Abstract
Numerous studies describe associations between markers of inflammation and arterial hypertension (aHT), but does that imply causality? Interventional studies that reduce blood pressure reduced also markers of inflammation, but does immunosuppression improve hypertension? Here, we review the available mechanistic data. Aberrant immunity can trigger endothelial dysfunction but is hardly ever the primary cause of aHT. Innate and adaptive immunity get involved once hypertension has caused vascular wall injury as immunity is a modifier of endothelial dysfunction and vascular wall remodelling. As vascular remodelling progresses, immunity-related mechanisms can become significant cofactors for cardiovascular (CV) disease progression; vice versa, suppressing immunity can improve hypertension and CV outcomes. Innate and adaptive immunity both contribute to vascular wall remodelling. Innate immunity is driven by danger signals that activate Toll-like receptors and other pattern-recognition receptors. Adaptive immunity is based on loss of tolerance against vascular autoantigens and includes autoreactive T-cell immunity as well as non-HLA angiotensin II type 1 receptor-activating autoantibodies. Such processes involve numerous other modulators such as regulatory T cells. Together, immunity is not causal for hypertension but rather an important secondary pathomechanism and a potential therapeutic target in hypertension.
Keywords: atherosclerosis, blood pressure, infection, inflammasome, stenosis
INTRODUCTION
Arterial hypertension (aHT) is a clinical syndrome with a plethora of underlying pathomechanisms, including mono- or multigenic traits, environmental factors, sleep apnoea, renal (vascular) disease and endocrinopathies [1]. A growing body of literature now also proposes a causative role of innate and/or adaptive immunity in aHT based on epidemiological and experimental studies in rodents. But why should evolution favour immunity as a regulator of blood pressure (BP)? BP control and host defence are all essential mechanisms of homeostasis in higher organisms. Infection can cause hypotension via fluid losses in fever, tachypnoea or diarrhoea as well as decreased fluid intake of the febrile patient. In addition, infection increases vascular permeability to allow the large pentameric IgM to reach interstitial compartments, but this mechanism also implies a decline in intravascular fluid and hypotension. Also sterile injuries caused by major trauma, toxins or ischaemia–reperfusion induce inflammation-related vascular fluid losses. Thus, the risk of inflammation-related hypotension may have favoured the selection of mechanisms that link immune activation to BP increases for short-term survival benefits. In this review, we summarize the available evidence and propose a concept if, when and why immunity contributes to BP control and aHT.
THE IMMUNE SYSTEM IN ARTERIAL : HYPERTENSION: PRIMARY CAUSE OR SECONDARY COFACTOR?
Does the immune system cause aHT?
To nominate innate or adaptive immunity as causative or an initiator of aHT would require distinct types of evidence. None of the monogenetic forms of aHT involve immunity-related genes but rather stress the role of hormones and the kidney in BP control [1]. Also, multiple genome-wide association studies (GWAS) identified numerous gene loci being associated with aHT, but none of these loci clearly host immunity-related genes [2]. These data do not support a causative role of the immune system in essential aHT (Table 1).
Table 1.
Point-to-point summary
| Immunity is not a primary cause of hypertension. |
| No monogenetic disorders of immunity leading to hypertension. |
| GWAS studies did not identify proven immunity-related risks alleles. |
| Innate immunity can be a secondary cause of hypertension. |
| Hypertension induces tissue injury, which leads to DAMP release. |
| DAMPs activate pattern recognition receptors like TLR. |
| Injury- and TLR-mediated macrophage activation leads to vascular wall inflammation. |
| Vascular wall inflammation increases stiffness and aggravates hypertension. |
| Adaptive immunity can cause or aggravate hypertension. |
| Loss of tolerance can cause immunization against vascular wall components. |
| In this manner antigen-presenting cells, T cells, and autoantibodies get involved. |
| Anti-AT2R IgG and other autoantibodies have been documented upon kidney transplantation or in other autoimmune disorders such as scleroderma. |
GWAS, genome-wide association studies; DAMP, damage-associated molecular patterns; TLR, toll-like receptor.
