Summary
The history of algodystrophy is controversial and its denomination has changed significantly over time. Silas Weir Mitchell described several cases of causalgia due to gunshot wounds that occurred during the American Civil War, increasing knowledge about this clinical condition. A later key milestone in the history of CRPS is tied to the name of Paul Sudeck that, using X-ray examinations, described findings of bone atrophy following a traumatic event or infection of the upper limb. The most widely accepted pathogenic hypothesis, proposed by Rene Leriche, supported a key role of the sympathetic nervous system in the onset of the typical clinical picture of the disease, which was thus defined as “reflex sympathetic dystrophy”. In the 50s John J. Bonica proposed a staging of CRPS. In a consensus conference held in Budapest in 2003, it was proposed a new classification system that included the presence of at least two clinical signs included in the four categories and at least three symptoms in its four categories. There have been other classification systems proposed for the diagnosis of CRPS, such as Veldman diagnostic criteria based on the presence of at least 4 signs and symptoms of the disease associated with a worsening of the same following the use of the limb and their location in the same area distal to the one that suffered the injury. On the other hand, the Atkins diagnostic criteria are much more objective than those proposed by IASP and are specifically applicable to an orthopaedic context. However, current classification systems and related criteria proposed to make a diagnosis of CRPS, do not include instrumental evaluations and imaging, but rely solely on clinical findings. This approach does not allow an optimal disease staging especially in orthopaedics.
Keywords: complex regional pain syndrome, neurogenic inflammation, vasomotor system, diagnosis, historical article
Historical perspective of CRPS
There are only few diseases that have such a controversial history as the Complex Regional Pain Syndrome (CRPS). Even its denomination underwent several changes to emphasize the prevalent pathogenic beliefs developed through the history of medicine.
Ambroise Paré (Figure 1), father of the modern surgery, was the first to describe a disorder that could be related to the current concept of CRPS. He successfully treated a severe and persistent pain syndrome that occurred to the French King Charles IX of Valois after a limb phlebotomy. It is said that thanks to his diagnostic and therapeutic skills, offered to the house of Valois, he managed to live a long life (about 80 years) in an historical period when male life expectancy was usually low. In fact, during the night of St. Bartholomew, when the massacre of the Huguenots was perpetrated, King Charles IX hid him in his closet and saved him. Paré identified also the “Phantom Limb” syndrome, another chronic painful disease, clinically close to CRPS (1).
Figure 1.
Portrait of James Bertrand representing the french surgeon Ambroise Paré.
The first written description of CRPS was made by Denmark, a british surgeon that used to work at the Royal Navy Hospital in the Hampshire. He published a case report of a soldier wounded by a bullet that had passed through his upper arm in the supracondylar region of the humerus during the siege of Badajoz (1812). The wound healed quickly but Doctor Denmark reported the following clinical situation at discharge: “I always found him with the forearm bent and in supine position and supported by the firm grasp of the other hand. The pain was of a ‘burning’ nature, and so violent as to cause a continual perspiration from his face”. Denmark linked the persistent and burning pain to the involvement of the radial nerve in the gunshot injury of the upper arm (2).
This accurate clinical case report was ignored at the time; however a few decades later the description of other clinical cases of gunshot wounds, occurred during the American Civil War, had a different fate. This was mainly due to Silas Weir Mitchell (Figure 2) and its good communication skills.
Figure 2.
Silas Weir Mitchell, american physician.
Silas Weir Mitchell was a doctor who dedicated the first years of his career to the care of wounded soldiers, in particularly in peripheral nerve injuries caused by gunshots, during the American Civil War. He was also a skilled storyteller and he included in his publications interesting psychological considerations in the clinical cases descriptions. In 1864 he published, in collaboration with George Morehouse and William Keen, the monograph “Gunshot Wounds and Other Injuries” that soon became the benchmark for the diagnosis and treatment of nerve damage until World War I.
Among the diseases accurately described by Mitchell there was a syndrome characterized by a typical chronic burning pain located distally to the peripheral nerve injury site and associated with skin disorders. The description given by the Author was very suggestive and finely described the signs and the symptoms characteristic of what we now call CRPS.
