Abstract
Purpose
Lean is a widely used quality improvement methodology initially developed and used in the automotive and manufacturing industries but recently expanded to the healthcare sector. This systematic literature review seeks to independently assess the effect of Lean or Lean interventions on worker and patient satisfaction, health and process outcomes, and financial costs.
Data sources
We conducted a systematic literature review of Medline, PubMed, Cochrane Library, CINAHL, Web of Science, ABI/Inform, ERIC, EMBASE and SCOPUS.
Study selection
Peer reviewed articles were included if they examined a Lean intervention and included quantitative data. Methodological quality was assessed using validated critical appraisal checklists. Publically available data collected by the Saskatchewan Health Quality Council and the Saskatchewan Union of Nurses were also analysed and reported separately.
Data extraction
Data on design, methods, interventions and key outcomes were extracted and collated.
Results of data synthesis
Our electronic search identified 22 articles that passed methodological quality review. Among the accepted studies, 4 were exclusively concerned with health outcomes, 3 included both health and process outcomes and 15 included process outcomes. Our study found that Lean interventions have: (i) no statistically significant association with patient satisfaction and health outcomes; (ii) a negative association with financial costs and worker satisfaction and (iii) potential, yet inconsistent, benefits on process outcomes like patient flow and safety.
Conclusion
While some may strongly believe that Lean interventions lead to quality improvements in healthcare, the evidence to date simply does not support this claim. More rigorous, higher quality and better conducted scientific research is required to definitively ascertain the impact and effectiveness of Lean in healthcare settings.
Keywords: Lean, Lean thinking, Lean interventions, quality improvement, healthcare
Introduction
Globally, healthcare systems are at a cross roads. Many political and healthcare leaders, and in fact the public itself is calling for, if not demanding, the redesign of healthcare delivery. The concern is fuelled by ever increasing costs and high expectations, while at the same time having surprisingly low rates of patient adherence to care and high rates of adverse events [1]. In response, many jurisdictions have attempted to introduce standardized protocols like Lean.
Lean is a widely used quality improvement methodology. Lean thinking was first developed in the automotive and manufacturing industries but it has recently expanded to the healthcare sector. Lean thinking begins with identifying and ‘removing waste’ in order to ‘add value’ to the customer or patient [2]. The Lean Enterprise Institute articulates five main principles of Lean: specify value from the standpoint of the customer, identify all the steps in the value stream and eliminate steps that do not create value, make the steps flow smoothly toward the customer, let customers pull value from the next upstream activity and begin the process again until a state of perfection is reached [3].
The introduction of these principles placed ‘customer value’ and ‘removing waste’ at the centre of Lean thinking. In this manner, the process is essentially driven by ‘what customers want’ and then organizational steps are taken to define which activities are considered to be ‘value-adding’ as opposed to ‘non-value adding’. ‘Value adding’ activities are encouraged because they directly contribute to creating a product or service a customer wants. On the other hand, ‘non-value adding’ activities are considered a waste and need to be removed or avoided [4].
To date, there have been a limited number of reviews of Lean or Lean interventions in healthcare. One of the reviews started with 207 articles under consideration. However, when the authors applied their inclusion criteria of only accepting papers that were published in peer review journals and studies that had quantifiable data available, it left them with merely 19 papers (9.2%) for critical appraisal [5].
Among the papers accepted, it was noted that the vast majority of studies had methodological limitations that undermined the validity of the results. These limitations included weak study designs, lack of statistical analysis, inappropriate statistical assumptions, inappropriate analysis, failure to rule out alternative hypotheses, no adjustment for confounding, selection bias and lack of control groups. The studies also did not review long-term organizational change, long-term impact or the independent effect of Lean while controlling for other organizational or staffing changes occurring at the same time [5]. Although this review was well-conducted, it was not a systematic literature review and it did not include a quality control checklist.
In North America, there are many examples of Lean healthcare interventions but the largest Lean transformation in the world was attempted in the province of Saskatchewan, Canada [6]. The Health Quality Council (HQC) of Saskatchewan concludes on its website that Lean increases patient safety by eliminating errors, increases patient satisfaction, reduces cost and improves patient health outcomes [7].
On the surface, Lean thinking seems to be an approach that generates positive results [8]. Yet, its application in healthcare has been controversial and its effectiveness questioned. As such, the purpose of this systematic literature review is to independently assess the effect of Lean thinking and Lean interventions on worker and patient satisfaction, health and process outcomes and financial costs.
Methods
We conducted an extensive systematic literature review on the following electronic databases: Medline, PubMed, Cochrane Library, CINAHL, Web of Science, ABI/Inform, ERIC, EMBASE and SCOPUS.
Searches were carried out using the following keywords: Lean Production System, Lean enterprise, Lean manufacturing, Virginia Mason Production System, Toyota Production System, Just in time production, Kaizen, HoshinKanri, Lean method, Lean thinking, Lean intervention, Lean healthcare, Lean principles, Lean process, Muda and Healthcare.
Peer-reviewed articles
Articles had to satisfy the following inclusion criteria to be considered: published in English, publicly available, peer reviewed, examined a Lean intervention and included quantitative data. These liberal criteria allowed the inclusion of a wide variety of relevant articles in our study. However, it also served as a means to exclude news reports, blog commentary, informational/promotional pieces and general ‘feel good’ success stories that lacked the necessary quantitative data to be able to critically judge the information presented.
The identification and approval of studies was carried out in three steps. First, the authors examined titles and abstracts to remove duplicates. Second, two of the authors (C.N. and M.L.) reviewed the full-text articles for relevance with regard to the field of healthcare and conformity to the inclusion criteria. Third, methodological quality was assessed by using validated critical appraisal checklists. The diffusion of innovations in health service checklists helped the authors assess the baseline comparability of the groups in each study, the research design, outcome measures and potential sources of bias. They were originally modelled after the Cochrane Effective Practice and Organization of Care Group for interventions in service delivery and organization [9]. Studies that scored >50% on the quality checklist were accepted (i.e. satisfied 6 or more out of 11 questions for before and after studies). Any disagreement between the two authors (C.N. and M.L.) was resolved by additional review and, if required, with a tie-breaking vote by the third author (J.M).
Grey literature
As mentioned, the largest Lean healthcare transformation in the world was attempted in the province of Saskatchewan, Canada [6]. The HQC has been surveying tens of thousands of patients over the years about their experiences in Saskatchewan hospitals. For the purposes of this systematic review, February 2012 was used as the cut-off point for the evaluation of pre- and post-Lean data as it coincided with the official date of the signed provincial contract with a Lean consultant firm [10]. A 26-month period was used to collect and analyse data on a monthly basis before Lean implementation (December 2009 to January 2012) and after Lean implementation (February 2012 to March 2014). This high quality data collected by certified Lean professionals have sample sizes ranging from 17 698 to 92 127 patients with a response rate of ∼51% and it is publicly available on a web site [11]. Additionally, the largest healthcare union or association in the province, the Saskatchewan Union of Nurses (SUN), contracted an external professional polling company to randomly survey 1500 nurses about their Lean experience in 2014 [12]. All 1500 nurses contacted, participated in the telephone survey.
