Abstract
Aim:
In this study, we aimed to estimate one- to five-year survival rates in Iranian patients with gastric cancer (GC). In addition, we preformed subgroup analyses and meta-regression to explore possible sources of heterogeneity between studies.
Background:
According to literatures, there has been increasing attention to the long-term survival rate in patients with GC in Iran. However, results have been inconsistent and remain controversial in overall survival rates.
Patients and methods:
Literature searches were conducted using PubMed, Scopus, and ISI, as well as Magiran, Medlib, SID, and Iran Medex databases. Studies were pooled and summary one to five survival rates were calculated. Univariate and multivariate regression analyses were used to explore possible sources of heterogeneity among studies. Subgroup analyses were also conducted. Analyses were conducted using the STATA statistical software package.
Results:
Final analysis of 29361 patients from 26 eligible studies was performed. The overall survival rate (one to five years) in all studies, by meta-analysis of 24, 14, 23, 12 and 22 studies were 52%, 31%, 24%, 22%, and 15%, respectively. Meta-regression analysis showed an increase in one- and five-year survival rate over the time (Reg Coef = 0.016, p= 0.04) and (Reg Coef= 0.021, p= 0.049), respectively. Positive heterogeneity was observed between quality of papers and data sources (P<0.001).
Conclusion:
More than half of GC deaths happened in the first year at diagnosis, and another 30% plus they occurred during the second year after confirmed diagnosis. Our results admit lower survival rates in Iran, similar to other developing countries.
Key Words: Gastric cancer, Survival rate, Meta-analysis, Systematic review, Heterogeneityndrial
Introduction
Every year, 7 million lives are lost due to preventable and treatable cancers (1). Incidence rates of cancers could increase substantially in the future, with up to 15 million new cases in 2020, most of which will be in developing countries (2). Among all cancer types, gastric cancer (GC) is one of the leading causes of death in recent decades, and its death toll has been steadily increasing in Asia and across the globe (3). Environmental factors such as obesity and gastroesophageal reflux disease are thought to contribute to its deadliness (4). At diagnosis, 23% of GC cases are localized, 32% are detected in the lymph nodes, and 34% are metastatic (5). In localized cases, treatment usually involves a combination of surgery, radiation, and chemotherapy, supplemented with adjuvant therapy (6, 7).
Misdiagnosis is the greatest obstacle facing treatment of GC in Iran (8-10). In most cases, by the time the disease is detected and properly diagnosed, surgery is the only viable option. Therefore, early detection and screening programs are critical to improve prognoses in GC patients (11, 12). In the last decade, there are a growing number of Iranian studies, which have focused on the rate of GC survival. Results of these studies indicate that survival rates in Iran are consistent with those in other developing countries, but lower than those in developed countries (13).
It is difficult to conduct population-based cancer studies in Iran, due to incomplete hospital records, careless registration processes, insufficient training, haphazard patient follow-up policies, and a lack of regional and provincial cancer centers. Inconsistent GC survival rates are also a prevalent feature in Iranian medicine, the lowest and highest of which were 81% (14) and 21% (15), respectively, for one year, and 31% (16) and 5.4% (17), respectively, for five years.
According to our research, no recent systematic review has focused on GC survival in Iran. The present study intends to contribute to the extant literature by providing a systematic review and meta-analysis of one- and five-year survival rates in Iranian GC patients, and performing subgroup analyses and meta-regression to explore possible sources of heterogeneity among included studies.
