed in polystyrene tubes (Falcon; 12 × 75 mm), and their optical densities were adjusted to 3.8–4.0 using a Densimat photometer (BioMérieux, Marcy l’Etoile, France). Slices of K. pneumoniae agarose plugs were digested using 50 U of XbaI (Takara) per slice for 4 h at 37°C, and electrophoresis was performed using a CHEF-DRIII system (Bio-Rad Laboratories, Hercules, CA, USA). Electrophoresis was conducted with a switch time of 6 s to 36 s for 18.5 h, and images were captured using a Gel Doc 2000 system (Bio-Rad) and converted to TIFF files. The TIFF files were analyzed using BioNumerics version 5.1 software (Applied Maths, Kortrijk, Belgium). A similarity analysis of the PFGE patterns was performed by calculating the Dice coefficients (SD) [36] and clustering was performed using the unweighted-pair group method with average linkages (UPGMA).
Multilocus sequence typing (MLST)
MLST with 7 genes (gapA, infB, mdh, pgi, phoE, rpoB and tonB) was performed on the isolates as previously described [37]. Alleles and sequence types (STs) were assigned using the K. pneumoniae MLST database (http://bigsdb.web.pasteur.fr/klebsiella/klebsiella.html).
Statistical analysis
SPSS software (version 15.0) was used to statistically analyze the data. Categorical variables were compared using the Fisher’s exact test. A P value <0.05 was considered to be statistically significant.
Results
Contamination rate of food samples with K. pneumoniae
In total, 998 food samples were tested in this study, and K. pneumoniae was cultured from 99 of those samples. Overall, 9.9% of the food samples were positive for K. pneumoniae. K. pneumoniae was cultured from 8.2% (4/49) of the fresh raw seafood samples, 13.8% (26/188) of the fresh raw chicken samples, 11.4% (34/297) of the frozen raw food samples and 7.5% (35/464) of the cooked food samples. The rates of K. pneumoniae isolation among sample types were significantly different (Fisher’s exact test, P<0.05). In total, 31, 33, and 35 strains were isolated from the food raw materials, processing, and marketing sectors, respectively.
Antimicrobial susceptibility patterns of the K. pneumoniae isolates
Antimicrobial susceptibility testing was conducted for the 99 K. pneumoniae isolates, and detailed information on the resistance rates to all of the tested antimicrobials is listed in Table 2. The highest resistance rate was observed for AMP, which reached 92.3% (n = 92), followed by resistance to TE (n = 31; 31.3%), SXT (n = 18; 18.2%), C (n = 10; 10.1%), and 12 other antimicrobials with resistance rates under 10.0%. There was no resistance noted to carbapenems (IPM, MEM). Notably, the resistances to 7 antimicrobials (GEN, CTX, FEP, ATM, SAM, CIP, or LVX) were detected only among fresh raw chicken isolates. Furthermore, the rate of resistance to 5 antimicrobials (CZO, PRL, SXT, C and TE) in fresh raw chicken isolates was significantly higher than in isolates from other types of samples (P<0.05). Two K. pneumoniae strains were detected as ESBL-producing; both were from fresh raw chicken samples.
Table 2. Antimicrobial Resistance Rates of 99 K. pneumoniae Isolates.
| Antimicrobial category | Antimicrobial | Range (μg/mL) | susceptible MIC | Intermediate MIC | Resistant MIC | Raw seafood isolates (n = 4) | Raw chicken isolates (n = 26) | Frozen raw food isolates (n = 34) | Cooked food isolates (n = 35) | Total |
|---|---|---|---|---|---|---|---|---|---|---|
| R (%) | R (%) | R (%) | R (%) | R (%) | ||||||
| Aminoglycosides | Amikacin | 8–32 | ≤8 | ≥32 | 0 | 0 | 0 | 0 | 0 | |
| Gentamicin | 2–8 | ≤2 | 4 | >8 | 0 | 5 (19.2%) | 0 | 0 | 5 (5.1%) | |
| Carbapenems | Imipenem | 1–8 | ≤8 | >8 | 0 | 0 | 0 | 0 | 0 | |
| Meropenem | 1–8 | ≤8 | >8 | 0 | 0 | 0 | 0 | 0 | ||
| 1st-generation cephalosporins | Cefazolin | 4–16 | ≤4 | 16 | >16 | 0 | 2 (7.7%) | 2 (5.9%) | 0 | 4 (4.0%) |
| 3rd- and 4th-generation cephalosporins | Ceftazidime | 1–16 | ≤1 | 2 | >16 | 0 | 0 | 0 | 0 | 0 |
| Cefotaxime | 1–32 | ≤1 | 2 | >32 | 0 | 1 (3.8%) | 0 | 0 | 1 (1.0%) | |
| Cefepime | 2–16 | ≤2 | >16 | 0 | 1 (3.8%) | 0 | 0 | 1 (1.0%) | ||
