Abstract
Small and rural hospitals face special challenges to implement and sustain organization-wide quality improvement (QI) initiatives due to limited resources and infrastructures. We studied the implementation of TeamSTEPPS, a national QI initiative, in 14 critical access hospitals. Drawing on QI and organization development theories, we propose five strategic preparation steps for TeamSTEPPS: assess needs, reflect on the context, set goals, develop a shared understanding, and select change agents. We explore how hospitals’ practices correspond to suggested best practices by analyzing qualitative data collected through quarterly interviews with key informants. We find that the level of deliberation was a key factor that differentiated hospitals’ practices. Hospitals that were more deliberate in preparing for the five strategic steps were more likely to experience engagement, perceive efficacy, foresee and manage barriers, and achieve progress during implementation. We discuss potential steps that hospitals may take to better prepare for TeamSTEPPS implementation.
Keywords: TeamSTEPPS, preparation strategy, implementation process, critical access hospital, qualitative research
Background
In a review of quality improvement (QI) efforts in the U.S. health care system, Chassin and Loeb (2011, p. 559) stated that “although many small successes have been achieved, they have often been short-lived. And they have not been enough to solve complex, persistent, and deeply rooted quality and safety problems.” Small and rural hospitals face additional challenges in implementing and sustaining organization-wide QI initiatives because they often have inadequate infrastructures to support QI planning and limited resources to subsidize QI activities (Casey & Moscovice, 2004; Paez, Schur, Zhao, & Lucado, 2012). Rooted in the QI and organization development (OD) literature, certain change management strategies may help these hospitals better engage in organization-wide QI initiatives within existing conditions (Bartunek, Balogun, & Do, 2011). By focusing on managing the implementation process, this perspective seeks to identify strategies that can guide organizations in deploying and sustaining effective QI solutions, which is critical for achieving high reliability and systematic improvement (Chassin & Loeb, 2011). In this study, we explore such strategies by examining the implementation of Team Strategies and Tools to Enhance Performance and Patient Safety (TeamSTEPPS), a national initiative for optimizing care quality and patient safety, in 14 critical access hospitals (CAHs).
TeamSTEPPS was developed by the Agency for Healthcare Research and Quality (AHRQ) and the Department of Defense as an evidence-based teamwork system for improving communication and teamwork among health care providers to enhance team performance and patient safety (AHRQ, 2013a; King et al., 2008). The scope of the intervention is broad because its ultimate goal is to optimize team performance and change patient safety culture in the entire organization, and complex because it involves not only training and multiple tools but also strategies and implementation guidelines for initiating and sustaining organization-wide changes (King et al., 2008). This can create challenges for organizations, especially those with limited resources and experience in managing large-scale, organization-wide QI efforts to initiate and sustain change. TeamSTEPPS is also an adaptable program, as hospitals are encouraged to tailor the implementation to fit their needs and contexts. This adds another layer of complexity because the existing guidelines do not provide specific recommendations on how to customize while maintaining rigor. Thus, hospitals employ a variety of approaches in preparing for and managing this change initiative, which provides an excellent arena for examining the relationship between preparation strategies and implementation dynamics and outcomes.
In the following sections, we establish our conceptual framework by identifying key factors that affect the implementation and sustainment of organization-wide change initiatives and proposing relevant preparation strategies for TeamSTEPPS in small and rural hospitals. We focus specifically on the preparation stage (i.e., before and during the initiation of the implementation) because decisions made at this stage can have a profound impact on subsequent implementation dynamics and outcomes. We then analyze data obtained from interviews with key informants at the 14 CAHs in order to explore how their approaches fit with suggested best practices for change management. We conclude with a discussion of potential steps that small and rural hospitals can take to better prepare for implementing TeamSTEPPS and other change initiatives.
New Contributions
Our study makes several contributions by exploring a new research question: how can health care organizations with limited resources and infrastructures prepare to implement and sustain organization-wide QI initiatives? First, because best practices suggested by existing theories of change (e.g., Kaluzny & Hernandez, 1983; O’Brien et al., 1995; Weiner, 2009) often require conditions that are difficult to improve expeditiously, we aimed to identify and examine strategies that can better engage organizations in QI initiatives within existing, restricted conditions. Second, through a prospective approach that followed 14 hospitals for 9 months as they initiated TeamSTEPPS, we gathered real-time information on implementation processes and events that allowed us to go beyond a simple assessment of outcomes and identify strengths and deficits in implementation practices.
Conceptual Framework
We draw on theories of organization-wide QI (O’Brien et al., 1995; Shortell, Bennett, & Byck, 1998), OD and Large Group Interventions (Bartunek et al., 2011; Bunker & Alban, 1997), and related organizational literature to formulate a conceptual framework related to preparation strategies for implementing change initiatives such as TeamSTEPPS.
From the organization-wide QI perspective, O’Brien et al. (1995) developed a model that identified four interrelated dimensions necessary for achieving lasting improvement: technical, cultural, strategic, and structural. The technical dimension refers to tools and techniques used in QI activities. The cultural dimension consists of QI-related beliefs, values, norms, and behaviors. The strategic dimension concerns the linkage between the QI effort and the organization’s overall strategy. The structural dimension includes both QI-specific structures (e.g., committees) and broader structural elements for supporting QI (e.g., information system). A number of empirical studies have provided evidence supporting the premise of these dimensions in affecting organization-level improvement (e.g., Gustafson et al., 2003; Shortell et al., 1995; Weiner, Alexander, Baker, Shortell, & Becker, 2006). Shortell et al. (1998) argued that the four QI dimensions must all be present for significant improvement to occur.
OD research has long focused on the strategic, cognitive, and emotional aspects of change process and offered insights regarding how to manage these aspects (Katz & Kahn, 1966; Kotter, 1996; Lawler & Worley, 2011). First, to engage an entire organization in the change process, leaders need to focus on strategizing the planned change by implementing interventions that are strategically important (Dutton, Ashford, O’Neill, & Lawrence, 2001), lay out a future state that is desirable to change recipients (Bunker & Alban, 1997), and create an organizational context that enables change-inducing behaviors (Burgelman, 1983). Second, leaders need to facilitate the development of change recipients’ collective understanding of what the change is about and what steps must be taken to make the change happen; that is, to facilitate change-related sensemaking (Gioia & Chittipeddi, 1991; Isabella, 1990; Weick, 1995). Third, leaders also need to manage emotions of the change recipients to reduce resistance (Ford, Ford, & D’Amelio, 2008; Huy, 2002; Sanchez-Burks & Huy, 2009). These three aspects are consistent with the organization-wide QI approach, as Shortell et al. (1998) noted that the full potential of change initiatives can only be realized when individuals and organizations are willing and able to manage and successfully meet physical, cognitive, and emotional demands.
Noticeable synergies emerge from the QI and OD theories regarding strategic, cognitive, and emotional factors pertinent to creating and sustaining organization-wide change. As shown in Table 1, we combine the three broad OD aspects with the four QI dimensions to create a conceptual framework that proposes five strategic steps that small and rural hospitals can engage during the preparation stage of TeamSTEPPS: assess needs, reflect on the context, set goals, develop a shared understanding, and select change agents. Table 1 also includes suggestions for how small and rural hospitals can employ these strategic steps to facilitate organization-wide change in general and TeamSTEPPS in particular.
Table 1.
