Abstract
As obesity rates increase, so too do the risks of type 2 diabetes, cardiovascular disease, and numerous other detrimental conditions. The prevalence of obesity in U.S. adults more than doubled between 1980 and 2010, from 15.0 to 36.1%. Although this trend may be leveling off, obesity and its individual, societal, and economic costs remain of grave concern. In June 2014, a Diabetes Care Editors’ Expert Forum convened to review the state of obesity research and discuss the latest prevention initiatives and behavioral, medical, and surgical therapies. This article, an outgrowth of the forum, offers an expansive view of the obesity epidemic, beginning with a discussion of its root causes. Recent insights into the genetic and physiological factors that influence body weight are reviewed, as are the pathophysiology of obesity-related metabolic dysfunction and the concept of metabolically healthy obesity. The authors address the crucial question of how much weight loss is necessary to yield meaningful benefits. They describe the challenges of behavioral modification and predictors of its success. The effects of diabetes pharmacotherapies on body weight are reviewed, including potential weight-neutral combination therapies. The authors also summarize the evidence for safety and efficacy of pharmacotherapeutic and surgical obesity treatments. The article concludes with an impassioned call for researchers, clinicians, governmental agencies, health policymakers, and health-related industries to collectively embrace the urgent mandate to improve prevention and treatment and for society at large to acknowledge and manage obesity as a serious disease.
Obesity is a crucial public health concern given its contribution to the risk of diabetes, cardiovascular disease (CVD), and other comorbidities. The prevalence of obesity (BMI ≥30.0 kg/m2) in U.S. adults more than doubled between 1980 and 2010, from 15.0 to 36.1% (1,2). More than two-thirds (68.7%) of all American adults are overweight or obese (BMI ≥25.0 kg/m2) (1). Although recent data suggest a leveling off in this trend, persistently high obesity rates remain of grave concern (3). Obesity rates are now also climbing in developing countries; worldwide, obesity has nearly doubled since 1980, affecting >500 million adults (4).
As obesity rates increase, so too do the risks of type 2 diabetes, CVD, hypertension, arthritis, cognitive impairment, and some cancers (5). In the U.S., diagnosed diabetes increased from 7.8 million in 1993 to 21 million in 2012, >8 million people remain undiagnosed, and an estimated 86 million adults have prediabetes (6,7). Population-based studies have suggested that ∼75% of hypertension is attributable to obesity (8), and approximately one-third of cancer deaths are linked to poor nutrition, excess weight, and sedentary lifestyle (9). Worldwide, 44% of the diabetes burden, 23% of ischemic heart disease, and 7–41% of certain cancers are attributable to excess weight (4). Obesity also decreases both health-related quality of life (10) and life expectancy (11).
The medical costs of obesity in the U.S. were estimated at $190 billion in 2012 (12). A recent systematic review found that, worldwide, obesity-related medical costs accounted for 0.7–2.8% of a country’s total health care expenditure and that people with obesity had medical costs ∼30% higher than their normal-weight peers (13).
With these alarming statistics in mind, a Diabetes Care Editors’ Expert Forum convened in June 2014 to review the state of obesity research and discuss prevention and treatment initiatives. This article summarizes the proceedings of that forum.
Obesity in Context
What explains the sharp uptick in obesity rates that occurred after 1980? Hindsight suggests that a combination of technological advances, certain agricultural and economic policies, and a decline in physical activity all contributed. In the 1970s, the U.S. enacted agricultural subsidies aimed at lowering food prices by encouraging increased production of crops such as corn and soybeans. Such subsidies, in concert with large-scale industrialized farming practices, resulted in an overabundance of inexpensive food. In addition to lowering the price of grains, subsidies reduced the cost of meat (from livestock fed on less expensive crops) and allowed the food manufacturing industry to produce a wide range of inexpensive and convenient—but also energy-dense and nutrient-poor—products (14).
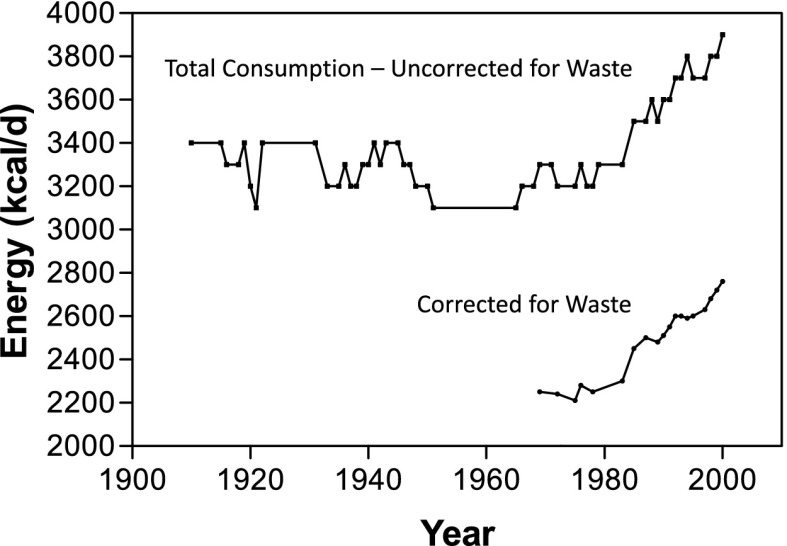
It has been suggested that chronic exposure to easily obtainable, highly palatable foods can cause the hedonic, or reward-based, neuronal pathway to override the homeostatic pathway that ordinarily controls energy balance (15). Average daily calorie consumption in the U.S. increased by 24.5%, or ∼530 calories, between 1970 and 2000 (Fig. 1) (16). Meanwhile, as dietary intake was observed to increase, both occupational and leisure-time energy expenditures declined (17,18). Similar patterns have become apparent elsewhere in the world (19).
Figure 1.
Food available for consumption, 1900–2000. Reprinted from ref. 16.
The complex issues of grain overproduction, fruit and vegetable underavailability, detrimental food processing and marketing practices, and consumer knowledge deficits are beyond the scope of this article but have been eloquently elucidated elsewhere (5,20).
Much Learned, More Still to Learn
In recent decades, there has been an impressive expansion in our knowledge base regarding obesity. We have learned that the genetic components of obesity are key contributors to individual risk. Studies involving families, twins, and adoption have shown that adiposity is highly heritable (21). Genome-wide association studies have demonstrated that numerous genes are associated with weight gain (22) and that the presence of risk alleles for multiple small-effect genes can result in marked cumulative effects on BMI (23). Genetics can also inform the selection of obesity interventions; one example is the Preventing Overweight Using Novel Dietary Strategies (POUNDS LOST) trial (24), in which carriers of the FTO variant risk allele lost weight more successfully on a high-protein than on a low-protein diet. Epigenetic factors can modify weight gain and aid in identifying individuals at higher risk for obesity (25,26). In addition, social factors appear to influence its occurrence (27).
The physiological milieu promoting obesity involves complex and interrelated metabolic factors. Once considered simple storage depots for body energy, adipocytes are now recognized as active endocrine cells that have many roles, including the regulation of metabolism, energy intake, and fat storage (28,29). Small adipocytes found in normal-weight individuals release adipokines that do not upset metabolic homeostasis, whereas enlarged adipocytes found in people with obesity release adipokines in larger amounts, which can promote inflammation and insulin resistance. More than 50 adipokines have been identified, perhaps the best known of which are leptin and adiponectin (29).
Research is similarly elucidating the neural pathways involved in regulating food intake and energy control and the ways in which genetic and early environmental factors can modulate the functioning of these pathways (30). Gut hormones such as ghrelin, cholecystokinin, peptide YY, and glucagon-like peptide 1 (GLP-1) appear to have key roles. Additionally, insulin resistance, inflammation, and the gut microbiome all affect weight (31,32).
Obesity-Related Metabolic Dysfunction
Obesity is associated with a constellation of metabolic abnormalities, including insulin resistance, β-cell failure, atherogenic dyslipidemia (i.e., high triglycerides, low HDL cholesterol, and increased small, dense LDL particles), and nonalcoholic fatty liver disease (NAFLD). However, not all people with obesity exhibit these abnormalities, and a metabolically healthy obese (MHO) phenotype (i.e., BMI ≥30.0 kg/m2 with normal fasting blood glucose, insulin sensitivity, lipid profile, and intrahepatic triglyceride [IHTG] content levels) has been described (33).
The MHO phenotype is more common in younger than in older people and occurs more often in women than in men. The proportion of the population with obesity considered to be MHO depends on the criteria used to define “metabolically healthy.” One study that applied five existing definitions of MHO to the same group of adults found prevalence rates ranging from 6.8 to 36.6% (34), whereas data from the 1999–2004 National Health and Nutrition Examination Surveys (35), which defined metabolic health as the presence of no more than one component of the metabolic syndrome, found that 29.2% of men and 35.4% of women with obesity were metabolically healthy. The most clinically relevant question, however, is whether there is something inherently different and protective in MHO individuals or whether, given more time or additional weight gain, their metabolic function will deteriorate into metabolically unhealthy obesity (MUO) (36). Accumulating evidence suggests that the MHO phenotype represents a distinct subset of the obese population and that people identified as MHO, while at higher risk for future diabetes and heart disease than their lean, metabolically normal counterparts, have lower risks than both people with obesity and lean people who are metabolically abnormal (37–41). Other studies have also supported the concept that individuals with the MHO phenotype are more resistant to the adverse metabolic effects of moderate weight gain (42).
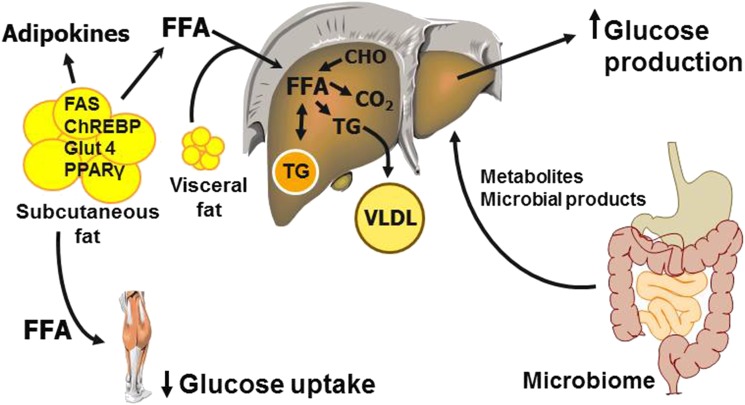
Several organs, including the liver, adipose tissue, skeletal muscle, and intestine, are involved in the pathophysiology and pathogenesis of obesity-related metabolic dysfunction (Fig. 2). For example, the liver is an important marker of metabolic health, and an increase in IHTG content is associated with multiorgan metabolic dysfunction. Triglycerides accumulate in hepatocytes if their rate of production (from fatty acids delivered from plasma or produced de novo) exceeds their rate of removal (via triglyceride lipolysis and fatty acid oxidation or secretion as VLDL particles). IHTG content is negatively correlated with insulin sensitivity in the liver (ability to suppress glucose production), skeletal muscle (ability to stimulate glucose uptake), and adipose tissue (ability to suppress lipolysis) (43). People with NAFLD also have an increase in hepatic de novo lipogenesis (44) and in VLDL-triglyceride secretion rate compared with people with obesity and normal IHTG content (45).
Figure 2.
Putative factors involved in the pathogenesis and pathophysiology of metabolic dysfunction associated with obesity. CHO, carbohydrate; ChREBP, carbohydrate response element–binding protein; FAS, fatty acid synthase; FFA, free fatty acid; Glut 4, glucose transporter 4; PPARγ, peroxisome proliferator–activated receptor γ; TG, triglyceride.
Adipose tissue is also a key organ in the development of metabolic dysfunction. Excessive circulating fatty acids, released from lipolysis of subcutaneous and visceral adipose tissue triglycerides, can cause hepatic and skeletal muscle insulin resistance (46,47). Compared with MHO individuals, people with MUO exhibit alterations in adipose tissue metabolic and immune function, including decreased expression of adipose tissue genes involved in fatty acid and glucose metabolism (48–51); increased collagen production (52); and increased markers of adipose tissue inflammation (53).
Recently, data from both preclinical and clinical studies have shown that intestinal microbiota are another potentially important regulator of metabolic health (54). People with insulin resistance and impaired glucose control have decreased microbial diversity (55), and transferring microbiota from metabolically healthy or metabolically unhealthy donors can transfer the donor’s metabolic phenotype to the recipient (56). Finally, the brain also modulates peripheral metabolism (57).
How Much Weight Loss Is Enough?
Although no current therapeutic approaches offer an obesity cure, losing weight significantly ameliorates obesity-associated morbidity and reduces its related costs. Even without reaching a BMI in the normal range (<25.0 kg/m2), people with obesity can accrue meaningful health benefits from weight loss (58). On the basis of evidence available at the time, the 1998 National Heart, Lung, and Blood Institute (NHLBI) obesity guidelines defined an initial goal of weight-loss therapy as ∼10% of body weight (59). More recent guidelines (60) noted that “although sustained weight loss of as little as 3%–5% of body weight may lead to clinically meaningful reductions in some cardiovascular risk factors, larger weight losses produce greater benefits” and set an initial goal of 5–10%. In addition to links between obesity and cardiovascular risk, excess weight may play an independent role in the development of microvascular diseases, including kidney disease (microalbuminuria) (61) and retinopathy (62).
