Abstract
Purpose:
To evaluate the shade reproduction of a pressable all-ceramic system placed on unstained and stained extracted maxillary central incisor using a color measurement spectrophotometer. In addition, to compare shade reproduction of this material with low translucency and medium opacity on unstained tooth and medium and high opacity on stained tooth.
Materials and Methods:
Total 45 discs, with difference in the opacity of core, were used. After spectrophotometric evaluation, shade reproduction of the discs was compared and calculated by formula: Δ E* = ([Δ L*]2+ [Δ a*]2+ [Δ b*]2)1/2.
Results:
Student's t-test showed that in a sample of 15, the values of Δ E* for Group I - LT (Us.T.) lie between 0 and l, for Group II - MO (for Us. as well as S.T.) between l and 2, for Group III - HO (S.T.) are all above 5. Comparison among groups after t-test showed that mean Δ E* values of Group I - LT is less than Group II - MO for the unstained tooth, Δ E* for Group II - MO is less than average Δ E* value of Group III - HO for stained tooth.
Conclusion:
All-ceramic with low translucency can be used for the fabrication of restoration on the unstained tooth as it gives the best shade reproduction. The medium opacity material may be used on the unstained as well as on stained tooth. However, the clinical implication of high opacity is limited when applied over the stained tooth as it is giving a shade reproduction, which is not within acceptable limits.
Keywords: Maxillary central incisor, pressable all-ceramics, shade reproduction, spectrophotometer
INTRODUCTION
Esthetics is a primary consideration for patients seeking prosthodontic treatment. The appearance of the maxillary anterior teeth is important not only to dental esthetics, but also to facial esthetics, as this tooth restore the natural color, translucency, and optimal dentolabial relations in harmony with the overall facial appearance.[1,2] Shade reproduction is one of the crucial determinants for the success of a restoration. In clinical practice, for heavily discolored teeth, keeping esthetics, durability, function, and longevity in consideration, ceramic crowns offer the best answer as compared to the other materials available.[3]
Patient's satisfaction for an esthetic restoration is primarily associated with surface, outline form, translucency, and color. Porcelain fused to metal restorations have certain disadvantages such as chipping of veneering ceramic, exposure of metal, and lack of translucency, the metals used in these restorations have the potential to cause allergic or toxic reactions within the soft or hard tissues.[4] Moreover, they have been known to cause “graying” of the gingival margin because of metal show through. Hence, their usage is declining.[5]
Recently, high-quality cosmetic dentistry has resulted in the development of all-ceramic materials.[6,7] Heat-pressed ceramic restorations have the potential to create excellent esthetic results in various situations for the fabrication of frameworks on vital and severely discolored preparations or titanium abutments as well. They possess color-rendering properties and optical properties that simulate natural teeth and have excellent biocompatibility, strength, and surface texture. The translucency provided by the restoration allows light transmission through to the underlying tooth, which minimizes gingival shadowing and yields an appearance of vitality.[8,9,10]
Core translucency and opacity has been identified as one of the primary factors controlling esthetics and a critical consideration in the selection of the materials. IPS e-max® is a lithium disilicate glass ceramic ingot with high translucency, low translucency, medium opacity, and high opacity. The available data on the translucency of shaded zirconia cores are limited. Barao, Adelino Ricardo et al. stated that color scale, light source during color evaluation, characteristic of core material, color of supporting tooth, presence of root post, and type of luting cement are clinical factors that may influence the esthetics of all-ceramic restorations. Laboratory factors such as technique for ceramic condensation, thickness, temperature, and number of firing cycles and integration with surrounding periodontal tissue also influence the esthetic result of these crowns.[11,12]
However, predominantly it is the core material that contributes to the color of an all-ceramic restoration. The opaque cores adequately mask the substructure and enable the fabrication of lifelike restorations.[13,14] Therefore, it could be hypothesized that different opacities of the core of pressable all-ceramic system mask the color of stained tooth. This study was aimed to evaluate the shade reproduction by the pressable all-ceramic system on unstained and stained tooth using different opacity ingots used for core build-up.
MATERIALS AND METHODS
Fabrication of all-ceramic cores [Figures 1 and 2]
Figure 1.

