Abstract
Objective
Drawing on interviews with home care clients and their family caregivers, we sought to understand how these individuals conceptualize safety in the provision and receipt of home care, how they promote safety in the home space and how their safety concerns differ from those of home support workers.
Design
In-depth, semi-structured interviews were conducted with clients and family caregivers. The analysis included topic and analytical coding of participants' verbatim accounts.
Setting
Interviews were completed in British Columbia, Canada.
Participants
Totally 82 clients and 55 caregivers participated.
Results
Clients and family caregivers identified three types of safety concerns: physical, spatial and interpersonal. These concerns are largely multi-dimensional and intersectional. We present a conceptual model of client and caregiver safety concerns. We also examine the factors that intensify and mitigate safety concerns in the home.
Conclusions
In spite of safety concerns, clients and family caregivers overwhelmingly prefer to receive care in the home setting. Spatial and physical concerns are the most salient. The financial burden of creating a safe care space should not be the client's alone to bear. The conceptualization and promotion of safety in home care must recognize the roles, responsibilities and perspectives of all of the actors involved, including workers, clients and their caregivers.
Keywords: safety, home care services, aged, caregivers, qualitative research
Introduction
Older adults and their family members have identified the home as the preferred location in which to age in place, and for over one million Canadians, home support services facilitate this [1]. Healthcare service providers also recognize the potential cost benefits of in-home service provision, and many are pursuing ‘home first’ policies that promote care in the home over other settings, such as residential or long-term care [2]. The provision and receipt of care in the home, however, can pose safety hazards for those involved. To date, research on safety in home care has emphasized potential biomedical and environmental hazards, with a focus on adverse events [3–7], and safety implications for home care staff [8–11].
Safety in home care not only includes the care received by clients, but also the safe delivery of care, location of care and the psycho-social interactions between the client, formal home care providers and family caregivers [7, 12, 13]. As home care is provided within a client's home, decisions about care provision are often at the discretion of clients and their family caregivers [14]. This can create a challenging environment in which to provide and receive care [15, 16]. Canadian studies investigating the incidence of safety-related events in home care estimate that 5.5–13.2% of home care clients will experience at least one adverse event [5, 7, 17] due to inadequate safety. Falls, in particular, are identified as a primary safety issue for home care clients [3, 18] and workers [16]. Other client safety issues and adverse events include unintended weight loss, infections, drug events and emergency room visits [3, 4, 6].
As home-based care is provided in non-institutional settings, and involves multiple stakeholders, general definitions of patient safety are not sufficiently broad to encompass all aspects of safety in the delivery and receipt of care at home [13, 19]. Numerous studies have examined safety concerns in home care, but have insufficiently considered the perspectives of all of the individuals implicated in the delivery and receipt of this care. The safety lens of home care should expand beyond the client, to include their family caregivers, as well as home care providers; each of these actors plays an integral role in effecting and maintaining safety [7, 20–23]. This paper advances an expanded understanding of safety in home care, by considering the perspectives of clients and family caregivers.
Researchers have noted that home care clients and family caregivers tend to think of safety in terms of challenges, concerns or risk rather than ‘safety’ [23, 24]. Clients have stated that home care provides a sense of security and they view their home as a safe place [25, 26]. While a limited number of studies have examined the perceptions of home care clients regarding safety, even fewer have considered those of caregivers. Sears [17] noted that family members are likely to be instrumental in identifying safety risks. However, information related to safety concerns for the client was often unavailable or not voiced until the event occurred [18, 27]. This lack of knowledge and training left some family members in perilous positions, unsure of their abilities as caregivers [28].
Our prior research led to the development of a conceptual model of safety in home care from the perspective of home support workers (HSWs) [16]. Workers identified four types of safety concerns: physical, spatial, interpersonal and temporal. Drawing on this existing model that reflects HSWs conceptualizations of safety, we applied the model to an analysis of the verbatim accounts of clients and their family caregivers. We sought to better understand how clients and family caregivers conceptualize safety, and whether in ways similar to and/or distinct from those of HSWs.
Methods
This paper is based on data from a larger mixed-methods study [15, 16] aimed at understanding key issues in the delivery and receipt of home support services from the perspectives of HSWs, older adult clients and the family who are involved in their daily care (herein referred to as ‘family caregivers’). We collected both quantitative and qualitative data through in-depth, semi-structured interviews. The client interview guide included questions about demographics, the context for receipt of home support services, services received, interactions with workers, health conditions, difficulties with activities of daily living (ADLs) and adverse events (see Table 1). Family caregivers were also asked about work-caregiving balance, caregiver burnout and fatigue and their own health and support needs.
