Abstract
Cannabinoids receive increasing interest as analgesic treatments. However, the clinical use of Δ9-tetrahydrocannabinol (Δ9-THC) has progressed with justified caution, which also owes to the incomplete mechanistic understanding of its analgesic effects, in particular its interference with the processing of sensory or affective components of pain. The present placebo-controlled crossover study therefore focused on the effects of 20 mg oral THC on the connectivity between brain areas of the pain matrix following experimental stimulation of trigeminal nocisensors in 15 non-addicted healthy volunteers. A general linear model (GLM) analysis identified reduced activations in the hippocampus and the anterior insula following THC administration. However, assessment of psychophysiological interaction (PPI) revealed that the effects of THC first consisted in a weakening of the interaction between the thalamus and the secondary somatosensory cortex (S2). From there, dynamic causal modeling (DCM) was employed to infer that THC attenuated the connections to the hippocampus and to the anterior insula, suggesting that the reduced activations in these regions are secondary to a reduction of the connectivity from somatosensory regions by THC. These findings may have consequences for the way THC effects are currently interpreted: as cannabinoids are increasingly considered in pain treatment, present results provide relevant information about how THC interferes with the affective component of pain. Specifically, the present experiment suggests that THC does not selectively affect limbic regions, but rather interferes with sensory processing which in turn reduces sensory-limbic connectivity, leading to deactivation of affective regions.
INTRODUCTION
Exogenous cannabinoids are increasingly acknowledged as an alternative option for the treatment of pain. The major ingredient of Cannabis sativa, Δ9-tetrahydrocannabinol (THC) (Mechoulam and Gaoni, 1965), has entered therapy of anorexia-associated weight loss (eg, in HIV), nausea and vomiting (eg, during chemotherapy), neuropathic pain in spastic paralysis (eg, in multiple sclerosis), and as an add-on to opioid pain treatment in cancer patients. However, its use for the treatment of pain (Farrell and Ritson, 2001) has progressed with justified caution (Kraft, 2012). This is owed to the risk of illicit use (Hall and Solowij, 1998) and also to the incomplete mechanistic understanding of its analgesic effects. It should be noted that studies in humans produced remarkably heterogeneous outcomes with respect to the effects of cannabis on pain, ranging from analgesia to hyperalgesia (Kraft, 2012; Walter et al, 2015b).
Effects of cannabinoids on pain are supported by several lines of molecular and functional evidence. Cannabinoid CB1 receptors (Devane et al, 1988; Matsuda et al, 1990) are ubiquitously present in the brain (Breivogel and Childers, 1998) and the spinal cord (Lindsey et al, 2005). Their activation may suppress the release of several neurotransmitters (Gulyas et al, 2004; Kano et al, 2009; Kofalvi et al, 2007; Piomelli, 2003), and thus regulate the function of several excitatory and inhibitory systems (Heifets and Castillo, 2009) such as glutamate, GABA, acetylcholine, and noradrenaline (Chevaleyre et al, 2006; Kano et al, 2009; Lovinger, 2008). CB1 receptor activations have been associated with several perceptual and cognitive effects. They include an inhibition of chronic inflammatory and neuropathic pain (Agarwal et al, 2007; Bishay et al, 2010), a modulation of sensory information processing (Dervaux et al, 2013; Tart, 1970), often described as taking on new qualities, including nociception (Walker and Huang, 2002), a disruption of filtering of non-salient information (D'Souza et al, 2012) and attentional salience processing (Bhattacharyya et al, 2012; Solowij et al, 1991), and an extinction of aversive memories (Marsicano et al, 2002).
The complex effects of cannabinoids on information processing, shared among various functional entities throughout the brain, suggest that cannabinoids may modulate pain perception by disturbing the connectivity within the human pain matrix (Apkarian et al, 2005; Bushnell et al, 1999; Price, 2000). As recently shown, THC reduces functional connectivity between the amygdala and the primary somatosensory cortex (S1) during pain processing, but it is not clear whether this effect results from reduced limbic output or reduced sensory input into the amygdala (Lee et al, 2013). Thus, the present study investigated effective connectivity of the pain matrix that is modulated by THC by applying dynamic causal modeling (DCM) and Bayesian model selection (BMS) to functional magnetic resonance imaging (fMRI) data collected during experimental pain stimulation. The results support the view that THC modulates effective connectivity in the somatosensory thalamocortical system, but additionally affects affective evaluation of pain by reducing sensory-limbic coupling.
MATERIALS AND METHODS
Subjects, Study Design, and Medications
The study (EudraCT-Nr. 2008-006881-27) followed the Declaration of Helsinki on Biomedical Research Involving Human Subjects and was approved by the Ethics Committee of the Medical Faculty of the Goethe University, Frankfurt am Main, Germany. Eight men (aged 24.9±2.0 years (mean±standard deviation), body weight 82.2±7.0 kg) and seven women (28±2.7 years, 64.7±8.7 kg) were enrolled after having given informed written consent (Thirty-six subjects were scheduled for the whole study including six possible replacements subjects. Fifteen subjects underwent the present protocol while 15 other subjects underwent a modified protocol that will be analyzed in an independent context.). The subjects' health was ascertained via medical history, a short physical examination, and routine clinical laboratory tests. At the beginning of each study day, a urine drug screening for THC, opiates, cocaine metabolites, amphetamines at baseline (Mahsan-Kombi/DOA 4-Test, MAHSAN Diagnostika Vertriebsgesellschaft mbH, Reinbek, Germany) was performed to detect carry-over effects or illicit cannabis consumption. Before the experiments, medications except contraceptives, alcohol and food were prohibited for 1 month, 24 or 6 h, respectively. During the study days, subjects were not allowed to consume anything except water.
Employing a double-blind placebo-controlled randomized crossover design, subjects received either an oral dose of 20 mg THC (two capsules containing each 10 mg THC dissolved in Adeps solidus, manufactured by the hospital pharmacy of the University of Heidelberg, Germany) or placebo (Adeps solidus), with a washout interval of 24 days (±14 days). The succession of treatments was sex-matched and five men and three women received THC during the first study period. Measurements took place before (baseline) and 2 h post medication (THC or placebo) when maximum pharmacological effects were expected (Hollister et al, 1981). During measurements after THC administration, plasma concentrations of THC and its metabolites THC-OH and THC-COOH were 6.4±3.9 ng/ml, 6±3.2 ng/ml, and 43.3±20.2 ng/ml (mean±standard deviation), respectively (for further details, see Walter et al, 2013).
Experimental Pain and Stimulation Protocol
Pain was induced by trigeminal excitation, using a chemical stimulus (Kobal, 1981, 1985). Short stinging sensations were induced to the nasal mucosa by delivering short (500 ms) pulses of gaseous CO2 to the subject's right nostril via a Teflon tube (outer diameter 4 mm). A concentration of 75% v/v ensured stimulation well above pain threshold (Oertel et al, 2012). To avoid mechanical or thermal co-stimulation, stimuli were embedded in a constantly flowing air stream (8 l/min) and applied via an olfactometer (Kobal, 1981; OM/2, Burghart Messtechnik GmbH, Wedel, Germany) that allowed for precise control of all parameters. CO2 is converted into bicarbonate and protons (Tarun et al, 2003), which have been shown to excite trigeminal nociceptors via activating TRPV1 (Reeh and Kress, 2001) or TRPA1 (Wang et al, 2010) ion channels. This pain model is well established for clinical pharmacological pain research (eg, Kobal et al, 1990; Lötsch et al, 1998, 2006) including fMRI assessments (Oertel et al, 2008).
