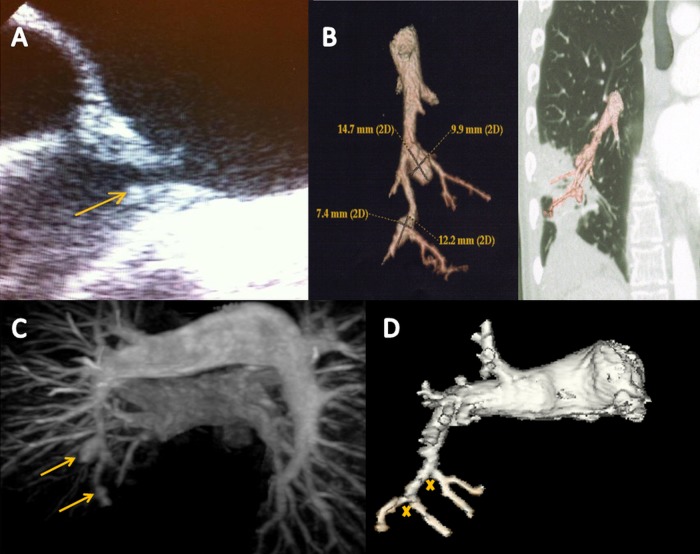
A patient was admitted for dyspnoea and recurrent fever (39°C) since 3 months. He had a previous history of pulmonary stenosis treated by open-heart commissurotomy in childhood and by pulmonary valve replacement with homograft 12 years ago. Clinical examination found a systolic murmur in the left parasternal area and crepitations at the right base of the lung. Chest X-ray found right lower lobe pneumonia. Transoesophageal echocardiography showed a moderate pulmonary insufficiency and large vegetation (10 mm) located on the anterior valve of pulmonary homograft (figure 1A). All blood cultures were positive for Aggregatibacter actinomycetemcomitans (HACEK group). Then, the diagnosis of pulmonary homograft endocarditis was done and an intravenous antibiotic treatment (ciprofloxacin and rifampicin) was begun. No portal of entry was detected. Blood culture became rapidly sterile but fever persisted. Fifteen days later, the patient presented a recurrence of acute dyspnoea. Chest CT and MRI detected new parenchymal condensations in the left lung and the development of a right lower lobe abscess associated with two mycotic pulmonary artery aneurysms (figure 1B,C). Antibiotic treatment was then optimised (the addition of metronidazole) and prolonged to 10 weeks. Fever disappeared 3 weeks after antibiotic treatment adjustment; MRI angiography performed 3 months later revealed the disappearance of parenchymal condensations and aneurysms (crosses mark ex-location on figure 1D).
Figure 1.
(A) Transoesophageal echocardiography showing pulmonary homograft endocarditis. (B) Chest CT revealed the development of a right lower lobe abscess associated with two mycotic pulmonary artery aneurysms. (C) MRI angiography detected two mycotic pulmonary artery aneurysms. (D) Three months later, MRI revealed the disappearance of aneurysms (crosses mark ex-location).
In conclusion, mycotic aneurysms are a cause of persistent fever in patients with infective endocarditis. Their occurrence in pulmonary homograft infective endocarditis is very rare and has to be known to order prompt management.
Footnotes
Contributors: All authors have contributed significantly to the submitted work. All authors have read and approved the submission of the manuscript.
Competing interests: None.
Provenance and peer review: Not commissioned; internally peer reviewed.