Abstract
Objective
This study examined (a) demographic and clinical characteristics associated with sleep-related problems (SRPs) among youth with anxiety disorders, and (b) the impact of anxiety treatment: cognitive-behavioral therapy (CBT; Coping Cat), medication (sertraline), their combination, and pill placebo on SRPs.
Method
Youth (N = 488, ages 7-17, 50% female, 79% White) with a principal diagnosis of generalized anxiety disorder, separation anxiety disorder, or social phobia participated. SRPs were reported by parents and youth.
Results
Findings differed by informant and by type of SRP, with evidence that SRPs are associated with age, anxiety severity, externalizing problems, functional impairment, and family burden at pretreatment. Anxiety treatment reduced SRPs; effect sizes were small to medium. Reductions in parent-reported separation-related sleep difficulties were significantly greater in active treatment than in the placebo condition, with the greatest reductions reported by parents of youth whose active treatment was multimodal or included sertraline. Youth whose anxiety treatment involved CBT reported significantly greater decreases in dysregulated sleep (e.g., sleeplessness).
Conclusions
Both CBT for anxiety and sertraline appear to be somewhat effective in reducing SRPs, and multimodal treatment may be preferable depending on the symptom presentation. To inform practice, future research should examine a broad range of SRPs, incorporate objective measures of sleep, and evaluate the impact of behavioral strategies that directly target SRPs in youth with anxiety disorders.
Keywords: sleep problems, anxiety, treatment
Recurrent sleep disruption in youth has physical health (Leproult, & Van Cauter, 2010) and mental healthlks (e.g., executive functions, academic performance, emotion regulation) consequences (Beebe et al., 2004; Dewald, Meijer, Oort, Kerkhof, & Bögels, 2010; Fallone, Owens, & Deane, 2002; Gregory, & O'Connor, 2002; Mindell et al., 2011). Childhood sleep-related problems (SRPs) previously documented include nightmares, difficulty falling or staying asleep, early waking, parasomnias, refusal to sleep alone, and bedtime resistance (Alfano, Ginsburg, & Kingery, 2007; Fallone et al., 2002; Gregory, Rijsdijk, Dahl, McGuffin, & Eley, 2006). Incidence of parent-reported SRPs among youth range from 10-75% (depending on assessment method), with difficulties persisting for several years (Gregory et al., 2006; Mindell et al., 2011; Morrison, McGee, & Stanton, 1992; Paavonen, Solantaus, Almqvist, & Aronen, 2003; Zuckerman, Stevenson, & Bailey, 1987). SRPs in childhood can persist into adolescence (Gregory & O'Connor, 2002) and adulthood (Gregory et al., 2005; Gregory, Van der Ende, Willis, & Verhulst, 2008), and may be a risk factor for subsequent emotion dysregulation (Chorney, Detweiler, Morris, & Kuhn, 2008).
SRPs have been linked to numerous mental health problems, including anxiety, depression, and attention difficulties (Chorney et al., 2008; Ivanenko, Crabtree, Obrien, & Gozal, 2006) as well as social problems (e.g., not getting along with peers; Paavonen et al., 2003). The prevalence of SRPs in clinically anxious youth ranges from 42% to 92% (Hansen, Skirbekk, Oerbeck, Richter, & Kristensen, 2011; Kendall & Pimentel, 2003; Masi et al., 2004; Pina, Silverman, Fuentes, Kurtines, & Weems, 2003; Storch, Murphy et al., 2008), with some data indicating that 55% of anxious youth exhibit multiple SRPs (Alfano et al., 2007; Alfano, Pina, Zerr, & Villalta, 2010). Among school-aged community children, SRPs are associated with trait anxiety (Mindell & Barrett, 2002) and anxiety sensitivity (Gregory, Eley, & Moffitt, 2005). Although most studies have relied on subjective reports, objective measures (i.e., polysomnography) have also shown the link between sleep disturbance and anxiety (e.g., Forbes et al., 2008).
SRPs can precede anxiety, although the relationship is likely bidirectional (Chorney et al., 2008; Gregory, & O'Connor, 2002; Gregory et al., 2005, 2006; Leahy & Gradisar, 2012; Ong, Wickramaratne, Tang, & Weissman, 2006). SRPs may reflect other sleep-interfering anxiety symptoms (e.g., compulsions, worrying; Piacentini, Bergman, Keller, & McCracken, 2003; Storch et al., 2008) and are part of diagnostic criteria (e.g., for generalized anxiety disorder, GAD; separation anxiety disorder, SAD; APA, 2013). At the same time, sleep disruption results in decreased emotion regulation (e.g., Sagaspe et al., 2006) and increased pain sensitivity (Roehrs, Hyde, Blaisdell, Greenwald, & Roth, 2006). Thus, sleep disruption may exacerbate emotional, behavioral, attentional, and somatic symptoms, further interfering with sleep quality (Alfano & Gamble, 2009). Given that sleep behaviors in young children reflect early attempts to self-regulate (Alfano & Gamble, 2009), persistent sleep disruption may represent a prodromal form of emotion dysregulation, sharing neurological and hormonal circuitry (Leahy & Gradisar, 2012).
The number and severity of SRPs differs across developmental levels (Alfano & Gamble, 2009; Gregory, & O'Connor, 2002; Storch et al., 2008). Independent of anxiety, SRPs are most common in early childhood (Alfano et al., 2010). While the number of SRPs decreases from early childhood to preadolescence, the association between SRPs and anxiety becomes stronger throughout childhood (Gregory, & O'Connor, 2002). Thus, it may be the persistence of sleep difficulties, rather than their mere presence, that increases risk for anxiety disorders. In a non-clinical sample, anxiety severity was positively associated with SRPs for all age groups, although SRPs were more strongly associated with particular aspects of anxiety (cognitive errors) among adolescents than among children (Alfano, Zakem, Costa, Taylor, & Weems, 2009). Furthermore, adolescents have displayed significant changes in sleep patterns at puberty, including delay of sleep initiation and daytime drowsiness (e.g., Crowley, Acebo, & Carskadon, 2007). Changes in sleep during adolescence may be due to external influences (e.g., social events) as well as pubertal changes in neurological processes (Hagenauer, Perryman, Lee, & Carskadon, 2009). Thus, the relationship between SRPs and anxiety disorders may change as a function of development.
SRPs among anxious youth may vary by gender, with females reporting greater numbers of SRPs (e.g., Storch et al., 2008). Specifically, nightmares, bedtime resistance, sleep anxiety, overtiredness, and excessive sleep have been found more common among females than males (Alfano et al., 2007; Alfano et al., 2010; Storch et al., 2008).
SRPs have been linked to externalizing problems (Angold, Costello, & Erkanli, 1999). Less self-reported sleep has been associated with self-reported attention problems and aggressive behavior (Gregory et al., 2008). Although research on the relationship between SRPs and oppositional defiant disorder (ODD) has yielded mixed results (e.g., Hvolby, Jørgensen, & Bilenberg, 2009; Mayes et al., 2009), approximately 25-50% of youth with ADHD have reported sleep-related difficulties (Owens, 2005) that may exacerbate attention difficulties (Alfano & Gamble, 2009). Frequent SRPs experienced by youth with ADHD include bedtime resistance, difficulty waking, and frequent waking (Cortese, Faraone, Konofal, & Lecendreux, 2009). The comorbid presentation of anxiety and ADHD has been shown to compound SRPs (Hansen et al., 2011; Mayes et al., 2009; Mick, Biederman, Jetton, & Faraone, 2000).