| Monobactams | Aztreonam | 2–16 | ≤2 | 16 | >16 | 0 | 0 | 0 | 0 | 0 |
| Penicillins | Ampicillin | 4–16 | ≤4–8 | 16 | >16 | 4 (100%) | 25 (96.2%) | 31 (91.2%) | 32 (91.4%) | 92 (92.9%) |
| Piperacillin | 4–64 | ≤4–16 | 32 | >64 | 0 | 3 (11.5%) | 0 | 1 (2.9%) | 4 (4.0%) | |
| Antipseudomonal penicillins+β-lactamase inhibitors | Amoxicillin-Clavulanate | 4/2-16/8 | ≤4/2-8/4 | 16/8 | >16/8 | 0 | 2 (7.7%) | 1 (2.9%) | 0 | 3 (3.0%) |
| Ampicillin-Sulbactam | 4/2-16/8 | ≤4/2-8/4 | 16/8 | >16/8 | 0 | 4(21.4%) | 0 | 0 | 4 (4.0%) | |
| Piperacillin-Tazobactam | 4/4-64/4 | ≤4/4 | 8/4-16/4 | >64/4 | 0 | 0 | 0 | 0 | 0 | |
| Others | Colistin | 0.5–2 | ≤0.5 | 1 | >2 | 0 | 0 | 0 | 0 | 0 |
| Folate pathway inhibitors | Trimethoprim-Sulfamethoxazole | 0.5/9.5-2/38 | ≤0.5/9.5 | 1/19 | >2/38 | 0 | 13 (50.0%) | 2 (5.9%) | 3 (8.6%) | 18 (18.2%) |
| Chloramphenicols | Chloramphenicol | 4–16 | ≤4 | 8–16 | >16 | 0 | 8 (30.8%) | 1 (2.9%) | 1 (2.9%) | 10 (10.1%) |
| Fluoroquinolones | Ciprofloxacin | 0.5–2 | ≤0.5–1 | 2 | >2 | 0 | 6 (23.1%) | 0 | 0 | 6 (5.9%) |
| Levofloxacin | 1–8 | ≤1 | >8 | 0 | 3 (11.5%) | 0 | 0 | 3 (3.0%) | ||
| Moxifloxacin | 1–4 | ≤1 | 2–4 | >4 | 0 | 0 | 0 | 0 | 0 | |
| Tetracycline antibiotics | Tetracycline | 2–8 | ≤2 | >8 | 0 | 21 (80.8%) | 4 (11.8%) | 6 (17.1%) | 31 (31.3%) |
Nineteen MDR strains were detected among 99 K. pneumoniae isolates. The proportions of MDR strains in different samples were 50.0% (14/28), 11.4% (4/35), 2.9% (1/34) and 0% (0/4), in fresh raw chicken, cooked food samples, frozen raw food and fresh raw seafood, respectively. The proportion of MDR isolates from fresh raw chicken samples was significantly higher than that from other types of samples (P<0.05).
Antimicrobial resistance determinants of the K. pneumoniae isolates
According to the results of antimicrobial susceptibility testing, 2, 16, 4 and 5 strains were selected to analyze ESBL genes, folate pathway inhibitor genes, fluoroquinolone resistance genes and aminoglycoside resistance genes, respectively. For the 2 ESBL strains, 8 β-lactamase genes and 5 AmpC genes were amplified. As shown in Table 3, 1 strain carried blaSHV, blaCTX-M-1 and blaCTX-M-10, and the other carried blaSHV. No blaCTX-M-9, blaCTX-M-14, blaDHA, blaTEM, baCMY, blaACT, or blaFOX genes were detected in these isolates.
Table 3. Characteristics of the 2 ESBL-Producing K. pneumoniae Isolates Detected in this Study.
| Strain ID | Antimicrobial resistance patterns a | ESBL genes | MLST type |
|---|---|---|---|
| SJZ2013N33 | GEN-CZO-CAZ-CTX-FEP-ATM-AMP-PRL-AMC-SAM-SXT-C-TE | SHV, CTX-M-1, CTX-M-10 | 1651 |
| SJZ2013N75 | GEN-CZO-CAZ-CTX-FEP-ATM-AMP-PRL-AMC-SAM-SXT-C-TE | SHV | 1652 |
a Abbreviations of antimicrobials: AMI, amikacin; GEN, gentamicin; IPM, imipenem; MEM, meropenem; CZO, cefazolin; CAZ, ceftazidime; CTX, cefotaxime; FEP, cefepime; ATM, aztreonam; AMP, ampicillin; PRL, piperacillin; AMC, amoxicillin-clavulanate; SAM, ampicillin-sulbactam; TZP, piperacillin-tazobactam; CL, colistin; SXT, trimethoprim-sulfamethoxazole; C, chloramphenicol; CIP, ciprofloxacin; LVX, levofloxacin; MXF, moxifloxacin; TE, tetracycline.
Eighteen isolates that showed trimethoprim-sulfamethoxazole resistance were selected for folate pathway inhibitor gene (dhfr) testing; 6 of the isolates were positive for dhfr. All of the 6 dhfr-positive isolates were isolated from fresh raw chicken, whereas no isolates from frozen raw food or cooked food samples tested were positive for dhfr.
Four isolates were tested for fluoroquinolone resistance determinants. Among the 7 plasmid-encoded fluoroquinolone resistance-associated genes analyzed in this study, namely qnrA, qnrB, qnrC, qnrD, qnrS, aac(6’)-Ib-cr, and qepA, 4 genes were detected (Table 4). Among the 4 tested isolates, aac(6’)-Ib-cr, qnrB, qnrA and qnrS were detected in 4, 2, 1 and 1 isolate(s), respectively. In addition, gyrA gene mutations, such as T247A (Ser83Ile; two isolates), C248T (Ser83Phe; one isolate), and A260C (Asp87Ala; one isolate), and the parC gene mutation C240T (Ser80Ile; one isolate), were identified.
