Abstract
Background:
The purpose of this article was to clarify the optimal management concerning transjugular intrahepatic portosystemic shunts (TIPSs) and surgical shunting in treating portal hypertension.
Methods:
All databases, including CBM, CNKI, WFPD, Medline, EMBASE, PubMed and Cochrane up to February 2014, were searched for randomized controlled trials (RCTs) comparing TIPS with surgical shunting. Four RCTs, which were extracted by two independent investigators and were evaluated in postoperative complications, mortality, 2- and 5-year survival, hospital stay, operating time and hospitalization charges.
Results:
The morbidity in variceal rehemorrhage was significantly higher in TIPS than in surgical shunts (odds ratio [OR] = 7.45, 95% confidence interval[CI]: (3.93–14.15), P < 0.00001), the same outcomes were seen in shunt stenosis (OR = 20.01, 95% CI: (6.67–59.99), P < 0.000001) and in hepatic encephalopathy (OR = 2.50, 95% CI: (1.63–3.84), P < 0.0001). Significantly better 2-year survival (OR = 0.66; 95% CI: (0.44–0.98), P = 0.04) and 5-year survival (OR = 0.44; 95% CI: (0.30–0.66), P < 0.00001) were seen in patients undergoing surgical shunting compared with TIPS.
Conclusions:
Compared with TIPS, postoperative complications and survival after surgical shunting were superior for patients with portal hypertension. Application of surgical shunting was recommended for patients rather than TIPS.
Keywords: Complications, Hypertension, Portacaval Shunt, Portal, Portosystemic Shunt, Surgical, Survival Rate, Transjugular Intrahepatic
INTRODUCTION
Portal hypertension, always accompanies by cirrhosis, can lead to lots of complications including varices hemorrhage, ascites, hypersplenism and hepatic encephalopathy.[1] The risk of varices bleeding in patients with portal hypertension was approximately 30% over 2 years. Nowadays, the treatment for patients with varices hemorrhage mainly depends on medical treatment, endoscopic therapy, and surgical shunting procedures.[2] Transjugular intrahepatic portosystemic shunts (TIPSs) are currently widely used to prevent or control variceal rebleeding for it could serve as a bridge to hepatic transplantation or fit for patients who are in need of portal decompression. TIPS was usually regarded as a first-line therapy and cost-effective solution to portal hypertension concomitant with variceal hemorrhage in recent years.[3] Therefore, TIPS has generally replaced surgical shunts, which require the involvement of surgeons and general anesthesia as the first treatment for patients with portal hypertension.[4]
Besides advantages of cost-effective and less invasive, TIPS, however, was always accompanied by complications mainly including stenosis/occlusion, recurrent varices hemorrhage, and hepatic encephalopathy.[5] Its effectiveness beyond surgical shunting in bridging to hepatic transplantation, to some extent, was arguable. In addition, with issues of postoperative shunt stenosis, thrombosis and migration, almost half of the patients undergoing TIPS experienced shunt failure within 1 year of TIPS placement.
However, surgical shunting that mostly refers to distal splenorenal shunts (DSRSs), portacaval shunts (PCSs) or H-graft PCSs (HGPCSs) has generally disappeared for the widespread application of TIPS.[6] Recent article reported that patients receiving DSRS would have significantly lower rebleeding and encephalopathy rates than TIPS in the management of refractory variceal bleeding.[7] Also, PCS was reported significantly superior to endoscopic therapy in a longer survival rate, less morbidity and lower direct and indirect costs.[8] With more randomized controlled trials (RCTs) comparing TIPS with surgical shunting undertaken, the optimal management for patients with portal hypertension can be tested.
There was still no all-round systemic evaluation comparing TIPS with surgical shunts for patients with portal hypertension. Specifically, we focused on comparing postoperative complications (including recurrent variceal hemorrhage, shunt stenosis, and encephalopathy), mortality and survival rate after surgery in patients undergoing TIPS versus surgical shunting. Therefore, we performed a meta-analysis of all RCTs concerning TIPS and surgical shunting (including DSRS, PCS, and HGPCS) to evaluate the optimal management for patients with portal hypertension. The aims of this study were to give more information concerning TIPS and surgical shunting with our proposed approach in evaluating the morbidity, mortality, and long-term survival.
METHODS
Search strategy and selection of papers
All databases including CBM, CNKI, WFPD, PubMed, Medline, EMBASE and Cochrane were searched using the MeSH terms: “Hypertension, Portal/complications,” “Liver Cirrhosis/complications,” “Portosystemic Shunt, Transjugular Intrahepatic/mortality,” “Portosystemic Shunt, Surgical,” “Esophageal and Gastric Varices/surgery,” “Hypertension, Portal/surgery” independently or in combination for clinical trials comparing TIPS with surgical shunts. All literatures were screened to identify all suitable published RCTs for eligibility until February 2014. All eligible RCTs were screened for their methods, characteristics and risk of bias strictly.
In this meta-analysis, two different kinds of groups were generated from the included papers that met the criterion: The TIPS group and the surgical shunting group. The surgical shunting group referred to traditional portosystemic shunts that contained DSRS, HGPCS, and PCS. In sub-group analysis, HGPCS and PCS could be recognized as one group for their similar modus operandi and decompression principle. In our research, 246 patients underwent TIPS and 247 patients underwent surgical shunts.
Reviewing and data extraction
All included RCTs were required to contain a direct comparison between portosystemic shunts (including DSRS, HGPCS, and PCS) and TIPS in a controlled manner. Each trial was required to include postoperative complications, mortality and long-term survival rate in detail.
