Abstract
Background
The recent focus on patient centered outcomes highlights the need to better describe recovery trajectories after injury. The purpose of this study was to characterize recovery trajectory subtypes that exist after non-neurologic injury.
Materials and Methods
A prospective, observational cohort of 500 adults with an injury severity score > 10 but without traumatic brain or spinal cord injury from 2009 – 2011 was formed. The Short Form-36 (SF-36) was administered at admission and repeated at 1, 2, 4 and 12 months after injury. Group based trajectory modeling (GBTM) was used to determine the number and shape of physical component score (PCS) and mental component score (MCS) trajectories.
Results
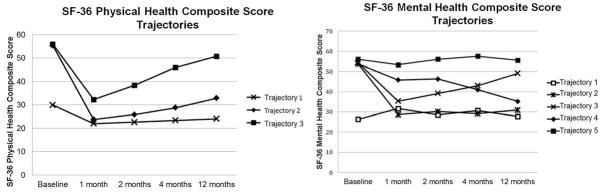
Three PCS trajectories and five MCS trajectories were identified. For PCS, trajectory 1 (10.4%) has low baseline scores, followed by no improvement over time. Trajectory 2 (65.6%) declines 1 month after injury then improves over time. Trajectory 3 (24.1%) has a sharp decline followed by rapid recovery. For MCS, trajectory 1 (9.4%) is low at baseline and remains low. Trajectory 2 (14.4%) has a large decrease post-injury and does not recover over the next twelve months. Trajectory 3 (22.7%) has an initial decrease in MCS early, followed by continuous recovery. Trajectory 4 (19.1%) has a steady decline over the study period. Trajectory 5 (34.3%) stays consistently high at all time points.
Conclusions
Recovery after injury is complex and results in multiple recovery trajectories. This has implications for patient centered clinical trial design and in development of patient specific interventions to improve outcomes.
Keywords: Quality of life, Recovery Trajectories, Injury, Trauma
INTRODUCTION
Injury remains a significant public health problem with more than 2.4 million people requiring hospitalization secondary to injury every year in the United States [1]. Only a small fraction of the injured die while in hospital and the vast majority survive to hospital discharge [1]. A growing body of research demonstrates that injury survivors will suffer a prolonged recovery lasting at least a year [2–5]. Most research in this patient population supports what is likely the prevailing mental model that clinicians have regarding recovery trajectories following injury. During the year after injury, patients have a significant drop in quality of life and functional ability followed by a generally upward rise during the recovery period. However, it is possible that not all patients will follow this usual recovery trajectory.
Longitudinal studies in other disciplines, particularly the social sciences, demonstrate that subpopulations may exist in a cohort that do not follow the prevailing trajectory [6–8]. To help identify individuals who follow similar paths over time with regard to an outcome, social scientists have applied group based trajectory modeling to longitudinal cohorts. Group based trajectory modeling is a specialized application of finite mixture modeling and has been increasingly utilized in the healthcare setting to identify specific clusters of individuals who follow similar recovery trajectories after an illness [8–10].
While there are studies that have examined the overall outcome trajectory of moderately to severely injured patients, most have not tested for the existence of subpopulations that may follow different post-injury recovery trajectories. Further, previous studies often include patients with spinal cord injury and traumatic brain injury which may obscure the presence of underlying trajectories. To address these gaps in the literature, we prospectively followed a cohort of patients to characterize the types of recovery trajectories that exist in the non-neurologically injured population. Based on prior research, we theorized that there would be at least four distinct recovery trajectories for each of the mental, physical and joint mental and physical functioning outcomes.