Preparation Strategies for TeamSTEPPS: A Conceptual Framework.
| QI/OD key factor | Strategic preparation steps | Implications for organization-wide change |
|---|---|---|
| Strategizing |
Assess needs
|
|
Reflect on the context
|
|
|
Set goals
|
|
|
| Sensemaking |
Develop a shared understanding
|
|
| Managing emotions |
Select change agents
|
|
Note. QI = quality improvement; OD = organization development.
First, assessing needs involves answering the questions: what change is needed and why is the intervention necessary? This step corresponds to the strategic dimension of QI and entails identifying what changes are strategically important (Dutton et al., 2001). To prepare for TeamSTEPPS, change leaders need to define the organization’s strategic goals and priorities, use data (e.g., performance, safety events, safety culture survey) to identify the needs for change in light of the goals and priorities, and assess the fit between TeamSTEPPS and the identified needs. With only limited resources to dispense, this step is critical for small and rural hospitals because it ensures that the hospital invests in the right intervention to achieve improvement where it is most needed.
Second, change leaders need to reflect on the organizational context and assess how it will affect the planned implementation, especially through “autonomous behaviors” that induce or hinder the change process (Burgelman, 1983). This step corresponds to the cultural dimension of QI. Leaders need to reflect on the cultural context, the timing for implementation, and the relationship between TeamSTEPPS and other organizational initiatives. Based on these reflections, change leaders may customize the implementation plan to accommodate the need for improving the culture, avoiding competing priorities, or creating a synergetic plan for complementary initiatives. In small and rural hospitals, this step may even lead to postponing the implementation if the context is not favorable and cannot be readily adjusted.
Third, setting goals involves defining implementation scope and identifying what, when, and where change ought to occur. This step corresponds to the strategic dimension of QI. Specific, attainable, and challenging goals motivate behaviors and direct attention and effort toward goal-relevant actions (Locke & Latham, 1990). In small and rural hospitals, QI activities are often added to change agents’ daily obligations. Setting specific and attainable goals helps leaders engage and motivate change agents, direct effort toward implementation-related activities, and create a sense of urgency. It also facilitates the measurement and celebration of implementation progress and results (Kotter, 1996).
Fourth, organizational change is a continuous sensemaking process in which individuals understand the change by connecting new ideas or realities with existing interpretative schemas (Bartunek et al., 2011). Sensemaking corresponds to the technical dimension of QI as it develops organization members’ knowledge about the intended change. During the preparation stage, change leaders need to develop a shared understanding of the planned intervention and its objective and pathway by amply communicating such information with change agents. This reduces resistance and cynicism toward change resulting from confusion and misunderstanding (Reichers, Wanous, & Austin, 1997). Furthermore, a shared understanding may facilitate the engagement of change leaders and agents in the strategizing steps.
Fifth, to anticipate and manage emotional aspects of change processes, change leaders can follow the final strategic step of intentionally selecting change agents who are willing and able to manage the emotional demands of the change initiative. This step entails assessing the alignment between change agents’ personal goals and those of the planned intervention and change agents’ emotional intelligence and resilience. For TeamSTEPPS, this preparation step partly pertains to the structural dimension of QI because, by design, the selected change agents will form the change team responsible for creating and spreading the change throughout the organization. The small and rural hospital context accentuates the importance of selecting change agents and developing a shared understanding because these hospitals usually do not have designated personnel or resources for implementing complex, large-scale initiatives like TeamSTEPPS.
The five strategic steps discussed above bear certain resemblance with the concept of organizational readiness for change. Weiner (2009) conceptualized organizational readiness as organizational members’ shared commitment and perceived efficacy for change. It is well accepted that readiness is a necessary condition for success in implementing planned change initiatives (Armenakis & Harris, 2009). However, current research on organizational readiness generally focuses on what organizations have (e.g., culture, resources, structure). By contrast, our discussion on preparation strategies focuses on what organizations and its members can do. The five proposed strategic steps outline how to customize initiation of an intervention to fit an organization’s existing conditions; thus, they are less dependent on resources and infrastructures. We speculate that the five preparation steps will contribute to building a state of strategic preparedness for change. Strategic preparedness refers to organization members’ collective understanding of what and why change is needed and how it can be realized. This requires a high level of mindfulness for organization members initiating and leading change (Gärtner, 2013; Weick, Sutcliffe, & Obstfeld, 1999). Our proposition is that, given TeamSTEPPS’ adaptability, hospitals with greater strategic preparedness as reflected in careful execution of the five strategic preparation steps will achieve better implementation dynamics and outcomes.
Method
Sample
Using a longitudinal qualitative research design, we prospectively studied TeamSTEPPS implementation in 14 CAHs. Consistent with implementation guidelines, we considered participation in the TeamSTEPPS Master Trainer training as the marker for initiating the implementation. In 2011 and 2012, a total of 14 Iowa CAHs registered for and completed the two-day Master Trainer training offered by a regional training organization free of charge. During the first day of a typical training, an experienced trainer introduced concepts, strategies, and tools related to teamwork and communication using the AHRQ TeamSTEPPS curriculum. Change-related topics including John Kotter’s (Kotter, 1996; Kotter & Rathgeber, 2006) model of organizational change, implementation timeline, and readiness assessment were discussed. During the second day, each hospital’s change team developed an initial plan for how to implement TeamSTEPPS in their own facility, followed by a discussion facilitated by the trainer. The TeamSTEPPS curriculum including standard training modules and presentations were provided to the change teams to help them train frontline staff at their own hospital.
Data Collection
Senior project personnel visited each participating hospital quarterly to gather information on their implementation processes and experiences. Interviewees usually involved change agents (e.g., change team members who received the Master Trainer training) and executive sponsors (e.g., administrators who supported the implementation, and may or may not have received the training). Across the 14 hospitals, quarterly interviews were conducted with 38 change agents, 28 executive sponsors, and 13 other staff involved in the implementation, which resulted in a total of 157 interviews during the first 9 months. The interviews lasted 30 to 45 minutes and, although conversational in nature, addressed the information points identified in a semistructured interview guide. The key information points included visions and goals, implementation events such as staff training and tool implementation, facilitators and barriers, outcomes and evaluations, and progress and sustainment. The first quarterly interview also retrospectively collected information on why the CAHs initiated TeamSTEPPS and how they engaged in preparing for implementation before and during the initiation of the intervention (i.e., the preparation stage). All interviews were recorded and transcribed. The interview guide and protocol were approved by the University of Iowa Institutional Review Board.
Coding
Transcripts were anonymized prior to coding and analyses by removing all hospital and interviewee identities. Based on the conceptual framework, we developed a coding scheme, which consisted of the five preparation steps. Two coders independently coded the transcripts for all hospitals. In this step, the coders identified relevant content and extracted transcript segments for each of the five preparation steps. For example, to code content for change agent selection, the coders extracted any transcript segment explaining “considerations involved in selecting each change team member, including team members’ own perceptions of why they were selected.” We organized the transcript segments chronologically in a spreadsheet for each hospital. One of the investigators reviewed the coded transcripts for each hospital. When there was a discrepancy in the codes (i.e., a transcript segment and its corresponding preparation step), the investigator and the coders jointly reviewed the relevant transcripts within their original context to reconcile until full consensus was reached.