During each experimental session, 25 CO2 stimuli were randomly interleaved with non-painful stimuli of 5 ppm H2S or 0.8 ppm vanillin (olfactory stimulants) to reduce a contextual modulation of pain due to attentional bias toward nociceptive stimuli or pain expectancy (Tracey et al, 2002; Walter et al, 2015a). Stimuli were delivered at a randomly spaced inter-stimulus interval (ISI) of 13.5–28.2 s (mean 18.9 s), which was long enough to minimize habituation and adaptation processes (Hummel et al, 1994). Subjects rated the sensory perceptions on 100-mm visual analog scales (VAS) displayed randomly within 3.4–6.6 s (mean 4.9 s) after each stimulus and querying pain (0, ‘no pain', to 100, ‘pain experienced at maximum'), smell (0, ‘no odor' to 100, ‘odor perceived at maximum intensity') or pleasantness (0, ‘very unpleasant' to 100, ‘very pleasant', 50 mm indicating hedonically inert stimuli). However, only one out of these three ratings was queried randomly at a time to limit the duration of the experiments. In addition, after the completion of each fMRI measurement session, subjects rated ‘fatigue', ‘drowsiness', ‘nausea', and ‘euphoria' by means of VAS (length 100 mm, ranging from ‘very weak' to ‘very strong'), ie, at baseline and at the end of the post-drug session. VAS ratings were compared between experimental conditions by means of analysis of variance for repeated measures (rm-ANOVA; SPSS version 22, IBM SPSS Statistics, Chicago) using a 2 × 2 design with ‘medication' (THC or placebo) and ‘session' (baseline or 2 h post medication) as within subject factors. The α level was set at 0.05 and corrected for multiple testing according to the conservative criterion of Bonferroni (Hochberg, 1988).
fMRI Image Acquisition
Employing an event-related design (Friston et al, 1998), the blood-oxygenation level-dependent (BOLD; Ogawa et al, 1990) response to the pain stimuli was recorded on a 3T MR head scanner (Siemens Magnetom Allegra, Siemens Medical Solutions, Erlangen, Germany) equipped with a combined single channel transmit and 4-channel receive head coil. The subject's head was immobilized using foam pads. In each session, 750 volumes (32 slices, 3 mm thick, 1 mm inter-slice gap, descending order) were recorded using a T2*-weighted gradient echo (GE) echo planar imaging (EPI) sequence (TR=2048 ms, TE=30 ms, flip angle=90°, echo spacing=420 μs, matrix size=64 × 64, and in-plane resolution=3 × 3 mm2). Following volume acquisition, a magnetic field map was acquired for correction of image distortions due to magnetic field inhomogeneities (Andersson et al, 2001; Hutton et al, 2002) using GE imaging with identical geometric parameters and two different TE values (4.89 and 7.35 ms), from which magnitude images and a phase difference map were calculated. In addition, a high-resolution T1-weighted anatomical image (1 mm isotropic resolution) was obtained for each subject via a three-dimensional (3D) magnetization prepared rapid acquisition of gradient echoes sequence (MP-RAGE; Mugler and Brookeman, 1991) using parameters TR=2200 ms, TE=3.93 ms, flip angle=9°, TI=900 ms, FOV=256 × 256 mm2 and one slab with 160 sagittal slices of 1 mm thickness, employing generalized autocalibrating partially parallel acquisitions (GRAPPA; Griswold et al, 2002) with an acceleration factor of 2 in phase encoding direction, yielding a duration of 4 min.
Data Analysis
Preprocessing of fMRI data
Spatial preprocessing of the MR data was performed using the statistical parametric mapping software SPM8 (Wellcome Department of Imaging Neuroscience, London, UK) (Friston et al, 1995; Worsley and Friston, 1995) on Matlab (version 8.3.0.532, MathWorks, Natick, MS). The first five volumes of each scanning block were discarded to ensure steady-state conditions. Volumes were realigned to the first volume and unwarped using the individual field map. The T1-weighted image was co-registered to the realigned and unwarped mean-EPI, segmented and normalized using 4th-degree B-spline interpolation (voxel size 3 × 3 × 3 mm3). Spatial normalization parameters were applied to all EPI volumes, which were smoothed with an isotropic 9-mm FWHM Gaussian kernel.
Assessment of THC effects on the activity of the pain matrix
THC effects on the processing of nociceptive information in the brain were identified globally by applying a general linear model (GLM) aimed at identifying the components of the pain matrix showing altered activations following THC administration, which was followed by analyses of functional and effective connectivity aimed at identifying the sources of interactions in the functional network.
General linear modeling
The four scanning sessions acquired during the two study days were specified in one model. In the first-level analysis, the observed neurophysiological responses were partitioned into components of interest, confounds and errors. Each nociceptive stimulus was included as an event with zero duration. Events of no interest, ie, olfactory stimuli, visual requests for ratings, and subsequent button presses, were modeled as separate regressors within the design matrix but omitted from second-level analyses. Furthermore, the six rotational and translational parameters from the rigid body transformation obtained during image realignment were included as covariates of no interest. All regressors were convolved with the canonical hemodynamic response function (HRF). Low frequency fluctuations of the MR signal were removed by applying a high pass filter at 128 Hz. Voxelwise coefficients for all regressors were estimated using least squares analysis. Following model estimation, effects of interest were tested using linear contrasts to generate statistical parametric maps of t-values for each subject.
Second-level analysis employed a factorial 2 × 2 ANOVA design with factors ‘medication' (placebo or THC) and ‘session' (baseline and post medication) to calculate the contrasts for the two-way interaction terms. The resulting statistical parametric maps (SPMt) were interpreted with regard to the probabilistic behavior of Gaussian random fields. Results are reported at p<0.05 (FWE-corrected) at peak position and a cluster size threshold of 5 voxels. The localization of brain activations, expressed in Montreal Neurological Institute (MNI) coordinates, was performed using the anatomy toolbox (version 2.5.2; Eickhoff et al, 2005) for those regions for which probability maps were available and the Talairach atlas for all other regions (Lancaster et al, 2000).
Psychophysiological interaction analysis
For analyses of psychophysiological interactions (PPI) (Friston et al, 1997), bi-linear models were used to identify brain regions that displayed THC-related changes in the correlations between the local activity and the activity in a distant seed region. The correlations were given by the mutual regression slopes. The ventral thalamus was chosen as the initial seed region based on its known role as a primary relay of sensory input to the cortex (Ab Aziz and Ahmad, 2006; Liang et al, 2011). The voxels from which activity vs time courses were extracted were taken from the main effect of ‘stimulus' in the GLM analysis. An anatomical mask of the bilateral thalamus as region of interest (ROI) was created using the WFU PickAtlas (Maldjian et al, 2003) to identify peak activation in this region. A BOLD time course averaged across a 5-mm sphere centered on the peak coordinate of the group-level GLM main effect was extracted for each subject using the first eigenvariate of the time series at the volume of interest (VOI). Adjustment for the F contrast of the effects of the nociceptive stimuli served to remove other covariates (see above).
The time series of the BOLD signal for the seed VOI was de-convolved for each subject. This yielded the time series of the neuronal activity (Gitelman et al, 2003). The PPI interaction regressor was obtained as the scalar product of (i) the experimental context (‘psychological variable') given from the main effects of pain stimuli applied either with or without THC and (ii) the time course of the neuronal activity at the seed region (‘physiological variable'). The interaction regressor was forward-convolved with the HRF. PPI effects were estimated by identifying voxels that displayed differences in the regression slope that depended on THC. The resulting statistical parametric maps (SPMt) were submitted to a random-effect group analysis (one sample t test) and thresholded at p=0.05, FWE-corrected.
Dynamic causal modeling
A dynamic causal model (DCM) (Friston et al, 2003) was built from the brain areas identified in the GLM and PPI analyses to infer the causal architecture of the coupled dynamical systems involved in the generation of THC effects via Bayesian selection of the most likely model from a set of candidate models describing mutual influences of neuronal systems as differential equations (Friston et al, 2003). To estimate the effective connectivity between different brain regions, the brain was considered as a dynamic system driven by external perturbations (eg, experimental stimuli); and a hemodynamic model was applied that estimated hypothetical BOLD signals in such a way that they best reflected the measured BOLD signals. The accuracy of each model in describing the measured data was quantified by a negative free energy value called ‘model evidence', which included a correction for model complexity. BMS was applied to obtain each model's probability to describe the observations relative to that of the other tested models.