Table 1.
Sample interview questions
| Client interview questions: |
|
| Family caregiver interview questions: |
|
Setting and participants
Ethics approval was granted from the University of British Columbia and the regional health authority in whose jurisdiction our study was conducted. Data were collected from January 2007 to July 2008 in British Columbia, Canada. Eligible clients were older adults (65+ years), currently receiving home support services from one regional health authority, and able to provide informed consent. Eligible caregivers included family members or close, family-like friends, who provided support to an older adult in receipt of home support services. For more information about recruitment, please see [15]. In total, 82 clients and 55 caregivers participated.
Data collection
Face-to-face interviews were completed by trained interviewers, in English, in a private location of the participant's choosing, typically the home. When requested, clients and their family caregivers were interviewed together. Interviews ranged from 60 to 90 min were digitally recorded and professionally transcribed verbatim. Transcripts were blinded, stored with IDs and entered into NVivo 10 for analysis. Although participants were asked specifically about adverse events, conversations about safety were cited throughout the interviews (see Table 1). As such, transcripts were reviewed in their entirety for this analysis.
Participant characteristics
The average client participant is a woman over the age of 80; the average caregiver, a woman over the age of 65, typically the daughter or wife of an older adult receiving home support (see Table 2). The home support services most often received are bathing and dressing, highlighting the physical nature of the support that clients require.
Table 2.
Participant characteristics
| Clients (n= 82) | Caregivers (n= 55) |
|---|---|
| Age | |
| Average: 83 years | Average: 67 years |
| Range: 65–96 years | Range: 46–91 years |
| Gender | |
| Female: n= 55 (67%) | Female: n= 46 (84%) |
| Male: n= 27 (33%) | Male: n= 9 (16%) |
| Marital status | |
| Married: n= 24 (29%) | Married: n= 38 (69%) |
| Widowed: n= 43 (52%) | Widowed: n= 10 (18%) |
| Separated/divorced/never married: n= 15 (18%) | Separated/divorced: n= 7 (13%) |
| Number of years receiving home support | Number of years being responsible for care |
| >1 year: n= 20 (24%) | Average: 7 years |
| 1–5 years: n= 37 (45%) | Range: 3 months to 33 years |
| 5–10 years: n= 13 (16%) | |
| >10 years: n= 12 (15%) | |
| Living arrangement | Relationship to client |
| Alone: n= 49 (60%) | Spouse: n= 25 (46%) |
| With spouse: n= 24 (29%) | Child: n= 24 (44%) |
| With adult child: n= 9 (11%) | Other: n= 9 (11%) |
| Most common types of care received | Employment status |
| Bathing: n= 68 (83%) | Not employed/retired: n= 39 (71%) |
| Dressing: n= 44 (54%) | Employed: n= 16 (29%) |
| Meal preparation: n= 31 (38%) | |
Analytical strategies
We engaged in thematic coding of the transcripts, based on an a priori coding structure [29]. The first author and two research assistants engaged in line-by-line coding of the transcripts. Rigour was established through a combination of standard techniques for qualitative research, including team meetings, an audit trail, analytic memo writing and peer debriefing [30–32].
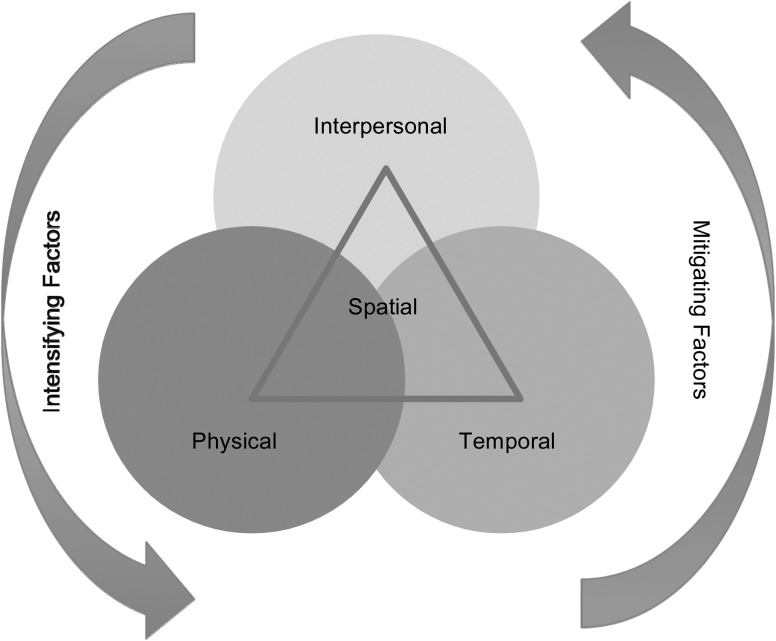
Our existing coding structure was based on a previous analysis of HSW safety concerns [16], in which four types of safety concerns were highlighted: physical, interpersonal, temporal and spatial. The initial analysis of HSWs' conceptualization of safety also highlighted factors that intensified or mitigated safety concerns (see Fig. 1). For HSWs, physical, interpersonal and temporal safety concerns existed separately but were also often co-existing and intersectional. The spatial intersects all of the safety concerns, highlighting the central role that space plays when care is provided in the private home of a client. This original conceptual model rooted in HSWs' perspectives on safety provided the high-level coding framework for the analysis of clients' and caregivers' transcripts. We developed several open codes to capture themes that were unique to this present analysis.
