SUMMARY
OBJECTIVE
A population-based study of 135 multidrug-resistant tuberculosis (MDR-TB) patients reported to the Centers for Disease Control and Prevention (CDC) during 2005–2007 found 73% were hospitalized. We analyzed factors associated with hospitalization.
METHODS
We assessed statistically significant multivariable associations with US in-patient TB diagnosis, frequency of hospitalization, length of hospital stay, and in-patient direct costs to the health care system.
RESULTS
Of 98 hospitalized patients, 83 (85%) were foreign-born. Blacks, diabetics, or smokers were more likely, and patients with disseminated disease less likely, to receive their TB diagnosis while hospitalized. Patients aged ⩾65 years, those with the acquired immune-deficiency syndrome (AIDS), or with private insurance, were hospitalized more frequently. Excluding deaths, length of stay was greater for patients aged ⩾65 years, those with extensively drug-resistant TB (XDR-TB), those residing in Texas, those with AIDS, those who were unemployed, or those who had TB resistant to all first-line medications vs. others. Average hospitalization cost per XDR-TB patient (US$285 000) was 3.5 times that per MDR-TB patient (US$81 000), in 2010 dollars. Hospitalization episode costs for MDR-TB rank third highest and those for XDR-TB highest among the principal diagnoses.
CONCLUSIONS
Hospitalization was common and remains a critical care component for patients who were older, had comorbidities, or required complex management due to XDR-TB. MDR-TB in-patient costs are among the highest for any disease.
Keywords: TB; drug resistance; cost, hospitalization; HIV/AIDS
In the United States, hospitalization is the most expensive component of management of tuberculosis (TB), including multidrug-resistant TB (MDR-TB, defined as TB resistant to at least isoniazid [INH] and rifampin [RMP]).1,2 Internationally, hospitalization and medication costs are the highest cost categories for MDR-TB care.3-5 The World Health Organization recommends out-patient MDR-TB treatment, due to its cost effectiveness.6 In a US study of human immunodeficiency virus (HIV) negative MDR-TB patients with resistance to a median of three drugs, out-patient treatment was feasible.7 To reduce US costs and improve care, there is a need to examine why MDR-TB patients are hospitalized in the United States.
We recently published the treatment practices, outcomes, and direct cost of illness for a population-based sample of 135 MDR-TB cases, including 5 (4%) with extensively drug-resistant TB (XDR-TB, defined as MDR-TB plus resistance to a fluoroquinolone and to a second-line injectable), 23 (17%) with pre-XDR-TB (MDR-TB and resistance to a fluoroquinolone or a second-line injectable), 32 (24%) with total first-line resistance, 58 (43%) with INH/RMP/rifabutin (RBT) resistance plus other resistance, and 17 (13%) with INH/RMP/RBT-only resistance.8 Of the 135 study patients, 98 (73%) were hospitalized more often (range 1–6), for on average 83 days (median 27) for non-XDR-TB and 357 days (median 282) for XDR-TB.8 Severe worsening of disease was the most common reason for hospitalization, accounting for 49/98 (50%) hospitalizations.8 Direct in- and out-patient costs averaged US$134 000 per MDR-TB patient and US$430 000 per XDR-TB patient, in 2010 dollars.8
To describe US MDR-TB in-patient care, we 1) identified patient characteristics associated with in-patient MDR-TB care, 2) present in-patient direct costs by patient characteristics, 3) identified characteristics associated with in-patient MDR-TB direct costs, and 4) compared MDR-TB in-patient costs to those of other diseases.
METHODS
The study was approved by the US Centers for Disease Control and Prevention (CDC) and local institutional review boards, which granted a waiver for patient informed consent and patient authorization. The methods of selecting the population-based sample from California (CA), New York City (NYC), and from Texas (TX) of MDR-TB patients reported to the CDC in 2005–2007 are described elsewhere.8 The sample included 130 MDR-TB and 5 XDR-TB cases, representing 36% of MDR-TB and 56% of XDR-TB US-reported cases during 2005–2007.