Although the precise “dose-response” relationships between weight loss and obesity-related complications vary, progress has been made in this area (Table 1) (63–80). If the objective of weight-loss therapy is to derive health benefits associated with the amelioration of complications, then the weight-loss goal should be established based on this evidence.
Table 1.
Evidence regarding therapeutic weight loss for complications of obesity
| Obesity complication | Weight loss required for therapeutic benefit (%) | Notes | References |
|---|---|---|---|
| Diabetes (prevention) |
3–10 |
Maximum benefit at 10% |
DPP Research Group, 2009 (63) |
| Garvey et al., 2014 (64) | |||
| Hypertension |
5 to >15 |
Blood pressure still decreasing at >15% |
Wing et al., 2011 (65) |
| Dyslipidemia |
3 to >15 |
Triglycerides still decreasing at >15% |
Wing et al., 2011 (65) |
| Hyperglycemia (elevated A1C) |
3 to >15 |
A1C still decreasing at >15% |
Wing et al., 2011 (65) |
| NAFLD |
10 |
Improves steatosis, inflammation, and mild fibrosis |
Assy et al., 2007 (66) |
| Dixon et al., 2004 (67) | |||
| Patel et al., 2009 (68) | |||
| Sleep apnea |
10 |
Little benefit at 5% |
Foster et al., 2009 (69) |
| Winslow et al., 2012 (70) | |||
| Osteoarthritis |
5–10 |
Improves symptoms and joint stress mechanics |
Christensen et al., 2007 (71) |
| Felson et al., 1992 (72) | |||
| Aaboe et al., 2011 (73) | |||
| Stress incontinence |
5–10 |
Burgio et al., 2007 (74) |
|
| Subak et al., 2009 (75) | |||
| Gastroesophageal reflex disease |
5–10 in women; 10 in men |
Singh et al., 2013 (76) |
|
| Tutuian, 2011 (77) | |||
| Polycystic ovary syndrome | 5–15 (>10 optimal) | Lowers androgens, improves ovulation, and increases insulin sensitivity | Panidis et al., 2008 (78) |
| Norman et al., 2002 (79) | |||
| Moran et al., 2013 (80) |
Intuitively, in improving metabolic risk factors, weight loss should also have a positive impact on mortality. However, this has been more difficult to show, in part because the extent and nature of the excess weight-mortality association remains a matter of debate (58). Some studies have suggested that this relationship resembles a U- or J-shaped curve with its lowest point at a BMI of ∼23 kg/m2, after taking into account confounding by smoking and reverse causation (i.e., low BMI caused by preexisting or subclinical chronic diseases) (81,82). Obesity has been found to lower life expectancy (11,83), and CVD has been identified as the major cause of excess mortality among people with obesity (84,85).
Conversely, studies in overweight individuals (BMI 25.0 to <30.0 kg/m2) have found little or no increased mortality risk, and some have shown reduced mortality rates compared with normal-weight individuals (85,86). However, interpretation of this phenomenon is complicated by methodological problems in BMI-mortality analysis, especially with regard to reverse causation and the use of a broad BMI category as the reference group (87). In addition, it seems likely that improved detection and treatment of conditions such as diabetes, hypertension, dyslipidemia, and sleep apnea have blunted the relative risk of obesity-related mortality over time. A 2013 meta-analysis of 97 studies (88) found that, relative to individuals of normal weight, there was no increased mortality risk even in individuals with grade 1 obesity (BMI 30.0 to <35.0 kg/m2; HR 0.95 [95% CI 0.88–1.01]), although individuals with obesity grades 2 and 3 combined (BMI ≥35.0 kg/m2) did have a significantly higher mortality rate (HR 1.29 [95% CI 1.18–1.41]). Because this meta-analysis was based on published literature without analyzing individual-level data, it could not fully address confounding by smoking behavior or the problem of reverse causation (89).
To date, bariatric surgery has most effectively demonstrated a reduction in mortality (90). Analysis of long-term follow-up data from the Swedish Obese Subjects (SOS) study found that bariatric surgery reduced cardiovascular deaths and first-time (fatal and nonfatal) cardiovascular events after a mean follow-up of 14.7 years (91).
Until recently, nonsurgical lifestyle interventions have failed to show a significant reduction in cardiovascular events, even after one to two decades of follow-up (92,93). However, the latest report from the Da Qing Diabetes Prevention Study of adults with impaired glucose tolerance demonstrated a reduction in CVD mortality, mainly in women, that began to emerge after 12 years but did not become statistically significant until 23 years after the initial 6-year intervention (94). The ongoing Action for Health in Diabetes (Look AHEAD) lifestyle intervention study has reported no significant reductions in cardiovascular morbidity and mortality over nearly 10 years in people with type 2 diabetes who are overweight or obese and who lost an average 6% of their baseline body weight (95). For now, the questions of whether and how much weight loss will reduce mortality remain unanswered.
Lifestyle Intervention and Behavioral Modification
Lifestyle interventions emphasizing reduced caloric intake and increased physical activity and incorporating behavioral modification techniques are considered first-line therapy for overweight and obesity (60). Because obesity arises from complex interactions between genetics and environmental factors, such interventions must focus not solely on the eating and exercise habits of people with obesity but rather on those habits in the context of the environment in which people live. Thus, lifestyle interventions must be tailored to the needs, preferences, and circumstances of individuals and adapted to the settings and populations in which they are provided (96).
Two lifestyle intervention studies—the Diabetes Prevention Program (DPP) (97) and Look AHEAD (98,99)—have yielded the most valuable information on the potential of such interventions to bring about significant long-term weight reduction. In the DPP, 3,234 adults with glucose tolerance test results indicative of prediabetes and a mean BMI of 34 kg/m2 were randomly assigned to placebo, metformin therapy, or a lifestyle intervention with the goal of achieving a weight loss ≥7% of initial body weight. After a mean follow-up of 2.8 years, weight loss in the lifestyle group averaged 5.5%, and the incidence of diabetes was reduced by 58% in the lifestyle group and 31% in the metformin group compared with placebo (97). Look AHEAD was designed to assess the long-term effects on cardiovascular morbidity and mortality of an intensive weight-loss program delivered over 4 years to adults with type 2 diabetes who were overweight or obese. The study included 5,145 participants assigned to either usual care (diabetes support and education) or the intervention, which aimed at reducing body weight by ≥10% (98). This intervention was found to have no significant effect on CVD mortality but did improve some CVD risk factors after a mean follow-up of 9.6 years and reduced mean weight by ≥8% by year 1 and >5% by year 8 (99,100).
Highly Variable Success
Participants in the DPP and Look AHEAD had similar rates of initial success. In the DPP, 49% of intervention participants met their weight-loss goal and 74% met their physical activity goal by week 24; 37% and 67%, respectively, met these goals by the final intervention visit (101). After 1 year in the Look AHEAD intervention, 37.8% of participants met their individual weight-loss goal (≥10% of initial weight) and 55.2% met the group average goal (≥7%) (100).
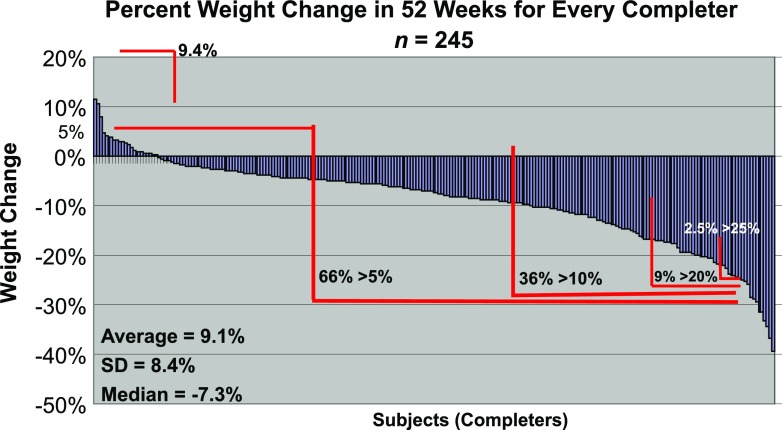
Although these average losses may seem modest, it is important to remember that success rates with lifestyle intervention are highly variable and a significant proportion of individuals achieve success far exceeding the mean results. Figure 3, which shows weight changes after 1 year for a series of 245 participants in the New York Obesity Nutrition Research Center (NYORC) weight-loss program, illustrates this point. Although 9.4% of these individuals experienced weight gain, the remainder lost weight, with more than one-third losing >10% and several losing >25% of their initial body weight.
Figure 3.
Percentage of weight change by subject (n = 245) at week 52 of the NYORC weight-loss program. Courtesy of Richard Weil, MEd, CDE (Columbia University, New York, NY); Betty Kovacs, MS, RD (Columbia University, New York, NY); and F.X.P.-S.
Real-World Challenges
Most intensive lifestyle programs (e.g., the DPP and Look AHEAD) have been carried out with highly structured interventions, employing protocols that may be difficult to implement in real-world settings (97,98,102,103). Despite the potential difficulties in replicating such programs, numerous promising efforts are underway to implement DPP-style interventions in creative and cost-effective ways in communities across the U.S. (104,105).
Predictors of Long-term Success
In general, lifestyle interventions appear to be moderately successful in inducing initial weight loss; however, weight regain often begins to occur after ∼6 months, as noted in both the DPP and Look AHEAD (99,106).
In the DPP, the likelihood of meeting weight-loss and activity goals increased with participants’ age (101); even after 10 years of follow-up, participants who were <45 years of age at randomization had less sustained weight loss than those ≥45 years of age (63). Those who performed more dietary self-monitoring and those who met the activity goal were more likely to meet their weight-loss goal. Importantly, initial success at week 24 predicted longer-term success at 3.2 years, with those achieving initial goals 1.5–3 times more likely to achieve the longer-term goals (101).
In Look AHEAD, lifestyle participants who lost ≥5% or ≥10% of body weight by year 1 were more likely to have these same losses by year 4. Those who maintained a loss of ≥10% for 4 years attended more treatment sessions and reported getting more physical activity and consuming fewer calories than those who did not. As in the DPP, older participants lost significantly more weight than younger participants throughout the study (107).
The ongoing National Weight Control Registry has yielded additional important insights into the factors that contribute to successful long-term weight management. Registry participants who have maintained an intentional weight loss of ≥30 lb for an average of 5.7 years report regularly self-monitoring, including recording their food intake and weighing themselves at least once weekly; eating a low-calorie, low-fat diet (1,300–1,400 kcal/day with ∼25% of calories from fat); eating breakfast daily; maintaining a consistent eating pattern across weekdays and weekends; and engaging in high levels of physical activity (expending >2,500 kcal/week for women and >3,200 kcal/week for men). Successful weight-loss maintainers also report continuing to adhere to the diet and exercise strategies they employed to lose weight, having low levels of depression and dietary disinhibition, and having had a medical trigger for their initial weight loss (108).
Of these factors, a high level of physical activity appears to be particularly important. A study by Jakicic et al. (109) demonstrated a dose-response relationship between the amount of exercise performed per week and long-term weight loss and maintenance in overweight adult women. Individuals who exercised ≥200 min/week had greater 18-month weight losses than those who were active either <150 or 151–199 min/week (–13.1, –3.5, and –8.5 kg, respectively).
Nonresponders: The Importance of Early Identification
Although quite a bit is known about successful weight losers, less is known about those who fail to respond to lifestyle interventions. In the NYORC program, for example, some participants not only failed to lose weight but actually gained weight over 1 year, even though they were highly invested in the program, had paid to participate, regularly attended sessions, and contributed actively. One can only surmise that some combination of genetic and environmental determinants is responsible for making weight loss more difficult for some people than for others. Until such factors are better understood, the finding that early success predicts long-term success becomes even more important; individuals who fail lifestyle intervention early on may be better served by pursuing alternatives such as pharmacotherapy or bariatric surgery than by continuing in a behavioral program in which they may be destined to fail.
Diabetes Pharmacotherapies: Weight Considerations
Associations between improved glycemic control and weight gain with traditional pharmacotherapies such as insulin, sulfonylureas, and thiazolidinediones are well documented (110–112). Weight gain is of less concern with modern analog insulin formulations, as seen in the Outcome Reduction With Initial Glargine Intervention (ORIGIN) trial (113). Weight gain with thiazolidinediones appears to be continuous and mostly subcutaneous, whereas that with sulfonylureas is central and occurs mostly in the first year (112).
Numerous factors have been found to predict weight responses to traditional diabetes pharmacotherapies. In the Action in Diabetes and Vascular Disease: Preterax and Diamicron MR Controlled Evaluation (ADVANCE) trial (114), older age, female sex, and current smoker status predicted weight loss, whereas higher A1C levels, more oral medications, Caucasian ethnicity, and, to a lesser extent, longer diabetes duration and higher systolic blood pressure, were associated with weight gain. The noninterventional Cardiovascular Risk Evaluation in People With Type 2 Diabetes on Insulin Therapy (CREDIT) study (115) of insulin started in routine care identified higher baseline A1C, higher insulin requirements, and lower baseline BMI as independent predictors of insulin-associated weight gain. These findings suggest that therapy-related weight gain may be attenuated by starting insulin earlier, before patients have a very poor A1C and have lost significant weight through poor glycemic control.