Materials used for the fabrication of all-ceramic cores
Figure 2.

Materials used for veneering and glazing the cores
The pressable all-ceramic system (IPS e-max® Press, Ivoclar Vivadent) with the difference in the opacity of core, lithium disilicate - reinforced ceramic: Low translucency, medium, and high opacity were used.
Equipments used in the study were EP 600 Combi furnace, Programmat P300 Furnace (for veneering dentin, enamel and glazing) (Manufacturer: Ivoclar Vivadent AG Bendererstrasse 2, 9494 Schaan Liechtenstein. Ivoclar Vivadent Marketing India Pvt. Ltd.) Colour measurement Spectrophotometer (Model CM-3600, Konica Minolta Sensing Singapore Pvt. Ltd.) [Figure 3a–c].
Figure 3.
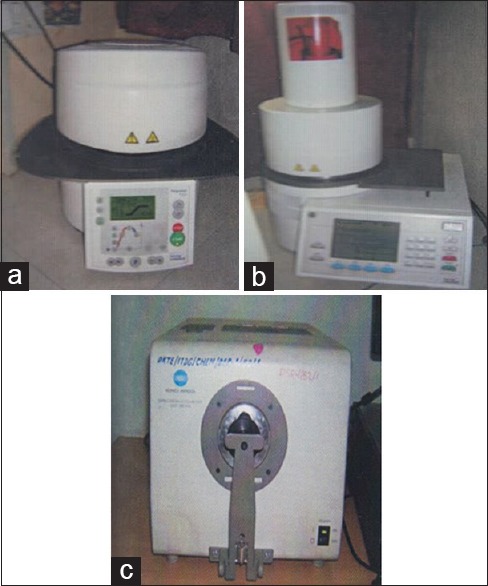
Equipment used in the study. (a) Combi furnace, (b) Programmate, (c) spectrophotometer
Sample collection for evaluation of ceramic discs on unstained and stained tooth
For the evaluation of ceramic discs on the stained tooth, natural, intrinsically stained, extracted maxillary central incisor was selected. Similarly, for the unstained tooth, the extracted caries-free, “A2” shade maxillary central incisor, with all intact surfaces was selected. These teeth were preserved in 5% normal saline solution at room temperature.
Mounting the unstained and stained tooth [Figure 4]
Figure 4.

Unstained and stained tooth mounted on acrylic block
For preparation of the labial surface of both unstained and stained tooth properly, the long axis of the tooth was kept perpendicular to the horizontal plane. It was mounted on the acrylic block, in such a way that the portion of the tooth above cementoenamel junction was exposed.
Preparation of unstained and stained tooth for receiving all-ceramic pressable lithium disilicate discs
While analyzing on the spectrophotometer with a small aperture, both for illumination and collection of light, the amount of reflected light is reduced, causing an inadequate reading of lightness. The curved surface of a tooth may have a negative impact on the uniform reflectance of light to the spectrophotometer. To minimize such inaccuracies, flat ceramic discs were used. The labial surface of both unstained and the stained tooth was prepared up to 1.5 mm for placing the discs.[15,16]
Preparation of the mold for standardization of the all-ceramic discs [Figures 5a–c and 6a–c]
Figure 5.
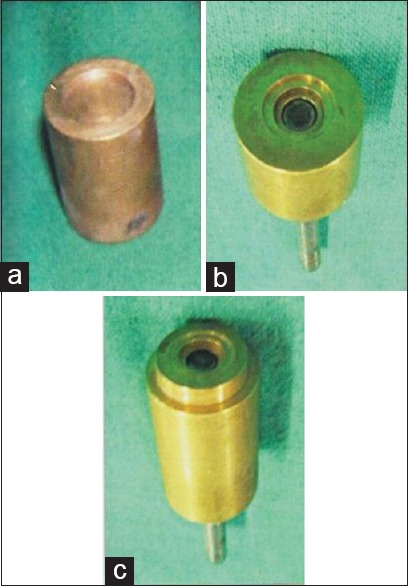
(a-c) Preparation of the mold for standardization of the all-ceramic discs
Figure 6.
