Abstract
Objectives
We provide the first known examination of differences in non-urgent and urgent emergency department usage between Hispanic and non-Hispanic white individuals, with varying levels of acculturation.
Methods
We pooled cross-sectional data for Hispanic and non-Hispanic white adults (ages 18–64) from the 2011–2013 National Health Interview Surveys. Using logistic regression models, we examined differences in past-year emergency department use, urgent emergency department use, and non-urgent emergency department use by acculturation level, which we measure by combining information on respondents’ citizenship status, birthplace, and length of stay (immigrants <5 , 5–10, >10 years in US; naturalized citizens; US-born).
Results
Overall, 17.8% of Hispanic individuals and 18.5% of non-Hispanic white individuals use the emergency department annually. Compared to U.S.-born non-Hispanic white individuals, the least acculturated Hispanic individuals are 14.4 percentage points (p<0.001) less likely to use the emergency department for any reason, 9.8 percentage points (p<0.001) less likely to use it for a non-urgent reason, and 5.3 percentage points (p<0.01) less likely to use it for an urgent reason.
Conclusions
Contrary to popular perception, the least acculturated Hispanic individuals are the least likely to use the emergency department. As acculturation level rises, so does one’s likelihood of using the emergency department, particularly for non-urgent visits.
INTRODUCTION
The crowding of U.S. emergency departments (EDs) is a known public health concern, and has been attributed, in part, to non-urgent ED use. Non-urgent emergency department (ED) visits are encounters that could have been safely delayed for up to 24 hours, or which could have been treated in a non-emergent care setting (1–3). Both non-urgent ED visits and ED overcrowding have been linked to several negative consequences, including increased pain and suffering, longer wait times, higher costs, more unnecessary procedures, missed opportunities for patients to build relationships with primary care providers, and reduced disaster preparedness (3–6).
Of the 116.8 million ED visits completed annually, almost 30% can be classified as non-urgent (1, 5). This phenomenon may worsen in the coming years, given the insurance expansions from the Affordable Care Act coupled with the shortage of primary care physicians in many communities (7–9). Several national organizations, including the Agency for Healthcare Research and Quality and the US Senate’s Subcommittee on Primary Health and Aging, have named reducing non-urgent ED visits as a key health policy priority (10, 11).
A perception exists, with limited empirical support, that minority populations contribute disproportionately to ED crowding and non-urgent ED visits (12–14). The rapidly-growing Hispanic population has come under particular fire, possibly due to concerns about health care service use among undocumented immigrants, a frequent media topic (15, 16). Though the most recent numbers available on this subject suggest that Hispanic individuals are more likely to use the ED for non-urgent or routine care, several accounts in the literature find otherwise (17–20). One reason for this discrepancy might be the tendency to treat Hispanic individuals as a monolithic group, rather than accounting for heterogeneity within the population (21). Accounting for the acculturation level of individuals is one increasingly popular mechanism for addressing these within-group differences.
Acculturation is defined as the degree to which an individual from one culture adopts the behaviors or characteristics of a different “host” culture (22). Applied to the field of health care, acculturation might play an important role in individuals’ willingness or ability to successfully navigate the health care system. A small but growing body of literature has examined the ways in which acculturation influences individuals’ health services use. Generally, higher acculturation levels are associated with improvements in access to and uptake of primary and preventive care. More specifically, studies have found that Hispanic individuals with higher levels of acculturation (i.e., greater assimilation into United States culture) have better insurance coverage, have a higher uptake of preventive and primary care services, and are more likely to have a usual source of health care, compared to individuals with lower levels of acculturation (23–33). In light of this body of evidence, one might expect that as Hispanic individuals become more acculturated, they are less likely to use the ED for non-urgent care, due to their better access to care in the community.
Despite a growing appreciation for the role of acculturation in health services use, no national-level study has examined how acculturation might affect the way in which Hispanic individuals interact with the ED. Two national studies have found that immigrants are less likely to use the ED, but did not examine the effect for Hispanic individuals alone (34, 35). Two smaller studies that have focused on Hispanic individuals alone had mixed results. On the one hand, Nandi et al. found no relationship between acculturation level and ED use among undocumented Mexican immigrants in New York City (36). On the other hand, Ortega et al. found that Mexican-born immigrants in the state of California are less likely to have used the ED in the past year, compared to U.S.- born Mexican individuals (37). Lastly, no known study has examined the relationship between acculturation level and non-urgent versus urgent ED use. This is an important distinction, given that non-urgent ED use is a noted public health concern.
In this paper, we first present a national-level overview on the relationship between Hispanic ethnicity and non-urgent or urgent ED use. Then, we present the first known examination of how non-urgent and urgent ED use differs among Hispanic individuals with different acculturation levels. Findings from this study may inform policy conversations about ED services use by Hispanic individuals in general, and Hispanic immigrants (both recent and earlier) in particular.
