Abstract
Until recently, the scientific community believed that post-exercise stretching could reduce delayed onset muscle soreness (DOMS), but recent reviews of studies on the topic have concluded that pre- or post-exercise static stretching has no effect on mitigating DOMS. However, the effect of proprioceptive neuromuscular facilitation (PNF) post-exercise stretching on preventing DOMS has not been adequately studied. The purpose of this study was to determine the effect of post-exercise PNF stretching on DOMS. Young adult participants (N=57) were randomly assigned to a PNF stretching group (n=19), a static stretching group (n=20), and to a no-stretching control group (n=18). All participants completed exercise designed to induce DOMS prior to post-exercise experimental stretching protocols. Participants rated their soreness level on a pain scale 24 and 48 hours post-exercise. A 3 × 2 mixed ANOVA showed there was an effect for time (p<.01). Post hoc testing revealed that DOMS pain significantly decreased (p<.05) from 24 to 48 hours post-exercise for the PNF and control groups, but not for the static stretching group. Other analyses revealed a significant correlation (r=.61, p<.01) between the pre- and post-exercise stretch scores and the 48 hour post-exercise pain score for the PNF group. Consistent with the results of previous research on post-exercise static stretching, these results indicate that post-exercise PNF stretching also does not prevent DOMS. However, the correlation analysis suggests it is possible the pre-stretch muscle contractions of the post-exercise PNF protocol may have placed a load on an already damaged muscle causing more DOMS for some participants.
Keywords: PNF, DOMS, stretching
INTRODUCTION
A dearth of physical activity and the high obesity rates among the American public are major public health concerns (14, 17, 19, 24). In an effort to mitigate sedentary behavior and disease prevalence, it is recommended that an individual exercises for 30 minutes a day, 5 or more days a week (7). For many exercisers, the fatigue of a strenuous workout is a satisfying sign of a productive session; however, the subsequent pain and stiffness associated with delayed onset muscle soreness (DOMS) is neither welcome nor positively reinforcing. DOMS pain can range from slight muscle discomfort to severe pain from unaccustomed exercise, and/or strenuous eccentric exercise, regardless of exercise experience (3). However, DOMS is often prevalent in those who are unaccustomed to exercise (3). DOMS typically occurs 8–10 hours after exercise and pinnacles between 24–72 hours after exercise (16). An increased risk of injury, decreased level of strength, and the pain associated with DOMS may deter people from exercising regularly (18). Although the exact causes of DOMS remain unknown, some theories suggest myofibrillar disturbances and micro-tears of the agonist skeletal muscle trigger an inflammatory response, which leads to muscle soreness (3, 4, 22).
Flexibility training has demonstrated the potential to provide a reduced risk of injury, enhanced athletic performance, sense of well-being, and in some cases a transient relief from DOMS (8, 20, 25). Exercisers may practice stretching as part of a warm-up routine, with the intent of preparing muscles to perform at peak level (20). However, post-exercise stretching may also help exercisers cool-down from their workout. Evidence concerning DOMS relief has suggested pre- or post-exercise static stretching should not be used as an overall treatment strategy for alleviating DOMS (9). However, evidence regarding the effects of other stretch modes (e.g., proprioceptive neuromuscular facilitation) have on DOMS still remains unclear in the literature (15).
A recent study prescribed an 8 week static or proprioceptive neuromuscular facilitation (PNF) stretch protocol to participants (2). After the 8 week stretching program was completed, there was an attenuation of exercise induced DOMS after bouts of eccentric resistance exercise in both stretch groups. This implies practicing PNF or static stretching may reduce DOMS if participation in a regular PNF or static stretch protocol is sustained over an extended period of time. However, it remains unknown if a single bout of PNF stretching after eccentric exercise abates DOMS. Accordingly, the purpose of this study was to investigate if post-exercise PNF stretching reduces DOMS.
METHODS
Participants
A sample of 57 young adult participants (29 males and 28 females) volunteered for the study. Means and standard deviations of the descriptive characteristics of the participants are shown in Table 1. A total of 19 participants were randomized to the PNF stretch group (9 males and 10 females), 20 participants were randomized to the static stretch group (14 males and 6 females), and 18 participants were randomized to the control group (5 males and 13 females). A substantial majority of the participants in this study had ages ranging from 18–25 years. Participants who were currently involved in intense physical conditioning (e.g., athletes), or who had a significant knee or upper leg injury were excluded from the study. Also, participants were asked to not exercise the lower extremities at least 48 hours prior to their visit. All participants had no DOMS at the onset of the study. Approval to conduct this study was granted by the University of North Dakota Institutional Review Board.