Methods
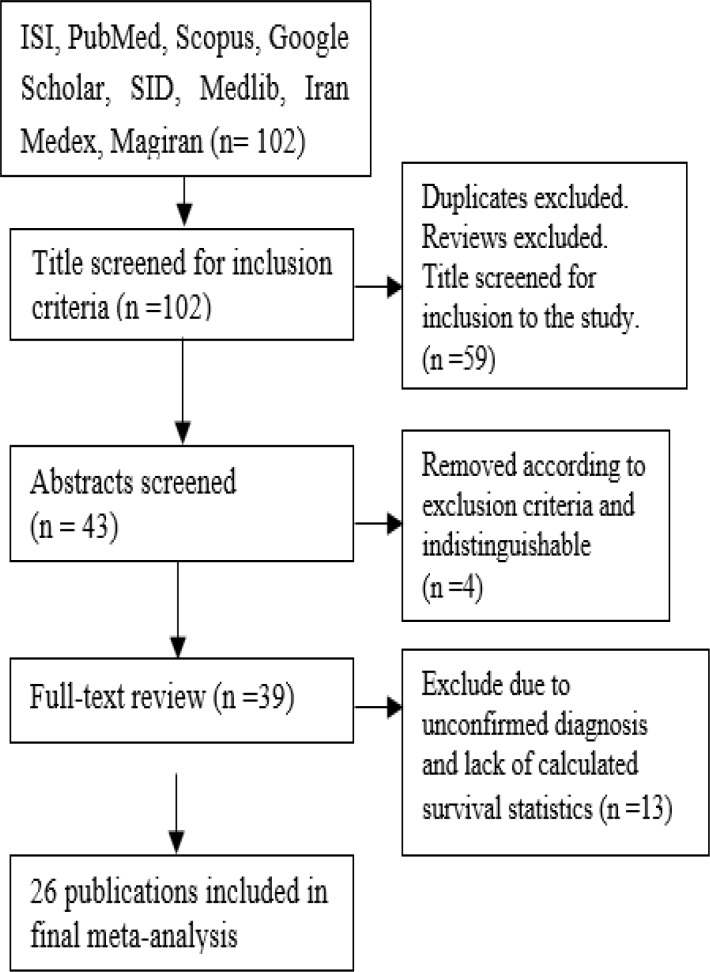
Through an electronic and manual search, 102 papers were identified (Table1). After exclusion of reviews and duplicate articles, as well as title screen, 43 separate publications remained for further appraisal. Remained articles, subsequent to abstract and full text review we removed 17 publications according to exclusion criteria and in final data set consisted of 26 publications (Figure 1). Interpretation results of table 2 shows attention to survival rate in patients with GC in Iran is increasing as if (64.4%) of final articles were published in 2011 onwards. Hospital records were the primary data source for the greater part of studies (61.5%). The pooled participants in the study were 29361 patients with GC (Table1).
Table 1.
Feature and characteristic studies included in study
| Ref. No. |
First Author (Year of Pub) |
Years of flow Sitting |
No. of Patients | Data source | Analysis | Survival Rate (%) |
Quality* | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1-Year | 2-Year | 3-Year | 4-Year | 5-Year | |||||||
| (19) | Biglarian A 2011 |
2002-2007, Tehran |
436 | Hospital records | Cox proportional hazards | 78 | 53 | 41 | 32 | 17 | High |
| (20) | Mehrabian AA 2010 |
2001-2006, National | 19537 | Iran Cancer Registration Center |
Life time table | 49 | 29 | 23 | 23 | 15 | High |
| (16) | Soroush A 2013 |
2008-2010, | 98 | Hospital records | Kaplan–Meier method and Cox proportional hazard models | 60 | 31 | High | |||
| (21) | Zare A 2013 |
1995-1999, National |
330 | Iran Cancer Institute | Cox proportional hazards model | 66 | 42 | 31 | 26 | 21 | High |
| (22) | Baghestani AR 2009 |
2003-2008, Tehran | 178 | Hospital records | Bayesian Weibull and Exponential models | 80 | 52 | 35 | High | ||
| (23) | Moghimi-Dehkordi B 2008 |
2001-2006, Tehran |
746 | Cancer Registry Center |
life-table method and Wilcoxon (Gehan) test | 73 | 50 | 40 | 33 | 29 | High |
| (24) | Samadi F 2007 |
2000-2004, Ardabil | 279 | Hospital records | Kaplan–Meier method and Cox proportional hazard models | 41 | 8 | High | |||
| (25) | Noorkojuri H 2013 |
2003-2008, Tehean |
216 | Tehran Cancer Registry | Cox proportional hazards and smoothing methods | 80 | 56 | 40 | 35 | 30 | High |
| (26) | Yazdani-Charati J 2014 |
2007-2010, Sari | 190 | Hospital records | Kaplan-Meier method |
45 | 26 | 8 | High | ||
| (27) | Ghadimi Gh 2011 |
1990-199, Babol |
484 | Cancer Registration Center | Weibull, Log-normal, and the Log-logistic model | 24 | 16 | 15 | High | ||
| (28) | Maroufizadeh S 2011 |
2003-1008, Tehean |
213 | Cancer Registration Center | Cox and Additive hazards models | 79 | 35 | 14 | High | ||
| (15) | Bashash M, 2011 |
2004, Ardabil |
261 | population-based cancer registries | Life-tables | 21 | High | ||||
| (29) | Movahedi M, 2009 |
2001-2005, National |
3189 | national cancer registry | Kaplan-Meier method |
48 | 27 | 19 | 16 | 13 | High |
| (17) | Veisani Y, 2013 |
2006-2011, Sanandaj |
239 | Hospital records | Kaplan-Meier method |