Primary outcomes to be assessed were mortality, 2- and 5-year survival and postoperative complications including recurrent variceal hemorrhage, shunt stenosis, and hepatic encephalopathy. Secondary outcomes to be assessed were length of hospital stay, operating time and hospitalization charges. Trials not reporting any of these parameters were excluded from the review.
Quality of studies
Each of these papers was assessed using a standardized evaluation form by two investigators (Author #1, Author #5) independently for extraction in this meta-analysis. When consensus couldn’t be reached, discussion and joint collection of the paper could resolve. Otherwise, a third reviewer (Author #2) would take part in the discussion and determine the definite inclusion of papers as a referee. General information collected from abstracts, included the authors, publication year, characteristics of patients and outcomes.
All papers were assessed for the risk of bias by two investigators (Author #1, Author #5) on the following areas: Random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective reporting, other sources of bias. The risk of bias was assessed as suggested in the Cochrane Handbook.[9]
Outcomes and definition
Outcomes, including morbidity, mortality, 2-year survival rate, 5-year survival rate, hospital stay, operating time and hospitalization charge, were extracted from included papers.
The major endpoints of this study were postoperative complications and survival. Survival was defined as the time from the shunt procedure to the time of death from any cause. Mortality in this meta-analysis was defined as postoperative death before discharge or within 30 postoperative days. Survival was noted at 2- and 5-year after surgical procedures.
Transjugular intrahepatic portosystemic shunt placement referred to the technical procedure via interventional therapy that stents were placed between the portal vein and hepatic vein until a 5–10 mmHg gradient was achieved. The technique of HGPCS was described that small-diameter (8–10 mm) externally ring-reinforced polytetrafluoroethylene graft was used with beveled ends oriented perpendicular (90°) to each other to accommodate for the orientation of the portal vein to the inferior vena cava. PCS was defined as direct PCS, usually side to side, rarely end to side. DSRS was defined as distal splenic vein and renal vein shunted from end to side.
Data analysis
The verified data were analyzed using Review Manager (Version 4.2, Oxford, England, The Cochrane Collaboration, 2003). The odds ratio (OR), mean difference (MD) and their corresponding 95% confidence intervals (95% CIs) were calculated for dichotomous or continuous outcome data respectively. Statistical heterogeneity was assessed with the I2 test and Q-test to justify the accuracy of the fixed or random effects model. A significant effect was assumed if the 95% CI did not include the value 1.0 for OR or 0 for MD. A fixed-effect model was used in case of no relevant statistical heterogeneity when I2 was <50% and P > 0.1. If the heterogeneity was high (I2 > 50% and P < 0.1), a sub-group analysis could be used to decrease the risk of bias. A fixed-effect model also could be used in Sub-group analysis for decreased heterogeneity. A random-effect model was used when I2 > 50% and P < 0.1.
RESULTS
Description of studies
Searching in Medline, EMBASE, PubMed and Cochrane data of clinical trials was 376 Trials. After checking for abstracts according to our predefined inclusion and exclusion criterion, 76 references remained for further evaluation. Eventually, four RCTs that documented adequate comparisons between TIPS and surgical shunting for portal hypertension were determined for this meta-analysis.[10,11,12,13] No additional eligible studies were found after carefully examined the reference lists of all included papers [Figure 1].
Figure 1.
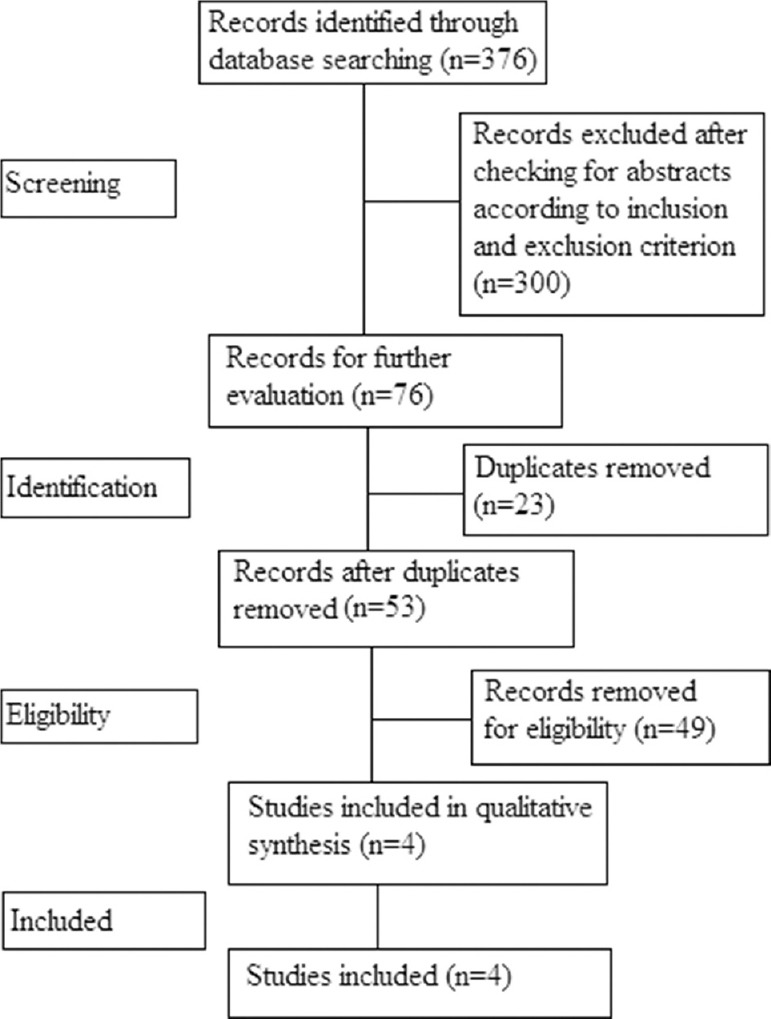
Flow chart showing study selection process.