Table 4. Characteristics of the Fluoroquinolone Resistance-Associated Genes in 4 Fluoroquinolone-Resistant or Intermediately Fluoroquinolone-Resistant K. pneumoniae Isolates Detected in this Study.
| Strain ID | Antimicrobial resistance patterns b | Fluoroquinolone resistance-associated genes | gyrA mutation |
|---|---|---|---|
| SJZ2013N75 a | GEN-CZO-CAZ-CTX-FEP-ATM-AMP-PRL-AMC-SAM-SXT-C-TE | qnrB, aac(6’)-Ib-cr | |
| SJZ2013N28 | AMP-PRL-SXT-C-CIP-TE | qnrB, aac(6’)-Ib-cr | |
| SJZ2013N70 | GEN-AMP-SAM-SXT-C-CIP-LVX-TE | qnrS, aac(6’)-Ib-cr | T247A (Ser83Ile) |
| SJZ2013N7 | GEN-AMP-SAM-C-CIP-LVX-TE | qnrA, aac(6’)-Ib-cr |
a SJZ2013N75 showed intermediate resistance to CIP.
b Abbreviations of antimicrobials: AMI, amikacin; GEN, gentamicin; IPM, imipenem; MEM, meropenem; CZO, cefazolin; CAZ, ceftazidime; CTX, cefotaxime; FEP, cefepime; ATM, aztreonam; AMP, ampicillin; PRL, piperacillin; AMC, amoxicillin-clavulanate; SAM, ampicillin-sulbactam; TZP, piperacillin-tazobactam; CL, colistin; SXT, trimethoprim-sulfamethoxazole; C, chloramphenicol; CIP, ciprofloxacin; LVX, levofloxacin; MXF, moxifloxacin; TE, tetracycline.
Among the aminoglycoside resistance-associated genes, the aacA4, aacC2, aadA1 genes were detected in 4, 3 and 1 isolate(s), respectively (Table 5). No aacC1, aadB, aphA6, armA, rmtB or Integron I genes were detected in this study. Among the 5 tested isolates, 3 isolates carried both aacA4 and aacC2; 1 isolate carried both aacA4 and aadA1, and 1 isolate carried none of these genes.
Table 5. Characteristics of the Aminoglycoside Resistance-Associated Genes in 5 Gentamicin-Resistant or Intermediately Gentamicin-Resistant K. pneumoniae Isolates Detected in this Study.
| Strain ID | Antimicrobial resistance patterns a | aminoglycoside resistance-associated genes |
|---|---|---|
| SJZ2013N33 | GEN-CZO-CAZ-CTX-FEP-ATM-AMP-PRL-AMC-SAM-SXT-C-TE | aacA4, aacC2 |
| SJZ2013N75 | GEN-CZO-CAZ-CTX-FEP-ATM-AMP-PRL-AMC-SAM-SXT-C-TE | aacA4, aacC2 |
| SJZ2013N70 | GEN-AMP-SAM-SXT-C-CIP-LVX-TE | aacA4, aadA1 |
| SJZ2013N7 | GEN-AMP-SAM-C-CIP-LVX-TE | aacA4, aacC2 |
| SJZ2013N4 | GEN-AMP-C |
a Abbreviations of antimicrobials: AMI, amikacin; GEN, gentamicin; IPM, imipenem; MEM, meropenem; CZO, cefazolin; CAZ, ceftazidime; CTX, cefotaxime; FEP, cefepime; ATM, aztreonam; AMP, ampicillin; PRL, piperacillin; AMC, amoxicillin-clavulanate; SAM, ampicillin-sulbactam; TZP, piperacillin-tazobactam; CL, colistin; SXT, trimethoprim-sulfamethoxazole; C, chloramphenicol; CIP, ciprofloxacin; LVX, levofloxacin; MXF, moxifloxacin; TE, tetracycline.
PFGE and MLST analysis of K. pneumoniae isolates
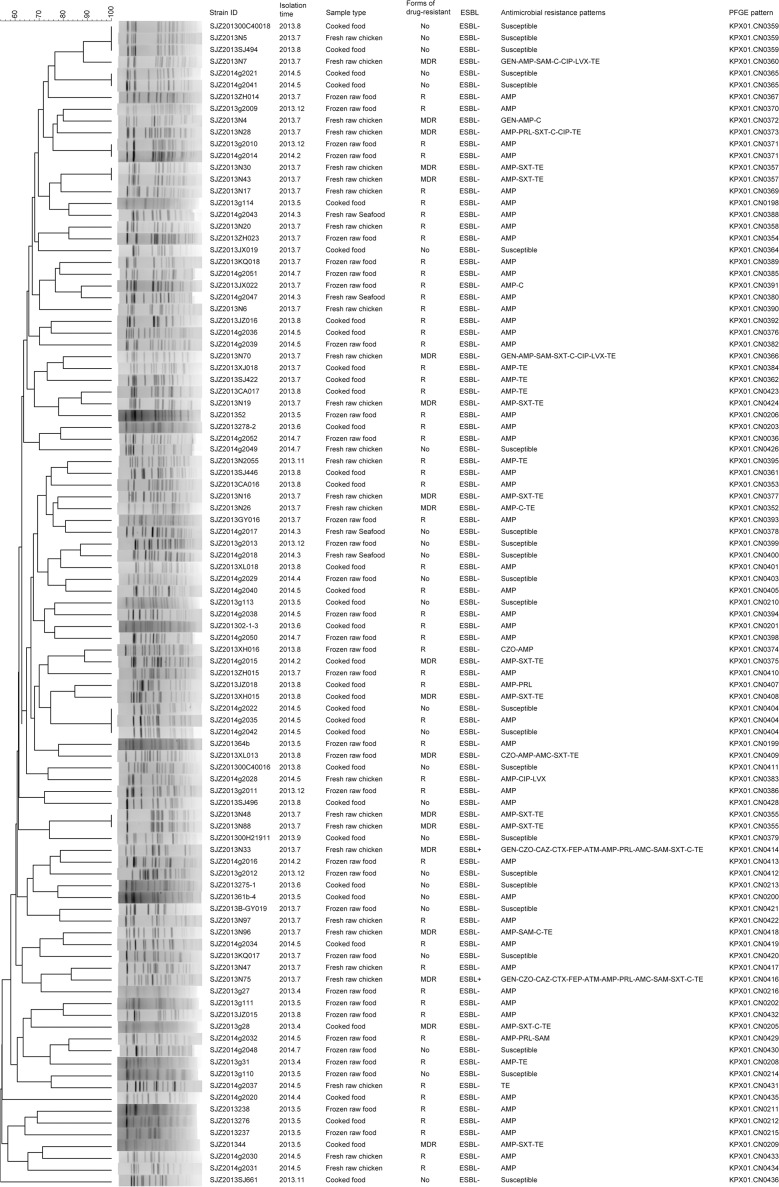
All the 99 isolates of K. pneumoniae were analyzed by PFGE, and 91 different PFGE patterns were obtained, with similarity values of 47.1% (Fig 1). Eighty-five (85.9%) isolates showed unique PFGE patterns. No dominant pattern was identified among these isolates. Only 6 patterns included more than 1 isolate. Two isolates of KPX01.CN0357 were isolated from fresh raw chicken samples collected from the same market at the same time; 3 isolates of KPX01.CN0404 were isolated from cooked food samples collected from the same restaurant at the same time; 2 isolates of KPX01.CN0365 were isolated from cooked food samples collected from different restaurants at the same time; and 2 isolates of KPX01.CN0355 were isolated from fresh raw chicken samples collected from different markets at the same time.
Fig 1. Clustering of the 99 K. pneumoniae Isolates Based on PFGE Patterns.
The strain ID, isolation time, sample type, forms of drug-resistant, ESBL detection, antimicrobial resistance pattern, and PFGE pattern of each isolate are listed to the left of the patterns. In the column of “forms of drug-resistant”, “No” means not resistant to all drugs, “R” means non-susceptibility to at least 1 agent in one or two antimicrobial categories, “MDR” means non-susceptibility to at least 1 agent in 3 or more antimicrobial categories.