Given that prior research has supported the efficacy of CBT and selective serotonin reuptake inhibitors for treating anxiety disorders (e.g., Kendall et al., 2008; Research Units on Pediatric Psychopharmacology Anxiety Study Group, 2001), reductions in SRPs following these treatments might be expected. However, few studies have examined treatment-related change in SRPs among anxious youth. Storch et al. (2008) found a significant reduction in the number of SRPs exhibited by youth with obsessive-compulsive disorder (OCD) after completing CBT, but it was unclear if this reflected decreased distress or decreased family accommodation (e.g., parents not allowing a child to sleep in their bed). In another study, anxious youth exhibited significantly greater reductions in clinician- and parent-reported SRPs following a course of fluvoxamine (compared to placebo; Alfano et al., 2007). The relative effects of CBT and pharmacotherapy on SRPs among anxious youth have not yet been studied.
The current study examined the relationship of SRPs to demographic (gender, age) and clinical characteristics (anxiety severity, functional impairment, externalizing problems, family burden, pubertal status) among anxiety-disordered youth. The impact of CBT, medication, and their combination on SRPs was also examined. We hypothesized that SRPs would differ as a function of pubertal status and would be positively associated with anxiety severity and comorbid externalizing problems. We also hypothesized that SRPs would be significantly associated with functional impairment and family burden, controlling for anxiety severity. We expected that active treatments (sertraline, CBT, and their combination) would result in significantly greater reductions in SRPs than pill placebo, and that treatment responders would show significantly greater reductions in SRPs than non-responders.
Method
Participants
Data from the Child/Adolescent Anxiety Multimodal Study (CAMS; Walkup et al., 2008) were analyzed. Participants were 488 youth (50% male) with a principal diagnosis of SAD, GAD, or social phobia (SoP) based on DSM-IV criteria (APA, 1994). They ranged in age from 7 to 17 years (M=10.72, SD=2.80). Youth were randomly assigned to: medication (sertraline, n = 133), CBT (Coping Cat; n = 139), their combination (n = 140), and pill placebo (n = 76). The sample was predominantly of non-Hispanic ethnicity (88%). The majority of the sample was White (79%, n = 385), followed by African American (9%, n = 44), Asian (3%, n = 12), American Indian (1%, n = 6), Native Hawaiian/Other Pacific Islander (<1%, n = 2), and other (8%, n = 39). Outside of anxiety, the most common comorbidities were ADHD (10%, n = 49), ODD (9%, n = 46), and OCD (9%, n = 42). Additional sample characteristics have been reported (Kendall et al., 2010). The attrition rate was low (Walkup et al., 2008).
Measures
Anxiety Disorders Interview Schedule-Child/Parent Versions (ADIS-IV-C/P; Silverman & Albano, 1996). The ADIS-IV-C/P is a clinician-administered, semi-structured interview that assesses anxiety disorders and associated psychopathology in youth. The ADIS-IV-C/P has excellent psychometric properties (Silverman, Saavedra, & Pina, 2001; Wood, Piacentini, Bergman, McCracken, & Barrios, 2002). Based on a review of 10% of videotaped assessments, interrater reliability for diagnostic status (intraclass correlation coefficients) ranged from .82 to .88.
Clinical Global Impressions-Improvement (CGI-I; Guy, 1976). The CGI-I provides a global rating of improvement in clinical presentation, ranging from 1 (very much improved) to 7 (very much worse). A CGI-I score of 1 (very much improved) or 2 (much improved) was used to designate treatment response.
Pediatric Anxiety Rating Scale (PARS; Research Units on Pediatric Psychopharmacology Anxiety Study Group, 2002). The PARS is a clinician-rated measure of anxiety severity in youth. The PARS is administered to the child and parent(s) together, and consists of a symptom checklist and seven global items. Global items are rated on a 6-point scale based on the number and frequency of symptoms, severity of distress, and interference with functioning. In CAMS, six of the seven global items were summed; the item assessing the number of symptoms present (per checklist) was not included in the total score due to concerns about item overlap. Reliability and validity of the PARS is acceptable (Research Units on Pediatric Psychopharmacology Anxiety Study Group, 2002). Inter-rater reliability in CAMS was excellent (>.97).
Child Anxiety Impact Scale-Parent Version (CAIS-P; Langley, Bergman, McCracken, & Piacentini, 2004; Langely et al., 2014). The CAIS-P is a 27-item, parent-report measure of anxiety-related interference in social activities, school, and home/family functioning. For this study, two items pertaining to sleep were not scored due to overlap with items on the sleep measure. The CAIS-P has good internal consistency and validity (Langely, 2004; Langely et al., ahead of print). Cronbach's alpha was .88 at pre- and .92 at post-treatment.
Child Behavior Checklist (CBCL; Achenbach & Rescorla, 2001). The CBCL is a 118-item parent-report measure of child psychopathology over the past six months. The psychometric properties of the CBCL have been demonstrated across a variety of populations (Achenbach & Rescorla, 2001). The current study used the CBCL Externalizing Problems score, which had a Cronbach's alpha of .96 at pre- and .99 at post-treatment.
Burden Assessment Scale (BAS; Reinhard, Gubman, Horwitz, & Minsky, 1994). The 21-item BAS measures caregiver burden associated with having a child with a mental health disorder. Parents indicated the degree to which the child's anxiety disrupts family life (5-point scale). Cronbach's alpha for the current sample was .91 at pre- and .93 at post-treatment.
Pubertal Development Scale (Petersen, Crockett, Richards, & Boxer, 1988). The PDS is a 5-item youth self-report measure of physical changes associated with puberty. With the exception of menarche, which is reported by females as present/absent, items are rated on a 1 (not yet started) to 4 (seems complete) scale and averaged. In the current sample, Cronbach's alpha was .87 for girls and .85 for boys.
Sleep composite measure. To assess SRPs, exploratory factor analyses (EFA) with maximum likelihood estimation were conducted using sleep items from parent- and child-report measures administered at pretreatment. Parent-rated sleep items (11 total) consisted of 6 items from the CBCL, 4 items from the Screen for Child Anxiety and Related Emotional Disorders (SCARED; Birmaher, 1997; Birmaher, Khetarpal, Brent, & Cully, 1997; Birmaher et al., 1999), and 1 item from the Multidimensional Anxiety Scale for Children (MASC; March, Parker, Sullivan, Stallings, & Conners, 1997). Child-rated sleep items (9 total) consisted of 4 items from the Physical Symptoms Checklist (PSC; Emslie et al., 2006), 4 items from the SCARED, and 1 item from the MASC. All items were rescaled using the least common multiple of the number of response options across measures. Based on the results of a parallel analysis of eigenvalues (Hayton, Allen, & Scarpello, 2004; Zwick & Velicer, 1986), three factors were extracted from parent-rated sleep items and two factors were extracted from child-rated sleep items. Varimax rotation was used to evaluate the solution. One factor from the parent-rated measure was not considered empirically-defined because it had fewer than three “marker” items (Brown, 2006); thus, a two-factor solution was evaluated. Items that loaded above |.40| on one factor and below |.30| on the other were retained. Based on low factor loadings, items pertaining to nightmares with specific content (i.e., something bad happening to the child or to his/her parents) were dropped from both the parent- and child-report scales. Two additional items were dropped from the parent-report: sleeping more than most kids and talking/walking during sleep. The resulting parent- and child-report SRP measures each consisted of a Dysregulated Sleep factor (3 parent-rated items, Cronbach's alpha = .63; 4 child-rated items, Cronbach's alpha = .71) and a factor reflecting Separation-Related Sleep Problems (3 parent-rated items, Cronbach's alpha = .75; 3 child-rated items, Cronbach's alpha = .69). These scales cover the SRPs most commonly endorsed in prior research sampling clinic-referred youth with the same principal diagnoses (Alfano et al., 2007). Tables 1 and 2 present EFA results.