MATERIALS AND METHODS
Study Setting and Sample
This was a prospective longitudinal study that followed traumatically injured patients for 12 months after injury. Patients were recruited from the Presley Memorial Trauma Center (PMTC) in Memphis, Tennessee from January 2009 to December 2011. The PMTC is a Level I trauma center with a catchment area that encompasses from western Tennessee, northern Mississippi, eastern Arkansas, and the boot-heel of Missouri. Patients were eligible for inclusion in the study if the patient was an adult (age ≥ 18) admitted to the PMTC who suffered either a penetrating or blunt injury, with an Injury Severity Score (ISS) greater than 10, who was admitted for more than twenty-four hours and who was able to speak English.. Patients were excluded from the study if they are more than twenty-four hours from the time of injury when they are admitted to the PMTC, if they had a significant head injury [defined as Head/Neck Abbreviated Injury Scale (AIS) >2 or a Glasgow Coma Score (GCS) < 15 at 24 hours after admission], if they had any spinal cord injury or any burn involving greater than 20% body surface area, if they were pregnant women (assessed by a urine pregnancy test), if they had a history of an injury in the past two years that required admission to a hospital, if they had a primary residence outside of the catchment area for the PMTC, or if they were incarcerated at the time of study enrollment.
Study personnel approached eligible patients at the time of hospital discharge. If the patient consented to study participation, the patient was given a baseline survey that included measures of socioeconomic status, co-morbidities, quality of life and functional ability (SF-36). The patients were followed as outpatients and the survey was repeated at 1, 2, 4, and 12 months after injury. To maintain the cohort, detailed contact information was obtained from each participant including the contact information for a next of kin that did not live in the same household. Before being considered lost to follow-up the participant and a next of kin were sent certified letters with the survey and a self addressed return envelope. If there was no response the National Death Index was searched to determine if the participant died during follow-up. If these methods were exhausted, the participant was considered lost to follow-up. The University of Tennessee Health Science Center Institutional Review Board approved this study.
Outcome Variables
We used the Short Form (36) Health Survey (SF-36) to evaluate quality of life after injury. The SF-36 produces an 8-scale profile of health that can be used to calculate summary physical and mental health composite scores. Both the physical and mental composite scores were used as outcome variables in the analysis. The SF-36 has been widely used and validated in the injured patient population [11–13].
Analysis
The primary aim of this study was to investigate trajectories of quality of life outcomes following injury. Group-based trajectory modeling (GBTM) was used to identify classes of individuals within the study sample that had varying and distinct patterns of recovery over the 12-month study. We performed this analysis with two different outcome variables, the SF-36 physical composite score (PCS) and the SF-36 mental composite score (MCS). The primary advantage of this type of analysis is that it is able to classify a dynamic outcome as distinct longitudinal trends among subgroups of a heterogeneous population. Each study participant was assigned to a single trajectory for each respective outcome through the use of posterior probabilities, which is carried out automatically during the TRAJ procedure in SAS. The Bayesian information criterion was used to determine the best fitting model for one to five trajectory subgroups. For each trajectory, descriptive analyses examining baseline patient characteristics were conducted. Chi-square tests were used to assess significant differences between trajectory subgroups. SAS 9.3 (Cary, NC) was used to conduct all analyses.
RESULTS
Cohort Characteristics
A total of 500 patients were enrolled in the study. Follow-up was 93% at 1 month, 82% at 2 months, 70% at 4 months and 58% at 12 months. No patients enrolled in the study were reported as deceased in the National Death Index during the one-year follow-up period. Approximately half of the sample was under 35 years of age at baseline (50.8%) and less than 10% was over 60 (7.0%), indicating a fairly young cohort. Half of the study sample was white (50.6%) and 64.8% were male. A large percentage of patients were uninsured at baseline (42.2%). Of those with insurance coverage, 34.2% had private insurance, 11.4% had Medicaid, and 5.6% had Medicare. About one-third of patients had injury severity scores (ISS) less than 15 (29.5), another third had ISS between 16 and 24 (36.8), and the last third had ISS equal to 25 or greater (30.4%). (Table 1)
Table 1.