Figure 1.
Home support workers' safety concerns [16].
Results
Prior research with home care clients and family caregivers has emphasized identifying and cataloguing adverse events [4, 7, 33]. With our interviews, we sought to more fully explore the topic of safety with clients and caregivers, examining both adverse events and everyday experiences of safety.
Types of safety concerns
Clients and family caregivers discussed three types of safety concerns: physical, spatial and interpersonal (see Table 3 for definitions and examples). Consistent with the HSWs in our larger study, the safety concerns most commonly cited by clients and their family caregivers were physical (e.g. worries about trips and falls) and spatial (e.g. concerns about unsafe spaces, including the bathing and cooking areas).
Table 3.
Types of safety concerns
| Type of safety concern | Example from client | Example from family caregiver |
|---|---|---|
| Physical | ||
| Concerns of a physical/medical nature, including musculoskeletal injuries, trips, falls and communicable diseases, related to both the experience of, and the potential risk for, physical harm. | ‘I cannot stand alone for any length of time. I need to hold on to something secure like bars that have been installed into the wall. Then I can step safely into the shower knowing that the people are right beside me. I cannot sit on that little stool and manage the water control or get out of the shower by myself.’ – Reanna | ‘We're just worried that she's going to fall down in the shower … she's getting weaker and weaker’ – Kelly |
| Spatial | ||
| Concerns based on features of the home space including physical characteristics of the inside and outside area of a client's home; spatial layout of the home; geographic location (e.g. dangerous neighbourhoods) and the adequacy of the ‘set-up’ of the home in terms of equipment and supplies; presence of hazards or threats (e.g. client's pet). | ‘Cleaning around the toilet requires lots of bending down. A lot of stuff just doesn't get done. Our home isn't as clean as it was, which is probably less healthy, but that's how it is.’ – Meredith | ‘Now I have to do all the cooking. Well, when [Mom] lost her sight, then it wasn't safe to leave her in the kitchen because she turned the stove on and, you know, and forget. Either forget or she couldn't see it, you know.’ – Kim |
| Interpersonal | ||
| Concerns arising from interactions between clients and their family members and/or their home care workers, impacting the client psychologically, socially or emotionally. | ‘I like some [HSWs] better than others. Some are kinder than others …. One came in, said ‘I don't do this, I don't do that.’ She was arrogant.’ – Antonia | ‘But we've had some terrible people [HSWs]. Twice the wife ended up in the hospital ‘cause they let her fall, yeah. And others were very argumentative. All they wanted to do was argue all the time.’ – Harry |
Safety concerns: multi-dimensionality and intersectionality
Also consistent with the HSW analysis, the responses of clients and their family caregivers emphasized how safety concerns are often multi-dimensional and intersectional in nature. In particular, physical and interpersonal concerns were often interconnected with spatial concerns. This highlights the central role of the private home as the site of care [34], and a potential source of safety concerns.
Physical/spatial safety concerns
Home care clients and family caregivers commonly cited safety concerns that reside at the intersection of physical and spatial; that is, concerns that deal with the wellbeing of the physical body and the private home space.
For instance, clients and family caregivers cited the overall cleanliness and hygiene of the home as a potential safety concern. This is a combination of concerns about physical safety (cleanliness and health) and spatial safety concerns (the home environment being clean and safe). For many clients in our study, ‘care plans’ do not permit housekeeping services. Bonnie needs help with vacuuming, and describes herself as at risk without it: ‘how can I vacuum when I need the walker to get around? I'm going to fall again … .’ Equally frustrating is the fact of having someone working in the home who potentially could, but who is not permitted to assist in maintaining a clean home space.