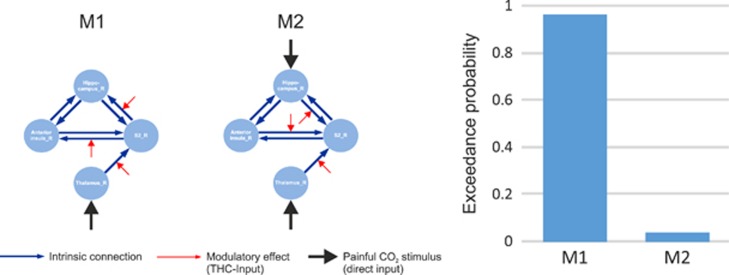
Following prior evidence (Lee et al, 2013), we focused on the relationship between the limbic and the somatosensory components of the pain matrix. DCM was applied to the time courses extracted from four ROIs identified during GLM and PPI analyses, ie, the right ventral thalamus, secondary somatosensory cortex (S2), the hippocampus, and the anterior insula. As in the PPI analysis, a BOLD time course averaged across a 5-mm sphere centered on the peak coordinates of the PPI and GLM interaction effect was extracted using the first eigenvariate of the time series. Based on prior knowledge (Oshiro et al, 2009; Sim et al, 2006), bidirectional intrinsic connections between S2 and anterior insula, between S2 and hippocampus, and between anterior insula and hippocampus were assumed. We compared two different models regarding the modulation of connections by THC, which are based on the following considerations: one hypothesis is that THC diminishes flow of sensory information into limbic structures in the lateral spinothalamic pathway that projects from the thalamus to the somatosensory cerebral cortical areas and is forwarded to components of the limbic system. The other hypothesis is that THC reduces limbic modulation of somatosensory cortices. Therefore, two models were defined (Figure 1): The first model (Model 1) implied that (i) THC mainly influenced the processing of sensory information coming from the thalamus and (ii) additionally altered the connections from the secondary somatosensory cortex to regions involved in affective evaluations of pain (anterior insula and hippocampus). The competing second model (Model 2) implied that (i) THC mainly influenced the processing of sensory information coming from the thalamus and (ii) additionally altered connections from the anterior insula and the hippocampus to the secondary somatosensory cortex. The models were compared by means of random-effects (RFX) analysis (Stephan et al, 2010) applying Bayesian criteria to determine the best model. The winning model was further analyzed with respect to consistency across subjects by applying a one-sample t-test to the ‘MAP' (maximum a posteriori) parameter estimates from the individual DCMs, separately for each parameter, ie, fixed connections, modulatory changes of connections and driving input.
Figure 1.
Left: Schematic structure of the two models compared in this study. In all models, seven intrinsic connections were defined (blue lines with arrows indicating the direction of connection). The driving input pain (black lines) enters the model via thalamus (model 1) and via thalamus and hippocampus (model 2), respectively. THC modulates the connection between thalamus and S2 (as known from the PPI analysis) and the connections from S2 to the anterior insula and to the hippocampus (model 1) or reverse, ie, from hippocampus and anterior insula to S2 (Model 2). Right: Result of Bayesian model selection on model level shows that exceedance probability of model 1 (EP: 0.96) exceeds model 2 by far (EP: 0.04).
RESULTS
All subjects finished the experiments, however, mild to moderate side effects occurred during the THC condition including an increase in the ratings for drowsiness, nausea, and euphoria (repeated-measures ANOVA: interaction ‘medication' (THC, placebo) by ‘session' (baseline, post-medication): all F(1,14)>4.94, all p<0.044), whereas fatigue was unaffected (F(1,14)=1.72, p=0.21). Further side effects during the THC condition comprised vomiting (n=2), tremor (n=2) and dizziness (n=2). Neither THC nor its main metabolites were detected in any baseline sample.
Similarly to a previous experiment employing similar stimuli (Lötsch et al, 2012), the nociceptive stimuli were always perceived as painful (median [interquartile range]: 48.63 [33.19, 67.44] mm VAS pain) but not smelly (0 [0.0, 6.31] mm VAS smell), whereas the H2S and vanillin were rated as smelly (31.44 [19.43, 47.5] and 22.06 [9.0, 31.9] mm VAS smell, respectively) but not painful (0 [0.0, 0.0] mm VAS pain). THC altered neither intensity perception (interaction ‘drug' by ‘measurement': F(1,14)=3.16, p=0.097) nor pleasantness rating (interaction ‘drug' by ‘measurement': F(1,14)=0.391, p=0.542) of the painful CO2 stimuli. The intensity rating of the control stimuli H2S and vanillin did not show any change, either (p>0.175). For vanillin, however, THC reduced the hedonic rating from pleasant to neutral (64.58 and 52.53 for the baseline and post-THC session, respectively; interaction ‘drug' by ‘measurement': F(1,14)=14.0, p=0.005)), while H2S remained unpleasant (p=0.476).
Whole Brain Analyses
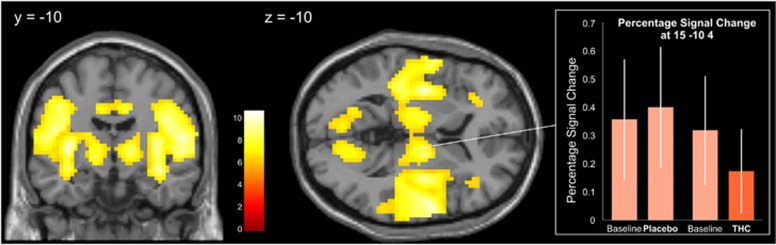
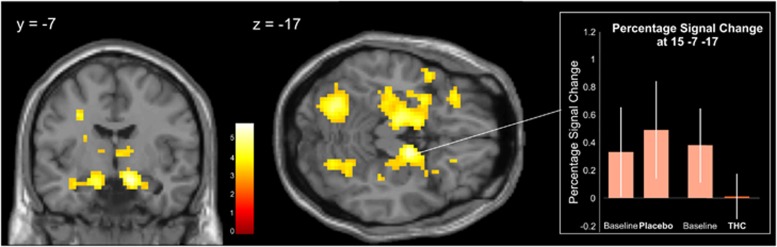
CO2 stimulus-induced brain activations were observed bilaterally, with slightly more pronounced activations in the right secondary somatosensory cortex, right postcentral gyrus (Figure 2, Table 1), which agrees with a previously observed right-hemisphere dominance of CO2 stimulus-induced brain activations (Hari et al, 1997), and in addition in the cingulate gyrus. THC significantly reduced the activations in the right anterior insula, the hippocampus, and the cerebellum (p<0.05, FWE-corrected, SPM contrast −1 1 1 −1 in the succession placebo baseline, placebo post-drug session, THC baseline, and THC post-drug session; Table 2 and Figure 3). Enhanced activity following THC administration was not found (no significant activation at p<0.001, uncorrected, SPM contrast 1 −1 −1 1).
Figure 2.
Brain regions that were activated by the CO2 pain stimulus (main effect ‘stimulus'). The topographies of differences in brain activations are superimposed upon slices of the canonical MR template implemented in SPM8. The significance at voxel level is color coded from red to white with increasing t-values. Voxels are shown at a threshold of p<0.001 (FWE-corrected, t>6.18). The bars show the effect size (mean and standard deviation) at coordinates of the right thalamus used as a seed region for subsequent PPI.
