Abstract
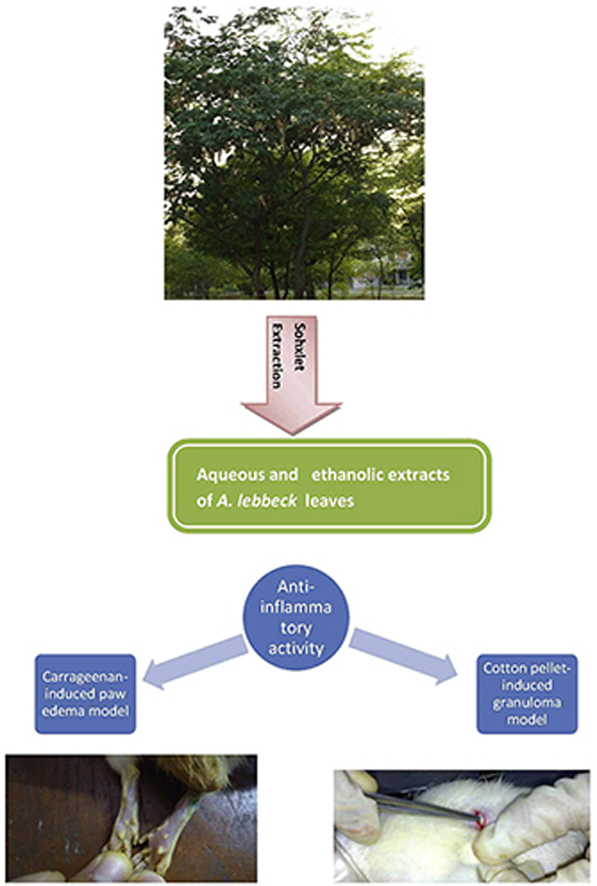
Albizzia lebbeck Benth. (Mimosaceae) is a medicinal tree used to treat several inflammatory ailments in the Indian traditional Ayurvedic system of medicine. The aim of the present study was to evaluate the possible anti-inflammatory activity of the aqueous (AE) and ethanolic (EE) extracts of the leaves of A. lebbeck to support the ethnopharmacological claims. The study was carried out using Wistar rats (100–150 g). The AE and EE were prepared using the Soxhlet extraction process. The anti-inflammatory activity of the AE and EE of the leaves of A. lebbeck were studied using carrageenan-induced paw edema and cotton pellet-induced granuloma models. The AE and EE of the leaves of A. lebbeck at doses of 50, 100, and 200 mg/kg p.o. (oral administration) showed a dose-dependent and significant (p < 0.05) inhibition of carrageenan-induced hind paw edema with maximum percentage inhibition (PI) values of 22.34, 30.85, 39.36 and 22.53, 32.98, 42.55, respectively. The AE and EE at doses of 50, 100, 200 mg/kg p.o. significantly (p < 0.05) inhibited granuloma formation with PI values of 19.07, 27.57, 38.55 and 23.93, 32.23, 42.33, respectively. The AE and EE of the leaves of A. lebbeck showed significant (p < 0.05) anti-inflammatory activity.
Keywords: Albizzia lebbeck leaves, Carrageenan, Cotton pellet, Percentage inhibition, Anti-inflammatory
Graphical abstract
1. Introduction
Understanding inflammation has always been an enigma for mankind. Something as minor as a bruise or something as major as a myocardial infarction can trigger this phenomenon. The major classes of drugs to suppress inflammation are nonsteroidal anti-inflammatory agents (NSAIDS) and corticosteroids but their toxic adverse effects such as epigastric distress, peptic ulceration, osteoporosis, and iatrogenic Cushing's syndrome have limited their use.1, 2 Looking at the present scenario, medicinal compounds derived from plant sources such as flavonoids, saponins, alkaloids, terpenoids, glycosides, and coumarins could provide an excellent fountainhead to develop new anti-inflammatory agents, which could be more efficacious, safer, affordable, and accessible for patients.