Analyses
We sought patterns of practices across hospitals regarding what differentiated their thinking and acting in preparing for the implementation. Two investigators reviewed the coded transcripts for each hospital and independently identified themes manifested in the hospitals’ practices. Themes were iteratively debated until the investigators reached consensus. By comparing across hospitals regarding their practices in each of the preparation steps, the level of deliberation demonstrated by the change leaders and agents emerged as a major differentiator for preparation practices. Table 2 provides a summary of the themes that emerged from the hospitals’ preparation practices.
Table 2.
Key Characteristics of Generic versus Focused Approach in Preparing for TeamSTEPPS.
| Hospital | Assess needs | Reflect on the context | Set goals | Develop a shared understanding | Select change agents |
|---|---|---|---|---|---|
| 1 | Lowa | Low | Low | Low | Low |
| No assessment | No reflection— seize the training opportunity | No specific goal | No knowledge, first learned from the training site | Members drafted | |
| 2 | Low | Low | Low | Low | Medium low |
| No assessment | No reflection— Seize the training opportunity | No specific goal | No knowledge, first learned from the training site | Members volunteered | |
| 3 | Low | Low | Low | Low | Medium low |
| No assessment | No reflection— Seize the training opportunity | No specific goal | No knowledge, first learned from the training site | Members volunteered | |
| 4 | Low | Medium low | Low | Medium low | Medium low |
| No assessment | Some reflection from previous experience | No specific goal | Some knowledge from previous training, no reflection | Members volunteered | |
| 5 | Medium low | Medium low | Low | Medium low | Medium low |
| Completed HSOPS, general assessment | Some reflection from previous experience | No specific goal | Some knowledge from previous training, no reflection | Members volunteered | |
| 6 | Low | Medium low | Low | Medium low | Medium low |
| No assessment | Some reflection from previous experience | No specific goal | Some knowledge from previous training, no reflection | Select from an existing group | |
| 7 | Low | Low | Low | Medium low | Low |
| No assessment | No reflection—Seize the retraining opportunity | No specific goal | Some knowledge from previous training, no reflection | Members drafted | |
| 8 | Medium low | Low | Low | Low | Medium low |
| Completed HSOPS, general assessment | No reflection— Minimum reflection by administrator, but not shared with others | No specific goal | No knowledge, first learned from the training site | Members volunteered | |
| 9 | Medium low | Medium high | Low | Medium low | Medium high |
| Completed HSOPS, general assessment | Good reflection on timing | No specific goal | Some knowledge | Frontline focused | |
| 10 | Medium low | Medium high | Low | Medium low | High |
| Completed HSOPS, general assessment | Good reflection on timing | No specific goal | Some knowledge | Influence focused, considered training ability | |
| 11 | Medium low | Medium high | Medium low | Medium high | Medium high |
| Completed HSOPS, general assessment | Good reflection on timing | General goal— To reduce readmission | Good knowledge from self-directed study | Frontline focused | |
| 12 | Low | High | Medium low | Medium high | High |
| Completed HSOPS before, no reassessment | Good reflection on timing and resources using previous experience | General goal—To improve patient safety culture | Good knowledge from previous training, sufficient reflection | Frontline and influence focused | |
| 13 | High | Medium high | Medium low | Medium high | Medium low |
| Highly deliberate assessment using HSOPS results | Good reflection on timing | General goal— To improve communication | Good knowledge from self-directed study | Select from an existing group | |
| 14 | Medium high | Medium low | Medium high | Medium low | Medium low |
| Deliberate assessment using HSOPS results | Some reflection on timing | Specific goal—To improve the handoff process | Some knowledge | Members volunteered |
Calibrated levels of evidence for deliberation: (a) high—demonstrates clear evidence for deliberate rationale and action in a preparation step; (b) medium high—demonstrates more evidence for deliberate than nondeliberate rationale and action; (c) medium low—demonstrates more evidence for nondeliberate than deliberate rationale and action; and (d) low—demonstrates clear evidence for nondeliberate rationale and action.
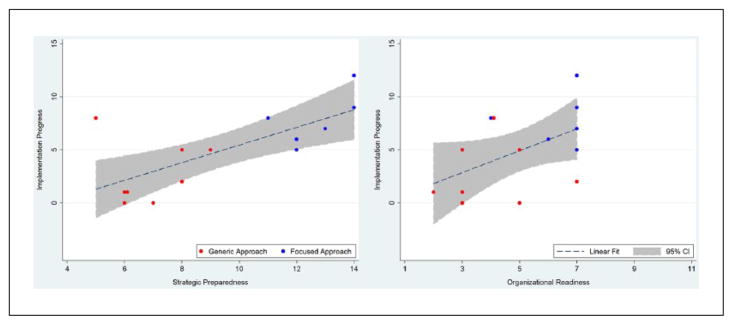
We applied both narrative and synthetic strategies in comparative analysis of the cases (Langley, 1999) to examine how strategic preparation corresponded with three implementation outcomes: implementation dynamics, implementation experience, and implementation progress. The narrative analysis involved constructing contextualized stories from the qualitative data. Specifically, informed by early coding and analysis, we used case studies to examine how TeamSTEPPS developed over time (i.e., implementation dynamics) in two hospitals, which exhibited high versus low levels of deliberation in their preparation. In addition, we reviewed the transcripts to identify themes related to mechanisms through which strategic preparation affected change leaders’ and team members’ experience.
The synthetic analysis involved taking the implementation process as a whole and constructing global measures from the qualitative data to describe its characteristics. To assess how strategic preparation corresponded with implementation progress, we constructed a global measure of strategic preparedness. Based on the “preparation steps” coding, two investigators independently assessed the evidence for deliberation demonstrated by the hospitals on each of the five steps (as shown in Table 2), using the calibration method commonly used in the fuzzy set analysis (Ragin, 2008a, 2008b). This method scales a case’s degree of membership in a defined set (in this study, the set is defined as a hospital executing deliberate rationale and action in preparing for TeamSTEPPS) based on the qualitative evidence. Full membership is based on clear evidence that a case is in the set. Full nonmembership is based on clear evidence that the case is out of the set. Acknowledging that most social phenomena do not always have cases with crystal clear states of full membership or nonmembership, the fuzzy set analysis enables researchers to calibrate a case’s degree of membership using intermediate points. For example, using a 4-point scale, two intermediate states are defined: A partial membership indicates more in than out of a given set and a partial nonmembership indicates more out than in a given set. Thus, we calibrated the levels of evidence for deliberation in each hospital’s case using the following anchors: (a) high (full membership)—demonstrates clear evidence for deliberate rationale and action in a preparation step; (b) medium high (partial membership)—demonstrates more evidence for deliberate than nondeliberate rationale and action; (c) medium low (partial nonmembership)—demonstrates more evidence for nondeliberate than deliberate rationale and action; and (d) low (full nonmembership)—demonstrates clear evidence for nondeliberate rationale and action. We calculated a global measure of strategic preparedness by summing the deliberation scores (1 = low to 4 = high) across five preparation steps, and then linked this measure to two additional measures that we created: (a) organizational readiness as captured by an existing TeamSTEPPS metric and (b) a global measure of implementation progress.