The characteristics and risk of bias for included four studies that compared TIPS and surgical shunting for portal hypertension are performed in Table 1 as suggested in the Cochrane Handbook. All included RCTs were published from 2000 to 2012. Three included papers reported patients from America while the remaining one from India [Table 1].
Table 1.
Characteristics of included RCTs and risk of the bias summary
| Author | Country | Study type | Publish year | Comparison | Random sequence generation | Allocation concealment | Blinding of participants and personnel | Blinding of outcome assessment | Incomplete outcome data | Selective reporting | Other bias |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Khaitiyar et al. | India | RCT | 2000 | TIPS versus DSRS | Low risk | High risk | Unclear | Low risk | Low risk | Low risk | Unclear |
| Henderson et al. | America | RCT | 2006 | TIPS versus DSRS | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Unclear |
| Rosemurgy et al. | America | RCT | 2012 | TIPS versus HGPCS | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Unclear |
| Orloff et al. | America | RCT | 2012 | TIPS versus PCS | Low risk | Low risk | Low risk | Low risk | Unclear | Low risk | Unclear |
TIPS: Transjugular intrahepatic portosystemic shunting; DSRS: Distal splenorenal shunts; PCS: Portacaval shunts; HGPCS: H-graft portacaval shunt; RCT: Randomized clinical trial.
From the four included trials, 493 patients of Child-pugh A to C were included in our analysis. Long-term results and postoperative complications mainly including recurrent variceal hemorrhage, shunt stenosis, and encephalopathy are summarized in Table 2.
Table 2.
Results and clinical characteristics comparing TIPS with surgical shunting
| Author | Comparison | Number of patients | Child-pugh(%) | Postoperative morbidity (%) | Mortality (%) | 1-year survival (%) | 2-year survival (%) | 5-year survival (%) | Operating time (h) (range) | Hospital stay (d)(SD) | Hospitalization charges ($) | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| A | B | C | Variceal rehemorrhage | Shunt stenosis | Hepatic encephalopathy | ||||||||||
| Khaitiyar et al. | TIPS versus DSRS | 35 versus 32 | 34 versus 31 | 66 versus 69 | 0 versus 0 | 26 versus 6 | 69 versus 6 | 43 versus 19 | 6 versus 6 | 83 versus 81 | 80 versus 81 | NA | NA | NA | NA |
| Henderson et al. | TIPS versus DSRS | 67 versus 73 | 58 versus 56 | 42 versus 44 | 0 versus 0 | 11 versus 6 | 82 versus 11 | 51 versus 49 | 1 versus 7 | 93 versus 88 | 88 versus 81 | 61 versus 62 | NA | 3 (4) versus 11 (11) | 21607 versus 28734 |
| Rosemurgy et al. | TIPS versus HGPCS | 66 versus 66 | 18 versus 14 | 38 versus 36 | 44 versus 50 | 30 versus 8 | 48 versus 11 | NA | 15 versus 20 | 64 versus 74 | 53 versus 68 | 31 versus 47 | NA | NA | NA |
| Orloff et al. | TIPS versus PCS | 78 versus 76 | 21 versus 20 | 50 versus 49 | 29 versus 32 | 41 versus 0 | 84 versus - | 61 versus 21 | 22 versus 23 | 55 versus 75 | 49 versus 68 | 20 versus 61 | 3 (1-25) versus 4 (3-11) | NA | NA |
TIPS: Transjugular Intrahepatic Portasystemic shunting; DSRS: Distal splenorenal shunts; PCS: Portacaval shunts; HGPCS: H-graft portacaval shunt; SD: Standard deviation; NA: Not applicable.
Postoperative morbidity
The most common postoperative complications were variceal rehemorrhage, shunt stenosis, and encephalopathy. Variceal rebleeding occurred in 27.6% of patients in TIPS group and in 4.5% of patients in surgical shunting group, shunt stenosis occurred in 66.1% of patients in TIPS group and in 9.9% of patients in surgical shunting group, hepatic encephalopathy occurred in 53.9% of patients in TIPS group and in 32.0% of patients in surgical shunting group.
