Abstract
Conversation and discourse analyses were used to examine medical problem presentation in pediatric care. Healthcare visits involving children with ASD and typically developing children were analyzed. We examined how children’s communicative and epistemic capabilities and their opportunities to be socialized into a competent patient role are interactionally achieved. We found that medical problem presentation is designed to contain a ‘pre-visit’ account of the interactional and epistemic work that children and caregivers carry out at home to identify the child’s health problems; and that the intersubjective accessibility of children’s experiences that becomes disrupted by ASD presents a dilemma to all participants in the visit. The article examines interactional roots of unmet healthcare needs and foregone medical care of people with ASD.
Keywords: autism spectrum disorders, children, conversation analysis, discourse analysis, healthcare encounters, medical problem presentation, unmet healthcare needs
Introduction
He (the doctor) did not engage with Alex, he engaged with me, but didn’t engage with Alex very much, so that’s a biggie. If they engage with Alex, like Doctor Taketa took the time, which is really important to me, he took the time and actually, “Alex, Alex,” or “What’s your name?”, and he’s like, “Alex!” He took the time to interact with him, where a lot of times the doctors are like, “What’s the problem?”, you know, “What’s going on?” Talk to him! See, engage him! He’ll say something to you, you may not understand it right away, but he’ll tell you something, which is really important because, I think, if any child- if you lower yourself to their eye level, they can relate to you.
In this interview excerpt, Simone, Alex’s mother, is reflecting on the different ways that two doctors interacted with her son during his recent healthcare visits. Diagnosed with Autistic Disorder (American Psychiatric Association 2000) just before he turned two years old, Alex is now eight and has little spoken language. Most doctors who see Alex rarely interact with him, but Alex’s pediatrician, Dr. Taketa, who specializes in ASD, is an exception. In just a few words, Simone succinctly describes the interactional patterns that often characterize healthcare encounters of children with ASD (Solomon et al. in press).
Paradoxically, however, Simone’s observations also describe the healthcare visits of most typically developing (TD) children. Research has consistently shown that TD children’s talk constitutes a small percentage of all discourse that takes place during their visits because they are rarely selected as speakers (Cahill 2010; Stivers 2001, 2011; Stivers and Majid 2007). That percentage increases incrementally with age, ranging between 3 and 14% (Cahill and Papageorgiou 2007; Stivers and Majid 2007; Tates and Meeuwesen 2000). It is the TD children’s caregivers, mostly mothers, who are the primary informants about the child’s symptoms and illness experiences (Cahill 2010; Stivers 2007; Tates and Meeuwesen 2001).
How and why does it matter, then, that a child with ASD is or is not engaged by the doctors? If TD children are often not expected to speak during their visits, how and why does it matter that a child with ASD is or is not expected to speak? These questions go to the core of the social construction of children’s tacitly assigned ‘rights’ to participate in healthcare visits. They bring into focus the minute but powerful social processes that afford children opportunities to enact their communicative and epistemic competence, and to be socialized into the role of a competent patient (Heritage 2009; Stivers 2001, 2011, 2012). For children with ASD, whether and how the doctors ‘lower themselves to their eye level’, as Simone says, by calling them by name, engaging them in greetings, and selecting them as speakers, subtly but powerfully projects the children as certain kinds of interactants, either potentially able or unable to participate in their healthcare visits (Heritage 1984; Searle 1969). It is this construction of Alex’s personhood that Simone reflects on in the excerpt above, arguing that the doctors should interact with him as they would with ‘any child’.
Understanding these dynamics is important for several reasons. While significant advances have been made in the scientific understanding of genetic, neuro-biological and cognitive processes underlying ASD symptomatology, little is known about the impact of socio-communicative and sensory impairments associated with ASD on the provision of healthcare (Accordino and Walkup 2015; Bauman 2010; Croen et al. 2015; Lajonchere et al. 2012; Solomon et al. in press; Volkmar et al. 2014a b). Equally unknown is how healthcare practices and contexts engender and problematize the manifestations of socio-communicative and behavioral challenges common in ASD (Lester and Paulus 2012).
Moreover, how doctors interact with TD children who have a chronic illness has been linked to parents’ adherence to treatment and satisfaction with care (Swedlund et al. 2012). Parents of children with ASD also greatly value the rapport that professionals build with their child, but they also explicitly insist on these professionals ‘knowing the child” before they provide treatment (Hodgetts et al. 2013, p. 144), which points to a distinction between knowing the child’s diagnosis and healthcare needs, and knowing the child as a person (Solomon et al. in press). Our analysis will illustrate the investment that parents of children with ASD make in orchestrating seemingly trivial but consequential interactions between their child and the doctor, e.g. a greeting at the start of the visit.
Getting to know the healthcare needs of patients with ASD is, however, a complex process (Warfield et al. 2015). Many health problems, ranging from those known to be associated with ASD (Bauman 2010; Goldson and Bauman 2007, Volkmar and Weisner 2009), to idiosyncratic health problems (Accordino and Walkup 2015), and life-threatening conditions (Radcliff 2013, Smith et al. 2012) often remain undiagnosed in individuals with ASD (Siegel and Gabriels 2014). Over and above the challenges inherent in identification of medical problems in everyday clinical practice, the risks of foregone care and ‘diagnostic overshadowing’ (Reiss and Szyszko 1983) loom large for patients with ASD. Communication challenges that affect “reporting of internal symptoms” (Henry et al. 2014, p.403) play a significant role in ‘diagnostic overshadowing’ experienced by children with ASD, and patients with ASD more generally (Levy and Perry 2011; Simonoff et al. 2008). The clinical encounter is in many ways the epicenter of healthcare, a site where the doctor, the parent and the child establish the parameters of the medical problem. Conceptualizing ‘diagnostic overshadowing’ in interactional terms makes it possible to ask: What are the interactional practices that constitute differential diagnosis-relevant communication? Which practices support or hinder this process? What are the tacit expectations regarding children’s role as competent socio-medical participants who contribute to identifying their own medical problems, and how do these expectations become visible during healthcare visits of children with ASD?
To address these questions, we utilize two distinct qualitative approaches, conversation analysis (CA) and discourse analysis (DA). We describe how TD children and their parents corroborate in identification and description of the children’s symptoms, and draw a contrast in how TD children perform in their healthcare visits compared to children with ASD. Such a comparison is not a ‘matching’ of two groups of children. Rather, we show how what is called ‘autism’ becomes “visible symbolically and discursively, as bodies and minds are positioned as ordered or disordered in relation to able-bodied assumptions” (Lester and Paulus 2012, p. 261).
To this end, we use the CA and DA approaches in an integrated, ‘mixed methods’ perspective (Creswell et al. 2007). We use CA to identify and contrast patterns of the participants’ social behavior, i.e. the conversational turn-taking and the sequential organization of child-parent-doctor interaction related to medical problem presentation. Additionally, we use DA to contextualize medical problem presentation in “the lifeworld” (Mishler 1984, p.104) of the parents and the doctors by capturing their narrated experiences - what is sometimes called ‘self-report’- as exemplified by Simone’s excerpt above. Our approach is especially well-suited for uncovering the interactional roots of foregone medical care for children with ASD: it reveals both “what is done” in child-parent-doctor interactions, and “how it is achieved” (Halkowski and Gill 2010, p.213; Maynard and Heritage 2005; Heritage 2009a b). The approach also reveals the particular interactional quandaries – e.g. diminished accessibility of children’s illness experiences - that constitute ASD as a problem for all the participants in the visit (Solomon et al. in press).
First, we examine how at the very start of the visit the doctors and the parents attribute to the children certain epistemic and experiential ‘rights’ related to their illness experiences (Stivers 2001, 2011), and how the children accept, claim, reject or overlook these ‘rights’. Second, we juxtapose and compare medical problem presentations during TD children’s visits and visits of children with ASD, with an eye for practices that instantiate the intersubjective accessibility of the children’s illness experiences in the time leading to the visit, and during the visit itself. We describe how, usually at the very start of the visit, the mothers and their TD children produce a shared, mutually ratified account of the interactional and epistemic work that they have been carrying out at home to identify and evaluate the nature of the child’s health problems. The account of this “pre-visit” work often legitimizes the reason for the visit (Heritage 2009).
We show that it is through these interactional processes that children are constituted, at least provisionally, as competent socio-medical participants, accountable and able to self-reflectively register, remember and describe their symptoms to their caregivers at home and to their doctors during the medical problem presentation. The goal of this article is to identify communication patterns that characterize how TD children’s health problems are described during the visits, and how interactional challenges inherent in ASD both influence and are engendered by such interactions (Lester and Paulus 2012).
Methods
Similar to most healthcare research, studies on healthcare of children with ASD in the U.S. have traditionally used large-scale, macro-level approaches (e.g. Kogan et al. 2008), making little connection between population-level findings, and the micro-level interactional processes that may contribute to them (Cicourel 2011). These studies reveal a contradictory picture: compared to other pediatric populations, children with ASD have increased unmet healthcare needs in spite of increased healthcare utilization (Bethel et al. 2014). Liptak et al. (2006) report that children with ASD in their study averaged outpatient visits that were twice as long compared to other children’s (31.9 min vs. 15.8 min). They also had significantly more outpatient visits (41.5 vs. 3.3) and physician visits (8.0 vs. 2.2) (Liptak et al. 2006, p. 876). Children with ASD in Croen and colleagues’ (2006) study were hospitalized at a higher rate, were nearly 9 times more likely to use psychotherapeutic medications, and twice as likely to use gastrointestinal agents than children without ASD. Their mean annual cost of healthcare per child was found to be more than three times higher than for children without ASD (Croen et al. 2006). On the other hand, children with ASD experience greater unmet healthcare needs and face significant disparities in receiving comprehensive, coordinated primary and specialty care, compared to children with other conditions (Chiri and Warfield 2012; Newacheck and Kim 2005; Tregnago and Cheak-Zamora 2012).
Our methodological approach identifies micro-level interactional processes that may be contributing to this complex picture (Cicourel 2011). Informed by the pediatric neurology (Bauman 2010; Bauman and Kemper 2005; Goldson and Bauman 2007) and developmental and behavioral pediatrics perspectives (Yin et al. 2013), our approach provides an understanding of healthcare encounter-level interactional processes that has both applied and theoretical value for autism research. To better illustrate the analytic rigor of this approach, we briefly outline conceptual foundations and research applications of CA and DA.