Albizzia lebbeck Benth. (Mimosaceae), commonly known as ‘Sirisa’ in Sanskrit, is a tall, unarmed, deciduous tree distributed throughout India. The traditional systems of medicine have been utilizing various parts of the tree to treat several inflammatory ailments such as asthma, bronchitis, arthritis, allergies, snake bites, fractures, hemicranias, gingivitis, toothaches, and sinusitis.3, 4 It is also claimed that the tree is useful in night blindness, cataract, leukoderma, erysipelas, leprosy, tuberculosis, scabies, amoebiasis, syphilis, spermatorrhoea, and piles.5, 6
The bark of A. lebbeck has stolen the limelight by its pleotropic activities such as anti-inflammatory, immunomodulatory, analgesic, antiarthritic, antioxidant, antimalarial, antitumor, and antifertility activities, pushing the leaves to the background.7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17 Despite the leaves being the most abundant and accessible medicinal part of the tree, possessing anticonvulsive, nootropic, antimicrobial, and antiulcer activities, there are no studies evaluating their anti-inflammatory activity.18, 19, 20, 21 Furthermore, phytochemical analysis of the leaves has revealed the presence of potentially bioactive alkaloids, triterpenoid saponins, and tri-O-glycoside flavonoids.22, 23, 24 This study was hence undertaken to evaluate the possible anti-inflammatory activity of aqueous (AE) and ethanolic (EE) extracts of the leaves of A. lebbeck in rats at different doses.
2. Materials and methods
2.1. Plant material
The leaves were obtained from the botanical garden of the Aligarh Muslim University (AMU), Aligarh in May 2011 and were authenticated by Dr Wazahat Hussain, a taxonomist, and a voucher specimen (voucher no. 2149) was deposited in the Department of Botany, AMU for further reference. The shade-dried leaves were ground homogenously using a mixer-grinder and approximately 100 g of the powder subjected to Soxhlet extraction, for 16 hours using 5 L of distilled water and 5 L of 99.9% ethanol (Scientific OEM, Mumbai, India) as solvents. The dark green, semi-solid extracts obtained were made free from the solvents by placing them in an incubator at 60°C for 12 hours. The yield of the AE was 21% and that of the EA was 12.398%. Previous toxicity studies of the leaves of A. lebbeck did not show any toxicity and behavioral changes in rats up to 2000 mg/kg p.o. (oral administration) dose,21 hence doses of 50, 100, and 200 mg/kg p.o. were selected for the present study.
2.2. Animals
Wistar rats (100–150 g) were obtained from the Animal House, Jawaharlal Nehru Medical College (JNMC), Aligarh. They were housed at a temperature of 24 ± 2°C, 12-hour light/dark cycles, 35–60% humidity, in polypropylene cages, and fed a standard rodent diet with water ad libitum. Animals were deprived of food but not water 4 hours before the experiment.
2.3. Drugs
Indomethacin (Merck, Bangalore, India), Diclofenac (Reckitt Benckiser, Gurgaon, India), and Carrageenan (Sigma Chemicals, St. Louis, MO, USA) were procured from the respective companies and were used in the study.
2.4. Ethical considerations
Experimental procedures and protocols used in this study were approved by the Institutional Animal Ethics committee of the JNMC and conform to the “Guidelines for care and use of animals in scientific research” (Indian National Science Academy 1998, Revised 2000).