Weight-Adding Effects of Other Common Medications
Some non–glucose-lowering medications commonly prescribed to people with diabetes have been linked to weight gain, including hormones such as corticosteroids (116); drugs affecting energy metabolism such as β-blockers (117) and antiepileptic medications that are more often used for diabetic neuropathy (e.g., gabapentin and pregabalin) (118); second-generation antipsychotics (119); and protease inhibitors (120).
Weight-Neutral or Weight-Lowering Effects of Newer Glucose-Lowering Medications
Metformin is the most widely used first-line agent for type 2 diabetes and is generally described as weight neutral. Dipeptidyl peptidase 4 (DPP-4) inhibitors, which enhance circulating GLP-1 and glucose-dependent insulinotropic polypeptide and thereby regulate insulin and glucagon secretion, have demonstrated weight neutrality (121–124). GLP-1 receptor agonists, which additionally slow gastric emptying and decrease appetite, cause moderate to significant weight loss while reducing glycemia (125–127). Sodium–glucose cotransporter 2 (SGLT2) inhibitors, which block glucose reabsorption in the kidney, improve glycemic control and result in moderate weight loss, with reductions in visceral and subcutaneous adipose tissue (22,128,129).
Potentially Weight-Neutral Combination Therapies
Given the differing weight effects of existing glucose-lowering pharmacotherapies, consideration of combination therapies appears warranted. One such combination involves a GLP-1 receptor agonist and long-acting insulin. This has been tested in insulin-naive people who are starting basal insulin and in people already on basal insulin therapy, adding a GLP-1 receptor agonist instead of mealtime insulin (130–133). Results include amelioration of weight gain, or weight loss, with improved glycemic control and reduction in the incidence of hypoglycemia compared with insulin alone. Although continuing metformin with all other agents is standard, other combination strategies involving incretin-based therapies and SGLT2 inhibitors might help to overcome compensatory eating and other mechanisms that appear to limit the weight-loss potential of individual drug classes, while further improving glycemic control (124,134).
Obesity Pharmacotherapies: Troubled Past, Promising Future
Although the history of obesity pharmacotherapy has been fraught with setbacks, several viable agents are now available, and expanding clinical experience is beginning to elucidate their most efficacious use (135). From the 1940s through the 1980s, pharmacological options for obesity were limited to phentermine and other appetite-suppressing sympathomimetics approved only for short-term use because of concerns about potential abuse. Later, other centrally acting agents were marketed in the U.S.—the amphetamine serotonergic-like drugs fenfluramine (1972) and dexfenfluramine (1996) and the serotonin-norepinephrine reuptake inhibitor sibutramine (1997). However, the first two of these (often used in the combination known as “fen-phen”) were withdrawn because of suspected heart valve damage and the third because of increased risk of cardiovascular events (136,137). Likewise, rimonabant, a cannabinoid receptor antagonist, was introduced in Europe in 2006 but later withdrawn because of links to severe mood disorders (138). Introduced in 1999, orlistat, a gastrointestinal (GI) lipase inhibitor, was, until recently, the only obesity medication approved for long-term use in the U.S. (139). However, four newer agents have since become available: 1) phentermine/topiramate extended release (ER), combining a sympathomimetic and an anticonvulsant, in 2012; 2) the 5-HT2c serotonin receptor agonist lorcaserin, in 2012; 3) naltrexone/bupropion ER, combining a dopamine/noradrenaline reuptake inhibitor and an opioid receptor antagonist, in 2014; and 4) a high-dose (3-mg) preparation of the GLP-1 receptor agonist liraglutide, in 2015 (140–143).
Although concerns about the safety of weight-loss medications remain, the rationale for their use in appropriate candidates is sound. When used as an adjunct to lifestyle intervention, these agents can help people who are struggling to achieve health benefits through weight loss by enhancing their ability to comply with a reduced-calorie diet. Numerous studies have shown that adding a weight-loss medication can yield greater weight loss than lifestyle intervention alone and allows people to sustain any loss for a longer period of time (144–154).
Recommendations for Use
Several principles guide the incorporation of weight-loss medications into the management of obesity. Importantly, current guidelines advise their use only for people with health risks and not merely for cosmetic reasons (6,155). In addition, prescribing information for phentermine/topiramate ER, lorcaserin, and naltrexone/bupropion ER calls for discontinuation after 12 weeks if weight loss is <5% on the maximal dose (156–158); liraglutide 3 mg should be discontinued if weight loss is <4% after 16 weeks (159). Obesity medications have some degree of primary failure, but the availability of multiple options means that, should one drug fail to yield significant weight loss, another drug can be tried. Finally, obesity should be considered a life-long disease requiring long-term treatment and follow-up.
Evidence for Efficacy
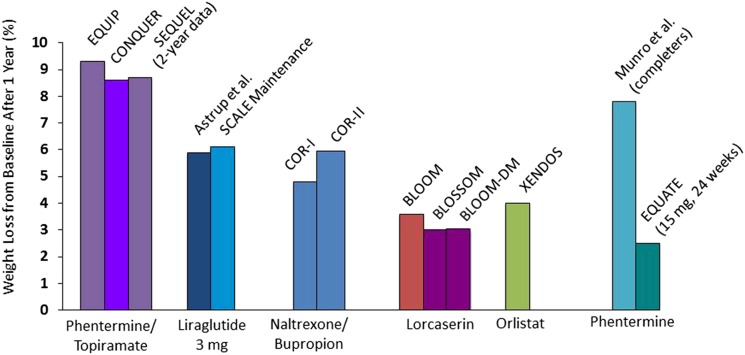
Head-to-head trials comparing the efficacy of obesity medications have not been published. However, one can predict relative effectiveness by comparing the placebo-subtracted weight losses resulting from their use in separate studies. In the study design of these clinical trials, all patients were placed on lifestyle interventions and then randomized to placebo versus weight-loss medication. Because the intensity of the lifestyle intervention was variable, placebo-subtracted weight loss can be used to compare weight loss attributable to the medications alone. Figure 4 shows such a comparison of intention-to-treat data, usually after 1 year on the maximum dose (144–154,160–162). In this analysis, phentermine/topiramate appears most efficacious, with a placebo-subtracted loss of ∼9%, followed by naltrexone/bupropion (∼6%), liraglutide (∼6%), lorcaserin (∼4%), and orlistat (∼3–5%). As with other chronic diseases when medications are discontinued, the effect of medication on weight loss is not sustained when the medication is discontinued; patients generally regain weight to a level determined by the intensity of the lifestyle intervention upon cessation of the medication. Still, each of these pharmacological options has the potential to achieve enough weight loss to have therapeutic benefit on at least some of the associated complications listed in Table 1.
Figure 4.
Comparative efficacy of weight-loss medications. All data are placebo-subtracted, maximal dose, 1-year results in intention-to-treat populations using last-observation-carried-forward method unless otherwise indicated (144–154,160–162).
The effects of these medications in prediabetes and diabetes—arguably, the most common and troublesome obesity complications—provide further support for their use. In a recent phentermine/topiramate ER study in people with prediabetes (64), drug-assisted weight loss reduced the incidence of progression to type 2 diabetes over 108 weeks by 79% compared with placebo.
Efficacy data are also strong in people who already have diabetes. Table 2 summarizes data from various studies on the effects of weight-loss drugs versus placebo on weight, A1C, and the need for oral glucose-lowering agents (150,163–167). For all, drug-assisted weight loss yields better glycemic control, while reducing the number and doses of glucose-lowering medications and generally lowering blood pressure and improving lipids. This suggests that weight-loss therapy should be considered in any newly diagnosed person with type 2 diabetes or whenever intensification of therapy is indicated to achieve A1C targets, as an adjunct or alternative to the addition of a conventional glucose-lowering agent.
Table 2.
Effects of weight-loss medications on glycemic control and the need for oral antidiabetes agents in people with type 2 diabetes
| Orlistat (163) | Lorcaserin (149) | Phentermine/ topiramate (164,165) | Naltrexone/ bupropion (166) | Liraglutide 3 mg (167) | |
|---|---|---|---|---|---|
| Weight loss (%)
Drug
Placebo |
|||||
| 6.2 |
4.5 |
9.6 |
5.0 |
6.0 |
|
| 4.3 |
1.5 |
2.6 |
1.8 |
2.0 |
|
| Initial A1C (%) |
8.1 |
8.1 |
8.6 |
8.0 |
8.0 |
| A1C change (%)
Drug
Placebo |
|||||
| −0.3 |
−0.9 |
−1.6 |
−0.6 |
? |
|
| +0.2 |
−0.4 |
−1.2 |
−0.1 |
? |
|
| Patients reaching an A1C ≤7% (%)
Drug
Placebo |
|||||
| ? |
50.4 |
53 |
44 |
69 |
|
| ? |
26.3 |
40 |
26 |
27 |
|
| Need for oral antidiabetes agents | ↓ | ↓ | ↓ | ↓ | ? |
Unanswered Questions
The most pressing unanswered question with regard to obesity pharmacotherapies is how well they perform in the long term. For the newest medications, we only have 2-year data. More must be learned about the optimal management of obesity over a lifetime and whether combination therapy may be a viable option. Clarification is needed on the efficacy of weight loss as a primary intervention for specific complications and the dose-response relationships between weight loss and meaningful improvements in those complications. Because obesity medications are adjunctive to lifestyle intervention, we must also refine our understanding of best practices for such interventions. This will give people with obesity, health care providers, and third-party payers a clearer idea of what can be expected from lifestyle programs. We also lack data and experience regarding lifestyle and pharmacological intervention in the rapidly growing population of elderly people with obesity. Answers to these questions will be needed to build a health-economic case for the medical treatment of obesity.
Finally, there remain numerous headwinds against the widespread uptake of available weight-loss medications. People with obesity face the prevailing attitude that their condition is a lifestyle choice rather than a disease. This attitude pervades not only the general public but also the health care professions, in part because of the lack of obesity training in medical schools and other health care academic programs. In addition, the history of failed obesity drugs has left many patients and providers reluctant to initiate even newer therapies. The need for lifestyle intervention also makes adoption of these therapies less appealing, both to primary care providers, who often have no local intervention programs available, and to patients, who may have to absorb the time and financial costs of participating in these programs. Insurance coverage for obesity medications and lifestyle interventions continues to be problematic. In addition, health care providers and their patients with obesity, who often are already taking multiple medications, may be reluctant to add to existing out-of-pocket costs and psychological “tablet burden” with yet another prescription.
One final key factor hindering the acceptance of obesity drugs is the lack of a widely accepted, medically meaningful, actionable diagnosis of obesity. Toward this end, an American Association of Clinical Endocrinologists (AACE) consensus development panel on obesity recently proposed an advanced framework for a new diagnosis of obesity as a chronic disease (168,169). This proposed strategy offers a guide to diagnosis based on both an anthropometric measure of adiposity (BMI) and a clinical component that indicates the degree to which excess adiposity is adversely affecting the patient’s health (presence and severity of weight-related complications).
Bariatric Surgery Options and Outcomes
The rationale for bariatric surgery is straightforward: it is, for now, the most effective means of producing short- and long-term weight losses of ≥15% and, as such, has the most successful track record in inducing remission in comorbidities and improving survival rates, quality of life, and social functioning (170). However, surgery is invasive, carries risk and initial cost, and is currently reserved for people with severe obesity who have failed to respond adequately to all other available treatments. A 1991 National Institutes of Health consensus conference recommended criteria for selection of surgical candidates that included age 18–65 years, BMI >40.0 kg/m2 or >35.0 kg/m2 with obesity-related comorbidity, understanding of the lifelong consequences of surgery, abstinence from drugs and alcohol, and agreement to long-term follow-up (171). These criteria have persisted with some modifications, including their expansion to younger and older people and inclusion of some patients with a BMI <35.0 kg/m2, particularly those with type 2 diabetes (60).