Conversation Analysis
CA’s focus on the use of language to accomplish social actions (Schegloff 2007) has turned it into a robust methodology for the analysis of medical encounters (Heritage and Maynard 2006a,b). Researchers studying social interaction in medical contexts have used CA to examine the overall structure of healthcare visits, the specific activities within the visits (e.g. problem presentation, treatment phase), the turn sequences in the visit (e.g. greetings, opening questions), or the design of the turns themselves (e.g. turn construction practices) (Heritage 2009; Heritage and Robinson 2006; Robinson and Heritage 2005). CA has been used extensively to examine recurrent patterns of child-parent-doctor interactions during healthcare visits (e.g. Stivers 2007, 2011)
Recent years have witnessed a considerable extension both of the CA methods and of their application to domains of medicine. Research on gaze, body movement, spatial alignments and medical instrumentation has elaborated CA into a multi-modal approach and has extended its reach into fields such as surgery (Mondada 2011), anesthesiology (Hindmarsh and Pilnick 2007), dentistry (Hindmarsh et al. 2011), and the uses of imaging technologies (Nishizaka 2013). CA methods have also been applied to medical specialties such as cancer (Beach and Anderson 2003), autoimmune deficiency syndrome (Peräkylä and Bor 1990), orthopedics (Hudak and Maynard 2011; Maynard and Hudak 2008), pediatric pain management (Clemente 2009), and a variety of aspects of childbirth (Kitzinger 2011). CA has also been used in studies of sensitive medical care topics such as future illness progression and end of life (Parry et al. 2014).
The quantitative extensions of CA have generated significant advances in the statistical modeling of outcomes of interactional practices, for example, determining the influence of question design on patient responses (Heritage and Robinson 2006; Robinson and Heritage 2005, 2006; Heritage et al. 2007), the significance of physicians’ opening remarks introducing vaccinations for parental adherence to the recommended vaccination regime (Opel et al. 2013), and how the effectiveness of clinicians’ recommendations against antibiotics is shaped by other characteristics of communication during the medical visit (Mangione Smith et al. 2006). These advances have led to the notion of a ‘conversation analytic intervention’ that captures the role of CA in intervention research (Robinson and Heritage 2014). In addition, CA has been effectively used for diagnostic purposes, e.g. in the development of diagnostic techniques to distinguish between patients who have suffered epileptic seizures from those who have not (Plug and Reuber 2009; Schwabe et al. 2007), and between patients experiencing dementia from those with other forms of memory loss (Jones et al. 2015).
CA has been used widely in research on various interactional aspects of autism (Dickerson et al. 2007; Korkiakangas et al. 2012; Marlaire and Maynard 1990; Maynard 2005; Maynard and Marlaire 1992; Muskett et al. 2010; Sterponi and Fasulo 2010; Stribling et al. 2007; Turowetz 2015), as well as schizophrenia (McCabe 2009), aphasia (Goodwin 2003; Wilkinson et al. 2007) and learning disabilities (Antaki and Wilkinson 2012).
Discourse Analysis
DA builds a wider analytic frame than does CA to understand interactional sequences by reaching beyond the ‘here and now’ of social interactions to enrich a sense of their context and to examine the circumstances and the sentiments that inform them. DA usually employs ethnographic and interpretive methodology that has been used in several branches of linguistics, and in psychology, sociology, anthropology, and education research (Schiffrin et al. 2001; Tannen et al. 2015).
The DA’s applications in medicine have been growing steadily in the past decades (Jones 2015). DA has been used in medical anthropology to elucidate the meanings, experiences, sensibilities and dilemmas that reside below the surface of people’s talk during medical visits (Mishler 1984; Strong 1979; Todd and Fisher 1993). Its application by physician-scholars such as Howard Waitzkin (1993) and Rita Charon (2001) has transformed the everyday practice of medicine.
The first application of DA to the study of autism in the U.S. was carried out on the ‘UCLA’s Ethnography of Autism’ project founded by clinical psychologist Lisa Capps (Losh and Capps 2003, 2006) and linguistic anthropologist Elinor Ochs, following their collaboration on family discourse and agoraphobia (Capps and Ochs 1995a b; Ochs 2002, 2015; Ochs and Solomon 2010; Ochs et al. 2004, 2005). It also has been used in a longitudinal mixed methods study ‘Autism in Urban Context’ for which data analyzed in this article were collected, that examines disparities in ASD diagnosis, interventions and services experienced by African American children with ASD and their families (Angell and Solomon 2014; Solomon and Lawlor 2013; Solomon et al. in press). Furthermore, DA has been widely used in research on social interactions and experiences of people with other conditions such as Alzheimer’s disease (Hamilton 1994) and traumatic brain injury (Coelho 1999).
In summary, in this article we use a mixed methods CA and DA approach to begin bridging macro- and micro-level processes in the study of medical problem presentation of children with ASD to better understand the causes of ‘diagnostic overshadowing’ and foregone care (Bauman 2010; Siegel and Gabriels 2014). Such a methodology is especially useful for the study of issues relevant to families of children with ASD and healthcare providers who serve them, and has a strong potential for developing empirically-grounded recommendations for clinical practice.
Recruitment, sample and data
The TD children’s data were collected for a pilot study on acute primary care visits. A total of seventy children’s visits with five pediatricians were video-recorded. The children were recruited through the pediatrician’s referral and were of elementary school age, predominantly white and middle class, and all lived in Southern California. The cases presented in the article are intended to be illustrative of the identified contrasts with the ASD cases rather than representative of the corpus itself, or of subsequent corpora that were collected, which has been done elsewhere (e.g. Stivers 2007; Mangione-Smith et al. 2006).
The healthcare visits of children with ASD were collected as part of an ethnographic, mixed methods study on African American families’ experiences of ASD diagnosis, interventions and services in Southern California (R01 MH089474, 2009–2012, O. Solomon, P.I.). A detailed description of the study can be found in Solomon and Lawlor (2013) and Solomon et al. (in press). The participants were recruited through four California Department of Developmental Disabilities regional centers, a children’s hospital, and a University Center for Excellence in Developmental Disabilities. Twenty-three families with a total of 25 children, 22 boys and 3 girls with ASD (APA 2000). participated in the study. The children were between 4 and 11 years old during data collection. For this article, we analyzed a sub-corpus of 16 healthcare visits involving 4 children with ASD, 4 mothers and 2 fathers; and 7 physicians: two pediatricians, one family practitioner, and three specialists. We also analyzed narrative interviews with 12 mothers and 4 doctors about their experiences during the visits and other related topics (Solomon et al. in press).
Data Analysis
CA was conducted through moment-by-moment analysis of video and transcripts that used CA conventions (Jefferson 2004). We identified communicative patterns that are so recurrent they can be defined as ‘practices’, designed to project a predictable range of responses. Collections of these practices were compiled to establish the range of interactional strategies used by the participants. Similar to CA, DA was conducted through multiple viewings and the moment-by-moment analysis of transcribed video- or audio- recorded interactions, but the analysis was focused on the participants’ perspectives and meanings. Beyond an utterance-by-utterance analysis of single interactions, DA was used to identify themes present within and across the data sample (e.g. Angell and Solomon 2014; Solomon 2004; Solomon and Lawlor 2013; Solomon et al. in press).
Results
Greeting sequences and speaker selection in problem presentation initiations
As a socio-cultural practice, greetings establish the conditions for a social encounter (Duranti 1997). They function as an acknowledgement of the other’s presence (Searle 1969; Schegloff 1979, 1986), while also marking him or her as a “distinct being worth recognizing” (Duranti 1997, p. 67). People use greetings to acknowledge and quickly negotiate ‘who is who to whom’.
In healthcare, patient-provider greetings mark the start of the visit (Robinson 1998), and are critical in establishing rapport and making patients and their family members feel comfortable (Amer and Fisher 2009; Makoul et al. 2007). Following the greetings, the provider ordinarily initiates the problem presentation (Robinson 2006, Heritage and Maynard 2006a b) by asking a question, often accompanied by eye gaze and body orientation, that selects the next speaker who could be the child (O:kay:. Irene:. What’s up.), the mother (What brings him here today?) or ambiguously both the child and the mother (How are we doing?) (Stivers 2001). An anticipated response to these questions is an account of the child’s health problems that, in a predictable fashion, may be provided by the child, the mother, or both. The predictable nature of such opening sequences - a greeting followed by speaker selection to initiate the problem presentation – is founded in the mutual orientation of the participants to identifying and addressing the child’s health problems and needs (Pilnick et al. 2009).
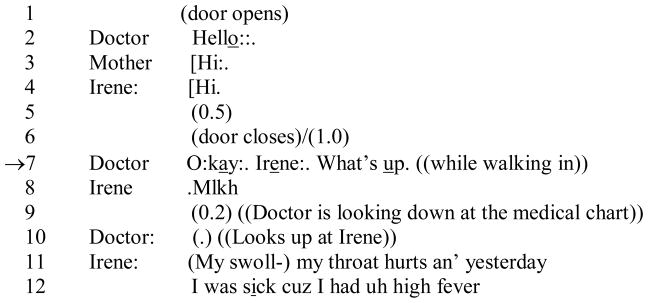
Speaker selection indexes the epistemic and interactional ‘rights’ to telling about the problem. Consider the brevity and effortlessness of the following greeting sequence, and the seamless transition to a problem presentation (Jefferson 1989) in which the doctor selects the child as the next speaker. The initiations of problem presentation are marked with an arrow (→).
Opening 1: TD Child.
Video analysis of this opening sequence shows that the doctor’s ‘hello’ in line 2, uttered while he is entering the room, is not specifically addressed to either the patient, Irene, or her mother by his gaze or in any other way. Both the mother and the child answer ‘Hi’ (overlapping lines 3 and 4). In line 7, the doctor then projects the next stage of the visit (O:kay:.), calls the child by name (Irene:.) and selects her as the next speaker in the problem presentation sequence (What’s up). As soon as the doctor looks up at Irene from the medical chart, she responds with a beginning of ‘pre-visit’ account of her health problems in lines 11 and 12.
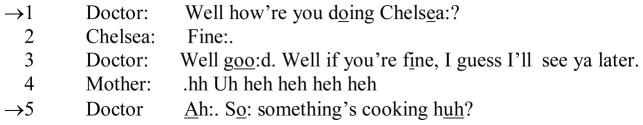
A similarly straightforward acknowledgement of a TD child’s identity and ‘rights’ to tell what problem brought her to the doctor’s office can be seen in the example below:
Opening 2: TD Child.
In this excerpt, the doctor’s greeting in line 1 is also an initiation of problem presentation directed to the child who responds to it as if it were a conventional ‘how are you’ (Robinson 1998, 2006). In response to Chelsea’s ‘Fine’, the doctor jokingly threatens to leave in line 3 (I guess I’ll see ya later.), before transitioning into the beginning of problem presentation with (So: something’s cooking huh?) in line 5.
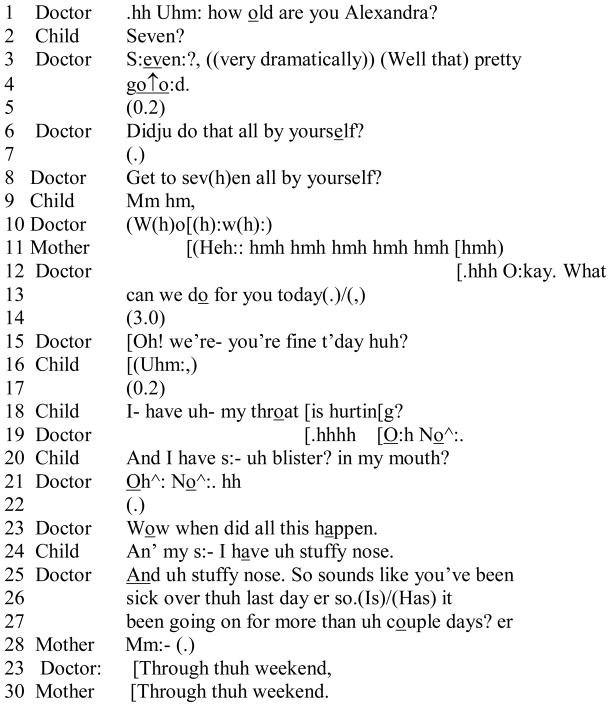
In our final example of an opening sequence involving a TD child, we see the doctor engaging the patient by calling her by name and asking her age (line 1).