“The skin affected in these cases was deep red or mottled, and red and pale in patches. The subcuticular tissues were nearly all shrunken and, where the palm alone was attacked, the part so diseased seemed to be a little depressed, firmer and less elastic than common. In the fingers there were often cracks in the altered skin, and the integuments presented the appearance of being tightly drawn over the subjacent tissues. The surface of all the affected parts was glossy and shiny as though it had been skillfully vanished. Nothing more curious than these red and shining tissues can be conceived of. In most of them the part was devoid of wrinkles and perfectly free from hair”.
Mitchell had a scientific correspondence with another great physician of that time, Sir James Paget, surgeon of the Queen Victoria, who believed that this disease was very similar to frostbite. “Mr. Paget’s comparison of chilblains is one we often use to describe these appearances, but in some instances we have been more strikingly reminded of the characters of certain large thin and polished scars” (3). Mitchell identified the primitive pathogenic role of the peripheral nerve injury and wrote that it was necessary to further investigate its features.
“Further study led us to suspect that the irritation of a nerve at the point of the wound might give rise to changes in the circulation and nutrition of the parts in its distribution, and that these alterations might be of themselves of a pain-producing nature” (4).
This clinical condition was later described as ‘causalgia’ in ‘Injuries of Nerves and Their Consequences’, a second book published by Mitchell in 1872 (5). He stated that the term was coined by Robley Dunglison in the first edition of Dictionary of Medical Science in 1874 (6). It seems to derive from the crasis between the Greek words καυσóς (heat) and ἄλγος (pain) to emphasize the clinical features of the body region affected by the pathological condition.
Another important step in the history of this disease is due to Paul Sudeck (Figure 3).
Figure 3.
Paul Sudeck.
In 1900 at the 29th Congress of the German Society of Surgery, Sudeck presented a paper entitled ‘Acute inflammatory bone atrophy’ describing the results of his experiments on patients who had undergone X-ray examinations (7). This radiographic technique had been very recently introduced into clinical practice and Sudeck had quickly become an expert.
He described examples of bone atrophy that could occur after an acute inflammation of the fingers, fractures of scaphoid, radius or shoulder, after ligament injury, soft tissue infection, nerve injury or herpes zoster infection.
Sudeck reported that this condition often disappeared as quickly as it had appeared and recovered fully, but sometimes persisted for a long time in an extremely disabling chronic form. The description he gave is very accurate and current:
“Irregular obliteration of the pattern of bony striation,… diffuse reduction in radiodensity of the bone image, with lacunae of spongiform bone,…the cortex is striated, especially in the digits, but does not show a reduction in thickness… It is likely that, in sites distant from the site of the illness, it takes the form of an inflammatory irritation, which involves nutritional problems… and in consequence resorption of bone. Evidently, it is not by nature a physiological resorption of inactive bone, but if I may so put it, an active atrophy”.
Nonne, a student of Sudeck, in the following year coined the name “Sudeck’s atrophy” for this particular form of bone atrophy and integrated the classification of atrophy proposed by Sudeck, describing five forms of the disease as following (8):
nutritional atrophy
disuse atrophy
senile atrophy
acute inflammatory reflex atrophy (Sudeck’s atrophy)
neuropathic atrophy.
The fundamental contribution from this great surgeon to the history of this disease is highlighted by the fact that ‘Sudeck’s atrophy’ is still a common term used to define algodystrophy.
Another milestone in the history of CRPS was the hypothesis that the sympathetic nervous system plays a major role in the origin of the signs and symptoms of the disease. This hypothesis was embraced by Rene Leriche (Figure 4), a military surgeon during World War I in Strasbourg.
Figure 4.
Rene Leriche.
In 1917, Leriche described a patient who complained of chronic hand pain and numbness after a gunshot wound on the right armpit. There were no ischemic signs. Leriche performed the first periarterial sympathectomy on this patient and referred of a complete resolution of the pain syndrome within two weeks. This surgical technique was later successfully used in other major syndromes characterized by vasomotor disturbances, such as Raynaud’s disease and scleroderma. Leriche coined the term “sympathetic neuritis” to show the fundamental role, in his opinion, of the sympathetic nervous system in the pathogenesis of neuropathic pain (9).