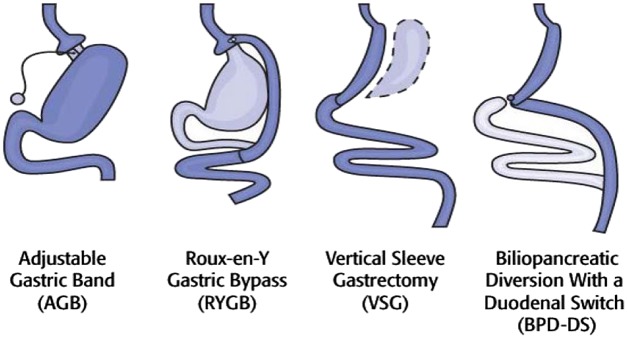
The four most common bariatric procedures are shown in Fig. 5 and have been described in detail elsewhere (170). All are now routinely performed laparoscopically. Adjustable gastric banding (AGB) is the simplest procedure and restricts intake by producing a very small gastric pouch above a band. Its primary benefits include low perioperative risk and adjustability, which enables both individual alteration of band tightness and reversibility (172). The Roux-en-Y gastric bypass (RYGB) produces a pouch similar in size to that of AGB and adds bypass of the stomach, duodenum, and proximal jejunum. This causes cessation of nutrient exposure to the mucosa of the bypassed upper GI tract, resulting in rapid entry of nutrients into the jejunum and a distal shifting of the site of digestion and nutrient absorption. The mechanism of action of RYGB is complex, involving multiple changes in gut hormone secretion and signaling, including a reduction in the release of ghrelin, a hormone that stimulates appetite and increased food intake; malabsorption of ingested energy-containing macronutrients may not be a factor (170). The vertical sleeve gastrectomy (VSG) reduces the size of the stomach by ∼85% and results in a reduction in ghrelin release (173). Its mechanism of action appears to involve altered GI gut hormone signaling, as gastric emptying increases after this procedure. VSG has become the most common bariatric surgical procedure in the U.S. because of its simplicity and lower perioperative incidence of complications compared with RYGB. Finally, the biliopancreatic diversion with a duodenal switch (BPD-DS) is a more complex, higher-risk procedure combining both restrictive (VSG) and malabsorptive (partial intestinal bypass) components (174). Although it may be superior to RYGB in long-term weight loss, direct comparative studies have been difficult to perform, and its associated short- and long-term complication rates have limited its acceptance in clinical practice (170,174).
Figure 5.
Bariatric surgical options. Image courtesy of Walter Pories, MD (East Carolina University, Greenville, NC).
Evidence for Efficacy: The Longitudinal Assessment of Bariatric Surgery Study
Only a few studies have reported outcomes for >2 years after surgery. Those that have were limited in generalizability, had generally poor retention, or included outdated procedures (175–180). To address this lack of long-term data in the U.S., the National Institute of Diabetes and Digestive and Kidney Diseases in 2003 formed the Longitudinal Assessment of Bariatric Surgery (LABS) Consortium to carry out a coordinated bariatric surgery research program (181). The LABS initiative aimed to assess the risks and benefits of bariatric surgery and identify predictors of optimal outcomes. It was divided into three phases: LABS-1 included all adults who had bariatric surgery performed by a certified surgeon at one of the six participating centers and evaluated short-term safety issues; LABS-2 is ongoing and evaluates the longer-term safety and efficacy of bariatric surgery; and LABS-3, also ongoing, focuses on the psychosocial aspects of obesity, quality of life, and possible mechanisms of surgery-induced diabetes remission (181).
Because of its detailed protocols and rigorous follow-up, the LABS initiative provides high-quality evidence regarding the efficacy of bariatric surgery and its effects on diabetes and other complications. Three-year weight-loss results from LABS-2 (182) (n = 2,458) showed a median loss of 41 kg for RYGB, corresponding to 31.5% of baseline weight. For AGB, these figures were 20 kg and 15.9%. Although weight loss was fairly uniform for 6 months, five distinct weight-loss trajectories later became apparent for each procedure and continued through 3 years. This phenomenon is in keeping with the highly variable weight loss reported with other treatments and emphasizes the importance of being able to stratify possible candidates by factors other than BMI.
Several observational studies have reported on weight loss ≥10 years after bariatric surgery (176,179,183). After RYGB, weight loss is rapid to a nadir exceeding a mean 30% by 18–24 months. Limited regain to a mean loss of ∼30% is followed by relatively stable weight over several years. Two randomized clinical trials have reported that weight loss after VSG is similar to, or somewhat less than, that after RYGB and superior to that after AGB (184,185). Weight loss after BPD-DS may be superior to that after RYGB, although the benefit of slightly greater weight loss with a greater risk for complications is uncertain.
Just as weight loss from RYGB was about twice that from AGB, so too were 3-year remission rates for obesity comorbidities, including diabetes, hypertension, and dyslipidemia (Table 3). Likewise, incidence rates of new comorbidities were all lower after RYGB than after AGB (182).
Table 3.
Three-year comorbidity responses in LABS-2 (182)
| Comorbidity | RYGB (%) | AGB (%) |
|---|---|---|
| Diabetes |
||
| Remission
Incidence |
61.9 |
37.1 |
| 0.9 |
3.2 |
|
| Hypertension |
||
| Remission
Incidence |
38.2 |
17.4 |
| 12.6 |
18.0 |
|
| Dyslipidemia |
||
| Remission Incidence | 61.9 |
27.1 |
| 3.2 | 16.0 |
The mechanisms explaining postsurgical remission of diabetes are not fully understood, although it does not appear to be caused by weight loss alone; in most cases, remission begins directly after surgery and before significant weight loss has occurred (186). Instead, this effect appears to be related to the degree to which food is excluded from the proximal gut (187,188). Gastric bypass has been shown to induce remission even in people with diabetes but not obesity (189). Recent LABS data for RYGB and AGB indicate that the incidence of remission progressively increases with increasing weight loss (190). The remission rate after RYGB was found to be superior to that after AGB, after controlling for weight loss. Thus, both use of RYGB and progressive weight loss are predictors of diabetes remission.
Safety Evidence
Concerns about the safety of bariatric surgery have become more widespread as these procedures have become more common. However, data from LABS-1 suggest that bariatric surgery is much safer now than it was 8–10 years ago (191). Longer-term complications and potential nutritional deficiencies associated with bariatric surgery have been recently reviewed elsewhere (60).
As with other obesity treatment modalities, unresolved issues related to bariatric surgery remain. Foremost is the need for improved methods of identifying appropriate surgery candidates. The ability to identify candidates on the basis of their physiological and personal characteristics rather than BMI alone would improve medical and quality-of-life outcomes by targeting surgical intervention to those most likely to accrue maximum benefit (192). Better understanding is needed of the variation in success rates and of the specific relationships between weight loss and changes in comorbidities. Strong evidence regarding preoperative predictors of success is also lacking.
Obesity Management Guidelines
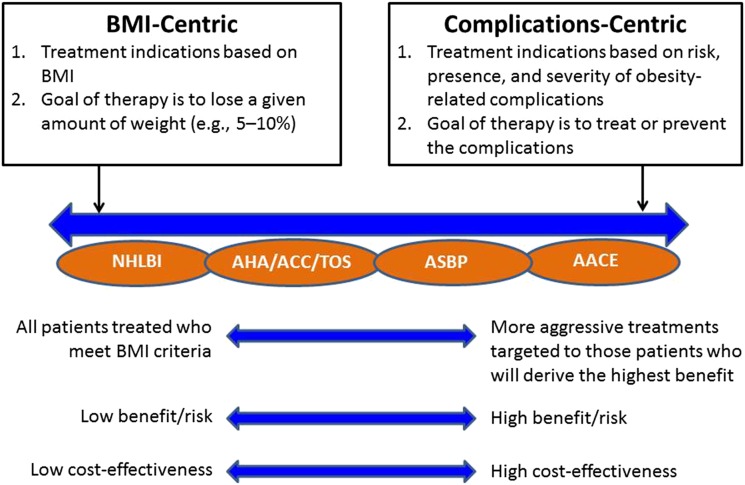
Recent decades have brought improvements in all three therapeutic modalities for obesity management: lifestyle interventions, medications, and bariatric surgery. The current challenge is to determine how best to use these tools, alone or in combination, balancing efficacy, safety, and costs. Toward that end, several organizations have developed recommendations to guide obesity treatment. Although all emphasize the health benefits of losing excess weight, these guidelines can be viewed as falling along a continuum from a more BMI-centric approach, with a goal of losing a given amount of weight, to a complications-centric model focused on preventing and treating complications (Fig. 6) (160).
Figure 6.
Spectrum of obesity guidelines.
The BMI-centric approach is best illustrated by the 1998 NHLBI guidelines (59), in which appropriate treatment is defined by baseline BMI, with patients having a BMI of 25.0–26.9 kg/m2 receiving dietary, physical activity, and behavior interventions and pharmacotherapy and surgery being added for those with progressively higher BMIs. Although this approach makes some allowances for comorbidities, it depends largely on BMI as the major determinant of appropriate treatment.
Two sets of guidelines—one from The Obesity Society (TOS), the American Heart Association (AHA), and the American College of Cardiology (ACC) (60) and the other from the American Society of Bariatric Physicians (ASBP) (193)—fall in the middle of the continuum. The TOS/AHA/ACC guidelines call for treatment for anyone with a BMI ≥25 kg/m2 but advise that treatment of complications should occur from the outset, regardless of patients’ weight-loss efforts. The ASBP obesity algorithm offers a hybrid approach that includes not only BMI, percentage of body fat, and waist circumference but also assessment of and treatment goals aimed at ameliorating the adverse health consequences of excess body fat.
Finally, there is the 2013 complications-centric approach developed by the AACE (155). In this model, weight loss becomes a therapeutic tool for the treatment of obesity-related complications, to a large extent independent of the degree of general adiposity or BMI. This approach targets more aggressive therapies to those who will derive the greatest benefits from weight loss—namely, those with weight-related complications—thereby optimizing benefit/risk outcomes and cost-effectiveness (160).
Treating Obesity as a Disease: Policy Implications and Future Directions
The past half-century has seen much progress in scientific discovery related to obesity and, to a lesser extent, the translation of this into advancements in management and prevention. Still, the obesity puzzle is far from complete. We have a mandate to fill in the gaps in our understanding of obesity, and there is some urgency to this mission given the high individual and societal costs involved.
Successfully managing and preventing obesity requires acknowledging obesity as a disease, as opposed to viewing it as the result of poor personal choices. Advances in our knowledge of homeostatic regulation of body weight, factors that impose obesity risk, biological resistance to weight loss in the presence of excess body weight, and the mechanisms by which excess weight drives metabolic, mechanical, and other comorbidities support a more modern view of people with obesity. Fifty years ago, it was widely assumed that preventing and reversing obesity would be a matter of education; once individuals knew what to eat and how to be physically active, they would lose weight and be cured. Clearly, this is not the case.
Although society as a whole does not yet universally acknowledge obesity as a disease, progress has been made among medical societies and policymakers. Chief among the medical societies is the American Medical Association, which passed a resolution in 2013 recognizing obesity and overweight as a chronic medical condition (de facto disease state) and urgent public health problem (194). The concept was also endorsed in a joint position statement of the medical professional societies most concerned with caring for patients with obesity (195). Obesity is also acknowledged as a chronic disease by the World Health Organization (196) and the U.S. Food and Drug Administration (FDA) (197).
The clinical practice guidelines discussed above will help to define best practices and an approach to obesity that is both more unified and more personalized to the needs of individual patients. In addition, the American Board of Obesity Medicine, established in 2011, now conducts annual credentialing examinations for physicians seeking certification of excellence in the practice of obesity medicine (198).
Several recent health policy initiatives are also encouraging. Among these are a 2012 Centers for Medicare & Medicaid Services decision to reimburse the costs of intensive behavioral intervention for obesity delivered by primary care providers (199) and a recent announcement that the Patient-Centered Outcomes Research Institute will provide substantial funding for research furthering obesity treatment in primary care settings (200). The FDA’s recent approval of four new medications to treat obesity has expanded therapeutic options, and coverage of these medications is now provided by more insurance payers, including the Federal Employees Health Benefits Program (201). Problems remain in terms of limitations on the amount of reimbursement allowed and the types of professionals who can provide them. In many cases, patients’ copayments remain prohibitive. Still, these are early positive developments that can and should be refined and improved over time.
Progress also has been made in addressing fraudulent claims by the manufacturers of commercial weight-loss products. Weight-loss products account for 13% of all Federal Trade Commission (FTC) fraud claims—more than twice that of any other category (202). The pervasive peddling of such spurious products minimizes the seriousness of obesity and undermines legitimate efforts of researchers to better understand and treat this disease. The FTC demonstrated commitment to the issue in imposing several fines in 2014, including a $46.5 million penalty on the makers of Sensa products (202).
Moving forward, we must better differentiate the therapies and initiatives aimed at obesity prevention from those targeting weight loss and those focused on weight-loss maintenance because the physiology, behavioral issues, and treatment goals of each are unique. For prevention, environmental defaults that promote a healthy lifestyle are important. Prevention must begin in the prenatal, neonatal, and early childhood periods when nutritional programming can affect chronic disease risk throughout life. Indeed, the origins of severe obesity in adulthood can be found in childhood. For weight-loss treatment, we will require better, more pragmatic models for delivering care in the primary care setting. Much more needs to be learned about the biology and psychology of weight-loss maintenance to develop more effective approaches.
Finally, more intensive public health campaigns and training opportunities are needed to better inform providers, industry representatives, insurers, regulators, policymakers, and the general public about the health impact of obesity and the need for medical management. Perpetuating the outdated view that obesity is simply a matter to be addressed by individuals choosing to eat less and exercise more does a disservice not only to the health care providers and researchers working to expand the evidence base for obesity treatment but also to people with obesity, whose very lives may depend on our collective resolve to take obesity seriously.