2.5. Carrageenan-induced rat paw edema model
The rats were divided into eight groups (n = 6), each receiving distilled water (control), diclofenac 20 mg/kg p.o. (reference standard), and 50, 100, 200 mg/kg p.o. dose of the AE and EE of A. lebbeck, respectively. Carrageenan (0.1 mL of 1%) was injected into the subplantar tissue of the right hind-paw of each rat. The volume of the carrageenan injected into the foot was measured at 0, 30, 60, 120, and 180 minutes using a plethysmometer (Biodevices, New Delhi, India). The percentage inhibition (PI) at each time interval was calculated25:
V0 = Mean paw volume at 0 hours
Vt = Mean paw volume at a particular time interval
2.6. Cotton pellet-induced granuloma model
The rats were divided into eight groups (n = 6), each receiving distilled water (control), indomethacin 10 mg/kg p.o. (reference standard), and 50, 100, 200 mg/kg p.o. dose of the AE and EE of A. lebbeck, respectively. Thirty minutes after drug administration, an autoclaved cotton pellet of 10 ± 1.0 mg was aseptically implanted subcutaneously in the back region of the rats while anesthetized with ether (Scientific OEM, Mumbai, India). Extracts were administered once daily for the next 7 days. On Day 8, animals were anesthetized again and cotton pellets (Datt Mediproducts Ltd., New Delhi, India) were removed surgically, freed from the extraneous tissue, and dried in a hot-air oven overnight at 60°C. The dried pellets were weighed and the increment in the dry weight of the pellets was taken as a measure of granuloma formation. The PI of granuloma tissue development was calculated26:
2.7. Estimation of median effective dose
The median effective dose (ED50) values were estimated using GraphPad Prism software version 5.03 (GraphPad Software Inc., San Diego, CA, USA). The PI values obtained from the carrageenan-induced paw edema and cotton pellet-induced granuloma models were initially normalized to percentage activity assuming that the maximal response (100%) is seen at the dose of 200 mg/kg and the minimal response (0%) is seen at the dose of 0 mg/kg of the AE and EE. The log–dose response curves were then generated using a normalized nonlinear regression curve model, and by interpolation of the log dose (best-fit value) 50% activity was obtained. The antilog of the obtained log dose produced the ED50 value.
2.8. Statistical analysis
Results were expressed as mean ± standard error of the mean (SEM). Statistical analysis was performed using one-way analysis of variance (ANOVA) followed by multiple Tukey's comparison tests. A p value < 0.05 was considered statistically significant.
3. Results
3.1. Carrageenan-induced paw edema model
The AE and EE of the leaves of A. lebbeck (50, 100, 200 mg/kg, p.o.) showed a dose-dependent, significant inhibition of carrageenan-induced rat paw edema from 0.5 hours to 3 hours following drug administration, compared to the control group. The maximum PI of paw edema by the AE was observed as 22.34 (p < 0.05), 30.85 (p < 0.05), and 39.36 (p < 0.05) at the doses of 50, 100, 200 mg/kg p.o., respectively. The maximum PI of paw edema by the EE was observed as 25.53 (p < 0.05), 32.98 (p < 0.05), and 42.55 (p < 0.05) at the doses of 50, 100, 200 mg/kg p.o., respectively. Diclofenac 20 mg/kg p.o. showed a maximum PI of 61.70% at 3 hours after its administration (Table 1). The ED50 values of the AE and the EE were 28.91 mg/kg and 27.23 mg/kg, respectively.
Table 1.
Effect of the AE and EE of the leaves of Albizzia lebbeck with carrageenan-induced paw edema in rats.
| Paw volume (mL) | ||||||
|---|---|---|---|---|---|---|
| Groups | Before | 0 h | 1/2 h | 1 h | 2 h | 3 h |
| Distilled water | 0.97 ± 0.03 | 1.03 ± 0.03 | 1.67 ± 0.07 | 1.97 ± 0.06 | 2.02 ± 0.07 | 1.97 ± 0.04 |
| Diclofenac 20 mg/kg | 1.00 ± 0.04 | 1.07 ± 0.06 | 1.48 ± 0.03* (35.94) | 1.63 ± 0.03* (40.23) | 1.58 ± 0.02* (48.48) | 1.43 ± 0.03* (61.70) |
| AE 50 mg/kg | 0.97 ± 0.04 | 1.07 ± 0.04 | 1.60 ± 0.03 (17.19) | 1.83 ± 0.03 (19.15) | 1.85 ± 0.02* (21.21) | 1.80 ± 0.03* (22.34) |
| AE 100 mg/kg | 0.95 ± 0.03 | 1.02 ± 0.03 | 1.52 ± 0.03 (21.88) | 1.73 ± 0.02* (24.47) | 1.75 ± 0.02* (26.26) | 1.67 ± 0.02* (30.85) |
| AE 200 mg/kg | 0.92 ± 0.03 | 0.98 ± 0.04 | 1.45 ± 0.02* (26.56) | 1.63 ± 0.03* (30.85) | 1.65 ± 0.04* (32.32) | 1.55 ± 0.03* (39.36) |
| EE 50 mg/kg | 0.95 ± 0.03 | 1.07 ± 0.03 | 1.60 ± 0.03 (17.19) | 1.81 ± 0.03* (21.27) | 1.83 ± 0.02* (23.23) | 1.77 ± 0.03* (25.53) |
| EE 100 mg/kg | 1.00 ± 0.03 | 1.07 ± 0.04 | 1.57 ± 0.03 (21.88) | 1.77 ± 0.05* (25.53) | 1.78 ± 0.03* (28.28) | 1.70 ± 0.03* (32.98) |
| EE 200 mg/kg | 0.98 ± 0.03 | 1.08 ± 0.01 | 1.53 ± 0.01 (29.69) | 1.72 ± 0.02* (32.21) | 1.73 ± 0.02* (34.34) | 1.62 ± 0.03* (42.55) |
Values are presented as the mean ± SEM, n = 6 in each group; values given in parentheses represent PI.