Is immunity a cofactor in aHT?
aHT induces vascular wall injury and remodelling. The immune system is a sensitive sensor of tissue injury and is involved in all phases of the injury itself as well as the compensatory mechanisms of regeneration or repair [3]. Sterile injuries activate innate immunity, i.e. cytokine and lipid mediators or inflammation as well as all sorts of leukocyte subsets that contribute to (vascular wall) inflammation in an antigen-independent manner [4, 5]. In case loss of tolerance occurs, also adaptive immunity may contribute to vascular wall inflammation [6, 7]. The resulting endothelial dysfunction and increased vascular wall stiffness further contribute to aHT. In fact, given the plethora of genetic, environmental, sleep-related, renovascular and endocrine causes for aHT, this secondary involvement of immunity during vascular wall injury and remodelling becomes a shared pathomechanism across the numerous diseases that share aHT as a common symptom [4, 5]. Alternatively, environmental factors may trigger aberrant immunity and drive vascular wall injury followed by hypertension, but few data support this theoretical consideration.
Together, the contribution of immunity to hypertension is most likely rather a secondary phenomenon upon vascular injury. However, immunity becomes an accelerating factor for aHT by increasing endothelial dysfunction and vascular wall stiffness. As such, the contribution of immunity to aHT is conceptually similar to that of aHT-induced vascular wall hypertrophy and calcification, which also increases peripheral resistance by reducing vascular wall compliance or that of aHT-induced chronic kidney disease, which accelerates aHT via renin-angiotensin system activation.
CLINICAL EVIDENCE LINKING : HYPERTENSION AND IMMUNITY
Epidemiological studies document associations
A population-based study of apparently healthy men observed a significant linear relationship between systolic BP, diastolic BP and mean arterial pressure with levels of sICAM-1 or IL-6 [8]. In the same cohort, inflammatory biomarkers were found to be strong predictors of future risk of cardiovascular (CV) non-fatal events and death, suggesting a causal relationship between BP, inflammation and atherogenesis. Other observational, cross-sectional studies of the general population confirmed these associations [9–15]. Furthermore, systolic BP was a strong and independent predictor of plasma C-reactive protein concentrations in patients with newly diagnosed, untreated aHT [16]. Other authors also found that levels of plasma-soluble CD40L, which contributes to the angiotensin II-induced pro-thrombotic state, vascular inflammation, oxidative stress and endothelial dysfunction, are increased in subjects with essential aHT and that platelets present a higher expression of CD40/CD40L [17]. Furthermore, in end-stage renal disease (ESRD) patients, the chronic volume overload, high sympathetic activity and high levels of angiotensin II not only trigger aHT but also exert an inflammatory and growth-promoting effect on the CV system in this high-risk population [18].
Can clinical studies also document causal relationships?
Evidence on a causal link between immunity and hypertension in humans is limited. As a future research line, clinical trials testing immunosuppressant drugs should be evaluated on their effect on BP, like it has been done in patients with psoriasis [19]. Vice versa, antihypertensive drugs and BP control may have an effect on inflammation biomarkers, thus, advocating important clinical implications for hypertension-related CV complications. In a study by Fliser et al. angiotensin II receptor blockade significantly reduced vascular microinflammation in patients with aHT by as early as 6 weeks of therapy. The beneficial CV effects of angiotensin II receptor antagonists could be due to their action in reducing inflammatory biomarkers [20]. These results were subsequently confirmed by Derosa et al. in a clinical trial including 276 essential hypertensive patients randomized to olmesartan, amlodipine or a single pill containing an olmesartan/amlodipine combination for 12 months [21]. This study demonstrated that olmesartan/amlodipine significantly decreased C-reactive protein level and that their combination was more effective than single monotherapies in reducing inflammatory biomarkers [21]. Moreover, in a randomized clinical trial in untreated hypertensive patients, amlodipine plus valsartan reduced circulating levels of endocan, which is a biomarker reflecting vascular inflammation and endothelial dysfunction in humans [22]. All in all, these findings support the hypothesis that angiotensin receptor blocker (ARB) and calcium antagonists may act as anti-inflammatory drugs in patients with essential aHT. However, future prospective and properly designed clinical studies are strongly needed to shed some light on whether or what class of antihypertensive drugs could be beneficial not only for BP control but for inflammation-related CV complications as well. More importantly, it could be postulated that immunotherapy might be useful to treat the most serious degrees of aHT. From this perspective of the problem, vaccines could be a therapeutic option for the treatment of aHT in the future.