Clients and family members identified the bathroom as the most ‘unsafe’ space in the home; family members, in particular those caring for individuals with suspected or diagnosed dementia, also identified the kitchen as a potentially dangerous location. For example, Bella is concerned for her mother's safety in the kitchen. She explained how the presence of home support assuages some safety concerns, ‘I can go to work. I don't have to worry that much. Of course I worry. This year [the] fire department came twice already to my house. Because she was boiling water in the kettle… so she put on the stove and the plastic melted and started a fire. And we have a sensor in the kitchen … I put [sensors] in the whole house.’
Interpersonal/spatial safety concerns
Another dominant theme regarding safety, in particular for clients, centred on privacy and security in the home. This reflects the intersection of interpersonal concerns (e.g. not trusting a worker) and spatial concerns (e.g. feeling as if strangers have access to the home). Helena, a client, described concerns about having a lockbox on her door to provide workers with access: ‘I said, “Are you trying to tell me that I am supposed to trust 250 or 300 homecare girls I've never seen before in my life? More than I would my family and my friends?”’ Flora, a client, felt the need to monitor some workers, ‘The majority of them [HSWs], I don't mind. But some of them are snooping. And I don't like that … I'm on their heels.’
Mitigating and intensifying factors
In addition to specifying safety concerns characteristic of home care, study participants identified factors that help mitigate and intensify their concerns (see Table 4). In several instances we see how one factor can be either intensifying or mitigating, depending on how it perceived. For example, the presence of workers can mitigate concerns, but when policies prevent them from addressing safety issues in the home (e.g. if a client's ‘care plan’ does not allow for vacuuming, cleaning for general hygiene), the workers presence can in fact exacerbate the perceived safety concern for clients. Similarly, home modifications can make the home feel safer, thereby lessening concerns; however, if cost is prohibitive or if modifications are not carefully implemented, they can potentially make the home less safe.
Table 4.
Mitigating and intensifying factors
| Factor | Description | Interview example |
|---|---|---|
| Mitigating | ||
| Workers provide peace of mind | While safety is a concern overall, workers provide ‘peace of mind.’ Workers provide an extra set of eyes, ears and hands in the home, often enhancing client safety through their presence and actions. | ‘They're here to assist me, to make sure that there's not a lot of bacteria, germs, that I'm not going to wear myself out … they're doing what they think is necessary to keep me in a relatively healthy environment. And I think they do a very good job of it.’ – Sheryl (Client) |
| Home modifications and equipment | Strategies and solutions that clients and family caregivers implement to make the home space safer, playing an active role in maintenance of safety in the home. Includes: grab rails, easy-to-grasp door handles, bathing chairs, hospital beds and equipment to facilitate lifts and transfers. | ‘I've done a lot over the years by myself, but it gets very tiring. And, you know, you get weary, yeah. And it was heavy lifting ‘cause [my husband] couldn't get out of the chair. We did finally go buy a chair, you know, the [kind that] lifts you up … It lifts the chair up so he can get out of the chair. But before that it was just a struggle. For both of us.’ – Martha (Family Caregiver) |
| Intensifying | ||
| Cost of home modifications and equipment | Costs of implementing safety solutions are prohibitive. While federal grants and non-profit organizations, such as the Red Cross, provide support, it often doesn't cover full cost of recommended/required modifications or equipment. | ‘This chair was more than $4000. The hospital bed, the mattress … I paid for everything. They can give me up to $3000 for the lift. It costs $19 000. Where am I going to come up with that money? He has a low pension, I never worked.’ – Eliana (Family caregiver) |
| Home modifications not well received | Home modifications may work for one partner in care (e.g. client, or worker) and may not work for another (e.g. family caregiver). Home modifications, while often essential, are not always well received by clients and/or family caregivers. | ‘The nurse came out and she said, “You have to raise your bed six inches.” Well, Nick is six feet tall and I'm five foot two. So putting John to bed at night presented kind of a problem for me… The bed's too high, yeah. We had a hell of a time the other night.’ – Lara (Family caregiver) |