Results
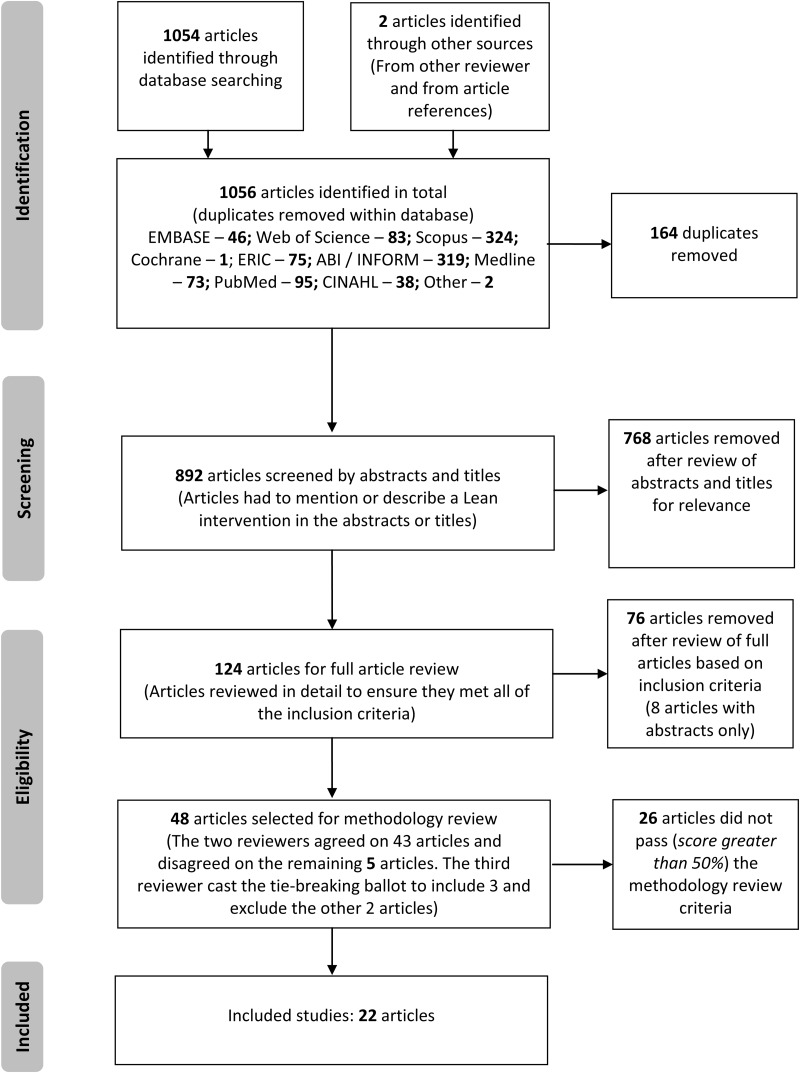
We identified a total of 1056 peer-reviewed articles of which 164 were removed as duplicates, 768 were removed due to lack of relevance to healthcare and 76 were removed because they did not meet the inclusion criteria. Among the 48 articles that were assessed for methodological quality, 22 articles passed [13–34] and 26 articles failed the checklist review [35–60] (Fig. 1 and Table 1). The original two reviewers (C.N. and M.L.) independently assessed and agreed on 43 studies with a tie breaking vote required by the third reviewer (J.M.) on five out of the 48 studies. Once finalized, the data from the included studies was pooled and summarized and confidence intervals for rate ratios were calculated with an established software application (SPSS 22.0).
Figure 1.
Prisma flow diagram of the included studies.
Table 1.
Detailed list of eligible peer review articles from the literature search
| Articles that passed methodology review | ||||||||
|---|---|---|---|---|---|---|---|---|
| First author's last name, year of publication, country where study was done | Study design | Number of participants | Location of intervention (ex. Emergency department) | Intervention | Intervention goal | Type of outcome | Quality scores | Outcome rate ratio and 95% CI |
| Health outcome studies | ||||||||
| Jha, 2012, USA [13] | Retrospective cohort | 6 000 000 | Hospital | Pay for performance | Reduce 30 day mortality rate | Health outcome | 9/11 Pass | 30 day mortality rate 0.08 (−0.30 to 0.46) |
| McCulloch, 2010, UK [14] | Interrupted time series | 2083 | Emergency surgery ward | PDCA | Reduced risk of care related harm | Health outcome | 6/11 Pass | Adverse events 0.91 (0.72–1.16) |
| Muder, 2008, USA [15] | Pre-/post-test | 215 | ICU and a surgical unit | Hand hygiene, contact precautions, active surveillance (TPS) | Reduce incidence of MRSA | Health outcome | 7/11 Pass | MRSA infections per 1000 patient days 2.47 (1.87–3.27) |
| Ellingson, 2011, USA [16] | Pre-/post- test | 109 | Veteran affairs hospital surgical ward | Systems and behaviour change to increase adherence to infection control precautions | Reduce in MRSA incidence rates | Health outcome | 7/11 Pass | MRSA incidence rate ratio 0.99 (0.98–1.01) |
| Process outcome studies | ||||||||
| Murrell, 2011, USA [17] | Pre-/post-test | 64 907 | Emergency department | Rapid triage and treatment | ED length of stay and physician wait time | Process outcome | 7/11 Pass | Unable to compute RR Length of stay reduced from 4.2 (4.2–4.3) to 3.6 (3.6–3.7) hours Physician start time reduced from 62.2 (61.5–63.0) to 41.9 (41.5–42.4) minutes |
| Kelly, 2007, Australia [18] | Pre-/post-test | 63 085 | Emergency department | Streaming of patients from triage, reallocation of medical and nursing staff (VSM) | Reduce number of patients who leave without being seen | Process outcome | 8/11 Pass | Left without being seen 0.99 (0.92–1.08) |
| Naik, 2012, USA [19] | Pre-/post-test | 22,527 | Emergency department | Identify and eliminate areas of waste | Emergency wait time | Process outcome | 6/11 Pass | Unable to compute RR Wait time reduced from 4.6 (4.5–4.9) to 4.0 (3.7–4.1) hours |
| Simons F, 2014, Netherlands [20] | Pre-/post-test | 8,009 | Operating room of University medical centre | DMAIC using A3 intervention | Door movements in the operating room | Process outcome | 6/11 Pass | Unable to compute RR Door movements reduced by 78% from an average of between 15 and 20 times per hour during surgery to 4 times per hour |
| Burkitt, 2009, USA [21] | Retrospective pre-/post | 2,550 | Veteran affairs surgical center | Staff training on hand hygiene, systematic culturing of all admissions, patient isolation | Increase appropriateness of perioperative antibiotics and reduction in length of stay | Process outcomes | 7/11 Pass | Length of stay 0.91 (0.76–1.08) |
| Weaver, 2013, USA [22] | Pre-/post-test | 2444 | Mental health clinic | Identify and eliminate areas of waste (TPS) | Improving number who attend first appointment, reduce wait for appointment | Process outcome | 9/11 Pass | Number who attended first appointment 1.0 (1.0–1.0) Wait reduced from 11 days to 8 days |
| LaGanga, 2011, USA [23] | Pre-/post-test | 1726 | Mental health center | Remove over booking | Increase capacity to admit new patients and reduce no-shows | Process outcome | 7/11 Pass | No shows 1.13 (1.03–1.23) |
| van Vliet, 2010, Netherlands [24] | Pre-/post-test | 1207 | Eye hospital | Identify and eliminate areas of waste | Reduce patient visits | Process outcome | 9/11 Pass | Patient visits 1.84 (1.33–2.56) |
| Martin, 2013, UK [25] | Pre-/post-test | 500 | Radiology department | Value stream analysis (VSM) | Reduce patient journey time | Process outcome | 6/11 Pass | Unable to compute. No pre and post raw data—only percentage changes were given |
| White, 2014, Ireland [26] | Cross-sectional study | 338 | Hospital | Implementation of productive ward program | Improve work engagement | Process outcome | 7/11 Pass | Overall work engagement score1.06 (0.96–1.18) |
| Ulhassan, 2014, Sweden [27] | Pre-/post-test | 263 | Emergency department and two cardiology wards | Identify and eliminate areas of waste (DMAIC) | Improve teamwork | Process outcome | 8/11 Pass | Overall inclusion 1.02 (0.74–1.42) Overall trust 1.04 (0.79–1.38) Overall productivity 1.0 (1.0–1.0) |
| Collar, 2012, USA [28] | Pre-/post-test | 234 | Otolaryngology operating room | Identify and eliminate areas of waste (DMAIC) | Improve efficiency and workflow | Process outcome | 7/11 Pass | Unable to compute due to data not being provided. Turn-over time reduced from 38.4 min to 29 min |
| Blackmore, 2013, USA [29] | Retrospective cohort | 200 | Breast clinic | Identify and eliminate areas of waste | Improve timeliness of diagnosis and reduce surgical consults | Process outcome | 6/11 Pass | Reduced surgical consults 4.60 (1.82–11.62) |
| Simons P, 2014, Netherlands [30] | Pre-/post-test | 167 | Radiotherapy department | Implementation of a standard operating procedure | Improve compliance to patient safety tasks | Process outcome | 8/11 Pass | Overall compliance 0.96 (0.58–1.58) |
| Mazzocato, 2012, Sweden [31] | Case study | 156 | Accident and Emergency department | Identify and eliminate areas of waste, system restructuring | Increase number of patients seen and discharged within four hours | Process outcome | 10/13 Pass | Discharged within four hours 1.07 (0.92–1.26) |
| Health and process outcome studies | ||||||||
| Vermeulen, 2014, Canada [32] | Pre-/post-test Only study with control group |