Direct in-patient costs to the health care system were calculated as follows. In-patient charges for hospitalizations during anti-tuberculosis treatment were collected from Medicare claims forms and converted to costs using hospital-specific operating cost-to-charge ratios.9 If a specific hospital’s cost-to-charge ratio was unavailable (n = 33 hospitalizations), the state’s average operating-cost-to-charge ratio was used (CA = 0.32, NY = 0.46, TX = 0.40).9 All costs were converted to 2010 US dollars10 and were adjusted for cost of living (CA = 1.13, NY = 1.08, TX = 0.94) to facilitate aggregation.11 We added estimated physician costs12 of US$238 for a moderately complex first day and US$131 for subsequent days, which we converted to costs by multiplying by the average cost-to-charge ratio for pulmonary diseases (0.502),13 and updated to 2010 dollars, for cost estimates of US$124 for the first day and US$68 for subsequent days. For 17 patients for whom hospitalization charge data were unavailable for ⩾1 hospitalization, we estimated the costs by multiplying hospitalization length by the average cost per day (US$1419) for patients for whom we had detailed data. Hospitalization episode costs were calculated using billing data and compared to those of other diseases listed in the Healthcare Cost and Utilization Project (HCUP) National In-patient Sample in 2012.14
We classified patients into three levels of illness severity: 1) those with TB-associated death during treatment, 2) those with any comorbidities, pregnancy, disseminated or extensive TB disease, and 3) those with none of the above factors.
We described in-patient TB diagnosis, hospitalization frequency, length of stay, and direct costs by patient characteristics. We assessed days from initial TB diagnosis to starting two or more second-line TB medications. Except when assessing the association of illness severity with costs, all cost estimates included those of MDR-TB patients who died. We also described in-patient insurance status (public/private) and the proportion of total direct costs contributed by hospitalization.
We report statistically significant multivariable associations of socio-demographic, clinical, and study site characteristics with outcomes: 1) in-patient TB diagnosis (vs. out-patient) based on the date of the first positive specimen, treatment start, or report date (using logistic regression); 2) hospitalization frequency (using Poisson regression); 3) hospital length of stay (using Cox proportional hazards); and 4) in-patient direct costs (using linear regression).
Variables in initial models were selected based on prior knowledge2 or expert opinion, and included sex, age group, race/ethnicity, foreign birth, homelessness, unemployment, illicit substance use, excess alcohol use, smoking, acquired immune-deficiency syndrome (AIDS), diabetes mellitus (DM), pregnancy, TB history, disseminated TB, receipt of TB clinic out-patient care, incarceration in a correctional institution, and long-term care facility residence. The hospitalization frequency, length of stay, and cost models also included drug resistance pattern, insurance status, and study site. The length of stay model excluded 13 patients who died. The hospitalization direct cost model also included hospital length of stay and whether a patient died during treatment to assess the intensity of cost by patient characteristic including illness severity and to control for the total number of days hospitalized, which represents an obvious determinant of total hospitalization cost.
Multivariable regression was used with backwards elimination of variables insignificant at P < 0.05 using SAS version 9.2/9.3 (Statistical Analysis System, Cary, NC, USA). We used backwards elimination to help select the final variables most related to the outcome of interest. Small sample sizes precluded systematic testing of interaction terms. Adjusted odds ratios (aORs) from logistic regression, rate ratios (aRRs) from Poisson regression, hazard ratios (aHRs) from Cox proportional hazards survival analysis, and linear regression coefficients (β) and their associated 95% confidence intervals (CIs) are reported.
RESULTS
Of 135 patients, 98 (73%) were hospitalized during MDR-TB treatment. Each patient was hospitalized for on average 94 days (Table 1). From a review of notations in available medical records, multiple reasons for hospitalization were noted. Severe worsening TB was the reason for 50% of the hospitalizations, followed by required initiation or changing of the treatment regimen (40%), implementation of respiratory isolation (21%), managing adverse events (7%), managing concurrent conditions (3%), and surgery (1%).