| Poorly executed care/insufficient worker training | When workers do not provide exemplary care, clients frequently perceive limited training as source of concern. | Dale, a client who repeatedly had to show workers how to use his glucose machine to monitor his diabetes: ‘Yeah, it's like a school here. They just get out of school and this has gotta be their first job. They come here, they don't know nothing. I have to teach them everything.’ |
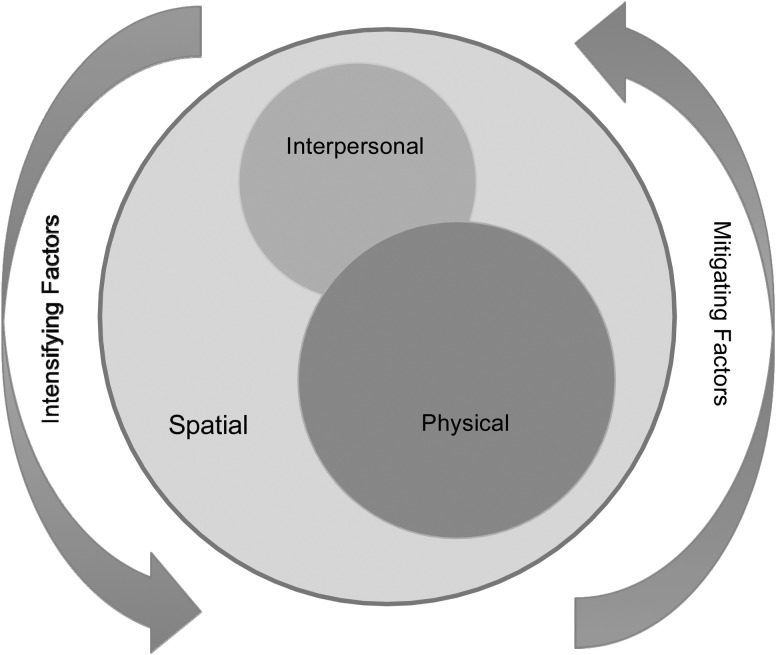
A revised conceptual model
We utilized the original conceptual model (see Fig. 1), developed through an analysis of HSWs discussion of safety [16], to initially code and organize the client and family transcripts. In applying the model to clients and family members, a slightly modified model emerged (see Fig. 2). In the revised model, temporal concerns have been removed, as only one interviewee discussed a concern that was temporal in nature. Also, the spatial node has been expanded, to highlight the dominant role that private home space plays in the participants' discussion of safety. Consistent with the initial HSW model, intensifying and mitigating factors encircle the concerns, as they have the ability to exacerbate or assuage the situation.
Figure 2.
Client and family caregivers' safety concerns.
Discussion
In spite of their safety concerns, participants overwhelming acknowledged that home is their preferred location to receive care (see [16]). Home is best, and more affordable from a health resource perspective [35], but the home must be safe for all individuals involved in the receipt and delivery of care. In these two companion studies, and the resultant conceptual models, all participants identify physical and spatial safety concerns as the most salient. While our previous analysis [16] demonstrated how HSWs enact strategies to create safe work environments, here we learned what home care clients and family caregivers do to create a safe living space. In order to preserve their own safety, clients and caregivers implemented numerous modification, tailored to the needs of their own home, to create a safer care space.
Making privately owned homes safer, however, requires resources, and many participants identified the cost of these changes as prohibitive. In the geographical location of our study, government and non-profit grants are available to support the purchase and installation of safety equipment (e.g. provincial Home Adaptations for Independence program). Awareness of and usage rates for these types of programs are often low. Provincial government research found that ‘Overall, few seniors … reported awareness of such programs (31 per cent) … only one in ten seniors had made any adaptations to their homes either with or without financial assistance’; those who are older and more frail are even less likely to know about such programs [36].
Clients and many of their caregivers are frail, and workers are also known to experience musculoskeletal injuries in the provision of home care [37]. Financial support for the creation of safe homes for older adults has the potential to prevent costly injuries to workers providing in-home care, to older clients wanting to age-in-place and to their caregivers, many of whom are older themselves (see Table 2). As homes become longer-term sites of care in lieu of more costly locations of healthcare provision [38], the financial burden of creating a safe care space should not be the client's alone to bear. This observation reflects also the findings of Lang et al. [4], who have noted that economic barriers for clients must be factored into our understanding of safety in home care. Similarly, the burden of maintaining hygienic home space should not fall solely on clients if they simultaneously serve as workspace for multiple care providers. Cutbacks and restructuring of the home care system in the locale of our study have resulted in fewer clients receiving assistance with housekeeping [39], exacerbating this type of safety concern. Clients consistently discussed the implications of living and receiving care in unhygienic and unsafe homes—placing this issue at the intersection of spatial and physical concerns.
Our model reinforces that safety in home care is multi-dimensional [22], and provides empirical support for Lang's [22] theorizing that safety in home care encompasses the physical, social, emotional and functional. With the empirical foundation of our two companion studies, our conceptual model shows that HSWs confront four distinct safety concerns: physical, spatial, interpersonal and temporal. In this present examination of clients and family caregivers, the temporal node was not salient in the new model.
