Abstract
We report a case of diffuse bilateral retinal and optic nerve sheath hemorrhages in an 8-week-old boy who was found unresponsive. The child underwent prolonged cardiopulmonary resuscitation and was found on admission to have a coagulopathy. An autopsy determined the cause of death to be a myocardial infarct in the distribution of an anomalous coronary artery. This case demonstrates the difficulty that may occur in establishing whether child abuse caused death in the setting of another potential cause of mortality.
Abusive head trauma (AHT) is the leading cause of death among victims of child abuse.1 It is characterized by injury to the skull and/or brain due to blunt impact or shaking. Characteristic findings include retinal and intracranial hemorrhage, cerebral edema, and/or fractures, all of which may or may not be present. Ophthalmologists are often consulted in cases of suspected abuse to evaluate for retinal hemorrhages which are reported to be present in 50%–100% of cases.1–3 Many cases of AHT lack external signs of trauma and are unwitnessed other than by the perpetrator. When evaluating retinal hemorrhages, it is important to consider the differential diagnosis. We present a case of diffuse bilateral retinal hemorrhages in an infant determined by the medical examiner to have died as a result of a congenital cardiac anomaly.
Case Report
The ophthalmology service at Emory University was consulted in a suspected case of AHT involving an 8-week-old boy. He was born full-term and had no known medical history, although family members reported that he slept “more than any infant they had ever known.” On the day of presentation, the child was cared for at home by his father, grandmother, and aunt. His mother reported finding the child still sleeping upon returning home from work. At the time he was found unconscious later in the evening, the child was lying in bed with his father. The father picked up the child to feed him and found him limp. The mother called the police and a nurse who lived nearby. The neighbor began cardiopulomonary resuscitation (CPR) with chest compressions. Emergency personnel found the patient in asystole and continued CPR with chest compressions in the field and then in the emergency room. The total time of chest compressions was approximately 35 minutes. Labs drawn in the first hour of admission revealed evidence of disseminated intravascular coagulation and anemia, with an activated partial thromboplastin time of 109.4 (normal, 26.8–35.6) and hemoglobin 6.4 (normal, 10.0–15.0). D-dimers, checked 11 hours after admission, were >10,000. During changing of the endotracheal tube 3 hours after admission, the child required further CPR, with compressions lasting 18 minutes.
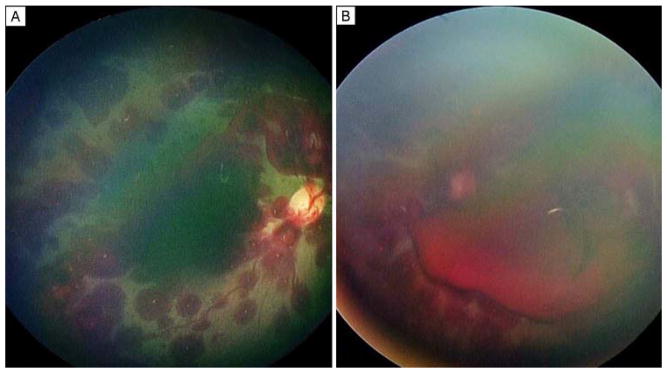
On ophthalmological examination, the infant had fixed, dilated pupils. Funduscopic examination of both eyes conducted 10 hours after admission (Figure 1) revealed extensive intraretinal hemorrhages from the posterior pole to the ora serrata as well preretinal hemorrhages in the right eye and a subhyaloid hemorrhage in the left eye.
FIG 1.
Diffuse intraretinal hemorrhages throughout the posterior pole of the right and left eyes. Preretinal hemorrhage is noted adjacent to the optic nerve in the right eye (A), and a large subhyaloid hemorrhage is present in the left eye (B).
Computed tomography (CT) demonstrated hypoxic-ischemic brain injury. No subdural or subarachnoid hemorrhages were reported. A skeletal survey was negative for fractures.