The 2 ESBL-producing isolates showed different PFGE patterns. An MLST analysis of these 2 isolates produced two unique STs (ST1651, ST1652; Table 3); neither has been previously reported.
Discussion
Foodborne bacteria are widely studied, but research on K. pneumoniae is scarce. In a previous survey conducted in the United States, 53 (16.1%) MDR K. pneumoniae strains were isolated from 330 farm-raised frozen shrimp that were imported from Thailand to the United States [9]. In another survey focusing on fresh vegetables in Spain, 9 K. pneumoniae strains were obtained from 160 vegetables, among which 1 (0.6%) was an MDR strain [8]. The major goal of this study was to evaluate the current frequency and antimicrobial resistance of K. pneumoniae strains in fresh raw seafood, fresh raw chicken, frozen raw food and cooked food samples in China. The incidence of K. pneumoniae in these samples was 9.9%, which shows that contamination of food with K. pneumoniae is common in this region of China. Furthermore, 19 (1.9%) MDR K. pneumoniae strains were isolated in this study, representing a lower percentage than that reported by Nawaz et al. [9] but a higher percentage than that reported by Falomir et al. [8].
The highest isolation rates for K. pneumoniae and MDR K. pneumoniae strains in this study were observed for fresh raw chicken samples. Fresh raw chicken is an important reservoir of antimicrobial-resistant K. pneumoniae. A recent study focused on retail raw chicken demonstrated that β-lactamases and ESBLs were emerging and prevalent in foodborne Salmonella in China [38]. Profitable chicken farms demand the extensive usage of antimicrobials to inhibit infectious diseases. However, the use of antimicrobials in these ecosystems may select for antimicrobial-resistant microorganisms. Hence, chicken meat may be a reservoir of antimicrobial-resistant bacteria such as K. pneumoniae, which constitutes a public health concern.
The resistance mechanisms of K. pneumoniae include the production of β-lactamases (including ESBLs and plasmid-mediated AmpCs) and carbapenemases, the production of biological membrane formation factors, the loss of outer membrane proteins, and antimicrobial efflux [39–41]. In this study, we investigated a total of 99 K. pneumoniae isolates from food; 4 strains were ESBL, and 1 strain produced an AmpC beta-lactamase. ESBL-producing K. pneumoniae strains have been shown to have a significant impact on the treatment options and clinical outcomes of patients. Likewise, they have been shown to cause higher morbidity and mortality [42–44]. Currently, ESBLs and AmpCs are the predominant β-lactamases that mediate Gram-negative bacterial resistance to new broad-spectrum β-lactam antimicrobials. ESBLs are mainly encoded by plasmids, whereas AmpCs are mainly encoded on the chromosome. The CTX-M type is the major phenotype of domestic ESBLs; it reportedly predominates worldwide, followed by the SHV type [45–47]. Recently, Enterobacteriaceae carrying blaCTX-M-type genes were isolated from chicken in several countries [38, 48–50]. In this study, both ESBL-producing K. pneumoniae strains carried the blaSHV gene, and one strain carried blaCTX-M genes. One strain isolated in this study carried at least 4 ESBL-associated genes, i.e., coexisting blaCTX-M-1, blaCTX-M-10, and blaSHV. The coexistence of multiple blaCTX-M-type genes in K. pneumoniae isolates was also reported in previous studies [51,52]. The detection of ESBL-producing strains and the coexistence of several ESBL-associated genes in the same isolates pose a serious epidemiological, clinical and public health threat.