The role of sympathetic activity in the genesis of several forms of chronic neuropathic pain syndromes was further stressed by James A. Evans, a physician at the Lahey Clinic in Burlington, Massachusetts, to whom we owe the term ‘Reflex Sympathetic Dystrophy’ (RSD). Between 1946 and 1947 he described 57 patients with a chronic pain syndrome characterized by intense pain and clinical signs that he explained as ‘sympathetic stimulation ‘(…) that is rubor, pallor or a mixture of both, sweating and atrophy (…)’. This syndrome had appeared after fractures (21%), sprains (21%), vascular complications (19%), amputation (9%), arthritis or osteitis (5%) and lacerations (2%) or minor injuries, including contusions (9%) and postural defects of the foot (7%). Evans noticed that sympathetic blocks usually relieved the pain, confirming the hypothesis that the condition was connected to an abnormality of the sympathetic nervous system. He supported the theory that an excess of afferential input related to the damaged tissue could start a chain of activation involving sympathetic neurons. The activity of sympathetic postganglionic fibers could produce spasms of the arteries and therefore ischemia with increased capillary filtration pressure, edema and swelling (10–13).
One year after Evans coined the term ‘Reflex Sympathetic Dystrophy (RSD)’, Philip S. Foisie, a surgeon working at the Boston City Hospital, suggested another pathogenic hypothesis. He stated that a persistent but low-grade arterial spasm appeared after the soft tissue injury could lead to a severe pain syndrome with allodynia, edema, muscle atrophy, osteoporosis, joint stiffness and reduced mobility. Foisie essentially argued that RSD might be better defined as a ‘traumatic arterial vasospasm’. According to him, the vasospasm of arterioles could lead to a decreased nutritive supply causing degenerative changes especially in the musculoskeletal system. He observed that the syndrome was even more likely in patients with compression injuries with an intracompartmental pressure increase. The ischemia might cause a microvascular damage that would further increase plasma extravasation due to the increased permeability of the capillary walls (14).
It should be emphasized that both Evans and Foisie suggested that sympathetic nerve blocks might be useful to relieve the pain. Evans sustained that the increased activity of the efferent sympathetic fibers was crucial for the maintenance of the vicious circle, while Foisie believed that the peripheral lesion was able to trigger the vasospasm. In the light of the current knowledge about the pathogenesis of CRPS, the theory of Foisie was certainly more reliable, but ironically it was not taken into consideration by the international scientific community, as shown by the fact that it was never cited even a few years after the publication, while Evans’ theory collected a remarkable mediatic success, so much so that the term ‘Reflex Sympathetic Dystrophy’ remained in place for decades and it’s still widely used.
In the 1950s, Algology, a new medical discipline, was born as an offshoot of Anesthesiology. The birth certificate could be identified in 1953 when John Bonica (Figure 5) published the book ‘The Management of Pain’ (15).
Figure 5.
John J. Bonica, founder of IASP.
He was an anesthesiologist from Filicudi, Sicily, who emigrated to New York with his family at the age of 11 years; he devoted much of his professional and research activity to pain syndromes care. He was the first to propose a staging for RSD with three clinical types deemed to be subsequent to each other. According to Bonica there are three stages of the disease:
- Stage 1 (acute), from the moment of the trauma to 3 months after, characterized by erythema, calor, edema, marked hyperhidrosis, a distribution of the pain not related to root nor nerve involvement, limited range of motion and reduced muscle strength with a negative X-ray examination, but a positive scintigraphy showing hyperaccumulation;
- Stage 2 (dystrophic), characterized by severe pain, edematous skin, decreased hair growth, discoloration with cyanotic areas, persistent hyperhidrosis, muscle weakness and limited range of motion of the affected joint or joints;
- Stage 3 (atrophic), from 6 weeks onwards, is characterized by decreased but still disabling pain that improves with rest and worsens with passive movements. The skin could be atrophic, thin, dry, sometimes ulcerated, cold, mottled or cyanotic in toto; there could be loss of joint range of motion and muscle strength with tendon atrophy, contractures, tremors and dystonia determining a significant motor impairment of the affected limb. At this stage the radiographic examination shows inhomogeneous regional osteoporosis (Sudeck’s atrophy).