METHODS
Data for this study come from the National Health Interview Survey (NHIS), an annual, nationally-representative, cross-sectional survey of the civilian, non-institutionalized population in the United States (38). The annual sample size is approximately 35,000 households (about 87,500 individuals), with a response rate between 75–82% for the years analyzed. The survey includes questions on basic health and demographic items, along with questions about ED use (38). We combine NHIS years 2011, 2012, and 2013 to form a pooled cross-section of data for individuals between the ages of 18 and 64. We limit our sample to individuals who identify either as Hispanic (any race) or as non-Hispanic white.
Our dependent variables of interest are binary indicators for any ED use, non-urgent ED use, and urgent ED use. Respondents were asked: “During the past 12 months, how many times have you gone to a hospital emergency room about your own health?” If a patient had any past-year ED use, he or she was asked whether any of ten attributes applied to his or her most recent ED visit. Five of these pertain to visit urgency: the visit resulted in hospital admission; the patient was advised by a health provider to go to ED; the problem was too serious for doctor’s office/clinic; only a hospital could help with the problem; or the patient arrived at ED by ambulance/other emergency vehicle. We use the information from these two questions to create dichotomous indicators for our outcome variables, consistent with the approach developed by Cunningham et al. (17, 39). An ED visit was classified as urgent if the individual indicated any of the above criteria applied; all other visits are classified as non-urgent.
We measure acculturation using a combination of several proxy variables that have been previously used in the literature: whether the individual is a U.S. citizen (yes, no); whether the individual was born in the U.S. (yes, no); and the amount of time a Hispanic individual has spent in the United States (40, 41). All individuals who were born outside of the United States were asked how long they have been in this country (less than one year, between one and five years, between five and 10 years, between 10 and 15 years, and 15 or more years). We use these measures to create five mutually exclusive categories of acculturation for the Hispanic individuals in our sample: (1) non-citizen immigrants who have been here for <5 years; (2) non-citizen immigrants who have been here for between five and 10 years; (3) non-citizen immigrants who have been here for 10 or more years; (4) immigrants who are naturalized citizens; and (5) U.S.-born individuals. We create parallel categories for all non-Hispanic white individuals in our sample.
Following the Andersen framework, we control for individual-level predisposing, enabling and need factors in our models (42). Turning first to predisposing characteristics, we include a dichotomous indicator for female gender, a continuous measure of age in years, and a categorical measure of marital status (married or living with a partner; divorced, widowed, or separated; and never married).
To control for enabling characteristics, we include a dummy variable for having usual source of care in the community (USOC); and categorical variables for insurance status (uninsured, publically insured, and any private insurance), education level (less than high school, high school graduate, college graduate, and graduate degree), employment status (unemployed, employed part-time, or employed full-time), and income (less than $25,000, between $25,000 and under $55,000, between $55,000 and under $75,000, and over $75,000). Need for health care services is controlled for using a dummy variable for individuals who reported having fair or poor health (versus good, very good, or excellent). We also include dichotomous indicators for individuals who reported previous diagnosis of any of the following conditions: asthma, diabetes, myocardial infarction, stroke, and heart disease.
Of the 314,526 individuals participating in the NHIS from 2011–2103, 146,978 met our age and ethnicity criteria. Of these, 40% were randomly selected to answer questions about their ED use, and 98% of these had complete information on the acculturation variables and other control variables in our model; these individuals comprise our final analytic sample (N=58,888).
In the first part of our analysis, we compare the unadjusted ED usage rates for Hispanic and non-Hispanic white individuals in our sample. We then repeat this comparison, breaking out the Hispanic individuals by acculturation level. For these two analyses, we use a test of proportions to determine statistical differences between groups. Finally, we estimate logistic regression models for each outcome of interest (any ED use, urgent ED use, and non-urgent ED use), obtaining marginal effects for each model. Our reference group is U.S.-born non-Hispanic white individuals.
All models include year indicators, and were estimated using Stata Version 13 (StataCorp, College Station, TX, USA). Survey weights were applied to obtain national estimates.
RESULTS
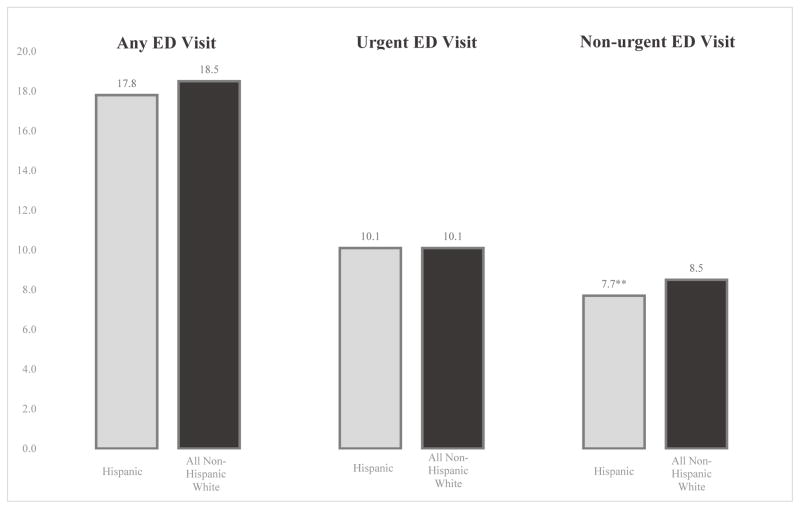
Figure 1 displays the unadjusted rates of ED usage among Hispanic and non-Hispanic white individuals. Rates of any ED use and urgent ED use do not differ statistically between these two groups. However, Hispanic individuals are less likely to use the ED for a non-urgent visit, compared to non-Hispanic white individuals. Specifically, 7.7% of Hispanic individuals have used the ED for a non-urgent reason in the past year, compared to 8.5% of non-Hispanic white individuals (p<0.01)
Figure 1.