The infant remained in poor condition with anoxic encephalopathy and was declared dead 4 days after admission. An autopsy was performed. There were no external signs of trauma. No bruising was noted under the surface of the scalp. The brain was swollen, consistent with anoxic encephalopathy. The subdural and subarachnoid spaces were free of hemorrhage. Neck dissection and spinal cord examination demonstrated focal minimal hemorrhage consistent with autopsy artifact. On microscopic examination, both eyes had subdural hemorrhage along the optic nerves with focal intradural hemorrhages in the right nerve. Marked hemorrhage was present throughout the nerve fiber layer of the retina (Figure 2), extending to the ora serrata in both eyes. The optic nerves and globes were removed without histological sectioning of orbital tissues. Gross examination of orbital soft tissue revealed multiple petechial hemorrhages.
FIG 2.
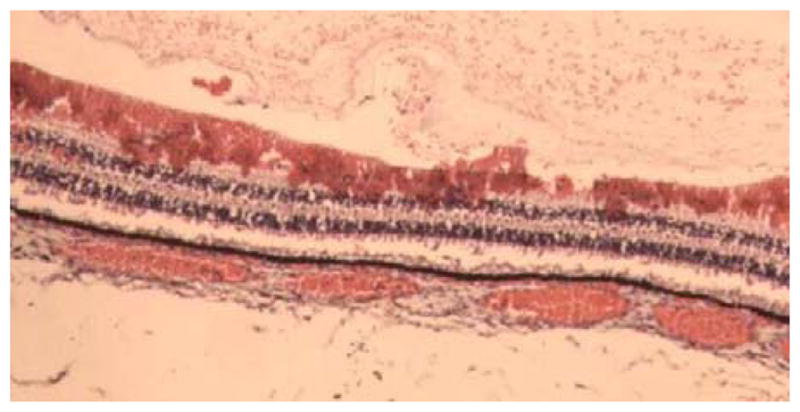
Histology showing hemorrhage throughout the nerve fiber layer.
Cardiac examination revealed an anomalous origin of the right coronary artery (RCA) within the left sinus of Valsalva. Histology demonstrated an associated subacute infarct adjacent to the atrioventricular node.
The medical examiner determined that the cause of death was cardiac arrest due to myocardial infarct in the region supplied by the anomalous artery with contributing anemia. Investigations by the police and medical examiner failed to substantiate abuse based on the accounts of multiple witnesses in the home throughout the day and evening, but the Child Protection Team was suspicious that abuse caused the injuries because of the extent of the retinal hemorrhages.
Discussion
We describe a case of diffuse retinal and optic nerve sheath hemorrhages in an 8-week-old boy whose death was ruled secondary to a congenital cardiac anomaly; autopsy demonstrated a myocardial infarct in the territory of an anomalous vessel. An anomalous origin of the RCA from the left sinus of Valsalva has been recognized as a cause of sudden cardiac arrest in the young. Fineschi and colleagues4 reported a 13-month-old infant who was found unresponsive in his crib. Six months prior to this he started to have episodes of apnea and seizures. A work-up that included a cardiology examination was normal. Autosopy revealed an RCA arising from the left sinus of Valsalva. The risk of sudden death associated with RCA anomalies has been reported to be as high as 20%–45%.5
The child was examined in the hospital by the child-abuse team, which concluded that the eye findings and unexplained cardiac arrest were suspicious for AHT. Forensic and radiographic examination failed to reveal further evidence of abuse. No intracranial subdural hemorrhages or bony fractures were found on CT scan or autopsy. Subdural hemorrhages are reported to be the most common sign in victims of AHT.1
The patient’s lab results support a diagnosis of disseminated intravascular coagulation (DIC) on admission, likely secondary to cardiogenic or hypotensive shock. Abuse or myocardial infarct could have caused DIC. There are case reports in the literature describing infantile retinal hemorrhages in the setting of coagulopathy.6,7 Agrawal and colleagues8 investigated the prevalence of retinal hemorrhages in critically ill children, noting retinal hemorrhages in 15.1% of 159 patients. The majority were described as mild or moderate in severity, although 6 patients had severe multilayered hemorrhages.