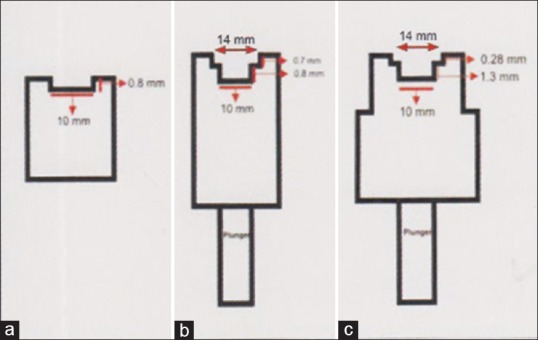
(a-c) Linear diagram of the mold
Three cylindrical brass molds, machined in three different cylindrical brass blocks, were prepared. For core: A circular depth of 0.8 mm and 10 mm internal diameter was made in the mold. Wax patterns of the cores were prepared in this mold. The ceramic ingots of “A” two veneering material were used for the fabrication of cores as per manufacturer's instructions. For dentin build-up: A circular depth of 0.8 mm and 10 mm internal diameter was made in another mold for receiving the finished core. Above this, another circular depth of 0.75 mm and l4 mm internal diameter was made for dentin build-up. Dentin veneering material IPS e-max® Ceram corresponding to “A2” shade was used. The dentin build-up was followed by enamel build-up. For enamel build-up: A circular depth of 1.3 mm and 10 mm internal diameter was made in the third mold for receiving the finished core-dentin complex. Above this, another circular depth of 0.3 mm and l4 mm internal diameter was made for receiving the enamel build-up. The core-dentin complex was kept in this mold for enamel build-up using IPS e-max® Ceram Transpa Incisal corresponding to “A2” shade.
Two different cylindrical metal plungers were fabricated for raising the core-veneer complex from the brass molds. Dentin and enamel veneering ceramics undergo volumetric firing shrinkage which is 30–38%. Hence, the internal diameters of the molds for dentin and enamel build-up were wider than the diameter of the specimen by 40%. In addition, the build-up was done 30–40% more than the required veneer thickness to compensate for the firing shrinkage.
Fabrication of the discs
The only difference was the use of different types of ceramic ingots for the fabrication of core: Low translucency, medium opacity, and high opacity. Final thickness of 1.5 mm of all discs was confirmed. In this way, total 45 discs, 15 each group were fabricated [Figure 7].
Figure 7.
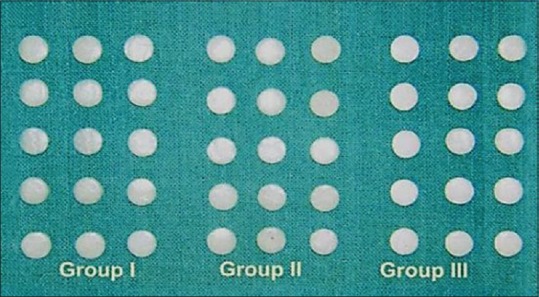
Total 45 samples of Group I - LT, Group II – MO, and Group III - HO
Spectrophotometric evaluation
Color measurement time was approximately l. 5 s (unit data output). Minimum interval between measurements was approximately 4 s, during day time. The aperture size of the spectrophotometer used was 8 mm in diameter.
Measurement data were automatically stored at the time of exposure. The instrument was attached to a computer which forms the interface among the spectrophotometer, user, and the printer [Figure 8]. Color difference from a target color can be measured and instantly displayed in a numerical form or on a spectral reflectance graph. Before the evaluation session, the spectrophotometer was calibrated against white and black working standard and then served as the standard backgrounds for the different samples discs. Each disc was placed on the prepared labial surface of the respective stained/unstained tooth in front of the aperture, perpendicular to the beam of the spectrophotometer. The readings of the disc were recorded in CIELAB system in the form of L* a* b* values. A total of three readings were taken and a mean value was obtained for each ceramic disc. Shade reproduction of the specimen was evaluated by change in color between the control and the specimens. Change in color was obtained by calculating Δ E by the formula: Δ E* = ([Δ L*]2+ [Δ a*]2+ [Δ b*]2)1/2 where Δ E* is the change in color and Δ L*, Δ a*, Δ b* represent the difference in L*, a*, b* values of the control and the ceramic discs. Based on, whether the spectrophotometric evaluation of the discs was performed on stained tooth or unstained tooth, the groups were named as: Group I - LT (Us.T.) control group: Discs with low translucency on unstained tooth. Experimental groups: Group II - MO (Us.T.), Group II - MO (S.T.): Discs with medium opacity on unstained and stained tooth, respectively, and Group III - HO (S.T.): Discs with high opacity on stained tooth.