6 845 185 | Emergency department | Training and system redesign | Left without being seen, discharged within 48 h, readmitted within 72 h, died within 7 days of discharge | Process and health outcome | 8/11 Pass | In comparison to control group: Left without being seen 1.05 (0.77–1.43) Discharged within 48 h 1.19 (0.72–1.98) Readmitted within 72 h of discharge 1.0 (1.0–1.0) Died within 7 days of discharge 1.03 (0.84–1.26) |
| Yousri, 2011, UK [33] | Pre-/post-test | 608 | Hospital | Identify and eliminate areas of waste | Overall mortality, 30 day mortality, door to theatre time, admission to a trauma ward | Health and process outcome | 6/11 Pass | 30 day mortality rate 1.71 (0.70–4.17) Door to theatre time within 24 h 1.17 (0.86–1.60) Admission to trauma bed 1.03 (0.90–1.20) |
| Ford, 2012, USA [34] | Pre-/post-test | 219 | Emergency department | Value stream analysis (VSM) | Reduce time dependant stroke care and stroke mimic | Process outcome and health outcome | 7/11 Pass | Percent of patients with DNT < 60 min 1.50 (1.21–1.86) Stroke mimic 0.64 (0.26–1.58) |
| Articles that failed methodology review | ||||||||
| First author's last name, year of publication, country where study was done | Study design | Number of participants | Location of intervention (ex. Emergency department) | Intervention | Intervention goal | Type of outcome | Quality scores | Major methodological drawbacks |
| Health outcome studies | ||||||||
| Ulhassan, 2013, Sweden [35] | Pre-/post-test | 4399 | Cardiology department | Changes to work structure and process | Improve patient care | Health outcome | 4/11 Fail |
|
| Wang, 2014, China [36] | Pre-/post-test | 622 | Nephrology department | Training, treatment of high risk patients, specialized outpatient clinic | Incidence of peritonitis | Health outcome | 4/11 Fail |
|
| Process outcome studies | ||||||||
| Wong, 2012, USA [37] | Pre-/post-test | 234 616 | Cytology laboratory | New imaging system, workflow redesign | Turnaround time, productivity and screening quality | Process outcome | 4/11 Fail |
|
| Lodge, 2008, UK [38] | Post-test | 9297 | Division of diagnostics and clinical support | Intranet based waiting list for radiology services | Reduce radiology wait times | Process outcome | 3/11 Fail |
|
| Willoughby, 2010, Canada [39] | Pre-/post-test | 1728 | Emergency department | Visual reminders, standard process worksheets (PDCA) | Improve wait times | Process outcome | 1/11 Fail |
|
| Piggott, 2011, Canada [40] | Pre-/post-test | 1666 | Emergency department | Identify and eliminate areas of waste (VSM) | Time to ECG, time to see MD, time to aspirin administration | Process outcome | 3/11 Fail |
|
| Mazzocato, 2014, Sweden [41] | Pre-/post-test | 1046 | Emergency department | Identify and eliminate areas of waste (VSM) | To reduce time to see MD, to increase number of patients leaving within 4 h, reduce number present at 4pm shift | Process outcome | 5/11 Fail |
|
| Richardson, 2014, USA [42] | Pre-/post-test | 565 | Emergency department | Educational training | Decrease wasted nursing time | Process outcome | 3/11 Fail |
|
| Wojtys, 2009, USA [43] | Pre-/post-test | 454 | Sport medicine practice | Identify and eliminate areas of waste (VSM) | Improve patient scheduling | Process outcome | 1/11 Fail |
|
| Niemeijer, 2012, Netherlands [44] | Pre-/post-test | 445 | Traumatology department | Identify and eliminate areas of waste (DMAIC) | Reduce length of stay and cost | Process outcome | 1/11 Fail |
|
| Hakim, 2014, USA [45] | Pre-/post-test | 361 | Medical and surgical units | Identify and eliminate areas of waste (PDCA) | Improve admission medication reconciliation | Process outcome | 3/11 Fail |
|
| van Lent, 2009, Netherlands [46] | Pre-/post-test | 255 | Chemotherapy day unit | Identify and eliminate areas of waste (PDCA) | Data efficiency, patient satisfaction and staff satisfaction | Process outcome | 4/11 Fail |
|
| Bhat, 2014, India [47] | Case study | 224 | Outpatient health information department | Identify and eliminate areas of waste (DMAIC) | Reduce registration time | Process outcome | 2/11 Fail |
|
| Al-Araidah, 2010, Jordan [48] | Case study | 217 | Inpatient pharmacy | Identify and eliminate areas of waste (DMAIC) | Lead time reduction | Process outcome | 4/11 Fail |
|
| Hydes, 2012, UK [49] | Pre-/post-test | 178 | Hospital | Value stream analysis (VSM) | Improve efficiency and patient satisfaction | Process outcome | 2/11 Fail |
|
| Smith, 2011, USA [50] | Pre-/post-test | 171 | Cystic fibrosis clinic | Identify and eliminate areas of waste (DMAIC) | Decrease non-value added time | Process outcome | 3/11 Fail |
|
| Kullar, 2010, UK [51] | Post-test | 141 | Cochlear implant unit | Value stream analysis (VSM) | Wait time for cochlear implantation | Process outcome | 1/11 Fail |
|
| Siddique, 2012, UK [52] | Post-test | 80 (or 129) | General surgery department | One stop cholecystectomy clinic | Waiting list time, number of hospital visits and pre op admissions | Process outcome | 4/11 Fail |
|
| Lunardini, 2014, USA [53] | Case series | 38 | Operating room | Value stream analysis (VSM) | To optimize instrument utilization | Process outcome | 4/13 Fail |
|
| Yeh, 2011, Taiwan [54] | Pre-/post-test | 36 | Private hospital | Identify and eliminate areas of waste (DMAIC) | Improve door to balloon time (AMI revascularization), length of stay | Process outcome | 3/11 Fail |
|
| Luther, 2014, UK [55] | Pre-/post-test | 20 | Medical admission unit ward | Identify and eliminate areas of waste (PDCA) | Improve patient handover | Process outcome | 3/11 Fail |
|
| Shah, 2013, USA [56] | Pre-/post-test | 17 | Breast imaging centre | Identify and eliminate areas of waste (VSM) | Improve workflow | Process outcome | 2/11 Fail |
|
| Gijo, 2013, India [57] | Case study | Not stated | Pathology department | Identify and eliminate areas of waste (DMAIC) | Reduce wait time | Process outcome | 2/11 Fail |
|
| Belter, 2012, USA [58] | Pre-/post-test | Not stated | Oncology outpatient | Identify and eliminate areas of waste (DMAIC) | Decrease patient wait times and improve communication | Process outcome | 2/11 Fail |
|
| Snyder, 2009, USA [59] | Pre-/post-test | Not stated | Rural healthcare organization | Training | Decrease supply time, patient wait time, documentation in EMR within 30 minutes | Process outcome | 0/11 Fail |
|
| Silva, 2012, USA [60] | Pre-/post-test | Not stated | Clinical engineering department | Identify and eliminate areas of waste (DMAIC) | Improve medical equipment inventory control | Process outcome | 0/11 Fail |
|
DMAIC: define, measure, analyse, improve, control; PDCA: plan do check act; TPS: Toyota production system; VSM: value stream mapping; DNT: door to needle time.