Table 1.
Hospitalization indicators by MDR-TB patient characteristic ordered from most to least percentage of total hospitalization costs (n = 135)
| Patient characteristic | n | Patients hospitalized* n |
Proportion of population hospitalized % |
Average hospitalizations/ patient n |
Average time hospitalized days |
Total hospitalization costs 2010 USD |
Average cost/hospitalized patient 2010 USD |
Proportion of hospitalized patients % |
Proportion hospitalization costs % |
|---|---|---|---|---|---|---|---|---|---|
| n | 135 | 98 | 98 | 98 | 97 | 97 | 97 | 98 | 97 |
| All | 135 | 98 | 73 | 1.5 | 94 | 8 694 679 | 89 636 | 100 | 100 |
| Foreign-born | 118 | 83 | 70 | 1.5 | 79 | 6 676 525 | 81 421 | 85 | 77 |
| Male | 68 | 49 | 72 | 1.6 | 100 | 4 801 511 | 97 990 | 51 | 55 |
| Smoker | 31 | 29 | 94 | 1.6 | 139 | 3 827 982 | 131 999 | 30 | 44 |
| Unemployed | 38 | 33 | 87 | 1.4 | 142 | 3 760 707 | 113 961 | 34 | 43 |
| No/unknown insurance while hospitalized | 30 | 30 | 100 | 1.5 | 180 | 3 687 449 | 122 915 | 31 | 42 |
| Asian | 72 | 45 | 63 | 1.7 | 60 | 3 664 970 | 83 295 | 45 | 42 |
| California resident | 78 | 52 | 67 | 1.6 | 46 | 3 650 123 | 71 571 | 53 | 42 |
| Public insurance while hospitalized | 29 | 29 | 100 | 1.8 | 78 | 3 395 038 | 117 070 | 30 | 39 |
| Prior TB | 48 | 35 | 73 | 1.6 | 109 | 3 290 983 | 94 028 | 36 | 38 |
| New York City resident | 40 | 32 | 80 | 1.4 | 74 | 3 024 828 | 94 526 | 33 | 35 |
| Hispanic or Latino | 42 | 35 | 83 | 1.2 | 105 | 2 876 500 | 82 186 | 36 | 33 |
| Self-reported diabetic | 24 | 23 | 96 | 1.6 | 123 | 2 722 214 | 118 357 | 24 | 31 |
| Excess alcohol user | 15 | 14 | 93 | 1.3 | 225 | 2 047 181 | 146 227 | 14 | 24 |
| TB resistant to all first-line medications | 32 | 26 | 81 | 1.4 | 83 | 2 038 124 | 81 525 | 26 | 23 |
| Texas resident | 17 | 14 | 82 | 1.4 | 314 | 2 019 727 | 144 266 | 14 | 23 |
| AIDS | 14 | 14 | 100 | 1.8 | 117 | 1 814 269 | 129 591 | 14 | 21 |
| Pre-XDR-TB | 23 | 17 | 74 | 1.4 | 136 | 1 727 311 | 101 607 | 18 | 20 |
| Homeless | 9 | 9 | 100 | 1.3 | 235 | 1 668 005 | 185 334 | 9 | 19 |
| Injection or non-injection drug user | 12 | 12 | 100 | 1.5 | 176 | 1 606 637 | 133 886 | 12 | 18 |
| Black or African American | 14 | 12 | 86 | 1.7 | 75 | 1 223 666 | 101 972 | 12 | 14 |
| XDR-TB | 5 | 4 | 80 | 1.5 | 357 | 1 141 945 | 285 486 | 4 | 13 |
| Died | 13 | 9 | 69 | 1.9 | 69 | 1 141 209 | 126 801 | 9 | 13 |
| Disseminated disease | 12 | 8 | 67 | 2.4 | 136 | 1 082 961 | 135 370 | 8 | 12 |
| Age ⩾65 years | 8 | 6 | 75 | 3 | 107 | 1 035 581 | 172 597 | 6 | 12 |
| Long-term care resident | 4 | 4 | 100 | 2.2 | 120 | 931 888 | 232 972 | 4 | 11 |
| Private insurance while hospitalized | 18 | 18 | 100 | 1.6 | 41 | 659 599 | 36 644 | 19 | 8 |
Hospitalized patients (n=98) comprised 73% of the total 135 MDR-/XDR-TB patients sampled. For one patient known to be hospitalized, length of stay and costs could not be estimated, hence n=97. Of the race/ethnic categories, the following percentages were foreign-born: 50% of Blacks, 79% of Whites, 93% of Hispanics, 99% of Asians.