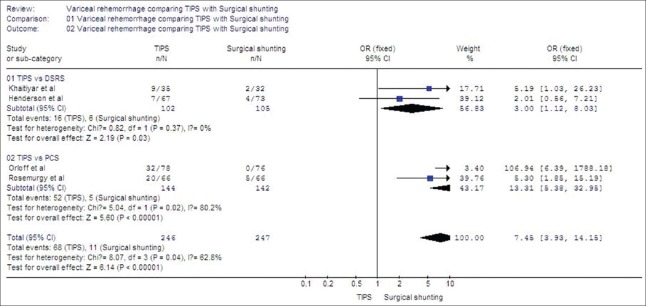
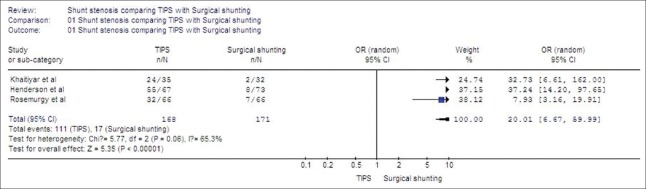
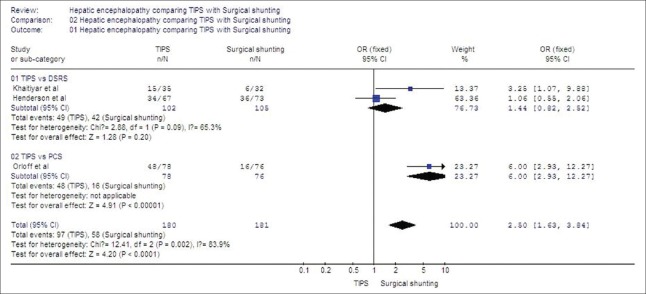
From our meta-analysis, morbidity in variceal rehemorrhage was significantly higher in TIPS than in surgical shunts (OR = 7.45, 95% CI: (3.93–14.15), P < 0.00001) [Figure 2]. Patients occurring postoperative shunt stenosis also was significantly higher in TIPS than in surgical shunts (OR = 20.01, 95% CI: (6.67–59.99), P < 0.000001) [Figure 3]. Besides, morbidity in hepatic encephalopathy was also significantly higher in TIPS than in surgical shunts (OR = 2.50, 95% CI: (1.63–3.84), P < 0.0001), especially when compared with PCS in sub-group analysis (OR = 6.00, 95% CI: (2.93–12.27), P < 0.00001) [Figure 4]. A sub-group analysis was conducted in the comparison of variceal rehemorrhage (χ2 = 8.07, P = 0.04, I2 = 62.8%) and hepatic encephalopathy (χ2 = 12.41, P = 0.002, I2 = 83.9%) to decrease high heterogeneity.
Figure 2.
Variceal rehemorrhage comparing transjugular intrahepatic portosystemic shunt with surgical shunting.
Figure 3.
Shunt stenosis comparing transjugular intrahepatic portosystemic shunt with surgical shunting.
Figure 4.
Hepatic encephalopathy comparing transjugular intrahepatic portosystemic shunt with surgical shunting.
Mortality
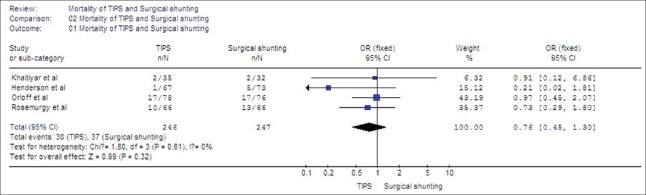
Mortality in this meta-analysis referred to the death rate at 30 days. In our research, all 4 RCTs reported mortality for evaluation.
Mortality was equivalent among patients undergoing TIPS or surgical shunts (OR = 0.76; 95% CI: (0.45–1.30), P = 0.32) [Figure 5]. No significant heterogeneity was found from the trials (χ2 = 1.80, P = 0.61, I2 = 0%).
Figure 5.
Mortality of transjugular intrahepatic portosystemic shunt and surgical shunting.
Long-term result
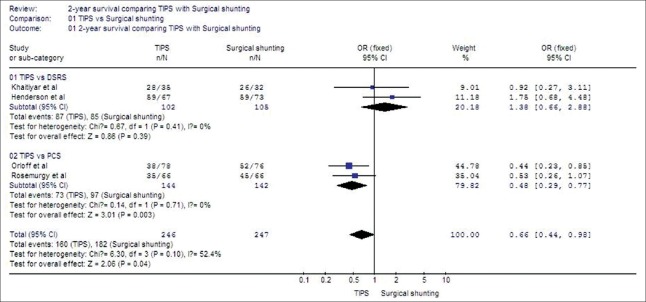
Survival at 2 years in sub-group analysis was also significantly higher among patients undergoing PCS than patients undergoing TIPS (OR = 0.48; 95% CI: (0.29–0.77), P = 0.003), but in sub-group analysis survival at 2 years was equivalent among patients undergoing TIPS and DSRS (OR = 1.38, 95% CI: (0.66–2.88), P = 0.39). Significant heterogeneity was found from the trials, and a sub-group analysis was conducted (χ2 = 6.30, P = 0.10, I2 = 52.4%) [Figure 6].
Figure 6.
Two-year survival comparing transjugular intrahepatic portosystemic shunt with surgical shunting.
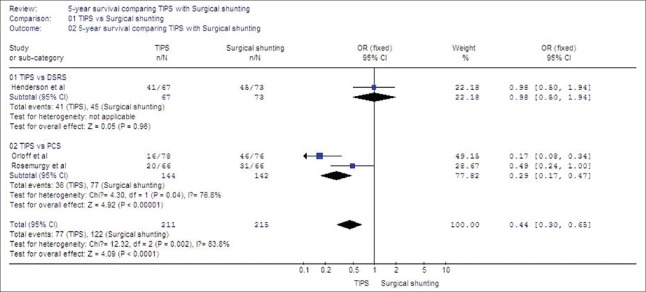
Survival at 5 years was greater for patients undergoing surgical shunting than patients undergoing TIPS (OR = 0.44; 95% CI: (0.30–0.65), P < 0.0001), and survival in sub-group analysis was also higher among patients undergoing PCS than patients undergoing TIPS (OR = 0.29; 95% CI: (0.17–0.47), P < 0.00001). Significant heterogeneity was found from the trials, and a sub-group analysis was conducted (χ2 = 12.32, P = 0.002, I2 = 83.8%) [Figure 7].
Figure 7.
Five-year survival comparing transjugular intrahepatic portosystemic shunt with surgical shunting.