MECHANISTIC LINKS BETWEEN : HYPERTENSION AND IMMUNITY
Innate immunity
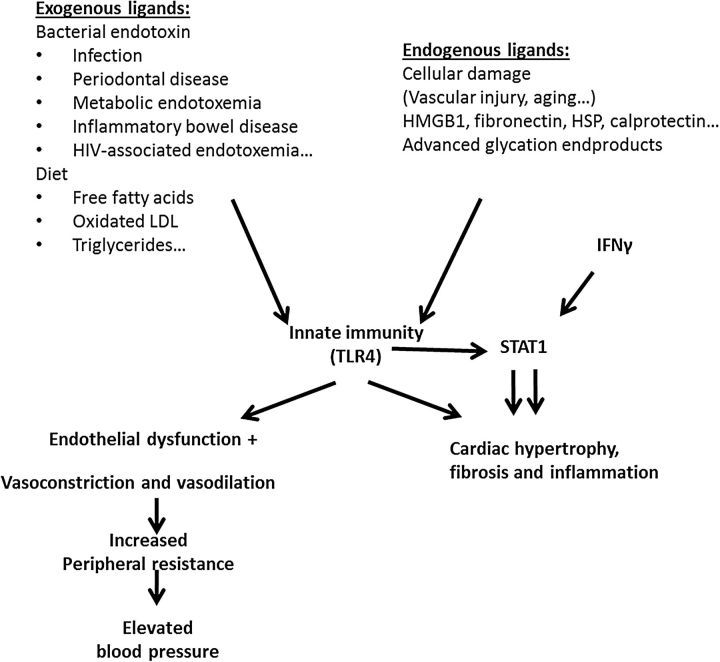
As the most data are available on the action of TLR4 on hypertensive target organ damage and hypertension, the focus here is set primarily on TLR4 (Figure 1). The best-known source of TLR4 ligand is lipopolysaccharide (LPS) derived from Gram-negative bacteria. Other TLR4 ligands, such as HMGB-1 and HSPs, exist and are released from dying cells during injury [23, 24]. In addition, vascular aging exposes immune cells to fibronectin breakdown products with TLR4 agonistic properties [25]. Importantly, vascular aging is the key event for systolic BP increase with age. Western diet is a large source of TLR4 ligands. Free fatty acids, oxLDL and triglycerides are known to activate TLR4 [26]. Proteins of the S100 family such as calprotectin are known TLR4 activators. Calprotectin is known to be present in inflammatory bowel disease and acute coronary plaque rupture [27]. Additionally, in context with diabetes, advanced glycation end product (AGE) not only activates the receptor for AGE (RAGE) but also acts as endogenous TLR4 ligands [28].
FIGURE 1:
Innate immunity in hypertension. A broad variety of endogenous and exogenous TLR4 ligands can activate immune signalling, which promotes vasoconstriction, peripheral resistance, and a rise in BP. Besides, interaction between innate and adaptive immune system induces CV damage such as cardiac hypertrophy, fibrosis and inflammation by involving the transcription factor STAT1. HMGB1, high-mobility group box-1; HSP, heat-shock protein; LPS, lipopolysaccharide; IFN-γ, interferon gamma; STAT, signal transducers and activators of transcription; TLR4, Toll-like receptor-4.
TLR4 is present on endothelial cells throughout the vasculature, and it is upregulated in human aHT as well as in spontaneously hypertensive rats [29]. TLR4 upregulation by angiotensin II contributes to vascular dysfunction through production of reactive oxygen species (ROS) [30]. This is evident for endothelial dysfunction and increased vascular constriction [31]. Similarly, TLR4 is involved in cardiac hypertrophy and fibrosis. Genetic deletion or blockade of TLR4 improves cardiac function, hypertrophy and fibrosis and attenuates myocardial inflammation [32].