Figure 8.
Spectrophotometric evaluation
RESULTS
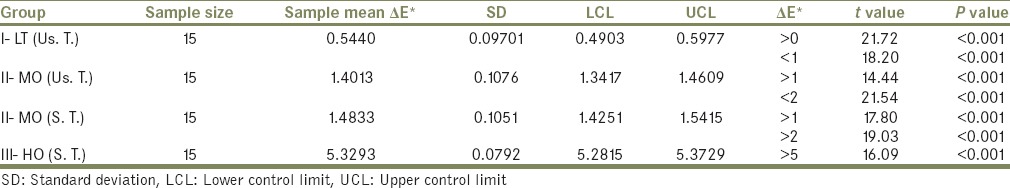
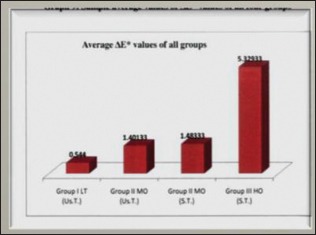
Student's t-test was applied for individual groups. The data are summarized in Table 1 and Graph 1 giving mean and standard deviation of Δ E* values for all the four groups. The sample values on Δ E* for all the four groups are graphically represented in Graphs 1 and 2. Δ E* for Group I - LT (Us.T) <0, for Group II - MO (for Us. as well as S.T.) between l and 2, for Group III - HO (S.T.) are all above 5. Comparison among groups after t-test showed mean Δ E* values of Group I - LT is less than Δ E* value of Group II - MO for unstained tooth, Δ E* for Group II - MO is less than Δ E* value of Group III - HO for stained tooth. Therefore, shade reproduction of Group I is better than Group II when tested on unstained tooth and Group II is better than Group III when tested on the stained tooth.
Table 1.
Summary and significance of the data
Graph 1.

Comparison of ΔE* values of all four groups
Graph 2.
Average ΔE* values of all four groups
T-test was applied for the comparison of mean Δ E* values of two groups on unstained tooth: From Table 2 and Graph 2, it was observed that mean Δ E* for Group I - LT (Us.T.) =0.544 and mean Δ E* for Group II - M.O. (Us.T.) =1.4013. It was concluded that average value of Δ E* for Group I - LT (Us.T.) was less than those obtained from Group II - MO (Us.T.). Therefore, shade reproduction by Group I - LT (Us.T.) was better than that of Group II - MO (Us.T.)
Table 2.
Test for comparison of ΔE* values of Group I- L. T. (Us. T.) and Group II-MO (Us. T.) and Group II- MO (S. T.) and Group III-Ho (S. T.)
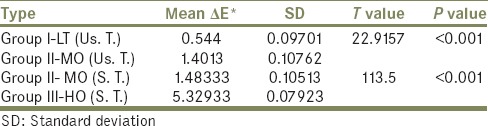
Again after the comparison of mean Δ E* values of two groups on stained tooth
It was observed that mean Δ E* for Group II - MO (S.T.) = l. 48333 and for Group III - H.O. (S.T.) =5.32933. It was concluded that average value of Δ E* for Group II -MO (S.T.) was less than those obtained from Group III - HO (S.T.). Therefore, shade reproduction by Group II - MO (S.T.) was far better than that for Group III - HO (S.T.).