Rate ratio <1 is intervention resulted in negative outcome; rate ratio >1 is intervention resulted in positive outcome.
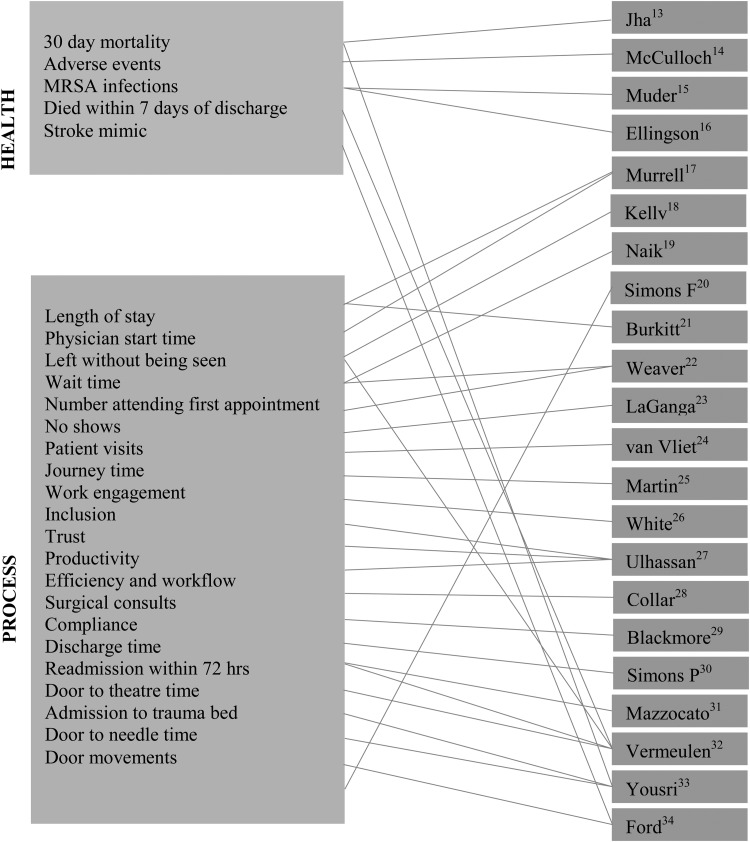
Among the 22 studies accepted, none used high quality experimental study designs (i.e. randomized controlled trials) or even lesser quality quasi-experimental study designs (i.e. prospective longitudinal cohorts). All study designs were of relatively low quality with almost all using before and after study designs without control groups. In fact, only one accepted study had a control group [26]. Among accepted studies, 4 were exclusively concerned with health outcomes, 3 included both health and process outcomes and 15 included process outcomes only (Fig. 2).
Figure 2.
Diagrammatic mapping of included studies to specific outcomes.
Health outcomes
Among the four accepted studies with health outcomes, only one found a statistically significant impact of Lean. They found a reduced relative rate of MRSA infections (RR = 2.47, 95% CI 1.87–3.27), although absolute reductions were very small [15]. The largest study by far included six million patients. This study found no impact of Lean on 30-day mortality rate post-hospital discharge (RR = 0.08, 95% CI −0.30 to 0.46) [13]. The other two studies under this category found no statistically significant impact on adverse events (RR = 0.91, 95% CI 0.72–1.16) or on MRSA incidence (RR = 0.99, 95% CI 0.98–1.01) [14,16] (Table 1).
Process outcomes
Among the 15 accepted studies that examined a vast array of process outcomes (including wait times, patient flow and workplace engagement, inclusion and productivity), only 2 found a statistically significant positive effect of Lean. The benefits included reduced patient visits (RR = 1.84, 95% CI 1.33–2.56) and reduced surgical consults (RR = 4.60, 95% CI 1.82–11.62) [24,29]. In five studies, rate ratios and confidence intervals were not computed because the authors did not include raw data (only summary data). None of the accepted studies reviewed actual financial costs (Table 1).
Health and process outcomes
Of the three articles that evaluated both health and process outcomes, only one article reported a positive effect of Lean in that it improved time dependent stroke care (RR = 1.50, 95% CI 1.21–1.86) [34]. Conversely, in a large study of over 6.8 million patients, Lean had no statistically significant impact on patients leaving without being seen (RR = 1.05, 95% CI 0.77–1.43), patients discharged within 48 h of presentation (RR = 1.19, 95% CI 0.72–1.98) or number of patients readmitted to the hospital within 72-h of discharge (RR = 1.00, 95% CI 1.00–1.00) [32] (Table 1).
The largest Lean healthcare transformation in the world – results from Saskatchewan
The HQC of Saskatchewan surveyed tens of thousands of patients discharged from hospitals pre- and post-Lean [11]. In this systematic review, the most relevant 30 outcomes are reported under the umbrella of 5 broad groupings, which include: self-reported health, hospital experience, communication, respect and patient management. Among the 30 outcomes considered, Lean had no statistically significant impact in 27 of them (Table 2). For example, 30 574 patients were surveyed on self-reported health with no observed impact from Lean (RR = 1.00, 95% CI 0.98–1.04). When measuring direct outcomes for 90 000 patients on their experience with doctors (RR = 1.01, 95% CI 1.00–1.02) and nurses (RR = 1.00, 95% CI 0.99–1.01), no effect of Lean was observed. Only three outcomes showed statistically significant positive outcomes of Lean including: staff washing or disinfecting their hands (RR = 1.179 07, 95% CI 1.05–1.10), staff checking ID bands (RR = 1.08, 95% CI 1.06–1.10) and patients given safety brochures (RR = 1.56, 95% CI 1.49–1.63). The results are found in Table 2.
Table 2.