MDR-TB = multidrug-resistant TB; USD = US dollar; TB = tuberculosis; AIDS = acquired immune-deficiency syndrome; XDR-TB = extensively drug-resistant TB.
We were able to determine hospitalization insurance status for 76 of the 98 patients who were hospitalized in the 135-patient sample. Of the 76 in-patients, 74% were covered by public sector funding (including 24 Medicaid, 4 Medicare, 2 military, 3 jail/prison, 23 with no insurance in publicly financed hospitals), 25% by private sources (18 private insurance, 1 with no insurance in a private hospital), and 1% (1) had other coverage (i.e., unable to be classified as public or private).
Black patients (aOR 4.9), diabetics (aOR 3.4), or smokers (aOR 3.1) were more likely to be diagnosed with TB while hospitalized, while patients with disseminated disease (aOR 0.1) were less likely to receive a TB diagnosis while hospitalized (Table 2). Patients who received their TB diagnosis while hospitalized had a significantly shorter time (median 7 vs. 12 weeks) to start two or more MDR-TB medications (aHR 2.3). MDR-TB patients with a history of homelessness (aHR 3.6), a history of injection or non-injection drug use (aHR 2.4), or with prior TB (aHR 2.3), also had a shorter time to starting MDR-TB treatment. Controlling for the preceding factors, it took longer for patients who were recently unemployed (aHR 0.4) or had disseminated TB (aHR 0.5) to start two or more MDR-TB medications.
Table 2.
MDR-TB patient characteristics and odds of TB diagnosis during hospitalization compared with diagnosis as out-patient
| Patient characteristic | aOR (95%CI) |
|---|---|
| Black or African American | 4.9 (1.3–19.0) |
| Diabetic, self-report | 3.4 (1.3–9.0) |
| Smoker | 3.1 (1.2–8.0) |
| Disseminated TB* | 0.1 (0.01–0.9) |
Defined as having ⩾2 non-contiguous sites of disease. The following percentages of patients were diagnosed with TB during hospitalization: 57% of Black/African Americans, 46% of diabetics, 45% of smokers, and 8% of patients with disseminated disease.
MDR-TB = multidrug-resistant tuberculosis; aOR = adjusted odds ratio; CI = confidence interval.
Patients with a greater frequency of hospitalizations during MDR-TB treatment included those aged ⩾65 years (aRR 2.5), those with AIDS (aRR 2.0), or those with private insurance (aRR 1.7) (Table 3).
Table 3.
MDR-TB patient characteristics* and rate of hospitalization frequency per patient vs. other MDR-TB patients
| Patient characteristic | aRR (95%CI) |
|---|---|
| Age ⩾65 years | 2.5 (1.4–4.0) |
| AIDS | 2.0 (1.3–3.1) |
| Covered by private insurance | 1.7 (1.1–2.5) |
Persons aged ⩾65 years, those with AIDS and persons with private insurance during hospitalization comprised respectively 6%, 14% and 19% of hospitalized patients.
MDR-TB = multidrug-resistant tuberculosis; aRR = adjusted rate ratio; CI = confidence interval; AIDS = acquired immune-deficiency syndrome.