Quinolones are broad-spectrum antimicrobial agents that have been widely used in clinical medicine and for raising food-producing animals (such as chicken in China). The isolation and characterization of ciprofloxacin- and levofloxacin-resistant K. pneumoniae from fresh raw chicken samples is corresponding to that fluoroquinolones have been used in chicken farms. Among the 7 plasmid-encoded fluoroquinolone resistance-associated genes, the aac(6’)-Ib-cr enzyme, qnrB, qnrA, and qnrS were the most prevalent plasmid-mediated mechanisms of quinolone resistance, as previously reported [29]. Several studies have suggested that, in K. pneumoniae, DNA gyrase A is a primary target of quinolones and that parC alterations play a complementary role in the development of higher-level fluoroquinolone resistance [30,53]. In contrast, one study reported that hypermutation in K. pneumoniae is uncommon and does not contribute to the accumulation of gyrA mutations or directly to ciprofloxacin resistance [54]. Sequence analysis of the gyrA gene in K. pneumoniae isolates from fresh raw chicken in this study identified 3 types of gyrA mutations (encoding Ser83Ile, Ser83Phe, and Asp87Ala substitutions) and 1 type of parC mutation (encoding Ser80Ile). These point mutations were previously reported in clinical K. pneumoniae cases and may be responsible for mediating resistance to fluoroquinolones [9,51,53,55]. The amino acid substitutions at positions 83 (Ser to Phe) and 80 (Ser to Ile) in gyrase A resemble a substitution that confers fluoroquinolone resistance in Salmonella spp. [56,57]. Among the aminoglycosides resistance-associated genes, the aacA4, aacC2, and aadA1 genes were detected in this study. These 3 genes were the major aminoglycosides resistance genes among clinical K. pneumoniae cases reported at a hospital in China [51], which suggests that the resistance genes in clinical strains may come from foodborne strains.
PFGE is a useful tool to reveal genotypic characteristics and to trace the reservoirs of infectious pathogens, the rates of transmission and the mechanisms of infectious diseases. The variety of different PFGE strain patterns in this study was unexpected. Except for 6 groups of isolates that had identical PFGE patterns, all other isolates showed unique PFGE patterns. Furthermore, the 2 ESBL-producing isolates showed different PFGE patterns and MLST types. These results reflected a high genetic diversity of foodborne K. pneumoniae isolates.
There were three limitations of this study. Firstly, this study had not included agricultural antimicrobial use data from the regions which supplied food to the farms, supermarkets, and restaurants from where we sampled food items. The second one was that not compared these foodborne K. pneumoniae isolates to clinical isolates from the same region. Furthermore, the use of agar SC and SS would underestimate the frequency of K. pneumoniae isolated, because these two seletive medium are designed to inhibit other microorganisms than Salmonella spp. and Shigella spp.
In conclusion, our results indicate that food, especially fresh raw chicken, is a reservoir of antimicrobial-resistant K. pneumoniae. They may have the potential to become a public health risk. Thus, our study demonstrates that improved monitoring and prevention strategies are urgently needed to better control the emergence and transmission of antimicrobial-resistant K. pneumoniae isolates.
Data Availability
All relevant data are within the paper.
Funding Statement
This work was supported by 2012ZX10004215, 2008ZX10004-008 from National Health and Family Planning Commission of the People's Republic of China (http://www.nhfpc.gov.cn/). HZ received the funding. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Podschun R, Ullmann U. Klebsiella spp. as nosocomial pathogens: epidemiology, taxonomy, typing methods, and pathogenicity factors. Clin. Microbiol Rev. 1998;11: 589–603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Struve C, Krogfelt KA. Pathogenic potential of environmental Klebsiella pneumoniae isolates. Environ Microbiol. 2004;6: 584–590. 10.1111/j.1462-2920.2004.00590.x [DOI] [PubMed] [Google Scholar]
- 3.Marchaim D, Navon-Venezia S, Schwaber MJ, Carmeli Y. Isolation of imipenem-resistant Enterobacter species: emergence of KPC-2 carbapenemase, molecular characterization, epidemiology, and outcomes. Antimicrob Agents Chemother. 2008;52: 1413–1418. 10.1128/AAC.01103-07 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pfeifer Y, Cullik A, Witte W. Resistance to cephalosporins and carbapenems in Gram-negative bacterial pathogens. Int J Med Microbiol. 2010;300: 371–379. 10.1016/j.ijmm.2010.04.005 [DOI] [PubMed] [Google Scholar]
- 5.Yang J, Luo Y, Cui S, Wang W, Han L. Diverse phenotypic and genotypic characterization among clinical Klebsiella pneumoniae and Escherichia coli isolates carrying plasmid-mediated quinolone resistance determinants. Microb Drug Resist. 2011;17: 363–367. 10.1089/mdr.2011.0034 [DOI] [PubMed] [Google Scholar]