Successfully combating the obesity epidemic will involve not only research to address remaining questions regarding mechanisms, prevention, and treatment but also the concerted efforts of governmental agencies and public health policymakers; contributions from the pharmaceutical, medical device, and insurance industries; and, perhaps most important and most difficult to achieve, a shift in prevailing attitudes about obesity throughout society. In the twenty-first century, we all have an imperative: we must do this because our future health demands it.
Article Information
Acknowledgments. Writing and editing support services for this article were provided by Debbie Kendall of Kendall Editorial in Richmond, VA. The Editorial Committee recognizes that the work of the journal and contributions such as this Expert Forum would not be possible without the dedicated work and continued support from many individuals. Specifically, the planning, logistics, and funding of the meeting and the incredible editorial support would not have been possible without the tireless effort of Chris Kohler and his staff at the American Diabetes Association (ADA) publications office. In addition, the Editorial Committee thanks Lyn Reynolds and her staff in the ADA editorial office for support and Anne Gooch at the Pennington Biomedical Research Center for her valuable assistance in helping to organize the Expert Forum.
W.T.C. is supported in part by grant number 1-U54-GM-104940 from the National Institute of General Medical Sciences of the National Institutes of Health.
Duality of Interest. W.T.C. has served as a principal investigator on clinical studies awarded to his institution from AstraZeneca, GlaxoSmithKline, Janssen, Lexicon, and Sanofi. He has served as a consultant to Intarcia Therapeutics and Sanofi. G.A.B. is a speakers’ bureau member for Eisai, Novo Nordisk, and Takeda/VIVUS and is a consultant to Herbalife and Medifast. P.D.H. or institutions with which he is associated receive funding for his advisory, speaking, and research activities from AstraZeneca, Eli Lilly and Company, Janssen, Novo Nordisk, Sanofi, and companies with undeclared products in development in this area. W.T.G. is a stockholder in Bristol-Myers Squibb, Eli Lilly and Company, Isis Pharmaceuticals, Merck, Novartis, and Pfizer. He has served on advisory boards for AstraZeneca, Boehringer Ingelheim, Daiichi-Sankyo, Eisai, Janssen, LipoScience, Novo Nordisk, Takeda, and VIVUS. He has research support from AstraZeneca, Eisai, Lexicon, Merck, Pfizer, Sanofi, and Weight Watchers. S.K. is a stock shareholder in Aspire Bariatrics, Human Longevity, and MetroMidwest Biotech and sits on advisory boards for or serves as a consultant to Aspire Bariatrics, Danone-Yakult, Novo Nordisk, NuSi, and Takeda. F.X.P.-S. serves on advisory panels for Eli Lilly and Company, McNeil Specialty Products, Novo Nordisk, and Zafgen. F.B.H. has received research support from the California Walnut Commission and Metagenics. I.R. serves on advisory boards for AstraZeneca/Bristol-Myers Squibb, Eli Lilly and Company, LabStyle Innovations, Medscape, Merck Sharp & Dohme, Novo Nordisk, Orgenesis, Sanofi, and SmartZyme Innovation. He is a consultant to AstraZeneca/Bristol-Myers Squibb, FutuRx, Gili Medical, Insuline Medical, and Kamada. He is on the speakers’ bureau of AstraZeneca/Bristol-Myers Squibb, Eli Lilly and Company, Johnson & Johnson, Merck Sharp & Dohme, Novartis, Novo Nordisk, Sanofi, and Teva. He is a stock shareholder in GlucoMe, Insuline Medical, LabStyle Innovations, Orgenesis, and SmartZyme Innovation. L.V.G. has served on advisory boards or as a speaker for AstraZeneca, Boehringer Ingelheim, Eli Lilly and Company, Janssen, Johnson & Johnson, Merck/Merck Sharp & Dohme, Novo Nordisk, and Sanofi. He has received research support from the European Union (HEPADIP and Resolve Consortium) and from the National Research Funds of Belgium. B.M.W. serves as a consultant to EnteroMedics. D.H.R. has served on advisory panels or as a speaker for Medscape, Novo Nordisk, Pfizer, Real Appeal, Takeda, and VIVUS and as a consultant to Novo Nordisk and Scientific Intake. She is a stock shareholder in Scientific Intake and Tulip Medical. No other potential conflicts of interest relevant to this article were reported.
References
- 1.Fryar CD, Carroll MD, Ogden CL. Prevalence of overweight, obesity, and extreme obesity among adults: United States, trends 1960–1962 through 2009–2010 [Internet], 2012. National Center for Health Statistics. Available from http://www.cdc.gov/nchs/data/hestat/obesity_adult_09_10/obesity_adult_09_10.htm. Accessed 24 September 2014
- 2.Flegal KM, Carroll MD, Kuczmarski RJ, Johnson CL. Overweight and obesity in the United States: prevalence and trends, 1960-1994. Int J Obes Relat Metab Disord 1998;22:39–47 [DOI] [PubMed] [Google Scholar]
- 3.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011-2012. JAMA 2014;311:806–814 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization. Global Health Risks [Internet], 2009. Available from http://www.who.int/healthinfo/global_burden_disease/global_health_risks/en. Accessed 24 September 2014
- 5.Trust for America’s Health and Robert Wood Johnson Foundation F as in Fat: How Obesity Threatens America’s Future. Washington, DC, Trust for America’s Health, 2012 [Google Scholar]
- 6.Centers for Disease Control and Prevention. Long-term trends in diabetes [Internet], 2014. Available from http://www.cdc.gov/diabetes/statistics/slides/long_term_trends.pdf. Accessed 24 September 2014
- 7.Centers for Disease Control and Prevention. National diabetes statistics report: estimates of diabetes and its burden in the United States, 2014 [Internet], 2014. Available from http://www.cdc.gov/diabetes/pubs/statsreport14/national-diabetes-report-web.pdf. Accessed 24 September 2014
- 8.Garrison RJ, Kannel WB, Stokes J 3rd, Castelli WP. Incidence and precursors of hypertension in young adults: the Framingham Offspring Study. Prev Med 1987;16:235–251 [DOI] [PubMed] [Google Scholar]
- 9.American Cancer Society. Cancer facts & figures, 2012 [Internet], 2012. Available from http://www.cancer.org/research/cancerfactsstatistics/cancerfactsfigures2012/. Accessed 24 September 2014 [Google Scholar]
- 10.Fontaine KR, Barofsky I. Obesity and health-related quality of life. Obes Rev 2001;2:173–182 [DOI] [PubMed] [Google Scholar]
- 11.Peeters A, Barendregt JJ, Willekens F, Mackenbach JP, Al Mamun A, Bonneux L; NEDCOM, the Netherlands Epidemiology and Demography Compression of Morbidity Research Group . Obesity in adulthood and its consequences for life expectancy: a life-table analysis. Ann Intern Med 2003;138:24–32 [DOI] [PubMed] [Google Scholar]
- 12.Cawley J, Meyerhoefer C. The medical care costs of obesity: an instrumental variables approach. J Health Econ 2012;31:219–230 [DOI] [PubMed] [Google Scholar]
- 13.Withrow D, Alter DA. The economic burden of obesity worldwide: a systematic review of the direct costs of obesity. Obes Rev 2011;12:131–141 [DOI] [PubMed] [Google Scholar]
- 14.Rudd Center for Food Policy & Obesity. Commodity policy and agricultural subsidies [Internet]. Available from http://yaleruddcenter.org/what_we_do.aspx?id=81. Accessed 29 September 2014
- 15.Lutter M, Nestler EJ. Homeostatic and hedonic signals interact in the regulation of food intake. J Nutr 2009;139:629–632 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Putnam J, Allshouse J, Kantor LS. U.S. per capita food supply trends: more calories, refined carbohydrates, and fats. FoodReview 2002;25:2–15 [Google Scholar]
- 17.Church TS, Thomas DM, Tudor-Locke C, et al. Trends over 5 decades in U.S. occupation-related physical activity and their associations with obesity. PLoS ONE 2011;6:e19657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ladabaum U, Mannalithara A, Myer PA, Singh G. Obesity, abdominal obesity, physical activity, and caloric intake in US adults: 1988 to 2010. Am J Med 2014;127:717–727e12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.World Health Organization/Food and Agriculture Organization of the United Nations. Global and regional food consumption patterns and trends. In Diet, Nutrition and the Prevention of Chronic Diseases: Report of the Joint WHO/FAO Expert Consultation. Geneva, World Health Organization, 2003 (Tech. Rep. Ser., no. 916) p. 13–29 [Google Scholar]
- 20.Bray GA. From farm to fat cell: why aren’t we all fat? Metabolism 2015;64:349–353 [DOI] [PubMed] [Google Scholar]
- 21.Maes HH, Neale MC, Eaves LJ. Genetic and environmental factors in relative body weight and human adiposity. Behav Genet 1997;27:325–351 [DOI] [PubMed] [Google Scholar]
- 22.Fall T, Ingelsson E. Genome-wide association studies of obesity and metabolic syndrome. Mol Cell Endocrinol 2014;382:740–757 [DOI] [PubMed] [Google Scholar]
- 23.Speliotes EK, Willer CJ, Berndt SI, et al.; MAGIC; Procardis Consortium . Association analyses of 249,796 individuals reveal 18 new loci associated with body mass index. Nat Genet 2010;42:937–948 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zhang X, Qi Q, Zhang C, et al. FTO genotype and 2-year change in body composition and fat distribution in response to weight-loss diets: the POUNDS LOST Trial. Diabetes 2012;61:3005–3011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Herrera BM, Keildson S, Lindgren CM. Genetics and epigenetics of obesity. Maturitas 2011;69:41–49 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Godfrey KM, Sheppard A, Gluckman PD, et al. Epigenetic gene promoter methylation at birth is associated with child’s later adiposity. Diabetes 2011;60:1528–1534 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Christakis NA, Fowler JH. The spread of obesity in a large social network over 32 years. N Engl J Med 2007;357:370–379 [DOI] [PubMed] [Google Scholar]
- 28.Halberg N, Wernstedt-Asterholm I, Scherer PE. The adipocyte as an endocrine cell. Endocrinol Metab Clin North Am 2008;37:753–768 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Greenberg AS, Obin MS. Obesity and the role of adipose tissue in inflammation and metabolism. Am J Clin Nutr 2006;83(Suppl.):461S–465S [DOI] [PubMed] [Google Scholar]
- 30.Lenard NR, Berthoud H-R. Central and peripheral regulation of food intake and physical activity: pathways and genes. Obesity (Silver Spring) 2008;16(Suppl. 3):S11–S22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hardy OT, Czech MP, Corvera S. What causes the insulin resistance underlying obesity? Curr Opin Endocrinol Diabetes Obes 2012;19:81–87 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sweeney TE, Morton JM. The human gut microbiome: a review of the effect of obesity and surgically induced weight loss. JAMA Surg 2013;148:563–569 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Phillips CM. Metabolically healthy obesity: definitions, determinants and clinical implications. Rev Endocr Metab Disord 2013;14:219–227 [DOI] [PubMed] [Google Scholar]
- 34.Phillips CM, Dillon C, Harrington JM, et al. Defining metabolically healthy obesity: role of dietary and lifestyle factors. PLoS ONE 2013;8:e76188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wildman RP, Muntner P, Reynolds K, et al. The obese without cardiometabolic risk factor clustering and the normal weight with cardiometabolic risk factor clustering: prevalence and correlates of 2 phenotypes among the US population (NHANES 1999-2004). Arch Intern Med 2008;168:1617–1624 [DOI] [PubMed] [Google Scholar]
- 36.Kramer CK, Zinman B, Retnakaran R. Are metabolically healthy overweight and obesity benign conditions?: A systematic review and meta-analysis. Ann Intern Med 2013;159:758–769 [DOI] [PubMed] [Google Scholar]
- 37.Garrison RJ, Castelli WP. Weight and thirty-year mortality of men in the Framingham Study. Ann Intern Med 1985;103:1006–1009 [DOI] [PubMed] [Google Scholar]
- 38.Hamer M, Stamatakis E. Metabolically healthy obesity and risk of all-cause and cardiovascular disease mortality. J Clin Endocrinol Metab 2012;97:2482–2488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hwang L-C, Bai C-H, Sun C-A, Chen C-J. Prevalence of metabolically healthy obesity and its impacts on incidences of hypertension, diabetes and the metabolic syndrome in Taiwan. Asia Pac J Clin Nutr 2012;21:227–233 [PubMed] [Google Scholar]
- 40.Chang Y, Kim B-K, Yun KE, et al. Metabolically-healthy obesity and coronary artery calcification. J Am Coll Cardiol 2014;63:2679–2686 [DOI] [PubMed] [Google Scholar]