Length of hospital stay
In the included RCTs, only 1 paper[11] reported the length of hospital stay in the form of the mean and standard deviation (SD) comparing TIPS with DSRS (3.1 [4.3 day] vs. 10.5 [11.3 day]), which suggested TIPS treatment had a shorter hospital stay [Table 2].
Hospitalization charges
In this research, only 1 trial[11] reported hospitalization charges comparing TIPS with DSRS (21,607 vs. 28,734). However, cost analysis data of this article showed no overall significant difference in the cost of managing patients with either procedure [Table 2].
Operating time
In our meta-analysis, only 1 paper[13] reported operating time in the form of the mean and the range comparing TIPS with PCS (3 [1.25–25] h vs. 3.8 [2.6–11] h) [Table 2].
DISCUSSION
Nowadays, TIPS placement has become the preferred first-line management for patients with portal hypertension.[14] The present study is the first meta-analysis of studies comparing TIPS with surgical shunting in patients with portal hypertension focused on complications and survival. This meta-analysis included four RCTs, the populations in three studies were from America and in the remaining study were from India.
Currently, there were few papers concerning TIPS versus surgical shunting in outcomes and survival rates, so the difference between TIPS and surgical shunting was unclear. In clinical practice, there was the lack of a definite guidance to determine the optimal treatment for patients with portal hypertension. This meta-analysis would help make a better decision in clinical work or develop a guideline.
Transjugular intrahepatic portosystemic shunt was generally considered as a first-line therapy in the definitive treatment of portal hypertension concomitant with variceal bleeding; however, trials comparing TIPS with surgical shunts were few and drew little attention, so some disadvantages of TIPS were ignored.[15] In this meta-analysis, we conducted a comparison between TIPS and surgical shunting in patients with cirrhosis, portal hypertension and bleeding varices from four trials, in order to get an all-around evaluation and give more information about how to decide the optimal management for patients with portal hypertension. As the measurement of patient's survival and postoperative complications was representative, we could conclude that long-term survival and morbidity after shunting were promoted by surgical shunting relative to TIPS. But surgical shunts in this meta-analysis included DSRS and HGPCS, and the relations between the two types of surgeries and TIPS were unclear. As a result, the outcomes of this meta-analysis were proved to be helpful in answering questions that arose when comparing TIPS with surgical shunting. Although each included trial didn’t individually reveal the comparison between surgical shunting and TIPS in all respects, the outcomes of this meta-analysis proved the superiority of surgical shunting over TIPS.
As a matter of fact, the outcomes were obvious that the results supported a role for surgical shunts in patients with portal hypertension over TIPS. In terms of morbidity, mortality, 2- and 5-year survival, surgical shunting was superior to TIPS as was the likelihood of shunt function. In the included papers, three of four trials found significantly higher postoperative bleeding, stenosis and encephalopathy rates after TIPS. Postoperative complications, including recurrent variceal hemorrhage, hepatic encephalopathy, shunt stenosis, severe infection and so on, were all deadly sign for patients after surgery that could lead to a series of disorders in metabolic systems.[16] Complications of TIPS placement proved to be critical when hepatic encephalopathy occurred, a limited number of procedures should be typically considered for the management.[17] The postoperative rehemorrhage rate of nearly 11% after TIPS was the lowest reported in included trials while the rebleeding rate was reaching 5.5% after DSRS in two included papers and 7.5% after HGPCS in included paper. Shunt stenosis could also cause recurrent variceal hemorrhage and result in a series of severe syndromes. The comparison of shunt stenosis between TIPS and surgical shunting was obvious as the rate was reaching almost 82% after TIPS and no more than 11% after surgical shunts.
However, TIPS should not be abandoned entirely. TIPS for patients with portal hypertension was widely spread. TIPS could effectively lower portal hypertension due to cirrhosis. According to past experience, it is significantly effective for hemorrhage of the digestive tract due to rupture of esophageal and fundic veins and for ascites and hydrothorax caused by portal hypertension.[18] Although shunt dysfunction has confused surgeons for the incidence of TIPS stenosis and occlusion, trials of successful treatment with TIPS of recurrent massive rectal bleeding due to portal hypertension has reinforced the confidence of surgeons in TIPS.[19] Recent article also reported bleeding from focal varices in the stoma could be treated with TIPS that spread the use of TIPS in other situations.[20] In addition, a 25% incidence of hernia complications following TIPS creation in patients being treated for refractory ascites was higher than expected.[21]
The most common indications for TIPS placement were refractory ascites and variceal hemorrhage, also in properly selected candidate, TIPS placement could serve as a bridge to liver transplantation for TIPS was initially less expensive and led to an easier transplantation process.[22] TIPS also performed as an effective way in preventing variceal rebleeding and may be more cost effective. In other words, it was equal to surgical procedures in preventing variceal rebleeding in patients who are medical failures.[23] Besides, when aimed at treating the Budd–Chiari syndrome, a therapeutic strategy has been proposed that angioplasty for short length venous stenosis, TIPS, and ultimately liver transplantation could be done in proper order.[24] Although TIPS revealed superiority in some parts of treatment in patients with portal hypertension, the results of this meta-analysis performed significant deficiency in morbidity and survival.
To some extent, people preferred shunting subjectively only when nonshunting modalities to control variceal bleeding failed or when these modalities were considered nonapplicable, thus strong points of this method were difficult to appear. This meta-analysis, which contained a number of patients in these trials, was able to give great credibility to the results and conclusions. PCS permanently stopped variceal bleeding and gained a longer time survival than TIPS, but nowadays the widespread practice of using PCS only served as a management for failure of endoscopic therapy or TIPS in unselected patients with cirrhosis.[25] However, the 2-year survival was higher in PCS than in TIPS (OR = 0.48; 95% CI: (0.29–0.77), P = 0.003), and 5-year survival after PCS was longer than that after TIPS (OR = 0.29; 95% CI: (0.17–0.47), P < 0.00001).