Table 1.
Factor loadings for parent-rated sleep items (N = 488).
| Separation | Dysregulated Sleep | |
|---|---|---|
| Sleeps less than most kids | .116 | .510 |
| Sleeps next to someone from family | .710 | .151 |
| Worry about sleeping alone | .977 | .213 |
| Scared if sleeps away from home | .438 | .081 |
| Trouble sleeping | .045 | .882 |
| Nightmares | .218 | .435 |
Table 2.
Factor loadings for child-rated sleep items (N = 488).
| Separation | Dysregulated Sleep | |
|---|---|---|
| Sleeplessness | .120 | .719 |
| Sleeps next to someone from family | .623 | .065 |
| Worry about sleeping alone | .922 | .159 |
| Scared if sleeps away from home | .426 | .111 |
| Trouble sleeping | .173 | .784 |
| Feeling drowsy or too sleepy | .031 | .459 |
| Nightmares or very strange dreams | .126 | .460 |
Procedures
Procedures were approved by relevant IRBs. Measures were administered at pre- and post-treatment by independent evaluators masked to treatment condition who were trained to a pre-specified reliability and monitored for drift. Randomly-selected, videotaped therapy sessions were reviewed for treatment fidelity and had excellent correspondence with the protocol. The CAMS design, rationale for treatments, and quality assurance procedures have been discussed by Compton et al. (2010).
Cognitive-behavioral therapy (CBT). CBT participants received 14, 60-minute sessions over 12 weeks. Treatment (Coping Cat; Kendall & Hedtke, 2006) was adapted to the youth's age (Kendall, Choudhury, Hudson, & Webb, 2002). Coping Cat trains skills for managing anxiety (e.g., cognitive restructuring; problem solving) and provides exposure to anxiety-provoking situations. Youth were assigned between-session treatment-related homework.
Pharmacotherapy. Pharmacotherapy consisted of eight, 30- to 60-minute sessions (weeks 1-4, 6, 8, 12) that involved discussing anxiety symptoms, overall functioning, treatment response, and adverse events in the context of supportive care. Providers checked-in with participants by phone during weeks without in-person sessions. Sertraline was administered on a fixed-flexible schedule beginning with 25 mg per day and adjusting up to 200 mg per day by week 8.
Combination therapy. Combination therapy consisted of all components of the CBT and the pharmacotherapy conditions. Sessions occurred on the same day whenever possible. Dose increases were determined with input from the CBT therapist.
Data Analytic Plan
Analyses used the intent-to-treat sample with multiple imputation for handling missing data (<10%) at posttreatment.1 ANOVA examined pretreatment SRPs by condition. T-tests and correlations evaluated relationships between SRPs and demographics, pubertal development, anxiety severity, functional impairment, externalizing problems, and family burden. Multiple regressions examined pretreatment SRPs, functional impairment and family burden, controlling for anxiety severity. Mixed-model ANOVA examined treatment-related changes in SRPs by type of treatment (e.g., active versus placebo). ANOVA examined treatment responders’ and non-responders’ SRPs, controlling for pretreatment SRPs. An alpha level of .01 was used.
Results
Preliminary Analyses
Pretreatment SRPs did not differ by condition. The correlation between parent and child report of sleep problems related to Separation was .63 (p < .01) at each time point. The correlation between parent and child report of Dysregulated Sleep was .28 (p < .01) at each time point. Within informant, inter-factor correlations at pre- and post-treatment ranged from .17 to .28 (all p-values < .01). Means and standard deviations are reported in Table 3.
Table 3.
Means and Standard Deviations for Sleep-Related Problems
| Sleep-Related Problems | Sertraline (n=133) | CBT (n=139) | Combination (n=140) | Placebo (n=76) | Total Sample (N=488) | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Pre | Post | Pre | Post | Pre | Post | Pre | Post | Pre | Post | |
| Parent-rated Separation | 8.21 (6.34) | 3.85 (5.12) | 7.50 (6.06) | 3.63 (4.80) | 8.19 (6.38) | 2.57 (3.37) | 8.67 (6.00) | 5.64 (5.93) | 8.08 (6.21) | 3.70 (4.83) |
| Child-rated Separation | 4.71 (5.45) | 2.69 (4.47) | 4.14 (4.84) | 2.32 (4.06) | 5.45 (5.34) | 2.28 (3.53) | 5.33 (5.50) | 3.65 (4.90) | 4.85 (5.27) | 2.62 (4.18) |
| Parent-rated Dysregulated Sleep | 4.56 (4.80) | 2.31 (3.54) | 4.68 (5.03) | 2.19 (3.04) | 5.89 (5.09) | 2.50 (3.49) | 4.83 (5.01) | 2.64 (3.84) | 5.02 (5.00) | 2.38 (3.42) |
| Child-rated Dysregulated Sleep | 4.89 (5.13) | 2.43 (3.73) | 5.89 (5.71) | 1.65 (2.68) | 6.10 (6.00) | 2.26 (3.69) | 5.22 (5.60) | 2.89 (5.04) | 5.57 (5.64) | 2.23 (3.68) |
Note. Means were calculated using imputed data. Standard deviations for the non-imputed dataset are reported, as multiple imputation procedures do not yield pooled standard deviation estimates. All pre-post differences were significant at p < .01. CBT = cognitive-behavioral therapy.
Demographics
Parent- and child-reported SRPs were not significantly related to gender. Child age in months was significantly and negatively associated with sleep problems related to Separation, as rated by parents (r = −.45, p < .001) and children (r = −.33, p < .001). Age was significantly and positively associated with Dysregulated Sleep by child report only (r = .14, p < .01).
Clinical Characteristics
Pubertal development was significantly and negatively associated with sleep problems related to Separation, as reported by parents (r = −.41, p < .001) and children (r = −.27, p < .001); however, these associations were not significant when controlling for age. Pubertal development was not related to parent- or child-rated Dysregulated Sleep.
Clinician-rated anxiety severity was significantly and positively associated with SRPs, as reported by parents (Separation: r = .20, p < .001; Dysregulated Sleep: r = .14, p < .01) and children (Separation: r = .17, p < .001; Dysregulated Sleep: r = .24, p < .001). Parent-reported externalizing problems were significantly associated with parent-rated SRPs (Separation: r = .15, p = .001; Dysregulated Sleep: r = .29, p < .001) but not with child-rated SRPs.
Parent-reported functional impairment was significantly and positively associated with parent-rated SRPs (Separation: r = .16, p < .001; Dysregulated Sleep: r = .18, p < .01) and child-rated Dysregulated Sleep (r = .27, p < .001), but not with child-rated sleep problems related to Separation. Controlling for age and anxiety severity, parent- and child-rated Dysregulated Sleep each significantly predicted functional impairment (parent: β=.13, t = 3.29, p = .001; child: β = .13, t = 3.00, p < .01), as did parent-rated sleep problems related to Separation (β =.17, t = 3.73, p < .001). Child-rated sleep problems related to Separation did not significantly predict functional impairment.