41 | 17 | 13 | 10 | 6 | High |
| (30) | Atoof F, 2010 |
1995-2004, Tehran |
330 | Hospital records | Kaplan-Meier and Weibull Cure Models | 32 | 20 | Medium | |||
| (31) | Roshanaei Gh, 2012 |
2003 – 2007, Tehran |
400 | Hospital records | Cox proportional hazards | 74 | 54 | 31 | 26 | 23 | Medium |
| (32) | Moghimi-Dehkordi B, 2007 |
2001-2005, Tehran |
442 | Cancer Registration Center | Kaplan–Meier and Cox proportional hazard models | 54 | 30 | 24 | 18 | 16 | Medium |
| (33) | Barfei F, 2014 |
2007-2008, Tehran |
99 | Hospital records | Kaplan–Meier and Cox proportional hazard models | 59 | 40 | 18 | Low | ||
| (34) | Kashani H, 2011 |
1995-1999, Tehran |
330 | Hospital records | Kaplan–Meier and Cox proportional hazard models | 62 | 41 | 31 | 24 | 20 | Medium |
| (35) | Baeradeh NA, 2015 |
2006-2010, Yazd |
136 | Hospital records | Kaplan–Meier and Cox proportional hazard models | 61 | 45 | 31 | 26 | 25 | Medium |
| (36) | Zeraati H, 2005 |
1995-1999, Tehran |
129 | Hospital records | A non-homogenous semi-Markovian stochastic process | 67 | 31 | 19 | Medium | ||
| (37) | Ghorbani S, 2013 |
2007-2012, Sari |
430 | Cancer Registration Center | Kaplan - Meier and univariate analysis |
64 | 44 | 34 | 28 | 19 | Medium |
| (14) | Roshanaei Gh, 2010 |
2003-2007, Tehran |
262 | Hospital records | Kaplan–Meier and Cox proportional hazard models | 81 | 45 | 30 | Low | ||
| (38) | Roshanaei Gh, 2011 |
2003-2007, Tehran |
93 | Hospital records | Kaplan–Meier models | 42 | 19 | 13 | Medium | ||
| (39) | Larizadeh MH,2013 | 2003-2011-Kerman | 82 | Hospital records | Kaplan-Meier methods | 53 | 22 | Low | |||
| (40) | Gohari MR, 2014 |
2002-2007, Tehran |
232 | Hospital records | Kaplan-Meier methods | 77 | 26 | Low | |||
Figure 1.
Flow diagram shows different steps involved in searching for relevant publications (2005–2015
Table 2.
Subcategories analysis of one to five survival rates by quality and data source
| Subcategories |
Survival Rate% (95% CI)
|
Heterogeneity
|
||||||
|---|---|---|---|---|---|---|---|---|
| 1-Year | 2-Year | 3-Year | 4-Year | 5-Year | I2 (%) | P value | ||
| Quality | High | 51(50-51) | 30(29-30) | 23(22-23) | 22(22-23) | 15(14-15) | 98.8 | <0.0001 |
| Medium | 63(61-65) | 42(39-44) | 29(28-31) | 24(22-26) | 19(18-21) | 89.6 | <0.0001 | |
| Low | 77(73-80) | - | 38(34-41) | 22(13-31) | 26(21-30) | 87.5 | <0.0001 | |
| Data Source | Hospital records | 67(65-68) | 41(38-43) | 27(26-29) | 22(20-24) | 16(14-17) | 96.7 | <0.0001 |
| Cancer registry center | 50(49-51) | 30(29-30) | 23(23-24) | 22(22-23) | 15(15-16) | 97.7 | <0.0001 | |
| Overall survival rate | 52(52-53) | 31(30-31) | 24(23-24) | 22(22-23) | 15(15-16) | 95.6 | <0.0001 | |
Twenty-four eligible papers including 28949 patients were included in meta-analysis to estimate of one-year survival rate. The overall one year survival rate in patients with GC in Iran was 0.52 (95% CI: 0.52 to 0.53). A significant heterogeneity among these studies was observed (heterogeneity statistic= 379.79, P<.001, I2= 98.5%, 95% CI 97.4–99.8) (Figure 2).