No matter what the surgical shunts include, the consecutive experiences of shunt operation are important for the improvement of surgical skills, both of the individual surgeon and the team.[26]
Since 1988, more and more patients have received HGPCS treatment for its effectiveness in reducing portal hypertension, and the outcome was favorable that the actual survival was better than predicted before.[27] The actual 5- and 10-year survival after HGPCS by Child Class was: (a) 67% and 33%, (b) 49% and 16%, (c) 29% and 7%.[28,29] HGPCS has been identified as an effective procedure for the treatment of variceal bleeding, as well as for the prevention of re-bleeding in patients, with a low rate of complications. Some papers indicated that PCS with a small diameter interposition H-graft was an effective procedure for the treatment of variceal bleeding or as an elective or emergency procedure with a low rate of complications.[30] Papers published recently also indicated that the actual survival after HGPCS was better than other surgical procedures.[31,32]
Central splenorenal shunt showed more negatively effect on hemodynamics of left kidney and symptoms of renal venous hypertension obviously due to shunting the large amounts of blood from a system of high pressure to a low.[33] In contrast, DSRS or 8 mm H-graft shunt showed similar efficacy to TIPS, and it also served as the proper choice in preventing recurrent variceal bleeding.[34] DSRS also revealed an effective and reliable procedure for children with portal hypertension and was still useful for selected pediatric patients.[35] DSRS was suggested to be useful for the management of esophagogastric varices in patients with idiopathic portal hypertension.[36] Although a number of surgical procedures have been developed to manage esophageal varices, DSRS with splenopancreatic disconnection plus gastric transection was considered as an adequate treatment for patients with esophagogastric varices.[37]
There still existed some limitations in this meta-analysis. The included studies regarding surgical shunting versus TIPS were rare, and surgical shunts in these papers included several kinds of operation methods. This could result in instability of the comparison between TIPS and surgical shunting as the different surgical types of shunts may lead to a slight bias of outcome. Although sub-group analysis was taken, the bias of the result still existed. The only way to solve the problem was that more clinical trials comparing surgical shunting with TIPS should be undertaken. Data such as cost and hospital stay from the included studies were rare, so further evidence concerning hospital charges and hospital stay was needed to fulfill this meta-analysis. Although TIPS was performed most often with the use of the covered stent currently, there were no studies comparing covered stent with surgical shunting scientifically. The outcomes and survival rates between covered and uncovered TIPS varied, Clark et al.[38] concluded that there were no differences in rates of encephalopathy or survival between covered and uncovered TIPS, but Bureau et al.[39] revealed Polytetrafluoroethylene-Coated Stents were superior to uncovered stents in morbidity, so more RCTs concerning covered stents versus surgical shunting should be conducted to provide more evidence. Limited RCTs concerning covered TIPS was the restriction in this meta-analysis, so more clinical trials should be undertaken. Finally, the risk of bias and heterogeneity of included RCTs were still existed according to the Cochrane Handbook. Allocation concealment was missed in some included RCTs and high risk of bias was existed in some parts of our bias summary, these could lead to the bias of outcomes and influence the validity of result to some extent, so Cochrane risk of bias should be examined exactly to reduce bias.
In summary, surgical shunting would be recommended because of increased survival rate and fewer postoperative complications when compared with TIPS. As the patients with portal hypertension concomitant with variceal hemorrhage always remained in a large number and needed necessary treatment, they should be given more surgical advices for the superiority concerning complications and survival.
ACKNOWLEDGMENTS
We would like to acknowledge the support of the Department of No. 1 Surgery, The First Hospital Affiliated to Anhui Chinese Medical University, China.
Footnotes
Edited by: Yi Cui
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.de Franchis R, Baveno V Faculty. Revising consensus in portal hypertension: Report of the Baveno V consensus workshop on methodology of diagnosis and therapy in portal hypertension. J Hepatol. 2010;53:762–8. doi: 10.1016/j.jhep.2010.06.004. [DOI] [PubMed] [Google Scholar]
- 2.Garcia-Tsao G, Bosch J. Management of varices and variceal hemorrhage in cirrhosis. N Engl J Med. 2010;362:823–32. doi: 10.1056/NEJMra0901512. [DOI] [PubMed] [Google Scholar]
- 3.Rosemurgy AS, Molloy DL, Thometz DP, Villadolid DV, Cowgill SM, Zervos EE. TIPS in Florida: Is its application a result of evidence-based medicine? J Am Coll Surg. 2007;204:794–801. doi: 10.1016/j.jamcollsurg.2007.01.014. [DOI] [PubMed] [Google Scholar]
- 4.Bureau C, Pagan JC, Layrargues GP, Metivier S, Bellot P, Perreault P, et al. Patency of stents covered with polytetrafluoroethylene in patients treated by transjugular intrahepatic portosystemic shunts: Long-term results of a randomized multicentre study. Liver Int. 2007;27:742–7. doi: 10.1111/j.1478-3231.2007.01522.x. [DOI] [PubMed] [Google Scholar]
- 5.Boyer TD, Haskal ZJ American Association for the Study of Liver Diseases. The Role of Transjugular Intrahepatic Portosystemic Shunt (TIPS) in the Management of Portal Hypertension: Update 2009. Hepatology. 2010;51:306. doi: 10.1002/hep.23383. [DOI] [PubMed] [Google Scholar]
- 6.Henderson JM, Nagle A, Curtas S, Geisinger M, Barnes D. Surgical shunts and TIPS for variceal decompression in the 1990s. Surgery. 2000;128:540–7. doi: 10.1067/msy.2000.108209. [DOI] [PubMed] [Google Scholar]
- 7.Jenkins RL, Gedaly R, Pomposelli JJ, Pomfret EA, Gordon F, Lewis WD. Distal splenorenal shunt: Role, indications, and utility in the era of liver transplantation. Arch Surg. 1999;134:416–20. doi: 10.1001/archsurg.134.4.416. [DOI] [PubMed] [Google Scholar]
- 8.Pierce DS, Sperry J, Nirula R. Cost-effective analysis of transjugular intrahepatic portosystemic shunt versus surgical portacaval shunt for variceal bleeding in early cirrhosis. Am Surg. 2011;77:169–73. [PubMed] [Google Scholar]
- 9.Higgins JP, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0. The Cochrane Collaboration. 2011. [Last updated on 2011 Mar]. Available from: http://www.cochrane-handbook.org .