Unadjusted percentage of non-elderly adults with past-year ED use, by ethnicity
*p < 0.05, ** p < 0.01, *** p < 0.001
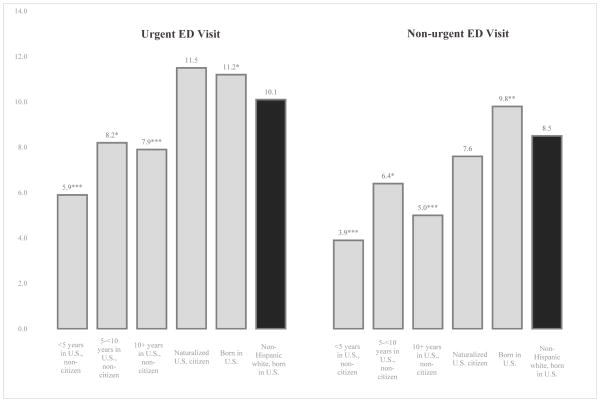
Figure 2 presents the unadjusted rate of urgent and non-urgent ED visits, by acculturation level, using US-born non-Hispanic white individuals as a reference group. Unadjusted rates of any ED use (urgent and non-urgent, combined) are available in Figure 1 of the online appendix. Overall, higher levels of acculturation are associated with greater ED use for both urgent and non-urgent conditions, and the least acculturated individuals are the least likely to use the ED for any reason. Specifically, only 5.9% and 3.9% of recent Hispanic immigrants (<5 years in U.S) had an urgent and non-urgent ED visit, respectively, compared with 10.1% (p<0.001) and 8.5% (p<0.001) of U.S-born non-Hispanic white individuals. Conversely, the most acculturated Hispanic individuals, especially US-born., use the ED at similar or greater rates than non-Hispanic whites do.
Figure 2.
Unadjusted percentage of non-elderly adults with past-year ED use, by acculturation level
*p < 0.05, ** p < 0.01, *** p < 0.001
Descriptive statistics for our analytic sample (Table 1) show a number of differences with respect to enabling and need characteristics. Less than 40% of the least acculturated individuals have a USOC, compared to over 80% in the non-Hispanic white group (p<0.001). Wide variation across groups is also seen for insurance status, educational level, and income. The least acculturated Hispanics are healthier than U.S.-born non-Hispanic whites, while more acculturated Hispanics have a lower health status.
Table 1.
Weighted summary statistics for Hispanic non-elderly adults and non-Hispanic white individuals born in the United States
| Hispanic
|
||||||
|---|---|---|---|---|---|---|
| In U.S. less than 5 years, non- citizen | In U.S. 5 to less than 10 years, non- citizen | In U.S. 10 or more years, non- citizen | Born outside of US, naturalized citizen | Born in U.S. | Non-Hispanic White, Born in the U.S. | |
| Number of observations | 522 | 1,065 | 4,018 | 3,089 | 6,204 | 41,984 |
| Predisposing | ||||||
| Female gender (%) | 47.6 | 51.3 | 48.4 | 54.9*** | 52.7*** | 51.7 |
| Age (mean) | 31.5*** | 33.3*** | 39.9*** | 44.9*** | 35.2*** | 42.7 |
| Marital status | ||||||
| Currently married (%) | 56.0 | 63.5*** | 66.3*** | 59.5*** | 45.9*** | 54.1 |
| Never married (%) | 35.8** | 26.5 | 18.2*** | 17.3*** | 37.7*** | 26.3 |
| Divorced or widowed (%) | 8.1*** | 10.0*** | 15.6*** | 23.2*** | 16.4*** | 19.5 |
| Enabling | ||||||
| Has U.S.O.C. (%) | 39.9*** | 49.0*** | 58.8*** | 78.1*** | 75.0*** | 83.8 |
| Insurance status | ||||||
| Uninsured (%) | 64.4*** | 74.0*** | 62.1*** | 27.9*** | 25.2*** | 15.0 |
| Privately insured (%) | 21.2*** | 15.2*** | 22.1*** | 50.5*** | 54.7*** | 72.4 |
| Publically insured (%) | 14.4 | 10.8 | 15.8** | 21.7*** | 20.1*** | 12.6 |
| Educational attainment | ||||||
| Less than high school (%) | 41.5*** | 52.2*** | 59.2*** | 28.3*** | 15.0*** | 7.2 |
| High school graduate (%) | 34.4*** | 33.6*** | 31.5*** | 41.5** | 54.5*** | 46.1 |
| College graduate (%) | 17.8*** | 12.1*** | 8.1*** | 24.0*** | 25.7*** | 35.6 |
| Graduate school graduate (%) | 6.3** | 2.2*** | 1.2*** | 6.3*** | 4.7*** | 11.2 |
| Annual income (individual) | ||||||
| Under $25,000 (%) | 55.6*** | 53.8*** | 45.8*** | 30.0*** | 29.7*** | 22.0 |
| $25,000 to less than $55,000 (%) | 29.5 | 33.5** | 38.9*** | 35.5*** | 31.9*** | 27.3 |
| $55,000 to less than $75,000 (%) | 7.0*** | 6.2*** | 8.1*** | 13.0 | 13.3 | 13.8 |
| Over $75,000 (%) | 7.9*** | 6.5*** | 7.1*** | 21.6*** | 25.1*** | 36.8 |
| Employment status | ||||||
| Unemployed (%) | 36.7*** | 30.4** | 31.3*** | 29.4** | 30.7*** | 27.1 |