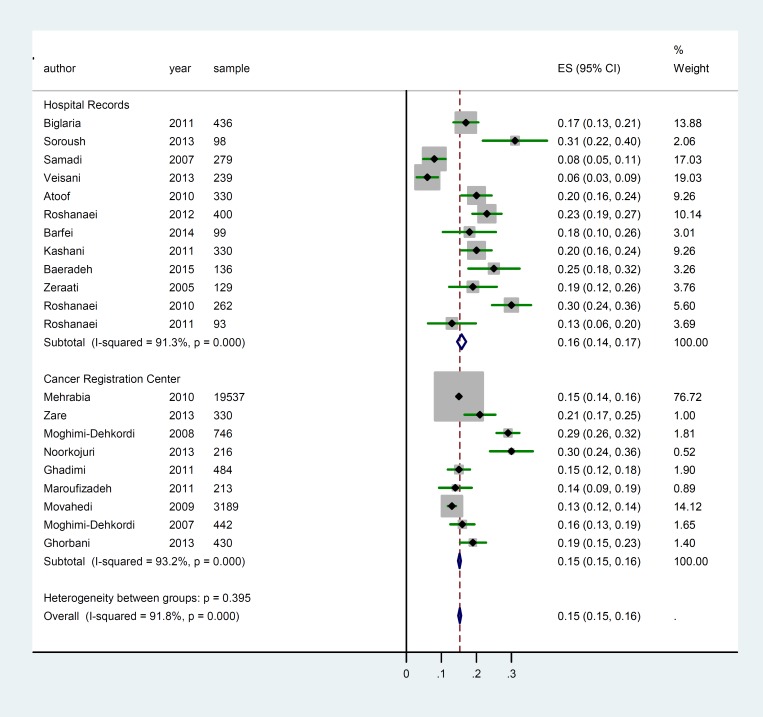
For Meta-analysis of five-year survival rate twenty-two publications with 28268 patients were considered. The overall five year survival rate in patients with GC in Iran was 0.15 (95% CI: 0.15 to 0.16).
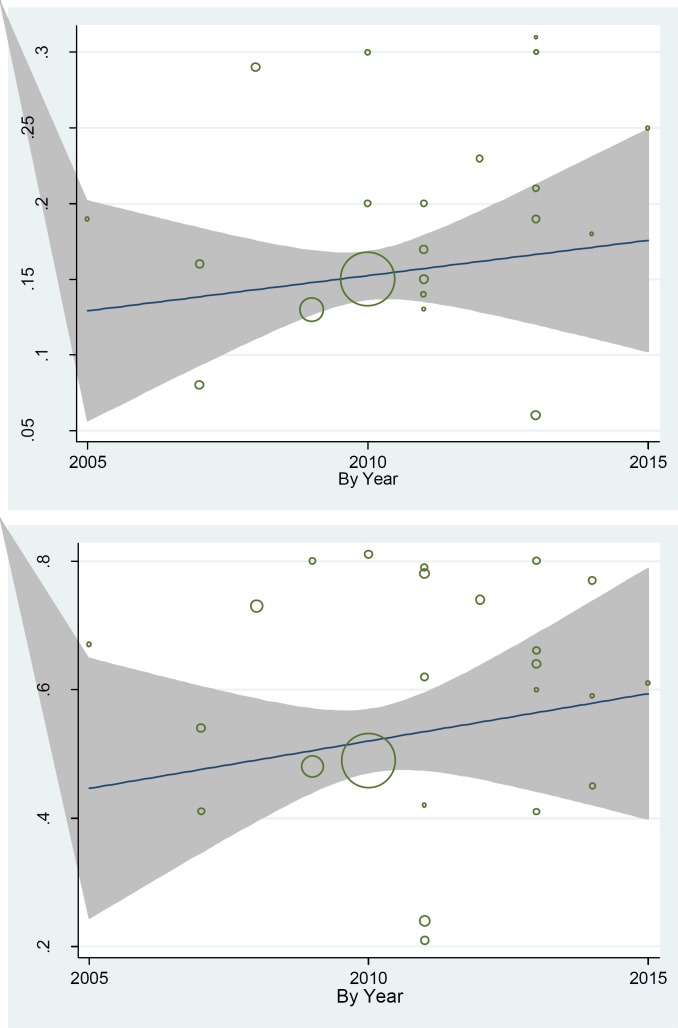
A significant heterogeneity among these studies was observed (heterogeneity statistic= 472.23, P<0.001, I 2 = 91.8% (95% CI: 90.1–93.5) (Fig. 3). Subgroup analysis was preformed to explore possible sources of heterogeneity among studies. Results of subgroup analysis showed a positive heterogeneity between quality of papers and data sources (P< 0.001). Table 2 presented these results; one- to five-year survival rate in publication with good quality is lower than articles with medium and low quality, respectively. Also one- to five-year survival rate in studies with cancer registry center data source is lower than hospital records. Results of meta-regression showed an association between publication year and one year survival rate, as well as five-year survival rate. Thus, year of publication is one of the main causes of variability in results of one- to five-year survival rate (Reg Coef= 0.016, p= 0.04) and (Reg Coef= 0.021, p= 0.049), respectively (Fig. 4). According to results, an increasing rate of survival was observed across the study period. Also, we examined sample size as another explanatory factor to variability in results, which showed sample size was another reason for this inconsistency in results (Reg Coef= 0.00033, p= 0.027). Studies with a large sample size had a lower survival rate compared to studies with small sample size.