Excluding those who died during treatment, the length of stay was longer (i.e., aHR of having a short length of stay was less) for patients aged ⩾65 years (aHR 0.1), those with XDR-TB (aHR 0.1), those residing in Texas (aHR 0.1), those with AIDS (aHR 0.2), those with pre-XDR-TB (aHR 0.3), the unemployed (aHR 0.4), or those with resistance to all first-line medications (aHR 0.5) (Table 4).
Table 4.
Patient characteristics and hazard of short length of stay* vs. other in-patients
| Patient characteristic | aHR (95%CI) |
|---|---|
| Age ⩾65 years | 0.1 (0.02–0.3) |
| XDR-TB | 0.1 (0.02–0.3) |
| Texas resident | 0.1 (0.06–0.3) |
| AIDS | 0.2 (0.1–0.4) |
| Pre-XDR-TB | 0.3 (0.1–0.6) |
| Unemployed | 0.4 (0.3–0.7) |
| TB resistant to all first-line medications | 0.5 (0.3–0.9) |
HR ratios show factors associated with a short period of hospitalization. Those with XDR-TB had a low hazard of a short stay, i.e., had long lengths of stay.
aHR = adjusted hazard ratio; CI = confidence interval; XDR-TB = extensively drug-resistant tuberculosis.
While foreign-born patients accounted for 87% (118/135) of the sample and 85% (83/98) of hospitalized patients, hospitalizations in this group represented 77% (US$6.7 million/US$8.7 million) of the burden of hospitalization cost in this population-based sample (Table 1). Costs per hospitalization episode averaged US$54 833 (median US$18 893) for MDR-TB and US$191 374 (median US$248 238) for XDR-TB (Table 5). Because MDR-TB patients averaged 1.5 hospitalization episodes during treatment, MDR-TB costs per patient averaged US$81 212 (median US$45 401) and XDR-TB costs per patient averaged US$285 486 (median US$319 370).
Table 5.
MDR-TB hospitalization costs in 2010 dollars
| Length of stay (n = 97) |
Cost/episode (n = 119) |
Cost/patient (n = 97) |
||||
|---|---|---|---|---|---|---|
| Average | Median | Average | Median | Average | Median | |
| MDR-/XDR-TB | 94 | 28 | 60 570 | 19 149 | 89 636 | 49 098 |
| MDR-TB | 83 | 27 | 54 833 | 18 893 | 81 212 | 45 401 |
| XDR-TB | 357 | 282 | 191 374 | 248 238 | 285 486 | 319 370 |
MDR-TB = multidrug-resistant tuberculosis; XDR-TB = extensively drug-resistant TB.
In bivariate analysis excluding in-patients who died of TB-related causes during MDR-TB treatment (n = 9, median US$58 052), costs were significantly greater (P < 0.05) for patients with moderate illness severity than for the remaining MDR-TB patients (n = 27, median US$85 445 vs. n = 61, median US$30 164). However, the multivariable cost model (goodness of fit R2 = 0.69) did not retain illness severity after controlling for number of days hospitalized (β=US$688): individual in-patient costs were greater for long-term care residents (β=US$108 448) or for patients with public insurance (β=US$35 616), and less for Texas residents (β=−US$97 984) than for other in-patients.