DISCUSSION
The face is the man's most individual characteristic, and the teeth comprise two-thirds of its structures. The dentist's responsibility to preserve, create, or enhance smile without impairing function is the foremost. Kelly et al. identified core translucency as one of the primary factors in controlling esthetics and a critical consideration in the selection of materials.[17,18]
In addition to the translucency, opacity and shade of the porcelain, the thickness and the combination of ceramic layers determine the final shade of an esthetic restoration. Other factors, including porcelain brand, batches, the number of porcelain firings, and condensation technique can also affect the final shade of porcelain.
Veneering of Pressable all-ceramic is favored for greater esthetics. Furthermore, the opacity of all core specimens increases after veneering because of the structure of the veneering porcelain, increased specimen thickness, reflectance at the interface between core and veneering porcelain, porosity between the layers, and any changes in the constituent core material with additional firing cycles. The ultimate translucency of the core and veneer system is important for optimal esthetics. Ceramic translucency can be affected by thickness, crystalline structure, and number of firings. Reduced crystalline content and a crystal refractive index close to that of the matrix cause less scattering of light. Lucite and lithium disilicate have refractive indices close to that of the porcelain matrix.[19]
In clinical practice, the color replication process for dental porcelain comprises a shade-selection phase followed by shade duplication. To evaluate color difference, there are two methods: The perceptional method and the instrumental measuring method. The most frequently applied method in clinical dentistry for color communication during the fabrication of indirect restorations is perceptional method. It relies on color perception by human eyes, which varies by person and is affected by many factors: Surrounding light condition, size of objects, background, and eye fatigue. In addition, the use of shade guide is highly subjective. It depends on the clinician's color perception, ambient light conditions, and the background against which the tooth is compared, all of which are subject to variance. With respect to human observation, color determination is dependent on previous eye exposure, object and illuminant position relative to the observer, and to each other and to color characteristics of the illuminant. The color perception of any individual may not be consistent from time to time. Any human color evaluation method is, therefore, susceptible to errors resulting from perceptual inconsistencies.[20] A means to improve assessment of tooth color is using spectrophotometer or colorimeters.
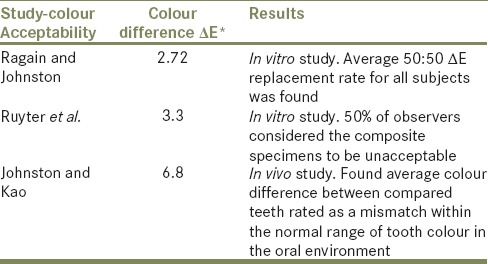
Wee et al.[21] summarized the studies [Tables 3 and 4] relevant to dental color-matching tolerance. Tables 1 and 2 showed that Group I – LT (Us.T.) had least color difference; therefore, the best shade reproduction among all the groups was tested. Group II - MO (Us.T.) and Group II - MO (S.T.) also showed less color difference, so there was a good shade reproduction. Whereas Group III - HO (S.T.) showed the highest color difference; therefore, shade reproduction was not rated as a match in the oral environment. After comparison, the shade reproduction by Group I - LT (Us.T.) was better than that of Group II - MO (Us.T.). The shade reproduction by Group II - MO (S.T.) was far better than that for Group III - HO (S.T.). Therefore, the study confirms the hypothesis.
Table 3.
Alvin G. Wee et al.[25] summary of studies relevant to dental colour-matching tolerance
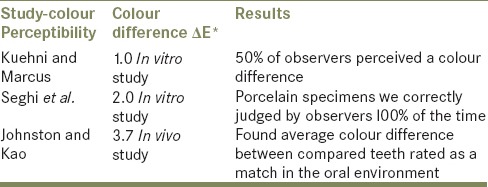
Table 4.