For clients and family caregivers, home care does not begin and end when workers come and go. For workers, home care occurs when they are present in clients' homes. For clients and family members, however, home is ever present and not temporally bound as a place that is safe or unsafe, regardless of the worker's presence. As such, clients' and families' conceptualizations of safety in home care are much broader, from a time perspective. HSWs' definitions of safety are temporally bound, often a ‘50 min hour’ [40]; this is not so for clients and caregivers. Safety in home care is not limited to the time in which home care is provided. Safety in home care is salient in both the presence and absence of workers. This further highlights the need to invoke the voices of clients and family caregivers in our understanding of safety in the home [4]. A limitation of this study is that our university ethics approval process did not permit us to match clients, family caregivers and workers. These triads would have allowed us to more comprehensively understanding safety from the perspective of all three parties in the same context. A further limitation of this study is that the findings are derived from one region, and we must exercise caution in generalizations to broader contexts. Globally speaking, however, medical and paraprofessional care is increasingly provided in the home [41, 42]. Homes around the world are not standardized [43], and as such pose myriad safety concerns, much like those discussed here (Table 5).
Table 5.
Quoted participants' characteristics
| Quoted participant | Characteristics |
|---|---|
| Clients | |
| Bonnie | 86 years old, widowed, receiving care for 6 years |
| Helena | 82 years old, divorced, receiving care for 7 years |
| Flora | 73 years old, widowed, receiving care for 11 years |
| Reanna | 70 years old, divorced, receiving care for 2 months |
| Meredith | 72 years old, married, receiving care for 7.5 years |
| Antonia | 88 years old, separated, receiving care for 25 years |
| Sheryl | 65 years old, widowed, receiving care for 3 years |
| Dale | 68 years old, never married, receiving care for 3 years |
| Family caregivers | |
| Bella | Mother receiving home care for 2.5 years |
| Kelly | Mother receiving home care for 2 years |
| Kim | Mother receiving home care for 10 years |
| Harry | Wife receiving home care for 8.6 years |
| Martha | Husband receiving home care for 9 months |
| Eliana | Husband receiving home care for 5 months |
| Lara | Husband receiving home care for 12 years |
To cultivate a true ‘culture of safety’ in home care, the conceptualization of safety in this unique setting must be broadened beyond the tabulation of adverse events. Previous studies that have endeavoured to capture adverse events in home care have recognized that the more ‘psycho-social injuries are more challenging to identify and evaluate’ [7, p. 16], and consequently have been excluded. Assessment tools, such as the Resident Assessment Tool-Home Care (RAI-HC) do capture variables such as ‘unsafe housing’ and ‘social isolation with distress’ [3], but do not adequately capture the unique and potentially unsafe environments that home care clients live in.
Future studies must capture the full range of safety concerns in home care; the interpersonal, spatial and physical nodes in our model provide a framework to guide future measurement efforts. Furthermore, future efforts to understand the nature of safety in home care must address safety concerns, in addition to adverse events [e.g. 44]. By assessing and potentially intervening at the concern, rather than the adverse event, at which point a harmful outcome has already occurred, there will greater opportunities for prevention; and prevention, throughout the healthcare system, is the ultimate goal of our efforts to define, conceptualize and track patient safety [45].
Funding
This work was supported by the Canadian Institutes of Health Research [grant number IOP-70684].
Acknowledgements
The authors acknowledge the client and caregivers who participated in the interviews upon which this article is based. The authors also recognize the contributions of research assistants: Danielle Hachborn, Dimitra Panagiotoglou and Kathryn Knudson.