One-way ANOVA followed by multiple Tukey's comparison test.
*p < 0.05, as compared to the control group.
AE = aqueous extract of the leaves of A. lebbeck; ANOVA = analysis of variance; EE = ethanolic extract of the leaves of A. lebbeck; PI = percentage inhibition; SEM = standard error of the mean.
3.2. Cotton pellet-induced granuloma model
The AE and EE showed a significant (p < 0.05) inhibition of the granuloma weight at all the doses. The PI of the granuloma weight by the AE was 19.07, 27.57, and 38.55 at the doses of 50, 100, 200 mg/kg p.o., respectively. The PI of the granuloma weight by the EE was 23.93, 32.23, and 42.33 at the doses of 50, 100, and 200 mg/kg p.o., respectively. Indomethacin 10 mg/kg p.o. showed the highest PI of 60.76 (p < 0.05). The anti-inflammatory action was dose-dependent for both the AE and EE (Table 2). The ED50 values of the AE and EE were 37.56 mg/kg and 30.17 mg/kg, respectively.
Table 2.
Effect of the AE and EE of the leaves of Albizzia lebbeck with the cotton pellet-induced granuloma model in rats.
| Groups | Dry weight of cotton pellet (mg) | PI |
|---|---|---|
| Distilled water | 51.07 ± 3.57236 | |
| Indomethacin 10 mg/kg | 20.04 ± 0.88921* | 60.76 |
| AE 50 mg/kg | 41.33 ± 2.53243* | 19.07 |
| AE 100 mg/kg | 36.99 ± 0.86422* | 27.57 |
| AE 200 mg/kg | 31.38 ± 1.02288* | 38.55 |
| EE 50 mg/kg | 38.85 ± 1.42238* | 23.93 |
| EE 100 mg/kg | 34.61 ± 0.54223* | 32.23 |
| EE 200 mg/kg | 29.45 ± 0.47099* | 42.33 |
Values are presented as the mean ± SEM, n = 6 in each group.
One-way ANOVA followed by multiple Tukey's comparison test.
*p < 0.05, as compared to the control group.
AE = aqueous extract of the leaves of A. lebbeck; ANOVA = analysis of variance; EE = ethanolic extract of the leaves of A. lebbeck; PI = percentage inhibition; SEM = standard error of the mean.