Alvin G. Wee et al.[25] summary of studies relevant to dental colour-matching tolerance
Core thickness required for this lithium disilicate - reinforced ceramic (IPS e-max® Press, Ivoclar Vivadent) is 0.8 mm and the veneering material is thinner, i.e. 0.7 mm. IPS e-max® ceramic veneering material has nano-fluorapatite and micro-fluorapatite crystals. They cause light scattering in a way that resembles the scattering by structure and components of tooth enamel. The variation in translucency and opacity of the core was the cause for the variation in Δ E* and the varying shade reproduction between the groups. It may be attributed to the differences in crystal volume and the refractive index.[22]
IPS e-max® Press, Ivoclar Vivadent has an unusual microstructure. Lithium disilicate (Li2Si2O5) consists of many small interlocking plate-like crystals that are randomly oriented. This ceramic is highly translucent due to optical compatibility between the glassy matrix and the crystalline phase, which minimizes internal scattering of light as it passes through it. Zirconium oxide and other oxides are added as opacifiers. A varying percentage of these opacifiers in the ingots could be the reason for varying color differences between the groups and so varying shade reproduction.[23,24]
Further “in-vivo” studies should be carried out to verify these results and to know their clinical significance. This is required as the oral cavity, i.e. oral fluids and soft tissues cannot be duplicated in vitro. This prevents direct application of these results obtained when applied in patient's mouth. Conditions not considered in this study include the color of underlying luting agent used for the restoration. This is because the shade of all-ceramic restorations is determined not only by the ceramic and the color of the underlying tooth structure, but also by the thickness and color of the luting agent specially in those all-ceramic restorations fabricated using a translucent core. Therefore, further studies on the interaction of the ceramic materials with luting agents and other substrate background are needed.
CONCLUSION
Within the limitations of this in vitro study, following conclusions were drawn:
The shade reproduction of Group I - LT (Us.T.) was the best among all the groups, so can be used for restorations on unstained tooth
The shade reproduction of Group II - MO (Us.T.) and Group II - MO (S.T.) was good, so may be used on unstained as well as on stained tooth
The shade reproduction of Group III - HO (S.T.) was not within acceptable range, so the clinical implication of Group III - HO may be limited when applied over intensely stained tooth.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Wee AG, Lindsey DT, Shroyer KM, Johnston WM. Use of a porcelain color discrimination test to evaluate color difference formulas. J Prosthet Dent. 2007;98:101–9. doi: 10.1016/S0022-3913(07)60043-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jorgenson MW, Goodkind RJ. Spectrophotometric study of five porcelain shades relative to the dimensions of color, porcelain thickness, and repeated firings. J Prosthet Dent. 1979;42:96–105. doi: 10.1016/0022-3913(79)90335-4. [DOI] [PubMed] [Google Scholar]
- 3.Li Q, Wang YN. Comparison of shade matching by visual observation and an intraoral dental colorimeter. J Oral Rehabil. 2007;34:848–54. doi: 10.1111/j.1365-2842.2006.01678.x. [DOI] [PubMed] [Google Scholar]
- 4.Christensen GJ. The confusing array of tooth-colored crowns. J Am Dent Assoc. 2003;134:1253–5. doi: 10.14219/jada.archive.2003.0361. [DOI] [PubMed] [Google Scholar]
- 5.Walton TR. A 10-year longitudinal study of fixed prosthodontics: Clinical characteristics and outcome of single-unit metal-ceramic crowns. Int J Prosthodont. 1999;12:519–26. [PubMed] [Google Scholar]
- 6.Shokry TE, Shen C, Elhosary MM, Elkhodary AM. Effect of core and veneer thicknesses on the color parameters of two all-ceramic systems. J Prosthet Dent. 2006;95:124–9. doi: 10.1016/j.prosdent.2005.12.001. [DOI] [PubMed] [Google Scholar]