TLR4 agonists and other danger signals activate cells of the monocyte/macrophage lineage in infection, sterile inflammation and in aHT or aHT-related target organ damage [33]. In addition, innate immunity directly triggers vasoconstriction and reduced vasorelaxation, which contribute to aHT by increasing peripheral resistance. Little evidence exists that innate mechanisms directly cause aHT. TLR4 contributes to BP regulation and vascular constriction in spontaneously hypertensive rats [34]. Mouse experiments revealed in an L-NAME-induced proinflammatory model of aHT that TLR4 signalling in BP elevation [31]. Here, the relevance of endogenous TLR4 ligands due to inflammation-induced damage was evidenced as link for ROS production causing increased vasoconstriction and BP elevation [31]. Whereas GWAS did not demonstrate a role for TLR4 in hypertension, human data of a smaller cohorts suggest an involvement of TLR4 ligands in BP regulation such as HMGB1 polymorphism [35]. It might be possible that specific patient characteristics are needed to reveal the influence of single nucleotide polymorphisms related to innate immune signalling.
During the past years, Titze and his group developed an interesting concept of how macrophages regulate salt-dependent volume and BP in salt-sensitive hypertension [36]. They showed that the skin and the lymphatic system represent a third space of salt storage in hypertensive and ESRD patients [37]. Salt retention was shown to increase local tonicity and to activate mononuclear phagocyte recruitment to the skin [38]. There they sense sodium accumulation and initiate mechanisms to reduce sodium deposition in the skin. A specific reduction in salt deposition in the skin reduces BP. Thus, in this context, innate immune cells act as ‘good guys’ sensing tonicity changes via nuclear factor of activated T-cell 5 (NFAT5; also called TONEBP) and regulating interstitial sodium balance.
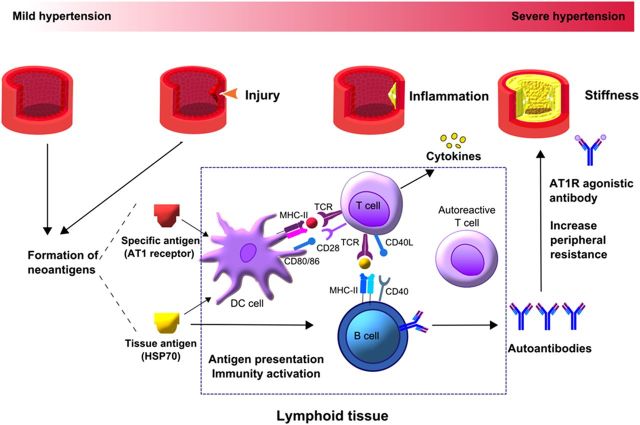
Adaptive immunity
Wallukat et al. first documented the causal role of non-HLA angiotensin II type 1 (AT(1)) receptor-activating autoantibodies for pregnancy-related hypertension and later also for kidney transplant-related malignant hypertension [39, 40]. They occur also in essential hypertension, especially in refractory hypertension [41]. Such antibodies bind to the extracellular domain of the AT(1) receptor and induce angiotensin II-independent receptor activation, which can be blocked with AT receptor blockers [39, 40]. Meanwhile, autoantibodies against other vascular antigens or heat-shock proteins have been identified [42, 43]. While transplant-related sensitization may involve alloimmunity, transplant-independent sensitization must involve other mechanisms [44]. Pregnancy itself could be excluded as a mode of sensitization [45]. One concept is that vascular injury, including hypertension-induced vascular injury, is a trigger for autoantigen modification and sensitization in genetically susceptible patients [1, 4, 6, 7]. Loss of tolerance is usually associated with variants in the human leukocyte antigen. In Chinese patients with essential hypertension, the HLA-DRB1(*) 04 allele is associated with the presence of anti-AT(1) receptor antibodies [46]. Upon loss of tolerance, the process of autoantigen presentation in the context of co-stimulatory molecules becomes the driving pathomechanism for the activation of autoreactive effector lymphocytes, which include B cells and various T-cell subsets [47]. As this process is located within secondary lymphoid organs, the vast majority of the mechanistic data relies on rodent models of hypertension. In fact, blocking or deleting the co-stimulatory molecules CD80 and CD86 on dendritic cells prevents hypertension and T-cell activation in both angiotensin II- and DOCA-salt-induced hypertension [48]. A recent study documents that dendritic cell activation involves the production of highly reactive γ-ketoaldehydes (isoketals) in hypertension that accumulate in dendritic cells and oxidize proteins [49]. Isoketal accumulation activates dendritic cell activation and their capacity to promote CD8+ T-cell proliferation, production of IFN-γ and IL-17A, and hypertension [49]. Kirabo et al. also found plasma F2-isoprostanes that are formed together with isoketals to be elevated in patients with essential hypertension, particularly in those with resistant hypertension [49]. The authors concluded that hypertension activates dendritic cells via promoting the formation of isoketals that in turn aggravate hypertension-related adaptive immunity, which further aggravates hypertension (Figure 2).