4. Discussion
In this study, we evaluated the anti-inflammatory activity of the AE and EE of the leaves of A. lebbeck by two experimental models, i.e., carrageenan-induced paw edema and cotton pellet-induced granuloma model. The carrageenan-induced paw edema model is used to screen the anti-inflammatory activity of a drug in the acute phase of inflammation. Edema induced by carrageenan is believed to be biphasic.27, 28 The first phase (1 hour) involves the release of serotonin and histamine and the second phase (> 1 hour) is mediated by cyclooxygenase products. Continuity between the two phases is provided by kinin.29 The AE and EE of the leaves of A. lebbeck significantly inhibited the edema formation in both the first and second phases. The anti-edematous activity of A. lebbeck in the first phase could be due to the possible suppression of histamine signaling by the mast cell stabilizing effect,10, 30, 31 and direct inhibition of histamine H1 receptor and histidine decarboxylase gene transcriptions.32 Another possible explanation could be the corticotrophic action of A. lebbeck as evidenced by a raise in plasma cortisol levels,33 which antagonizes nuclear factor-kappa-B (NF-κB).34 In the present study, the anti-edematous activity of the AE and EE persisted in the second phase with the maximal effect observed at 3 hours. This could be explained by the possible inhibition of the release and/or action of kinin and prostaglandin by A. lebbeck.8
The cotton pellet-induced granuloma method is a well-known model to screen the anti-inflammatory activity in the chronic phase of inflammation,35 which is characterized by monocyte infiltration, fibroblast proliferation, angiogenesis, and exudation.36 The dry weight of the cotton pellet correlates well with the amount of granulomatous tissue formed.37 In this study, the AE and EE decreased the dry weight of the granuloma significantly when compared to the control groups. This may be due to the ability of A. lebbeck in reducing the number of fibroblasts, preventing angiogenesis and synthesis of collagen and mucopolysaccharide.9 The suppression of the T helper 1 (Th-1) T-lymphocyte pathway, which releases inflammatory cytokines such as interleukin-12 and interferon-γ, may also be responsible for this action.38 However, mechanistic studies measuring specific cytokine levels may help elucidate this reasoning.
A previous study evaluating the anti-inflammatory activity of the bark of A. lebbeck showed a maximum PI of 58.94 and 53.57 for the EE in the carrageenan-induced paw edema and cotton pellet granuloma models, respectively.9 In the present study, the EE of the leaves showed a maximum PI of 42.55 and 42.33 in the respective models. Hence, it is suggested that the anti-inflammatory activity of the bark is higher than that of the leaves.
The preliminary phytochemical analysis of the leaves of A. lebbeck shows the presence of several compounds such as alkaloids, steroids, terpenoids, tannins, glycosides, flavonoids, and saponins.39 The high performance thin layer chromatography (HPTLC) profile studies on the petroleum ether extract revealed the presence of 10 different alkaloids with retention factor (Rf) values between 0.02 and 0.85. The ethyl acetate extract displayed the presence of five different alkaloids with Rf values between 0.09 and 0.84. The methanolic extract disclosed the presence of four different alkaloids with Rf values ranging from 0.02 to 0.79.22 Each of these 19 alkaloids is yet to be characterized. Two-dimensional paper chromatography studies on the hydroethanolic extract of the leaves disclosed the presence of two tri-O-glycoside flavonols, i.e., kaempferol 3-O-α rhamnopyranosyl(1→6)-β-glucopyranosyl(1→6)-o-galactopyranoside and quercetin 3-O-α rhamnopyranosyl(1→6)-β-glucopyranosyl(1→6)-β-galactopyranoside. Their structures were elucidated by electrospray ionization mass spectrometry (ESI-MS) and 1H and 13C nuclear magnetic resonance (NMR) spectral analysis.24 The n-butanolic fraction of the methanolic extract of leaves when subjected to HPTLC revealed the presence of a triterpenoid saponin, i.e., albiziahexoside(α-l-rhamonopyranosyl-(1→4)-α-l-rhamonopyranosyl-(1→2)-β-d-xylopyranosyl)-3-O-β-d-xylopyranosyl-(1→2)-α-l-arabinopyranosyl-(1→6)-2-acetamido-2-deoxy-β-d-glucopyranosyloleanolate). Its structure was characterized by NMR and fast atom bombardment mass spectroscopy (FABMS).23
It is difficult to attribute the observed effects of the leaves of A. lebbeck to any one particular chemical moiety. Flavonoids and saponins are known to exhibit their anti-inflammatory effect by several mechanisms40, 41 along with a wide spectrum of other pharmacological effects such as analgesic, antioxidant, antimicrobial, antiviral, anticancer, antidiabetic, and antiplatelet activities.42 Hence, in light of present experimental and HPTLC data available, the anti-inflammatory activity of the leaves of A. lebbeck could be attributed to its flavonoids and saponins.