| Employed, part time (%) | 9.0 | 10.3 | 9.6 | 8.4** | 10.8 | 10.7 |
| Employed, full time (%) | 54.3*** | 59.2** | 59.1*** | 62.1 | 58.4*** | 62.2 |
| Need | ||||||
| Health status | ||||||
| Reported health fair or poor (%) | 10.0 | 9.6 | 13.7*** | 16.2*** | 12.1*** | 10.6 |
| Asthma (%) | 3.8*** | 5.2*** | 4.1*** | 11.3*** | 15.3 | 13.7 |
| Diabetes (%) | 2.0** | 2.3*** | 7.4 | 9.7*** | 7.3** | 6.2 |
| Heart Disease (%) | 1.0 | 7.4** | 1.2*** | 2.1 | 1.7*** | 2.8 |
| Myocardial Infarction (%) | 0.6 | 0.6** | 0.8*** | 1.5 | 1.3** | 2.1 |
| Stroke (%) | 0.0 | 0.5 | 1.1 | 1.6 | 1.5 | 1.5 |
Note: Bivariate analyses comparing each Hispanic group to non-Hispanic white individuals born in the U.S. were conducted using the test of proportions in Stata. Weighted percentages are shown; counts are not weighted. Non-Hispanic white individuals born outside of the U.S. were included in regression analysis, but for brevity, descriptive statistics for these groups are not shown. Income data come from a singly imputed dataset. P-values were adjusted using the Bonferroni correction.
p < 0.05,
p < 0.01,
p < 0.001
Table 2 displays the differences in any past-year ED use by ethnicity and acculturation from the regression model. The full output for the model is available in Table 1 of the online appendix. Our findings indicate that Hispanic individuals were less likely than US-born non-Hispanic whites to use the ED in the past year for any reason. Furthermore, these differences were more pronounced for those with lower levels of acculturation. Among the reference group of US-born non-Hispanic white individuals, the intercept indicates that the adjusted percentage of ED use was 19.4% after controlling for model covariates. Among the least acculturated Hispanic group, the adjusted percentage was 14.4 (p<0.001) percentage points lower, for an adjusted rate of 5.0%. The most acculturated Hispanic individuals were only 1.3 percentage points less likely to use the ED compared to US-born non-Hispanic whites, for an adjusted rate of 18%.
Table 2.
Adjusted percentage point difference in the likelihood of having any past-year ED use among Hispanic and non-Hispanic white non-elderly adults
| Any ED Visit Percentage point difference (Standard Error) |
Urgent ED Visit Percentage point difference (Standard Error) |
Non-Urgent ED Visit Percentage point difference (Standard Error) |
|
|---|---|---|---|
| Hispanic, in U.S. <5 years, non-citizen | −14.4*** (2.4) | −5.3** (1.8) | −9.8***† (2.0) |
| Hispanic, in U.S. 5 - <10 years, non-citizen | −7.9*** (1.4) | −2.1* (1.0) | −5.9*** (1.3) |
| Hispanic, in U.S. 10+ years, non-citizen | −10.2*** (0.9) | −3.1*** (0.7) | −7.5 *** (0.7) |
| Hispanic, naturalized citizen | −2.6** (0.9) | −0.0 (0.7) | −2.7*** (0.7) |
| Hispanic, born in U.S. | −1.3* (0.6) | −0.1 (0.5) | −1.2** (0.4) |
| Non-Hispanic white, in U.S. <5 years, non-citizen | 3.1 (3.8) | 1.8 (2.8) | 1.4 (2.3) |
| Non-Hispanic white, in U.S. 5 - <10 years, non- citizen | −5.6* (2.9) | −6.0* (1.6) | −0.6 (1.9) |
| Non-Hispanic white, in U.S. 10+ years, non-citizen | −0.7 (2.3) | 1.0 (1.6) | −2.0 (1.8) |
| Non-Hispanic white, naturalized citizen | −2.0 (1.3) | −0.5 (0.9) | −1.6 1.0) |
|
| |||
| Intercept (non-Hispanic white, born in U.S.) | 19.4% | 10.9% | 8.4% |
|
| |||
| Observations | 58,888 | 58,888 | 58,888 |
Note: Results come from weighted logistic regression models that controlled for gender, age, marital status, usual source of care status, insurance status, education level, annual income, employment status, and health status.
p < 0.05,
p < 0.01,
p < 0.001
An out-of-sample prediction occurs for non-urgent use by Hispanic non-citizens who have been in the US for less than five years. This is due to a relatively smaller cell size for this population and outcome.