In order to measure organizational readiness, two investigators independently evaluated each hospital using the TeamSTEPPS Organizational Readiness Assessment Checklist (AHRQ, 2013b). This scoring metric consisted of 12 readiness factors (e.g., sufficient staff with the necessary characteristics and attitudes to serve as instructors) that were judged either as present or absent in a hospital. In order to measure implementation progress, we first constructed a timeline to reflect what implementation events happened in each hospital during the first 9 months. For this step, four coders worked in pairs and each pair coded transcripts for half of the hospitals. Coders independently coded transcripts related to two types of key implementation events—staff training and tool implementation. Staff training was coded as to the scope of the training (using a coding scheme based on AHRQ’s definitions of training module: introduction, essentials, and fundamentals), who received the training, and when it was conducted. Tool implementation was coded as to which tool was implemented, in which unit or department, and when it was implemented. Coders then compiled the information and created a timeline for each hospital capturing what and when implementation events occurred. One of the investigators reviewed and reconciled each hospital’s timeline with the coders using the same reconciliation method discussed above. Based on the timelines, two investigators independently scored each hospital’s implementation events using a metric developed by the authors. The score incorporated two dimensions—intensity (1 for each tool implemented, and 1 to 3 depending on each training event’s scope) and spread (1 = a single unit, 2 = multiple units). The two scores were multiplied to measure each implementation event.
Before reconciliation, the inter-rater agreement (calculated as intraclass correlation coefficient for a single measurement) was .83, .84, and .93 for the strategic preparedness, organizational readiness, and implementation progress scores, respectively. The two investigators discussed scores for each preparation step, readiness factor, and implementation event until there was agreement. Scores were then summed to measure respective constructs. We explored the overall pattern of relationships between these constructs using scatterplots.
Results
Applying the conceptual framework, we identified a range of practices in preparing for TeamSTEPPS. Despite the idiosyncratic circumstances that shaped the hospitals’ considerations and actions, a consistent theme emerged from our analysis; that is, hospitals varied noticeably in the level of deliberation that the change leaders and teams demonstrated in preparing for each of the five strategic steps. In light of this theme, we first describe preparation practices in each step and identify patterns across the 14 hospitals. Second, we draw on two hospitals’ implementation experiences as case studies to explain how different preparation approaches affected subsequent implementation dynamics within each hospital. Last, we explore the effects of strategic preparation on change leaders and teams’ experience as well as implementation progress.
Approaches in Preparing for TeamSTEPPS
Assess Needs
Practices in this step ranged from completely skipping it to using the AHRQ Hospital Survey on Patient Safety Culture (HSOPS) to identify specific areas for improvement. Hospitals also varied in the extent to which they used the assessment results to inform decisions. Following the implementation guideline, hospitals were instructed by the training organization to complete the HSOPS survey and review results before attending the Master Trainer training. This step was intended to assist hospitals in evaluating their specific improvement needs and the fit between Team-STEPPS and their needs. We noted that seven hospitals skipped this step and five other hospitals completed the survey, but did not substantially use the results to inform their decisions. Two themes emerged in explaining why a careful assessment was skipped. First, many interviewees reflected that they did not have a clear perspective about how the assessment would affect implementation. A common expression was that the team did not “connect the dots.” Second, several hospitals expressed that time constraint had limited their ability to complete a thorough assessment. These themes are illustrated in the following quotes:
I think we did not have a clear picture of what we would be focusing on. We had been doing a lot of other trainings. So, I thought I was going to learn a concrete process.
We had done it (HSOPS) but we hadn’t gotten our report back and it was just to the final minutes before the class when we finally got some information.
Subsequently, change leaders often had difficulty articulating what specific QI needs had motivated the implementation. Instead, three general motivational narratives were used: to improve patient safety, to improve teamwork and communication, and to make culture change.
I don’t think there was any critical incident or specific data that we were looking at that made us realize we really needed to do this. I think we all know that this is really important and is going to be focused on even more in the future. . . . It is important enough that we need to focus on and improve even though we don’t have a lot [safety events]. But, if you get one, one is too many.
In comparison, two hospitals used HSOPS results to identify specific improvement needs; and the leaders from these hospitals articulated why TeamSTEPPS is an appropriate intervention. One change leader explained:
When we got our [HSOPS] response back, we looked at those. Communication was one of our biggest issues. Our staff as well as I felt what we saw as incidents or issues in our facility always came down to communication problems. It was a big issue, so we thought TeamSTEPPS would be a perfect thing.
Reflect on the Context
Our analysis revealed that hospitals’ context reflection focused primarily on the timing for implementation and whether it would compete with other demanding organization-wide initiatives. However, hospitals varied in whether they tailored their implementation plans based on such reflections. Some hospitals that did not have prior knowledge of TeamSTEPPS were prompted by the opportunity to participate in the free training. Other hospitals had prior knowledge about TeamSTEPPS and decided to pursue the training opportunity even though they recognized that the context and timing were not ideal for implementation at their facilities. An interviewee explained:
We were already looking at TeamSTEPPS. It was something we had been throwing around for a while. But the timing was not necessarily the best for us. Yet the training was available and we wanted to take advantage of it.
Several hospitals demonstrated high levels of evidence for deliberation in reflecting on the context. Among these, a few mentioned that they previously postponed participation in TeamSTEPPS due to other priorities. Others used their reflection to formulate a tailored plan; for example, forming an “experimental team” to “test implement” in a limited area. A change team member from one hospital that had failed a previous attempt to implement TeamSTEPPS reflected:
We looked back in retrospect at what went wrong last time and why things didn’t get implemented. We thought our job was to throw everything out there and say “here’s the entire program.” We were not ready for that. With a little more knowledge and a little more experience under our belts now, we knew what was needed. Let’s just roll out one thing at a time so that it’s not so overwhelming for us and for staff.
Other organizational contexts such as cultural or resource conditions were not explicitly discussed by change leaders as part of their reflection. This may be due to two related factors: (a) hospitals in our sample all decided to implement TeamSTEPPS (i.e., the selection effect) and (b) cultural and resource conditions were often not favorable in small and rural hospitals. Participants may have thus been reluctant to acknowledge specific negative conditions that they ignored when they undertook the initiative.
Set Goals
Almost universally, hospitals in our sample failed to identify specific goals for their implementation. Some change teams developed vague, all-inclusive goals. For example, an interviewee stated:
I think our goal is to implement as many of the practices and tools as we can. I guess to develop that culture. . . . I think the big picture is that, in two or three years, we want to feel like that we have a little more teamwork culture across the organization.
One hospital was an exception in this aspect and did identify specific goals for implementation. The hospital’s change team went off to the training without a clear plan. However, the interviews revealed that the team met immediately after the training to plan for implementation and identified improving the handoff process as their specific goal. A change team member described:
Handoff was one of the areas that we struggled in our HSOPS survey. . . . We thought that the ‘I PASS the BATON’ tool would positively influence that and decided to start with focusing on improving handoff.
Develop a Shared Understanding
Developing a shared understanding of what Team-STEPPS is and what it takes to implement was challenging due to its dual-feature of complexity and adaptability. We found that hospitals often had limited understanding about the nature and scope of TeamSTEPPS. A high level of evidence for shared understanding typically came from (a) hospitals that previously received TeamSTEPPS training, failed to implement it, and had sufficient reflection on their experience or (b) hospitals whose leaders had been actively exploring TeamSTEPPS-related knowledge from various sources such as AHRQ, affiliated hospitals, and professional networks.
Some oversimplified understanding included interpreting TeamSTEPPS as a QI program, a communication tool box, or a patient safety initiative. Our analyses suggested that the lack of communication between the training site and the hospitals, as well as between hospital executive sponsors and selected change agents, before the Master Trainer training hindered the development of an adequate understanding. The “train the trainer” model was confusing to many people. The lack of understanding was illustrated in the following quotes:
I guess we didn’t know a lot about it. . . . I thought that it was just going to be about patient safety.