Among the merits of John Bonica there was also the foundation of the first scientific society devoted exclusively to the study of pain in 1973: The International Association for the Study of Pain (IASP). One of the several aims of the society was to standardize the taxonomy of the complex world of pain, in particular chronic pain. Among the several types of chronic pain the one reported in Reflex Sympathetic Dystrophy was challenging to define. A first consensus conference was organized by IASP in 1988 at Schloss Rettershof, near Frankfurt, and a second one in Orlando, Florida in 1993 (16), in order to create shared criteria that could support the diagnosis of Reflex Sympathetic Dystrophy. Firstly, it was established that the dystrophic aspect was entirely secondary to the more clinically significant pain symptom, and Bonica proposed to rename the disease as ‘Complex Regional Pain Syndrome (CRPS)’. In fact he wanted to emphasize that the predominant aspect of the disease was the localization of pain in a particular anatomical region, not necessarily limited to the distribution of roots or nerves. The adjective ‘complex’ was related to the very diverse pathogenic and clinical aspects of this syndrome.
Therefore, the Orlando conference established that CRPS could be diagnosed in presence of the following conditions:
a noxious event or immobilization able to start the process;
allodynia, hyperalgesia or anyway pain out of proportion compared to the precipitating event;
presence of edema, changes in skin blood flow or abnormal sudomotor activity of the affected region in any stage of the disease process;
the diagnosis can be excluded if the presence of this kind of pain and dysfunction could be related to other diseases.
According to IASP, CRPS is a syndrome characterized by a continuing regional pain (spontaneous and/or evoked) that is seemingly disproportionate in time or degree to the usual course of any known trauma or other lesion. The pain is regional (not in specific nerve territory or dermatome) and usually has a distal predominance of abnormal sensory, motor, sudomotor, vasomotor, and/or trophic findings. The syndrome shows variable progression over time.
In the same conference in Orlando it was decided to discriminate between the form characterized by the evidence of obvious nerve damage (CRPS type II, corresponding to causalgia) and the form without demonstrable nerve lesions (CRPS type I).
Although CRPS type I and II had clinical features that can overlap considerably, there are important differences between the two forms. CRPS type II is characterized by a typical neuropathic pain; on the other hand, CRPS type I shows the characteristics of mixed or even mainly nociceptive pain. CRPS type II can also develop after a clearly detectable injury to a nerve or plexus, while in CRPS type I peripheral nerve damage is rarely detectable.
Orlando Conference Criteria showed a high sensitivity, close to 90%, but a low specificity, less than 50%, thus resulting in misdiagnosing diseases very different from CRPS. In other words they were able to intercept all patients with CRPS on the basis of particular clinical features. Yet, according to critics, they included even those who were not suffering from CRPS but from other medical conditions with similar clinical features. For example, IASP Orlando criteria for the diagnosis of CRPS would be met by nearly 40% of patients with diabetic neuropathy. In fact they show mechanical allodynia, changes in skin temperature and asymmetries often associated with edema.
Then it also appeared another major issue of these diagnostic criteria: they are not based on objective data but only on reported symptoms.
Norman Harden, a Chicago Pain Medicine Specialist, and Stephen Bruehl, Pain Medicine Specialist in Washington, both prominent members of IASP Task Force on CRPS, published in 1999 two articles about a multicentric study carried out in order to test the internal validity (which defined whether the classification criteria were correct in the sample of individuals included in the study) and the external validity (which defined the degree of generalizability of the findings of a study to the entire population) of the Orlando criteria (17, 18). Their purpose was to check if CRPS patients showed such a complex of diagnostic symptoms and if these criteria allowed discriminating between patients suffering from real CRPS and those suffering from similar conditions (e.g. diabetic neuropathy). Moreover they sought to identify whether some signs not included in the diagnostic criteria, such as motor abnormalities or trophic changes, were frequent enough to be added to them.
The results of the study led to a proposal of a substantial revision of the Orlando criteria. The main change proposed by Harden et al. was to add clinical signs, as shown in Figure 6 (17).
Figure 6.
Revision of CRPS diagnostic criteria proposed by Harden et al.
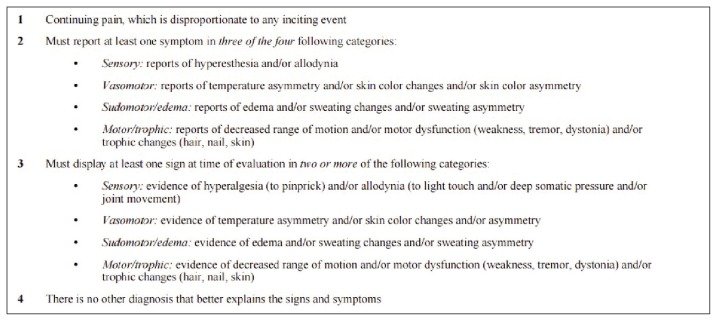
In a subsequent consensus conference held in Budapest in 2003 a new classification system was proposed. It involved the presence of at least two clinical signs included in the four categories and at least three symptoms in its four categories, as shown in Figure 7 (19).