Table 1.
Descriptive Statistics of the Participants
| Overall (N=57) | PNF (n=19) | Static (n=20) | Control (n=18) | |
|---|---|---|---|---|
| Height (cm) | 165.6 ± 28.9 | 158.9 ± 22.9 | 180.5 ± 34.0 | 156.1 ± 22.2 |
| Weight (kg) | 75.2 ± 13.1 | 72.2 ± 10.4 | 82.0 ± 15.4 | 70.96 ± 10.1 |
| BMI (kg/m2) | 24.6 ± 2.7 | 23.7 ± 2.4 | 25.7 ± 3.1 | 24.4 ± 2.2 |
Values represent Means ± standard deviation
Protocol
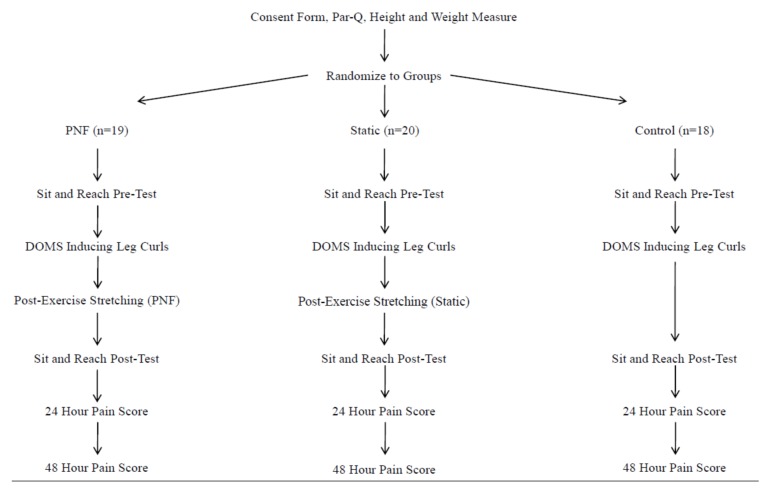
A post-test only study design was used to examine the purpose of this study. Participants were randomly assigned to one of two experimental groups: PNF stretch, static stretch, or no- stretch control. A simple randomization technique was used to place participants in these groups (21). The dependent variables were the pain scores reported by participants at 24 ± 2 hours and 48 ± 2 hours post-exercise; while, the independent variables were the flexibility scores from two sit-and-reach tests and the randomized stretch protocol. A schematic of the experimental design is depicted in Figure 1.
Figure 1.
Flow chart.
Height and weight were measured at the testing facility using standard techniques and equipment. BMI was calculated as weight in kilograms divided by height in meters squared and rounded to the nearest tenth (6). Participants then warmed up by jogging for 5–10 minutes until they were ready to perform exercise. After the warm-up was completed, participants performed a standard sit-and-reach test; the data were recorded in centimeters. During the sit-and-reach test, participants removed their shoes, kept their legs straight and feet flat against the box, and reached forward with both hands, holding for a 3-second count until their measurement was recorded.
Following the sit-and-reach test, each participant performed DOMS inducing leg curls on a Paramount Leg Curl SP 5100 weight machine (Paramount Fitness Corp; Los Angeles, CA). After an initial set with little resistance for familiarization to the machine, participants were given a predicted resistance that fit their 8–12 repetition max. During each set, participants concentrically contracted their hamstring muscles in an untimed, controlled manner. In order to place an emphasis on the eccentric phase of the leg curl, participants eccentrically lowered the weight for a 5-second count per rep after completing the concentric phase, as a means for inducing DOMS. Participants completed 3 sets of 8–12 reps during which muscular failure was achieved for each set (i.e., physically incapable of completing another repetition because their hamstrings muscles were too fatigued). The DOMS inducing protocol was modeled after a previous study (13). All participants received strong verbal encouragement during exercise to generate maximal force and effort.