Data collected by the Saskatchewan health quality council
| Saskatchewan health quality council—pre- and post-Lean data | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| SHQC variables | Pre-Lean (December 2009–January 2012) |
Post-Lean (February 2012–March 2014) |
Total sample size (n) | Rate ratio | 95% CI | ||||
| Sample size (N) | % | LCL–UCL | Sample size (n) | % | LCL–UCL | ||||
| Reported health | |||||||||
| High self-reported health | 16 637 | 34.52 | 26.78–37.96 | 13 937 | 34.75 | 26.16–38.58 | 30 574 | 1.00 | 0.98–1.04 |
| Hospital experience | |||||||||
| Patient experience—quality of care transitions | 42 435 | 31.48 | 28.45–35.43 | 36 000 | 32.80 | 28.09–35.78 | 78 435 | 1.02 | 1.00–1.03 |
| Percentage of patients rating their hospital as 9 or 10/10 | 16 526 | 51.95 | 47.42–59.38 | 13 803 | 52.93 | 46.76–60.05 | 30 329 | 1.01 | 0.99–1.04 |
| Percentage of patients reporting they would definitely recommend the hospital to family and friends | 16 498 | 58.8 | 52.78–64.60 | 13 828 | 57.38 | 52.13–65.25 | 30 326 | 0.98 | 0.94–1.01 |
| Communication | |||||||||
| Patient experience—quality of communication with nurses | 50 162 | 68.30 | 64.26–70.71 | 41 965 | 69.31 | 63.91–71.07 | 92 127 | 1.01 | 1.00–1.02 |
| Patient experience—Quality of communication with doctors | 49 826 | 73.78 | 70.36–76.47 | 41 593 | 73.93 | 70.01–76.81 | 91 419 | 1.00 | 0.99–1.01 |
| Percentage of patients reporting they always received good communication about medicines | 18 852 | 50.19 | 43.55–54.78 | 16 504 | 49.94 | 43.08–55.26 | 35 356 | 0.99 | 0.97–1.02 |
| Percentage of patients responding nurses always listened to them carefully | 16 750 | 63.60 | 56.93–68.46 | 14 045 | 64.76 | 56.30–69.08 | 30 795 | 1.02 | 1.00–1.04 |
| Percentage of patients responding nurses always explained things clearly | 16 699 | 63.95 | 57.53–69.03 | 13 937 | 64.90 | 56.88–69.68 | 30 636 | 1.01 | 1.00–1.03 |
| Percentage of patients responding doctors always explained things clearly | 16 637 | 67.07 | 61.02–72.30 | 13 885 | 66.98 | 60.39–72.93 | 30 522 | 1.00 | 0.99–1.01 |
| Percentage of patients responding doctors always listened to them carefully | 16 562 | 70.92 | 65.07–75.99 | 13 830 | 71.52 | 64.46–76.61 | 30 392 | 1.00 | 0.99–1.02 |
| Treatment plan explained clearly | 15 753 | 77.79 | 73.25–83.37 | 13 201 | 78.58 | 72.69–83.93 | 28 954 | 1.01 | 1.00–1.01 |
| Family encouraged to participate in care plan | 13 955 | 80.60 | 75.47–85.78 | 11 809 | 81.31 | 74.92–86.33 | 25 764 | 1.00 | 0.99–1.02 |
| Percentage of patients reporting staff took their preferences into account discussing health needs | 12 886 | 24.88 | 19.16–30.93 | 10 980 | 26.28 | 18.56–31.52 | 23 866 | 1.05 | 1.00–1.10 |
| Percentage of patients reporting staff always told them what their new medicine was for | 9468 | 64.17 | 54.65–70.10 | 8292 | 63.29 | 54.00–70.67 | 17 760 | 0.99 | 0.97–1.01 |
| Percentage of patients reporting staff always talked to them about medication side effects | 9413 | 36.09 | 28.32–43.58 | 8245 | 36.54 | 27.67–44.22 | 17 658 | 1.01 | 0.97–1.05 |
| Respect | |||||||||
| Percentage of patients responding nurses always treated them with courtesy and respect | 16 800 | 77.28 | 71.41–81.50 | 14 056 | 78.26 | 70.85–81.87 | 30 856 | 1.00 | 0.99–1.01 |
| Percentage of patients responding doctor always treated them with courtesy and respect | 16 661 | 83.27 | 78.51–87.48 | 13 906 | 83.25 | 78.00–87.99 | 30 567 | 1.00 | 0.99–1.01 |
| Staff respect culture, beliefs, values | 15 753 | 92.23 | 89.18–95.68 | 13 221 | 92.43 | 88.83–96.03 | 28 974 | 1.00 | 0.99–1.01 |
| Doctors treated patients as a partner in care | 15 736 | 82.47 | 78.04–87.34 | 13 159 | 83.3 | 77.52–87.85 | 28 895 | 1.01 | 1.00–1.02 |
| Staff treated patients as a partner in care | 15 552 | 78.85 | 73.68–83.80 | 13 054 | 80.07 | 73.13–84.34 | 28 606 | 1.02 | 1.00–1.03 |
| Doctors respect culture, beliefs, values | 15 493 | 93.81 | 87.18–91.45 | 12 948 | 94.39 | 91.13–97.49 | 28 441 | 1.00 | 1.00–1.00 |
| Patient care management | |||||||||
| Percentage of patients responding their pain was always well managed | 22 183 | 63.90 | 57.35–67.38 | 19 174 | 61.55 | 56.90–67.82 | 41 357 | 0.96 | 0.95–0.98 |
| Percentage of patients reporting they always received help they needed when they wanted it | 17 599 | 60.50 | 53.98–65.39 | 15 737 | 59.12 | 53.57–65.60 | 33 336 | 0.98 | 0.96–1.01 |
| Unnecessarily long wait time for room | 16 607 | 79.45 | 74.62–84.29 | 13 889 | 79.18 | 74.08–84.83 | 30 496 | 1.00 | 0.99–1.02 |
| Staff washed or disinfected their hands | 16 529 | 43.49 | 36.41–48.27 | 13 839 | 46.71 | 35.76–48.91 | 30 368 | 1.07 | 1.05–1.10 |
| Discharge organization | 16 432 | 27.71 | 23.05–33.91 | 13 753 | 27.88 | 22.45–34.50 | 30 185 | 1.00 | 0.97–1.10 |
| Suffered medical error | 15 976 | 3.70 | 1.26–5.75 | 13 352 | 3.77 | 1.10–6.00 | 29 328 | 0.98 | 0.87–1.10 |
| Staff checked ID band before care | 14 085 | 60.52 | 50.31–63.18 | 12 224 | 65.42 | 49.73–63.76 | 26 309 | 1.08 | 1.06–1.10 |
| Given patient safety brochure | 10 854 | 30.64 | 18.58–41.42 | 8980 | 36.63 | 17.85–42.16 | 19 834 | 1.56 | 1.49–1.63 |
Pre- and post-Lean periods were identical (26 months each).
In 2014, the SUN randomly surveyed 1500 nurses on their Lean experience [12]. Among nurses who had direct experience with Lean (729–173 nurses—depending on the variable), 15 outcomes were reviewed. All 15 outcomes reported a statistically significant negative effect of Lean on nurse engagement, usefulness, patient care, time for patient care, workplace issues, availability of supplies, workload, stress and patient safety (Table 3). For example, the following outcomes were reduced, nurse engagement (RR = 0.50, 95% CI 0.40–0.65), quality of patient care (RR = 0.23, 95% CI 0.17–0.31) and patient safety (RR = 0.44, 95% CI 0.37–0.53) while the nurses workload and stress levels increased (RR = 0.29, 95% CI 0.24–0.35) (Table 3).
Table 3.