The consensus in the literature is that CPR is not a significant risk factor for severe retinal hemorrhages.3,8,9 However, isolated case reports exist of severe retinal hemorrhages following CPR. Kramer and Goldstein10 reported a case of diffuse intraretinal and subhyaloid hemorrhages in a 17-month old infant following in-hospital CPR.
The Child Protection Team suspected abuse based on the retinal hemorrhages. The medical examiner considered the autopsy findings, laboratory results, and investigation of the circumstances preceding the death before ruling death to be of natural causes. In a case such as this, it may be difficult to determine whether abuse led to myocardial infarction and subsequent coagulopathy or whether the infant suffered an infarct and then developed signs of cerebral hypoxia and retinal hemorrhages as a result of complications of the infarct and its treatment.
Acknowledgments
Supported in part by NIH Departmental Core Grant EY006360 and Research to Prevent Blindness, Inc, New York, New York.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Lopes NR, Eisenstein E, Williams LC. Abusive head trauma in children: a literature review. J Pediatr (Rio J) 2013;89:426–33. doi: 10.1016/j.jped.2013.01.011. [DOI] [PubMed] [Google Scholar]
- 2.Bhardwaj G, Chowdhury V, Jacobs MB, Moran KT, Martin FJ, Coroneo MT. A systematic review of the diagnostic accuracy of ocular signs in pediatric abusive head trauma. Ophthalmology. 2010;117:983–92. doi: 10.1016/j.ophtha.2009.09.040. [DOI] [PubMed] [Google Scholar]
- 3.Binenbaum G, Forbes BJ. The eye in child abuse: key points on retinal hemorrhages and abusive head trauma. Pediatr Radiol. 2014;44(Suppl 4):S571–7. doi: 10.1007/s00247-014-3107-9. [DOI] [PubMed] [Google Scholar]
- 4.Fineschi V, Maresi E, DiPadua M, Riezzo I, Neri M. Sudden cardiac death due to anomalous origin of the right coronary artery: a case report in a child. Int J Cardiol. 2006;108:426–8. doi: 10.1016/j.ijcard.2005.03.076. [DOI] [PubMed] [Google Scholar]
- 5.Burke A, Tavora F. Practical Cardiovascular Pathology. Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins; 2011. [Google Scholar]
- 6.De Leeuw M, Beuls E, Jorens P. Delta-storage pool disease as a mimic of abusive head trauma in a 7-month-old baby: a case report. J Forensic Leg Med. 2013;20:520–21. doi: 10.1016/j.jflm.2013.03.021. [DOI] [PubMed] [Google Scholar]
- 7.Hendrickson DJ, Knisely AS, Coulter K, et al. An inborn error of bile salt transport with features mimicking abusive head trauma. Child Abuse Negl. 2010;34:472–6. doi: 10.1016/j.chiabu.2009.11.008. [DOI] [PubMed] [Google Scholar]
- 8.Agrawal S, Peters MJ, Adams GG, Pierce CM. Prevalence of retinal hemorrhages in critically ill children. Pediatrics. 2012;129:1388–96. doi: 10.1542/peds.2011-2772. [DOI] [PubMed] [Google Scholar]
- 9.Odom A, Christ E, Kerr N, et al. Prevalence of retinal hemorrhages in pediatric patients after in-hospital cardiopulmonary resuscitation: a prospective study. Pediatrics. 1997;99:e3. doi: 10.1542/peds.99.6.e3. [DOI] [PubMed] [Google Scholar]
- 10.Kramer K, Goldstein B. Retinal hemorrhages following cardiopulmonary resuscitation. Clin Pediatr. 1993;32:366–8. doi: 10.1177/000992289303200610. [DOI] [PubMed] [Google Scholar]