After completing the DOMS inducing leg curls, participants completed the stretch protocol. In the PNF stretch group, participants were placed in a supine position on the floor. The stretched leg was fully extended on the primary investigator’s (PI) shoulder as a passive assist and was elevated until the participant self-reported a maximal stretch on the hamstrings muscles. When the participant reached maximal stretch on the hamstrings muscles, the “contract-relax-agonist-contract” PNF stretch protocol was performed; whereby, the participant maximally contracted the hamstrings isometrically for 5 seconds against the shoulder of the PI followed by 5 seconds of rest. After, the participant contracted the quadriceps muscles for 5 seconds, the PI then moved the leg to a further stretched position of the hamstrings and held it there for 5 seconds (2). This protocol was repeated twice on both legs with a 4 second break between sets.
In the static group, participants sat on the floor with their legs apart, fully extended, and with their knees locked. Participants reached toward one foot with both hands while the PI pushed on their back as a passive assist while keeping their legs fully extended. When the participant self-reported their maximal stretch on the hamstrings muscles, the stretch was held for 10 seconds with 4 seconds rest between stretches, for 2 sets on both legs.
Those who were randomized to the control group performed no post-exercise stretch and passively sat in a chair for the approximate duration it would have taken for a PNF or static stretch protocol to be completed. After completing the protocols, all participants performed another sit-and-reach test, as a means of assessing if flexibility levels changed from pre- to post-test.
Post-exercise DOMS was assessed using a modified version of the Muscle Soreness Scale utilized by High et al. (12). This 6-point scale provides descriptive phrases to help identify the participant’s level of muscle soreness that ranged from “complete absence of soreness” to “severe pain that limits your ability to move/unbearably painful.”
Exact time specifications were given to participants at the conclusion of their visit to inform participants when to report their DOMS scores. Participants reported their first soreness questionnaire score 24 ± 2 hours after the stretch protocol was completed, while the subsequent questionnaire score was reported 48 ± 2 hours after completing the stretch protocol. Both questionnaires were conducted via e-mail. In order to limit the influence of participant’s free-living behavior on DOMS scores, participants were advised to not engage in any moderate-to-vigorous physical activity or any exercising of the hamstrings muscles, engage in massage treatment, or take non-steroidal anti-inflammatory drugs until they completed their 48 hour soreness questionnaire (3).
Statistical Analysis
All analyses were conducted with IBM SPSS statistics software. A 3×2 (group × time) mixed ANOVA (Holm-Sidak post-hoc method) with pain measures taken at 24 ± 2 hours and 48 ± 2 hours post-exercise was used to test if PNF stretching abated DOMS. Pearson correlations were used to test the association between pain scores and pre- and post-test flexibility scores and pre-post flexibility change. Statistical significance was set at an α-level of 0.05 for all analyses.
RESULTS
Means and standard deviations of the participants’ flexibility and soreness levels are reported in Table 2. It should be noted the pre-exercise stretch scores were relatively consistent across all groups, suggesting no single group was substantially more flexible than another.
Table 2.
Means and standard deviations of the participant’s flexibility and soreness level.
| Overall (N=57) | PNF (n=19) | Static (n=20) | Control (n=18) | |
|---|---|---|---|---|
| Pre-exercise SS (cm) | 6.3 ± 9.8 | 5.2 ± 10.2 | 6.0 ± 9.7 | 7.9 ± 9.7 |