Figure 4.
Meta-regression plots of change in one and five survival rate according to changes in continuous study moderator’s year
Results
Using electronic searches, 102 papers were identified. After exclusion of reviews and duplicate articles and title screen, 43 separate publications remained for further appraisal. Remained articles, subsequent to abstract and full text review, we removed 17 publications according to the exclusion criteria and in the final data set consisted of 26 publications (Fig. 1). Interpretation results of table 2 shows attention to survival rate in patients with GC in Iran is increasing as if (64.4%) of final articles were published in 2011onwards. Primary data source for the greater part of studies (61.5) was hospital records.
The pooled participants in study were 29361 patients with GC (Table 1).
Twenty-four eligible papers, including 28949 patients were included in meta-analysis to estimate one-year survival rate. The overall one-year survival rate in patients with GC in Iran was 0.52 (95% CI: 0.52 to 0.53). There was a significant heterogeneity among these studies (heterogeneity statistic = 379.79, P<0.001, I 2 = 98.5%, 95% CI 97.4–99.8) (Fig. 2).
For Meta-analysis of five-year survival rate, we considered twenty-two publications with 28268 patients. The overall five year survival rate in patients with GC in Iran was 0.15 (95% CI, 0.15 to 0.16). A significant heterogeneity among these studies was observed (heterogeneity statistic= 472.23, P<0.001, I 2= 91.8% (95% CI: 90.1–93.5) (Fig. 3). Subgroup analysis was performed to explore possible sources of heterogeneity among studies. Results of subgroup analysis showed a positive heterogeneity between quality of papers and data sources (P<0.001). Table 2 presented these results; one- to five-year survival rate in publication with good quality is lower than articles with medium and low quality, respectively. Also, one- to five- year survival rate in studies with cancer registry center data source is lower than hospital records. Results of meta-regression showed an association between publication year and one-year survival rate, as well as five-year survival rate. Thus, year of publication is a cause of variability in results of one and five year survival rate (Reg Coef= 0.016, p= 0.04) and (Reg Coef= 0.021, p= 0.049), respectively (Fig. 4). According to results, an increasing survival rate across the study period was observed. Also, we examined the sample size as other explanatory factor to variability in results and results showed sample size was another reason for this inconsistency in results (Reg Coef= 0.00033, p= 0.027). Studies with larger sample size had a lower survival rate.
Figure 3.
Meta-analysis of the five year survival rate by different data source (Hospital Records and Cancer Registry Centers)
Discussion
In the present meta-analysis, we employed a large sample size to generate a reliable estimation of GC patient survival rates. We found a significant heterogeneity in our results, sources of which we explored using meta-regression and stratified subgroup analysis according to characteristics of the included studies. Our results showed that sample size and publication year were significant contributing factors to heterogeneity, where larger sample size and later year of publication were associated with a lower recorded rate of survival. In the present study, heterogeneity might result from different characteristics of patients, differing stages of disease progression, adjuvant treatment, duration of patient follow-up, or histological type. Due to limited resources in previous studies, we were unable to specify the role of these features that might contribute to disparate survival rates.
Ultimately, 26 studies were incorporated into our meta-analysis. Estimation of overall survival rate, and the one- through five-year rates of 24, 14, 23, 12, and 22 were 52%, 31%, 24%, 22%, and 15%, respectively. These numbers indicate that more than half of GC deaths occurred within the first year following diagnosis, and another 30% took place during the second year. It is the greatest difficulty about patients with GC in Iran versus worthwhile clinical finding to correct rational strategies to address these problems. Various histological and demographic factors such as age, gender, surgery and treatment type, cancer site, grade of tumor, as well as metastasis have been found to impact the rate of GC survival in Iran. An investigation into risk factors associated with GC may help to reduce the probability of death in patients. Other strategies include a comprehensive follow-up plan for patients with premature signs of the disease, as well as the study and application of suitable treatments (5).