Most of the relationship between Hispanic acculturation and ED use is driven by differences in non-urgent visits, as opposed to urgent ED visits. Specifically, the adjusted percentage of the least acculturated Hispanic individuals with a non-urgent visit was 9.8 (p=.000) percentage points lower than that of U.S-born non-Hispanic whites. In comparison, US-born Hispanic individuals were only 1.2 (p<0.01) percentage points less likely to have a non-urgent ED visit than their non-Hispanic counterparts.
The estimate for non-urgent ED use among the least acculturated group represents a slight out-of-sample prediction. Notably, in the bivariate analysis before controlling for any confounders, this relationship was negative and highly significant due to the very small percentage of least acculturated individuals who use the ED for non-urgent reasons. In the multivariate analysis, this negative difference was slightly exacerbated after adding measures of socioeconomic resources. More specifically, the least acculturated group is less educated, has lower income, and is more likely to be uninsured or publically insured (versus privately insured) -- and each of these is associated with greater non-urgent ED.
In an alternative specification, we collapsed the two least acculturated categories (<5 years and 5–10 years) into one group, so that all non-citizens were classified as having been in the U.S. for either less than 10 years, or for 10 or more years. In this model, both of the non-citizen groups were the least likely to have a non-urgent ED visit. This is perhaps because the 10-year threshold may not capture meaningful variation in length of stay as it relates to ED use.
In a second specification, we eliminated the separate categories for naturalized citizens, rolling these individuals into their respective “years in US” categories. The positive relationship between acculturation level and ED use remained strong in this model, with the least acculturated individuals the least likely to use the ED. Finally, we reran our original models using U.S.-born Hispanic individuals as our reference category. In this specification, the least acculturated individuals are again the least likely to use the ED, while naturalized Hispanic citizens use the ED at rates statistically similar to those of US-born Hispanic individuals.
We also conducted sensitivity analyses to assess whether interview language accounted for any of the observed associations. The NHIS collects language of interview data for only a non-random subset of about 40% of respondents (43). As a sensitivity analysis, however, we did rerun our models on the subset of individuals without missing data on this measure and included a control measure for language spoken (English only, Spanish only, Spanish and English). Our main results were robust to these sensitivity analyses, suggesting our findings may not be explained by differences in English language proficiency.
DISCUSSION
Using recent, national-level data, we find that Hispanic non-elderly adults overall use the ED for urgent visits at similar rates to those of non-Hispanic whites, and at lower rates for non-urgent visits. When Hispanic individuals in our sample are broken out into groups by acculturation level, we find a positive relationship between acculturation level and ED use, counter to our hypothesis. After adjusting for patient level characteristics, the association becomes even more prominent, with the least acculturated individuals using the ED at remarkably lower rates than non-Hispanic whites, and the most acculturated individuals using the ED at rates almost identical to non-Hispanic whites.
Several factors may explain the acculturation finding. First, the literature suggests that less acculturated individuals use fewer preventive and primary care services, compared to their more acculturated counterparts (23–33). When combined with our results, this suggests that less acculturated individuals may demand less health care overall, while more acculturated individuals appear to closely mimic their non-Hispanic white counterparts in terms of health services use.
A second explanation for our key findings concerning the association between acculturation and ED use have to do with documentation concerns. Contrary to concerns that immigrants might be straining health care resources, we find that that Hispanic non-citizens of all acculturation levels are less likely to demand care in the ED. Recent immigrants in particular appear to avoid use of the ED for non-urgent reasons. For immigrants who are undocumented, fear of discovery and subsequent deportation might play a role in the decision to seek care in the ED (44). A recent survey of ED patients at two California hospitals found that 12% of undocumented Hispanic immigrants expressed a fear of discovery in the ED (44). By virtue of the NHIS sample design, undocumented individuals are likely underrepresented in the dataset. To the extent that these individuals are represented in the sample, fear of discovery may provide one explanation for the lower rates of ED use by the least acculturated group. Furthermore, the possible underrepresentation of this group in the sample suggests that the association we estimated between acculturation and ED use may, in fact, be conservative.
Other unmeasured variables may also help explain the lower rates of ED use we estimated among the least acculturated. Though we do control for the health status elements available in the NHIS, the difference in care-seeking could be due to additional, unmeasured health needs. We also do not have measures available to assess differences in cultural views regarding how the ED is intended to be used (e.g., for true emergencies only, as opposed to for non-urgent care when other care sites aren’t open or otherwise accessible). As individuals become more acculturated to the U.S., they might also become more accustomed to American knowledge and beliefs surrounding the use of ED as a convenient alternative to other care sites (45).