| Post-exercise SS (cm) | 7.9 ± 9.7 | 6.2 ± 10.3 | 8.5 ± 9.7 | 9.0 ± 9.4 |
| 24 hour PE-PS | 2.1 ± 0.9 | 2.2 ± 0.8 | 2.3 ± 1.1 | 1.9 ± 0.9 |
| 48 hour PE-PS | 1.8 ± 1.0 | 1.6 ± 1.0 | 2.0 ± 1.1 | 1.7 ± 0.9 |
| Pre-Post FC (cm) | 1.6 ± 1.8 | 1.1 ± 1.4 | 2.5 ± 1.4 | 1.0 ± 2.1 |
| 24 to 48h PSC | 0.4 ± 0.9 | 0.6 ± 0.9 | 0.3 ± 1.0 | 0.2 ± 0.8 |
Values represent Means ± standard deviation. SS= static stretch, PE-PS= post-exercise pain score, FC= flexibility change, PSC= pain score change
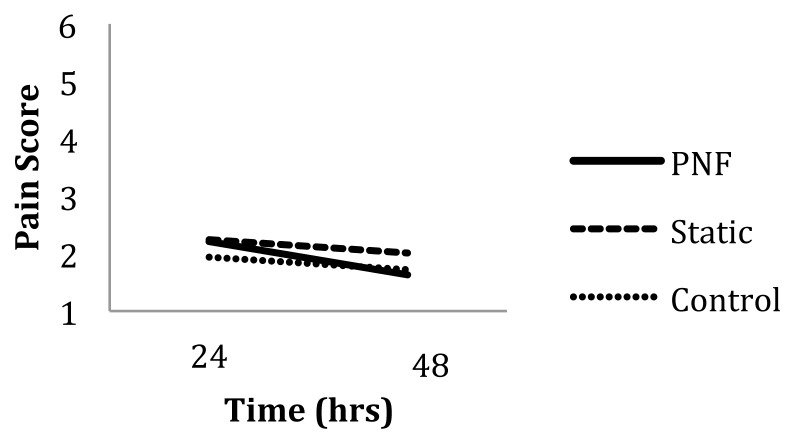
The results of the 3×2 mixed ANOVA showed an effect for time (p<.05); whereby, post hoc testing revealed that DOMS pain significantly decreased (p<.05) from 24 to 48 hours post-exercise for the PNF and control groups, but not for the static stretch group. These data are graphically presented in Figure 2.
Figure 2.
Treatment effects.
The correlations of flexibility scores with soreness ratings are shown in Table 3 below. A significant positive correlation between the pre- and post-exercise stretch score changes and the 48-hour pain score for the PNF group (r=.61, p<.01) indicates a moderate to strong association between pre-post flexibility increase and pain scores 48 hours after the DOMS inducing exercise. In contrast, there was a significant negative correlation between the pre- and post-exercise stretch score changes and the 24 hour pain score for the static stretch group (r=−.60, p<.01) suggesting a moderate to strong association between pre-post flexibility increase and lower pain scores 48 hours after the DOMS inducing exercise.
Table 3.
Correlations of flexibility scores with soreness ratings.
| Pre-test +24 hrs |
Post-test +24 hrs |
Pre-test +48 hrs |
Post-test +48 hrs |
Flex change +24 hrs |
Flex change +48 hrs |
|
|---|---|---|---|---|---|---|
| PNF | .08 | .13 | .26 | .34 | .33 | .61** |
| Static | .26 | .17 | .38 | .34 | −.60** | −.32 |
| Control | −.11 | −.08 | .24 | .29 | .18 | .20 |
p<.01
DISCUSSION
The results of this study did not support the premise that either PNF or static stretching post exercise significantly reduces DOMS, further contributing to the literature suggesting a single bout of post-exercise stretching does not attenuate DOMS. The correlations suggest PNF stretching made DOMS scores higher if there was a positive change in pre-post flexibility level. A positive change in flexibility level implies the stretch protocol was effective in making the agonist muscles immediately more elastic. Consequently, the positive correlation in the PNF stretch data suggests that the higher pain levels are likely the result of an added strain (stretch) being placed on an already fatigued muscle group after completing vigorous, eccentric resistance exercise. This added strain placed on the hamstrings muscles likely resulted in higher DOMS levels. PNF stretching also depresses the muscle spindle, causing muscles to further lengthen during the stretch (10). The lengthening and strain of a muscle group undergoing PNF stretching may cause a heightened inflammatory response as a result of added muscle tissue damage, therefore inducing high levels of DOMS, especially in those unaccustomed to eccentric resistance training or flexibility training.
In the case of the static stretching group, participants experienced lower levels of DOMS 24 hours post-exercise if there was a pre-post flexibility change. These results conflict with the evidence suggesting post-exercise static stretching does not reduce DOMS (9).
There is also a large amount of variability in how quickly DOMS scores decrease. DOMS can begin to mitigate between 24–72 hours post-exercise (16). Although it remains unclear as to why someone may recover from DOMS faster than another, training status and genetic components contribute to DOMS recovery independent of other modes of DOMS relief (22). Recovery from DOMS is likely going to be expedited in a younger, fitter population such as the cohort used in this study.