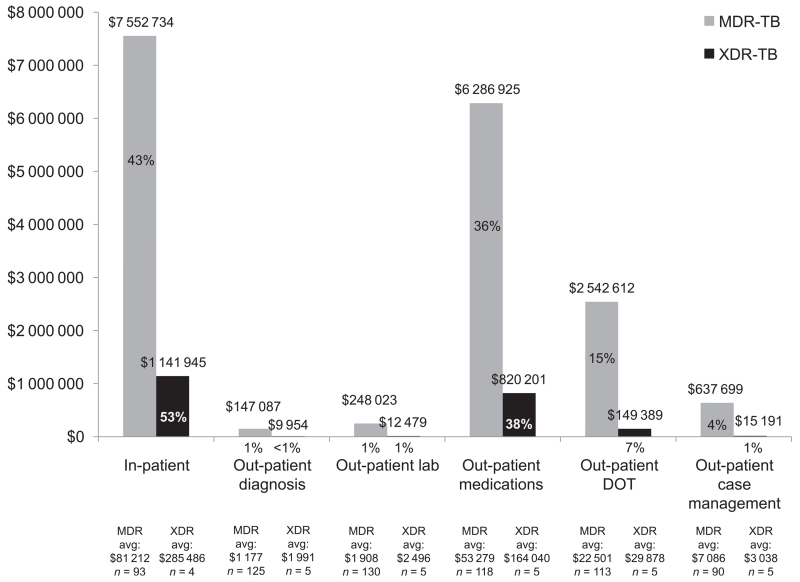
Hospitalization was the highest MDR-TB cost category, representing 44% of combined MDR/XDR-TB costs or, separately, 43% of MDR-TB and 53% of XDR-TB direct costs (Figure). The cost of out-patient medications (average US$76 000 or 36% of MDR-TB and US$201 000 or 38% of XDR-TB direct costs) was the next highest cost category.
Figure.
Composition of MDR-TB direct costs in 2010 dollars. MDR-TB = multidrug-resistant tuberculosis; XDR-TB = extensively drug-resistant TB; lab = laboratory; DOT = directly observed therapy.
From the HCUP, the average cost (converted to 2010 dollars) for any TB hospitalization episode, including drug-susceptible TB, was approximately US$23 000 and ranked 24th among 262 principal diagnosis categories.14 If drug-resistant TB were considered separately, using costs from this study, MDR-TB in-patient costs (US$55 000 per episode) would rank third, after respiratory distress (US$62 000) and pre-term birth (US$58 000), and XDR-TB in-patient costs (US$191 000 per episode) would top the list.
DISCUSSION
This study found a high rate of treatment success in a resource-rich setting with hospitalization commonly used for MDR-TB treatment. Whether such high success could be achieved in the United States without hospitalization could not be addressed in the study. However, in the United States, hospitalization remains a critical component of MDR-TB care for approximately three fourths of patients, many of whom require complex management. MDR-TB patients who were older, had AIDS, had disease resistant to multiple anti-tuberculosis medications, or were long-term care residents, had more frequent, longer, or more costly hospitalizations.
MDR-TB and XDR-TB patients can be treated primarily in an out-patient setting. However, the percentage of MDR-TB patients hospitalized did not change significantly over time compared with a 1996 study (73% vs. 71%).2 In our study, patients were hospitalized for longer (due to lower mortality, 9% vs. 46%), and had more drug resistance (median 5 medications, range 2–16 vs. 4, range 2–8), which cost more (median US$24 000, average US$51 000 more per patient). Hospitalization of US MDR-TB patients facilitates the application of injectable medications and frequent treatment monitoring, as well as patient adherence during the initial phase of treatment.
Diagnosis of TB during hospitalization resulted in more rapid initiation on MDR-TB medications. Initial diagnosis of TB while hospitalized was more likely for Blacks, patients with DM, or those who smoked. Blacks utilize hospital emergency rooms disproportionately more than other racial/ethnic populations, which might have increased their likelihood of an in-patient TB diagnosis.15-17 Diabetics and smokers, populations at increased risk of progressing to TB disease once infected or having recurrent TB once treated,18,19 might have been hospitalized for symptoms associated with those conditions and recognized as having TB. Patients with disseminated TB disease were less likely to be diagnosed with TB in the hospital, and also had a significantly longer time to MDR-TB diagnosis. Patients with disseminated TB often present with a variety of symptoms that takes time for providers to assess, and those with extra-pulmonary disease can be difficult to diagnose if TB is not initially suspected.