Family burden was positively and significantly associated with parent-rated SRPs (Separation: r = .22, p < .001; Dysregulated Sleep: r= .21, p < .001) and child-rated sleep problems related to Separation (r = .17, p < .001), but not with child-rated Dysregulated Sleep. Controlling for anxiety severity, parent-rated SRPs significantly predicted family burden (Separation: β =.17, t = 3.78, p < .001; Dysregulated Sleep: β =.17, t =3.84, p < .001). Child-rated sleep problems related to Separation also significantly predicted family burden when controlling for anxiety severity (β =.13, t = 2.83, p < .01). Controlling for age and anxiety severity, child-rated Dysregulated Sleep was not related to family burden.
Treatment-Related Change in SRPs
A 2 (treatment type: active vs. non-active) × 2 (time) mixed-model ANOVA examined treatment effects on SRPs. There were significant main effects of time for sleep problems related to Separation (parent- report: F = 131.32, p < .001, η2 = .23; child-report: F = 41.89, p < .001, η2 = .09) as well as Dysregulated Sleep (parent-report: F = 47.53, p < .001, η2 = .11; child-report: F = 67.30, p < .001, η2 = .14). Compared to placebo, active treatment (sertraline, CBT, combination) resulted in significantly greater reductions in sleep problems related to Separation, as reported by parents (F = 6.52, p = .01, η2 = .01) but not by children. There were no significant treatment type X time interactions for parent- or child-rated Dysregulated Sleep.
For participants in active treatment only, a 2 × 2 mixed-model ANOVA examined the impact of combined treatment versus sertraline alone or CBT alone on SRPs. Multimodal treatment was associated with significantly greater reductions in sleep problems related to Separation, as rated by parents (F = 9.69, p < .01, η2 = .01) and children (F = 10.78, p = .001, η2 = .02). There were no significant treatment type X time interactions for parent- or child-rated Dysregulated Sleep.
A 2 (presence/absence of CBT) × 2 (time) mixed-model ANOVA examined the impact of CBT on SRPs. There were significant main effects of time for sleep problems related to Separation (parent-report: F = 323.17, p < .001, η2 = .43; child-report: F = 93.77, p < .001, η2 = .18) and Dysregulated Sleep (parent-report: F = 99.70, p < .001, η2 = .21; child-report: F = 148.47, p < .001, η2 = .26). There were no significant treatment type X time interactions for sleep problems related to Separation. Relative to conditions that did not include CBT (sertraline, placebo), the CBT conditions (CBT, combination) were associated with significantly greater reductions in Dysregulated sleep by child report (F = 8.60, p < .01, η2 = .02) but not by parent report.
A 2 (presence/absence of sertraline) × 2 (time) mixed-model ANOVA examined the impact of sertraline on SRPs. There were significant main effects of time for all SRPs (parent-rated Separation: F = 337.37, p < .001, η2 = .44; child-rated Separation: F = 100.86, p < .001, η2 = .19; parent-rated Dysregulated Sleep: F = 105.06, p < .001, η2 = .22; child-rated Dysregulated Sleep: F = 167.95, p < .001, η2 = .29). Conditions that included sertraline (sertraline; combination) were associated with significantly greater reductions in parent-rated sleep problems related to Separation (F = 11.81, p = .001, η2 = .02) than conditions that did not include sertraline (CBT, placebo). There were no significant treatment type X time interactions for child-rated sleep problems related to Separation, or for parent- or child-rated Dysregulated Sleep.
Relationship to Change in Anxiety
A series of ANCOVA examined differences between treatment responders and non-responders in posttreatment SRPs, controlling for pretreatment SRPs and age. Treatment responders had significantly lower posttreatment scores on the Separation scale, as rated by parents (F = 103.15, p < .001, η2 = .07) and children (F = 36.24, p < .001, η2 = .04). Treatment responders also had significantly lower posttreatment scores on Dysregulated Sleep scale, as rated by parents (F = 13.05, p < .001, η2 = .02) and children (F = 18.02, p < .001, η2 = .03).
Discussion
The present findings highlight the separate role of (a) dysregulated sleep and (b) sleep difficulties related to separating from caregivers. These SRPs were differentially associated with age, child functional impairment, and family burden. Additionally, the findings suggest that treating anxiety (CBT and sertraline) has some beneficial effects on SRPs; effect sizes were small to medium and differed somewhat by treatment type and informant.
Unlike prior research that examined the number of SRPs reported by parents or children (Alfano et al., 2010; Gregory, & O'Connor, 2002; Storch et al., 2008), this study examined the severity of parent- and child-rated SRPs. There were no gender differences in SRPs. Age was negatively associated with separation-related sleep problems, as rated by parents and youth, and positively associated with youth-rated dysregulated sleep. In line with prior research, youth with higher anxiety severity displayed more severe SRPs (across informants), and parent-rated SRPs were positively associated with comorbid externalizing problems, functional impairment, and family burden (Ivanenko, 2006; Alfano et al., 2009). Youth-rated sleep problems related to separation were associated with family burden only, whereas youth-rated dysregulated sleep was associated with functional impairment only.
Both separation-related sleep difficulties and dysregulated sleep improved over time, and reductions in separation-related sleep difficulties reported by parents were greater for those in active treatment than in the placebo condition, with the greatest reductions exhibited by youth whose anxiety treatment was multimodal/sertraline. Dysregulated sleep improved over time in all treatment conditions (including placebo), with significantly greater reductions reported by youth whose anxiety treatment included CBT. Across informants, treatment responders exhibited greater reductions in both types of SRPs than did non-responders.
Previous longitudinal research indicated that the total number of SRPs decreases with age while the association between SRPs and anxiety stabilizes with age (Gregory, & O'Connor, 2002). The current results suggest that this pattern is driven by reductions in separation-related sleep difficulties as children age. Beyond sleep disturbance, separation anxiety symptoms are more prevalent among younger children than adolescents (Allen, Lavallee, Herren, Ruhe, & Schneider, 2010). Perhaps as youth enter puberty, families are more reluctant to share a bed and parents are less likely to accommodate anxiety symptoms, allowing youth to tolerate separation-related distress. Consistent with pubertal changes in sleep, older youth reported greater sleep dysregulation; however, parent-rated dysregulated sleep was not related to age (Crowley et al., 2007). It may be that younger children are more likely to seek comfort from their parents when experiencing dysregulated sleep, and that youth become less likely to share such difficulties with their parents as they age. Findings highlight the need for multi-informant assessment of SRPs in future research.
Surprisingly, youth reports of dysregulated sleep difficulties, but not separation-related sleep difficulties, were associated with greater functional impairment. Perhaps families grow accustomed to altered sleeping arrangements such that the separation difficulties no longer interfere with the child's functioning. However, both parent- and youth-rated sleep difficulties related to separation were positively associated with family burden. Youth with higher sleep anxiety and emotional problems have exhibited higher rates of co-sleeping compared to healthy peers (Allen et al., 2010). Perhaps it is parental accommodation that burdens the family but leads to little interference elsewhere. Youth–reported dysregulated sleep was not associated with family burden, which may again reflect discrepancies in parent and youth reports of dysregulated sleep. It's possible that when youth experience difficulty falling and staying asleep but do not share their concerns or seek help from parents, family members remain unaware of these difficulties and do not perceive any associated burden.