Results of the present study suggest that the overall five-year survival rate in Iran (15%) is lower than the survival rate in countries such as China (29.6%), the United States (37%), Switzerland (22%), France (30%), and Japan (40-60%)(1, 13, 41). We classify possible explanations for this inconsistency into three main factors: cancer stage at diagnosis, patient characteristics, and treatment process. In most studies, late diagnosis was related to a lower survival rate, while diagnosis at an early stage was determined to be the most important predictive factor for survival. In terms of patient characteristics, a lower survival rate was associated with older and socioeconomically disadvantaged patients, as well as those who did not respond favorably to the treatment. Finally, mixed therapies incorporating chemotherapy, radiotherapy, and surgery were shown to strongly enhance the rate of survival.
As mentioned, a nationwide lack of cancer registry centers presents an additional obstacle to investigating GC in Iran, and the results of this study demonstrate this limitation. Although 64.4% of sources were derived from cancer registry data, the overall survival rates were lower than the results obtained from hospital records. Hospital records in developing countries are generally limited because data are missing, riddled with errors, or not deliberately gathered for the purpose of later scrutiny. Additionally, eligible patients for the present study were from one distinct hospital and could not represent all coverage patients in a population.
The present meta-analysis expanded the number of participants to produce reliable and generalizable results regarding the GC survival rate in Iran. Limitations of this study were heterogeneity among 26 included studies, a scarcity of abstracts, and the inclusion of only 11 studies out of 102 gathered due to lack of available survival statistics. These limitations could impact the findings of this analysis.
According to our research, more than half of GC deaths occurred in the first year after diagnosis, and another 30% took place during the second year. These findings support previous reports that suggest a poor diagnosis is the greatest challenge to GC patients in Iran.
Note
(Please cite as: Yousef Veisani, Ali Delpisheh. Survival rate of gastric cancer in Iran; a systematic review and meta-analysis. Gastroenterol Hepatol Bed Bench 2016;9(2):78-86).
References
- 1.Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011;61:69–90. doi: 10.3322/caac.20107. [DOI] [PubMed] [Google Scholar]
- 2.Pourhoseingholi MA, Vahedi M, Baghestani AR. Burden of gastrointestinal cancer in Asia; an overview. Gastroenterol Hepatol Bed Bench. 2015;8:19–27. [PMC free article] [PubMed] [Google Scholar]
- 3.Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer. 2010;127:2893–917. doi: 10.1002/ijc.25516. [DOI] [PubMed] [Google Scholar]
- 4.Pourfarzi F, Whelan A, Kaldor J, Malekzadeh R. The role of diet and other environmental factors in the causation of gastric cancer in Iran—A population based study. Int J Cancer. 2009;125:1953–60. doi: 10.1002/ijc.24499. [DOI] [PubMed] [Google Scholar]
- 5.Sjoquist KM, Burmeister BH, Smithers BM, Zalcberg JR, Simes RJ, Barbour A, et al. Survival after neoadjuvant chemotherapy or chemoradiotherapy for resectable oesophageal carcinoma: an updated meta-analysis. Lancet Oncol. 2011;12:681–92. doi: 10.1016/S1470-2045(11)70142-5. [DOI] [PubMed] [Google Scholar]
- 6.Yonemura Y, Endou Y, Sasaki T, Hirano M, Mizumoto A, Matsuda T, et al. Surgical treatment for peritoneal carcinomatosis from gastric cancer. Eur J Surg Oncol. 2010;36:1131–138. doi: 10.1016/j.ejso.2010.09.006. [DOI] [PubMed] [Google Scholar]
- 7.Veisani Y, Delpisheh A, Sayehmiri K, Rahimi E. Survival rate estimation and its associated factors in patients with stomach cancer in Tohid Hospital in Sanandaj. Scientific Journal of Kurdistan University of Medical Sciences. 2013;18:1–8. [Google Scholar]