- 41.Appleton SL, Seaborn CJ, Visvanathan R, et al.; North West Adelaide Health Study Team . Diabetes and cardiovascular disease outcomes in the metabolically healthy obese phenotype: a cohort study. Diabetes Care 2013;36:2388–2394 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Fabbrini E, Yoshino J, Yoshino M, et al. Metabolically normal obese people are protected from adverse effects following weight gain. J Clin Invest 2015;125:787–795 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Korenblat KM, Fabbrini E, Mohammed BS, Klein S. Liver, muscle, and adipose tissue insulin action is directly related to intrahepatic triglyceride content in obese subjects. Gastroenterology 2008;134:1369–1375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lambert JE, Ramos-Roman MA, Browning JD, Parks EJ. Increased de novo lipogenesis is a distinct characteristic of individuals with nonalcoholic fatty liver disease. Gastroenterology 2014;146:726–735 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Fabbrini E, Mohammed BS, Magkos F, Korenblat KM, Patterson BW, Klein S. Alterations in adipose tissue and hepatic lipid kinetics in obese men and women with nonalcoholic fatty liver disease. Gastroenterology 2008;134:424–431 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Boden G. Fatty acid-induced inflammation and insulin resistance in skeletal muscle and liver. Curr Diab Rep 2006;6:177–181 [DOI] [PubMed] [Google Scholar]
- 47.Boden G, Chen X, Ruiz J, White JV, Rossetti L. Mechanisms of fatty acid-induced inhibition of glucose uptake. J Clin Invest 1994;93:2438–2446 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Fabbrini E, Magkos F, Mohammed BS, et al. Intrahepatic fat, not visceral fat, is linked with metabolic complications of obesity. Proc Natl Acad Sci USA 2009;106:15430–15435 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Herman MA, Peroni OD, Villoria J, et al. A novel ChREBP isoform in adipose tissue regulates systemic glucose metabolism. Nature 2012;484:333–338 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Graham TE, Kahn BB. Tissue-specific alterations of glucose transport and molecular mechanisms of intertissue communication in obesity and type 2 diabetes. Horm Metab Res 2007;39:717–721 [DOI] [PubMed] [Google Scholar]
- 51.Kursawe R, Eszlinger M, Narayan D, et al. Cellularity and adipogenic profile of the abdominal subcutaneous adipose tissue from obese adolescents: association with insulin resistance and hepatic steatosis. Diabetes 2010;59:2288–2296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Sun K, Kusminski CM, Scherer PE. Adipose tissue remodeling and obesity. J Clin Invest 2011;121:2094–2101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Lumeng CN, Saltiel AR. Inflammatory links between obesity and metabolic disease. J Clin Invest 2011;121:2111–2117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Khan MT, Nieuwdorp M, Bäckhed F. Microbial modulation of insulin sensitivity. Cell Metab 2014;20:753–760 [DOI] [PubMed] [Google Scholar]
- 55.Karlsson FH, Tremaroli V, Nookaew I, et al. Gut metagenome in European women with normal, impaired and diabetic glucose control. Nature 2013;498:99–103 [DOI] [PubMed] [Google Scholar]
- 56.Vrieze A, Van Nood E, Holleman F, et al. Transfer of intestinal microbiota from lean donors increases insulin sensitivity in individuals with metabolic syndrome. Gastroenterology 2012;143:913–916 [DOI] [PubMed] [Google Scholar]
- 57.Parlevliet ET, Coomans CP, Rensen PC, Romijn JA. The brain modulates insulin sensitivity in multiple tissues. Front Horm Res 2014;42:50–58 [DOI] [PubMed] [Google Scholar]
- 58.Ogden CL, Yanovski SZ, Carroll MD, Flegal KM. The epidemiology of obesity. Gastroenterology 2007;132:2087–2102 [DOI] [PubMed] [Google Scholar]
- 59.National Heart, Lung, and Blood Institute Obesity Education Initiative Expert Panel on the Identification, Evaluation, and Treatment of Obesity in Adults. Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults: the evidence report. National Heart, Lung, and Blood Institute, 1998 (report no. 98-4083) [Google Scholar]
- 60.Jensen MD, Ryan DH, Apovian CM, et al. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. J Am Coll Cardiol 2014;63(25 Pt B):2985–3023 [DOI] [PubMed] [Google Scholar]
- 61.Chang A, Van Horn L, Jacobs DR Jr, et al. Lifestyle-related factors, obesity, and incident microalbuminuria: the CARDIA (Coronary Artery Risk Development in Young Adults) study. Am J Kidney Dis 2013;62:267–275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.van Leiden HA, Dekker JM, Moll AC, et al. Blood pressure, lipids, and obesity are associated with retinopathy: the Hoorn Study. Diabetes Care 2002;25:1320–1325 [DOI] [PubMed] [Google Scholar]
- 63.Diabetes Prevention Program Research Group 10-year follow-up of diabetes incidence and weight loss in the Diabetes Prevention Program Outcomes Study. Lancet 2009;374:1677–1686 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Garvey WT, Ryan DH, Henry R, et al. Prevention of type 2 diabetes in subjects with prediabetes and metabolic syndrome treated with phentermine and topiramate extended release. Diabetes Care 2014;37:912–921 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Wing RR, Lang W, Wadden TA, et al.; Look AHEAD Research Group . Benefits of modest weight loss in improving cardiovascular risk factors in overweight and obese individuals with type 2 diabetes. Diabetes Care 2011;34:1481–1486 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Assy N, Hussein O, Abassi Z. Weight loss induced by orlistat reverses fatty infiltration and improves hepatic fibrosis in obese patients with non-alcoholic steatohepatitis. Gut 2007;56:443–444 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Dixon JB, Bhathal PS, Hughes NR, O’Brien PE. Nonalcoholic fatty liver disease: improvement in liver histological analysis with weight loss. Hepatology 2004;39:1647–1654 [DOI] [PubMed] [Google Scholar]
- 68.Patel AA, Torres DM, Harrison SA. Effect of weight loss on nonalcoholic fatty liver disease. J Clin Gastroenterol 2009;43:970–974 [DOI] [PubMed] [Google Scholar]
- 69.Foster GD, Borradaile KE, Sanders MH, et al.; Sleep AHEAD Research Group of Look AHEAD Research Group . A randomized study on the effect of weight loss on obstructive sleep apnea among obese patients with type 2 diabetes: the Sleep AHEAD study. Arch Intern Med 2009;169:1619–1626 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Winslow DH, Bowden CH, DiDonato KP, McCullough PA. A randomized, double-blind, placebo-controlled study of an oral, extended-release formulation of phentermine/topiramate for the treatment of obstructive sleep apnea in obese adults. Sleep 2012;35:1529–1539 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Christensen R, Bartels EM, Astrup A, Bliddal H. Effect of weight reduction in obese patients diagnosed with knee osteoarthritis: a systematic review and meta-analysis. Ann Rheum Dis 2007;66:433–439 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Felson DT, Zhang Y, Anthony JM, Naimark A, Anderson JJ. Weight loss reduces the risk for symptomatic knee osteoarthritis in women. the Framingham Study. Ann Intern Med 1992;116:535–539 [DOI] [PubMed] [Google Scholar]
- 73.Aaboe J, Bliddal H, Messier SP, Alkjær T, Henriksen M. Effects of an intensive weight loss program on knee joint loading in obese adults with knee osteoarthritis. Osteoarthritis Cartilage 2011;19:822–828 [DOI] [PubMed] [Google Scholar]
- 74.Burgio KL, Richter HE, Clements RH, Redden DT, Goode PS. Changes in urinary and fecal incontinence symptoms with weight loss surgery in morbidly obese women. Obstet Gynecol 2007;110:1034–1040 [DOI] [PubMed] [Google Scholar]
- 75.Subak LL, Wing R, West DS, et al.; PRIDE Investigators . Weight loss to treat urinary incontinence in overweight and obese women. N Engl J Med 2009;360:481–490 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Singh M, Lee J, Gupta N, et al. Weight loss can lead to resolution of gastroesophageal reflux disease symptoms: a prospective intervention trial. Obesity (Silver Spring) 2013;21:284–290 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Tutuian R. Obesity and GERD: pathophysiology and effect of bariatric surgery. Curr Gastroenterol Rep 2011;13:205–212 [DOI] [PubMed] [Google Scholar]
- 78.Panidis D, Farmakiotis D, Rousso D, Kourtis A, Katsikis I, Krassas G. Obesity, weight loss, and the polycystic ovary syndrome: effect of treatment with diet and orlistat for 24 weeks on insulin resistance and androgen levels. Fertil Steril 2008;89:899–906 [DOI] [PubMed] [Google Scholar]
- 79.Norman RJ, Davies MJ, Lord J, Moran LJ. The role of lifestyle modification in polycystic ovary syndrome. Trends Endocrinol Metab 2002;13:251–257 [DOI] [PubMed] [Google Scholar]
- 80.Moran LJ, Ko H, Misso M, et al. Dietary composition in the treatment of polycystic ovary syndrome: a systematic review to inform evidence-based guidelines. J Acad Nutr Diet 2013;113:520–545 [DOI] [PubMed] [Google Scholar]
- 81.Prospective Studies Collaboration Body-mass index and cause-specific mortality in 900 000 adults: collaborative analyses of 57 prospective studies. Lancet 2009;373:1083–1096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Berrington de Gonzalez A, Hartge P, Cerhan JR, et al. Body-mass index and mortality among 1.46 million white adults. N Engl J Med 2010;363:2211–2219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Fontaine KR, Redden DT, Wang C, Westfall AO, Allison DB. Years of life lost due to obesity. JAMA 2003;289:187–193 [DOI] [PubMed] [Google Scholar]
- 84.Dorn JM, Schisterman EF, Winkelstein W Jr, Trevisan M. Body mass index and mortality in a general population sample of men and women. The Buffalo Health Study. Am J Epidemiol 1997;146:919–931 [DOI] [PubMed] [Google Scholar]
- 85.McGee DL; Diverse Populations Collaboration . Body mass index and mortality: a meta-analysis based on person-level data from twenty-six observational studies. Ann Epidemiol 2005;15:87–97 [DOI] [PubMed] [Google Scholar]
- 86.Flegal KM, Graubard BI, Williamson DF, Gail MH. Excess deaths associated with underweight, overweight, and obesity. JAMA 2005;293:1861–1867 [DOI] [PubMed] [Google Scholar]
- 87.Willett WC, Hu FB, Thun M. Overweight, obesity, and all-cause mortality. JAMA 2013;309:1681. [DOI] [PubMed] [Google Scholar]
- 88.Flegal KM, Kit BK, Orpana H, Graubard BI. Association of all-cause mortality with overweight and obesity using standard body mass index categories: a systematic review and meta-analysis. JAMA 2013;309:71–82 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Tobias DK, Hu FB. Does being overweight really reduce mortality? Obesity (Silver Spring) 2013;21:1746–1749 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Sjöström L, Narbro K, Sjöström CD, et al.; Swedish Obese Subjects Study . Effects of bariatric surgery on mortality in Swedish obese subjects. N Engl J Med 2007;357:741–752 [DOI] [PubMed] [Google Scholar]
- 91.Sjöström L, Peltonen M, Jacobson P, et al. Bariatric surgery and long-term cardiovascular events. JAMA 2012;307:56–65 [DOI] [PubMed] [Google Scholar]
- 92.Uusitupa M, Peltonen M, Lindström J, et al.; Finnish Diabetes Prevention Study Group . Ten-year mortality and cardiovascular morbidity in the Finnish Diabetes Prevention Study—secondary analysis of the randomized trial. PLoS ONE 2009;4:e5656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Li G, Zhang P, Wang J, et al. The long-term effect of lifestyle interventions to prevent diabetes in the China Da Qing Diabetes Prevention Study: a 20-year follow-up study. Lancet 2008;371:1783–1789 [DOI] [PubMed] [Google Scholar]
- 94.Li G, Zhang P, Wang J, et al. Cardiovascular mortality, all-cause mortality, and diabetes incidence after lifestyle intervention for people with impaired glucose tolerance in the Da Qing Diabetes Prevention Study: a 23-year follow-up study. Lancet Diabetes Endocrinol 2014;2:474–480 [DOI] [PubMed] [Google Scholar]
- 95.Wing RR, Bolin P, Brancati FL, et al.; Look AHEAD Research Group . Cardiovascular effects of intensive lifestyle intervention in type 2 diabetes. N Engl J Med 2013;369:145–154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.National Heart, Lung, and Blood Institute, North American Association for the Study of Obesity. The practical guide: identification, evaluation, and treatment of overweight and obesity in adults. National Institutes of Health, 2000 (NIH publication no. 00-4084) [Google Scholar]
- 97.Knowler WC, Barrett-Connor E, Fowler SE, et al.; Diabetes Prevention Program Research Group . Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med 2002;346:393–403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Ryan DH, Espeland MA, Foster GD, et al.; Look AHEAD Research Group . Look AHEAD (Action for Health in Diabetes): design and methods for a clinical trial of weight loss for the prevention of cardiovascular disease in type 2 diabetes. Control Clin Trials 2003;24:610–628 [DOI] [PubMed] [Google Scholar]