The cost of in-patient care, largely paid for by the public sector, drives the costs of MDR-TB, and is among the highest for any disease. Although foreign-born MDR-TB patients made up 85% of MDR-TB in-patients, their hospitalizations accounted for 77% of the costs because they were hospitalized for fewer days than US-born MDR-TB patients. The per-patient hospitalization cost for XDR-TB (US$285 000) was 3.5 times that for MDR-TB (US$81 000) in 2010 dollars. The cost per patient was significantly higher for residents of long-term care facilities or those covered by the public sector (approximately three fourths of MDR-TB in-patients). HCUP data corroborate higher hospitalization costs for TB patients hospitalized in government-owned rather than in private non-profit or for-profit-owned hospitals.14
The main hospital for TB patients in Texas had significantly longer hospitalizations than the other study sites, but at a lower average cost per day. Of 14 hospitalized Texas patients, nine were known to have received care at the Texas Center for Infectious Disease (TCID) Hospital, which specializes in treating patients—typically diagnosed elsewhere—who are difficult to manage in an out-patient setting or who have an anticipated long length of stay. TCID costs exclude overhead for diagnostic equipment included by acute general hospitals for diagnostic services and management of complex comorbidities (J Elkins, TCID Hospital Superintendent, personal communication, October 2014). As a publicly funded state hospital, TCID’s per diem rates reflect only its high-volume services and state-determined salary and benefits rates. In contrast, patients in CA and NYC received care at a variety of hospitals.
There appeared to be two MDR-TB care strategies practiced by providers at our study sites: 1) brief and costly initial hospitalization, followed by a long period of out-patient care, or 2) long, publicly funded hospitalization at a specialty facility. While the focus of this paper is on hospitalization, we examined whether the strategies had an impact on total (in-patient and out-patient) MDR-TB direct costs, and found that the cost averages (P = 0.9) and medians (P = 0.8) did not differ significantly among the three study sites. Additional studies would be needed to compare MDR-TB care strategies by type of hospital.
Study limitations included the unavailability of detailed hospitalization data for 17 patients and charges data for 11 hospitalizations. Insurance status was only known for 76 hospitalized patients. Costs for one patient known to be hospitalized could not be estimated because we had neither the hospital length of stay nor the hospital charges. Treatment adherence through to completion was uniformly high for all studied patients; we could not assess whether in-patient care was required to ensure adherence.
CONCLUSIONS
Hospitalization costs for MDR-TB are among the highest for any disease in the United States. Patients with MDR-TB who were older, had AIDS, or had more extensive drug-resistant TB were hospitalized more frequently, for a longer duration, and at a greater cost than other MDR-TB patients. Hospitalization remains a critical care component and facilitates treatment for these complex cases. Prevention of hospitalization for MDR-TB will depend on factors such as the development of new oral medications for treatment, prevention of TB-related AIDS, and primary and secondary prevention of multidrug-resistant TB.
Acknowledgements
The study authors thank the many persons involved with study data collection, data management, and data analysis consultation. The authors would like to specifically acknowledge the contribution of A Vernon to the discussion of care strategies for multidrug-resistant tuberculosis.
Disclaimer: The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the US Centers for Disease Control and Prevention.
Footnotes
Conflicts of interest: none declared.