- 8.Mehrabian AA, Esna-Ashari F, Zham H, Hadizadeh M, Bohlooli M, Khayamzadeh M, et al. Gastric cancer prevalence, according to survival data in Iran (National Study-2007) Iranian J Pub Health. 2010;39:27–31. [PMC free article] [PubMed] [Google Scholar]
- 9.Delpisheh A, Veisani Y, Sayehmiri K, Rahimi E. Esophageal carcinoma: long-term survival in consecutive series of patients through a retrospective cohort study. Gastroenterol Hepatol Bed Bench. 2014;7:101–107. [PMC free article] [PubMed] [Google Scholar]
- 10.Yarhusseini A, Sharifzadeh L, Delpisheh A, Veisani Y, Sayehmiri F, Sayehmiri K. Survival rate of esophageal carcinoma in Iran - a systematic review and meta-analysis. Iran J Cancer Prevent. 2014;7:61–5. [PMC free article] [PubMed] [Google Scholar]
- 11.Mousavi SM, Somi MH. Gastric cancer in Iran 1966-2006. Asian Pac J Cancer Prev. 2009;10:407–12. [PubMed] [Google Scholar]
- 12.Delpisheh A, Veisani Y, Sayehmiri K, Rahimi E. Smoking and Histological Factors Influencing Long-term Survival of Gastric Carcinoma in Consecutive Patient Series. Middle East J Cancer. 2014;5:129–135. [Google Scholar]
- 13.Crew KD, Neugut AI. Epidemiology of gastric cancer. World J Gastroenterol. 2006;12:354–62. doi: 10.3748/wjg.v12.i3.354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Roshanaei G, Kazemnejad A, Sedighi S. Postoperative Survival Estimation of Gastric Cancer Patients in Cancer Institute of Tehran, Imam Khomeini Hospital and Its Relative Factors. Sci J Hamadan Univ Med Sci. 2010;17:13–8. [Google Scholar]
- 15.Bashash M, Yavari P, Hislop TG, Shah A, Sadjadi A, Babaei M, et al. Comparison of two diverse populations, British Columbia, Canada, and Ardabil, Iran, indicates several variables associated with gastric and esophageal cancer survival. J Gastrointest Cancer. 2011;42:40–45. doi: 10.1007/s12029-010-9228-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Soroush A. Surgical outcome in patients with gastrointestinal malignancies; a report from a large referral hospital, 2008-2010. Middle East J Dig Dis. 2013;5:201–208. [PMC free article] [PubMed] [Google Scholar]
- 17.Veisani Y, Delpisheh A, Sayehmiri K, Rahimi E. Demographic and histological predictors of survival in patients With gastric and esophageal carcinoma. Iran Red Crescent Med J. 2013;15:547–53. doi: 10.5812/ircmj.11847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Vagetti GC, Barbosa Filho VC, Moreira NB, Oliveira Vd, Mazzardo O, Campos Wd. Association between physical activity and quality of life in the elderly: a systematic review, 2000-2012. Rev Bras Psiquiatr. 2014;36:76–88. doi: 10.1590/1516-4446-2012-0895. [DOI] [PubMed] [Google Scholar]
- 19.Biglarian A, Hajizadeh E, Kazemnejad A, Zali M. Application of artificial neural network in predicting the survival rate of gastric cancer patients. Iran J Public Health. 2011;40:80–6. [PMC free article] [PubMed] [Google Scholar]
- 20.Meh1rabian A, Esna-Ashari F, Zham H, Hadizadeh M, Bohlooli M, Khayamzadeh M, et al. Gastric cancer prevalence, according to survival data in iran (national study-2007) Iran J Public Health. 2010;39:27–31. [PMC free article] [PubMed] [Google Scholar]
- 21.Zare A, Mahmoodi M, Mohammad K, Zeraati H, Hosseini M, Naieni KH. Survival analysis of patients with gastric cancer undergoing surgery at the iran cancer institute: a method based on multi-state models. Asian Pac J Cancer Prev. 2013;14:6 369–73. doi: 10.7314/apjcp.2013.14.11.6369. [DOI] [PubMed] [Google Scholar]
- 22.Baghestani AR, Hajizadeh E, Fatemi SR. Bayesian analysis for survival of patients with gastric cancer in Iran. Asian Pacific J Cancer Prev. 2009;10:823–26. [PubMed] [Google Scholar]
- 23.Moghimi-Dehkordi B, Safaee A, Zali MR. Survival rates and prognosis of gastric cancer using an actuarial life-table method. Asian Pac J Cancer Prev. 2008;9:317–21. [PubMed] [Google Scholar]
- 24.Samadi F, Babaei M, Yazdanbod A, Fallah M, Nouraie M, Nasrollahzadeh D, et al. Survival rate of gastric and esophageal cancers in Ardabil province, North-West of Iran. Arch Iran Med. 2007;10:32–7. [PubMed] [Google Scholar]