Table 1. Clusters of Brain Regions That Were Activated During the CO2 Pain Stimulus (Main Effect ‘Stimulus' in a 2 × 2 Factorial Design, Contrast 1 1 1 1 in the Succession Placebo Baseline Session, Placebo Post-Drug Session and THC Baseline Session, THC Post-Drug Session, Resp.).
| Brain regions within cluster |
MNI coordinates |
t-values of peak coordinates | ||
|---|---|---|---|---|
| x | y | z | ||
| Right rolandic operculum/insula/superior temporal gyrus | 57 | −4 | 10 | 10.73 |
| Right anterior and median cingulate gyri/supplementary motor area | 12 | −16 | 37 | 9.35 |
| Right calcarine fissure/left calcarine fissure/left cuneus | 15 | −73 | 7 | 8.03 |
| Right postcentral gyrus | 27 | −28 | 52 | 7.74 |
| Right cerebellum | 18 | −64 | −26 | 6.86 |
| Left cerebellum | −12 | −64 | −26 | 6.75 |
| Left inferior frontal gyrus | −36 | 8 | 16 | 6.63 |
| Right superior occipital gyrus | 18 | −82 | 28 | 6.58 |
| Right thalamusa | 15 | −10 | 4 | 8.64 |
Results reflect a 14-subject analysis. Voxels are given at a threshold of p<0.05 (FWE-corrected, cluster size threshold 5 voxels). Coordinates are reported in MNI space (mm).
Activity when applying an anatomical mask of the bilateral thalamus to identify region of interest (ROI) for connectivity analyses.
Table 2. Clusters of Brain Regions That Were Less Activated During the THC Condition in the Post-Drug Session (Interaction ‘Drug' by ‘Measurement' in a 2 × 2 Factorial Design, Contrast −1 1 1 −1 in the Succession Placebo Baseline Session, Placebo Post-Drug Session and THC Baseline Session, THC Post-Drug Session, Resp.).
| Brain regions within cluster |
MNI coordinates |
t-values of peak coordinates | ||
|---|---|---|---|---|
| x | y | z | ||
| Right insula/inferior frontal gyrus | 33 | 23 | 10 | 5.84 |
| Right hippocampus/parahippocampal gyrus | 15 | −7 | −17 | 5.42 |
| Left cerebellum | −27 | −67 | −20 | 4.56 |
Results reflect a 14-subject analysis. Voxels are given at a threshold of p<0.05 (FWE-corrected, cluster size threshold 5 voxels). Coordinates are reported in MNI space (mm).
Figure 3.
Brain regions that were deactivated by THC administration (interaction ‘drug', ie, placebo or THC) by ‘measurement' (ie, baseline or post-drug session). The topographies of differences in brain activations are superimposed upon slices of the canonical MR template implemented in SPM8. The significance at voxel level is color coded from red to white with increasing t-values. Voxels are shown at a threshold of p<0.001 (uncorrected, t>3.25). The bars show the effect size (mean and standard deviation) at the coordinates of the right hippocampus used as seed region for subsequent PPI.
ROI in Functional Imaging
Psychophysiological interaction
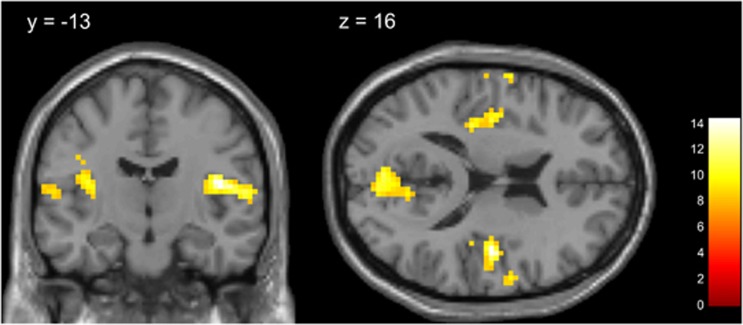
The seed region for the PPI analysis was located in the right ventral thalamus at MNI coordinates x=15, y=−10, z=4, which had been identified by an ROI analysis of the bilateral thalamus as showing local peak activation within this region during pain stimulation (main effect ‘stimulus'). The most pronounced PPI for this seed region was found with the right secondary somatosensory cortex (S2) at coordinates x=45, y=−13, z=16 (peak-level p<0.05, FWE corrected; Table 3 and Figure 4). THC induced a decrease in the connectivity between the thalamus and S2. This was supported by a tendency toward lower pain intensity following THC administration (repeated measures ANOVA: interaction ‘medication' by ‘session': F(1,14)=3.16, p=0.097). An additional analysis performed solely to accommodate a previous finding (Lee et al, 2013) verified a reduced connectivity also between the amygdala and primary somatosensory cortex (see Supplementary Materials).
Table 3. Brain Regions That Showed Reduced Functional Connectivity to the Seed Region Right Thalamus (x=15, y=−10, z=4) after THC Administration (Seed Region × (non-THC condition−THC condition)).
| Brain regions within cluster |
MNI coordinates |
t-values of peak coordinates | ||
|---|---|---|---|---|
| x | y | z | ||
| Right rolandic operculum/Heschl gyrus/insula/postcentral gyrus/superior temporal gyrus/precentral gyrusa | 45 | −13 | 16 | 14.23 |
| Right calcarine fissure/cuneus Left calcarine fissure/cuneus | −3 | −79 | 16 | 11.12 |
| Left postcentral gyrus | −63 | −1 | 13 | 11.04 |
| Left postcentral gyrus/insula/rolandic operculum/Heschl gyrus | −36 | −13 | 16 | 10.45 |
| Right putamen | 36 | −4 | −5 | 10.09 |
| Right supramarginal gyrus/Heschl gyrus/rolandic operculum | 45 | −25 | 19 | 9.73 |
| Left Heschl gyrus/superior temporal gyrus/postcentral gyrus/rolandic operculum | −57 | −13 | 10 | 8.84 |
Results reflect a 14-subject analysis. Voxels are given at a threshold of p<0.05 (FWE-corrected, cluster size threshold 5 voxels). Coordinates are reported in MNI space (mm).
Peak coordinates of this cluster are used as region of interest (ROI) for dynamic causal modeling (DCM).
Figure 4.
Brain regions that showed reduced functional connectivity to the seed region right thalamus (x=15, y=−10, z=4) after THC administration (PPI, seed region × (non-THC condition−THC condition)). The topographies of differences in brain activations are superimposed upon slices of the canonical MR template implemented in SPM8. The significance at voxel level is color coded from red to white with increasing t-values. Voxels are shown at a threshold of p<0.05 (FWE-corrected, t>7.94).
Dynamic causal modeling
The analysis of effective brain connectivity focused on four regions that previously had been identified by means of GLM (hippocampus: x=15, y=−7, z=−17, anterior insula: x=33, y=23, z=10) and PPI analysis (thalamus: x=15, y=−10, z=4, S2: x=45, y=−13, z=16) as regions where THC influenced the nociceptive activation and connectivity, respectively. DCM analysis compared models that included the regions and the direction of their interconnections that were influenced by THC. BMS showed that THC influenced the forward connections, starting from S2 to the anterior insula and to the hippocampus (model 1). This model was much more likely (exceedance probability 0.96) than THC influences on the direct nociceptive input to limbic areas with subsequent influence on sensory areas (model 2, exceedance probability 0.04). The parameters of the winning model 1 (Figure 1) showed that the connection strengths between thalamus and S2 and from S2 to the anterior insula or to the hippocampus decreased significantly under THC influence (Table 4).