Opening 3: TD child.
Playfully building on this opening, the doctor goes on to invite Alexandra to present the reason for her visit, finally transitioning to address her mother ((Is)/(Has) it been going on for more than uh couple days? er) in lines 26 and 27 about the onset of the symptoms a typical transition for a child of this age (Stivers 2007).
As exemplified by these segments, the greeting sequences in TD children’s visits data are characterized by seamless turn-taking (Hello::. Hi:. Hi) accomplished without significant delay (Jefferson 1989; Sacks et al. 1974). These greeting sequences are a site where a provisional agreement is established by the participants on ‘who is who to whom’, including an evaluation of what kind of an interactant the child is. This momentary evaluation of the child’s personhood evinced by how he or she participates in the greeting sequence, gives the doctor a basis for making interactional choices regarding how much to engage the child as a speaker in the problem presentation.
The seamless nature of TD child-parent-doctor interactions is often conveyed through metaphors of ‘social choreography’ and ‘dance of three partners’ (Aronsson and Rindstedt 2011; Clemente 2009; Gabe et al. 2004; Tates et al. 2002). By contrast, our analysis of greeting sequences in visits of children with ASD reveals that even such a seemingly simple sequence may become a difficult to accomplish interactional achievement that takes many more turns and a much longer time to carry out than the greetings in the TD children’s data. Moreover, establishing ‘who is who to whom’ and positioning the child with ASD as a certain kind of a participant in the visit takes more interactional work, as we show below.
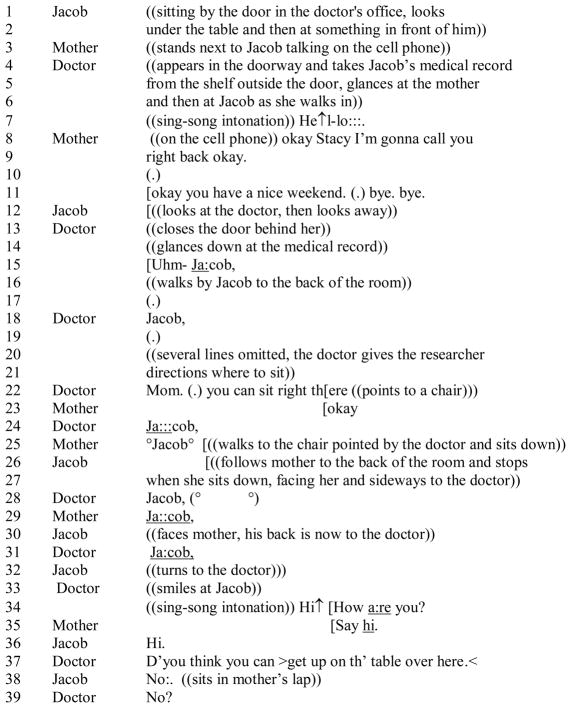
Consider the following interaction when Jacob, a nine-year old boy who has been diagnosed with ASD, and his mother came to see their family physician, Dr. Green, for a routine check up and to get help with Jacob’s allergies. Similar to example 1, the doctor says ‘hello’ as she is coming through the door (line 7). In this case, however, neither the mother who is on the cell phone, nor the child responds.
Opening 4: Child with ASD.
Subsequently to her initial ‘hello’ in line 7, the doctor elicits attentional engagement from Jacob by repeating his name five times (line 15, 18, 24, 28, and 31). After Jacob turns to the doctor in line 32, she renews her greeting (line 34) and Jacob responds (Hi.) in line 36 after being prompted to do so by his mother in line 35. A total of 19 seconds elapses between the doctor’s first ‘He↑l-lo:’ and Jacob’s response in line 36. The doctor’s next turn is to ask Jacob to sit on the exam table, to get him in position for a physical examination (line 37), which Jacob declines in line 38, getting into his mother’s lap instead.
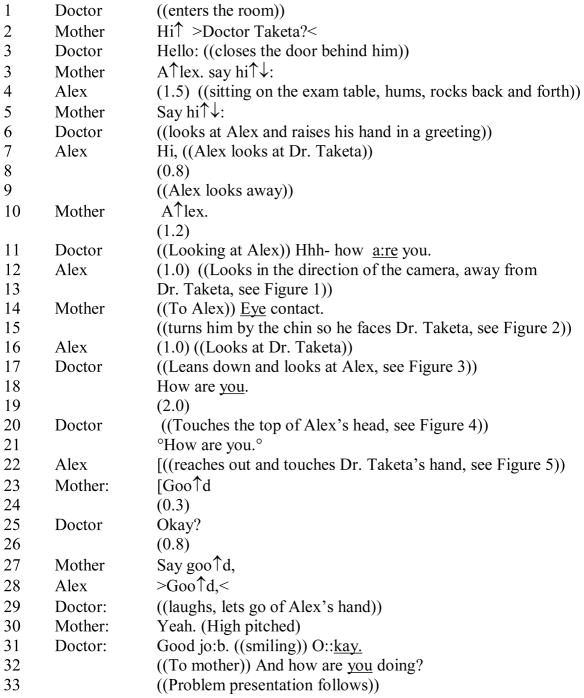
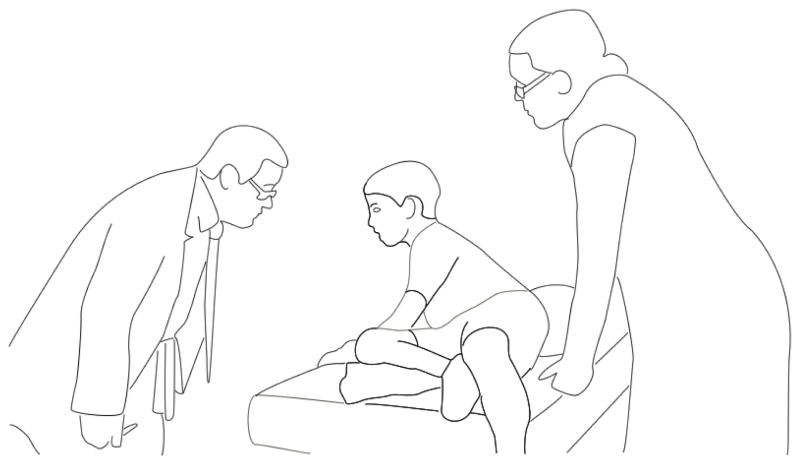
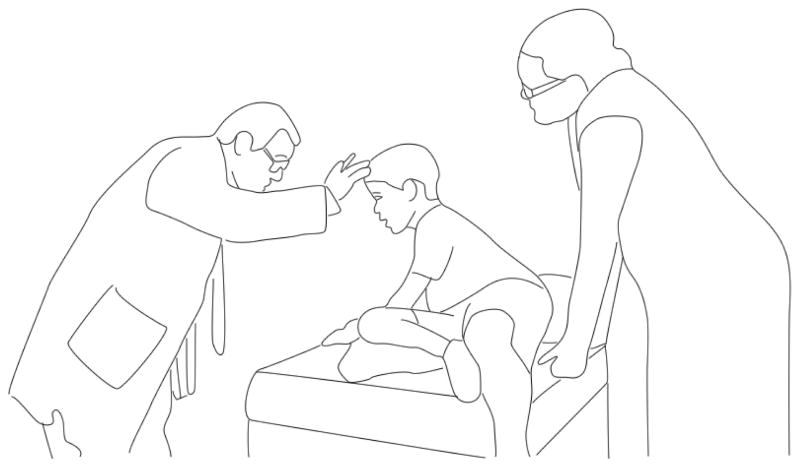
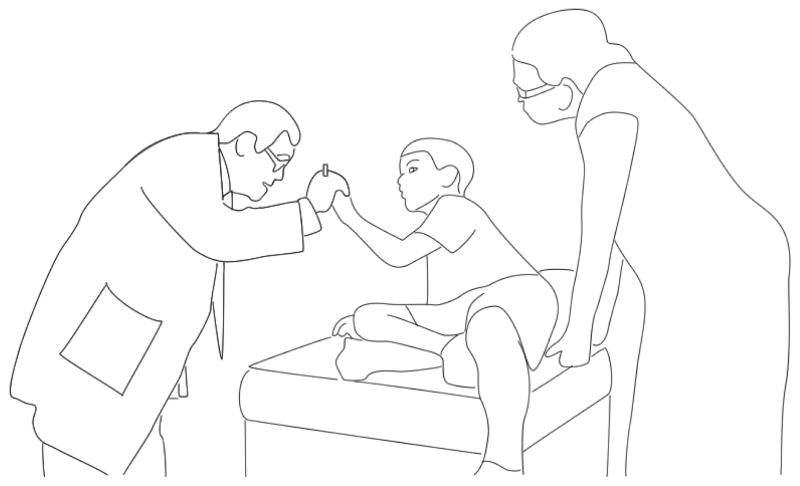
The attentional management of opening sequences may be more challenging for a child with severe ASD symptoms. Consider the opening sequence that was recorded during a visit that Alex, whose mother, Simone, was quoted in the beginning of this article, had with his pediatrician, Dr. Taketa. Alex’s spoken language is limited (Tager-Flusberg and Kasari 2013), and he is considered ‘nonverbal’ by most doctors who see him, but not by his mother. In the following segment, the opening sequence is accomplished over a 23 second period through a series of actions to coordinate Alex’s facial orientation, eye gaze and vocalizations into a reciprocal interaction with Dr. Taketa. The line drawings, created from video frames, show how Simone shapes Alex’s body into a normative posture indexing attention and social engagement (Solomon 2011). Noticeable here is the considerable amount of coordinated, joint effort by both the doctor and the mother oriented to the task of achieving an extended greeting between Alex and the doctor, despite the fact that Alex produced a prompted (lines 3 and 5), responsive ‘Hi,’ in line 7.
Opening 5: Child with ASD.
In this case, as the transcript shows, Dr. Taketa invests considerable effort in recognizing Alex and engaging him as a co-interactant. Simone is also strongly invested in this enterprise, as both the transcript and the article’s opening quotation illustrate. In an ethnographic interview Dr. Taketa, who made ASD his practice specialty, reflected on his experiences (see also Solomon et al. in press): “It’s too easy to get frustrated and be dismissive of some of the difficult autistic children, because they’re running around the office more, they may be more destructive, it’s hard, very hard to do an exam, you don’t know how far you’re getting through.” In spite of these difficulties, Dr. Taketa described children with ASD as intentional actors with rich subjectivity:“They have the logic going on in their own brain. They’re interpreting the world in a different way, they’re speaking a different language, so the burden is upon me to understand them as much as it is for them to understand our world. No, it’s not about decreased intelligence, it’s a different world. That’s what I keep in mind. That helps me”.