FIGURE 2:
Adaptive immunity in hypertension. aHT induces vascular injury, which supports neoantigen formation and, in susceptible individuals, eventually loss of tolerance. This process involves neoantigen presentation by dendritic cells and B cells within secondary lymphoid tissues. Loss of tolerance implies that this process overcomes the anergy of autoreactive lymphocytes leading to their activation and clonal expansion. The results are autoantibody production and an increasing number of autoreactive T-effector cells that drive and accelerate vascular wall inflammation and remodelling once they reach the vasculature. As a result, increased vascular stiffness and peripheral resistance occur, which both aggravate the preexisting aHT.
Autoimmunity cannot only aggravate hypertension via humoral mechanisms such as anti-AT(1) receptor antibodies but also via T-cell-mediated inflammation. Antigen-specific T-helper cells may drive humoral immunity by supporting B-cell proliferation. In addition, CD8+ T-effector cells infiltrate the vascular wall, a process that increases vascular wall inflammation, stiffness and narrowing of the lumen, which all increase peripheral resistance. In fact, athymic nude mice or T-cell-deficient mice are protected from experimental hypertension as reviewed in Refs. [4, 7]. Furthermore, non-specific immunosuppressive drugs such as mycophenolate mofetil, cyclosporine A, cyclophosphamide or NF-κB inhibitors lower BP in rodent models of hypertension [7]. This finding was subsequently confirmed in humans with essential hypertension, which markedly improved upon treatment of their psoriasis or rheumatoid arthritis with mycophenolate mofetil [50]. Innate and adaptive immunity are both regulated by CD4/CD25/Foxp3+ regulatory T cells; hence, adoptive transfer of such regulatory T cells improved angiotensin II- or aldosterone-induced hypertension [7, 51].
In this context, it is of interest that high salt conditions can drive autoreactive Th17 cells via NFAT5 and serum/glucocorticoid-regulated kinase 1 signalling. This was formally demonstrated in a rodent model of autoimmune encephalomyelitis but might also apply to autoimmunity-related hypertension [52, 53].
As another potential mechanism that links immunity with hypertension, renal immune cell infiltrates have been found to be associated with decreased pressure natriuresis and aHT [54, 55]. Proving a potential causal relationship between renal interstitial inflam-295 mation and aHT would require a selective deletion of renal immune cell infiltrates, which is not possible with immunosuppressive drugs with systemic actions; hence, this concept could not yet be validated.
Together, immune activation during hypertension involves the adaptive immune system in several ways. Some patients develop autoantibodies against angiotensin receptors, with agonistic properties that can be neutralized with ARB. Autoimmunity can also be directed against vascular wall antigens with subsequent T-cell-dependent vascular wall inflammation, which increases vascular resistance. These processes are secondary mechanisms to existing hypertension and may operate in a subset but not necessarily in all patients.
CONFLICT OF INTEREST STATEMENT
None declared. The results presented in this article have not been published previously in whole or part.
ACKNOWLEDGEMENT
The authors thank Yajuan Liu for her help with Figure 2.