References
- 1.Brown RE, Miller B, Taylor WR, et al. Healthcare expenditures for tuberculosis in the United States. Arch Intern Med. 1995;155:1595–1600. [PubMed] [Google Scholar]
- 2.Rajbhandary SS, Marks SM, Bock NN. Costs of patients hospitalized for multidrug-resistant tuberculosis. Int J Tuberc Lung Dis. 2004;8:1012–1016. Updated to 2010 dollars. [PMC free article] [PubMed] [Google Scholar]
- 3.Fitzpatrick C, Floyd K. A systematic review of the cost and cost-effectiveness of treatment for MDR-TB. Pharmacoeconomics. 2012;30:63–80. doi: 10.2165/11595340-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 4.Diel R, Rutz S, Castell S, Schaberg T. Tuberculosis: cost of illness in Germany. Eur Respir J. 2012;40:143–151. doi: 10.1183/09031936.00204611. [DOI] [PubMed] [Google Scholar]
- 5.Pooran A, Pieterson E, Davids M, Theron G, Dheda K. What is the cost of diagnosis and management of drug resistant tuberculosis in South Africa? PLOS ONE. 2013;8:e54587. doi: 10.1371/journal.pone.0054587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.World Health Organization . Guidelines for the programmatic management of drug-resistant tuberculosis: 2011 update. WHO; Geneva, Switzerland: [Accessed December 2015]. 2011. WHO/HTM/TB/2011.6. http://whqlibdoc.who.int/publications/2011/9789241501583_eng.pdf. [Google Scholar]
- 7.Burgos M, Gonzalez LC, Paz EA, Gournis E, Kawamura LM, Schecter G. Treatment of multidrug-resistant tuberculosis in San Francisco: an out-patient-based approach. Clin Infect Dis. 2005;40:968–975. doi: 10.1086/428582. [DOI] [PubMed] [Google Scholar]
- 8.Marks SM, Flood J, Seaworth, et al. TB Epidemiologic Studies Consortium Treatment practices, outcomes, and costs of multidrug-resistant and extensively drug-resistant tuberculosis, United States, 2005–2007. Emerg Infect Dis. 2014;20:812–820. doi: 10.3201/eid2005.131037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Centers for Medicare and Medicaid Services . 2005 operating cost to charge ratios (OPCCR). FY2005 impact file (in-patient prospective payment system) Centers for Medicare and Medicaid Services; Washington DC, USA: 2005. https/www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/index.htm?redirect=/acuteinpatientpps/ [Google Scholar]
- 10.Bureau of Labor Statistics . Consumer price index: all urban consumers, medical care. BLS; Washington DC, USA: [Accessed December 2015]. Series ID CUUR0000SAM. (Check–no date of publication) http://data.bls.gov/cgi-bin/surveymost. [Google Scholar]
- 11.Centers for Medicare and Medicaid Services . 2005 Medicare geographic adjustment factors. Centers for Medicare and Medicaid Services; 2005. [Google Scholar]
- 12.Mag Mutual Healthcare Solutions . 2009 Physicians’ Fee & Coding Guide. Mag Mutual; Duluth, GA, USA: 2008. [Google Scholar]
- 13.The DRG handbook: comparative clinical and financial standards. Solucient; 1998. p. 21. [Google Scholar]
- 14.Agency for Healthcare Research and Quality . Healthcare cost and utilization project national in-patient sample. US Department of Health & Human Services; Rockville, MD, USA: [Accessed December 2015]. 2015. http://hcupnet.ahrq.gov. [Google Scholar]
- 15.Roby DH, Nicholson GL, Kominski GF. African Americans in commercial HMOs more likely to delay prescription drugs and use the emergency room. University of California; LosAngeles, CA, USA: 2009. University of California Los Angeles Center for Health Policy Research. Health Policy Research Brief. [PubMed] [Google Scholar]
- 16.Frank JW, Andrews CM, Green TC, Samuels AM, Trinh TT, Friedmann PD. Emergency Department utilization among recently released prisoners: a retrospective cohort study. BMC Emerg Med. 2013;13:16. doi: 10.1186/1471-227X-13-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cox S, Dean T, Posner SF, et al. Disparities in reproductive health-related visits to the Emergency Department in Maryland by age and race, 1999–2005. J Women’s Health. 2011;20:1833–1838. doi: 10.1089/jwh.2010.2554. [DOI] [PubMed] [Google Scholar]
- 18.Harries AD, Satyanarayana S, Kumar AMV, et al. Epidemiology and interaction of diabetes mellitus and tuberculosis and challenges for care: a review. Public Health Action. 2013;3(Suppl 1):S3–S9. doi: 10.5588/pha.13.0024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yen Y-F, Yen M-Y, Lin Y-S, et al. Smoking increases risk of recurrence after successful anti-tuberculosis treatment: a population-based study. Int J Tuberc Lung Dis. 2014;18:492–498. doi: 10.5588/ijtld.13.0694. [DOI] [PubMed] [Google Scholar]