Our results have several important implications for future research. First, prior research has suggested that individuals who do not have access to primary care tend to seek treatment for non–urgent conditions in the ED more frequently than those who do have a primary care provider. If less acculturated Hispanic individuals are not receiving care in the community though a USOC, it is reasonable to anticipate that they would use the ED more frequently for both non-urgent treatment (i.e., as a substitute for primary care) and urgent visits (e.g., for acute exacerbations of ambulatory care sensitive conditions). Our results suggest that this is not the case for urgent or non-urgent ED use. Future research might seek to explain whether less acculturated individuals who do not seek care in a USOC or in an ED have a lower evaluated or perceived need for health care, or if they are forgoing needed care. Further, researchers should explore whether forgone care in any setting results in poorer outcomes or greater costs when these individuals eventually come into contact with the system.
Our results further suggest that treating Hispanic individuals as one group, without accounting for heterogeneity within the population, may be masking important within-group differences in health services use. Acculturation offers one mechanism for elucidating these within-group differences, and future research should continue to explore how this construct affects demand for health services among Hispanic individuals and other minorities.
We note several limitations and caveats to our study. First, only 40% of the adults in the NHIS were asked about their ED use (46). Though this subsample of adults is randomly selected by the survey designers, we did note some differences in marital status and income between the adults who were asked about their ED use and those who were not. Specifically, those asked about their ED use were less likely to be married (55% vs. 73%) or have an income over $75,000 (31% vs. 41%). Additionally, there are limitations related to measuring health care need. First, self-reported diagnoses (e.g., diabetes) can be a biased indicator of need, since individuals with inadequate access to health care are less likely to receive a diagnosis from a provider. Second, due to language and other cultural norms, the same value of self-reported health status may be associated with a higher level of actual health status among Spanish-speaking Hispanics than among non-Hispanic Whites value (e.g., “fair” in English denotes subpar health, but its translation [“regular”] in Spanish denotes okay health) (47, 48). Since less acculturated individuals are less likely to have a USOC, and more likely to take the survey in Spanish, the overall direction of bias resulting from these measurement errors is unknown.
A final limitation has to do with the way we proxy for acculturation, a construct that is difficult to measure (49, 50) . Single-dimension proxy measures have been criticized as being limited in scope or sensitivity. However, they are often the only measures available in large survey datasets, such as the NHIS, and are frequently used in the literature for that reason. Future studies should explore the relationship between acculturation and ED use by employing more comprehensive acculturation scales, such as those described by Thomson and Hoffman, should these data become available (49).
Despite these limitations, this study provides the first known examination of the association between acculturation and ED use, and provides updated, nationally generalizable insight on the relationship between Hispanic ethnicity and ED use. Overall, our results suggest Hispanic individuals in general, and recent immigrants in particular, are not disproportionally contributing to ED use. In fact, the converse appears to be true: recent immigrants demand the least care from the ED, especially for non-urgent conditions.
Supplementary Material
Footnotes
Disclosures
Dr. Cummings’ effort was supported by the National Institute of Mental Health (K01MH095823). The authors have no conflicts of interest to disclose. This paper was presented at AcademyHealth’s Annual Research Meeting, June 2015, Minneapolis, MN, and the Southern Economic Association’s Annual Meeting, November 2015, New Orleans, LA.
Contributor Information
Lindsay Allen, Rollins School of Public Health, Emory University, 1518 Clifton Road, Atlanta, GA.
Janet Cummings, Rollins School of Public Health, Emory University, 1518 Clifton Road, Atlanta, GA.
References
- 1.Niska RB, Farida, Jianmin Xu. National Health Statistics Reports. 2010. National Hospital Ambulatory Medical Care Survey: 2007 Emergency Department Summary; p. 26. [PubMed] [Google Scholar]
- 2.Young GP, Wagner MB, Kellermann AL, et al. Ambulatory visits to hospital emergency departments. Patterns and reasons for use. 24 Hours in the ED Study Group. JAMA : the journal of the American Medical Association. 1996;276:460–465. doi: 10.1001/jama.276.6.460. [DOI] [PubMed] [Google Scholar]
- 3.Weinick RM, Burns RM, Mehrotra A. Many emergency department visits could be managed at urgent care centers and retail clinics. Health affairs. 2010;29:1630–1636. doi: 10.1377/hlthaff.2009.0748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hospital-Based Emergency Care: At the Breaking Point. The National Academies Press; 2007. [Google Scholar]