REFERENCES
- 1.Coffman TM. Under pressure: the search for the essential mechanisms of hypertension. Nat Med 2011; 17: 1402–1409 [DOI] [PubMed] [Google Scholar]
- 2.Simino J, Rao DC, Freedman BI. Novel findings and future directions on the genetics of hypertension. Curr Opin Nephrol Hypertens 2012; 21: 500–507 [DOI] [PubMed] [Google Scholar]
- 3.Medzhitov R. Origin and physiological roles of inflammation. Nature 2008; 454: 428–435 [DOI] [PubMed] [Google Scholar]
- 4.De Ciuceis C, Rossini C, La Boria E, et al. Immune mechanisms in hypertension. High Blood Press Cardiovasc Prev 2014; 21: 227–234 [DOI] [PubMed] [Google Scholar]
- 5.De Miguel C, Rudemiller NP, Abais JM, et al. Inflammation and hypertension: new understandings and potential therapeutic targets. Curr Hypertens Rep 2015; 17: 507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mathis KW, Broome HJ, Ryan MJ. Autoimmunity: an underlying factor in the pathogenesis of hypertension. Curr Hypertens Rep 2014; 16: 424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rodriguez-Iturbe B, Pons H, Quiroz Y, et al. Autoimmunity in the pathogenesis of hypertension. Nat Rev Nephrol 2014; 10: 56–62 [DOI] [PubMed] [Google Scholar]
- 8.Chae CU, Lee RT, Rifai N, et al. Blood pressure and inflammation in apparently healthy men. Hypertension 2001; 38: 399–403 [DOI] [PubMed] [Google Scholar]
- 9.Bautista LE, Atwood JE, O'Malley PG, et al. Association between C-reactive protein and hypertension in healthy middle-aged men and women. Coron Artery Dis 2004; 15: 331–336 [DOI] [PubMed] [Google Scholar]
- 10.Bautista LE, Lopez-Jaramillo P, Vera LM, et al. Is C-reactive protein an independent risk factor for essential hypertension? J Hypertens 2001; 19: 857–861 [DOI] [PubMed] [Google Scholar]
- 11.Bautista LE, Vera LM, Arenas IA, et al. Independent association between inflammatory markers (C-reactive protein, interleukin-6, and TNF-alpha) and essential hypertension. J Hum Hypertens 2005; 19: 149–154 [DOI] [PubMed] [Google Scholar]
- 12.Engstrom G, Janzon L, Berglund G, et al. Blood pressure increase and incidence of hypertension in relation to inflammation-sensitive plasma proteins. Arterioscler Thromb Vasc Biol 2002; 22: 2054–2058 [DOI] [PubMed] [Google Scholar]
- 13.Fernandez-Real JM, Vayreda M, Richart C, et al. Circulating interleukin 6 levels, blood pressure, and insulin sensitivity in apparently healthy men and women. J Clin Endocrinol Metab 2001; 86: 1154–1159 [DOI] [PubMed] [Google Scholar]
- 14.Ito H, Ohshima A, Tsuzuki M, et al. Association of serum tumour necrosis factor-alpha with serum low-density lipoprotein-cholesterol and blood pressure in apparently healthy Japanese women. Clin Exp Pharmacol Physiol 2001; 28: 188–192 [DOI] [PubMed] [Google Scholar]
- 15.Sung KC, Suh JY, Kim BS, et al. High sensitivity C-reactive protein as an independent risk factor for essential hypertension. Am J Hypertens 2003; 16: 429–433 [DOI] [PubMed] [Google Scholar]
- 16.Schillaci G, Pirro M, Gemelli F, et al. Increased C-reactive protein concentrations in never-treated hypertension: the role of systolic and pulse pressures. J Hypertens 2003; 21: 1841–1846 [DOI] [PubMed] [Google Scholar]
- 17.Yan JC, Ma GS, Wu ZG, et al. Increased levels of CD40-CD40 ligand system in patients with essential hypertension. Clin Chim Acta 2005; 355: 191–196 [DOI] [PubMed] [Google Scholar]
- 18.Zoccali C, Mallamaci F, Tripepi G. Novel cardiovascular risk factors in end-stage renal disease. J Am Soc Nephrol 2004; 15 (Suppl 1): S77–S80 [DOI] [PubMed] [Google Scholar]
- 19.Brown G, Malakouti M, Wang E, et al. Anti-IL-17 phase II data for psoriasis: a review. J Dermatolog Treat 2015; 26: 32–36 [DOI] [PubMed] [Google Scholar]
- 20.Fliser D, Buchholz K, Haller H; EUropean Trial On Olmesartan and Pravastatin In InflammationAtherosclerosis Investigators. Antiinflammatory effects of angiotensin II subtype 1 receptor blockade in hypertensive patients with microinflammation. Circulation 2004; 110: 1103–1107 [DOI] [PubMed] [Google Scholar]