5. Conclusion
It can be concluded that the AE and the EE of the leaves of A. lebbeck possess anti-inflammatory activity thus validating the ethnopharmacological claims. This knowledge could be tapped to formulate new agents to treat inflammatory and allergic ailments.
Conflicts of interest
All authors declare no conflicts of interest.
Footnotes
Peer review under responsibility of The Center for Food and Biomolecules, National Taiwan University.
References
- 1.Grosser T., Smyth E., Fitzgerald G.A. Goodman and Gilman's the pharmacological basis of therapeutics. In: Brunton L., editor. Anti-inflammatory, Antipyretic and Analgesic Agents: Pharmacotherapy of Gout. 12th ed. McGraw-Hill; New York, NY: 2011. pp. 959–1000. [Google Scholar]
- 2.Chorousus G.P. Basic and clinical pharmacology. In: Katzung B.G., Masters S.B., Trevor A.J., editors. Adrenocorticosteroids and Adrenocortical Antagonists. 12th ed. McGraw-Hill; New York, NY: 2012. pp. 697–711. [Google Scholar]
- 3.Ayurvedic Pharmacopoeia Committee . Controller of Publications; New Delhi: 2001. Department of AYUSH, Ministry of Health and Family Welfare, Government of India. Ayurvedic Pharmacopoeia of India. [Google Scholar]
- 4.Kirtikar K.R., Basu B.D. 2nd ed. Panini Office Indian Press; Allahabad: 1919. Indian Medicinal Plants. [Google Scholar]
- 5.Nadkarni K.M. 3rd ed. Bombay Popular Prakashan; Mumbai: 1982. Indian Materia Medica. [Google Scholar]
- 6.Rajagopalan K., Sivarajan V.V., Varier P.R. 2nd ed. Orient Longmans; Madras: 1993. Indian Medicinal Plants. [Google Scholar]
- 7.Das A.K., Ahmed F., Bachar S.C., Kundu J., Dev S. Anti-inflammatory effect of Albizzia lebbeck (Benth.) bark. J Biol Sci. 2003;3:685–687. [Google Scholar]
- 8.Pramanik K.C., Bhattacharya P., Chatterjee T.K., Mandal S.C. Antiinflammatory activity of methanol extract of Albizzia lebbeck (Mimosaceae) bark. Eur Bull Drug Res. 2005;13:71–75. [Google Scholar]
- 9.Babu P.N., Pandikumar P., Ignacimuthu S. Anti-inflammatory activity of Albizia lebbeck Benth., an ethnomedicinal plant, in acute and chronic animal models of inflammation. J Ethnopharmacol. 2009;125:356–360. doi: 10.1016/j.jep.2009.02.041. [DOI] [PubMed] [Google Scholar]
- 10.Baruah C.C., Gupta P.P., Patnaik G.K., Dubey M.P., Goel R.K., Dhawan B.N. Comparative study of the anti-PCA and mast-cell stabilizing activity fractions of Albizzia Lebbeck: a traditional medicinal plant. J Med Arom Plant Sci. 2000;22:59–63. [Google Scholar]
- 11.Achinto S., Munirudin A. The analgesic and the anti-inflammatory activity of the extract of Albizia lebbeck in animal models. Pak J Pharm Sci. 2009;22:74–77. [PubMed] [Google Scholar]
- 12.Pathak N., Gohil P., Patel N., Kasture S., Jivani N., Bhalodia Y. Curative effect of Albizia lebbeck methanolic extract against adjuvant arthritis with special reference to bone erosion. Int J Pharm Sci Drug Res. 2009;1:183–187. [Google Scholar]
- 13.Nimish L.P., Natvarlal J.P., Sanjay B.K., Niruddin P.J., Yagnik S.B., Shailesh V.M. Curative effect of Albizia lebbeck methanolic extract against adjuvant arthritis with special reference to bone erosion. Indian J Pharm Res Dev. 2010;1:183–187. [Google Scholar]