In this interview excerpt, Dr. Taketa explains how, for him, ASD has turned from a problem of impaired communication to a problem of “a different language” that he takes upon himself to master, and of a “different world” that, he believes, he can understand. The effort that Dr. Takeda makes to engage Alex in a greeting testifies to his commitment to interact with Alex as a person in his own right, to “see” and “know” Alex as someone worthy of recognition, and by extension, worthy of the effort of providing high quality care. Dr. Taketa’ effort also affirms Simone’s orchestration of Alex’s ‘presentation of self’ during this healthcare visit (Goffman 1955) that inevitably, for Simone, is linked to
Dr. Taketa’s perception of Alex as a responsive, speaking, and relational being (Solomon et al. in press). The significance of Simone’s efforts is supported by studies showing that doctors are more likely to view a patient positively if they perceive the patient to have positive affect (Street et al. 2007). Micro-level analysis of such interactions provides a lens onto other kinds of work that Simone and other mothers of children with ASD carry out both at the doctor’s office, and at home when their children become ill. The next section describes this interactional work in more detail.
Problem presentation and the intersubjective accessibility of children’s illness experiences
Comparing and contrasting video-recorded problem presentation sequences of TD children and children with ASD, we identified the following interactional dynamic: even when the mother was the primary informant about the TD child’s medical problem, the child was presented as a corroborative witness and experiencer of that problem. In our data, a TD child’s health problem was frequently constituted via a mother’s narrative account about eliciting and attending to the child’s complaints and descriptions of discomfort at home; closely observing the child’s physical appearance and behavior changes; and comparing her observations with what she considers ‘usual’ for her child. The child’s health problem may also be grounded in the mother’s description of the frequency, appearance and change of the child’s upper respiratory and nasal discharge, vomiting, diarrhea, and other physical manifestations of illness. Such ‘pre-visit’ epistemic and interactional work is premised upon two tacit expectations: that the child is intersubjectively ‘readable’ and comprehensible to the mother (Solomon and Lawlor 2013), and that the child possesses the self-reflective and communicative competence to participate in the ‘pre-visit’ epistemic work by describing and indicating discomfort and other experiences.
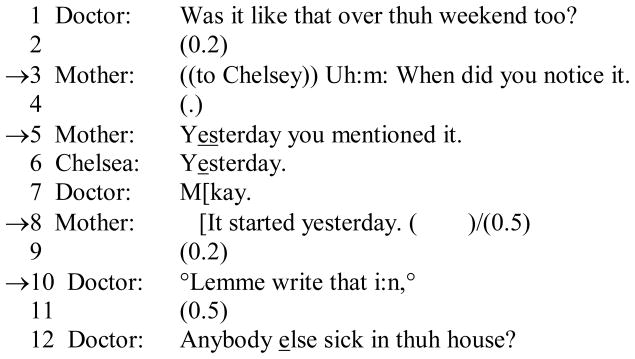
In the following example, the pediatrician’s question about the onset of symptoms is the object of corroborated recollection between an eleven-year old TD child, Chelsea, and her mother. The mother’s first question at line 3 asks Chelsey when she noticed the symptoms, and subsequently the mother makes a distinction between her daughter’s ‘noticing’ the symptoms and ‘mentioning’ them to the mother the previous day (line 5). Chelsea then confirms ‘yesterday’ as the point at which her symptoms emerged.
Presenting problem 1: TD Child.
Here both mother and pediatrician treat ‘yesterday’ as the answer of record (at lines 7, 8 and 10) only after the child’s confirmation at line 6. In this excerpt, the child is treated as an agentive participant in the conversation, and the mother as an observer, interpreter and historian of her daughter’s experiences and signs of illness.
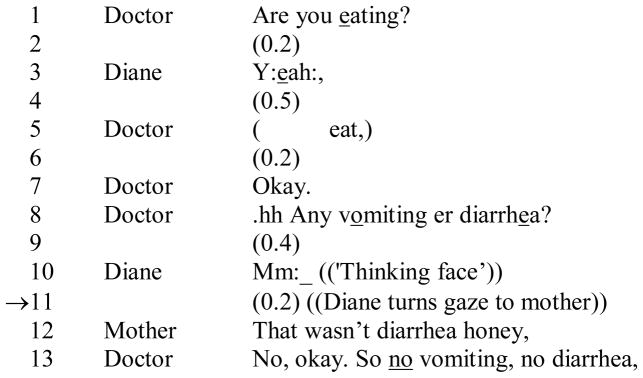
In cases where children may be unable to answer a question by themselves, they and their caregivers can make references to previous common experiences, as in the next case where the child, Diane, aged nine, has difficulty in answering a question about vomiting and diarrhea. Faced with this question (line 8), she hesitates (line 9), assumes a ‘thinking face’ (line 10), and then turns to gaze at her mother (line 11). At this point the mother unhesitatingly offers an evaluation of what Diane has silently evoked as a past, potentially problematic occurrence, the knowledge and significance of which they both share (line 12):
Presenting problem 2: TD Child.
It is noticeable that the mother’s response, which is registered by the pediatrician at line 13, was directed to the child, Diane, and that Diane’s silent query is itself a component of the conclusion that the pediatrician proceeds to enter into the patient’s chart. The important insight here lies in the reference to the previous experiences in the home, accomplished by only eye gaze that Diane directs at her mother. The child and her mother demonstrate to each other and to the doctor that they both remember, share and agree upon an interpretation of Diane’s past experience that could be a sign of illness.
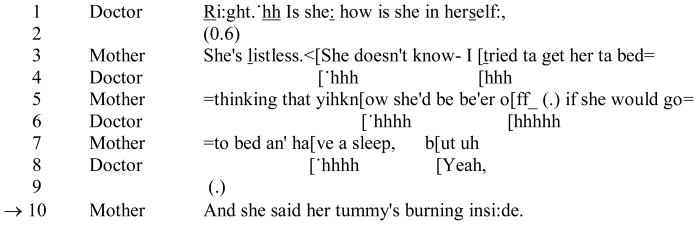
Finally even where the child is not physically present, as in the following ‘after hours’ phone call to a primary care physician, the mother unhesitatingly quotes the conversation she has had with her four year old daughter about her symptoms (line 10):
Presenting problem 3.
TD Child
Here, although the child is physically absent, she is framed in the mother-doctor phone conversation as an agent whose description of her experiences (‘she said her tummy’s burning insi:de’) and, by extension, her previous conversation with her mother about them, are presented as direct reported speech. These three excerpts demonstrate the social enactment of agency, accountability and personhood that is unhesitatingly attributed to even quite young TD children in pediatric settings, and is successfully taken up by them.
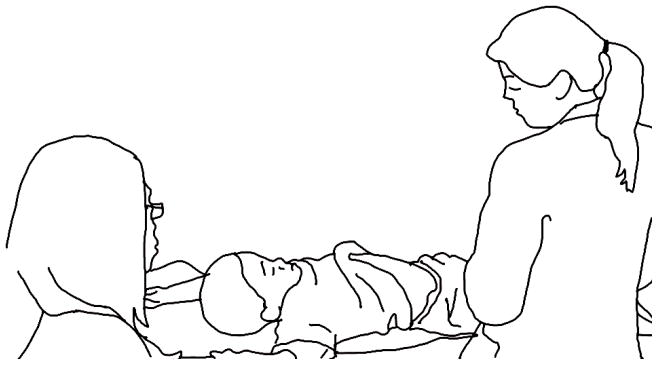
Such accounts are rare in the data of children with ASD. In the example below, Leo, who is 8 years old and who was diagnosed with ASD at age 3, is asked by his gastroenterologist to point to a place where his stomach hurts. Instead of pointing, he responds by inflating his stomach so it moves up and down five times, a response that the doctor treats as amusing but insufficient as she immediately redirects her question to Leo’s mother. Leo’s father is also in the room during the visit, however, most of the questions that the doctor asks, including the question about the location of Leo’s stomach pain, are directed to and are answered by the mother, which indicates the doctor’s and the mother’s mutual orientation to her accountability as the main historian, observer and interpreter of Leo’s illness experiences and symptoms.
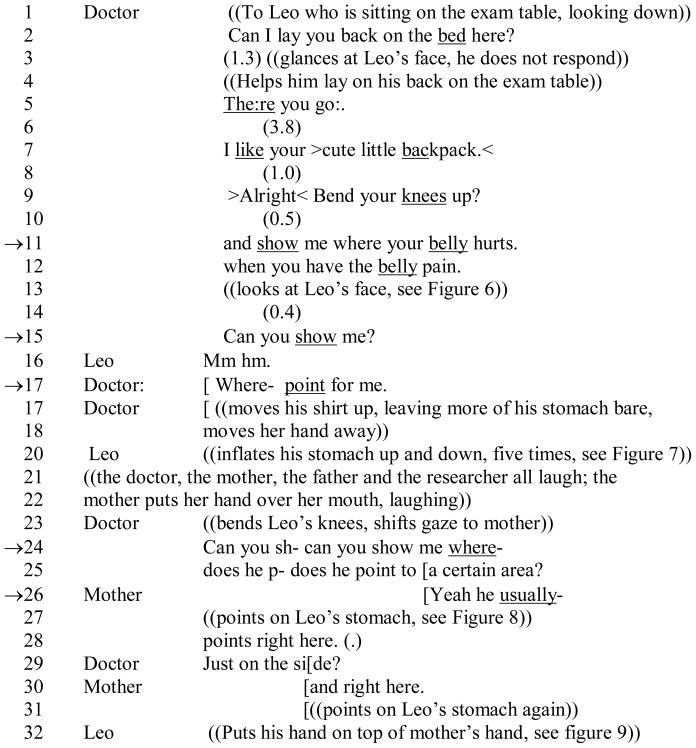
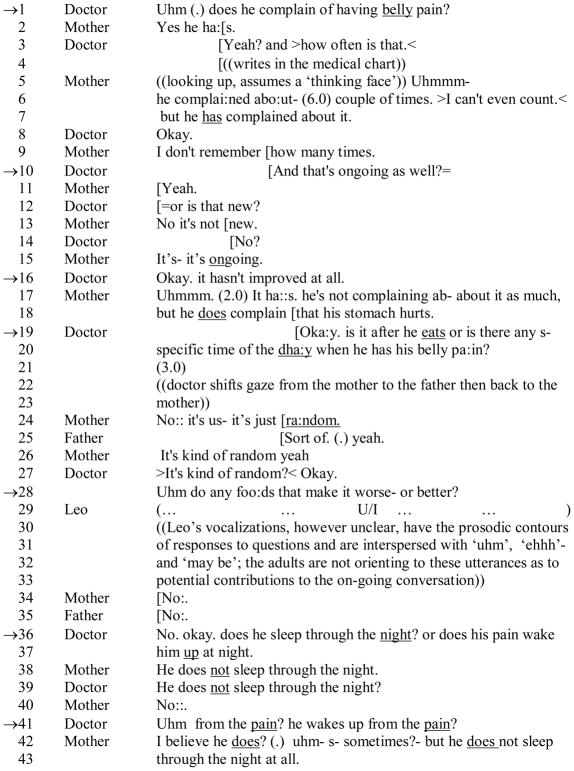
Presenting Problem 4: Child with ASD.