Table 4. Connectivity Estimates from the Winning Model 1.
| Parameter | Mean±SD (Hz) | t-test (t; p) |
|---|---|---|
| Intrinsic connections (a parameter) | ||
| Thalamus→S2 | 0.57±0.46 | t(13)=4.56; p=0.001 |
| S2→anterior insula | 0.11±0.32 | t(13)=1.26; p=0.229 |
| S2→hippocampus | 0.35±0.64 | t(13)=2.06; p=0.06 |
| Anterior insula→hippocampus | −0.39±0.72 | t(13)=−2.03; p=0.064 |
| Anterior insula→S2 | −0.18±0.96 | t(13)=−0.72; p=0.483 |
| Hippocampus→S2 | −0.19±0.69 | t(13)=−1.05; p=0.31 |
| Hippocampus→anterior insula | 0.01±0.46 | t(13)=0.07; p=0.949 |
| THC effect on connections (b parameter) | ||
| Thalamus→S2 | −0.81±0.76 | t(13)=−3.97; p=0.002 |
| S2→anterior insula | −0.41±0.59 | t(13)=−2.59; p=0.022 |
| S2→hippocampus | −0.29±0.5 | t(13)=−2.2; p=0.046 |
| Direct input pain (c parameter) | ||
| Thalamus | 0.3±0.29 | t(13)=3.87; p=0.002 |
Results are given as means (±standard deviation) and t-values followed by the number of degrees of freedom in parentheses and the p-value. A two-sided one-sample t-test against zero was performed.
DISCUSSION
Although the observed cerebral effects were not associated with major behavioral consequences, they provide nevertheless a plausible and statistically supported explanation regarding the analgesic effects of THC observed in clinical settings such as chronic pain conditions. These effects were associated with a modulation of nociceptive thalamocortical connectivity. The model selection analysis considered controversial assumptions about cannabis-induced modulation of interactions between affective and sensory processing underlying pain perception. It clearly favored a modulation of the affective component of pain on the basis of reduced sensory input into the limbic system. Tentatively, this could answer the open question concerning the direction of THC-induced reduced functional connectivity between amygdala and primary somatosensory cortex (Lee et al, 2013).
The observation of deactivated limbic regions is in line with the observation that THC predominantly influences affective rather than sensory processing of nociceptive information. For example, administration of 5 mg oral THC in combination with 0.02 mg/kg intravenous morphine produced analgesic effects only on the affective but not on the sensory component of pain during heat stimulation (Roberts et al, 2006). Similarly, oral administration of 15 mg THC reduced the affective ratings of heat pain stimuli (Lee et al, 2013). The notion that THC influences predominantly the affective components of pain is further corroborated by THC's reported efficacy in chronic pain conditions (Abrams et al, 2007; Berman et al, 2004; Noyes et al, 1975; Nurmikko et al, 2007; Svendsen et al, 2004), especially when a psychological component such as pronounced distress is involved (Fernandez and Turk, 1992; Martin and Lichtman, 1998).
The identified brain regions, ie anterior insular cortex and hippocampus, correspond well with the assumption that THC effects on pain have a profound affective component. The (anterior) insula is involved in the identification of salient stimuli from a stream of sensory stimuli. It participates in most cognitive activities (Gasquoine, 2014), and has been proposed as an integral hub mediating the flow of information across brain regions (Menon and Uddin, 2010) via its bidirectional connections with most parts of the brain. The hippocampus, on the other hand, has been associated with novelty detection during acute painful stimulation (Bingel et al, 2002; Schneider et al, 2001). Hippocampal activity was reduced when attention was directed away from the painful stimulus (Ploghaus et al, 2000), and it was most consistently observed in studies in which pain perception was increased by expectations or anxiety rather than by augmented nociceptive input (Leknes and Tracey, 2007). THC effects on the hippocampus are also in line with observations that cannabis contributes to the extinction of aversive memories to noxious stimuli (Marsicano et al, 2002).
However, cannabinoids have been associated not only with effects on the affective but also, although more rarely, with the sensory component of pain. Specifically in mouse experiments, THC significantly decreased the response latencies to heat stimuli (hot plate, tail flick; Martin and Lichtman, 1998). This was interpreted as indicating antinociceptive effects on a sensory level (Bloom and Dewey, 1978; Chesher et al, 1973), which would further agree with cannabinoid receptors being present in pain circuits from the peripheral sensory nerve endings up to the brain (Manzanares et al, 2006). Endocannabinoids are also involved in endogenous pain inhibition (Walker et al, 2001), as shown in models of chronic inflammatory and neuropathic pain (Agarwal et al, 2007; Bishay et al, 2010). Local injections of cannabinoid receptor agonists reduce pain in various rodent models (Agarwal et al, 2007; Kehl et al, 2003; Lozano-Ondoua et al, 2010). A few human studies also demonstrated a decreased sensitivity and increased tolerance to pain in a THC dose-dependent manner (Cooper et al, 2013; Greenwald and Stitzer, 2000), which is in line with the observation of reduced coupling between thalamus and S2 as the lateral spinothalamic tract is critical for the sensory-discriminative processing of pain (Maihofner et al, 2006; Price, 2002). The fact that subjects tended to perceive CO2 stimuli as less intense during THC administration would support this effect. A covariation analysis using the pain ratings to analyze interindividual variability on neuronal effects was impossible because the perceived pain was queried alternatively with smell and pleasantness and therefore not available for each stimulus. Of note, the differences between the ratings of pain intensity and pleasantness of the CO2 stimuli acquired after THC administration and at baseline did not correlate with the respective changes in the ratings of adverse effects, ie, drowsiness, nausea, euphoria, and fatigue, as indicated by always non-significant correlations (p-values always >0.05, Spearman's ρ never exceeding a low value of 0.26).
A recent imaging study demonstrated a THC-induced reduced functional connectivity between the amygdala and S1 in an experimental model inducing pain by means of capsaicin application (Lee et al, 2013). This effect could be reproduced in the present data (see Supplementary Material). However, such a conclusion, ie, that THC predominantly affects the limbic rather than the sensory processing of nociceptive information, was probably premature as with the exclusively used PPI method, the direction of the influence could not be identified.
To explore the influence of THC on connectivity between brain areas, we performed a PPI analysis to identify regions showing THC-induced altered connectivity with the ventral thalamus. No connectivity changes from thalamus to areas primarily processing affective components of pain could be identified although multiple ascending pain pathways transmit information from thalamus to the limbic system (Ab Aziz and Ahmad, 2006). Indeed, the PPI analysis identified S2 as the brain region showing the strongest reduction of functional connectivity with the thalamus upon THC administration. The activation detected in the present study is located at a minimally more anterior position than a previously shown hotspot of a thalamus-to-somatosensory cortex resting-state functional connectivity (Behrens et al, 2003). Given the observed PPI between the thalamic coordinate and the somatosensory cortex, the assumption that the present coordinates reflect the activity in thalamic sensory nuclei seems plausible. Furthermore, the results of the DCM analysis and subsequent BMS suggest that THC additionally modulated the information flow from the secondary somatosensory cortex to regions involved in the affective evaluation of pain rather than the opposite, ie, reducing the connection strength from limbic to somatosensory regions as previously interpreted from a PPI analysis (Lee et al, 2013).
Following the establishment of a plausible model of the THC effects on cerebral pain processing, a few further alternatives were additionally addressed: This first included two extreme alternatives to the present model, ie, a model that included direct pain inputs to the hippocampus and to the thalamus with separate influences of THC but without THC action on sensory-limbic connections (model 3; see Supplementary Material), and a further model that included THC effects on all intrinsic connections (model 4; see supplementary materials). These modifications did not change the results of the BMS, which still identified model 1 as clearly outperforming all other models (EP>90; details not shown). Moreover, the direction of influence from sensory to limbic areas also persisted when second, model comparisons were extended to two further models that were mainly identical to models 1 and 2 with the exception that both, incoming and outgoing limbic connections, were modulated by THC. Third, M1 is still favored when receiving the same direct input (ie in the thalamus and hippocampus) as M2. Fourth, as observations in laboratory animals suggested a direct THC influence on limbic regions, a model that included a direct influence of THC on hippocampus and anterior insula was considered in the BMS; however, it was assigned a probability of only 0.098. Of note, when analyzing only the baseline data acquired in the absence of any treatment, BMS also favored model 1 (EP: 0.91); however, in contrast to the model including THC data, the connection from thalamus to S2 was strengthened by the pain stimuli (b-parameter: 0.51±0.56, p=0.005). Moreover, the parameters modulating the connection from S2 to hippocampus and anterior insula missed statistical significance (b-parameter: −0.05 and −0.09, respectively, with p=0.77 and 0.33, respectively), implying that a reduction of the transmission of nociceptive information to affective regions is consistent only in the presence of THC. Taken together, the exploration of several further models suggested by reported evidence or consisting in extreme or reasonable further alternatives did not result in any challenge of the present model.