- 14.Resmi C.R., Venukmar M.R., Latha M.S. Antioxidant activity of Albizia lebbeck Benth in alloxan treated diabetic rats. Indian J Physiol Pharmacol. 2006;50:297–302. [PubMed] [Google Scholar]
- 15.Qureshi S.A., Mohiuddin S., Fatima B., Badary Y. Laboratory studies on some plant extracts as mosquito larvicides. Pak J Sci Ind Res. 1986;29:361–365. [Google Scholar]
- 16.Haque N., Chowdhary S.A.R., Nutan M.T.H., Rahman G.M.S., Rahman K.M., Rashid M.A. Evaluation of antitumor activity of some medicinal plants of Bangladesh by potato disc bioassay. Fitoterapia. 2000;11:547–552. doi: 10.1016/s0367-326x(00)00162-3. [DOI] [PubMed] [Google Scholar]
- 17.Gupta R.S., Chaudhary R., Yadav R.K., Verma S.K., Dobhal M.P. Effect of saponins of Albizzia lebbeck (L.) Benth. bark on the reproductive system of male albino rats. J Ethnopharmacol. 2005;96:31–36. doi: 10.1016/j.jep.2004.07.025. [DOI] [PubMed] [Google Scholar]
- 18.Kasture V.S., Chopade C.T., Deshmukh V.K. Anticonvulsive activity of Albizia lebbeck, Hibiscus rosa sinesis and Butea monosperma in experimental animals. J Ethnopharmacol. 2000;71:65–75. doi: 10.1016/s0378-8741(99)00192-0. [DOI] [PubMed] [Google Scholar]
- 19.Une H.D., Pal S.C., Kasture V.S., Kasture S.B. Nootropic and anxiolytic activity of saponins of Albizia lebbeck leaves. Pharmacol Biochem Behav. 2005;69:439–444. doi: 10.1016/s0091-3057(01)00516-0. [DOI] [PubMed] [Google Scholar]
- 20.Mohammed N.B., Edward G.W., Marimuthu A.J. In vitro anti-bacterial activity of leaves extracts of Albizia lebbeck Benth against some selected pathogens. Asian Pacific J Trop Biomed. 2012;2:859–862. [Google Scholar]
- 21.Shirode D., Patel T., Roy S.P. Anti-ulcer properties of 70% ethanolic extract of leaves of Albizzia lebbeck. Phcog Mag. 2008;4:228–231. [Google Scholar]
- 22.Mohammed N.B., Wesely E.G., Johnson M. High performance thin layer chromatography profile studies on the alkaloids of Albizia lebbeck. Asian Pacific J Trop Biomed. 2012;2:1–6. [Google Scholar]
- 23.Ueda M., Tokunaga T., Okazaki M., Sata N.U., Ueda K., Yamamura S. Albiziahexoside: a potential source of bioactive saponin from the leaves of Albizzia lebbeck. Nat Prod Res. 2003;17:329–335. doi: 10.1080/1057563031000072578. [DOI] [PubMed] [Google Scholar]
- 24.Amani M.D., El-Mousallamy Leaf flavanoids of Albizzia lebbeck. Phytochemistry. 1998;48:759–761. doi: 10.1016/s0031-9422(97)01117-5. [DOI] [PubMed] [Google Scholar]
- 25.Winter C.A., Risely E.A., Nuss G.W. Carrageenin-induced edema in the hind paw of rat as an assay for antiinflammatory drugs. Proc Soc Exp Biol Med. 1962;111:544–547. doi: 10.3181/00379727-111-27849. [DOI] [PubMed] [Google Scholar]
- 26.Winter C.A., Porter C.A. Effect of alteration in side chain upon anti-inflammatory and liver glycogen activities in hydrocortisone esters. J Am Pharm Assoc. 1957;46:515–519. doi: 10.1002/jps.3030460902. [DOI] [PubMed] [Google Scholar]
- 27.Vinegar R., Schreiber W., Hugo R.J. Biphasic development of carrageenan edema in rats. J Pharmacol Exp Ther. 1969;166:96–103. [PubMed] [Google Scholar]
- 28.Di Rosa M., Giroud J.P., Willoughby D.A. Studies on the mediators of the acute inflammatory response induced in rats in different sites by carrageenan and turpentine. J Pathol. 1971;104:15–29. doi: 10.1002/path.1711040103. [DOI] [PubMed] [Google Scholar]