Leo responds affirmatively with (Mm hm. ) at line 16 to the Doctor’s request in lines 11 and 12 (show me where your belly hurts when you have the belly pain), which, after a pause and the doctor’s expectant gaze at Leo’s face, is followed by another request, a question at line 15 (‘Can you show me?’). Leo’s reply ‘Mm hm.’ (line 16) indicates that he may know that he has been selected as a next speaker and that he is to take the next turn or make the next move. When the doctor pursues her request for information a second time at line 17 (Point for me), Leo gives an embodied response in line 20, inflating his stomach up and down five times. However amusing this response is to the doctor, it is framed as inadequate relative to her request for a demonstrative point. She immediately turns to the mother for guidance: Can you sh- can you show me where- does he p- does he point to a certain area? (lines 24 and 25). When the mother describes and points on Leo’s stomach the location of pain that he has indicated to her in the past (lines 26, 27, 28, 30 and 31), Leo immediately places his hand on top of his mothers’ (line 32).
This action raises an important, but epistemologically problematic, question concerning how intersubjectivity may be accomplished with individuals diagnosed with ASD. On the one hand, Leo’s action may be seen as a purely behavioral response to the sensation of the mother’s hand on his stomach. A more ‘generous’ interpretation (Ochs and Solomon 2010), however, would be to infer that Leo is joining his mother in indicating the location of his pain. Perhaps a mother’s extensive embodied, haptic and relational experience and knowledge of her child (De Wolfe 2014; Eyal and Hart 2010; Lawlor 2004; Silverman 2011; Solomon and Lawlor 2013) may enable her to respond to the question regarding the location of his pain. Here we simply note that our observer’s problem in understanding these data is one which we share with the doctor and, to some degree, perhaps with the mother as well.
The remarkable feature of this child-mother-doctor interaction is, first, that there is a distributed way to locate ‘the belly pain’ carried out by Leo (by inflating his stomach) and his mother (by pointing on its surface). Second, the mother’s response implies that at home, or somewhere other than in the doctor’s office, Leo is able to carry out the action that he was just unable to carry out for the doctor, i.e. to point to the place on his body where he experiences pain. Thus, Leo’s mother portrays him as an accountable experiencer, communicator and epistemic ‘owner’ of his illness, and thus as a child who is ‘readable’ and intersubjectively accessible to her (Solomon and Lawlor 2013). It has been suggested that children with ASD may have atypical perception of pain (American Psychiatric Association 2013), which potentially makes indicating its location more challenging on top of the communicative limitations associated with an ASD diagnosis.
Leo may also face other difficulties during this healthcare visit that are linked to the morpho-syntactic properties of the doctor’s utterances directed to him. First, the flow of the doctor’s talk and her other social actions include a complement on Leo’s ‘cute little backpack’, a directive to bend his knees, a manipulation of Leo’s body, and then a question about the location of his stomach pain. In order to parse and comprehend these actions, and to locate ‘show me where your belly hurts’ (line 11) as the question that warrants a response, Leo needs to be what Jefferson (1984) called “other-attentive”, i.e. able to attend to the doctor’s concerns and to know how to indicate and describe his pain to her in ways that make it understandable. Second, if he was not having stomach pain when the doctor asked “show me where your belly hurts” (line 11), it may be difficult for him to have a non-literal, asynchronous interpretation and infer that the doctor is referring to real events projected into the indefinite past. We are left to wonder whether Dr. Taketa’s ‘different language’ approach to communication with children with ASD may have resulted in different turn-construction practices and morpho-syntactic structures in such an interaction. These difficulties may point to a set of problems linked to the nature and the logic of a ‘project’ that constitutes a healthcare visit, i.e. that the questions about Leo’s stomach pain relate to Leo’s previous experiences, and necessitate that he is able to both access and narrate them with others’ worldview in mind. These are exactly the kinds of events, however, that TD children and their mothers come together to address in their ‘pre-visit’ epistemic and interactional work that becomes articulated to the doctor during problem presentation.
The intersubjective accessibility of Leo’ s illness experience appears uncertain in the rest of this visit as well. This can be gleaned from the following interaction that took place during history-taking phase earlier in the visit than the interaction discussed above. This example shows the complexity of interpreting pain and discomfort experienced by a child with ASD who communicates verbally but still may be unable to describe his experiences, leaving his parents without a corroborated account.
In the following example, the doctor is seated facing Leo’s mother and father, who are seated next to one another while Leo is standing between them:
Presenting problem 5: Child with ASD.
This excerpt shows the doctor’s attempts to establish history of Leo’s stomach pain (lines 1, 3, 10, 12, 16, 19, 20, 28, 36, 37, 39 and 41) and the difficulty that Leo’s parents have in describing his symptoms, their timing and even whether they are associated with him waking up at night. These descriptions point to the challenges that Leo’s mother and father face in having the kinds of “pre-visit” conversations with Leo that we have described in the three examples involving TD children.
Discussion
Physicians working in the U.S. pediatric primary and specialty care settings see a significant percentage of children diagnosed with ASD (APA 2000, 2013), yet how this condition affects child-parent-doctor communication during medical problem presentation has not been sufficiently examined. Large-scale studies (e.g. Croen et al. 2006; Kogan et al. 2008) have presented a contradictory picture of increased healthcare utilization co-occurring with unmet healthcare needs, which has been attributed to several separate factors: the children’s communicative limitations; ambiguous symptom presentation; atypical displays of discomfort; and sensory, vestibular and self-regulatory challenges that affect their behavior and make participation in the healthcare encounter difficult (Goldson and Bauman 2007; Lajonchere et al. 2012). Our goal was to describe social processes and interactional patterns that reveal how such challenges converge during pediatric encounters to influence child-parent-doctor communication, potentially negatively affecting quality of the children’s healthcare and contributing to mis-diagnosis, foregone medical care, and unmet healthcare needs.
We have described two frequently encountered difficulties in visits with children diagnosed with ASD: recognition of the child as an agentive patient that is highly desirable on socio-medical and ethical grounds, and yet is difficult to achieve; and problem presentation and symptom descriptions that present difficulties for children with ASD and their parents. In particular, children with ASD may be unavailable for the kinds of “pre-visit” problem-oriented conversations with their parents that allow the latter to present corroborated symptom reports grounded in children’s experiences. Children with ASD may also have difficulty with certain language practices, including morpho-syntactical constructions that depend on perspective-taking or other abilities that are part of normative communicative competence tacitly expected of children during healthcare visits. This may hinder the visit’s progress while, simultaneously, undermining the significance of the child as a subject-actor in the context of his or her own medical needs.
Our contrastive analysis of the healthcare encounters data of TD children and children with ASD also points to a larger challenge of socializing children with ASD into the role of competent recipients of healthcare, a process that is tacitly taken for granted in healthcare encounters of TD children where the gradual attribution of responsibility to provide medically-relevant information increases with the child’s age (Cahill and Papageorgiou 2007; Stivers 2011; Stivers and Majid 2007; Tates and Meeuwesen 2000). These processes of, and opportunities for, socialization into an increasingly competent patient role can be clearly seen during video-analysis of healthcare visits, in the sequential organization of greeting sequences at the onset of the visit that acknowledges the child as a competent and responsive interactant, and in the minutia of turn-taking, e.g. in a doctor’s fleeting glance to the child’s face while waiting for a reply to a questions, before the doctor shifts the gaze to the parent. The paucity of these opportunities and expectations for a responsive action of children with ASD may mean a lifelong challenge of receiving care (Nicolaidis et al. 2013) that is described in such detail by those researchers who document cases of serious and life-threatening conditions of adults with this diagnosis (e.g. Radcliffe 2013, Smith et al. 2012). Systematically adapting healthcare environments in ways that depart from the tacit expectations grounded in the TD children’s behavior during visits, and that provide more socializing opportunities for children with ASD, may be a necessary first step in addressing the problem of ‘diagnostic overshadowing’ (Siegel and Gabriels 2014) and foregone care (Bauman 2010).
Our analysis has limitations in that we brought together white middle-class TD children’s healthcare encounters collected in more socio-economically advantaged areas of Los Angeles County to compare them with healthcare encounters of African American children with ASD of variable socio-economic status, collected in more disadvantaged areas of the Los Angeles County. While this may seem a problematic comparison, we argue that the tacit expectations of the processes presumed necessary for the interactional achievement of the healthcare visits are powerfully organized by the behavior and capabilities of the white middle class TD pediatric population who are perceived to be the ‘norm’ of comportment, communication and self-directed insight about their illness experiences (Stivers and Majid 2007).
Our analysis points to the critical need for additional resources and strategies that may facilitate how children with ASD function as corroborating witnesses of their own illness experiences and medical complaints. Because the healthcare encounter is the epicenter of healthcare, maximum inclusion of children with ASD in their encounters is consistent with the health equity goals for this traditionally underserved population and would be an important contribution to public health more generally.
FIGURE 1.
FIGURE 2.
FIGURE 3.
FIGURE 4.
FIGURE 5.
FIGURE 6.
FIGURE 7.
FIGURE 8.
FIGURE 9.
Acknowledgments
We thank all the children and their families who participated in this research. We thank Tanya Stivers for making the TD children’s data available for this comparative analysis. The data collection of healthcare encounters of children with ASD was supported by a grant ‘Autism in Urban Context: Linking Heterogeneity with Health and Service Disparities’ (R01 MH089474, 2009–2012, O. Solomon, P.I.). The content of this article is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Mental Health or the National Institutes of Health.
We are deeply grateful to the children and their families who participated in the two studies discussed in this article. The data corpus of healthcare visits of children with ASD was collected as part of a larger study ‘Autism in Urban Context: Linking Heterogeneity with Health and Service Disparities’ supported by the National Institute of Mental Health (R01MH089474, 2009–2012, O. Solomon, P.I.). The content of this article is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Mental Health or the National Institutes of Health. Olga Solomon thanks the members of the Autism in Urban Context research team: Mary Lawlor, ScD, Sharon Cermak, EdD, Marie Poulsen, PhD, Thomas Valente, PhD, and Marian Williams, PhD; and gratefully acknowledges the financial support for the Autism in Urban Context project provided by the Chan Division of Occupational Science and Occupational Therapy at the USC Ostrow School of Dentistry. A portion of this paper was presented by Olga Solomon as part of a keynote panel ‘Autism and Society: Taking Stock of the History and Meaning of Autism Research’ organized by Roy Richard Grinker at the International Meeting for Autism Research, Salt Lake City, UT, May 14, 2015.