Finally, reports of a THC-related increase in the brain perfusion, which subsequently caused fluctuations of the BOLD signal in several brain regions including the insula (Dodel et al, 2004; van Hell et al, 2011), point at a possible confounder that was not addressed in the present study as heart rate and respiration variability were not recorded. The referenced experiments were performed while subjects were in resting state, which has been highlighted to be particularly vulnerable to misinterpreting artifacts as neuronal responses (Dodel et al, 2004).
CONCLUSIONS
In this work, we present THC effects on the cerebral processing of nociceptive information. THC modulates effective connectivity between the sensory thalamus and the secondary sensory cortex, but additionally reduces information flow from S2 to limbic regions. These findings have consequences for the way THC effects are currently interpreted: as cannabinoids are increasingly considered in pain treatment, present results provide relevant information about how THC interferes with the affective component of nociception. Specifically, THC does not selectively affect limbic regions, but rather interferes with sensory processing which in turn reduces sensory-limbic connectivity, leading to deactivation of affective regions.
FUNDING AND DISCLOSURE
The authors declare no conflict of interest.
Acknowledgments
This work was supported by the Deutsche Forschungsgemeinschaft, DFG Lo 612/10-1 (JL). The funders had no role in method design, data selection and analysis, decision to publish, or preparation of the manuscript. Concentrations of exogenous and endogenous cannabinoids and results of electrical pain threshold measurements obtained within the reported study were analyzed separately in a non-redundant context (Walter et al, 2015a). RD received compensation as a Consultant for MR scanner procurement by the Wellcome Trust Centre for Neuroimaging, UCL, London, UK.
Footnotes
Supplementary Information accompanies the paper on the Neuropsychopharmacology website (http://www.nature.com/npp)
Supplementary Material
References
- Ab Aziz CB, Ahmad AH (2006). The role of the thalamus in modulating pain. Malays J Med Sci 13: 11–18. [PMC free article] [PubMed] [Google Scholar]
- Abrams DI, Jay CA, Shade SB, Vizoso H, Reda H, Press S et al (2007). Cannabis in painful HIV-associated sensory neuropathy: a randomized placebo-controlled trial. Neurology 68: 515–521. [DOI] [PubMed] [Google Scholar]
- Agarwal N, Pacher P, Tegeder I, Amaya F, Constantin CE, Brenner GJ et al (2007). Cannabinoids mediate analgesia largely via peripheral type 1 cannabinoid receptors in nociceptors. Nat Neurosci 10: 870–879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andersson JL, Hutton C, Ashburner J, Turner R, Friston K (2001). Modeling geometric deformations in EPI time series. Neuroimage 13: 903–919. [DOI] [PubMed] [Google Scholar]
- Apkarian AV, Bushnell MC, Treede RD, Zubieta JK (2005). Human brain mechanisms of pain perception and regulation in health and disease. Eur J Pain 9: 463–484. [DOI] [PubMed] [Google Scholar]
- Behrens TE, Johansen-Berg H, Woolrich MW, Smith SM, Wheeler-Kingshott CA, Boulby PA et al (2003). Non-invasive mapping of connections between human thalamus and cortex using diffusion imaging. Nat Neurosci 6: 750–757. [DOI] [PubMed] [Google Scholar]
- Berman JS, Symonds C, Birch R (2004). Efficacy of two cannabis based medicinal extracts for relief of central neuropathic pain from brachial plexus avulsion: results of a randomised controlled trial. Pain 112: 299–306. [DOI] [PubMed] [Google Scholar]
- Bhattacharyya S, Crippa JA, Allen P, Martin-Santos R, Borgwardt S, Fusar-Poli P et al (2012). Induction of psychosis by Delta9-tetrahydrocannabinol reflects modulation of prefrontal and striatal function during attentional salience processing. Arch Gen Psychiatry 69: 27–36. [DOI] [PubMed] [Google Scholar]
- Bingel U, Quante M, Knab R, Bromm B, Weiller C, Büchel C (2002). Subcortical structures involved in pain processing: evidence from single-trial fMRI. Pain 99: 313–321. [DOI] [PubMed] [Google Scholar]
- Bishay P, Schmidt H, Marian C, Haussler A, Wijnvoord N, Ziebell S et al (2010). R-flurbiprofen reduces neuropathic pain in rodents by restoring endogenous cannabinoids. PLoS One 5: e10628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bloom AS, Dewey WL (1978). A comparison of some pharmacological actions of morphine and delta9-tetrahydrocannabinol in the mouse. Psychopharmacology (Berl) 57: 243–248. [DOI] [PubMed] [Google Scholar]
- Breivogel CS, Childers SR (1998). The functional neuroanatomy of brain cannabinoid receptors. Neurobiol Dis 5(6 Pt B): 417–431. [DOI] [PubMed] [Google Scholar]
- Bushnell MC, Duncan GH, Hofbauer RK, Ha B, Chen JI, Carrier B (1999). Pain perception: is there a role for primary somatosensory cortex? Proc Natl Acad Sci USA 96: 7705–7709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chesher GB, Dahl CJ, Everingham M, Jackson DM, Marchant-Williams H, Starmer GA (1973). The effect of cannabinoids on intestinal motility and their antinociceptive effect in mice. Br J Pharmacol 49: 588–594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chevaleyre V, Takahashi KA, Castillo PE (2006). Endocannabinoid-mediated synaptic plasticity in the CNS. Annu Rev Neurosci 29: 37–76. [DOI] [PubMed] [Google Scholar]
- Cooper ZD, Comer SD, Haney M (2013). Comparison of the analgesic effects of dronabinol and smoked marijuana in daily marijuana smokers. Neuropsychopharmacology 38: 1984–1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- D'Souza DC, Fridberg DJ, Skosnik PD, Williams A, Roach B, Singh N et al (2012). Dose-related modulation of event-related potentials to novel and target stimuli by intravenous delta(9)-THC in humans. Neuropsychopharmacology 37: 1632–1646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dervaux A, Bourdel MC, Laqueille X, Krebs MO (2013). Neurological soft signs in non-psychotic patients with cannabis dependence. Addict Biol 18: 214–221. [DOI] [PubMed] [Google Scholar]
- Devane WA, Dysarz FA 3rd, Johnson MR, Melvin LS, Howlett AC (1988). Determination and characterization of a cannabinoid receptor in rat brain. Mol Pharmacol 34: 605–613. [PubMed] [Google Scholar]
- Dodel S, Poline JB, Anton JL, Brett M (eds) (2004). The influence of heart beat and respiration on functional connectivity networks. Biomedical Imaging: Nano to Macro, 2004. IEEE International Symposium; 15–18 April 2004.