Figure 7.
Budapest diagnostic criteria for CRPS.
With the reduction of the number of symptoms needed (three instead of four) the criteria showed a sensitivity of 0.85 and a specificity of 0.69, which was a good compromise between the ability to find the patients affected by CRPS and the inclusion of those not suffering from typical CRPS.
It was proposed to keep within the classification criteria the need of four symptoms to diagnose CRPS in order to provide greater strength to the results of the studies. It should be highlighted, however, that this discrepancy represents a weak point in the Budapest criteria.
The IASP Task Force for the classification of chronic pain accepted and codified the “Budapest criteria” both for diagnosis and for clinical research. The same IASP Task Force also identified a subpopulation consisting of approximately 15% of subjects definitely affected by CRPS that did not meet the above criteria. Therefore they thought it was necessary to add a third subtype called “CRPS - not otherwise specified”. Thus IASP suggested the final classification, showed in Figure 8 (20–23).
Figure 8.
Subtypes of CRPS proposed by IASP.
Other diagnostic criteria have been proposed for CRPS. Peter Veldman, a dutch surgeon, proposed in 1993 the following criteria (24):
-
Four or five of these conditions:
unexplained diffuse pain
difference in skin colour relative to other limb
diffuse edema
difference in skin temperature relative to other limb
limited active range of motion.
Occurrence or increase of above signs and symptoms after use
Above signs and symptoms present in an area larger than the area of primary injury or operation and including the area distal to the primary injury.
Veldman published a paper on Lancet, supporting the hypothesis of an inflammatory pathogenesis of CRPS, already formulated by Sudeck in his last years of scientific activity (25). He believed that CRPS is due to an exaggerated inflammatory response to a local noxious stimulus, emphasizing that the secondary muscle damage had a prominent role in the clinical picture of this disease characterized by disabling pain. Veldman criticized the subdivision in stages proposed by IASP algologists and identified cold forms, less frequent, and warm forms, more common (24).
Moreover, Atkins et al. (26) proposed diagnostic criteria for CRPS applicable specifically in the orthopaedic field:
- neuropathic pain, nondermatomal, without cause, burning, with associated allodynia and hyperpathia;
- vasomotor instability and abnormalities of sweating. Warm red and dry, cool blue, and clammy or an increase in temperature sensitivity. Associated with an abnormal temperature difference between the limbs;
- swelling;
- loss of joint mobility with associated joint and soft tissue contracture, including skin thinning and hair and nail dystrophy.
These clinical findings are backed up by an increased uptake on delayed bone scintigraphy early in CRPS and a radiographic evidence of osteoporosis after 3 months.
The diagnosis is excluded by the existence of conditions that would otherwise account for the degree of dysfunction.
These criteria came up from orthopaedic experience, in particular of the upper limb trauma and they are much more objective than IASP ones.
Critical issues of the IASP classification (Budapest Criteria)
IASP criteria that were defined during Budapest consensus conference must be considered valid for the diagnosis of chronic pain in CRPS in a clinical setting in order to provide differential diagnosis with other causes of chronic pain. Therefore these criteria lose their validity if applied to other settings such as an orthopaedic environment. Their most useful value lies not in the ability to allow a clear diagnosis, but to lay the foundation of an appropriate differential diagnosis with other forms of chronic neuropathic pain, such the one experienced by the patient suffering from diabetic neuropathy. Moreover, the flexibility of these criteria are supported by the same IASP members that modified the number of positive diagnostic criteria required in clinical setting compared to those required in the field of scientific research.
It is well known that Budapest criteria do not include diagnostic imaging measures. In long term chronic pain it could be possible to find a positive scintigraphy and/or nuclear magnetic resonance, but there is no doubt that in the early stages of CRPS an increased uptake on bone scintigraphy or the presence of edema on nuclear magnetic resonance should be considered as always present. At a subsequent stage, the bone scan returns to normality, but, on conventional radiography, a rapid loss of bone mass might appear in subchondral or subperiosteal areas, caused by marked demineralization, which can involve progressively the whole affected district. At this stage also the magnetic resonance imaging does not show bone marrow edema.