Appendix: Glossary of transcript symbols (Jefferson 2004, p. 13–31)
- [
A left bracket indicates the point of overlap onset.
- =
Equal signs indicate no break or gap. A pair of equal signs, one at the end of one line and one at the beginning of a next, indicate no break between the two lines.
- (0.0)
Numbers in parentheses indicate elapsed time by tenths of seconds
- (.)
A dot in parentheses indicates a brief interval.
- ____
Underscoring indicates some form of stress, via pitch and/or amplitude.
- ::
Colons indicate prolongation of the immediately prior sound. The longer the colon row, the longer the prolongation.
- ↑↓
Arrows indicate shifts into especially high or low pitch.
- .,?
Punctuation markers are used to indicate ‘the usual’ intonation (falling, continuing, and rising, respectively).
- WORD
Upper case indicates especially loud sounds relative to the surrounding talk.
- °word°
Degree signs bracketing an utterance or utterance-part indicate that the sounds are softer than the surrounding talk.
- –
A dash indicates a cut-off.
- > <
Right/left carats bracketing an utterance or utterance-part indicate that the bracketed material is speeded up, compared to the surrounding talk.
- < >
Left/right carats bracketing an utterance or utterance-part indicate that the bracketed material is slowed down, compared to the surrounding talk.
- wohhrd
A row of ‘h’s within a word indicates breathiness.
- (( ))
Doubled parentheses contain transcriber’s descriptions.
- (word)
Parenthesized words and speaker designations are unclear.
Footnotes
Ethical approval statement: All procedures performed in this research were approved by the Institutional Review Boards of our respective universities and conducted in accordance with the ethical standards of the institutional and/or national research committees and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Contributor Information
Olga Solomon, Chan Division of Occupational Science and Occupational Therapy, University of Southern California, Los Angeles, USA.
John Heritage, Department of Sociology, University of California Los Angeles, Los Angeles, USA.
Larry Yin, Department of Pediatrics, USC Keck School of Medicine, University of Southern California, Los Angeles, USA; USC University Center for Excellence in Developmental Disabilities, Children’s Hospital Los Angeles, Los Angeles, USA; Chan Division of Occupational Science and Occupational Therapy, University of Southern California, Los Angeles, USA.
Douglas Marynard, Department of Sociology, University of Wisconsin-Madison, Madison, USA.
Margaret Bauman, Department of Anatomy and Neurobiology, Boston University School of Medicine, Boston, USA. Integrated Center for Child Development, Newton, USA.
References
- Accordino RE, Walkup JT. The medical and psychiatric evaluation of the nonverbal child. Journal of the American Academy of Child and Adolescent Psychiatry. 2015;54(1):3–5. doi: 10.1016/j.jaac.2014.09.018. [DOI] [PubMed] [Google Scholar]
- Amer A, Fisher H. “Don’t call me ‘Mom’”: How parents want to be greeted by their pediatrician. Clinical Pediatrics. 2009;48(7):720–722. doi: 10.1177/0009922809333973. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: American Psychiatric Publishing; 2000. text revision. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5. Washington, DC: American Psychiatric Publishing; 2013. [Google Scholar]
- Angell AM, Solomon O. The social life of health records: Understanding families’ experiences of autism. Social Science & Medicine. 2014;117:50–57. doi: 10.1016/j.socscimed.2014.07.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Antaki C, Wilkinson R. Conversation analysis and the study of atypical populations. In: Sidnell J, Stivers T, editors. Handbook of conversation analysis. New York: Blackwell; 2012. pp. 533–550. [Google Scholar]
- Aronsson K, Rindstedt C. Alignments and face-work in paediatric visits: Toward a social choreography of multiparty talk. In: Candlin CN, Sarangi S, editors. Handbook of communication in organisations and professions. Boston: de Gruyter; 2011. pp. 121–142. [Google Scholar]
- Atkinson JM, Heritage J. Structures of social action. Cambridge: Cambridge University Press; 1984. [Google Scholar]
- Bauman ML. Medical comorbidities in autism: challenges to diagnosis and treatment. The Journal of the American Society for Experimental NeuroTherapeutics. 2010;7(3):320–327. doi: 10.1016/j.nurt.2010.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bauman ML, Kemper TL. Structural brain anatomy in autism: what is the evidence? In: Bauman ML, Kemper TK, editors. The neurobiology of autism. 2. Baltimore: John Hopkins University Press; 2005. pp. 121–135. [Google Scholar]
- Beach WA, Anderson JK. Communication and cancer? Part I: The noticeable absence of interactional research. Journal of Psychosocial Oncology. 2003;21(3):1–23. [Google Scholar]
- Bethell CD, Lindly O, Kogan M, Zuckerman K. Health care quality for children: The position of autism spectrum disorder. In: Patel VB, Preedy VR, Martin CR, editors. Comprehensive guide to autism. New York: Springer; 2014. pp. 139–165. [Google Scholar]
- Cahill P. Children’s participation in their primary care consultations. In: Gardner H, Forrester M, editors. Analysing interactions in childhood: Insights from conversation analysis. West Sussex, UK: Wiley-Blackwell; 2010. pp. 128–145. [Google Scholar]
- Cahill P, Papageorgiou A. Triadic communication in the primary care paediatric consultation: A review of the literature. British Journal of General Practice. 2007;57(544):904–911. doi: 10.3399/096016407782317892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Capps L, Ochs E. Constructing panic: The discourse of agoraphobia. Cambridge: Harvard University Press; 1995a. [Google Scholar]
- Capps L, Ochs E. Out of place: Narrative insights into agoraphobia. Discourse Processes. 1995b;19(3):407–439. [Google Scholar]
- Charon R. Narrative medicine: a model for empathy, reflection, profession, and trust. JAMA. 2001;286(15):1897–1902. doi: 10.1001/jama.286.15.1897. [DOI] [PubMed] [Google Scholar]
- Cicourel AV. Evidence and inference in macro-level and micro-level healthcare studies. In: Candlin CN, Sarangi S, editors. Handbook of communication in organisations and professions. Vol. 3. Boston: de Gruyter; 2011. pp. 61–82. [Google Scholar]
- Coelho CA. Discourse analysis in traumatic brain injury. In: McDonald S, Code C, Togher L, editors. Communication disorders following traumatic brain injury. Hove: Psychology Press; 1999. pp. 55–79. [Google Scholar]
- Clemente I. Progressivity and participation: Children’s management of parental assistance in paediatric chronic pain encounters. Sociology of Health & Illness. 2009;31:872–888. doi: 10.1111/j.1467-9566.2009.01156.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clemente I, Lee S, Heritage J. Children in chronic pain: Promoting pediatric patients’ symptom accounts in tertiary care. Social Science & Medicine. 2008;66(6):1418–1428. doi: 10.1016/j.socscimed.2007.11.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Creswell JW, Fetters MD, Ivankova NV. Designing a mixed methods study in primary care. Annals of Family Medicine. 2007;2:7–12. doi: 10.1370/afm.104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Croen LA, Najjar DV, Ray GT, Lotspeich L, Bernal P. A comparison of health care utilization and costs of children with and without autism spectrum disorders in a large group-model health plan. Pediatrics. 2006;118(4):1203–1211. doi: 10.1542/peds.2006-0127. [DOI] [PubMed] [Google Scholar]
- Croen LA, Zerbo O, Qian Y, Massolo ML, Rich S, Sidney S, Kripke C. The health status of adults on the autism spectrum. Autism. 2015 doi: 10.1177/1362361315577517. [DOI] [PubMed] [Google Scholar]
- De Wolfe J. Parents of children with autism: An ethnography. New York: Palgrave Macmillan; 2014. [Google Scholar]
- Dickerson P, Stribling P, Rae J. Tapping into interaction: How children with autistic spectrum disorders design and place tapping in relation to activities in progress. Gesture. 2007;7(3):271–303. [Google Scholar]
- Duranti A. Universal and culture-specific properties of greetings. Journal of Linguistic Anthropology. 1997;7:63–97. [Google Scholar]
- Eyal G, Hart B. How parents of autistic children became ‘experts on their own children’: Notes towards a sociology of expertise. Berkeley Journal of Sociology. 2010;54:3–17. [Google Scholar]
- Gabe J, Olumide G, Bury M. ‘It Takes Three to Tango’: A Framework for Understanding Patient Partnership in Paediatric Clinics. Social Science & Medicine. 2004;59(5):1071–1079. doi: 10.1016/j.socscimed.2003.09.035. [DOI] [PubMed] [Google Scholar]
- Geertz C. “From the native’s point of view”: On the nature of anthropological understanding. Bulletin of the American Academy of Arts and Sciences. 1974:26–45. [Google Scholar]
- Goffman E. On face work: an analysis of ritual elements of social interaction. Psychiatry. 1955;18(3):213–231. doi: 10.1080/00332747.1955.11023008. [DOI] [PubMed] [Google Scholar]
- Goldson E, Bauman M. Medical health assessment and treatment issues in autism. In: Gabriels RL, Hill R, editors. Growing up with Autism: Working with school-age children and adolescents. New York: Guilford; 2007. pp. 39–57. [Google Scholar]
- Goodwin C. Conversational frameworks for the accomplishment of meaning in aphasia. In: Goodwin C, editor. Conversation and brain damage. New York: Oxford University Press; 2003. pp. 90–116. [Google Scholar]
- Halkowski T, Gill VT. Conversation analysis and ethnomethodology: The centrality of interaction. In: Bourgeault IL, DeVries R, Dingwall R, editors. Handbook of qualitative health research. London: Sage; 2010. pp. 212–228. [Google Scholar]
- Hamilton H. Conversation with an Alzheimer’s patient: interactional sociolinguistic study. Cambridge: Cambridge University Press; 1994. [Google Scholar]
- Henry CA, Nowinski L, Koesterer K, Ferrone C, Spybrook J, Bauman M. Low rates of depressed mood and depression diagnoses in a clinic review of children and adolescents with autistic disorder. Journal of Child and Adolescent Psychopharmacology. 2014;24(7):403–406. doi: 10.1089/cap.2014.0024. [DOI] [PubMed] [Google Scholar]
- Heritage J. Garfinkel and ethnomethodology. Oxford: Blackwell; 1984. [Google Scholar]
- Heritage J. Conversation analysis as an approach to the medical encounter. In: McKinlay JB, Marceau L, editors. e-Source: Behavioral and Social Science Research Interactive Textbook. Office of Behavioral and Social Science Research; 2009a. http://www.esourceresearch.org. [Google Scholar]