- Eickhoff SB, Stephan KE, Mohlberg H, Grefkes C, Fink GR, Amunts K et al (2005). A new SPM toolbox for combining probabilistic cytoarchitectonic maps and functional imaging data. Neuroimage 25: 1325–1335. [DOI] [PubMed] [Google Scholar]
- Farrell M, Ritson B (2001). Cannabis and health. Br J Psychiatry 178: 98. [DOI] [PubMed] [Google Scholar]
- Fernandez E, Turk DC (1992). Sensory and affective components of pain: separation and synthesis. Psychol Bull 112: 205–217. [DOI] [PubMed] [Google Scholar]
- Friston KJ, Buechel C, Fink GR, Morris J, Rolls E, Dolan RJ (1997). Psychophysiological and modulatory interactions in neuroimaging. Neuroimage 6: 218–229. [DOI] [PubMed] [Google Scholar]
- Friston KJ, Fletcher P, Josephs O, Holmes A, Rugg MD, Turner R (1998). Event-related fMRI: characterizing differential responses. Neuroimage 7: 30–40. [DOI] [PubMed] [Google Scholar]
- Friston KJ, Harrison L, Penny W (2003). Dynamic causal modelling. Neuroimage 19: 1273–1302. [DOI] [PubMed] [Google Scholar]
- Friston KJ, Holmes AP, Poline JB, Grasby PJ, Williams SC, Frackowiak RS et al (1995). Analysis of fMRI time-series revisited. Neuroimage 2: 45–53. [DOI] [PubMed] [Google Scholar]
- Gasquoine PG (2014). Contributions of the insula to cognition and emotion. Neuropsychol Rev 24: 77–87. [DOI] [PubMed] [Google Scholar]
- Gitelman DR, Penny WD, Ashburner J, Friston KJ (2003). Modeling regional and psychophysiologic interactions in fMRI: the importance of hemodynamic deconvolution. Neuroimage 19: 200–207. [DOI] [PubMed] [Google Scholar]
- Greenwald MK, Stitzer ML (2000). Antinociceptive, subjective and behavioral effects of smoked marijuana in humans. Drug Alcohol Depend 59: 261–275. [DOI] [PubMed] [Google Scholar]
- Griswold MA, Jakob PM, Heidemann RM, Nittka M, Jellus V, Wang J et al (2002). Generalized autocalibrating partially parallel acquisitions (GRAPPA). Magn Reson Med 47: 1202–1210. [DOI] [PubMed] [Google Scholar]
- Gulyas AI, Cravatt BF, Bracey MH, Dinh TP, Piomelli D, Boscia F et al (2004). Segregation of two endocannabinoid-hydrolyzing enzymes into pre- and postsynaptic compartments in the rat hippocampus, cerebellum and amygdala. Eur J Neurosci 20: 441–458. [DOI] [PubMed] [Google Scholar]
- Hall W, Solowij N (1998). Adverse effects of cannabis. Lancet 352: 1611–1616. [DOI] [PubMed] [Google Scholar]
- Hari R, Portin K, Kettenmann B, Jousmaki V, Kobal G (1997). Right-hemisphere preponderance of responses to painful CO2 stimulation of the human nasal mucosa. Pain 72: 145–151. [DOI] [PubMed] [Google Scholar]
- Heifets BD, Castillo PE (2009). Endocannabinoid signaling and long-term synaptic plasticity. Annu Rev Physiol 71: 283–306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hochberg Y (1988). A sharper Bonferroni procedure for multiple tests of significance. Biometrika 75: 800–802. [Google Scholar]
- Hollister LE, Gillespie HK, Ohlsson A, Lindgren JE, Wahlen A, Agurell S (1981). Do plasma concentrations of delta 9-tetrahydrocannabinol reflect the degree of intoxication? J Clin Pharmacol 21(8–9 Suppl): 171S–177S. [DOI] [PubMed] [Google Scholar]
- Hummel T, Gruber M, Pauli E, Kobal G (1994). Chemo-somatosensory event-related potentials in response to repetitive painful chemical stimulation of the nasal mucosa. Electroencephalogr Clin Neurophysiol 92: 426–432. [DOI] [PubMed] [Google Scholar]
- Hutton C, Bork A, Josephs O, Deichmann R, Ashburner J, Turner R (2002). Image distortion correction in fMRI: a quantitative evaluation. Neuroimage 16: 217–240. [DOI] [PubMed] [Google Scholar]
- Kano M, Ohno-Shosaku T, Hashimotodani Y, Uchigashima M, Watanabe M (2009). Endocannabinoid-mediated control of synaptic transmission. Physiol Rev 89: 309–380. [DOI] [PubMed] [Google Scholar]
- Kehl LJ, Hamamoto DT, Wacnik PW, Croft DL, Norsted BD, Wilcox GL et al (2003). A cannabinoid agonist differentially attenuates deep tissue hyperalgesia in animal models of cancer and inflammatory muscle pain. Pain 103: 175–186. [DOI] [PubMed] [Google Scholar]
- Kobal G (1981) Elektrophysiologische Untersuchungen des Menschlichen Geruchsinnes. Thieme-Verlag: Stuttgart. [Google Scholar]
- Kobal G (1985). Pain-related electrical potentials of the human nasal mucosa elicited by chemical stimulation. Pain 22: 151–163. [DOI] [PubMed] [Google Scholar]
- Kobal G, Hummel C, Nuernberg B, Brune K (1990). Effects of pentazocine and acetylsalicylic acid on pain-rating, pain-related evoked potentials and vigilance in relationship to pharmacokinetic parameters. Agents Actions 29: 342–359. [DOI] [PubMed] [Google Scholar]
- Kofalvi A, Pereira MF, Rebola N, Rodrigues RJ, Oliveira CR, Cunha RA (2007). Anandamide and NADA bi-directionally modulate presynaptic Ca2+ levels and transmitter release in the hippocampus. Br J Pharmacol 151: 551–563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kraft B (2012). Is there any clinically relevant cannabinoid-induced analgesia? Pharmacology 89: 237–246. [DOI] [PubMed] [Google Scholar]
- Lancaster JL, Woldorff MG, Parsons LM, Liotti M, Freitas CS, Rainey L et al (2000). Automated Talairach atlas labels for functional brain mapping. Hum Brain Mapp 10: 120–131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee MC, Ploner M, Wiech K, Bingel U, Wanigasekera V, Brooks J et al (2013). Amygdala activity contributes to the dissociative effect of cannabis on pain perception. Pain 154: 124–134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leknes S, Tracey I (2007) Hippocampus and Entorhinal Complex, Functional Imaging Chapter of the Encyclopedia of Pain Springer Verlag: Berlin, Heidelberg. [Google Scholar]
- Liang M, Mouraux A, Iannetti GD (2011). Parallel processing of nociceptive and non-nociceptive somatosensory information in the human primary and secondary somatosensory cortices: evidence from dynamic causal modeling of functional magnetic resonance imaging data. J Neurosci 31: 8976–8985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindsey KP, Glaser ST, Gatley SJ (2005). Imaging of the brain cannabinoid system. Handb Exp Pharmacol 168: 425–443. [DOI] [PubMed] [Google Scholar]
- Lötsch J, Ahne G, Kunder J, Kobal G, Hummel T (1998). Factors affecting pain intensity in a pain model based upon tonic intranasal stimulation in humans. Inflamm Res 47: 446–450. [DOI] [PubMed] [Google Scholar]
- Lötsch J, Stuck B, Hummel T (2006). The human mu-opioid receptor gene polymorphism 118A>G decreases cortical activation in response to specific nociceptive stimulation. Behav Neurosci 120: 1218–1224. [DOI] [PubMed] [Google Scholar]
- Lötsch J, Walter C, Felden L, Noth U, Deichmann R, Oertel BG (2012). The human operculo-insular cortex is pain-preferentially but not pain-exclusively activated by trigeminal and olfactory stimuli. PLoS One 7: e34798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lovinger DM (2008). Presynaptic modulation by endocannabinoids. Handb Exp Pharmacol 184: 435–477. [DOI] [PubMed] [Google Scholar]
- Lozano-Ondoua AN, Wright C, Vardanyan A, King T, Largent-Milnes TM, Nelson M et al (2010). A cannabinoid 2 receptor agonist attenuates bone cancer-induced pain and bone loss. Life Sci 86: 646–653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maihofner C, Herzner B, Otto Handwerker H (2006). Secondary somatosensory cortex is important for the sensory-discriminative dimension of pain: a functional MRI study. Eur J Neurosci 23: 1377–1383. [DOI] [PubMed] [Google Scholar]