Given that SRPs are linked to poor physical health (Leproult & Van Cauter, 2010) and decreased emotion regulation (Sagaspe et al., 2006), and predict difficulties with anxiety and depression in adulthood (Gregory et al., 2005), it is encouraging that both separation-related sleep difficulties and dysregulated sleep among youth with anxiety can be improved by anxiety treatment: the findings indicate that CBT and sertraline are each associated with some improvements in SRPs. Because CBT can involve decreasing family accommodation and practicing sleeping apart from a caregiver, it is surprising that sertraline was associated with a greater reduction in parent-rated sleep concerns related to separation. However, CBT in CAMS did not directly address parent-child interactions at bedtime; SRPs may be further reduced when they are a focus of CBT. Given that multimodal treatment was superior to monotherapy and that both forms of monotherapy reduced separation-related sleep concerns, it may be that sertraline and CBT had an additive effect.
All treatment conditions were associated with decreases in dysregulated sleep, though active anxiety treatment involving CBT was superior to treatment without CBT. This may reflect CBT-related decreases in worry, which can contribute to difficulties falling and staying asleep. Alternatively, the difference in effect between CBT and sertraline may be due to adverse effects of sertraline on sleep (Rynn, Siqueland, & Rickels, 2001; Rynn et al., 2015). The possibility that medication improves some SRPs (e.g., related to separation concerns) but interferes with other aspects of sleep (e.g., architecture; Zhang et al., 2013) underscores the need for studies designed to evaluate a broad range of sleep outcomes. Overall, the current findings suggest that both CBT and sertraline are somewhat effective in reducing SRPs, and that multimodal treatment may be preferable for addressing separation-related sleep concerns, but additional research is required to make specific practice recommendations.
Limitations merit comment. First, assessments relied on retrospective self- and parent-report, and did not address the extent to which SRPs were persistent and distinct from normal sleep disruptions in youth. Future research should incorporate objective measures of sleep (e.g., polysomnography; actigraphy) and sleep logs that assess disturbances in real time with less influence from recall bias (Forbes et al., 2008). Second, the measure of SRPs was developed for this study using items from non-sleep measures administered to the same sample used to test hypotheses; thus, some SRPs (e.g., sleepwalking) were not represented and there was potential for capitalization on chance characteristics of the data. Also, because approximately half of the SRP items were embedded in anxiety measures, reductions in SRPs may partly reflect a halo effect related to improvement in anxiety symptoms. Third, family accommodation of youth SRPs was not assessed. Given the relationship of SRPs to family burden and the lack of impairment associated with youth-rated separation concerns, accommodations may have been in place to help youth sleep. Family accommodation of youth anxiety symptoms is common (Benito et al., 2015; Lebowitz et al., 2013), yet little is known about how it relates to SRPs and how it may be impacted by CBT and sertraline. Finally, data were collected from a well-characterized, treatment-seeking sample of anxious youth that was predominantly non-Hispanic White; results may not generalize to other groups. Future studies should examine the mechanism by which successful anxiety treatment impacts SRPs (e.g., reducing anxious cognitions, emotion dysregulation, or family accommodation) using diverse samples, and may benefit from distinguishing biological and behavioral components (e.g., sleep hygiene). Additionally, the impact of sleep-focused behavioral interventions for youth with anxiety disorders should be investigated.
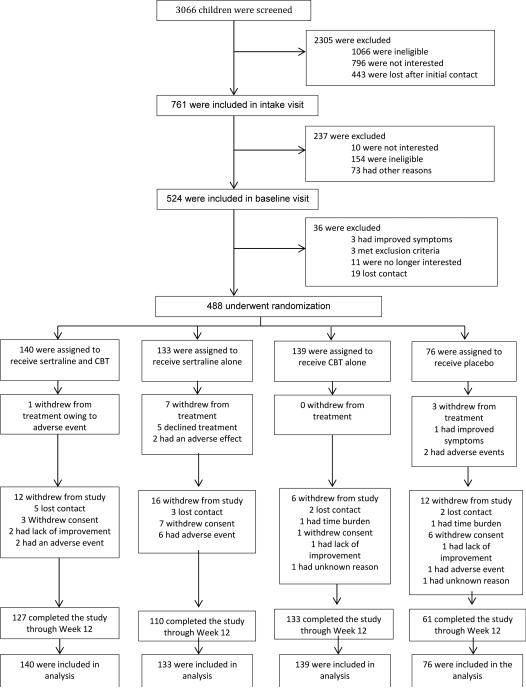
Figure 1.
CONSORT Flow diagram reproduced from the Child/Adolescent Anxiety Multimodal Study (Walkup et al., 2008).
Acknowledgments
This research was supported by NIMH grants (MH063747 to Kendall; MH64003 to Birmaher; MH64003 to Compton; MH64088 to Piacentini; MH64089 to Walkup; MH64092 to Albano). Views expressed within this article represent those of the authors and are not intended to represent the position of NIMH, NIH, or DHHS.
Footnotes
(ClinicalTrials.gov number, NCT00052078.)
Results are reported for the pooled dataset whenever possible; for analyses in which multiple imputation procedures did not yield pooled estimates, results for non-imputed data are reported.
Contributor Information
Nicole E. Caporino, Department of Psychology, Georgia State University
Kendra L. Read, Department of Psychology, Temple University, Philadelpha, PA
Nina D. Shiffrin, Department of Psychology, Temple University, Philadelpha, PA
Cara A. Settipani, Department of Psychology, Temple University, Philadelpha, PA
Scott N. Compton, Department of Psychiatry and Behavioral Services, Duke University Medical Center, Durham, NC
Joel Sherrill, Division of Services and Intervention Research, National Institute of Mental Health, Bethesda, MD.
John Piacentini, Semel Institute for Neuroscience and Human Behavior, University of California Los Angeles, Los Angeles, CA.
John Walkup, Division of Child and Adolescent Psychiatry, Weill Cornell Medical College, New York, NY.
Golda Ginsburg, Division of Child and Adolescent Psychiatry, The Johns Hopkins University School of Medicine, Baltimore, MD.
Boris Birmaher, Western Psychiatric Institute and Clinic, University of Pittsburg Medical Center, Pittsburgh, PA.
Dara Sakolsky, Western Psychiatric Institute and Clinic, University of Pittsburg Medical Center, Pittsburgh, PA.
Elizabeth Gosch, Department of Psychology, Philadelphia College of Osteopathic Medicine, Philadelphia, PA.
Courtney Keeton, Division of Child and Adolescent Psychiatry, The Johns Hopkins University School of Medicine, Baltimore, MD.
Anne Marie Albano, Department of Psychiatry, Columbia Medical Center, New York, NY.