- 5.Uscher-Pines L, Pines J, Kellermann A, et al. Emergency department visits for nonurgent conditions: systematic literature review. The American journal of managed care. 2013;19:47–59. [PMC free article] [PubMed] [Google Scholar]
- 6.Derlet RW, Richards JR. Overcrowding in the nation's emergency departments: complex causes and disturbing effects. Annals of emergency medicine. 2000;35:63–68. doi: 10.1016/s0196-0644(00)70105-3. [DOI] [PubMed] [Google Scholar]
- 7.Smulowitz PB, O’Malley J, Yang X, et al. Increased Use of the Emergency Department After Health Care Reform in Massachusetts. Annals of emergency medicine. 2014;64:107–115. doi: 10.1016/j.annemergmed.2014.02.011. [DOI] [PubMed] [Google Scholar]
- 8.Medford-Davis LN, Eswaran V, Shah RM, et al. The Patient Protection and Affordable Care Act's Effect on Emergency Medicine: A Synthesis of the Data. Annals of emergency medicine. 2015 doi: 10.1016/j.annemergmed.2015.04.007. [DOI] [PubMed] [Google Scholar]
- 9.Cheung PT, Wiler JL, Ginde AA. Changes in barriers to primary care and emergency department utilization. Archives of Internal Medicine. 2011;171:1393–1400. doi: 10.1001/archinternmed.2011.350. [DOI] [PubMed] [Google Scholar]
- 10.AHRQ Health Care Innovations Exchange. Reducing Non-Urgent Emergency Services. 2015. [Google Scholar]
- 11.Subcommittee on Primary Health and Aging. Subcommittee Hearing - Diverting Non-urgent Emergency Room Use: Can It Provide Better Care and Lower Costs? 2011. [Google Scholar]
- 12.LaCalle E, Rabin E. Frequent Users of Emergency Departments: The Myths, the Data, and the Policy Implications. Annals of emergency medicine. 2010;56:42–48. doi: 10.1016/j.annemergmed.2010.01.032. [DOI] [PubMed] [Google Scholar]
- 13.Fox M. Who's Packing ERs? Not the Uninsured. 2010 [Google Scholar]
- 14.Millerick SG. New Aetna Study Finds African Americans and Hispanics Use Emergency Room for Asthma Incidents More Often Than Whites. 2010. [Google Scholar]
- 15.Davidson LJ, Elaine, Collins Lois. The myths and realities of illegal immigration. 2010. Fact or fiction? [Google Scholar]
- 16.LaJeunesse WLA. Emergency Rooms Full of Illegal Immigrants. 2005. [Google Scholar]
- 17.Cunningham PJ, Clancy CM, Cohen JW, et al. The use of hospital emergency departments for nonurgent health problems: a national perspective. Medical care research and review : MCRR. 1995;52:453–474. doi: 10.1177/107755879505200402. [DOI] [PubMed] [Google Scholar]
- 18.Villani J, Mortensen K. Nonemergent emergency department use among patients with a usual source of care. Journal of the American Board of Family Medicine : JABFM. 2013;26:680–691. doi: 10.3122/jabfm.2013.06.120327. [DOI] [PubMed] [Google Scholar]
- 19.Hong R, Baumann BM, Boudreaux ED. The emergency department for routine healthcare: Race/ethnicity, socioeconomic status, and perceptual factors. The Journal of emergency medicine. 2007;32:149–158. doi: 10.1016/j.jemermed.2006.05.042. [DOI] [PubMed] [Google Scholar]
- 20.Centers for Disease Control and Prevention. National Hospital Ambulatory Medical Care Survey: 2011 Emergency Department Summary Tables. 2011. [Google Scholar]
- 21.Weinick RM, Jacobs EA, Stone LC, et al. Hispanic healthcare disparities: challenging the myth of a monolithic Hispanic population. Medical care. 2004;42:313–320. doi: 10.1097/01.mlr.0000118705.27241.7c. [DOI] [PubMed] [Google Scholar]
- 22.Lara M, Gamboa C, Kahramanian MI, et al. Acculturation and Latino health in the United States: a review of the literature and its sociopolitical context. Annual review of public health. 2005;26:367–397. doi: 10.1146/annurev.publhealth.26.021304.144615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Thamer M, Richard C, Casebeer AW, et al. Health insurance coverage among foreign-born US residents: the impact of race, ethnicity, and length of residence. American journal of public health. 1997;87:96–102. doi: 10.2105/ajph.87.1.96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Granados G, Puvvula J, Berman N, et al. Health care for Latino children: impact of child and parental birthplace on insurance status and access to health services. American journal of public health. 2001;91:1806–1807. doi: 10.2105/ajph.91.11.1806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Solis JM, Marks G, Garcia M, et al. Acculturation, access to care, and use of preventive services by Hispanics: findings from HHANES 1982–84. American journal of public health. 1990;80(Suppl):11–19. doi: 10.2105/ajph.80.suppl.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wells KB, Golding JM, Hough RL, et al. Acculturation and the probability of use of health services by Mexican Americans. Health services research. 1989;24:237–257. [PMC free article] [PubMed] [Google Scholar]
- 27.Clark L. Mexican-origin mothers' experiences using children's health care services. Western journal of nursing research. 2002;24:159–179. doi: 10.1177/01939450222045815. [DOI] [PubMed] [Google Scholar]
- 28.Anderson LM, Wood DL, Sherbourne CD. Maternal acculturation and childhood immunization levels among children in Latino families in Los Angeles. American journal of public health. 1997;87:2018–2021. doi: 10.2105/ajph.87.12.2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chesney AP, Chavira JA, Hall RP, et al. Barriers to medical care of Mexican-Americans: the role of social class, acculturation, and social isolation. Medical care. 1982;20:883–891. doi: 10.1097/00005650-198209000-00002. [DOI] [PubMed] [Google Scholar]