- Heritage J. Negotiating the legitimacy of medical problems. In: Brashers DE, Goldsmoth DL, editors. Communicating to manage health and illness. New York: Routeledge; 2009b. pp. 161–178. [Google Scholar]
- Heritage J. Territories of knowledge, territories of experience: empathic moments in interaction. In: Stivers T, Mondada L, Steensig J, editors. The morality of knowledge in conversation. Vol. 29. New York: Cambridge University Press; 2011. pp. 159–183. [Google Scholar]
- Heritage J. Epistemics in conversation. In: Sidnell J, Stivers T, editors. The handbook of conversation analysis. Vol. 121. Malden: Blackwell; 2012. pp. 370–394. [Google Scholar]
- Heritage J, Maynard D, editors. Communication in medical care: interactions between primary care physicians and patients. Cambridge: Cambridge University Press; 2006a. [Google Scholar]
- Heritage J, Maynard DW. Problems and prospects in the study of physician-patient interaction: 30 years of research. Annual Review of Sociology. 2006b;32:351–374. [Google Scholar]
- Heritage J, Robinson JD. The structure of patients’ presenting concerns: physicians’ opening questions. Health Communication. 2006;19(2):89–102. doi: 10.1207/s15327027hc1902_1. [DOI] [PubMed] [Google Scholar]
- Heritage J, Robinson JD, Elliott M, Beckett M, Wilkes M. Reducing patients’ unmet concerns: the difference one word can make. Journal of General Internal Medicine. 2007;22:1429–33. doi: 10.1007/s11606-007-0279-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hindmarsh J, Pilnick A. Knowing bodies at work: Embodiment and ephemeral teamwork in anaesthesia. Organization Studies. 2007;28(9):1395–416. [Google Scholar]
- Hindmarsh J, Reynolds P, Dunne S. Exhibiting understanding: The body in apprenticeship. Journal of Pragmatics. 2011;43:489–503. [Google Scholar]
- Hodgetts S, Nicholas D, Zwaigenbaum L, McConnell D. Parents’ and professionals’ perceptions of family-centered care for children with autism spectrum disorder across service sectors. Social Science & Medicine. 2013;96:138–146. doi: 10.1016/j.socscimed.2013.07.012. 2013. [DOI] [PubMed] [Google Scholar]
- Hudak PL, Clark SJ, Raymond G. How surgeons design treatment recommendations in orthopaedic surgery. Social Science & Medicine. 2011;73:1028–1036. doi: 10.1016/j.socscimed.2011.06.061. [DOI] [PubMed] [Google Scholar]
- Hudak PL, Maynard DW. An interactional approach to conceptualising small talk in medical interactions. Sociology of health & illness. 2011;33(4):634–653. doi: 10.1111/j.1467-9566.2011.01343.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jefferson G. Glossary of transcript symbols with an introduction. Pragmatics and Beyond New Series. 2004;125:13–31. [Google Scholar]
- Jefferson G. Preliminary notes on a possible metric which provides for a ‘standard maximum’ silences of approximately one second in conversation. In: Roger D, Bull P, editors. Conversation: An interdisciplinary perspective. Clevedon: Multilingual Matters; 1989. pp. 166–196. [Google Scholar]
- Jefferson G. Stepwise transition out of topic to inappropriately next positioned matters. In: Atkinson JM, Heritage JC, editors. Structures of Social Action: Studies in Conversation Analysis. Cambridge: Cambridge University Press; 1984. pp. 194–222. [Google Scholar]
- Jones RH. Discourse and health communication. In: Tannen D, Hamilton HE, Schiffrin D, editors. Handbook of discourse analysis. 2. Malden: Wiley Blackwell; 2015. pp. 841–857. [Google Scholar]
- Jones D, Drew P, Elsey C, Blackburn D, Wakefield S, Harkness K, Reuber M. Conversational assessment in memory clinic encounters: Interactional profiling for differentiating dementia from functional memory disorders. Ageing and Mental Health. 2015 doi: 10.1080/13607863.2015.1021753. [DOI] [PubMed] [Google Scholar]
- Kitzinger C. Working with childbirth helplines: The contributions and limitations of conversation analysis. In: Antaki C, editor. Applied conversation analysis: intervention and change in institutional talk. New York: Palgrave Macmillan; 2011. pp. 98–118. [Google Scholar]
- Kogan MD, Strickland BB, Blumberg SJ, Singh GK, Perrin JM, van Dyck PC. A national profile of the health care experiences and family impact of autism spectrum disorder among children in the United States, 2005–2006. Pediatrics. 2008;122(6):e1149–e1158. doi: 10.1542/peds.2008-1057. [DOI] [PubMed] [Google Scholar]
- Korkiakangas TK, Rae JP, Dickerson P. The interactional work of repeated talk between a teacher and a child with autism. Journal of Interactional Research in Communication Disorders. 2012;3:1–25. [Google Scholar]
- Lajonchere C, Jones N, Coury DL, Perrin JM. Leadership in health care, research, and quality improvement for children and adolescents with autism spectrum disorders: Autism Treatment Network and autism intervention research network on physical health. Pediatrics. 2012;130:S62–S68. doi: 10.1542/peds.2012-0900C. [DOI] [PubMed] [Google Scholar]
- Lawlor MC. Mothering work: Negotiating health care, illness and disability, and development. In: Esdaile SA, Olson JA, editors. Mothering occupations: challenge, agency, and participation. Philadelphia: FA Davis; 2004. pp. 306–23. [Google Scholar]
- Lester JN, Paulus TM. Performative acts of autism. Discourse & Society. 2012;23(3):259–273. [Google Scholar]
- Levy A, Perry A. Outcomes in adolescents and adults with autism: A review of the literature. Research in Autism Spectrum Disorders. 2011;5:1271–1282. [Google Scholar]
- Liptak GS, Stuart T, Auinger P. Health care utilization and expenditures for children with autism: data from US national samples. Journal of Autism and Developmental Disorders. 2006;36(7):871–879. doi: 10.1007/s10803-006-0119-9. [DOI] [PubMed] [Google Scholar]
- Losh M, Capps L. Narrative ability in high-functioning children with autism or Asperger’s syndrome. Journal of autism and developmental disorders. 2003;33(3):239–251. doi: 10.1023/a:1024446215446. [DOI] [PubMed] [Google Scholar]
- Losh M, Capps L. Understanding of emotional experience in autism: Insights from the personal accounts of high-functioning children with autism. Developmental Psychology. 2006;42(5):809–881. doi: 10.1037/0012-1649.42.5.809. [DOI] [PubMed] [Google Scholar]
- Makoul G, Zick A, Green M. An evidence-based perspective on greetings in medical encounters. Archives of Internal Medicine. 2012;167(11):1172–1176. doi: 10.1001/archinte.167.11.1172. [DOI] [PubMed] [Google Scholar]
- Mangione-Smith R, Elliott MN, Stivers T, et al. Ruling out the need for antibiotics: Are we sending the right message? Archives of Pediatric and Adolescent Medicine. 2006;160:945–52. doi: 10.1001/archpedi.160.9.945. [DOI] [PubMed] [Google Scholar]
- Marlaire CL, Maynard DW. Standardized testing as an interactional phenomenon. Sociology of Education. 1990;63:83–101. [Google Scholar]
- Maynard DW. Social actions, gestalt coherence, and designations of disability: Lessons from and about autism. Social Problems. 2005;52(4):499–524. [Google Scholar]
- Maynard DW, Heritage J. Conversation analysis, doctor–patient interaction and medical communication. Medical Education. 2005;39(4):428–435. doi: 10.1111/j.1365-2929.2005.02111.x. [DOI] [PubMed] [Google Scholar]
- Maynard DW, Hudak PL. Small talk, high stakes: Interactional disattentiveness in the context of prosocial doctor-patient interaction. Language in Society. 2008;37(05):661–688. [Google Scholar]
- Maynard DW, Marlaire CL. Good Reasons for Bad Testing Performance: The Interactional Substrate of Educational Exams. Qualitative Sociology. 1992;15:177–202. [Google Scholar]
- McCabe R. Specifying interactional markers of schizophrenia in clinical consultations. In: Leudar I, Costall A, editors. Against theory of mind. New York: Palgrave Macmillan; 2009. pp. 108–125. [Google Scholar]
- Mishler E. The discourse of medicine: Dialectics of medical interview. New York: Greenwood; 1984. [Google Scholar]
- Mondada L. The organization of concurrent courses of action in surgical demonstrations. In: Streeck J, Goodwin C, Lebaron C, editors. Embodied interaction: Language and body in the material world. Cambridge: Cambridge University Press; 2011. pp. 207–26. [Google Scholar]
- Muskett T, Perkins M, Clegg J, Body R. Inflexibility as an interactional phenomenon: Using conversation analysis to re-examine a symptom of autism. Clinical Linguistics & Phonetics. 2010;24:1–16. doi: 10.3109/02699200903281739. [DOI] [PubMed] [Google Scholar]
- Newacheck PW, Kim SE. A national profile of health care utilization and expenditures for children with special health care needs. Archives of Pediatric Adolescent Medicine. 2005;59(1):10–17. doi: 10.1001/archpedi.159.1.10. [DOI] [PubMed] [Google Scholar]
- Nicolaidis C, Raymaker D, McDonald K, Dern S, Boisclair WC, Ashkenazy E, Baggs A. Comparison of healthcare experiences in autistic and non-autistic adults: a cross-sectional online survey facilitated by an academic-community partnership. Journal of General Internal Medicine. 2013;28(6):761–769. doi: 10.1007/s11606-012-2262-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nishizaka A. Distribution of visual orientations in prenatal ultrasound examinations: When the healthcare provider looks at the pregnant woman’s face. Journal of Pragmatics. 2013;51:68–86. [Google Scholar]
- Ochs E. Becoming a speaker of culture. In: Kramsch C, editor. Language acquisition and language socialization: Ecological perspectives. London: Continuum; 2002. pp. 99–120. [Google Scholar]
- Ochs E. Corporeal reflexivity and autism. Integrative Psychological and Behavioral Science. 2015;49(2):275–287. doi: 10.1007/s12124-015-9306-6. [DOI] [PubMed] [Google Scholar]
- Ochs E, Solomon O. Autistic sociality. Ethos. 2010;38(1):69–92. [Google Scholar]
- Ochs E, Solomon O, Sterponi L. Limitations and transformations of habitus in child-directed communication. Discourse Studies. 2005;7(4–5):547–583. [Google Scholar]
- Ochs E, Kremer-Sadlik T, Sirota KG, Solomon O. Autism and the social world: an anthropological perspective. Discourse Studies. 2004;6(2):147–183. [Google Scholar]
- Opel DJ, Heritage J, Taylor JA, Mangione-Smith R, Showalter Salas H, DeVere V, Zhou C, Robinson JD. The architecture of provider-parent vaccine discussions at health supervision visits. Pediatrics. 2013;132(6):1–10. doi: 10.1542/peds.2013-2037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parry R, Land V, Seymour J. How to communicate with patients about future illness progression and end of life: a systematic review. BMJ Supportive & Palliative Care. 2014;4:331–341. doi: 10.1136/bmjspcare-2014-000649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pilnick A, Hindmarsh J, Gill VT. Beyond ‘doctor and patient’: developments in the study of healthcare interactions. Sociology of health & illness. 2009;31(6):787–802. doi: 10.1111/j.1467-9566.2009.01194.x. [DOI] [PubMed] [Google Scholar]