Some limitations of this study should be noted. First, researchers lacked the ability to truly control the participant’s free-living behavior. Although participants were advised not to seek DOMS relief or engage in certain activities, those who may have sought relief from their soreness may have reported lower DOMS scores. Another limitation of this study was the self-report DOMS questionnaire. Self-report questionnaires measuring DOMS could be subject to misinterpretation of the questions being asked and an under-estimation of DOMS scores as a result of social desirability recall bias (5). Although self-report questionnaires are a popular and economical method for measuring DOMS, some technologies have the ability to more objectively measure DOMS. Finally, the participants of this study were predominately young adults. Future studies should examine the effects of a single bout of post-exercise PNF stretching on DOMS in an older cohort.
In order to gain an objective measure of DOMS, researchers should continue to investigate DOMS prevention and treatment using Infra-Red technologies (1). This technique of measuring DOMS is likely more accurate than using a self-report questionnaire. Researchers should also continue to investigate the effects of flexibility and DOMS as it remains unknown if the PNF stretch protocol was responsible for the attenuation of DOMS scores in Chen et al. (2), or if flexibility alone was responsible for the decrease in DOMS scores.
Although often neglected by exercisers, flexibility training is an important component to fitness (11). It is recommended that an individual engages in flexibility training for each major muscle-tendon group for 60 seconds per exercise, for at least 2 days per week in order to maintain joint range of motion (7). However, like all other types of exercise one chooses to participate in, the frequency, intensity, type, and duration of all modes of exercise should be controlled. Those who are not fit or unaccustomed to exercise or flexibility training should avoid long, vigorous bouts of eccentric exercise or stretching as a means for avoiding high levels of DOMS. Participating in a progressive exercise and stretch routine may help one become more accustomed to exercise and flexibility training causing DOMS levels to slowly decrease. Furthermore, those who practice flexibility training may see lower levels of DOMS after a bout of vigorous, eccentric resistance exercise. Exercise professionals should also use DOMS prevention strategies such as progressively acclimating muscles to eccentric activity or engaging in a regular stretch routine, rather than relying on DOMS treatment strategies. Overall, DOMS prevention strategies appear to be more effective than DOMS treatment strategies (3, 22, 23).
Exercisers should use PNF stretching as a means of reducing DOMS with extreme caution. DOMS prevention strategies and other modes of treating DOMS should be considered by exercise professionals and exercisers.
ACKNOWLEDGEMENTS
A special thanks to Ronald H. Brinkert, Josh D. Guggenheimer, and David R. Paul for their contributions to this project.
REFERENCES
- 1.Al-Nakhli H, Petrofsky J, Laymon M, Berk L. The use of thermal infra-red imaging to detect delayed onset muscle soreness. J Vis Exp. 2012;59:1–9. doi: 10.3791/3551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chen C, Nosaka K, Chen H, Lin M, Tseng K, Chen T. Effects of flexibility training on eccentric exercise-induced muscle damage. Med Sci Sports Exerc. 2011;43:491–500. doi: 10.1249/MSS.0b013e3181f315ad. [DOI] [PubMed] [Google Scholar]
- 3.Cheung K, Hume P, Maxwell L. Delayed onset muscle soreness treatment strategies and performance factors. Sports Med. 2003;33:145–164. doi: 10.2165/00007256-200333020-00005. [DOI] [PubMed] [Google Scholar]
- 4.Cleak M, Eston R. Muscle soreness, swelling, stiffness and strength loss after intense eccentric exercise. Br J Sp Med. 1992;26:267–272. doi: 10.1136/bjsm.26.4.267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dollman J, Okely A, Hardy L, Timperio A, Salmon J, Hills A. A hitchhiker’s guide to assessing young people’s physical activity: deciding what method to use. J Sci Med Sport. 2009;12:518–525. doi: 10.1016/j.jsams.2008.09.007. [DOI] [PubMed] [Google Scholar]