The only information I received prior [to going to the training] was from our administrator that it was a way to improve communication.
I first heard about it from the training site. I knew it said Master Trainer training, but I don’t think I really connected the dots that it meant we were going to be the trainers. I thought we were going to learn about it and bring it back. . . . After we left the training site, it was a totally different expectation for us.
We found that the lack of understanding had triggering effects on other steps of preparation. Hospitals that had low levels of understanding often failed to carefully assess their improvement needs, reflect on their contexts, set specific goals, or select change agents purposefully. Examples below illustrate how the lack of understanding may have affected the hospitals’ planning activities:
We were getting different messages on how to approach this. There were so many different ways we could start and we were not sure what the best way was.
I don’t think we really knew who we should pick when we were not really sure what all this was exactly.
Select Change Agents
As many of the CAHs had accumulated experiences in other QI-related initiatives, change leaders often developed appreciation of staff members’ characteristics and their own approaches for selecting change agents. Several deliberate rationales emerged in explaining how change agents were selected, often shaped by the hospitals’ idiosyncratic contexts and the executive sponsors’ logics. These rationales included frontline-focused selection, influence-based selection, and performance-based selection, as illustrated below.
It really has to come from the frontline and they have to be the ones to implement it, make it work for them.
The staff definitely had more faith in certain people. . . . It [selecting those people] was important to get the buy-in.
Part of our culture is to look at our high performers. . . . They want new challenges and new growth; and so they were nominated.
In other hospitals, the selection was based on volunteering or drafting, which was considered to be less deliberate because the selection was not supported by an explicit rationale. Selecting change agents who could fulfill the training needs (i.e., someone with the skill or experience to do internal training) was a weak link in most hospitals’ preparation. One interviewee explained:
When we left [the training], we didn’t feel like we were master trainers . . . I’m sure if there was a team of master trainers who could come in and do our training for us, we would let them because none of us was prepared to be the trainer.
Generic Versus Focused Approach
As shown in Table 2, we identified two distinct groups of hospitals that adopted different approaches in preparing for TeamSTEPPS. The first eight hospitals exhibited low or medium low levels of evidence for deliberation on all five steps. We categorized these hospitals as adopting a generic approach where the hospitals intended to use TeamSTEPPS for general QI purposes without exercising deliberation in customizing and strategically preparing for its implementation. The other six hospitals demonstrated high or medium high levels of evidence for deliberation on one or more strategic steps. Although there was no consistent pattern regarding which combination of strategic steps the hospitals “decided” to be deliberate about, we found that context reflection and change agent selection were two aspects where many demonstrated a certain level of deliberation, partly due to the experiences gained from previous change initiatives. In comparison, very few hospitals deliberately assessed the facilities’ specific needs or set specific goals for implementation. No hospital demonstrated high levels of evidence for deliberation on all five steps. Nevertheless, we categorized these six hospitals as adopting a focused approach in preparing for Team-STEPPS because their practices reflect certain efforts to customize this large, complex initiative to fit into their existing conditions and QI needs.
Implementation Dynamics
In order to clearly illustrate how different approaches to preparation strategy influenced subsequent implementation dynamics, we compare and contrast two exemplary hospitals’ experiences. We draw on Hospital A’s experience to show how the lack of deliberation on five preparation steps resulted in obstructive dynamics and a stalemate in the implementation process. By contrast, Hospital B’s experience showed progressive dynamics, which benefited from deliberate preparation for some if not all of the strategic steps.
Hospital A
Hospital A was a rural medical center affiliated with a regional health system. It included a 25-bed CAH, four clinics, and a nursing home. Its implementation process commenced with an enthusiastic decision made by the Chief Executive Officer (CEO) who was intrigued by TeamSTEPPS’ evidence-based approach when he first learned about it.
I think the impetus was that we got the invite [from the training site]. I have always been very interested in anything we do for performance improvement. It seemed like TeamSTEPPS fit right into that. It could give us the science that we need to prove to the clinicians that it works.
In planning for TeamSTEPPS, the CEO employed a top-down, all-inclusive approach, focusing on selecting leaders that could influence most units and employees. A change team was formed, which consisted of four administrators (i.e., the CEO, the Chief Nursing Officer [CNO], the Quality Director, and the Lab Manager) and one staff nurse. The CEO explained:
Our original plan was to get the leaders in place and on board with it. Then, I would hope that other people will follow. I thought the Quality Director should be the champion for this, and then the CNO because it would involve nursing. We have a combined manager position here for the lab and the clinics. The lab and nursing have to work closely together so that I thought it would be beneficial to have that manager go. . . . With her, we can also influence the clinic to make sure we speak the same language . . .
The change team supported the idea of implementing TeamSTEPPS. However, no assessment or action plan was developed during the 9 months that we followed Hospital A. Change team members all undertook multiple responsibilities that compete for their time and attention. They did not make TeamSTEPPS a priority in the absence of a concrete plan. As a result, the team did not carry out coordinated implementation activities during the 9-month period with the exception that the concept of TeamSTEPPS was briefly introduced to managers and team leaders at a management meeting. The lack of plan and action was reflected by the change team six months into the implementation:
We are all convinced by the idea. But what we really need to get at is just sitting down to set our goals and make a plan. We’ve done a lot of unofficial talking, but no one has said this is what we should do and act on it. I would like to see a little bit of that.
Hospital A’s implementation process highlighted the obstructive dynamics commonly experienced by other hospitals that initiated TeamSTEPPS using an all-inclusive, generic approach: (a) with the generic approach, change leaders tended to start the implementation without specifying its goals or strategic direction, or justifying its importance; (b) the lack of strategic direction reduced the sense of urgency and commitment and, in several cases, created frustration among change agents who often faced time constraint and competing priorities; and (c) the lack of strategic direction and commitment prolonged the “planning” stage and delayed concrete implementation activities. Table 3 shows exemplary quotes from other hospitals that demonstrated similar dynamics.
Table 3.
Exemplary Quotes for Implementation Dynamics.
| Dynamics | Generic approach | Focused approach |
|---|---|---|
| Strategic direction | “We are focusing on communication, but do not have anything specific in mind.”—Hospital 2 | “Our goal was to get everybody trained before the end of the year . . . our next goal was to work on SBAR with the Med-Surg Floor.”— Hospital 9 |
| “Whatever we could to promote teamwork, safety, those types of things.”— Hospital 6 | “The AHRQ survey showed our weak area was communication openness, which was how we came about picking Huddle.”—Hospital 10 | |
| Sense of urgency and commitment | “It hasn’t been figured out who will lead this.”—Hospital 1 | “I took the lead on the training because I felt my schedule allowed me to try to do some legwork for us.”—Hospital 9 |
| “Getting the people together to get the changes made becomes a challenge because we are dealing with patients on a daily basis.”—Hospital 5 | “We meet at least monthly.”— Hospital 12 | |
| “Our hardest thing is to get our meetings scheduled.”— Hospital 7 | “The four of us have been in this since the beginning. We’re there to back each other. We’re pretty dedicated to this.”—Hospital 13 | |
| Implementation activity | “We’re in limbo now. Each of us has got different projects that we’re working on. We have not come together again to work on it.”—Hospital 1 | “We decided to start off with training briefing in the Lab. We role-modeled the first day and let them do it.”—Hospital 10 |
| “Even though we have not done anything officially with TeamSTEPPS, but we know it’s there.”—Hospital 2 | “People feel that there’s a time constraints; and that’s why we’re taking baby steps in implementation. Let’s just keep it moving forward.”— Hospital 12 |
Hospital B
Hospital B was a 25-bed, independent CAH, which included a hospital, a physician clinic, and a home health agency. The hospital’s CNO and Quality Director decided to implement TeamSTEPPS with an aim to improve communication between the hospital and the home health agency. The communication issue was identified as a key factor contributing to the high readmission rate among the hospital’s elderly patient population. In planning for TeamSTEPPS, the CNO and Quality Director selected five staff nurses and nurse managers from different units that they described as “movers and shakers” for making changes. The Quality Director described the rationale for selecting change agents,
We looked at our group that we already set up for other [QI] purposes. . . . Administrator A [the CNO] had done a little self-evaluation with each of them on how they would react to change. So, she kind of knew which one may be on the edge.