Data collected by the Saskatchewan Union of Nurses
| Saskatchewan Union of Nurses (SUN)—Lean Healthcare 2014 Survey | |||||
|---|---|---|---|---|---|
| Strongly disagree (%) | Strongly agree (%) | n | Rate ratio | 95% CI | |
| Experience with Leana | |||||
| Lean activities engage frontline registered nurses | 23.00 | 10.00 | 729 | 0.50 | 0.40–0.65 |
| Ideas put forward by registered nurses are taken seriously | 30.50 | 6.10 | 729 | 0.27 | 0.20–0.37 |
| Registered nurse input is meaningfully incorporated into the Lean process | 35.70 | 6.00 | 729 | 0.25 | 0.18–0.33 |
| Registered nurses feel safe and supported in voicing criticisms and concerns about Lean initiatives | 41.00 | 5.60 | 729 | 0.21 | 0.16–0.30 |
| Lean is a useful support for the nursing process | 38.30 | 4.00 | 729 | 0.17 | 0.11–0.24 |
| Lean leads to improvements in direct patient care | 38.20 | 5.80 | 729 | 0.23 | 0.17–0.31 |
| Lean has resulted in policies and procedures that improve the workplace | 29.10 | 5.20 | 729 | 0.23 | 0.17–0.33 |
| Declined |
Improved |
n |
Rate ratio |
95% CI |
|
| Did Lean decline, stay the same or improveb | |||||
| The quality of supplies | 42.20 | 9.90 | 1173 | 0.37 | 0.31–0.44 |
| The availability of supplies | 50.50 | 17.90 | 1173 | 0.58 | 0.52–0.66 |
| The time available for direct patient care | 41.40 | 10.40 | 1173 | 0.38 | 0.32–0.47 |
| Workload and stress | 49.50 | 7.90 | 1173 | 0.29 | 0.24–0.35 |
| Patient safety | 31.00 | 10.60 | 1173 | 0.44 | 0.37–0.53 |
| The ability to meet professional standards in the nursing process | 34.50 | 9.30 | 1173 | 0.37 | 0.31–0.45 |
| Time and opportunity for clinical education and training | 35.00 | 7.50 | 1173 | 0.33 | 0.27–0.41 |
| Staff morale and engagement | 58.20 | 7.80 | 1173 | 0.30 | 0.25–0.36 |
Note: Rate ratio <1 = negative impact of intervention; rate ratio >1 = positive impact of intervention.
an, sample size—individuals who say they have been involved personally in a workplace Lean initiative. Likert scale was used (where 1 means ‘strongly disagree’ and 5 means ‘strongly agree’).
bn, sample size—individuals who say their workplace has gone through a Lean improvement process (denominator equals 1500).
Discussion
The purpose of this systematic literature review was to independently assess the effect of Lean thinking or Lean interventions on worker and patient satisfaction, health and process outcomes and financial costs.
For worker satisfaction, the largest study was carried out by the SUN. With every outcome reviewed, Lean had an overall negative effect on worker satisfaction [12]. Among other accepted studies from the electronic search of peer reviewed articles, Lean was shown to have no impact on workplace engagement, inclusion and productivity [26,27]. These outcomes are surprising in that worker engagement and input are essential for Lean principles to succeed [2].
For patient satisfaction, the largest dataset available has been collected by the Saskatchewan HQC [11]. When measuring direct outcomes for patient experience with doctors and nurses, no statistically significant positive or negative effect of Lean was observed. In the 22 studies accepted from the electronic search of peer reviewed articles, none directly evaluated patient satisfaction. That is also surprising because Lean reportedly begins with identifying and ‘removing waste’ in order to ‘add value’ to the customer or patient [2]. That said, it is unclear if other variables, like reduced number of medical consultations were used as proxy outcomes for patient satisfaction and what the patient's perception is (positive or negative) as a result of receiving less visits with their physician [24,29].
Among health outcomes like mortality, no study found a statistically significant impact of Lean. As mentioned previously, the largest study included six million patients and found no impact of Lean on 30-day mortality rate post-hospital discharge [13]. This is perhaps not surprising as Lean potentially only influences healthcare delivery. It obviously has no impact on complex health outcomes like patient adherence to care, let alone the behavioural or social determinants of health [1].
With regard to safety and errors, our systematic review shows that one study found no impact on adverse events while two studies had conflicting results on the impact of Lean on MRSA incidence [14–16]. The suggested impact of Lean on variables like adverse events is interesting because hospitals everywhere have successfully implemented various safety interventions that have proved effective but are not directly related with Lean. For example, the Agency for Healthcare Research and Quality estimates that 1.3 million fewer patients were harmed in American hospitals from 2010 to 2013. These outcomes were mostly due to common sense efforts to reduce surgical site infections, adverse drug events and other preventable incidents. As such, it is unclear what, if any, was the independent effect of Lean in comparison to a multitude of other diverse initiatives to promote safety and reduce errors in healthcare [61].
Although reduced financial cost is a reported benefit of Lean, it is worthy to note that we were unable to identify a single study that had actual quantifiable data to that effect. The province of Saskatchewan appears to be the only jurisdiction with actual financial cost information. External consultant fees were originally estimated to be $40.5 million but were reduced to $35 million when the Lean contract was terminated early [62]. Additionally, $17 million per year was required for internal kaizen promotion offices or $51 million total over the first 3 years. In return, official estimates of cost savings from the Saskatchewan health regions totalled $56934.26 [63]. If the numbers reported are accurate and true, it will mean that $1511 was spent on Lean for every one dollar saved by the province.
Strengths and limitations
The key strengths of our study are that it was a systematic review of Lean interventions in healthcare, it used a quality control checklist, and included a separate examination of both peer-reviewed articles and grey literature. There are also several limitations to our study. First, there are many and quite differing definitions of Lean in healthcare. This study did not attempt to strictly define what Lean is but rather relied on the definitions used by the authors of the articles included in our systematic review. Second, the outcomes were too diverse to permit a meta-analysis. Third, the study designs under review did not incorporate the use of control groups and therefore, it is unclear if the results are actually valid or what the results would be in comparison with a control group. Finally, the pre Lean HQC data for the province of Saskatchewan includes three small pilot projects in three health regions. However, month-to-month comparisons pre- and post-Lean found no statistically significant difference from the small pilot projects.
Comparison of findings
The results of our systematic review on Lean thinking and Lean interventions in healthcare provide additional insight and support the findings of other recent systematic reviews [5,64]. For example, Vest et al. [5] concluded that Lean interventions mainly focused on process outcomes in healthcare. Similarly, a Lean review completed by Mason et al. [64] found that the studies demonstrated improved process outcomes.
However, both Vest et al. [5] and Mason et al. [64] acknowledged that when critically examined, only a few articles met the inclusion criteria for their respective reviews. While Lean was found to be successful in some process outcomes, there were several and serious concerns with the reported study findings. Specifically, they noted that the articles reviewed were fraught with systematic bias, imprecision and serious methodological limitations, which undermined the validity of the results and made measuring and interpreting the true and independent effect of Lean on process and healthcare outcomes unclear and difficult.
Conclusion
The findings of our systematic review suggest that Lean interventions have: (i) no statistically significant association with patient satisfaction and health outcomes, (ii) a negative association with financial costs and worker satisfaction and (iii) potential yet inconsistent benefits on process outcomes like patient flow (reduced patient visits, reduced surgical consults, improved time dependent care) and safety (washing hands, staff checking ID bands and giving patients safety brochures).
More rigorous, higher quality and better conducted scientific research is required to definitively ascertain the impact and effectiveness of Lean in healthcare settings.
While some may strongly believe that Lean interventions lead to quality improvements in healthcare, the evidence to date simply does not support this claim. It is far more likely that Lean is but one of many strategies that might or might not have an impact on healthcare delivery.
The reality is that there are a multitude of internal and external variables that impact complex healthcare and process outcomes and that the independent effect of a specific intervention such as Lean is potentially minimal. For now, the question remains whether continuing to heavily invest in Lean is bringing us closer to or taking us further away from a much needed, viable, long-term solution to an increasingly problematic and unsustainable healthcare delivery system.