- 25.Noorkojuri H, Hajizadeh E, Baghestani A, Pourhoseingholi M. Application of smoothing methods for determining of the effecting factors on the survival rate of gastric cancer patients. Iran Red Crescent Med J. 2013;15:166–72. doi: 10.5812/ircmj.8649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yazdani-Charati J, Janbabaei G, Etemadinejad S, Sadeghi S, Haghighi F. Survival of patients with stomach adenocarcinoma in North of Iran. Gastroenterol Hepatol Bed Bench. 2014;7:211–17. [PMC free article] [PubMed] [Google Scholar]
- 27.Ghadimi M, Mahmoodi M, Mohammad K, Zeraati H, Rasouli M, Sheikhfathollahi M. Family history of the cancer on the survival of the patients with gastrointestinal cancer in northern Iran, using frailty models. BMC Gastroenterol. 2011;11 doi: 10.1186/1471-230X-11-104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Maroufizadeh S, Hajizadeh E, Baghestani AR, Fatemi SR. Multivariate analysis of prognostic factors in gastric cancer patients using additive hazards regression models. Asian Pac J Cancer Prev. 2011;12:1697–702. [PubMed] [Google Scholar]
- 29.Movahedi M, Afsharfard A, Moradi A, Nasermoaddeli A, Khoshnevis J, Fattahi F, et al. Survival rate of gastric cancer in Iran. J Res Med Sci. 2009;14:367–73. [PMC free article] [PubMed] [Google Scholar]
- 30.Atoof F, Mahmoudi M, Zeraati H, Rahimi Foroushani A, Moravveji AR. Survival analysis of gastric cancer patients refering to Emam-Khomeini hospital using Weibull cure model. Feyz. 2011;14:405–13. [Google Scholar]
- 31.Roshanaei Gh, Safari M, Baghestani AR, Sadighi S. Assessment of the Survival Risk Factors in Patients with Gastric Cancer in Cancer Institute of Imam Khomeni Hospital between 2003-2007. Zahedan University of Medical Sciences Journal. 2012;20:40–50. [Google Scholar]
- 32.Moghimi Dehkordi B, Rajaeefard A, Tabatabaee H, Zeighami B, Safaee A, Tabeie Z. Modeling survival analysis in gastric cancer patients using the proportional Hazards Model of Cox. Iranian Journal of Epidemiology. 2007;3:19–24. [Google Scholar]
- 33.Barfei F, Abbasi M, Khodabakhshi R, Gohari M. Survival analysis of patients with adenocarcinoma gastric cancer in Fayazkhsh hospital, Tehran. RJMS. 2014;21:1–9. [Google Scholar]
- 34.Kashani H, Mahmoodi M, Zeraati H, Rahimi A, Jalali A. Disease-free survival of postoperative gastric cancer patients: a competing risks analysis. Journal of School of Public Health and institute of Public Health Research. 2011;8:51–62. [Google Scholar]
- 35.Baeradeh N, Lotfi M, Fallahzadeh H, Kargar S, Salman Roghani H. Survival rate of patients with stomach cancer and its effective factors in Yazd Province. The Journal of Community Health Research. 2015;3:278–87. [Google Scholar]
- 36.Zeraati H, Mahmoudi M, Kazemnejad A, Mohammad K, Haddad P. Postoperative survival in patients with adenocarcinomatous pathology and lymph node metastasis: a method based on stochastic processes. Hakim. 2006;8:15–20. [Google Scholar]
- 37.Ghorbani Gholiabad S, Yazdani Cherati J, Jan Babaim G, Shabankhani B. Survival of patients with gastric cancer in Mazandaran Province, 2007-2012. J Mazandaran Univ Med Sci. 2013;23:43–50. [Google Scholar]
- 38.Roshanaei G, Kazemnejad A, Sadighi S. Survival estimating following recurrence in gastric cancer patients and its relative factors. Koomesh. 2011;12:223–28. [Google Scholar]
- 39.Larizadeh MH. Survival in nonmetastatic gastric cancer patients. J Kerman Univ Med Sci. 2013;20:470–80. [Google Scholar]
- 40.Gohari MR, Mokhtari P, Pourhoseingholi MN, Biglarian A. Artificial Neural Network in survival analysis of gastric cancer patients. Payesh. 2014;13:285–91. [Google Scholar]
- 41.Yang XQ, Yan L, Chen C, Hou JX, Li Y. Application of C12 multi-tumor marker protein chip in the diagnosis of gastrointestinal cancer: results of 329 surgical patients and suggestions for improvement. Hepatogastroenterology. 2009;56:1388–94. [PubMed] [Google Scholar]