- 30.Findley SE, Irigoyen M, Schulman A. Children on the move and vaccination coverage in a low-income, urban Latino population. American journal of public health. 1999;89:1728–1731. doi: 10.2105/ajph.89.11.1728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hu DJ, Covell RM. Health care usage by Hispanic outpatients as function of primary language. The Western journal of medicine. 1986;144:490–493. [PMC free article] [PubMed] [Google Scholar]
- 32.Marks G, Garcia M, Solis JM. Health risk behaviors of Hispanics in the United States: findings from HHANES, 1982–84. American journal of public health. 1990;80(Suppl):20–26. doi: 10.2105/ajph.80.suppl.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Moore P, Fenlon N, Hepworth JT. Indicators of differences in immunization rates of Mexican American and white non-Hispanic infants in a Medicaid managed care system. Public health nursing (Boston, Mass) 1996;13:21–30. doi: 10.1111/j.1525-1446.1996.tb00214.x. [DOI] [PubMed] [Google Scholar]
- 34.Mohanty SA, Woolhandler S, Himmelstein DU, et al. Health care expenditures of immigrants in the United States: a nationally representative analysis. American journal of public health. 2005;95:1431. doi: 10.2105/AJPH.2004.044602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tarraf W, Vega W, González HM. Emergency department services use among immigrant and non-immigrant groups in the United States. Journal of Immigrant and Minority Health. 2014;16:595–606. doi: 10.1007/s10903-013-9802-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Nandi A, Galea S, Lopez G, et al. Access to and use of health services among undocumented Mexican immigrants in a US urban area. American journal of public health. 2008;98:2011. doi: 10.2105/AJPH.2006.096222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ortega AN, Fang H, Perez VH, et al. Health care access, use of services, and experiences among undocumented Mexicans and other Latinos. Archives of Internal Medicine. 2007;167:2354–2360. doi: 10.1001/archinte.167.21.2354. [DOI] [PubMed] [Google Scholar]
- 38.Centers for Disease Control and Prevention. About the National Health Interview Survey. 2012 Available at: http://www.cdc.gov/nchs/nhis/about_nhis.htm.
- 39.Sarver JH, Cydulka RK, Baker DW. Usual source of care and nonurgent emergency department use. Academic emergency medicine : official journal of the Society for Academic Emergency Medicine. 2002;9:916–923. doi: 10.1111/j.1553-2712.2002.tb02193.x. [DOI] [PubMed] [Google Scholar]
- 40.Mansfield W. Measuring Acculturation in the US Hispanic Population Wendy Mansfield, Jordon Peugh, Jannet Torres, and Tom Wells Knowledge Networks. [Google Scholar]
- 41.Thomson MD, Hoffman-Goetz L. Defining and measuring acculturation: A systematic review of public health studies with Hispanic populations in the United States. Social Science & Medicine. 2009;69:983–991. doi: 10.1016/j.socscimed.2009.05.011. [DOI] [PubMed] [Google Scholar]
- 42.Andersen RM. Revisiting the Behavioral Model and Access to Medical Care: Does it Matter? Journal of Health and Social Behavior. 1995;36:1–10. [PubMed] [Google Scholar]
- 43.United States Census Bureau. National Health Interview Survey CAPI Manual for NHIS Field Representatives. 2013. [Google Scholar]
- 44.Maldonado CZ, Rodriguez RM, Torres JR, et al. Fear of discovery among Latino immigrants presenting to the emergency department. Academic emergency medicine : official journal of the Society for Academic Emergency Medicine. 2013;20:155–161. doi: 10.1111/acem.12079. [DOI] [PubMed] [Google Scholar]
- 45.Uscher-Pines L, Pines J, Kellermann A, et al. Deciding to Visit the Emergency Department for Non-Urgent Conditions: A Systematic Review of the Literature. The American journal of managed care. 2013;19:47. [PMC free article] [PubMed] [Google Scholar]
- 46.Division of Health Interview Statistics. 2012 National Health Interview Survey Public Use Data Release. [Accessed 4/18/2014];NHIS Survey Description 2013. 2014 Available at: ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/Dataset_Documentation/NHIS/2012/srvydesc.pdf.
- 47.Sudano JJ, Perzynski A, Love TE, et al. Measuring disparities: bias in the Short Form-36v2 among Spanish-speaking medical patients. Medical care. 2011;49:480–488. doi: 10.1097/MLR.0b013e31820fb944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Viruell-Fuentes EA, Morenoff JD, Williams DR, et al. Language of Interview, Self-Rated Health, and the Other Latino Health Puzzle. American journal of public health. 2011;101:1306–1313. doi: 10.2105/AJPH.2009.175455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Thomson MD, Hoffman-Goetz L. Defining and measuring acculturation: a systematic review of public health studies with Hispanic populations in the United States. Social science & medicine (1982) 2009;69:983–991. doi: 10.1016/j.socscimed.2009.05.011. [DOI] [PubMed] [Google Scholar]
- 50.Alegria M. The challenge of acculturation measures: what are we missing? A commentary on Thomson & Hoffman-Goetz Social science & medicine (1982) 2009;69:996–998. doi: 10.1016/j.socscimed.2009.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.