- 6.Kuchenmüller T, Abela-Ridder B, Corrigan T, Tritscher A. World Health Organization initiative to estimate the global burden of foodborne diseases. Rev Sci Tech. 2013;32: 459–467. [DOI] [PubMed] [Google Scholar]
- 7.McLinden T, Sargeant JM, Thomas MK, Papadopoulos A, Fazil A. Component costs of foodborne illness: a scoping review. BMC Public Health. 2014;14: 509 10.1186/1471-2458-14-509 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Falomir MP, Rico H, Gozalbo D. Enterobacter and Klebsiella species isolated from fresh vegetables marketed in Valencia (Spain) and their clinically relevant resistances to chemotherapeutic agents. Foodborne Pathog Dis. 2013;10: 1002–1007. 10.1089/fpd.2013.1552 [DOI] [PubMed] [Google Scholar]
- 9.Nawaz M, Khan SA, Tran Q, Sung K, Khan AA, Adamu I, et al. Isolation and characterization of multidrug-resistant klebsiella spp. Isolated from shrimp imported from Thailand. Int J Food Microbiol. 2012;155: 179–184. 10.1016/j.ijfoodmicro.2012.02.002 [DOI] [PubMed] [Google Scholar]
- 10.Wu H, Liu BG, Liu JH, Pan YS, Yuan L, Hu GZ. Phenotypic and molecular characterization of CTX-M-14 extended-spectrum β-lactamase and plasmid-mediated act-like AmpC β-lactamase produced by Klebsiella pneumoniae isolates from chickens in Henan Province, China. Genet Mol Res. 2012;11: 3357–3364. 10.4238/2012.September.24.1 [DOI] [PubMed] [Google Scholar]
- 11.Calbo E, Freixas N, Xercavins M, Riera M, Nicolás C, Monistrol O, et al. Foodborne nosocomial outbreak of SHV1 and CTX-M-15-producing Klebsiella pneumoniae: epidemiology and control. Clin Infect Dis. 2011;52: 743–749. 10.1093/cid/ciq238 [DOI] [PubMed] [Google Scholar]
- 12.Clinical and Laboratory Standards Institute (CLSI). Performance standards for antimicrobial susceptibility testing; Twenty-first informational supplement. CLSI document M100-S24:2014. Wayne, PA: CLSI; 2014.
- 13.Magiorakos AP, Srinivasan A, Carey RB, Carmeli Y, Falagas ME, Giske CG, et al. Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: an international expert proposal for interim standard definitions for acquired resistance. Clin Microbiol Infect. 2012;18: 268–281. 10.1111/j.1469-0691.2011.03570.x [DOI] [PubMed] [Google Scholar]
- 14.Schlesinger J, Navon-Venezia S, Chmelnitsky I, Hammer-Münz O, Leavitt A, Gold HS, et al. Extended-spectrum beta-lactamases among Enterobacter isolates obtained in Tel Aviv, Israel. Antimicrob Agents Chemother. 2005;49: 1150–1156. 10.1128/AAC.49.3.1150-1156.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Krishnamurthy V, Vijaykumar GS, Sudeepa KM, Prashanth HV, Prakash R, Nagaraj ER. Phenotypic and genotypic methods for detection of extended spectrum β lactamase producing Escherichia coli and Klebsiella pneumoniae isolated from ventilator associated pneumonia. J Clin Diagn Res. 2013;7: 1975–1978. 10.7860/JCDR/2013/6544.3376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kawakami S, Ono Y, Yamamoto M, Matumura M, Okamoto R, Inoue M, et al. [Extended-spectrum beta-lactamase (ESBL) produced by Escherichia coli and Klebsiella pneumoniae isolated from Teikyo University Hospital—the second report]. Kansenshogaku Zasshi. 2000;74: 24–29. 10.11150/kansenshogakuzasshi1970.74.24 [DOI] [PubMed] [Google Scholar]
- 17.Gao W, Sun Z, Yin J, Wang Q, Cheng J, Ye Y, et al. Studies on resistance and genotypes of CTX-M extended-spectrum-beta-lactamase-producing Klebsiella pneumoniae in Anhui province. Chin J Antibiot. 2009;34: 48–51. [Google Scholar]
- 18.Messai Y, Iabadene H, Benhassine T, Alouache S, Tazir M, Gautier V, et al. Prevalence and characterization of extended-spectrum beta-lactamases in Klebsiella pneumoniae in Algiers hospitals (Algeria). Pathol Biol. 2008;56: 319–325. 10.1016/j.patbio.2008.05.008 [DOI] [PubMed] [Google Scholar]
- 19.Oliver A, Pérez-Díaz JC, Coque TM, Baquero F, Cantón R. Nucleotide sequence and characterization of a novel Cefotaxime-hydrolyzing beta-lactamase (CTX-M-10) isolated in Spain. Antimicrob Agents Chemother. 2001;45: 616–620. 10.1128/AAC.45.2.616-620.2001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Espedido BA, Steen JA, Ziochos H, Grimmond SM, Cooper MA, Gosbell IB, et al. Whole genome sequence analysis of the first Australian OXA-48-producing outbreak-associated Klebsiella pneumoniae isolates: the resistome and in vivo evolution. PLOS ONE. 2013;8: e59920 10.1371/journal.pone.0059920 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zhang Y, Zhang K. Study on b-lactams resistance and genotype of blactamases in plasmid-mediated AmpC b-lactamases and ESBLs producing bacteria. Chin J Microbiol Immunol. 2004;24: 577–582. [Google Scholar]