Before training, the change team held a conference call with the training site to get a preview of TeamSTEPPS and discuss expectations. The implementation plan was not specified at this stage, but the team reflected later that the conference call prepared them with basic knowledge about TeamSTEPPS and helped them develop a plan soon after the training.
We did the conference call and Administrator A told us what she knew about it. I don’t remember that we had a definite plan. . . . It was just to get us prepared. It was mainly after the training when we got the plan.
The team’s plan focused on (a) providing training to three employee groups including nurses, managers, and home health staff and (b) adopting SBAR and CUS (i.e., TeamSTEPPS tools for communicating critical information and safety concerns) in practice. As in many other hospitals in our sample, the change team at Hospital B was challenged by competing priorities and getting buy-in. Nevertheless, the team was able to meet regularly and develop activities following their plan. The team introduced SBAR and CUS to nurses at the hospital and home health agency during the first quarter. The team noted that actual utilization of these tools was less consistent and needed reinforcement as the implementation continued. Three training sessions were delivered in the second and third quarters. By the third quarter, the executive sponsors and the change team considered the implementation to be active and moving forward.
Hospitals with a focused preparation approach often showed progressive dynamics in their implementation that can be characterized by having a strategic direction and a sense of urgency, which leads to concrete planning and actions. Table 3 presents exemplary quotes to illustrate such dynamics. In Hospital B, several factors contributed to fostering such dynamics: (a) the change leader had some knowledge of TeamSTEPPS, which influenced her selection of change agents and knowledge sharing; (b) the change leader and team had specific improvement needs in mind, which facilitated the development of an action plan; (c) the team was made up of all frontline staff who had more boots-on-the-ground knowledge about improvement opportunities; and (d) the team felt empowered by the leader, and had ideas to act on concrete tools. A team member described:
Once we understood and had some basis with TeamSTEPPS . . . we were to say, “Here are some tools that we want to try.” It became our idea. . . . Luckily we have Administrator A [the CNO] and Administrator B [the Quality Director] to help us, too, because they’re at the manager level.
Strategic Preparedness in Small and Rural Hospitals
Based on our observations, we proposed that the application of a focused approach in preparing for TeamSTEPPS contributes to building a state of strategic preparedness for change, which is different than the state of organizational readiness previously examined in the literature. Strategic preparedness is particularly important for small and rural hospitals because it can facilitate the implementation process without demanding excessive resources. We thus explain how strategic preparedness affected the experience and progress outcomes of TeamSTEPPS with the themes that emerged in our coding and analysis.
Strategic Preparedness and Implementation Experience
Strategic preparedness (or lack of it) can shape the implementation process by affecting change leaders’ and change team members’ individual and collective experiences. Our analysis indicated that high levels of strategic preparedness affected change experiences through three mechanisms: keeping the change team focused and engaged, helping the change team foresee and appropriately manage implementation barriers, and enhancing the change team’s perception of control and efficacy.
First, strategic preparedness derived from deliberation during the preparation stage, especially deliberation on assessing needs and setting goals, helped the change teams focus on identified needs and goals, which in turn facilitated implementation progress. One hospital’s change team provided an account of how the identified needs and goals helped the team engage in implementation and move forward. During the first two quarters, the team described that, with a specific focus on handoff, they were able to use tools from TeamSTEPPS to plan training and to use at the bedside. In the third quarter, the team achieved significant progress in “hardwiring” the handoff tools. The level of engagement from all change team members was high as evident in their uniform account of what planning, training, and implementation events had occurred. By contrast, hospitals that adopted the generic approach often had difficulties in organizing implementation-related events such as group meetings. As a result, change team members often expressed different perceptions of the implementation status.
Second, strategic preparedness derived from deliberating on context reflection and change agent selection helped the change teams foresee potential issues or barriers, and prompted the teams to take actions to appropriately manage such issues or barriers. For example, one executive sponsor used her reflection on the organizational context to strategize how to engage physicians in the implementation. By contrast, a lack of deliberation often resulted in implementation issues and barriers not being effectively managed. The common issues and barriers experienced by these hospitals in TeamSTEPPS implementation included resistance from change recipients, low commitment from change agents, disruptions due to competing priorities, and staff turnover.
Third, at the individual level, strategic preparedness enabled change team members to develop a cognitive state that embraced both mindfulness and flexibility, and improved their perceived control and change efficacy. Such a cognitive state helped the individuals as well as the teams to be more persistent and confident while facing challenges and barriers. An administrator described:
For us, EMR [electronic medical record] was a bit of a barrier. We knew it was coming, so this wasn’t the most ideal time [for TeamSTEPPS]. . . . So, we slowed down [during EMR implementation]. But, our goal certainly has not changed. We’re still moving forward, pushing education out, keeping people in the loop, and bringing it [TeamSTEPPS] up to keep it as a focus.
In comparison, change team members from the hospitals with low levels of strategic preparedness experienced anxiety, feeling overwhelmed, and other negative emotions. Such emotional reactions are illustrated as follows:
I didn’t know what I was getting into. It was more than I had anticipated. I was really nervous.
I think this is always a barrier that it’s one more thing we have to do. There’s always something new. It doesn’t seem like anything ever gets taken away, but you get more jobs that you have to do all the time. So, you know, that was my initial response.
Strategic Preparedness and Implementation Progress
Applying the synthetic strategy (Langley, 1999), we explored the relationships of strategic preparedness and organizational readiness with implementation progress across the hospitals. The hospitals exhibited varying levels of overall strategic preparedness ranging from 5 to 14 (on a 20-point scale). To assess hospitals’ organizational readiness for TeamSTEPPS, 12 readiness factors were evaluated. Organizational readiness scores of the 14 hospitals fell between 2 and 7, which indicated “not ready.” According to the TeamSTEPPS implementation guideline, any score lower than nine suggests the organization may not be ready for TeamSTEPPS. Scores lower than six indicate that significant improvement is needed. Our observation is consistent with the literature, which suggests that it is very difficult for small and rural hospitals to muster the resources, time, and personnel to establish organizational readiness to implement large-scale change initiatives like TeamSTEPPS (Casey & Moscovice, 2004).