Authors’ contributions
J.M. and M.L. contributed to the original conception and design of the study. C.N. and M.L. were responsible for the acquisition of data. M.L. was in charge of the data analysis. J.M., M.L. and C.N. contributed to the interpretation of the data and the drafting of and critical revisions to the manuscript. All authors read and approved the final manuscript.
Funding
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Conflict of interest statement
None declared.
References
- 1.Lemstra M. Saskatchewan Health. Regina: Benchmark Publishing, 2012. [Google Scholar]
- 2.Institute for Healthcare Improvement. Going Lean in Healthcare. IHI Innovation Series White Paper Cambridge: Institute for Healthcare Improvement, 2005. www.IHI.org (26 January 2015, date last accessed). [Google Scholar]
- 3.Lean Enterprise Institute. Principles of Lean. Lean Enterprise Institute, 2015. www.lean.org (28 January 2015, date last accessed). [Google Scholar]
- 4.Joosten T, Bongers I, Janssen R. Application of Lean thinking to health care: issues and observations. Int J Qual Health Care 2009;21:341–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Vest JR, Gamm LD. A critical review of the research literature on Six Sigma, Lean and StuderGroup's Hardwiring Excellence in the United States: the need to demonstrate and communicate the effectiveness of transformation strategies in healthcare. Implementation Sci 2009;4:35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Saskatoon Star Phoenix. Lean Machine Saskatoon, 2014. www.thestarphoenix.com (26 January 2015, date last accessed). [Google Scholar]
- 7.Health Quality Council of Saskatchewan. Continuous Improvement: Lean. Saskatoon: Health Quality Council, 2015. www.hqc.sk.ca (26 January 2015, date last accessed). [Google Scholar]
- 8.Katz-Navon T, Naveh E, Stern Z. The moderate success of quality of care improvement efforts: three observations on the situation. Int J Qual Health Care 2007;19:4–7. [DOI] [PubMed] [Google Scholar]
- 9.Greenhalgh T, Robert G, Bate P, et al. Diffusion of Innovations in Health Service Organizations: A Systematic Literature Review. Malden, MA: Blackwell Publishing Ltd, 2005. [Google Scholar]
- 10.Saskatchewan Ministry of Health. Contract Agreement: Province of Saskatchewan & John Black & Associates LLC http://www.health.gov.sk.ca/lean-contract (16 February 2015, date last accessed).
- 11.Health Quality Council of Saskatchewan. Quality Insight: Measuring, Learning, Improving. Saskatoon: Health Quality Council, 2015. (accessed 26 January 2015) www.hqc.sk.ca. [Google Scholar]
- 12.Saskatchewan Union of Nurses. Lean Healthcare 2014 Member Survey. Regina: Praxis Analytics, 2014. [Google Scholar]
- 13.Jha AK, Joynt KE, Orav EJ, et al. The Long-term effect of premier pay for performance on patient outcomes. New Engl J Med 2012;366:1606–15. [DOI] [PubMed] [Google Scholar]
- 14.McCulloch P, Kreckler S, New S, et al. Effect of a ‘Lean’ intervention to improve safety processes and outcomes on a surgical emergency unit. BMJ (Online) 2010;341:1043–6. [DOI] [PubMed] [Google Scholar]
- 15.Muder RR, Cunningham C, McCray E, et al. Implementation of an industrial systems-engineering approach to reduce the incidence of methicillin-resistant Staphylococcus aureus infection. Infect Control Hosp Epidemiol 2008;29:702–8. [DOI] [PubMed] [Google Scholar]
- 16.Ellingson K, Muder RR, Jain R, et al. Sustained reduction in the clinical incidence of methicillin-resistant Staphylococcus aureus colonization or infection associated with a multifaceted infection control intervention. Infect Control Hosp Epidemiol 2011;32:1–8. [DOI] [PubMed] [Google Scholar]
- 17.Murrell KL, Offerman SR, Kauffman MB. Applying Lean: implementation of a rapid triage and treatment system. West J Emerg Med 2011;12:184–91. [PMC free article] [PubMed] [Google Scholar]
- 18.Kelly A, Bryant M, Cox L, et al. Improving emergency department efficiency by patient streaming to outcomes-based teams. Australian Health Rev 2007;31:16–21. [DOI] [PubMed] [Google Scholar]
- 19.Naik T, Duroseau Y, Zehtabchi S, et al. A structured approach to transforming a large Public Hospital Emergency Department via Lean methodologies. J Healthcare Qual: Promoting Excellence Healthcare 2012;34:86–97. [DOI] [PubMed] [Google Scholar]
- 20.Simons F, Aij K, Widdershoven G, et al. Patient safety in the operating theatre: how A3 thinking can help reduce door movement. Int J Qual Health Care. 2014;26:366–71. [DOI] [PubMed] [Google Scholar]
- 21.Burkitt KH, Mor MK, Jain R, et al. Toyota production system quality improvement initiative improves perioperative antibiotic therapy. Am J Manag Care 2009;15:633–42. [PubMed] [Google Scholar]
- 22.Weaver A, Greeno CG, Goughler DH, et al. The impact of system level factors on treatment timeliness: utilizing the Toyota production system to implement direct intake scheduling in a semi-rural community mental health clinic. J Behav Health Serv Res 2013;40:294–305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.LaGanga LR. Lean service operations: reflections and new directions for capacity expansion in outpatient clinics. J Oper Manage 2011;29:422–33. [Google Scholar]
- 24.van Vliet EJ, Sermeus W, van Gaalen CM, et al. Efficacy and efficiency of a Lean cataract pathway: a comparative study. Qual Saf Health Care 2010;19:e13. [DOI] [PubMed] [Google Scholar]
- 25.Martin AJ, Hogg P, Mackay S. A mixed model study evaluating Lean in the transformation of an Orthopaedic Radiology service. Radiography 2013;19:2–6. [Google Scholar]
- 26.White M, Wells JS, Butterworth T. The impact of a large-scale quality improvement programme on work engagement: Preliminary results from a national cross-sectional-survey of the ‘Productive Ward’. Int J Nurs Stud 2014; doi:10.1016/j.ijnurstu.2014.05.002 [DOI] [PubMed] [Google Scholar]
- 27.Ulhassan WMP, Sandahl CP, Westerlund HP, et al. Antecedents and characteristics of Lean thinking implementation in a Swedish Hospital: a case study. Qual Manag Health Care 2013;22:48–61. [DOI] [PubMed] [Google Scholar]
- 28.Collar RM, Shuman AG, Feiner S, et al. Lean management in academic surgery. J Am College Surgeons 2012;214:928–36. [DOI] [PubMed] [Google Scholar]
- 29.Blackmore CC, Edwards JW, Searles C, et al. Nurse practitioner-staffed clinic at Virginia Mason improves care and lowers costs for women with benign breast conditions. Health Affairs 2013;32:20–6. [DOI] [PubMed] [Google Scholar]
- 30.Simons PAM, Houben R, Benders J, et al. Does compliance to patient safety tasks improve and sustain when radiotherapy treatment processes are standardized? Eur J Oncol Nurs 2014;18:459–65. [DOI] [PubMed] [Google Scholar]
- 31.Mazzocato P, Holden RJ, Brommels M, et al. How does Lean work in emergency care? A case study of a Lean-inspired intervention at the Astrid Lindgren Children's hospital, Stockholm, Sweden. BMC Health Serv Res 2012;12:28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Vermeulen MJ, Stukel TA, Guttmann A, et al. Evaluation of an Emergency Department Lean process improvement program to reduce length of stay. Ann Emerg Med 2014;64:427–38. [DOI] [PubMed] [Google Scholar]