- 10.Khaitiyar JS, Luthra SK, Prasad N, Ratnakar N, Daruwala DK. Transjugular intrahepatic portosystemic shunt versus distal splenorenal shunt – A comparative study. Hepatogastroenterology. 2000;47:492–7. [PubMed] [Google Scholar]
- 11.Henderson JM, Boyer TD, Kutner MH, Galloway JR, Rikkers LF, Jeffers LJ, et al. Distal splenorenal shunt versus transjugular intrahepatic portal systematic shunt for variceal bleeding: A randomized trial. Gastroenterology. 2006;130:1643–51. doi: 10.1053/j.gastro.2006.02.008. [DOI] [PubMed] [Google Scholar]
- 12.Rosemurgy AS, Frohman HA, Teta AF, Luberice K, Ross SB. Prosthetic H-graft portacaval shunts vs transjugular intrahepatic portasystemic stent shunts: 18-year follow-up of a randomized trial. J Am Coll Surg. 2012;214:445–53. doi: 10.1016/j.jamcollsurg.2011.12.042. [DOI] [PubMed] [Google Scholar]
- 13.Orloff MJ, Vaida F, Haynes KS, Hye RJ, Isenberg JI, Jinich-Brook H. Randomized controlled trial of emergency transjugular intrahepatic portosystemic shunt versus emergency portacaval shunt treatment of acute bleeding esophageal varices in cirrhosis. J Gastrointest Surg. 2012;16:2094–111. doi: 10.1007/s11605-012-2003-6. [DOI] [PubMed] [Google Scholar]
- 14.Helton WS, Maves R, Wicks K, Johansen K. Transjugular intrahepatic portasystemic shunt vs surgical shunt in good-risk cirrhotic patients: A case-control comparison. Arch Surg. 2001;136:17–20. doi: 10.1001/archsurg.136.1.17. [DOI] [PubMed] [Google Scholar]
- 15.Clark W, Hernandez J, McKeon B, Villadolid D, Al-Saadi S, Mullinax J, et al. Surgical shunting versus transjugular intrahepatic portasystemic shunting for bleeding varices resulting from portal hypertension and cirrhosis: A meta-analysis. Am Surg. 2010;76:857–64. [PubMed] [Google Scholar]
- 16.LaBerge JM. Transjugular intrahepatic portosystemic shunt - Role in treating intractable variceal bleeding, ascites, and hepatic hydrothorax. Clin Liver Dis. 2006;10:583–98. doi: 10.1016/j.cld.2006.08.004. ix. [DOI] [PubMed] [Google Scholar]
- 17.Ahuja NK, Ally WA, Caldwell SH. Direct acting inhibitors of ammoniagenesis: A role in post-TIPS encephalopathy? Ann Hepatol. 2014;13:179–86. [PubMed] [Google Scholar]
- 18.Qin JP, Jiang MD, Tang W, Wu XL, Yao X, Zeng WZ, et al. Clinical effects and complications of TIPS for portal hypertension due to cirrhosis: A single center. World J Gastroenterol. 2013;19:8085–92. doi: 10.3748/wjg.v19.i44.8085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yesilkaya Y, Çil B, Peynircioglu B, Simsek H. Successful treatment with transjugular intrahepatic portosystemic shunt (TIPS) of recurrent massive rectal bleeding due to portal hypertension: Case report. Turk J Gastroenterol. 2013;24:363–6. doi: 10.4318/tjg.2013.0612. [DOI] [PubMed] [Google Scholar]
- 20.Saad WE, Saad NE, Koizumi J. Stomal varices: Management with decompression tips and transvenous obliteration or sclerosis. Tech Vasc Interv Radiol. 2013;16:176–84. doi: 10.1053/j.tvir.2013.02.005. [DOI] [PubMed] [Google Scholar]
- 21.Smith MT, Rase B, Woods A, Trotter J, Gipson M, Kondo K, et al. Risk of hernia incarceration following transjugular intrahepatic portosystemic shunt placement. J Vasc Interv Radiol. 2014;25:58–62. doi: 10.1016/j.jvir.2013.09.003. [DOI] [PubMed] [Google Scholar]
- 22.Bonnel AR, Bunchorntavakul C, Rajender Reddy K. Transjugular intrahepatic portosystemic shunts in liver transplant recipients. Liver Transpl. 2014;20:130–9. doi: 10.1002/lt.23775. [DOI] [PubMed] [Google Scholar]
- 23.Boyer TD, Henderson JM, Heerey AM, Arrigain S, Konig V, Connor J, et al. Cost of preventing variceal rebleeding with transjugular intrahepatic portal systemic shunt and distal splenorenal shunt. J Hepatol. 2008;48:407–14. doi: 10.1016/j.jhep.2007.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hefaiedh R, Cheikh M, Marsaoui L, Ennaifer R, Romdhane H, Ben Nejma H, et al. The Budd-Chiari syndrome. Tunis Med. 2013;91:376–81. [PubMed] [Google Scholar]
