Abstract
There are few reports on the primary percutaneous treatment of Lutembacher's syndrome for which surgery has been the traditionally accepted modality of treatment. Concerns for percutaneous treatment in this entity are: (1) it is technically demanding and the dual lesion renders negotiation of catheters and balloons difficult; (2) redo valvulotomy in the presence of an atrial septal device would be difficult; (3) it may not be suitable for all patients with the condition. We describe percutaneous treatment by a hitherto undescribed technique of separate low septal puncture and review the existing literature.
Keywords: Congenital Heart Disease
Introduction
Lutembacher's syndrome, a concomitant congenital atrial septal defect (ASD) and rheumatic mitral stenosis (MS), was first described by Lutembacher in 1916.1 Although traditionally treated by open heart surgery,2 it is amenable to percutaneous treatment. However, the reports of definitive percutaneous treatment are still anecdotal.3–11 Mitral valve (MV) interventions performed surgically have comparable rates of restenosis to percutaneous valvulotomy. Apart from the cosmetic reasons, redo surgery poses a higher risk to the patient while primary percutaneous treatment leaves an option for first surgery at a lower risk or the use of other techniques such as retrograde percutaneous valvulotomy. Here we present a case of Lutembacher's syndrome treated percutaneously by a technique of separate low atrial septal puncture and review the cases described in the literature.
Case report
A young patient diagnosed with ostium secundum ASD (22 mm) and rheumatic MS (0.9 cm2) was taken for definitive percutaneous treatment. The patient was planned to undergo percutaneous valvulotomy followed by device closure of the ASD.
The MV was pliable and suitable for percutaneous valvulotomy. The ASD was 22 mm in diameter with adequate margins. The patient was given standard premedication. The transmitral gradient was not recorded because of the presence of the large ASD. It was decided to make a low septal puncture (figure 1) (separate from the ASD) which would provide support to the shaft and necessary curve to orientate the balloon towards the MV. Entry into the left ventricle (LV) was expected to be difficult so it was decided to use an over-the-wire technique using an 0.032 inch exchange length J-tip guidewire. (figure 2) The coil wire was exchanged for a J-tip guidewire and the MV was negotiated through to enter the LV. An Accura balloon (23–26 mm) was tracked over and MV dilation was successfully achieved. The MV area increased to 1.8 cm2 with no mitral regurgitation. In the second sitting the ostium secundum ASD was successfully closed with a 26 mm device (Lifetech delivery system 12 F Sesrcare; figure 3). The procedure was uneventful, as was the patient's subsequent hospital stay.
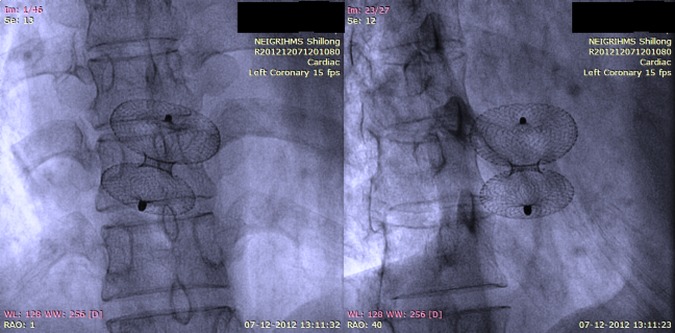
Figure 1.
Low trans-septal puncture performed separately from the atrial defect to provide the stability and necessary orientation for crossing the mitral valve.
Figure 2.
J-tip guidewire being used to track the balloon into the left ventricle and subsequent inflation.