- 22.Pérez-Pérez FJ, Hanson ND. Detection of plasmid-mediated AmpC beta-lactamase genes in clinical isolates by using multiplex PCR. J Clin Microbiol. 2002;40: 2153–2162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Coudron PE, Hanson ND, Climo MW. Occurrence of extended-spectrum and AmpC beta-lactamases in bloodstream isolates of Klebsiella pneumoniae: isolates harbor plasmid-mediated FOX-5 and ACT-1 AmpC betalactamases. J Clin Microbiol. 2003;41: 772–777. 10.1128/JCM.41.2.772-777.2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Leavitt A, Chmelnitsky I, Ofek I, Carmeli Y, Navon-Venezia S. Plasmid pKpQIL encoding KPC-3 and TEM-1 confers carbapenem resistance in an extremely drug-resistant epidemic Klebsiella pneumoniae strain. J Antimicrob Chemother. 2010;65: 243–248. 10.1093/jac/dkp417 [DOI] [PubMed] [Google Scholar]
- 25.Robicsek A, Strahilevitz J, Jacoby GA, Macielag M, Abbanat D, Park CH, et al. Fluoroquinolone-modifying enzyme: a new adaptation of a common aminoglycoside acetyltransferase. Nat Med. 2006;12: 83–88. 10.1038/nm1347 [DOI] [PubMed] [Google Scholar]
- 26.Kim HB, Park CH, Kim CJ, Kim EC, Jacoby GA, Hooper DC. Prevalence of plasmid-mediated quinolone resistance determinants over a 9-year period. Antimicrob Agents Chemother. 2009;53: 639–645. 10.1128/AAC.01051-08 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cavaco LM, Hasman H, Xia S, Aarestrup FM. qnrD, a novel gene conferring transferable quinolone resistance in Salmonella enterica serovar Kentucky and Bovismorbificans strains of human origin. Antimicrob Agents Chemother. 2009;53: 603–608. 10.1128/AAC.00997-08 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Robicsek A, Sahm DF, Strahilevitz J, Jacoby GA, Hooper DC. Broader distribution of plasmid-mediated quinolone resistance in the United States. Antimicrob Agents Chemother. 2005;49: 3001–3003. 10.1128/AAC.49.7.3001-3003.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Park CH, Robicsek A, Jacoby GA, Sahm D, Hooper DC. Prevalence in the United States of aac(6’)-Ib-cr encoding a ciprofloxacin-modifying enzyme. Antimicrob Agents Chemother. 2006;50: 3953–3955. 10.1128/AAC.00915-06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Weigel LM, Steward CD, Tenover FC. gyrA mutations associated with fluoroquinolone resistance in eight species of Enterobacteriaceae. Antimicrob Agents Chemother. 1998;42: 2661–2667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zimhony O, Chmelnitsky I, Bardenstein R, Goland S, Hammer Muntz O, Navon Venezia S, et al. Endocarditis caused by extended-spectrum-beta-lactamase-producing Klebsiella pneumoniae: emergence of resistance to ciprofloxacin and piperacillin-tazobactam during treatment despite initial susceptibility. Antimicrob Agents Chemother. 2006;50: 3179–3182. 10.1128/AAC.00218-06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hujer KM, Hujer AM, Hulten EA, Bajaksouzian S, Adams JM, Donskey CJ, et al. Analysis of antibiotic resistance genes in multidrug-resistant Acinetobacter sp. Isolates from military and civilian patients treated at the Walter Reed Army Medical Center. Antimicrob Agents Chemother. 2006;50: 4114–4123. 10.1128/AAC.00778-06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ma L, Lin CJ, Chen JH, Fung CP, Chang FY, Lai YK, et al. Widespread dissemination of aminoglycoside resistance genes armA and rmtB in Klebsiella pneumoniae isolates in Taiwan producing CTX-M-type extended-spectrum beta-lactamases. Antimicrob Agents Chemother. 2009;53: 104–111. 10.1128/AAC.00852-08 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bissonnette L, Roy PH. Characterization of In0 of Pseudomonas aeruginosa plasmid pVS1, an ancestor of integrons of multiresistance plasmids and transposons of Gram-negative bacteria. J Bacteriol. 1992;174: 1248–1257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Han H, Zhou H, Li H, Gao Y, Lu Z, Hu K, et al. Optimization of pulse-field gel electrophoresis for subtyping of Klebsiella pneumoniae. Int J Environ Res Public Health. 2013;10: 2720–2731. 10.3390/ijerph10072720 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Dice LR. Measures of the amount of ecologic association between species. Ecology. 1945;26: 297–302. 10.2307/1932409 [DOI] [Google Scholar]
- 37.Diancourt L, Passet V, Verhoef J, Grimont PA, Brisse S. Multilocus sequence typing of Klebsiella pneumoniae nosocomial isolates. J Clin Microbiol. 2005;43: 4178–4182. 10.1128/JCM.43.8.4178-4182.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wu H, Wang Y, Wu Y, Qiao J, Li H, Zheng S, et al. Emergence of β-lactamases and extended-Spectrum β-lactamases (ESBLs) producing salmonella in retail raw chicken in China. Foodborne Pathog Dis. 2015;12: 228–234. 10.1089/fpd.2014.1859 [DOI] [PubMed] [Google Scholar]