Philip C. Kendall, Department of Psychology, Temple University, Philadelpha, PA
References
- Achenbach TM, Rescorla L. Manual for the ASEBA school-age forms and profiles. Research Center for Children, Youth, & Families; Burlington: 2001. [Google Scholar]
- Alfano CA, Gamble AL. The role of sleep in childhood psychiatric disorders. In Child and Youth Care Forum. 2009;38(6):327–340. doi: 10.1007/s10566-009-9081-y. doi:10.1007/s10566-009-9081-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alfano CA, Ginsburg GS, Kingery JN. Sleep-related problems among children and adolescents with anxiety disorders. Journal of the American Academy of Child and Adolescent Psychiatry. 2007;46(2):224–232. doi: 10.1097/01.chi.0000242233.06011.8e. doi: 10.1097/01.chi.0000242233.06011.8e. [DOI] [PubMed] [Google Scholar]
- Alfano CA, Pina AA, Zerr AA, Villalta IK. Pre-sleep arousal and sleep problems of anxiety-disordered youth. Child Psychiatry and Human Development. 2010;41(2):156–167. doi: 10.1007/s10578-009-0158-5. doi: 10.1007/s10578-009-0158-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alfano CA, Zakem AH, Costa NM, Taylor LK, Weems CF. Sleep problems and their relation to cognitive factors, anxiety, and depressive symptoms in children and adolescents. Depression and Anxiety. 2009;26(6):503–512. doi: 10.1002/da.20443. [DOI] [PubMed] [Google Scholar]
- Allen JL, Lavallee KL, Herren C, Ruhe K, Schneider S. DSM-IV criteria for childhood separation anxiety disorder: Informant, age, and sex differences. Journal of Anxiety Disorders. 2010;24(8):946–952. doi: 10.1016/j.janxdis.2010.06.022. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 4th ed. Washington, DC.: 1994. [Google Scholar]
- American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Arlington, VA.: 2013. [Google Scholar]
- Angold A, Costello EJ, Erkanli A. Comorbidity. Journal of Child Psychology and Psychiatry. 1999;40(1):57–87. doi: 10.1111/1469-7610.00424. [PubMed] [Google Scholar]
- Beebe DW, Wells CT, Jeffries J, Chini B, Kalra M, Amin R. Neuropsychological effects of pediatric obstructive sleep apnea. Journal of the International Neuropsychological Society. 2004;10(07):962–975. doi: 10.1017/s135561770410708x. doi: 10.1017/S135561770410708X. [DOI] [PubMed] [Google Scholar]
- Benito KG, Caporino NE, Frank HE, Ramanujam BA, Garcia A, Freeman J, Storch EA. Development of the Pediatric Accommodation Scale : Reliability and validity of clinician- and parent-report measures. Journal of Anxiety Disorders. 2015;29(1):14–24. doi: 10.1016/j.janxdis.2014.10.004. [DOI] [PubMed] [Google Scholar]
- Birmaher B. Division of Child Psychiatry. Western Psychiatric Institute and Clinic; Pittsburgh, PA: Screening for child anxiety related emotional disorders (SCARED). [Google Scholar]
- Birmaher B, Brent DA, Chiappetta L, Bridge J, Monga S, Baugher M. Psychometric properties of the Screen for Child Anxiety Related Emotional Disorders (SCARED): A replication study. Journal of the American Academy of Child and Adolescent Psychiatry. 1999;38(10):1230–1236. doi: 10.1097/00004583-199910000-00011. doi: 10.1097/00004583-199910000-00011. [DOI] [PubMed] [Google Scholar]
- Birmaher B, Khetarpal S, Brent D, Cully M. The Screen for Child Anxiety Related Emotional Disorders (SCARED): Scale construction and psychometric characteristics. Journal Of The American Academy Of Child & Adolescent Psychiatry. 1997;36(4):545–553. doi: 10.1097/00004583-199704000-00018. doi: 10.1097/00004583-199704000-00018. [DOI] [PubMed] [Google Scholar]
- Brown TA, Kenny DA, editors. Confirmatory factor analysis for applied research. Guilford Press; New York, NY: 2006. Introduction to CFA. pp. 40–102. [Google Scholar]
- Chorney DB, Detweiler MF, Morris TL, Kuhn BR. The interplay of sleep disturbance, anxiety, and depression in children. Journal of Pediatric Psychology. 2008;33(4):339–348. doi: 10.1093/jpepsy/jsm105. doi: 10.1093/jpepsy/jsm105. [DOI] [PubMed] [Google Scholar]
- Compton SN, Walkup JT, Albano A, Piacentini JC, Birmaher B, Sherrill JT, March JS. Child/Adolescent Anxiety Multimodal Study (CAMS): Rationale, design, and methods. Child and Adolescent Psychiatry and Mental Health. 2010;4 doi: 10.1186/1753-2000-4-1. doi:10.1186/1753-2000-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cortese S, Faraone SV, Konofal E, Lecendreux M. Sleep in children with attention-deficit/hyperactivity disorder: Meta-analysis of subjective and objective studies. Journal of the American Academy of Child and Adolescent Psychiatry. 2009;48(9):894–908. doi: 10.1097/CHI.0b013e3181ac09c9. doi: 10.1097/CHI.0b013e3181ac09c9. [DOI] [PubMed] [Google Scholar]
- Cortesi F, Gianotti F, Sebastiani T, Vagnoni C, Marioni P. Cosleeping versus solitary sleeping in children with bedtime problems: child emotional problems and parental distress. Behavioral Sleep Medicine. 2008;6(2):89–105. doi: 10.1080/15402000801952922. doi: 10.1080/15402000801952922. [DOI] [PubMed] [Google Scholar]
- Crowley SJ, Acebo C, Carskadon MA. Sleep, circadian rhythms, and delayed phase in adolescence. Sleep Medicine. 2007;8(6):602–612. doi: 10.1016/j.sleep.2006.12.002. doi: 10.1016/j.sleep.2006.12.002. [DOI] [PubMed] [Google Scholar]
- Dewald JF, Meijer AM, Oort FJ, Kerkhof GA, Bögels SM. The influence of sleep quality, sleep duration and sleepiness on school performance in children and adolescents: A meta-analytic review. Sleep Medicine Reviews. 2010;14(3):179–189. doi: 10.1016/j.smrv.2009.10.004. doi: 10.1016/j.smrv.2009.10.004. [DOI] [PubMed] [Google Scholar]
- Emslie G, Kratochvil C, Vitiello B, Silva S, Mayes T, McNulty, March J. Treatment for adolescents with depression study (TADS): Safety results. Journal of the American Academy of Child and Adolescent Psychiatry. 2006;45(12):1440–1455. doi: 10.1097/01.chi.0000240840.63737.1d. doi: 10.1097/01.chi.0000240840.63737.1d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fallone G, Owens JA, Deane J. Sleepiness in children and adolescents: Clinical implications. Sleep Medicine Reviews. 2002;6(4):287–306. doi: 10.1053/smrv.2001.0192. doi: 10.1053/smrv.2001.0192. [DOI] [PubMed] [Google Scholar]
- Forbes EE, Bertocci MA, Gregory AM, Ryan ND, Axelson DA, Birmaher B, Dahl RE. Objective sleep in pediatric anxiety disorders and major depressive disorder. Journal of the American Academy of Child and Adolescent Psychiatry. 2008;47(2):148–155. doi: 10.1097/chi.0b013e31815cd9bc. doi: 10.1097/chi.0b013e31815cd9bc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gregory AM, Caspi A, Eley TC, Moffitt TE, O'Connor TG, Poulton R. Prospective longitudinal associations between persistent sleep problems in childhood and anxiety and depression disorders in adulthood. Journal of Abnormal Child Psychology. 2005;33(2):157–163. doi: 10.1007/s10802-005-1824-0. doi: 10.1007/s10802-005-1824-0. [DOI] [PubMed] [Google Scholar]