- 99.Look AHEAD Research Group Eight-year weight losses with an intensive lifestyle intervention: the look AHEAD study. Obesity (Silver Spring) 2014;22:5–13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Pi-Sunyer X, Blackburn G, Brancati FL, et al.; Look AHEAD Research Group . Reduction in weight and cardiovascular disease risk factors in individuals with type 2 diabetes: one-year results of the look AHEAD trial. Diabetes Care 2007;30:1374–1383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Wing RR, Hamman RF, Bray GA, et al.; Diabetes Prevention Program Research Group . Achieving weight and activity goals among diabetes prevention program lifestyle participants. Obes Res 2004;12:1426–1434 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Ackermann RT, Finch EA, Brizendine E, Zhou H, Marrero DG. Translating the Diabetes Prevention Program into the community: the DEPLOY pilot study. Am J Prev Med 2008;35:357–363 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Perri MG. Effects of behavioral treatment on long-term weight loss: lessons learned from the look AHEAD trial. Obesity (Silver Spring) 2014;22:3–4 [DOI] [PubMed] [Google Scholar]
- 104.Delahanty LM, Nathan DM. Implications of the diabetes prevention program and Look AHEAD clinical trials for lifestyle interventions. J Am Diet Assoc 2008;108(Suppl. 1):S66–S72 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Albright AL, Gregg EW. Preventing type 2 diabetes in communities across the U.S.: the National Diabetes Prevention Program. Am J Prev Med 2013;44(Suppl. 4):S346–S351 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Ratner RE; Diabetes Prevention Program Research . An update on the Diabetes Prevention Program. Endocr Pract 2006;12(Suppl. 1):20–24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Wadden TA, Neiberg RH, Wing RR, et al.; Look AHEAD Research Group . Four-year weight losses in the Look AHEAD study: factors associated with long-term success. Obesity (Silver Spring) 2011;19:1987–1998 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Wing RR, Phelan S. Long-term weight loss maintenance. Am J Clin Nutr 2005;82(Suppl.):222S–225S [DOI] [PubMed] [Google Scholar]
- 109.Jakicic JM, Winters C, Lang W, Wing RR. Effects of intermittent exercise and use of home exercise equipment on adherence, weight loss, and fitness in overweight women: a randomized trial. JAMA 1999;282:1554–1560 [DOI] [PubMed] [Google Scholar]
- 110.UK Prospective Diabetes Study (UKPDS) Group Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet 1998;352:837–853 [PubMed] [Google Scholar]
- 111.UK Prospective Diabetes Study (UKPDS) Group Effect of intensive blood-glucose control with metformin on complications in overweight patients with type 2 diabetes (UKPDS 34). Lancet 1998;352:854–865 [PubMed] [Google Scholar]
- 112.Kahn SE, Haffner SM, Heise MA, et al.; ADOPT Study Group . Glycemic durability of rosiglitazone, metformin, or glyburide monotherapy. N Engl J Med 2006;355:2427–2443 [DOI] [PubMed] [Google Scholar]
- 113.Gerstein HC, Bosch J, Dagenais GR, et al.; ORIGIN Trial Investigators . Basal insulin and cardiovascular and other outcomes in dysglycemia. N Engl J Med 2012;367:319–328 [DOI] [PubMed] [Google Scholar]
- 114.van Dieren S, Czernichow S, Chalmers J, et al. Weight changes and their predictors amongst 11 140 patients with type 2 diabetes in the ADVANCE trial. Diabetes Obes Metab 2012;14:464–469 [DOI] [PubMed] [Google Scholar]
- 115.Balkau B, Home PD, Vincent M, Marre M, Freemantle N. Factors associated with weight gain in people with type 2 diabetes starting on insulin. Diabetes Care 2014;37:2108–2113 [DOI] [PubMed] [Google Scholar]
- 116.Stimson RH, Walker BR. Glucocorticoids and 11beta-hydroxysteroid dehydrogenase type 1 in obesity and the metabolic syndrome. Minerva Endocrinol 2007;32:141–159 [PubMed] [Google Scholar]
- 117.Sharma AM, Pischon T, Hardt S, Kunz I, Luft FC. Hypothesis: β-adrenergic receptor blockers and weight gain: a systematic analysis. Hypertension 2001;37:250–254 [DOI] [PubMed] [Google Scholar]
- 118.DeToledo JC, Toledo C, DeCerce J, Ramsay RE. Changes in body weight with chronic, high-dose gabapentin therapy. Ther Drug Monit 1997;19:394–396 [DOI] [PubMed] [Google Scholar]
- 119.Tschoner A, Engl J, Laimer M, et al. Metabolic side effects of antipsychotic medication. Int J Clin Pract 2007;61:1356–1370 [DOI] [PubMed] [Google Scholar]
- 120.Stricker RB, Goldberg B. Weight gain associated with protease inhibitor therapy in HIV-infected patients. Res Virol 1998;149:123–126 [DOI] [PubMed] [Google Scholar]
- 121.Inzucchi SE, Bergenstal RM, Buse JB, et al. Management of hyperglycemia in type 2 diabetes: a patient-centered approach: position statement of the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care 2012;35:1364–1379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Inzucchi SE, Bergenstal RM, Buse JB, et al. Management of hyperglycemia in type 2 diabetes, 2015: a patient-centered approach: update to a position statement of the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes Care 2015;38:140–149 [DOI] [PubMed] [Google Scholar]
- 123.Scheen AJ, Van Gaal LF. Combating the dual burden: therapeutic targeting of common pathways in obesity and type 2 diabetes. Lancet Diabetes Endocrinol 2014;2:911–922 [DOI] [PubMed] [Google Scholar]
- 124.Cornell S. Differentiating among incretin therapies: a multiple-target approach to type 2 diabetes. J Clin Pharm Ther 2012;37:510–524 [DOI] [PubMed] [Google Scholar]
- 125.DeFronzo RA, Ratner RE, Han J, Kim DD, Fineman MS, Baron AD. Effects of exenatide (exendin-4) on glycemic control and weight over 30 weeks in metformin-treated patients with type 2 diabetes. Diabetes Care 2005;28:1092–1100 [DOI] [PubMed] [Google Scholar]
- 126.Buse JB, Rosenstock J, Sesti G, et al.; LEAD-6 Study Group . Liraglutide once a day versus exenatide twice a day for type 2 diabetes: a 26-week randomised, parallel-group, multinational, open-label trial (LEAD-6). Lancet 2009;374:39–47 [DOI] [PubMed] [Google Scholar]
- 127.Van Gaal L, Scheen A. Weight management in type 2 diabetes: current and emerging approaches to treatment. Diabetes Care 2015;38:1161–1172 [DOI] [PubMed] [Google Scholar]
- 128.Bolinder J, Ljunggren Ö, Kullberg J, et al. Effects of dapagliflozin on body weight, total fat mass, and regional adipose tissue distribution in patients with type 2 diabetes mellitus with inadequate glycemic control on metformin. J Clin Endocrinol Metab 2012;97:1020–1031 [DOI] [PubMed] [Google Scholar]
- 129.Bays HE, Weinstein R, Law G, Canovatchel W. Canagliflozin: effects in overweight and obese subjects without diabetes mellitus. Obesity (Silver Spring) 2014;22:1042–1049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Buse JB, Bergenstal RM, Glass LC, et al. Use of twice-daily exenatide in basal insulin-treated patients with type 2 diabetes: a randomized, controlled trial. Ann Intern Med 2011;154:103–112 [DOI] [PubMed] [Google Scholar]
- 131.Riddle MC, Aronson R, Home P, et al. Adding once-daily lixisenatide for type 2 diabetes inadequately controlled by established basal insulin: a 24-week, randomized, placebo-controlled comparison (GetGoal-L). Diabetes Care 2013;36:2489–2496 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Rosenstock J, Fonseca VA, Gross JL, et al.; Harmony 6 Study Group . Advancing basal insulin replacement in type 2 diabetes inadequately controlled with insulin glargine plus oral agents: a comparison of adding albiglutide, a weekly GLP-1 receptor agonist, versus thrice-daily prandial insulin lispro. Diabetes Care 2014;37:2317–2325 [DOI] [PubMed] [Google Scholar]
- 133.Gough SC, Bode B, Woo V, et al.; NN9068-3697 (DUAL-I) trial investigators . Efficacy and safety of a fixed-ratio combination of insulin degludec and liraglutide (IDegLira) compared with its components given alone: results of a phase 3, open-label, randomised, 26-week, treat-to-target trial in insulin-naive patients with type 2 diabetes. Lancet Diabetes Endocrinol 2014;2:885–893 [DOI] [PubMed] [Google Scholar]
- 134.Wilding JPH, Norwood P, T’joen C, Bastien A, List JF, Fiedorek FT. A study of dapagliflozin in patients with type 2 diabetes receiving high doses of insulin plus insulin sensitizers: applicability of a novel insulin-independent treatment. Diabetes Care 2009;32:1656–1662 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Kim GW, Lin JE, Blomain ES, Waldman SA. Antiobesity pharmacotherapy: new drugs and emerging targets. Clin Pharmacol Ther 2014;95:53–66 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.U.S. Food and Drug Administration. FDA announces withdrawal fenfluramine and dexfenfluramine (fen-phen) [Internet], 15 September 1997. Available from http://www.fda.gov/Drugs/DrugSafety/PostmarketDrugSafetyInformationforPatientsandProviders/ucm179871.htm. Accessed 17 December 2014
- 137.U.S. Food and Drug Administration. Meridia (sibutramine): market withdrawal due to risk of serious cardiovascular events [Internet], 8 October 2010. Available from http://www.fda.gov/Safety/MedWatch/SafetyInformation/SafetyAlertsforHumanMedicalProducts/ucm228830.htm. Accessed 17 December 2014
- 138.European Medicines Agency. Public statement on Acomplia (rimonabant): withdrawal of the marketing authorisation in the European Union [Internet], 30 January 2009. Available from http://www.ema.europa.eu/docs/en_GB/document_library/Public_statement/2009/11/WC500012189.pdf. Accessed 17 December 2014
- 139.Zhi J, Melia AT, Guerciolini R, et al. Retrospective population-based analysis of the dose-response (fecal fat excretion) relationship of orlistat in normal and obese volunteers. Clin Pharmacol Ther 1994;56:82–85 [DOI] [PubMed] [Google Scholar]
- 140.U.S. Food and Drug Administration. FDA approves weight-management drug Qsymia [Internet], 17 July 2012. Available from http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm312468.htm. Accessed 17 December 2014
- 141.U.S. Food and Drug Administration. FDA approves Belviq to treat some overweight or obese adults [Internet], 27 June 2012. Available from http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm309993.htm. Accessed 17 December 2014
- 142.U.S. Food and Drug Administration. FDA approves weight-management drug Contrave [Internet], 10 September 2014. Available from http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm413896.htm. Accessed 17 December 2014
- 143.U.S. Food and Drug Administration. FDA approves weight-management drug Saxenda [Internet], 23 December 2014. Available from http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm427913.htm. Accessed 9 February 2015
- 144.Torgerson JS, Hauptman J, Boldrin MN, Sjöström L. XENical in the prevention of diabetes in obese subjects (XENDOS) study: a randomized study of orlistat as an adjunct to lifestyle changes for the prevention of type 2 diabetes in obese patients. Diabetes Care 2004;27:155–161 [DOI] [PubMed] [Google Scholar]
- 145.Allison DB, Gadde KM, Garvey WT, et al. Controlled-release phentermine/topiramate in severely obese adults: a randomized controlled trial (EQUIP). Obesity (Silver Spring) 2012;20:330–342 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Gadde KM, Allison DB, Ryan DH, et al. Effects of low-dose, controlled-release, phentermine plus topiramate combination on weight and associated comorbidities in overweight and obese adults (CONQUER): a randomised, placebo-controlled, phase 3 trial. Lancet 2011;377:1341–1352 [DOI] [PubMed] [Google Scholar]
- 147.Garvey WT, Ryan DH, Look M, et al. Two-year sustained weight loss and metabolic benefits with controlled-release phentermine/topiramate in obese and overweight adults (SEQUEL): a randomized, placebo-controlled, phase 3 extension study. Am J Clin Nutr 2012;95:297–308 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Fidler MC, Sanchez M, Raether B, et al.; BLOSSOM Clinical Trial Group . A one-year randomized trial of lorcaserin for weight loss in obese and overweight adults: the BLOSSOM trial. J Clin Endocrinol Metab 2011;96:3067–3077 [DOI] [PubMed] [Google Scholar]
- 149.Smith SR, Weissman NJ, Anderson CM, et al.; Behavioral Modification and Lorcaserin for Overweight and Obesity Management (BLOOM) Study Group . Multicenter, placebo-controlled trial of lorcaserin for weight management. N Engl J Med 2010;363:245–256 [DOI] [PubMed] [Google Scholar]
- 150.O’Neil PM, Smith SR, Weissman NJ, et al. Randomized placebo-controlled clinical trial of lorcaserin for weight loss in type 2 diabetes mellitus: the BLOOM-DM study. Obesity (Silver Spring) 2012;20:1426–1436 [DOI] [PubMed] [Google Scholar]