The implementation progress score ranged from 0 to 12. This score captured overall progression of a hospital’s implementation activities in the first 9 months. It does not definitively indicate the success or failure of the implementation because the implementation was unfolding at the time of assessment and each hospital could embrace different “end goals” for implementation. The early progress, however, is critical in making implementation activities visible, maintaining the momentum, and keeping the initiative alive; which in turn are important for the diffusion and sustainment of changes (Berwick, 2003; Kotter, 1996). We found that hospitals that adopted a generic approach made slower progress: Seven out of the eight hospitals’ progress scores were at or below the lowest score of the group that adopted a focused approach. In fact, five of those hospitals experienced a noticeable stalemate where virtually no implementation event or planning activity occurred between our quarterly visits. In comparison, hospitals that adopted a focused approach managed to continue making progress including organizing training events or rolling out selected tools; and in so doing kept the implementation viable. Comparing across hospitals, we found an overall positive relationship between the level of strategic preparedness and the implementation progress (see Figure 1). We also found that organizational readiness was positively related to both strategic preparedness and implementation progress, but the relationship between organizational readiness and progress had a more scattered pattern than that between preparedness and progress.
Figure 1.
Relationships of strategic preparedness and organizational readiness with implementation progress
Discussion
Managing large-scale QI initiatives to achieve organization-wide improvement is a challenging but indispensable task faced by all health care organizations. Previous research (Shortell et al., 1998; Weiner, 2009) has provided theoretical and empirical support for the importance of an organization’s cultural, structural, and resource contexts, and readiness for change derived from those contexts, for facilitating the success of QI initiatives. However, small and rural hospitals often cannot wait until all the resource and infrastructure conditions improve and the organization becomes ready to start important QI efforts such as TeamSTEPPS. Our study thus contributes to the literature by providing insight into the strategies that can help small and rural hospitals with restricted conditions prepare for organization-wide QI initiatives. Adopting a change management perspective, this research explores why certain management practices facilitate the implementation of a complex QI program. Our findings contribute to the ongoing effort to use organization and implementation sciences to inform QI practice and further understand what health care organizations can do to generate systematic change (Damschroder et al., 2009; Harvey & Kitson, 2015).
Our main findings suggest that the level of deliberation on the five preparation steps is a key factor that differentiated CAHs’ practices in preparing for TeamSTEPPS. The preparation practices and the varying levels of strategic preparedness derived from them lead to different early implementation outcomes. Change leaders and teams were more likely to experience engagement, perceive efficacy, foresee and manage barriers, and achieve progress during the implementation when they were more mindful in reflecting on the hospital’s specific needs and context, strategizing about goals and change agent selection, and developing a shared understanding. This finding is consistent with the QI and OD theories that suggest strategizing, sensemaking, and emotion managing as critical aspects of the change process that need to be carefully managed, especially during the preparation stage (Bartunek et al., 2011). Our finding connotes an emerging argument in the literature that suggests deliberation or mindfulness may enhance readiness for change (Gärtner, 2013; Gondo, Patterson, & Palacios, 2013).
We also found that developing a shared understanding of TeamSTEPPS among change leaders and agents is critically important because it influenced the deliberation on other strategic aspects. A lack of adequate understanding contributed to some hospitals’ practices in making hasty and uninformed decisions regarding the implementation. Such decisions in turn affected change agents’ behaviors and experiences in the subsequent stages. This finding is consistent with existing theory that suggests understanding and meaning assigned to the planned change can influence change recipients’ responses and thereby the direction of change (e.g., Balogun & Johnson, 2005; Gioia & Chittipeddi, 1991). What differentiates our finding is that many change leaders themselves did not fully understand the nature and scope of this QI initiative; and therefore missed the opportunity to leverage the sensemaking tactics suggested by theory.
Our findings offer several practical implications for hospital leaders, change teams, training organizations, and AHRQ. First, despite their limited resources and lack of readiness, some hospitals in our sample made good progress in training and implementing TeamSTEPPS curriculum and tools in the first 9 months. Under restricted conditions, leaders of small and rural hospitals should not simply pass on the opportunity to initiate TeamSTEPPS. Nor should they initiate it without a clear plan. Instead, they should deliberately assess their organizations’ needs and context, and select appropriate goals and change agents to better prepare for implementation. Second, leaders and change teams should develop and communicate an adequate understanding of TeamSTEPPS before initiating it in order to facilitate planning and subsequent implementation. Third, for many small and rural hospitals, the training organization’s invitation to participate in the Master Trainer training is often their first contact with TeamSTEPPS. Training organizations can benefit from intentionally communicating knowledge about TeamSTEPPS before the actual training by offering an overview of its scope and structure, explaining the “train the trainer” model, providing simple yet succinct instruction on what steps need to be taken to prepare, and allowing adequate time for completing these steps. The instruction should go beyond the usual steps to complete the HSOPS survey and readiness assessment, and extend to other areas of preparation such as goal setting and change agent selection. Last, two preparation steps (i.e., assessing needs and reflecting on the context) were already incorporated in the implementation guide. However, we found that small and rural hospitals rarely took the recommended actions for several reasons. Besides the lack of understanding and time, the complexity of the guidelines themselves seemed to hinder hospitals from taking these actions. AHRQ should consider simplifying the implementation guideline in general and/or developing a separate guide for what steps must be taken before attending the Master Trainer training as decisions made during this stage often cannot be reversed (e.g., decisions to implement and change agent selection).
Our study has several strengths including the prospectively collected primary data, use of multiple case sites and multiple informants for each site in data collection, and analyses guided by a conceptual framework synthesized from various streams of literature. Despite these strengths, the study has several limitations that lead to new avenues of research. First, we took a holistic approach in assessing hospitals’ preparation strategies. As a result, the relationship between the five preparation steps and how they individually or interactively affect the change process were not untangled in this study. Future research is needed to tease out and test these individual effects on implementation processes and outcomes. Second, the use of implementation progress as we operationalized it to capture how the implementation process unfolds is a new, not yet validated approach for evaluation. Hospitals might have well-thought-out goals for training or tool implementation, which serve as a better benchmark for evaluating the implementation outcome (although we did not find evidence for such goals in our sample). Future research may develop hospital-specific criteria for evaluating the implementation outcome. Also, as with case study research in general, we are limited in our ability to generalize the findings to other QI implementations or implementation of TeamSTEPPS in other organizational settings (e.g., large hospitals or systems). We tried to support the validity of our findings with rigorous methods and iterative analyses. Nevertheless, future research that investigates QI preparation strategy and its relationship with implementation process in other contexts can help gauge the generalizability of our findings and contribute to our understanding in the area of QI and change management.
Acknowledgments
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by funding from the Agency for Healthcare Research and Quality, R18-HS018396 and R03-HS024112. The content is solely the responsibility of the authors and does not necessarily represent the official views of the AHRQ.
Footnotes
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Agency for Healthcare Research and Quality. About TeamSTEPPS. 2013a doi: 10.1080/15360280802537332. Retrieved from http://teamstepps.ahrq.gov/about-2cl_3.htm. [DOI] [PubMed]
- Agency for Healthcare Research and Quality. Is your organization ready for TeamSTEPPS™? 2013b Retrieved from http://teamstepps.ahrq.gov/TeamSTEPPSReadiness.pdf.