- Peräkylä A, Bor R. Interactional problems of addressing ‘dreaded issues’ in HIV counselling. AIDS Care. 1990;2(4):325–338. doi: 10.1080/09540129008257748. [DOI] [PubMed] [Google Scholar]
- Plug L, Reuber M. Conversation analysis can help in the distinction of epileptic and non-epileptic seizure disorders: A case comparison. Seizure. 2009;18:43–50. doi: 10.1016/j.seizure.2008.06.002. [DOI] [PubMed] [Google Scholar]
- Radcliff L. Breast cancer and autism. Journal of the Advanced Practitioner in Oncology. 2013;4(2):113–117. [PMC free article] [PubMed] [Google Scholar]
- Reiss S, Szyszko J. Diagnostic overshadowing and professional experience with mentally retarded persons. American Journal of Mental Deficiency. 1983;87(4):396–402. [PubMed] [Google Scholar]
- Robinson JD. Getting down to business: Talk, gaze, and body orientation during openings of doctor-patient consultations. Human Communication research. 1998;25(1):97–123. [Google Scholar]
- Robinson JD. An interactional structure of medical activities during acute visits and its implications for patients’ participation. Health Communication. 2003;15(1):27–59. doi: 10.1207/S15327027HC1501_2. [DOI] [PubMed] [Google Scholar]
- Robinson JD. Soliciting patients’ presenting concerns. In: Heritage J, Maynard D, editors. Communication in medical care: Interactions between primary care physicians and patients. Cambridge: Cambridge University Press; 2006. pp. 22–47. [Google Scholar]
- Robinson JD, Stivers T. Achieving activity transitions in physician-patient encounters. Human Communication Research. 2001;27(2):253–298. [Google Scholar]
- Robinson JD, Heritage J. The structure of patients’ presenting concerns: The relevance of current symptoms. Social Science and Medicine. 2005;61(2):481–493. doi: 10.1016/j.socscimed.2004.12.004. [DOI] [PubMed] [Google Scholar]
- Robinson JD, Heritage J. Physicians’ opening questions and patients’ satisfaction. Patient Education and Counseling. 2006;60(3):279–285. doi: 10.1016/j.pec.2005.11.009. [DOI] [PubMed] [Google Scholar]
- Robinson JD, Heritage J. Intervening with conversation analysis: The case of medicine. Research on Language and Social Interaction. 2014;47(3):201–218. [Google Scholar]
- Sacks H, Schegloff EA, Jefferson G. A simplest systematics for the organization of turn-taking for conversation. Language. 1974;50:696–735. [Google Scholar]
- Searle JR. Speech acts: An essay in the philosophy of language. Cambridge: Cambridge University Press; 1969. [Google Scholar]
- Schegloff EA. Identification and Recognition in Telephone Conversation Openings. In: Psathas G, editor. Everyday language: Studies in ethnomethodology. New York: Irvington; 1979. pp. 23–78. [Google Scholar]
- Schegloff EA. The routine as achievement. Human Studies. 1986;9:111–151. [Google Scholar]
- Schegloff EA. Sequence organization in interaction: Volume 1: A primer in conversation analysis. Vol. 1. New York: Cambridge University Press; 2007. [Google Scholar]
- Schiffrin D, Tannen D, Hamilton HE, editors. The handbook of discourse analysis. Malden: Blackwell; 2001. [Google Scholar]
- Schwabe M, Howell SJ, Reuber M. Differential diagnosis of seizure disorders: A conversation analytic approach. Social Science and Medicine. 2007;65:712–24. doi: 10.1016/j.socscimed.2007.03.045. [DOI] [PubMed] [Google Scholar]
- Siegel M, Gabriels RL. Psychiatric hospital treatment of children with autism and serious behavioral disturbance. Special Issue: Acute Management of Autism Spectrum Disorders Child and Adolescent Psychiatric Clinics of North America. 2014;23:125–142. doi: 10.1016/j.chc.2013.07.004. [DOI] [PubMed] [Google Scholar]
- Silverman C. Understanding autism: Parents, doctors, and the history of a disorder. Princeton: Princeton University Press; 2011. [Google Scholar]
- Simonoff E, Pickles A, Charman T, Chandler S, Loucas T, Baird G. Psychiatric disorders in children with autism spectrum disorders: prevalence, comorbidity, and associated factors in a population-derived sample. Journal of American Academy of Child and Adolescent Psychiatry. 2008;47(8):921–929. doi: 10.1097/CHI.0b013e318179964f. [DOI] [PubMed] [Google Scholar]
- Smith MD, Graveline PJ, Smith JB. Autism and obstacles to medical diagnosis and treatment: Two case studies. Focus on Autism and Other Developmental Disabilities. 2012;27(3):189–195. [Google Scholar]
- Solomon O. Narrative introductions: discourse competence of children with autistic spectrum disorders. Discourse Studies. 2004;6(2):253–276. [Google Scholar]
- Solomon O. Body in autism: A view from social interaction. In: McPherron P, Ramanathan V, editors. Language, body, and health. Boston: Walter de Gruyton; 2011. pp. 105–141. [Google Scholar]
- Solomon O, Lawlor MC. ‘And I look down and he is gone’: narrating autism, elopement and wandering in Los Angeles. Social Science & Medicine. 2013;94:106–114. doi: 10.1016/j.socscimed.2013.06.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solomon O, Angell AM, Yin L, Lawlor M. ‘You can turn off the light if you’d like’: Pediatric healthcare visits for children with autism spectrum disorder as an interactional achievement. Medical Anthropology Quarterly. doi: 10.1111/maq.12237. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sterponi L, Fasulo A. How to go on: Intersubjectivity and progressivity in the communication of a child with autism. Ethos. 2010;38:116–142. [Google Scholar]
- Stivers T. Negotiating who presents the problem: Next speaker selection in pediatric encounters. Journal of Communication. 2001;51(2):1–31. [Google Scholar]
- Stivers T. Prescribing under pressure: Parent-physician conv,ersations and antibiotics. New York: Oxford University Press; 2007. [Google Scholar]
- Stivers T. Socializing children into the patient role. In: Duranti A, Ochs E, Schieffelin BB, editors. Handbook of language socialization. Malden: Wiley-Blackwell; 2011. pp. 247–67. [Google Scholar]
- Stivers T. Physician–child interaction: When children answer physicians’ questions in routine medical encounters. Patient Education and Counseling. 2012;87:3–9. doi: 10.1016/j.pec.2011.07.007. [DOI] [PubMed] [Google Scholar]
- Stivers T, Majid A. Questioning children: Interactional evidence of implicit bias in medical interviews. Social Psychology Quarterly. 2007;70(4):424–41. [Google Scholar]
- Street RL, Gordon H, Hailet P. Physicians’ communication and perception of patients: is it how they look, how they talk, or is it just the doctor? Social Science & Medicine. 2007;65:586–598. doi: 10.1016/j.socscimed.2007.03.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stribling P, Rae J, Dickerson P. Two forms of spoken repetition in a girl with autism. International Journal of Language & Communication Disorders. 2007;42:427–444. doi: 10.1080/13682820601183659. [DOI] [PubMed] [Google Scholar]
- Strong PM. The ceremonial order of the clinic: parents, doctors, and medical bureaucracies. London: Routledge; 1979. [Google Scholar]
- Swedlund MP, Schumacher JB, Young HN, Cox ED. Effect of communication style and physician–family relationships on satisfaction with pediatric chronic disease care. Health Communication. 2012;27(5):498–505. doi: 10.1080/10410236.2011.616632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tager-Flusberg H, Kasari C. Minimally verbal school-aged children with autism spectrum disorder: The neglected end of the spectrum. Autism Research. 2013;6(6):468–478. doi: 10.1002/aur.1329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tates K, Meeuwesen L. ‘Let Mum have her say’: turn taking in doctor–parent–child communication. Patient Education and Counseling. 2000;40(2):151–162. doi: 10.1016/s0738-3991(99)00075-0. [DOI] [PubMed] [Google Scholar]
- Tates K, Meeuwesen L. Doctor–parent–child communication. A (re) view of the literature. Social Science & Medicine. 2001;52(6):839–851. doi: 10.1016/s0277-9536(00)00193-3. [DOI] [PubMed] [Google Scholar]
- Tates K, Elbers E, Meeuwesen L, Bensing J. Doctor–parent–child relationships: A ‘pas de trois. ’ Patient Education and Counseling. 2002;48(1):5–14. doi: 10.1016/s0738-3991(02)00093-9. [DOI] [PubMed] [Google Scholar]
- Tannen D, Hamilton HE, Schiffrin D. The handbook of discourse analysis. 2. Malden: Wiley Blackwell; 2015. [Google Scholar]
- Todd AD, Fisher E, editors. The social organization of doctor-patient communication. Greenwood. Norwood: Ablex; 1993. [Google Scholar]
- Tregnago MK, Cheak-Zamora NC. Systematic review of disparities in health care for individuals with autism spectrum disorders in the United States. Research in Autism Spectrum Disorders. 2012;6(3):1023–1031. [Google Scholar]
- Turowetz J. The interactional production of a clinical fact in a case of autism. Qualitative Sociology. 2015;38 in press. [Google Scholar]
- Volkmar FR, Weisner LA. A practical guide to autism: what every parent, family member, and teacher should know. Hoboken: Wiley; 2009. [Google Scholar]
- Volkmar FR, Rowberry J, De Vinck-Baroody O, Gupta AR, Leung J, Meyers J, Vaswani N, Weisner LA. Medical care in autism and related conditions. In: Volkmar FR, Paul R, Pelphrey K, editors. Handbook of autism and developmental disorders. Hoboken: John Wiley & Sons; 2014a. pp. 532–554. [Google Scholar]
- Volkmar F, Siegel M, Woodbury-Smith M, King B, McCracken J, State M. Practice parameter for the assessment and treatment of children and adolescents with autism spectrum disorder. Journal of American Academy of Child and Adolescent Psychiatry. 2014b;53(2):237–57. doi: 10.1016/j.jaac.2013.10.013. [DOI] [PubMed] [Google Scholar]
- Waitzkin H. The politics of medical encounters: How patients and doctors deal with social problems. New Haven: Yale University Press; 1993. [Google Scholar]
- Warfield ME, Crossman MK, Delahaye J, Der Weerd E, Kuhlthau KA. Physician perspectives on providing primary medical care to adults with autism spectrum disorders (ASD) Journal of Autism and Developmental Disorders. 2015;45:2209–2217. doi: 10.1007/s10803-015-2386-9. [DOI] [PubMed] [Google Scholar]
- Wilkinson R, Gower M, Beeke S, Maxim J. Adapting to conversation as a language-impaired speaker: Changes in aphasic turn construction over time. Communication and Medicine. 2007;4:79–97. doi: 10.1515/CAM.2007.009. [DOI] [PubMed] [Google Scholar]
- Yin L, McLennan M, Bellou TF. Overweight in children with intellectual disabilities: No simple matter. Infant, Child, & Adolescent Nutrition. 2013;5(2):92–96. [Google Scholar]