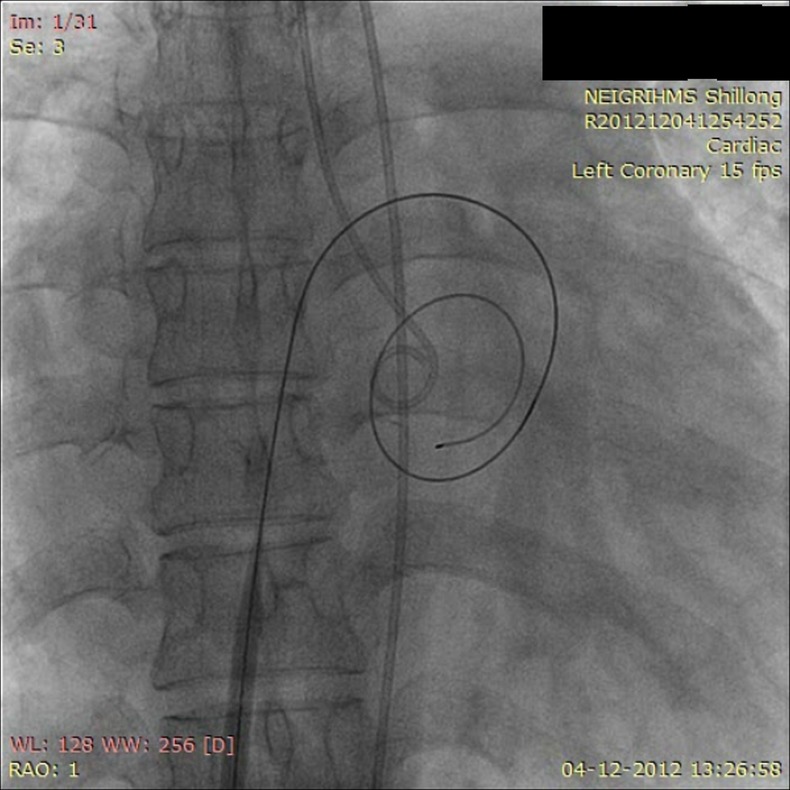
Figure 3.
Device closure of the atrial septal defect. Note the orientation of the device in relation to the septum.
Discussion
Multiple structural heart diseases in one patient influence the natural history and the procedural success of catheter-based treatment unfavourably. The percutaneous treatment of Lutembacher's syndrome was first described by Ruiz and colleagues in 1992 as a palliative rescue procedure.12 In case studies to date, the success rate of combined percutaneous treatment is very high with no short-term or long-term complications (table 1). It is also reported to reduce the mortality and morbidity associated with cardiac surgery, physiological trauma and length of hospital stay. However, the percutaneous approach of treatment in Lutembacher's syndrome has many technical difficulties, such as pushing the Inoue balloon across the stenosed MV necessitating the use of alternative and innovative methods. Some of the described methods (although not specifically in relation to Lutembacher's syndrome) include the use of flotation balloon catheters, the reverse loop method, catheter sliding method, over-the-wire method, modified over-the-wire technique and reshaping the stylet. Another important consideration is the size of the septal defect as the defects can be large and the margins can be thin. The preferred techniques are an optimum transoesophageal echocardiographic image or measuring the stretched balloon diameter. In patients with Lutembacher's syndrome in whom definitive percutaneous repair is contemplated, a separate low septal puncture can be a useful strategy to provide the balloon shaft with the desired stability for easy manipulation and necessary curve so that entry to the LV is facilitated. LV entry is facilitated by use of a J-tip exchange length guidewire which can be used to enter the LV and subsequently track the balloon over it as negotiation of the coil wire into the LV can be difficult. Apart from cosmetic reasons and avoiding the complications of surgery, primary percutaneous treatment keeps open the option of surgery in cases of restenosis. In contrast, surgery offered as the primary treatment in Lutembacher's syndrome leaves patients with a comparable risk of restenosis to balloon mitral valvulotomy and, in addition, the possibility of high-risk redo surgery. On the other hand, balloon mitral valvulotomy will be difficult in the presence of a patch in the septum.
Table 1.
Percutaneous repair of Lutembacher's syndrome
| Year | Authors | Number of cases | Hardwire used | Special challenge/technique |
|---|---|---|---|---|
| 1999 | Joseph et al3 | 1 | The mitral valve was dilated using a 25 mm diameter cylindrical single balloon (Joseph mitral balloon catheter, Numed, Ontario, Canada). The ASD was closed using a 16 mm Amplatzer septal occluder (AGA Medical, Golden Valley, Minnesota, USA) | Modified over the wire technique, atrial septal aneurysm |
| 2000 | Chau et al4 | 1 | The mitral valve was crossed and dilated twice with an Inoue balloon catheter set at 25 mm and 26 mm, respectively; 20 mm Amplatzer atrial septal defect occluder (AGA Medical) | Nil |
| 2003 | Ahmed et al5 | 1 | Size 28 Inoue balloon catheter (Toray, Houston, Texas, USA), Amplatzer septal occluder (AGA Medical) | Nil |
| 2005 | Xiang-qian et al6 | 1 | 26 mm diameter cylindrical single balloon (Jin Chang Medical), 24 mm ASD occluder (Lifetech Scientific) |
Balloon flotation catheter used to cross the mitral valve |
| 2007 | Ho et al7 | 1 | Inoue balloon (Toray), 19 mm Amplatzer septal occlude | JR 6 F used for LV entry |
| 2010 | Özdemir et al8 | 1 | Inoue balloon catheter set (Toray),16 mm Amplatzer septal occluder device (AGA Medical) | Nil |
| 2011 | Behjatiardakani et al9 | 2 | Inoue balloon, 32 mm Amplatzer septal occlude | Nil |
| 2012 | Sena et al10 | 1 | Inoue balloon catheter 26 mm | Palliative BMV as a bridge to surgery |
ASD, atrial septal defect; BMV, balloon mitral valvulotomy; LV, left ventricle.