- Gregory AM, Eley TC, Moffitt TE. Sleep problems, anxiety and cognitive style in school-aged children. Infant and Child Development. 2005;33(2):157–163. doi: 10.1007/s10802-005-1824-0. [Google Scholar]
- Gregory AM, O'Connor TG. Sleep problems in childhood: A longitudinal study of developmental change and association with behavioral problems. Journal of the American Academy of Child and Adolescent Psychiatry. 2002;41(8):964–971. doi: 10.1097/00004583-200208000-00015. doi: 10.1097/00004583-200208000-00015. [DOI] [PubMed] [Google Scholar]
- Gregory AM, Rijsdijk FV, Dahl RE, McGuffin P, Eley TC. Associations between sleep problems, anxiety, and depression in twins at 8 years of age. Pediatrics. 2006;118(3):1124–1132. doi: 10.1542/peds.2005-3118. doi: 10.1542/peds.2005-3118. [DOI] [PubMed] [Google Scholar]
- Gregory AM, Van der Ende J, Willis TA, Verhulst FC. Parent-reported sleep problems during development and self-reported anxiety/depression, attention problems, and aggressive behavior later in life. Archives of Pediatrics & Adolescent Medicine. 2008;162(4):330–335. doi: 10.1001/archpedi.162.4.330. [DOI] [PubMed] [Google Scholar]
- Guy W. Clinical global impression scale. The ECDEU Assessment Manual for Psychopharmacology-Revised. 1976;76(338):218–222. [Google Scholar]
- Hagenauer MH, Perryman JI, Lee TM, Carskadon MA. Adolescent changes in the homeostatic and circadian regulation of sleep. Developmental Neuroscience. 2009;31(4):276–284. doi: 10.1159/000216538. doi: 10.1159/000216538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hansen BH, Skirbekk B, Oerbeck B, Richter J, Kristensen H. Comparison of sleep problems in children with anxiety and attention deficit/hyperactivity disorders. European Child and Adolescent Psychiatry. 2011;20(6):321–330. doi: 10.1007/s00787-011-0179-z. doi: 10.1007/s00787-011-0179-z. [DOI] [PubMed] [Google Scholar]
- Hayton JC, Allen DG, Scarpello V. Factor retention decisions in exploratory factor analysis: A tutorial on parallel analysis. Organizational Research Methods. 2004;7(2):191–205. doi: 10.1177/1094428104263675. [Google Scholar]
- Hvolby A, Jørgensen J, Bilenberg N. Parental rating of sleep in children with attention deficit/hyperactivity disorder. European Child & Adolescent Psychiatry. 2009;18(7):429–438. doi: 10.1007/s00787-009-0750-z. doi: 10.1007/s00787-009-0750-z. [DOI] [PubMed] [Google Scholar]
- Ivanenko A, Crabtree VM, Obrien LM, Gozal D. Sleep complaints and psychiatric symptoms in children evaluated at a pediatric mental health clinic. Journal of Clinical Sleep Medicine. 2006;2(1):42–48. [PubMed] [Google Scholar]
- Kendall PC, Choudhury M, Hudson J, Webb A. The CAT project therapist manual. Workbook Publishing; Ardmore, PA: 2002. [Google Scholar]
- Kendall PC, Compton S, Walkup J, Birmaher B, Albano AM, Sherrill J, Piacentini J. Clinical characteristics of anxiety disordered youth. Journal of Anxiety Disorders. 2010;24:360–365. doi: 10.1016/j.janxdis.2010.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendall PC, Hudson JL, Gosch E, Flannery-Schroeder E, Suveg C. Cognitive-behavioral therapy for anxiety disordered youth: a randomized clinical trial evaluating child and family modalities. Journal of Consulting and Clinical Psychology. 2008;76(2):282. doi: 10.1037/0022-006X.76.2.282. [DOI] [PubMed] [Google Scholar]
- Kendall PC, Hedtke KA. Cognitive-behavioral therapy for anxious children: Therapist manual. 3rd ed. Workbook Publishing; Ardmore, PA: 2006. [Google Scholar]
- Kendall PC, Pimentel SS. On the physiological symptom constellation in youth with generalized anxiety disorder (GAD). Journal of Anxiety Disorders. 2003;17(2):211–221. doi: 10.1016/s0887-6185(02)00196-2. doi: 10.1016/S0887-6185(02)00196-2. [DOI] [PubMed] [Google Scholar]
- Langley AK, Bergman RL, McCracken J, Piacentini JC. Impairment in childhood anxiety disorders: Preliminary examination of the child anxiety impact scale-parent version. Journal of Child and Adolescent Psychopharmacology. 2004;14(1):105–114. doi: 10.1089/104454604773840544. doi: 10.1089/104454604773840544. [DOI] [PubMed] [Google Scholar]
- Langley AK, Falk A, Peris T, Wiley JF, Kendall PC, Ginsburg G, Piacentini J. The Child Anxiety Impact Scale: Examining parent-and child-reported impairment in child anxiety disorders. Journal of Clinical Child and Adolescent Psychology. 2014;43(4):579–591. doi: 10.1080/15374416.2013.817311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leahy E, Gradisar M. Dismantling the bidirectional relationship between pediatric sleep and anxiety. Clinical Psychologist. 2012;16(1):44–56. doi: 10.1111/j.1742-9552.2012.00039.x. [Google Scholar]
- Lebowitz ER, Woolston J, Bar-Haim Y, Dauser C, Warnick E, Warnick E, Leckman JF. Depression and Anxiety. 2013;30(1):47–54. doi: 10.1002/da.21998. doi: 10.1002/da.21998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leproult R, Van Cauter E. Role of sleep and sleep loss in hormonal release and metabolism. Endocrine Development. 2010;17:11–21. doi: 10.1159/000262524. doi:10.1159/000262524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- March JS, Parker JD, Sullivan K, Stallings P, Conners CK. The multidimensional anxiety scale for children (MASC): Factor structure, reliability, and validity. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36(4):554–565. doi: 10.1097/00004583-199704000-00019. doi: 10.1097/00004583-199704000-00019. [DOI] [PubMed] [Google Scholar]
- Masi G, Millepiedi S, Mucci M, Poli P, Bertini N, Milantoni L. Generalized anxiety disorder in referred children and adolescents. Journal of the American Academy of Child and Adolescent Psychiatry. 2004;43(6):752–760. doi: 10.1097/01.chi.0000121065.29744.d3. doi: 10.1097/01.chi.0000121065.29744.d3. [DOI] [PubMed] [Google Scholar]
- Mayes SD, Calhoun SL, Bixler EO, Vgontzas AN, Mahr F, Hillwig-Garcia J, Parvin M. ADHD subtypes and comorbid anxiety, depression, and oppositional-defiant disorder: Differences in sleep problems. Journal of Pediatric Psychology. 2009;34(3):328–337. doi: 10.1093/jpepsy/jsn083. doi: 10.1093/jpepsy/jsn083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mick E, Biederman J, Jetton J, Faraone SV. Sleep disturbances associated with attention deficit hyperactivity disorder: The impact of psychiatric comorbidity and pharmacotherapy. Journal of Child and Adolescent Psychopharmacology. 2000;10(3):223–231. doi: 10.1089/10445460050167331. doi: 10.1089/10445460050167331. [DOI] [PubMed] [Google Scholar]