References
- 1.Canadian Home Care Association. Portraits of Home Care in Canada: 2013. Canada: CHCA, 2013. http://www.cdnhomecare.ca/content.php?doc=274(22 August 2015, date last accessed). [Google Scholar]
- 2.Canadian Home Care Association. Home is BestTM: Developing an Integrated Primary and Home & Community Care System. Canada: CHCA, High Impact Practices [Newsletter] 2012. http://www.cdnhomecare.ca/media.php?mid=2906 (22 August 2015, date last accessed). [Google Scholar]
- 3.Doran DM, Hirdes J, White N, et al. The Nature and Burden of Safety Problems Among Canadian Home Care Clients: Evidence From the RAI-HC Reporting System for Three Provinces and One Territory. Edmonton, AB: Canadian Patient Safety Institute, 2009. http://www.patientsafetyinstitute.ca (22 August 2015, date last accessed). [Google Scholar]
- 4.Lang A, Macdonald MT, Storch J, et al. Researching triads in home care: perceptions of safety from home care clients, their caregivers, and providers. Home Health Care Manag Pract 2014;26:59–71. [Google Scholar]
- 5.Johnson KG. Adverse events among Winnipeg home care clients. Healthc Q 2006;9:127–34. [DOI] [PubMed] [Google Scholar]
- 6.Masotti P, McColl MA, Green M. Adverse events experienced by homecare patients: a scoping review of the literature. Int J Qual Health Care 2010;22:115–25. [DOI] [PubMed] [Google Scholar]
- 7.Sears N, Baker GR, Barnsley J, et al. The incidence of adverse events among home care patients. Int J Qual Health Care 2013;25:16–28. [DOI] [PubMed] [Google Scholar]
- 8.Büssing A, Höge T. Aggression and violence against home care workers. J Occup Health Psychol 2004;9:206–19. [DOI] [PubMed] [Google Scholar]
- 9.Dellve L, Lagerstrom M, Hegberg M. Work-system risk factors for permanent work disability among home-care workers: a case-control study. Int Arch Occup Environ Health 2003;76:216–24. [DOI] [PubMed] [Google Scholar]
- 10.Heacock H, Paris-Seeley N, Tokuno C, et al. Development and evaluation of an affordable lift device to reduce musculoskeletal injuries among home support workers. Appl Ergon 2004;35:393–9. [DOI] [PubMed] [Google Scholar]
- 11.Howard N, Adams D. An analysis of injuries among home health care workers using the Washington State workers’ compensation claims database. Home Health Care Serv Q 2010;29:55–74. [DOI] [PubMed] [Google Scholar]
- 12.Macdonald M, Lang A, MacDonald J. Mapping a research agenda for home care safety: perspectives from researchers, providers, and decision makers. Can J Aging 2011;30:233–45. [DOI] [PubMed] [Google Scholar]
- 13.Stevenson L, McRae C, Mughal W. Moving to a culture of safety in community home health care. J Health Serv Res Policy 2008;13:20–4. [DOI] [PubMed] [Google Scholar]
- 14.Lang A. There's no place like home: research, practice and policy perspectives regarding safety in homecare. Int J Qual Health Care 2010;22:75–7. [DOI] [PubMed] [Google Scholar]
- 15.Sims-Gould J, Byrne K, Beck C, et al. Workers’ experiences of crises in the delivery of home support services to older clients: a qualitative study. J Appl Gerontol 2013;32:31–50. [DOI] [PubMed] [Google Scholar]
- 16.Craven C, Byrne K, Sims-Gould J, et al. Types and patterns of safety concerns in home care: staff perspectives. Int J Qual Health Care 2012;24:525–31. [DOI] [PubMed] [Google Scholar]
- 17.Sears NE. Harm From Home Care: A Patient Safety Study Examining Adverse Events in Home Care [Doctoral Dissertation]. Toronto, ON: University of Toronto, 2008. [Google Scholar]
- 18.Forbes DA, Markle-Reid M, Hawranik P, et al. Availability and acceptability of Canadian home and community-based services: perspectives of family caregivers of persons with dementia. Home Health Care Serv Q 2008;27:75–99. [DOI] [PubMed] [Google Scholar]
- 19.Lang A, Edwards N. Safety in Home Care: Broadening the Patient Safety Agenda to Include Home Care Services. Edmonton, AB: Canadian Patient Safety Institute, 2006. http://www.patientsafetyinstitute.ca. [Google Scholar]
- 20.Canadian Patient Safety Institute. Accelerating the Integration of Home Care Client Safety Tools and Resources: Strategies and Recommendations. Canada: CPSI, 2013. [Google Scholar]
- 21.Health Council of Canada. Seniors in Need, Caregivers in Distress: What are the Home Care Priorities for Seniors in Canada? Toronto, ON: Health Council of Canada, 2012. [Google Scholar]
- 22.Lang A, Edwards N, Fleiszer A. Safety in home care: a broadened perspective of patient safety. Int J Qual Health Care 2008;20:130–5. [DOI] [PubMed] [Google Scholar]
- 23.Stevenson L, Lang A, Macdonald M, et al. Safety in home care: thinking outside the hospital box. Healthc Q 2012;15:68–72. [DOI] [PubMed] [Google Scholar]