- 21.Derosa G, Cicero AF, Carbone A, et al. Results from a 12 months, randomized, clinical trial comparing an olmesartan/amlodipine single pill combination to olmesartan and amlodipine monotherapies on blood pressure and inflammation. Eur J Pharm Sci 2014; 51: 26–33 [DOI] [PubMed] [Google Scholar]
- 22.Celik T, Balta S, Karaman M, et al. Endocan, a novel marker of endothelial dysfunction in patients with essential hypertension: comparative effects of amlodipine and valsartan. Blood Press 2015; 24: 55–60 [DOI] [PubMed] [Google Scholar]
- 23.Bald T, Quast T, Landsberg J, et al. Ultraviolet-radiation-induced inflammation promotes angiotropism and metastasis in melanoma. Nature 2014; 507: 109–113 [DOI] [PubMed] [Google Scholar]
- 24.Chen XL, Sun L, Guo F, et al. High-mobility group box-1 induces proinflammatory cytokines production of Kupffer cells through TLRs-dependent signaling pathway after burn injury. PLoS One 2012; 7: e50668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Takasaki I, Chobanian AV, Sarzani R, et al. Effect of hypertension on fibronectin expression in the rat aorta. J Biol Chem 1990; 265: 21935–9 [PubMed] [Google Scholar]
- 26.Bae YS, Lee JH, Choi SH, et al. Macrophages generate reactive oxygen species in response to minimally oxidized low-density lipoprotein: toll-like receptor 4- and spleen tyrosine kinase-dependent activation of NADPH oxidase 2. Circ Res 2009; 104: 210–218, 21p following 218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Baumann M, Schmaderer C, Burkhardt K, et al. MRP8/14 is associated with systemic inflammation in stable coronary atherosclerosis in men. Eur J Clin Invest 2011; 41: 1261–1267 [DOI] [PubMed] [Google Scholar]
- 28.Hodgkinson CP, Laxton RC, Patel K, et al. Advanced glycation end-product of low density lipoprotein activates the toll-like 4 receptor pathway implications for diabetic atherosclerosis. Arterioscler Thromb Vasc Biol 2008; 28: 2275–2281 [DOI] [PubMed] [Google Scholar]
- 29.Eissler R, Schmaderer C, Rusai K, et al. Hypertension augments cardiac Toll-like receptor 4 expression and activity. Hypertens Res 2011; 34: 551–558 [DOI] [PubMed] [Google Scholar]
- 30.De Batista PR, Palacios R, Martin A, et al. Toll-like receptor 4 upregulation by angiotensin II contributes to hypertension and vascular dysfunction through reactive oxygen species production. PLoS One 2014; 9: e104020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sollinger D, Eissler R, Lorenz S, et al. Damage-associated molecular pattern activated Toll-like receptor 4 signalling modulates blood pressure in L-NAME-induced hypertension. Cardiovasc Res 2014; 101: 464–472 [DOI] [PubMed] [Google Scholar]
- 32.Dange RB, Agarwal D, Masson GS, et al. Central blockade of TLR4 improves cardiac function and attenuates myocardial inflammation in angiotensin II-induced hypertension. Cardiovasc Res 2014; 103: 17–27 [DOI] [PubMed] [Google Scholar]
- 33.Pryshchep O, Ma-Krupa W, Younge BR, et al. Vessel-specific Toll-like receptor profiles in human medium and large arteries. Circulation 2008; 118: 1276–1284 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bomfim GF, Dos Santos RA, Oliveira MA, et al. Toll-like receptor 4 contributes to blood pressure regulation and vascular contraction in spontaneously hypertensive rats. Clin Sci (Lond) 2012; 122: 535–543 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Yao Y, Guo D, Yang S, et al. HMGB1 gene polymorphism is associated with hypertension in Han Chinese population. Clin Exp Hypertens 2015; 37: 166–171 [DOI] [PubMed] [Google Scholar]
- 36.Machnik A, Neuhofer W, Jantsch J, et al. Macrophages regulate salt-dependent volume and blood pressure by a vascular endothelial growth factor-C-dependent buffering mechanism. Nat Med 2009; 15: 545–552 [DOI] [PubMed] [Google Scholar]
- 37.Kopp C, Linz P, Dahlmann A, et al. 23Na magnetic resonance imaging-determined tissue sodium in healthy subjects and hypertensive patients. Hypertension 2013; 61: 635–640 [DOI] [PubMed] [Google Scholar]