- Mindell JA, Barrett KM. Nightmares and anxiety in elementary-aged children: Is there a relationship? Child: Care, Health and Development. 2002;28(4):317–322. doi: 10.1046/j.1365-2214.2002.00274.x. doi: 10.1046/j.1365-2214.2002.00274.x. [DOI] [PubMed] [Google Scholar]
- Mindell JA, Owens J, Alves R, Bruni O, Goh DY, Hiscock H, Sadeh A. Give children and adolescents the gift of a good night's sleep: A call to action. Sleep Medicine. 2011;12(3):203–204. doi: 10.1016/j.sleep.2011.01.003. [DOI] [PubMed] [Google Scholar]
- Morrison DN, McGee ROB, Stanton WR. Sleep problems in adolescence. Journal of the American Academy of Child and Adolescent Psychiatry. 1992;31(1):94–99. doi: 10.1097/00004583-199201000-00014. doi: 10.1097/00004583-199201000-00014. [DOI] [PubMed] [Google Scholar]
- Ong SH, Wickramaratne P, Tang M, Weissman MM. Early childhood sleep and eating problems as predictors of adolescent and adult mood and anxiety disorders. Journal of Affective Disorders. 2006;96(1):1–8. doi: 10.1016/j.jad.2006.05.025. doi: 10.1016/j.jad.2006.05.025. [DOI] [PubMed] [Google Scholar]
- Owens JA. The ADHD and Sleep Conundrum: A Review. Journal Of Developmental And Behavioral Pediatrics. 2005;26(4):312–322. doi: 10.1097/00004703-200508000-00011. doi:10.1097/00004703-200508000-00011. [DOI] [PubMed] [Google Scholar]
- Paavonen EJ, Solantaus T, Almqvist F, Aronen ET. Four-year follow-up study of sleep and psychiatric symptoms in preadolescents: Relationship of persistent and temporary sleep problems to psychiatric symptoms. Journal of Developmental and Behavioral Pediatrics. 2003;24(5):307–314. doi: 10.1097/00004703-200310000-00001. [DOI] [PubMed] [Google Scholar]
- Petersen AC, Crockett L, Richards M, Boxer A. A self-report measure of pubertal status: Reliability, validity, and initial norms. Journal of Youth and Adolescence. 1988;17(2):117–133. doi: 10.1007/BF01537962. doi: 10.1007/BF01537962. [DOI] [PubMed] [Google Scholar]
- Piacentini J, Bergman RL, Keller M, McCracken J. Functional impairment in children and adolescents with obsessive-compulsive disorder. Journal of Child and Adolescent Psychopharmacology. 2003;13(2, Supplement 1):61–69. doi: 10.1089/104454603322126359. doi: 10.1089/104454603322126359. [DOI] [PubMed] [Google Scholar]
- Pina AA, Silverman WK, Fuentes RM, Kurtines WM, Weems CF. Exposure-based cognitive-behavioral treatment for phobic and anxiety disorders: Treatment effects and maintenance for Hispanic/Latino relative to European-American youths. Journal of the American Academy of Child and Adolescent Psychiatry. 2003;42(10):1179–1187. doi: 10.1097/00004583-200310000-00008. doi: 10.1097/00004583-200310000-00008. [DOI] [PubMed] [Google Scholar]
- Reinhard SC, Gubman GD, Horwitz AV, Minsky S. Burden assessment scale for families of the seriously mentally ill. Evaluation and program planning. 1994;17(3):261–269. doi: 10.1016/0149-7189(94)90004-3. [Google Scholar]
- Research Units on Pediatric Psychopharmacology Anxiety Study Group Fluvoxamine for the treatment of anxiety disorders in children and adolescents. New England Journal of Medicine. 2001;344(17):1279–1285. doi: 10.1056/NEJM200104263441703. [DOI] [PubMed] [Google Scholar]
- Research Units on Pediatric Psychopharmacology Anxiety Study Group The pediatric anxiety rating scale (PARS): Development and psychometric properties. Journal of the American Academy of Child and Adolescent Psychiatry. 2002;41(9):1061–1069. doi: 10.1097/00004583-200209000-00006. doi: 10.1097/00004583-200209000-00006. [DOI] [PubMed] [Google Scholar]
- Roehrs T, Hyde M, Blaisdell B, Greenwald M, Roth T. Sleep loss and REM sleep loss are hyperalgesic. Sleep. 2006;29(2):145–151. doi: 10.1093/sleep/29.2.145. [DOI] [PubMed] [Google Scholar]
- Rynn MA, Siqueland L, Rickels K. Placebo-controlled trial of sertraline in the treatment of children with generalized anxiety disorder. The American Journal of Psychiatry. 2001;158(12):2008–2014. doi: 10.1176/appi.ajp.158.12.2008. doi:10.1176/appi.ajp.158.12.2008. [DOI] [PubMed] [Google Scholar]
- Rynn MA, Walkup JT, Compton SN, Sakolsky DJ, Sherrill JT, Shen S, Birmaher B. Child/Adolescent Anxiety Multimodal Study: Evaluating Safety. Journal of the American Academy of Child & Adolescent Psychiatry. 2014;54(3):180–190. doi: 10.1016/j.jaac.2014.12.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sagaspe P, Sanchez-Ortuno M, Charles A, Taillard J, Valtat C, Bioulac B, Philip P. Effects of sleep deprivation on Color-Word, Emotional, and Specific Stroop interference and on self-reported anxiety. Brain and Cognition. 2006;60(1):76–87. doi: 10.1016/j.bandc.2005.10.001. doi: 10.1016/j.bandc.2005.10.001. [DOI] [PubMed] [Google Scholar]
- Silverman W, Albano A. The anxiety disorders interview schedule for DSM-IV: Child and parent version. Graywind; San Antonio: 1996. [Google Scholar]
- Silverman WK, Saavedra LM, Pina AA. Test-retest reliability of anxiety symptoms and diagnoses with the anxiety disorders interview schedule for DSM-IV: Child and parent versions. Journal of the American Academy of Child and Adolescent Psychiatry. 2001;40(8):937–944. doi: 10.1097/00004583-200108000-00016. doi: 10.1097/00004583-200108000-00016. [DOI] [PubMed] [Google Scholar]
- Storch EA, Murphy TK, Lack CW, Geffken GR, Jacob ML, Goodman WK. Sleep-related problems in pediatric obsessive-compulsive disorder. Journal of anxiety disorders. 2008;22(5):877–885. doi: 10.1016/j.janxdis.2007.09.003. doi: 10.1016/j.janxdis.2007.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walkup JT, Albano AM, Piacentini J, Birmaher B, Compton SN, Sherrill JT, Kendall PC. Cognitive behavioral therapy, sertraline, or a combination in childhood anxiety. New England Journal of Medicine. 2008;359(26):2753–2766. doi: 10.1056/NEJMoa0804633. doi: 10.1056/NEJMoa0804633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wood JJ, Piacentini JC, Bergman RL, McCracken JT, Barrios V. Concurrent validity of the anxiety disorders section of the Anxiety Disorders Interview Schedule: Child/Parent Versions. Journal of Clinical Child and Adolescent Psychology. 2002;40:335–342. doi: 10.1207/S15374424JCCP3103_05. [DOI] [PubMed] [Google Scholar]
- Zhang B, Hao Y, Jia F, Tang Y, Li X, Liu W, Arnulf I. Sertraline and rapid eye movement sleep without atonia: An 8-week, open-label study of depressed patients. Progress in Neuro-Psychopharmacology and Biological Psychiatry. 2013;47:85–92. doi: 10.1016/j.pnpbp.2013.08.010. [DOI] [PubMed] [Google Scholar]
- Zuckerman B, Stevenson J, Bailey V. Sleep problems in early childhood: Continuities, predictive factors, and behavioral correlates. Pediatrics. 1987;80(5):664–671. [PubMed] [Google Scholar]
- Zwick WR, Velicer WF. Comparison of five rules for determining the number of components to retain. Psychological Bulletin. 1986;99(3):432. doi10.1037/0033-2909.99.3.432. [Google Scholar]