- 151.Greenway FL, Fujioka K, Plodkowski RA, et al.; COR-I Study Group . Effect of naltrexone plus bupropion on weight loss in overweight and obese adults (COR-I): a multicentre, randomised, double-blind, placebo-controlled, phase 3 trial. Lancet 2010;376:595–605 [DOI] [PubMed] [Google Scholar]
- 152.Apovian CM, Aronne L, Rubino D, et al.; COR-II Study Group . A randomized, phase 3 trial of naltrexone SR/bupropion SR on weight and obesity-related risk factors (COR-II). Obesity (Silver Spring) 2013;21:935–943 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Wadden TA, Hollander P, Klein S, et al.; NN8022-1923 Investigators . Weight maintenance and additional weight loss with liraglutide after low-calorie-diet-induced weight loss: the SCALE Maintenance randomized study. Int J Obes (Lond) 2013;37:1443–1451 [DOI] [PubMed] [Google Scholar]
- 154.Astrup A, Carraro R, Finer N, et al.; NN8022-1807 Investigators . Safety, tolerability and sustained weight loss over 2 years with the once-daily human GLP-1 analog, liraglutide. Int J Obes (Lond) 2012;36:843–854 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Garber AJ, Abrahamson MJ, Barzilay JI, et al.; American Association of Clinical Endocrinologists . AACE comprehensive diabetes management algorithm 2013. Endocr Pract 2013;19:327–336 [DOI] [PubMed] [Google Scholar]
- 156.VIVUS. Qsymia prescribing information [Internet], 2014. Available from https://www.qsymia.com/pdf/prescribing-information.pdf. Accessed 17 December 2014
- 157.Eisai. Belviq prescribing information [Internet], 2012. Available from https://www.belviq.com/pdf/Belviq_Prescribing_information.pdf. Accessed 17 December 2014
- 158.Takeda Pharmaceuticals. CONTRAVE prescribing information [Internet], 2014. Available from http://general.takedapharm.com/content/file.aspx?filetypecode=CONTRAVEPI&cacheRandomizer=aaa3d519-2e84-4e5d-bb7a-5759af394a09. Accessed 17 December 2014
- 159.Novo Nordisk. Saxenda prescribing information [Internet], 2014. Available from http://novo-pi.nnittest.com/saxenda.pdf. Accessed 9 February 2015
- 160.Garvey WT. New tools for weight-loss therapy enable a more robust medical model for obesity treatment: rationale for a complications-centric approach. Endocr Pract 2013;19:864–874 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Aronne LJ, Wadden TA, Peterson C, Winslow D, Odeh S, Gadde KM. Evaluation of phentermine and topiramate versus phentermine/topiramate extended-release in obese adults. Obesity (Silver Spring) 2013;21:2163–2171 [DOI] [PubMed] [Google Scholar]
- 162.Munro JF, MacCuish AC, Wilson EM, Duncan LJP. Comparison of continuous and intermittent anorectic therapy in obesity. BMJ 1968;1:352–354 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Hollander PA, Elbein SC, Hirsch IB, et al. Role of orlistat in the treatment of obese patients with type 2 diabetes. A 1-year randomized double-blind study. Diabetes Care 1998;21:1288–1294 [DOI] [PubMed] [Google Scholar]
- 164.Garvey WT, Ryan DH, Bohannon NJV, et al. Weight-loss therapy in type 2 diabetes: effects of phentermine and topiramate extended release. Diabetes Care 2014;37:3309–3316 [DOI] [PubMed] [Google Scholar]
- 165.Garvey WT, Troupin B, Tam P, Najarian T, Peterson C, Day WW. One-year treatment with VI-0521 in type 2 diabetes demonstrates continued glycemic improvement and weight loss. Diabetes 2009;58(Suppl. 1):A95 [Google Scholar]
- 166.Hollander P, Gupta AK, Plodkowski R, et al.; COR-Diabetes Study Group . Effects of naltrexone sustained-release/bupropion sustained-release combination therapy on body weight and glycemic parameters in overweight and obese patients with type 2 diabetes. Diabetes Care 2013;36:4022–4029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Drugs.com. People with type 2 diabetes achieve 6% weight loss with liraglutide 3 mg in phase 3a obesity trial [Internet], 2013. Available from http://www.drugs.com/clinical_trials/type-2-diabetes-achieve-6-weight-loss-liraglutide-3-mg-phase-3a-obesity-trial-15264.html. Accessed 18 December 2014
- 168.Garvey WT, Garber AJ, Mechanick JI, et al.; on behalf of the AACE Obesity Scientific Committee . American Association of Clinical Endocrinologists and American College of Endocrinology consensus conference on obesity: building an evidence base for comprehensive action. Endocr Pract 2014;20:956–976 [DOI] [PubMed] [Google Scholar]
- 169.Garvey WT, Garber AJ, Mechanick JI, et al.; on behalf of the AACE Obesity Scientific Committee . American Association of Clinical Endocrinologists and American College of Endocrinology position statement on the 2014 advanced framework for a new diagnosis of obesity as a chronic disease. Endocr Pract 2014;20:977–989 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Pories WJ, Mehaffey JH, Staton KM. The surgical treatment of type two diabetes mellitus. Surg Clin North Am 2011;91:821–836, viii [DOI] [PubMed] [Google Scholar]
- 171.Consensus Development Conference Panel Gastrointestinal surgery for severe obesity. Ann Intern Med 1991;115:956–961 [PubMed] [Google Scholar]
- 172.Sultan S, Parikh M, Youn H, Kurian M, Fielding G, Ren C. Early U.S. outcomes after laparoscopic adjustable gastric banding in patients with a body mass index less than 35 kg/m2. Surg Endosc 2009;23:1569–1573 [DOI] [PubMed] [Google Scholar]
- 173.Langer FB, Reza Hoda MA, Bohdjalian A, et al. Sleeve gastrectomy and gastric banding: effects on plasma ghrelin levels. Obes Surg 2005;15:1024–1029 [DOI] [PubMed] [Google Scholar]
- 174.Hess DS, Hess DW. Biliopancreatic diversion with a duodenal switch. Obes Surg 1998;8:267–282 [DOI] [PubMed] [Google Scholar]
- 175.Buchwald H, Avidor Y, Braunwald E, et al. Bariatric surgery: a systematic review and meta-analysis. JAMA 2004;292:1724–1737 [DOI] [PubMed] [Google Scholar]
- 176.Pories WJ, Swanson MS, MacDonald KG, et al. Who would have thought it? An operation proves to be the most effective therapy for adult-onset diabetes mellitus. Ann Surg 1995;222:339–350; discussion 350–352 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Favretti F, Segato G, Ashton D, et al. Laparoscopic adjustable gastric banding in 1,791 consecutive obese patients: 12-year results. Obes Surg 2007;17:168–175 [DOI] [PubMed] [Google Scholar]
- 178.Higa K, Ho T, Tercero F, Yunus T, Boone KB. Laparoscopic Roux-en-Y gastric bypass: 10-year follow-up. Surg Obes Relat Dis 2011;7:516–525 [DOI] [PubMed] [Google Scholar]
- 179.Sjöström L, Lindroos A-K, Peltonen M, et al.; Swedish Obese Subjects Study Scientific Group . Lifestyle, diabetes, and cardiovascular risk factors 10 years after bariatric surgery. N Engl J Med 2004;351:2683–2693 [DOI] [PubMed] [Google Scholar]
- 180.Adams TD, Davidson LE, Litwin SE, et al. Health benefits of gastric bypass surgery after 6 years. JAMA 2012;308:1122–1131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Belle SH, Berk PD, Courcoulas AP, et al.; Longitudinal Assessment of Bariatric Surgery Consortium Writing Group . Safety and efficacy of bariatric surgery: Longitudinal Assessment of Bariatric Surgery. Surg Obes Relat Dis 2007;3:116–126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Courcoulas AP, Christian NJ, Belle SH, et al.; Longitudinal Assessment of Bariatric Surgery (LABS) Consortium . Weight change and health outcomes at 3 years after bariatric surgery among individuals with severe obesity. JAMA 2013;310:2416–2425 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Christou NV, Sampalis JS, Liberman M, et al. Surgery decreases long-term mortality, morbidity, and health care use in morbidly obese patients. Ann Surg 2004;240:416–423; discussion 423–424 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Schauer PR, Kashyap SR, Wolski K, et al. Bariatric surgery versus intensive medical therapy in obese patients with diabetes. N Engl J Med 2012;366:1567–1576 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Lee WJ, Chong K, Ser KH, et al. Gastric bypass vs sleeve gastrectomy for type 2 diabetes mellitus: a randomized controlled trial. Arch Surg 2011;146:143–148 [DOI] [PubMed] [Google Scholar]
- 186.Lim EL, Hollingsworth KG, Aribisala BS, Chen MJ, Mathers JC, Taylor R. Reversal of type 2 diabetes: normalisation of beta cell function in association with decreased pancreas and liver triacylglycerol. Diabetologia 2011;54:2506–2514 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Scopinaro N, Papadia F, Marinari G, Camerini G, Adami G. Long-term control of type 2 diabetes mellitus and the other major components of the metabolic syndrome after biliopancreatic diversion in patients with BMI < 35 kg/m2. Obes Surg 2007;17:185–192 [DOI] [PubMed] [Google Scholar]
- 188.Dixon JB, O’Brien PE, Playfair J, et al. Adjustable gastric banding and conventional therapy for type 2 diabetes: a randomized controlled trial. JAMA 2008;299:316–323 [DOI] [PubMed] [Google Scholar]
- 189.Lee WJ, Wang W, Lee YC, Huang MT, Ser KH, Chen JC. Effect of laparoscopic mini-gastric bypass for type 2 diabetes mellitus: comparison of BMI >35 and <35 kg/m2. J Gastrointest Surg 2008;12:945–952 [DOI] [PubMed] [Google Scholar]
- 190.Purnell J, Selzer F, Wahed A, et al. Improved probability of diabetes remission 3 years after Roux-en-Y gastric bypass (GBP) compared to laparoscopic gastric banding (LAGB) controlling for percentage weight change: results from the Longitudinal Assessment of Bariatric Surgery (LABS) 2 study. Poster presented at The Obesity Society’s ObesityWeek 2014, 2–7 November 2014, Boston Convention and Exhibition Center, Boston, MA
- 191.Flum DR, Belle SH, King WC, et al.; Longitudinal Assessment of Bariatric Surgery (LABS) Consortium . Perioperative safety in the longitudinal assessment of bariatric surgery. N Engl J Med 2009;361:445–454 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Konttinen H, Peltonen M, Sjöström L, Carlsson L, Karlsson J. Psychological aspects of eating behavior as predictors of 10-y weight changes after surgical and conventional treatment of severe obesity: results from the Swedish Obese Subjects intervention study. Am J Clin Nutr 2015;101:16–24 [DOI] [PubMed] [Google Scholar]
- 193.Seger JC, Horn DB, Westman EC, et al. Obesity algorithm presented by the American Society of Bariatric Physicians [Internet]. Available from www.obesityalgorithm.org. Accessed 17 December 2014
- 194.American Medical Association. AMA Resolution No. 420 (A-13) [Internet], 2013. Available from http://www.ama-assn.org/assets/meeting/2013a/a13-addendum-refcomm-d.pdf. Accessed 7 January 2015
- 195.American Society for Metabolic and Bariatric Surgery, The Obesity Society, American Society of Bariatric Physicians, American Association of Clinical Endocrinologists. Obesity is a disease: leading obesity groups agree [Internet], 2013. Available from http://connect.asmbs.org/PDF%20Documents/Press%20Releases/2013/Obesity%20is%20a%20Disease-%20Leading%20Obesity%20Groups%20Agree.pdf. Accessed 21 December 2014
- 196.World Health Organization. Obesity: Preventing and Managing the Global Epidemic: Report of a WHO Consultation. Geneva, World Health Organization, 2000 (WHO Tech. Rep. Ser., no. 894) [PubMed]
- 197.U.S. Food and Drug Administration. FDA’s obesity working group report: questions and answers [Internet]. Available from http://www.fda.gov/Food/FoodScienceResearch/ConsumerBehaviorResearch/ucm082094.htm#gen2211. Accessed 7 January 2015
- 198.American Board of Obesity Medicine. Home page [Internet]. Available from http://abom.org. Accessed 21 December 2014
- 199.Centers for Medicare & Medicaid Services. National coverage determination (NCD) for intensive behavioral therapy for obesity (210.12) [Internet]. Available from http://www.cms.gov/medicare-coverage-database/details/ncd-details.aspx?NCDId=353&ncdver=1&CoverageSelection=Both&ArticleType=All&PolicyType=Final&s=All&KeyWord=obesity&KeyWordLookUp=Title&KeyWordSearchType=And&bc=gAAAABAAAAAA&. Accessed 21 December 2014
- 200.Patient-Centered Outcomes Research Institute. PCORI board approves $102 million in support for 46 new research projects [Internet], 2014. Available from http://www.pcori.org/content/pcori-board-approves-102-million-support-46-new-research-projects. Accessed 21 December 2014
- 201.The Obesity Society. A promising milestone in coverage for obesity treatments [Internet], 2014. Available from http://www.obesity.org/publications/a-promising-milestone-in-coverage-for-obesity-treatments.htm. Accessed 21 December 2014
- 202.Wyatt E. Weight-loss companies charged with fraud [Internet], The New York Times 7 January 2014. Available from http://www.nytimes.com/2014/01/08/business/us-charges-4-companies-with-deception-in-weight-loss-products.html?_r=0. Accessed 21 December 2014