- 38.Machnik A, Dahlmann A, Kopp C, et al. Mononuclear phagocyte system depletion blocks interstitial tonicity-responsive enhancer binding protein/vascular endothelial growth factor C expression and induces salt-sensitive hypertension in rats. Hypertension 2010; 55: 755–761 [DOI] [PubMed] [Google Scholar]
- 39.Dragun D, Muller DN, Brasen JH, et al. Angiotensin II type 1-receptor activating antibodies in renal-allograft rejection. N Engl J Med 2005; 352: 558–569 [DOI] [PubMed] [Google Scholar]
- 40.Wallukat G, Homuth V, Fischer T, et al. Patients with preeclampsia develop agonistic autoantibodies against the angiotensin AT1 receptor. J Clin Invest 1999; 103: 945–952 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Liao YH, Wei YM, Wang M, et al. Autoantibodies against AT1-receptor and alpha1-adrenergic receptor in patients with hypertension. Hypertens Res 2002; 25: 641–646 [DOI] [PubMed] [Google Scholar]
- 42.Dragun D, Catar R, Philippe A. Non-HLA antibodies in solid organ transplantation: recent concepts and clinical relevance. Curr Opin Organ Transplant 2013; 18: 430–435 [DOI] [PubMed] [Google Scholar]
- 43.Pons H, Ferrebuz A, Quiroz Y, et al. Immune reactivity to heat shock protein 70 expressed in the kidney is cause of salt-sensitive hypertension. Am J Physiol Renal Physiol 2013; 304: F289–F299 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Giral M, Foucher Y, Dufay A, et al. Pretransplant sensitization against angiotensin II type 1 receptor is a risk factor for acute rejection and graft loss. Am J Transplant 2013; 13: 2567–2576 [DOI] [PubMed] [Google Scholar]
- 45.Honger G, Cardinal H, Dieude M, et al. Human pregnancy and generation of anti-angiotensin receptor and anti-perlecan antibodies. Transpl Int 2014; 27: 467–474 [DOI] [PubMed] [Google Scholar]
- 46.Zhu F, Sun Y, Wang M, et al. Correlation between HLA-DRB1, HLA-DQB1 polymorphism and autoantibodies against angiotensin AT(1) receptors in Chinese patients with essential hypertension. Clin Cardiol 2011; 34: 302–308 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Goodnow CC. Multistep pathogenesis of autoimmune disease. Cell 2007; 130: 25–35 [DOI] [PubMed] [Google Scholar]
- 48.Vinh A, Chen W, Blinder Y, et al. Inhibition and genetic ablation of the B7/CD28 T-cell costimulation axis prevents experimental hypertension. Circulation 2010; 122: 2529–2537 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kirabo A, Fontana V, De Faria AP, et al. DC isoketal-modified proteins activate T cells and promote hypertension. J Clin Invest 2014; 124: 4642–4656 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Herrera J, Ferrebuz A, Macgregor EG, et al. Mycophenolate mofetil treatment improves hypertension in patients with psoriasis and rheumatoid arthritis. J Am Soc Nephrol 2006; 17: S218–S225 [DOI] [PubMed] [Google Scholar]
- 51.Idris-Khodja N, Mian MO, Paradis P, et al. Dual opposing roles of adaptive immunity in hypertension. Eur Heart J 2014; 35: 1238–1244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kleinewietfeld M, Manzel A, Titze J, et al. Sodium chloride drives autoimmune disease by the induction of pathogenic TH17 cells. Nature 2013; 496: 518–522 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Wu C, Yosef N, Thalhamer T, et al. Induction of pathogenic TH17 cells by inducible salt-sensing kinase SGK1. Nature 2013; 496: 513–517 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Franco M, Martinez F, Quiroz Y, et al. Renal angiotensin II concentration and interstitial infiltration of immune cells are correlated with blood pressure levels in salt-sensitive hypertension. Am J Physiol Regul Integr Comp Physiol 2007; 293: R251–R256 [DOI] [PubMed] [Google Scholar]
- 55.Franco M, Tapia E, Bautista R, et al. Impaired pressure natriuresis resulting in salt-sensitive hypertension is caused by tubulointerstitial immune cell infiltration in the kidney. Am J Physiol Renal Physiol 2013; 304: F982–F990 [DOI] [PMC free article] [PubMed] [Google Scholar]