- 29.Salvemini D., Wang Z.Q., Wyatt P.S. Nitric oxide: a key mediator in the early and late phase of carrageenan-induced rat paw inflammation. Br J Pharmacol. 1996;118:829–838. doi: 10.1111/j.1476-5381.1996.tb15475.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Shashidhara S., Bhandarkar A.V., Deepak M. Comparative evaluation of successive extracts of leaf and stem bark of Albizzia lebbeck for mast cell stabilization activity. Fitoterapia. 2008;79:301–302. doi: 10.1016/j.fitote.2008.01.006. [DOI] [PubMed] [Google Scholar]
- 31.Tripathi R.M., Sen P.C., Das P.K. Further studies on the mechanism of the anti-anaphylactic action of Albizzia lebbeck, an Indian indigenous drug. J Ethnopharmacol. 1979;1:397–400. doi: 10.1016/s0378-8741(79)80004-5. [DOI] [PubMed] [Google Scholar]
- 32.Nurul I.M., Mizuguchi H., Shahriar M. Albizzia lebbeck suppresses histamine signalling by the inhibition of hisamine H1 receptor and histidine decarboxylase gene transcriptions. Int Immunopharmacol. 2011;11:1766–1772. doi: 10.1016/j.intimp.2011.07.003. [DOI] [PubMed] [Google Scholar]
- 33.Tripathi S.N., Shukla P. Effect of histamine and Albizzia lebbek Benth. on guinea pig adrenal glands. Indian J Exp Biol. 1979;17:915–917. [PubMed] [Google Scholar]
- 34.Almawi W.Y., Melemedjian O.K. Negative regulation of nuclear factor-kappa B activation and function by glucocorticoids. J Mol Endocrinol. 2002;28:69–78. doi: 10.1677/jme.0.0280069. [DOI] [PubMed] [Google Scholar]
- 35.Vogel H.G. 2nd ed. Springer; New York, NY: 2002. Drug Discovery and Evaluation, Pharmacological Assay. [Google Scholar]
- 36.Majno G. Chronic inflammation: links with angiogenesis and wound healing. Am J Pathol. 1998;153:1035. doi: 10.1016/S0002-9440(10)65648-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zhu Z.Z., Ma K.J., Ran X. Analgesic, anti-inflammatory and antipyretic activities of the petroleum ether fractions from the ethanol extract of Desmodium podocarpum. J Ethnopharmacol. 2011;133:1126–1131. doi: 10.1016/j.jep.2010.11.042. [DOI] [PubMed] [Google Scholar]
- 38.Yadav S.S., Galib, Prajapati P.K., Ashok B.K., Ravishankar B. Evaluation of immunomodulatory activity of “Shirishavaleha” – an Ayurvedic compound formulation in albino rats. J Ayurveda Integr. 2011;2:192–196. doi: 10.4103/0975-9476.90775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rahul C., Lincy J., Methew G., Pankaj P. Pharmacognostic standardization and phytochemical screening of Albizzia lebbeck. J Chem Pharm Res. 2010;2:432–443. [Google Scholar]
- 40.Romano B., Pagano E., Montanaro V., Fortunato A.L., Milic N., Borrelli F. Novel insights into the pharmacology of flavonoids. Phytother Res. 2013;27:1588–1596. doi: 10.1002/ptr.5023. [DOI] [PubMed] [Google Scholar]
- 41.Francis G., Kerem Z., Makkar H.P., Becker K. The biological action of saponins in animal systems: a review. Br J Nutr. 2002;88:587–605. doi: 10.1079/BJN2002725. [DOI] [PubMed] [Google Scholar]
- 42.Xiao J., Chen T., Cao H. Flavonoid glycosylation and biological benefits. Biotechnol Adv. 2014;14:92–95. doi: 10.1016/j.biotechadv.2014.05.004. [DOI] [PubMed] [Google Scholar]