- Maldjian JA, Laurienti PJ, Kraft RA, Burdette JH (2003). An automated method for neuroanatomic and cytoarchitectonic atlas-based interrogation of fMRI data sets. Neuroimage 19: 1233–1239. [DOI] [PubMed] [Google Scholar]
- Manzanares J, Julian M, Carrascosa A (2006). Role of the cannabinoid system in pain control and therapeutic implications for the management of acute and chronic pain episodes. Curr Neuropharmacol 4: 239–257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marsicano G, Wotjak CT, Azad SC, Bisogno T, Rammes G, Cascio MG et al (2002). The endogenous cannabinoid system controls extinction of aversive memories. Nature 418: 530–534. [DOI] [PubMed] [Google Scholar]
- Martin BR, Lichtman AH (1998). Cannabinoid transmission and pain perception. Neurobiol Dis 5(6 Pt B): 447–461. [DOI] [PubMed] [Google Scholar]
- Matsuda LA, Lolait SJ, Brownstein MJ, Young AC, Bonner TI (1990). Structure of a cannabinoid receptor and functional expression of the cloned cDNA. Nature 346: 561–564. [DOI] [PubMed] [Google Scholar]
- Mechoulam R, Gaoni Y (1965). Hashish. IV. The isolation and structure of cannabinolic cannabidiolic and cannabigerolic acids. Tetrahedron 21: 1223–1229. [DOI] [PubMed] [Google Scholar]
- Menon V, Uddin LQ (2010). Saliency, switching, attention and control: a network model of insula function. Brain Struct Funct 214: 655–667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mugler JP 3rd, Brookeman JR (1991). Rapid three-dimensional T1-weighted MR imaging with the MP-RAGE sequence. J Magn Reson Imaging 1: 561–567. [DOI] [PubMed] [Google Scholar]
- Noyes R Jr, Brunk SF, Baram DA, Canter A (1975). Analgesic effect of delta-9-tetrahydrocannabinol. J Clin Pharmacol 15: 139–143. [DOI] [PubMed] [Google Scholar]
- Nurmikko TJ, Serpell MG, Hoggart B, Toomey PJ, Morlion BJ, Haines D (2007). Sativex successfully treats neuropathic pain characterised by allodynia: a randomised, double-blind, placebo-controlled clinical trial. Pain 133: 210–220. [DOI] [PubMed] [Google Scholar]
- Oertel BG, Preibisch C, Martin T, Walter C, Gamer M, Deichmann R et al (2012). Separating brain processing of pain from that of stimulus intensity. Hum Brain Mapp 33: 883–894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oertel BG, Preibisch C, Wallenhorst T, Hummel T, Geisslinger G, Lanfermann H et al (2008). Differential opioid action on sensory and affective cerebral pain processing. Clin Pharmacol Ther 83: 577–588. [DOI] [PubMed] [Google Scholar]
- Ogawa S, Lee TM, Kay AR, Tank DW (1990). Brain magnetic resonance imaging with contrast dependent on blood oxygenation. Proc Natl Acad Sci USA 87: 9868–9872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oshiro Y, Quevedo AS, McHaffie JG, Kraft RA, Coghill RC (2009). Brain mechanisms supporting discrimination of sensory features of pain: a new model. J Neurosci 29: 14924–14931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piomelli D (2003). The molecular logic of endocannabinoid signalling. Nat Rev Neurosci 4: 873–884. [DOI] [PubMed] [Google Scholar]
- Ploghaus A, Tracey I, Clare S, Gati JS, Rawlins JN, Matthews PM (2000). Learning about pain: the neural substrate of the prediction error for aversive events. Proc Natl Acad Sci USA 97: 9281–9286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Price DD (2000). Psychological and neural mechanisms of the affective dimension of pain. Science 288: 1769–1772. [DOI] [PubMed] [Google Scholar]
- Price DD (2002). Central neural mechanisms that interrelate sensory and affective dimensions of pain. Mol Interv 2: 392–403, 339. [DOI] [PubMed] [Google Scholar]
- Reeh PW, Kress M (2001). Molecular physiology of proton transduction in nociceptors. Curr Opin Pharmacol 1: 45–51. [DOI] [PubMed] [Google Scholar]
- Roberts JD, Gennings C, Shih M (2006). Synergistic affective analgesic interaction between delta-9-tetrahydrocannabinol and morphine. Eur J Pharmacol 530: 54–58. [DOI] [PubMed] [Google Scholar]
- Schneider F, Habel U, Holthusen H, Kessler C, Posse S, Muller-Gartner HW et al (2001). Subjective ratings of pain correlate with subcortical-limbic blood flow: an fMRI study. Neuropsychobiology 43: 175–185. [DOI] [PubMed] [Google Scholar]
- Sim K, Cullen T, Ongur D, Heckers S (2006). Testing models of thalamic dysfunction in schizophrenia using neuroimaging. J Neural Transm 113: 907–928. [DOI] [PubMed] [Google Scholar]
- Solowij N, Michie PT, Fox AM (1991). Effects of long-term cannabis use on selective attention: an event-related potential study. Pharmacol BiochemBehav 40: 683–688. [DOI] [PubMed] [Google Scholar]
- Stephan KE, Penny WD, Daunizeau J, Moran RJ, Friston KJ (2009). Bayesian model selection for group studies. Neuroimage 46: 1004–1017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stephan KE, Penny WD, Moran RJ, den Ouden HE, Daunizeau J, Friston KJ (2010). Ten simple rules for dynamic causal modeling. Neuroimage 49: 3099–3109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Svendsen KB, Jensen TS, Bach FW (2004). Does the cannabinoid dronabinol reduce central pain in multiple sclerosis? Randomised double blind placebo controlled crossover trial. BMJ 329: 253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tart CT (1970). Marijuana intoxication common experiences. Nature 226: 701–704. [DOI] [PubMed] [Google Scholar]
- Tarun AS, Bryant B, Zhai W, Solomon C, Shusterman D (2003). Gene expression for carbonic anhydrase isoenzymes in human nasal mucosa. Chem Senses 28: 621–629. [DOI] [PubMed] [Google Scholar]
- Tracey I, Ploghaus A, Gati JS, Clare S, Smith S, Menon RS et al (2002). Imaging attentional modulation of pain in the periaqueductal gray in humans. J Neurosci 22: 2748–2752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Hell HH, Bossong MG, Jager G, Kristo G, van Osch MJ, Zelaya F et al (2011). Evidence for involvement of the insula in the psychotropic effects of THC in humans: a double-blind, randomized pharmacological MRI study. Int J Neuropsychopharmacol 14: 1377–1388. [DOI] [PubMed] [Google Scholar]
- Walker JM, Huang SM (2002). Cannabinoid analgesia. Pharmacol Ther 95: 127–135. [DOI] [PubMed] [Google Scholar]
- Walker JM, Strangman NM, Huang SM (2001). Cannabinoids and pain. Pain Res Manag 6: 74–79. [DOI] [PubMed] [Google Scholar]
- Walter C, Dimova V, Bu J, Parnham MJ, Oertel BG, Lotsch J (2015. a). Inverted perceptual judgment of nociceptive stimuli at threshold level following inconsistent cues. PLoS One 10: e0132069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walter C, Ferreiros N, Bishay P, Geisslinger G, Tegeder I, Lotsch J (2013). Exogenous Delta9-tetrahydrocannabinol influences circulating endogenous cannabinoids in humans. J Clin Psychopharmacol 33: 699–705. [DOI] [PubMed] [Google Scholar]
- Walter C, Oertel BG, Lötsch J (2015. b). THC may reproducibly induce electrical hyperalgesia in healthy volunteers. Eur J Pain 19: 516–518. [DOI] [PubMed] [Google Scholar]
- Wang YY, Chang RB, Liman ER (2010). TRPA1 is a component of the nociceptive response to CO2. J Neurosci 30: 12958–12963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Worsley KJ, Friston KJ (1995). Analysis of fMRI time-series revisited—again. Neuroimage 2: 173–181. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.