Conclusion
Percutaneous interventional treatment of Lutembacher's syndrome is feasible in suitable patients but can be complex, requiring alternative or modified methods for crossing the MV and accurate sizing of the septal defect. In most cases the procedure can be safely and effectively carried out with presently available techniques and should be considered as an alternative to surgical therapy. A pre-planned strategy with prior anticipation of difficulties in catheter manipulation will improve the chances of success.
Footnotes
Contributors: All the authors were actively involved in the care and management of the patient and in the drafting, revision and final approval of the manuscript.
Competing interests: None.
Ethics approval: Obtained from the institute ethical committee.
Provenance and peer review: Not commissioned; internally peer reviewed.
References
- 1.Perloff JK. Atrial septal defect in: the clinical recognition of congenital heart disease. 4th edn Philadelphia: WB Saunders, 1994:233–99. [Google Scholar]
- 2.MuIIer WH, Jr, LittIefieId JB, Beckwith JR. SurgicaI treatment of Lutembacher 's syndrome. J Thorac Cardiovasc Surg 1966;51:66–70. [PubMed] [Google Scholar]
- 3.Joseph G, et al. Definitive percutaneous treatment of Lutembacher's syndrome. Catheter Cardiovasc Interv 1999;48:199–204. [DOI] [PubMed] [Google Scholar]
- 4.Chau EMC, Lee C-H, Chow WH, et al. Transcatheter treatment of a case of Lutembacher syndrome. Catheter Cardiovasc Interv 2000;50:68–70. [DOI] [PubMed] [Google Scholar]
- 5.Ahmed WA, Al-Shaibi KF, Chamsi-Pasha H, et al. Non-surgical correction of Lutembacher syndrome. Saudi Med J 2003;3:307–8. [PubMed] [Google Scholar]
- 6.Xiang-qian S, Sheng-hua Z, Tao Z, et al. Trascatheter treatment of Lutembacher syndrome. Chin Med J 2005;118:1843–5. [PubMed] [Google Scholar]
- 7.Ho C-L, Liang K-W, Fu Y-C, et al. Transcatheter therapy of Lutembacher syndrome. J Chin Med Assoc 2007;70:253–6. [DOI] [PubMed] [Google Scholar]
- 8.Özdemir AO, Kumbasar D, Dinçer I, et al. [Percutaneous treatment of Lutembacher syndrome: a case report.] Türk Kardiyol Dern Arş (Arch Turk Soc Cardiol) 2010;38:47–9. [PubMed] [Google Scholar]
- 9.Behjatiardakanil M, Rafiei M, Nough H, et al. Trans-catheter therapy of Lutembacher syndrome: a case report. Acta Medica Iranica 2011;49: 327–30. [PubMed] [Google Scholar]
- 10.Sena JP, Martinelli G, Ramos D, et al. Percutaneous mitral valvotomy in a patient with Lutembacher syndrome as a bridge to definitive surgical intervention. Rev Bras Cardiol Invasive 2012;20:1. [Google Scholar]
- 11.Cheng TO. Coexistent atrial septal defect and mitral stenosis (Lutembacher syndrome): an ideal combination for percutaneous treatment. Catheter Cardiovasc Interv 1999;48:205–6. [DOI] [PubMed] [Google Scholar]
- 12.Ruiz CE, Gamra H, Mahrer P, et al. Percutaneous closure of a secundum atrial septal defect and double balloon valvulotomy of a severe mitral and aortic valve stenosis in a patient with Lutembacher's syndrome and severe pulmonary hypertension. Cathet Cardiovas Diagn 1992;25:309–12. [DOI] [PubMed] [Google Scholar]