- 39.Anderl JN, Franklin MJ, Stewart PS. Role of antibiotic penetration limitation in Klebsiella pneumoniae biofilm resistance to ampicillin and ciprofloxacin. Antimicrob Agents Chemother. 2000;44: 1818–1824. 10.1128/AAC.44.7.1818-1824.2000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hernández-Allés S, Benedí VJ, Martínez-Martínez L, Pascual A, Aguilar A, Tomás JM, et al. Development of resistance during antimicrobial therapy caused by insertion sequence interruption of porin genes. Antimicrob Agents Chemother. 1999;43: 937–939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Schneiders T, Amyes SG, Levy SB. Role of AcrR and ramA in fluoroquinolone resistance in clinical Klebsiella pneumoniae isolates from Singapore. Antimicrob Agents Chemother. 2003;47: 2831–2837. 10.1128/AAC.47.9.2831-2837.2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Dhillon RH, Clark J. ESBLs: A clear and present danger? Crit Car. Res Pract. 2012;2012: 625170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Meier S, Weber R, Zbinden R, Ruef C, Hasse B. Extendedspectrum β-lactamase-producing Gram-negative pathogens in community-acquired urinary tract infections: an increasing challenge for antimicrobial therapy. Infection. 2011;39: 333–340. 10.1007/s15010-011-0132-6 [DOI] [PubMed] [Google Scholar]
- 44.Tumbarello M, Sanguinetti M, Montuori E, Trecarichi EM, Posteraro B, Fiori B, et al. Predictors of mortality in patients with bloodstream infections caused by extended-spectrum-beta-lactamase producing Enterobacteriaceae: importance of inadequate initial antimicrobial treatment. Antimicrob Agents Chemother. 2007;51: 1987–1994. 10.1128/AAC.01509-06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.An S, Chen J, Wang Z, Wang X, Yan X, Li J, et al. Predominant characteristics of CTX-M-producing Klebsiella pneumoniae isolates from patients with lower respiratory tract infection in multiple medical centers in China. FEMS Microbiol Lett. 2012;332: 137–145. 10.1111/j.1574-6968.2012.02586.x [DOI] [PubMed] [Google Scholar]
- 46.Turner MS, Andersson P, Bell JM, Turnidge JD, Harris T, Giffard PM. Plasmid-borne blaSHV genes in Klebsiella pneumoniae are associated with strong promoters. J Antimicrob Chemother. 2009;64: 960–964. 10.1093/jac/dkp338 [DOI] [PubMed] [Google Scholar]
- 47.Younes A, Hamouda A, Dave J, Amyes SG. Prevalence of transferable blaCTX-M-15 from hospital- and community-acquired Klebsiella pneumoniae isolates in Scotland. J Antimicrob Chemother. 2011;66: 313–318. 10.1093/jac/dkq453 [DOI] [PubMed] [Google Scholar]
- 48.Belmar Campos C, Fenner I, Wiese N, Lensing C, Christner M, Rohde H, et al. Prevalence and genotypes of extended spectrum beta-lactamases in Enterobacteriaceae isolated from human stool and chicken meat in Hamburg, Germany. Int J Med Microbiol. 2014;304: 678–684. 10.1016/j.ijmm.2014.04.012 [DOI] [PubMed] [Google Scholar]
- 49.Casella T, Rodríguez MM, Takahashi JT, Ghiglione B, Dropa M, Assunção E, et al. Detection of blaCTX-M-type genes in complex class 1 integrons carried by Enterobacteriaceae isolated from retail chicken meat in Brazil. Int J Food Microbiol. 2015;197: 88–91. 10.1016/j.ijfoodmicro.2014.12.001 [DOI] [PubMed] [Google Scholar]
- 50.Chon JW, Jung HI, Kuk M, Kim YJ, Seo KH, Kim SK. High occurrence of extended-Spectrum β-lactamase-producing salmonella in broiler carcasses from poultry slaughterhouses in South Korea. Foodborne Pathog Dis. 2015;12: 190–196. 10.1089/fpd.2014.1847 [DOI] [PubMed] [Google Scholar]
- 51.Li B, Yi Y, Wang Q, Woo PC, Tan L, Jing H, et al. Analysis of drug resistance determinants in Klebsiella pneumoniae isolates from a tertiary-care hospital in Beijing, China. PLOS ONE. 2012;7: e42280 10.1371/journal.pone.0042280 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Woodford N, Eastaway AT, Ford M, Leanord A, Keane C, Quayle RM, et al. Comparison of BD Phoenix, Vitek 2 and MicroScan automated systems for detection and inference of mechanisms responsible for carbapenem resistance in Enterobacteriaceae. J Clin Microbiol. 2010;48: 2999–3002. 10.1128/JCM.00341-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Deguchi T, Fukuoka A, Yasuda M, Nakano M, Ozeki S, Kanematsu E, et al. Alterations in the GyrA subunit of DNA gyrase and the ParC subunit of topoisomerase IV in quinolone-resistant clinical isolates of Klebsiella pneumoniae. Antimicrob Agents Chemother. 1997;41: 699–701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Aathithan S, French GL. Hypermutability in clinical isolates of Klebsiella pneumoniae is uncommon and is unrelated to ciprofloxacin resistance. Int J Antimicrob Agents. 2010;36: 239–242. 10.1016/j.ijantimicag.2010.04.010 [DOI] [PubMed] [Google Scholar]
- 55.Chen FJ, Lauderdale TL, Ho M, Lo HJ. The roles of mutations in gyrA, parC and OmpK35 in fluoroquinolone resistance in Klebsiella pneumoniae. Microb Drug Resist. 2003;9: 265–271. 10.1089/107662903322286472 [DOI] [PubMed] [Google Scholar]
- 56.Hopkins KL, Davies RH, Threlfall EJ. Mechanisms of quinolone resistance in Escherichia coli and salmonella: recent developments. Int J Antimicrob Agents. 2005;25: 358–373. 10.1016/j.ijantimicag.2005.02.006 [DOI] [PubMed] [Google Scholar]
- 57.Velhner M, Kozoderović G, Grego E, Galić N, Stojanov I, Jelesić Z, et al. Clonal spread of Salmonella enterica serovar Infantis in Serbia: acquisition of mutations in the topoisomerase genes gyrA and parC leads to increased resistance to fluoroquinolones. Zoonoses Public Health. 2014;61: 364–370. 10.1111/zph.12081 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All relevant data are within the paper.