- 6.Flegal K, Carroll M, Kit B, Ogden C. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999–200. JAMA. 2012;307:491–497. doi: 10.1001/jama.2012.39. [DOI] [PubMed] [Google Scholar]
- 7.Garber C, Blissmer B, Deschenes M, Franklin B, Lamonte M, Lee I, Nieman D, Swain D. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitniss in apparently healthy adults: guidance for prescribing exercise. Med Sci Sports Exerc. 2011;43:1337–1359. doi: 10.1249/MSS.0b013e318213fefb. [DOI] [PubMed] [Google Scholar]
- 8.Hartig D, Henderson J. Increasing hamstring flexibility decreases lower extremity overuse injuries in military basic trainees. Am J Sports Med. 1999;27:173–176. doi: 10.1177/03635465990270021001. [DOI] [PubMed] [Google Scholar]
- 9.Hebert R, de Noronha M, Kamper S. Stretching to prevent or reduce muscle soreness after exercise. Chohrane Data of Syst Rev. 2011;7:1–38. doi: 10.1002/14651858.CD004577.pub3. [DOI] [PubMed] [Google Scholar]
- 10.Heckman C, Gorassini M, Bennett D. Persistent inward currents in motorneuron dendrites: implications for motor output. Muscle Nerve. 2005;31:135–156. doi: 10.1002/mus.20261. [DOI] [PubMed] [Google Scholar]
- 11.Hendric A. Flexibility and the Conditioning Program. Nat Str Cond Assoc J. 1993;15:62–66. [Google Scholar]
- 12.High D, Howley E, Franks B. The effects of static stretching and warm-up on prevention of delayed-onset muscle soreness. Res Quart. 1989;60:357–361. doi: 10.1080/02701367.1989.10607463. [DOI] [PubMed] [Google Scholar]
- 13.Hilbert J, Sforzo G, Swensen T. The effects of massage on delayed onset muscle soreness. Br J Sports Med. 2003;37:72–75. doi: 10.1136/bjsm.37.1.72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hoyert D, Xu J. Deaths: preliminary data for 2011. NVSR. 2012;61:1–7. [PubMed] [Google Scholar]
- 15.Hume P, Cheung K, Maxwell L, Weerapong P. DOMS: an overview of treatment strategies. ISMJ. 2004;5:98–118. [Google Scholar]
- 16.Lee J, Goldfarb A, Rescino M, Hegde S, Patrick S, Apperson K. Eccentric exercise effect on blood oxidative-stress markers and delayed onset of muscle soreness. Med Sci Sports Exerc. 2002;34:443–448. doi: 10.1097/00005768-200203000-00010. [DOI] [PubMed] [Google Scholar]
- 17.Mokdad A, Marks S, Stroup D, Gerberding J. Actual causes of death in the United States, 2000. JAMA. 2004;291:1238–1245. doi: 10.1001/jama.291.10.1238. [DOI] [PubMed] [Google Scholar]
- 18.MacIntyre D, Reid W, McKenzie D. Delayed muscle soreness. The inflammatory response to muscle injury and its clinical implications. Sports Med. 1995;20:24–40. doi: 10.2165/00007256-199520010-00003. [DOI] [PubMed] [Google Scholar]
- 19.Ogden C, Carroll M, Kit B, Flegal K. Prevalence of obesity and trends in body mass index among US children and adolescents, 1999–2000. JAMA. 2012;307:483–490. doi: 10.1001/jama.2012.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Reisman S, Walsh L, Proske U. Warm-up stretches reduce sensations of stiffness and soreness after eccentric exercise. Med Sci Sports Exerc. 2005;37:929–936. [PubMed] [Google Scholar]
- 21.Suresh K. An overview of randomization techniques: an unbiased assessment of outcome in clinical research. J Hum Reprod Sci. 2011;4:8–11. doi: 10.4103/0974-1208.82352. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 22.Szymanski D. Recommendations for the avoidance of delayed onset muscle soreness. Strength Cond J. 2001;23:7–13. [Google Scholar]
- 23.Torres R, Riberio F, Duarte J, Cabri J. Evidence of the physiotherapeutic interventions used currently after exercise-induced muscle damage: systematic review and meta-analysis. Phys Ther Sport. 2012;13:101–114. doi: 10.1016/j.ptsp.2011.07.005. [DOI] [PubMed] [Google Scholar]
- 24.Van Gall L, Mertens I, De Block C. Mechanisms linking obesity with cardiovascular disease. Nature. 2006;444:875–880. doi: 10.1038/nature05487. [DOI] [PubMed] [Google Scholar]
- 25.Witvrouw E, Mahieu N, Danneels L, McNair P. Stretching and injury prevention. Sports Med. 2004;34:443–449. doi: 10.2165/00007256-200434070-00003. [DOI] [PubMed] [Google Scholar]