- 24.Lang A, Macdonald M, Storch J, et al. Home care safety perspectives from clients, family members, caregivers and paid providers. Healthc Q 2009;12:97–101. [DOI] [PubMed] [Google Scholar]
- 25.Aoun S, O'Connor M, Skett K, et al. Do models of care designed for terminally ill ‘home alone’ people improve their end-of-life experience? A patient perspective. Health Soc Care Community 2012;20:599–606. [DOI] [PubMed] [Google Scholar]
- 26.Lang A, Macdonald M, Stevenson L, et al. State of the Knowledge Regarding Safety In Home Care In Canada: An Environmental Scan. Edmonton, AB: Canadian Patient Safety Institute, 2009. http://www.patientsafetyinstitute.ca (22 August 2015, date last accessed). [Google Scholar]
- 27.Armstrong-Esther C, Hagen B, Sandilands M, et al. A longitudinal study of home care clients and their informal carers. Br J Community Nurs 2005;10:284–91. [DOI] [PubMed] [Google Scholar]
- 28.Macdonald M, Lang A, Storch J, et al. Safety in Home Care for Unpaid Caregivers: A Scoping Literature Review. Edmonton, AB: Canadian Patient Safety Institute, 2010. http://www.patientsafetyinstitute.ca (22 August 2015, date last accessed). [Google Scholar]
- 29.Pope C, Ziebland S, Mays N. Qualitative research in health care: analysing qualitative data. BMJ 2000;320:114–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Caelli K, Ray L, Mill J. ‘Clear as mud’: toward greater clarity in generic qualitative research. Int J Qual Methods 2003;2. [Google Scholar]
- 31.Eakin JM, Mykhalovskiy E. Reframing the evaluation of qualitative health research: reflections on a review of appraisal guidelines in the health sciences. J Eval Clin Pract 2003;9:187–94. [DOI] [PubMed] [Google Scholar]
- 32.Koch T. Establishing rigour in qualitative research: the decision trail. J Adv Nurs 2006;53:91–100. [DOI] [PubMed] [Google Scholar]
- 33.Blais R, Sears NA, Doran D, et al. Assessing adverse events among home care clients in three Canadian provinces using chart review. BMJ Qual Saf 2013;0:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cloutier DS, Martin-Matthews A, Byrne K, et al. The space between: using ‘relational ethics’ and ‘relational space’ to explore relationship-building between care providers and care recipients in the home space. Soc Cult Geogr 2015;16:764–82. [Google Scholar]
- 35.Hollander M, Chappell N. Final Report Of The National Evaluation Of The Cost-Effectiveness Of Home Care: A Report Prepared For The Health Transition Fund, Health Canada. Victoria, BC: Centre on Aging, University of Victoria, 2002. www.homecarestudy.com. [Google Scholar]
- 36.Office of the Seniors Advocate. B.C. Seniors Survey: Bridging the Gaps. Victoria, BC: Office of the Seniors Advocate, 2015. https://www.seniorsadvocatebc.ca/reports/ (22 August 2015, date last accessed). [Google Scholar]
- 37.Zeytinoğlu IU, Denton MA, Webb S, et al. Self-reported musculoskeletal disorders among visiting and office home care workers. Women Health 2001;31:1–35. [DOI] [PubMed] [Google Scholar]
- 38.Grignon M, Bernier NF. Financing Long-Term Care in Canada. Montréal, QB: Institute for Research on Public Policy, Study No. 33, 2012. http://irpp.org/research-studies/study-no33/ (22 August 2015, date last accessed). [Google Scholar]
- 39.Cohen M, McLaren A, Sharman Z, et al. From Support to Isolation: The High Cost of BC's Declining Home Support Services. Vancouver, BC: Canadian Centre for Policy Alternatives, 2006. https://www.policyalternatives.ca/publications/reports/support-isolation (22 August 2015, date last accessed). [Google Scholar]
- 40.Martin-Matthews, 2010. Time Matters: Negotiating Daily Life and the Work Day for Elderly Clients and their Home Support Workers. Keynote presented at British Society of Gerontology 2010; Brunel University.
- 41.Accreditation Canada and the Canadian Home Care Association. Home care in Canada: advancing quality improvement and integrated care. 2015. http://www.euro.who.int/en/publications/abstracts/home-care-in-europe.-the-solid-facts (22 August 2015, date last accessed).
- 42.Tarricone R, Tsorous AD. Home Care in Europe: The Solid Facts. WHO European Regional Office, 2008. http://www.euro.who.int/en/publications/abstracts/home-care-in-europe.-the-solid-facts (22 August 2015, date last accessed). [Google Scholar]
- 43.Milligan C. Location or dis-location? Towards a conceptualization of people and place in the care-giving experience. Soc Cult Geography 2013;4:455–70. [Google Scholar]
- 44.Doran DM, Baker GR, Szabo C, et al. Identification of serious and reportable events in home care: a Delphi survey to develop consensus. Int J Qual Health Care 2014;26:136–43. [DOI] [PubMed] [Google Scholar]
- 45.World Health Organization. Patient safety. 2015. http://www.who.int/patientsafety/en/ (22 August 2015, date last accessed).