- Armenakis AA, Harris SG. Reflections: Our journey in organizational change research and practice. Journal of Change Management. 2009;9:127–142. [Google Scholar]
- Balogun J, Johnson G. From intended strategies to unintended outcomes: The impact of change recipient sensemaking. Organization Studies. 2005;26:1573–1601. [Google Scholar]
- Bartunek JM, Balogun J, Do B. Considering planned change anew: Stretching large group interventions strategically, emotionally, and meaningfully. Academy of Management Annals. 2011;5(1):1–52. [Google Scholar]
- Berwick DM. Disseminating innovations in health care. Journal of the American Medical Association. 2003;289:1969–1975. doi: 10.1001/jama.289.15.1969. [DOI] [PubMed] [Google Scholar]
- Bunker B, Alban B. Large Group Interventions: Engaging the whole system for rapid change. San Franscisco, CA: Jossey-Bass; 1997. [Google Scholar]
- Burgelman RA. A model of the interaction of strategic behavior, corporate context, and the concept of strategy. Academy of Management Review. 1983;8(1):61–70. [Google Scholar]
- Casey MM, Moscovice I. Quality improvement strategies and best practices in critical access hospitals. Journal of Rural Health. 2004;20:327–334. doi: 10.1111/j.1748-0361.2004.tb00046.x. [DOI] [PubMed] [Google Scholar]
- Chassin MR, Loeb JM. The ongoing quality improvement journey: Next stop, high reliability. Health Affairs. 2011;30:559–568. doi: 10.1377/hlthaff.2011.0076. [DOI] [PubMed] [Google Scholar]
- Damschroder L, Aron D, Keith R, Kirsh S, Alexander J, Lowery J. Fostering implementation of health services research findings into practice: A consolidated framework for advancing implementation science. Implementation Science. 2009;4(1):50. doi: 10.1186/17485908-4-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dutton JE, Ashford SJ, O’Neill RM, Lawrence KA. Moves that matter: Issue selling and organizational change. Academy of Management Journal. 2001;44:716–736. [Google Scholar]
- Ford JD, Ford LW, D’Amelio A. Resistance to change: The rest of the story. Academy of Management Review. 2008;33:362–377. [Google Scholar]
- Gärtner C. Enhancing readiness for change by enhancing mindfulness. Journal of Change Management. 2013;13(1):52–68. [Google Scholar]
- Gioia DA, Chittipeddi K. Sensemaking and sensegiving in strategic change initiation. Strategic Management Journal. 1991;12:433–448. [Google Scholar]
- Gondo M, Patterson KDW, Palacios ST. Mindfulness and the development of a readiness for change. Journal of Change Management. 2013;13(1):36–51. [Google Scholar]
- Gustafson DH, Sainfort F, Eichler M, Adams L, Bisognano M, Steudel H. Developing and testing a model to predict outcomes of organizational change. Health Services Research. 2003;38:751–776. doi: 10.1111/1475-6773.00143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harvey G, Kitson A. Implementing evidence-based practice in healthcare: A facilitation guide. New York, NY: Routledge; 2015. [Google Scholar]
- Huy QN. Emotional balancing of organizational continuity and radical change: The contribution of middle managers. Administrative Science Quarterly. 2002;47(1):31–69. [Google Scholar]
- Isabella LA. Evolving interpretations as a change unfolds: How managers construe key organizational events. Academy of Management Journal. 1990;33(1):7–41. [Google Scholar]
- Kaluzny AD, Hernandez SR. Managing change in health care organizations. Medical Care Research and Review. 1983;40:161–203. doi: 10.1177/107755878304000301. [DOI] [PubMed] [Google Scholar]
- Katz DT, Kahn RL. The social psychology of organizations. New York, NY: Wiley; 1966. [Google Scholar]
- King HB, Battles J, Baker DP, Alonoso A, Salas E, Webster J, … Salisbury M. TeamSTEPPS™: Team strategies and tools to enhance performance and patient safety. In: Henriksen K, Battles J, Keyes M, Grady M, editors. Advances in patient safety: New directions and alternative approaches. Vol. 3. Rockville, MD: Agency for Healthcare Research and Quality; 2008. Retrieved from http://www.ncbi.nlm.nih.gov/books/NBK43686/ [PubMed] [Google Scholar]
- Kotter JP. Leading change. Boston, MA: Harvard Business School Press; 1996. [Google Scholar]
- Kotter JP, Rathgeber H. Our iceberg is melting: Changing and succeeding under any conditions. New York, NY: St. Martin’s Press; 2006. [Google Scholar]
- Langley A. Strategies for theorizing from process data. Academy of Management Review. 1999;24:691–710. [Google Scholar]
- Lawler EE, Worley CG. Built to change: How to achieve sustained organizational effectiveness. San Francisco, CA: John Wiley; 2011. [Google Scholar]
- Locke EA, Latham GP. A theory of goal setting & task performance. Englewood Cliffs, NJ: Prentice-Hall; 1990. [Google Scholar]
- O’Brien JL, Shortell SM, Hughes EF, Foster RW, Carman JM, Boerstler H, O’Connor EJ. An integrative model for organization-wide quality improvement: Lessons from the field. Quality Management in Health Care. 1995;3(4):19–30. doi: 10.1097/00019514-199503040-00003. [DOI] [PubMed] [Google Scholar]
- Paez K, Schur C, Zhao L, Lucado J. A national study of nurse leadership and supports for quality improvement in rural hospitals. American Journal of Medical Quality. 2012;28:127–134. doi: 10.1177/1062860612451851. [DOI] [PubMed] [Google Scholar]
- Ragin CC. Measurement versus calibration: A set-theoretic approach. In: Box-Steffensmeier J, Brady H, Collier D, editors. The Oxford handbook of political methodology. New York, NY: Oxford University Press; 2008a. pp. 174–198. [Google Scholar]
- Ragin CC. Redesigning social inquiry: Fuzzy sets and beyond. Chicago, IL: University of Chicago Press; 2008b. [Google Scholar]
- Reichers AE, Wanous JP, Austin JT. Understanding and managing cynicism about organizational change. Academy of Management Executive. 1997;11(1):48–59. [Google Scholar]
- Sanchez-Burks J, Huy QN. Emotional aperture and strategic change: The accurate recognition of collective emotions. Organization Science. 2009;20(1):22–34. [Google Scholar]
- Shortell SM, Bennett CL, Byck GR. Assessing the impact of continuous quality improvement on clinical practice: What it will take to accelerate progress. Milbank Quarterly. 1998;76:593–624. doi: 10.1111/1468-0009.00107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shortell SM, O’Brien JL, Carman JM, Foster RW, Hughes EF, Boerstler H, O’Connor EJ. Assessing the impact of continuous quality improvement/total quality management: Concept versus implementation. Health Services Research. 1995;30:377–401. [PMC free article] [PubMed] [Google Scholar]
- Weick KE. Sensemaking in organizations. Thousand Oaks, CA: Sage; 1995. [Google Scholar]
- Weick KE, Sutcliffe KM, Obstfeld D. Organizing for high reliability: Processes of collective mindfulness. In: Sutton RS, Staw B, editors. Research in organizational behavior. Vol. 21. Stanford, CA: JAI; 1999. pp. 81–123. [Google Scholar]
- Weiner BJ. A theory of organizational readiness for change. Implementation Science. 2009;19(4):67. doi: 10.1186/1748-5908-4-67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiner BJ, Alexander JA, Baker LC, Shortell SM, Becker M. Quality improvement implementation and hospital performance on patient safety indicators. Medical Care Research and Review. 2006;63:29–57. doi: 10.1177/1077558705283122. [DOI] [PubMed] [Google Scholar]