In our opinion, imaging evaluation should be incorporated within the system of CRPS diagnostic criteria, allowing a better staging of the disease process and providing important information on the effectiveness of the therapeutic intervention used.
Moreover, considering the wide variety in terms of type and amount by which CRPS signs and symptoms could appear, we propose an algorithm (Figure 9) that could explain in a simple but comprehensive way the nosological classification which in our opinion this disease should have.
Figure 9.
Hypothesis of pathogenic factors leading to CRPS.
Conclusions
The CRPS is a complex clinical syndrome that detects several contributing factors, in particular concerning the traumatic or surgical events. The clinical presentation of this syndrome is a consequence of a multifactorial pathogenic process that recognizes peripheral and central mechanisms and has extremely variable clinical manifestations (27–29).
An early diagnosis is mandatory for therapeutic success and functional outcome. The therapeutic approach with more possibilities of success in the early stages is eminently pharmacological, because the inhibition of an altered inflammatory response might be resolutive; in an advanced phase it will be necessarily global.
This comprehensive approach should include not only a pharmacological therapy, but also physical therapy, therapeutic exercise, and neurorehabilitation, psychological and educational interventions to modulate chronic pain.
References
- 1.Paré A. Of the Cure of Wounds of the Nervous System. The Collected Works of Ambroise Pare; Milford House, New York: 1634. [Google Scholar]
- 2.Denmark A. An Example of Symptoms resembling Tic Douleureux, produced by a wound in the Radial Nerve. Med Chir Trans. 1813;4:48–52. [PMC free article] [PubMed] [Google Scholar]
- 3.Paget J. Clinical lecture on some cases of local paralysis. Med Times and Hosp Gaz Lond. 1864;1:331–2. [Google Scholar]
- 4.Mitchell SW, Morehouse GR, Keen WW. Gunshot Wounds and Other Injuries of Nerves. JB Lippincott; Phildelphia: 1864. [DOI] [PubMed] [Google Scholar]
- 5.Mitchell SW. Injuries of nerves and their consequences. JB Lippincott; Phildelphia: 1872. [Google Scholar]
- 6.Dunglison R. A Dictionary of Medical Science. Philadelphia: Blanchard & Lea; 1874. [Google Scholar]
- 7.Sudeck P. Über die akute entzündliche Knochenatrophie. Arch Klin Chir. 1900;62:147–56. [Google Scholar]
- 8.Nonne M. Über radiographisch nachweisbare akute und kronisch “Knochenatrophie” (Sudek) bei Nerve-Erkrankungen. Fortschr Geb Roentgenstr. 1901–1902;5:293–7. [Google Scholar]
- 9.Leriche R. De la causalgie envisagee comme une nevrite due sympathique et de son traitment par la denudation et l’excision des plexus nerveux peri-arteriels. Presse Medicale. 1916;24:178–80. [Google Scholar]
- 10.Evans JA. Reflex sympathetic dystrophy. Surg Clin North America. 1946;26:780–90. [PubMed] [Google Scholar]
- 11.Evans JA. Reflex sympathetic dystrophy. Surg Gynecol Obstet. 1946;82:36–44. [PubMed] [Google Scholar]
- 12.Evans JA. Sympathectomy for reflex sympathetic dystrophy: A case report of twenty-nine cases. JAMA. 1946;132:620–3. doi: 10.1001/jama.1946.02870460010003. [DOI] [PubMed] [Google Scholar]
- 13.Evans JA. Reflex sympathetic dystrophy: report of 57 cases. Ann Intern Med. 1947;26:417–26. doi: 10.7326/0003-4819-26-3-417. [DOI] [PubMed] [Google Scholar]
- 14.Foisie PS. Traumatic arterial vasospasm. N Engl J Med. 1947;237:295–302. doi: 10.1056/NEJM194708282370901. [DOI] [PubMed] [Google Scholar]
- 15.Bonica JJ. The Management of Pain. Lea & Febiger; Philadelphia: 1953. [Google Scholar]