- 25.Orloff MJ. Fifty-three years’ experience with randomized clinical trials of emergency portacaval shunt for bleeding esophageal varices in Cirrhosis: 1958-2011. JAMA Surg. 2014;149:155–69. doi: 10.1001/jamasurg.2013.4045. [DOI] [PubMed] [Google Scholar]
- 26.Sato Y, Oya H, Yamamoto S, Kobayashi T, Nakatsuka H, Watanabe T, et al. A 10-year experience of shunt surgery for esophago-gastric varices in a single center in Japan. Hepatogastroenterology. 2011;58:444–52. [PubMed] [Google Scholar]
- 27.Rosemurgy AS, 2nd, Bloomston M, Zervos EE, Goode SE, Pencev D, Zweibel B, et al. Transjugular intrahepatic portosystemic shunt versus H-graft portacaval shunt in the management of bleeding varices: A cost-benefit analysis. Surgery. 1997;122:794–9. doi: 10.1016/s0039-6060(97)90089-1. [DOI] [PubMed] [Google Scholar]
- 28.Rosemurgy AS, Serafini FM, Zweibel BR, Black TJ, Kudryk BT, Nord HJ, et al. Transjugular intrahepatic portosystemic shunt vs. small-diameter prosthetic H-graft portacaval shunt: Extended follow-up of an expanded randomized prospective trial. J Gastrointest Surg. 2000;4:589–97. doi: 10.1016/s1091-255x(00)80107-9. [DOI] [PubMed] [Google Scholar]
- 29.Rosemurgy AS, Zervos EE, Bloomston M, Durkin AJ, Clark WC, Goff S. Post-shunt resource consumption favors small-diameter prosthetic H-graft portacaval shunt over TIPS for patients with poor hepatic reserve. Ann Surg. 2003;237:820–5. doi: 10.1097/01.SLA.0000072102.38993.05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sriussadaporn S, Pak-art R, Sriussadaporn S. Small-diameter H-graft portacaval shunt for variceal hemorrhage: Experience at King Chulalongkorn Memorial Hospital. J Med Assoc Thai. 2004;87:427–31. [PubMed] [Google Scholar]
- 31.Cowgill SM, Thometz D, Clark W, Villadolid D, Carey E, Pinkas D, et al. Conventional predictors of survival poorly predict and significantly underpredict survival after H-graft portacaval shunts. J Gastrointest Surg. 2007;11:89–94. doi: 10.1007/s11605-006-0041-7. [DOI] [PubMed] [Google Scholar]
- 32.Costa G, Cruz RJ, Jr, Abu-Elmagd KM. Surgical shunt versus TIPS for treatment of variceal hemorrhage in the current era of liver and multivisceral transplantation. Surg Clin North Am. 2010;90:891–905. doi: 10.1016/j.suc.2010.04.015. [DOI] [PubMed] [Google Scholar]
- 33.Aliev MM, Yuldashev RZ, Adilova GS, Yusupaileva GA. Renal blood flow before and after portosystemic shunt in children with portal hypertension. Pediatr Surg Int. 2014;30:295–9. doi: 10.1007/s00383-014-3463-4. [DOI] [PubMed] [Google Scholar]
- 34.Berzigotti A, García-Pagán JC. Prevention of recurrent variceal bleeding. Dig Liver Dis. 2008;40:337–42. doi: 10.1016/j.dld.2007.12.003. [DOI] [PubMed] [Google Scholar]
- 35.Moon SB, Jung SE, Ha JW, Park KW, Seo JK, Kim WK. The usefulness of distal splenorenal shunt in children with portal hypertension for the treatment of severe thrombocytopenia and leukopenia. World J Surg. 2008;32:483–7. doi: 10.1007/s00268-007-9356-0. [DOI] [PubMed] [Google Scholar]
- 36.Yoshida H, Mamada Y, Taniai N, Mineta S, Kawano Y, Mizuguchi Y, et al. Shunting and nonshunting procedures for the treatment of esophageal varices in patients with idiopathic portal hypertension. Hepatogastroenterology. 2010;57:1139–44. [PubMed] [Google Scholar]
- 37.Yoshida H, Mamada Y, Taniai N, Tajiri T. New trends in surgical treatment for portal hypertension. Hepatol Res. 2009;39:1044–51. doi: 10.1111/j.1872-034X.2009.00549.x. [DOI] [PubMed] [Google Scholar]
- 38.Clark W, Golkar F, Luberice K, Toomey P, Paul H, Marcadis A, et al. Uncovering the truth about covered stents: Is there a difference between covered versus uncovered stents with transjugular intrahepatic portosystemic shunts? Am J Surg. 2011;202:561–4. doi: 10.1016/j.amjsurg.2011.06.021. [DOI] [PubMed] [Google Scholar]
- 39.Bureau C, Garcia-Pagan JC, Otal P, Pomier-Layrargues G, Chabbert V, Cortez C, et al. Improved clinical outcome using polytetrafluoroethylene-coated stents for TIPS: Results of a randomized study. Gastroenterology. 2004;126:469–75. doi: 10.1053/j.gastro.2003.11.016. [DOI] [PubMed] [Google Scholar]