- 7.Hedge C, Nitin A, Vijia S, Anil SR, Ramya D. Metal free restorations. J Interdiscip Dent. 2011;1:10–3. [Google Scholar]
- 8.Cao J, He HM, Wang ZY. Colour stability against accelerated aging of alumina- and leucite-based ceramics materials. Int Chin J Dent. 2007;7:41–52. [Google Scholar]
- 9.Tan PL, Dunne JT., Jr An esthetic comparison of a metal ceramic crown and cast metal abutment with an all-ceramic crown and zirconia abutment: A clinical report. J Prosthet Dent. 2004;91:215–8. doi: 10.1016/j.prosdent.2003.12.024. [DOI] [PubMed] [Google Scholar]
- 10.Okubo SR, Kanawati A, Richards MW, Childress S. Evaluation of visual and instrument shade matching. J Prosthet Dent. 1998;80:642–8. doi: 10.1016/s0022-3913(98)70049-6. [DOI] [PubMed] [Google Scholar]
- 11.Seghi RR, Hewlett ER, Kim J. Visual and instrumental colorimetric assessments of small color differences on translucent dental porcelain. J Dent Res. 1989;68:1760–4. doi: 10.1177/00220345890680120801. [DOI] [PubMed] [Google Scholar]
- 12.Ishikawa-Nagai S, Sawafuji F, Tsuchitoi H, Sato RR, Ishibashi K. Using a computer color-matching system in color reproduction of porcelain restorations. Part 2: Color reproduction of stratiform-layered porcelain samples. Int J Prosthodont. 1993;6:522–7. [PubMed] [Google Scholar]
- 13.Holloway JA, Miller RB. The effect of core translucency on the aesthetics of all-ceramic restorations. Pract Periodontics Aesthet Dent. 1997;9:567–74. [PubMed] [Google Scholar]
- 14.Douglas RD, Przybylska M. Predicting porcelain thickness required for dental shade matches. J Prosthet Dent. 1999;82:143–9. doi: 10.1016/s0022-3913(99)70147-2. [DOI] [PubMed] [Google Scholar]
- 15.Dancy WM, Yaman P, Dennison JB, O’Brien WJ, Razzoog ME. Colour measurement as quality criteria for clinical shade matching of porcelain crowns. J Esthet Dent. 2003;15:114–22. doi: 10.1111/j.1708-8240.2003.tb00327.x. [DOI] [PubMed] [Google Scholar]
- 16.Okamura M, Chen KK, Kakigawa H, Kozono Y. Application of alumina coping to porcelain laminate veneered crown: Part 1 masking ability for discolored teeth. Dent Mater J. 2004;23:180–3. doi: 10.4012/dmj.23.180. [DOI] [PubMed] [Google Scholar]
- 17.Antonson SA, Anusavice KJ. Contrast ratio of veneering and core ceramics as a function of thickness. Int J Prosthodont. 2001;14:316–20. [PubMed] [Google Scholar]
- 18.Heffernan MJ, Aquilino SA, Diaz-Arnold AM, Haselton DR, Stanford CM, Vargas MA. Relative translucency of six all-ceramic systems. Part I: Core materials. J Prosthet Dent. 2002;88:4–9. [PubMed] [Google Scholar]
- 19.Heffernan MJ, Aquilino SA, Diaz-Arnold AM, Haselton DR, Stanford CM, Vargas MA. Relative translucency of six all-ceramic systems. Part II: Core and veneer materials. J Prosthet Dent. 2002;88:10–5. [PubMed] [Google Scholar]
- 20.Nakamura T, Saito O, Fuyikawa J, Ishigaki S. Influence of abutment substrate and ceramic thickness on the colour of heat-pressed ceramic crowns. J Oral Rehabil. 2002;29:805–9. doi: 10.1046/j.1365-2842.2002.00919.x. [DOI] [PubMed] [Google Scholar]
- 21.Wee AG, Monaghan P, Johnston WM. Variation in color between intended matched shade and fabricated shade of dental porcelain. J Prosthet Dent. 2002;87:657–66. doi: 10.1067/mpr.2002.125727. [DOI] [PubMed] [Google Scholar]
- 22.Dozic A, Kleverlaan CJ, Meegdes M, van der Zel J, Feilzer AJ. The influence of porcelain layer thickness on the final shade of ceramic restorations. J Prosthet Dent. 2003;90:563–70. doi: 10.1016/s0022-3913(03)00517-1. [DOI] [PubMed] [Google Scholar]
- 23.Chu FC, Chow TW, Chai J. Contrast ratios and masking ability of three types of ceramic veneers. J Prosthet Dent. 2007;98:359–64. doi: 10.1016/S0022-3913(07)60120-6. [DOI] [PubMed] [Google Scholar]
- 24.Mackert JR, Jr, Russell CM. Leucite crystallization during processing of a heat-pressed dental ceramic. Int J Prosthodont. 1996;9:261–5. [PubMed] [Google Scholar]