- 16.Merskey H, Bogduk N. International Association for the Study of Pain Task Force on Taxonomy: classification of chronic pain: descriptions of chronic pain syndromes and definitions of pain terms. 2nd edition. Seattle (WA): IASP Press; 1994. [Google Scholar]
- 17.Harden RN, Bruehl S, Galer BS, Saltz S, Bertram M, Backonja M, Gayles R, Rudin N, Bhugra MK, Stanton-Hicks M. Complex regional pain syndrome: are the IASP diagnostic criteria valid and sufficiently comprehensive? Pain. 1999;83(2):211–9. doi: 10.1016/s0304-3959(99)00104-9. [DOI] [PubMed] [Google Scholar]
- 18.Bruehl S, Harden RN, Galer BS, Saltz S, Bertram M, Backonja M, Gayles R, Rudin N, Bhugra MK, Stanton-Hicks M. External validation of IASP diagnostic criteria for Complex Regional Pain Syndrome and proposed research diagnostic criteria. International Association for the Study of Pain. Pain. 1999;81(1–2):147–54. doi: 10.1016/s0304-3959(99)00011-1. [DOI] [PubMed] [Google Scholar]
- 19.Harden RN, Bruehl S, Perez RS, Birklein F, Marinus J, Maihofner C, Lubenow T, Buvanendran A, Mackey S, Graciosa J, Mogilevski M, Ramsden C, Chont M, Vatine JJ. Validation of proposed diagnostic criteria (the “Budapest Criteria”) for Complex Regional Pain Syndrome. Pain. 2010;150(2):268–74. doi: 10.1016/j.pain.2010.04.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bruehl S, Harden RN, Galer BS, Saltz S, Backonja M, Stanton-Hicks M. Complex regional pain syndrome: are there distinct subtypes and sequential stages of the syndrome? Pain. 2002;95(1–2):119–24. doi: 10.1016/s0304-3959(01)00387-6. [DOI] [PubMed] [Google Scholar]
- 21.Harden RN, Baron R, Janig W. Complex Regional Pain Syndrome, Progress in Pain Research and Management. Vol. 22. IASP Press; Seattle: 2001. [Google Scholar]
- 22.Harden RN, Bruehl S, Stanton-Hicks M, Wilson PR. Proposed new diagnostic criteria for complex regional pain syndrome. Pain Med. 2007;8(4):326–31. doi: 10.1111/j.1526-4637.2006.00169.x. [DOI] [PubMed] [Google Scholar]
- 23.Harden RN, Bruehl S, Perez RS, Birklein F, Marinus J, Maihofner C, Lubenow T, Buvanendran A, Mackey S, Graciosa J, Mogilevski M, Ramsden C, Chont M, Vatine JJ. Validation of proposed diagnostic criteria (the “Budapest Criteria”) for Complex Regional Pain Syndrome. Pain. 2010;150(2):268–74. doi: 10.1016/j.pain.2010.04.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Veldman PH, Reynen HM, Arntz IE, Goris RJ. Signs and symptoms of reflex sympathetic dystrophy: prospective study of 829 patients. Lancet. 1993;342(8878):1012–6. doi: 10.1016/0140-6736(93)92877-v. [DOI] [PubMed] [Google Scholar]
- 25.Sudeck P. Die sogen akute Knochenatrophie als Entzündungsvorgang. Der Chirurg. 1942;15:449–58. [Google Scholar]
- 26.Atkins RM, Duckworth T, Kanis JA. Algodystrophy following Colles’ fracture. J Hand Surg Br. 1989;14(2):161–4. doi: 10.1016/0266-7681_89_90118-6. [DOI] [PubMed] [Google Scholar]
- 27.Harden RN, Bruehl S, Perez RS, Birklein F, Marinus J, Maihofner C, Lubenow T, Buvanendran A, Mackey S, Graciosa J, Mogilevski M, Ramsden C, Schlereth T, Chont M, Vatine JJ. Development of a severity score for CRPS. Pain. 2010;151(3):870–6. doi: 10.1016/j.pain.2010.09.031. [DOI] [PubMed] [Google Scholar]
- 28.Marinus J, Moseley GL, Birklein F, Baron R, Maihöfner C, Kingery WS, van Hilten JJ. Clinical features and pathophysiology of complex regional pain syndrome. Lancet Neurol. 2011;10(7):637–48. doi: 10.1016/S1474-4422(11)70106-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Burton AW, Bruehl S, Harden RN. Current diagnosis and therapy of complex regional pain syndrome: refining diagnostic criteria and therapeutic options. Expert Rev Neurother. 2005;5(5):643–51. doi: 10.1586/14737175.5.5.643. [DOI] [PubMed] [Google Scholar]