- 33.Yousri TA, Khan Z, Chakrabarti D, et al. Lean thinking: can it improve the outcome of fracture neck of femur patients in a district general hospital? Injury 2011;42:1234–7. [DOI] [PubMed] [Google Scholar]
- 34.Ford AL, Williams JA, Spencer M, et al. Reducing door-to-needle times using Toyota's Lean manufacturing principles and value stream analysis. Stroke 2012;43:3395–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ulhassan WMP, Sandahl CP, Westerlund HP, et al. Antecedents and characteristics of Lean thinking implementation in a Swedish Hospital: a case study. Qual Manag Health Care 2013;22:48–61. [DOI] [PubMed] [Google Scholar]
- 36.Wang J, Zhang H, Liu J, et al. Implementation of a continuous quality improvement program reduces the occurrence of peritonitis in PD. Renal Failure 2014;36:1029–32. [DOI] [PubMed] [Google Scholar]
- 37.Wong R, Levi AW, Harigopal M, et al. The positive impact of simultaneous implementation of the BD focal point GS imaging system and Lean principles on the operation of gynecologic cytology. Arch Pathol Lab Med 2012;136:183–9. [DOI] [PubMed] [Google Scholar]
- 38.Lodge A, Bamford D. New development: using Lean techniques to reduce radiology waiting times. Public Money Manage 2008;28:49–52. [Google Scholar]
- 39.Willoughby KA, Chan BTB, Strenger M. Achieving wait time reduction in the emergency department. Leadersh Health Serv 2010;23:304–19. [Google Scholar]
- 40.Piggott Z, Weldon E, Strome T, et al. Application of Lean principles to improve early cardiac care in the emergency department. Can J Emerg Med 2011;13:325–32. [DOI] [PubMed] [Google Scholar]
- 41.Mazzocato P, Thor J, Bäckman U, et al. Complexity complicates Lean: lessons from seven emergency services. J Health Organ Manag 2014;28:266–88. [DOI] [PubMed] [Google Scholar]
- 42.Richardson D, Rupp V, Long K, et al. Using Lean methodology to decrease wasted RN time in seeking supplies in emergency departments. J Nurs Adm 2014;44:606–11. http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=ovfto&NEWS=N&AN=00005110-201411000-00010. [DOI] [PubMed] [Google Scholar]
- 43.Wojtys EM, Schley L, Overgaard KA, et al. Applying Lean techniques to improve the patient scheduling process. J Healthcare Qual: Promoting Excellence Healthcare 2009;31:10–6. [DOI] [PubMed] [Google Scholar]
- 44.Niemeijer GCPM, Trip AP, de Jong LJM, et al. Impact of 5 years of Lean six sigma in a University Medical Center. Qual Manag Health Care 2012;21:262–8. [DOI] [PubMed] [Google Scholar]
- 45.Hakim H. Not just for cars: Lean methodology. Nurs Manag 2014;45:39–43. [DOI] [PubMed] [Google Scholar]
- 46.van Lent WA, Goedbloed N, van Harten WH. Improving the efficiency of a chemotherapy day unit: applying a business approach to oncology. Eur J Cancer 2009;45:800–6. [DOI] [PubMed] [Google Scholar]
- 47.Bhat S, Gijo EV, Jnanesh NA. Application of Lean Six Sigma methodology in the registration process of a hospital. Int J Product Perform Manag 2014;63:613–43. [Google Scholar]
- 48.Al-Araidah O, Momani A, Khasawneh M, et al. Lead-time reduction utilizing Lean tools applied to healthcare: the inpatient pharmacy at a local hospital. J Healthcare Qual: Promoting Excellence Healthcare 2010;32:59–66. [DOI] [PubMed] [Google Scholar]
- 49.Hydes T, Hansi N, Trebble TM. Lean thinking transformation of the unsedated upper gastrointestinal endoscopy pathway improves efficiency and is associated with high levels of patient satisfaction. BMJ Qual Safety 2012;21:63–9. [DOI] [PubMed] [Google Scholar]
- 50.Smith C, Wood S, Beauvais B. Thinking Lean: implementing DMAIC methods to improve efficiency within a cystic fibrosis clinic. J Healthcare Quality 2011;33:37–46. [DOI] [PubMed] [Google Scholar]
- 51.Kullar P, Harris F, Lloyd SK, et al. The use of Lean Thinking techniques in implementing the Department of Health, UK, 18-week waiting time directive for cochlear implantation. Cochlear Implants Int: Interdisciplinary J 2010;11:133–45. [DOI] [PubMed] [Google Scholar]
- 52.Siddique K, Elsayed S, Cheema R, et al. One-stop cholecystectomy clinic: an application of Lean thinking--can it improve the outcomes? J Perioper Pract 2012;22:360–5. http://onlinelibrary.wiley.com/o/cochrane/clcentral/articles/185/CN-00917185/frame.html. [DOI] [PubMed] [Google Scholar]
- 53.Lunardini D, Arington R, Canacari EG, et al. Lean principles to optimize instrument utilization for spine surgery in an academic medical center: an opportunity to standardize, cut costs, and build a culture of improvement. Spine 2014;39:1714–7. [DOI] [PubMed] [Google Scholar]
- 54.Yeh HL, Lin CS, Su CT, et al. Applying Lean six sigma to improve healthcare: an empirical study. Afr J Bus Manag 2011;5:12356–70. [Google Scholar]
- 55.Luther V, Hammersley D, Chekairi A. Improving patient handover between teams using a business improvement model: PDSA cycle. Br J Hosp Med 2014;75:44–7. [DOI] [PubMed] [Google Scholar]
- 56.Shah CJ, Sullivan JR, Gonyo MB, et al. Practice policy and quality initiatives: using Lean principles to improve screening mammography workflow. RadioGraphics 2013;33:1505–17. [DOI] [PubMed] [Google Scholar]
- 57.Gijo EV, Antony J, Hernandez J, et al. Reducing patient waiting time in a pathology department using the Six Sigma methodology. Leadersh Health Serv 2013;26:253–67. [Google Scholar]
- 58.Belter D, Halsey J, Severtson H, et al. Evaluation of outpatient oncology services using Lean methodology. Oncol Nurs Forum 2012;39:136–40. [DOI] [PubMed] [Google Scholar]
- 59.Snyder KD, McDermott M. A rural hospital takes on Lean. J Healthcare Qual 2009;31:23–8. [DOI] [PubMed] [Google Scholar]
- 60.Silva APS, Palermo JM, Gibertoni A, et al. Inventory quality control in clinical engineering: a Lean Six Sigma approach. 2012 Pan American Health Care Exchanges, PAHCE 2012 - Conference, Workshops, and Exhibits Cooperation / Linkages: An Independent Forum for Patient Aare and Technology Support; 2012. [Google Scholar]
- 61.Agency for Healthcare Research and Quality. 17% Percent Reduction in Hospital-Acquired Conditions. Rockville, MD: Agency for Healthcare Research and Quality, 2014. http://www.ahrq.gov/news/newsroom/speech/sp120114.html (4 February 2015, date last accessed). [Google Scholar]
- 62.Canadian Broadcast Corporation. Controversial Lean Company's Contract Ending Early. Regina: Canadian Broadcast Corporation, 2014. www.cbc.ca (4 February 2015, date last accessed). [Google Scholar]
- 63.Regina Leader Post. Mandryk: Wall must avoid another Lean mess Regina: Regina. Leader Post, 2015. www.leaderpost.com (4 February 2015, date last accessed). [Google Scholar]
- 64.Mason SE, Nicolay CR, Darzi A. The use of Lean and Six Sigma methodologies in surgery: a systematic review. Surgeon 2014;13:1–10. [DOI] [PubMed] [Google Scholar]