Cohort Characteristics
| Frequency (%) | |
|---|---|
| Age Group | |
| 18–35 | 254 (50.8) |
| 36–45 | 91 (18.2) |
| 46–60 | 120 (24.0) |
| >60 | 35 (7.0) |
| Gender | |
| Male | 324 (64.8) |
| Female | 176 (35.2) |
| Race | |
| White | 253 (50.6) |
| Black | 243 (48.6) |
| Relationship Status | |
| Married | 154 (30.8) |
| Divorced | 76 (15.2) |
| Widowed | 13 (2.6) |
| Separated | 23 (4.6) |
| Never Married | 189 (37.8) |
| Member of an unmarried couple | 45 (9.0) |
| Employment | Baseline |
| Employed for wages | 256 (51.2) |
| Self-employed | 66 (13.2) |
| Out of work more than 1 year | 58 (11.6) |
| Out of work for less than 1 year | 52 (10.4) |
| Retired | 14 (2.8) |
| Unable to work | 27 (5.4) |
| Individual Income | |
| Less than $10,000 | 214 (42.8) |
| $10,000 – less than $15,000 | 56 (11.2) |
| $15,000 – less than $25,000 | 62 (12.4) |
| $25,000 – less than $35,000 | 48 (9.6) |
| $35,000 – less than $50,000 | 32 (6.4) |
| $50,000 – less than $75,000 | 28 (5.6) |
| $75,000 or more | 28 (5.6) |
| Don’t know | 32 (6.4) |
| ISS | |
| 11 – 15 | 148 (29.5) |
| 16 – 24 | 184 (36.8) |
| 25 – 34 | 123 (24.6) |
| 35 and greater | 29 (5.8) |
| Hypotension | |
| No | 440 (88.0%) |
| Yes | 39 (7.8%) |
| Insurance | |
| Private | 171 (34.2%) |
| Medicare | 28 (5.6%) |
| Medicaid | 57 (11.4%) |
| Self-Pay | 211 (42.2%) |
SF-36 Scores
The mean physical composite score was 52.9 at baseline and dropped to 25.6 at the 1 month follow-up. The average PCS score continued to increase throughout the study and reached 35.9 at the final follow-up time point. MCS scores averaged 52.2 at baseline and decreased to 42.3 at 1 month follow-up. For the remainder of the study, MCS means were stable (44.0 at 2 month follow-up, 44.4 at 4 month follow-up, and 44.4 at 12 month follow-up). (Table 2)
Table 2.
Mean Scores of SF-36 Subscales
| Baseline | 1 Month | 2 Months | 4 Months | 12 Months | |
|---|---|---|---|---|---|
| SF-36, Mean (SD) | |||||
| Physical Function | 89.6 (22.3) | 16.5 (22.4) | 24.7 (26.5) | 36.2 (30.7) | 48.6 (32.2) |
| Role limitations due to physical health | 86.3 (31.8) | 5.1 (18.9) | 9.4 (25.8) | 18.6 (33.4) | 34.8 (43.0) |
| Role limitations due to emotional problems | 85.1 (33.7) | 37.6 (45.6) | 43.1 (45.4) | 44.7 (45.0) | 52.2 (44.6) |
| Energy/Fatigue | 67.2 (24.2) | 31.6 (22.1) | 39.3 (21.7) | 43.5 (22.5) | 45.3 (24.2) |
| Emotional well-being | 80.6 (20.8) | 57.5 (23.6) | 59.3 (23.3) | 60.4 (24.0) | 60.7 (25.3) |
| Social functioning | 88.6 (23.4) | 34.4 (30.2) | 43.9 (29.8) | 53.8 (30.3) | 59.8 (31.9) |
| Pain | 87.4 (23.2) | 22.6 (22.2) | 34.6 (26.3) | 43.2 (27.3) | 48.6 (29.1) |
| General Health | 78.0 (23.6) | 62.4 (21.7) | 59.5 (22.2) | 58.0 (22.9) | 55.5 (25.3) |
| Physical Composite Score | 52.9 (9.6) | 25.6 (7.6) | 28.3 (9.0) | 32.0 (10.3) | 35.9 (11.7) |
| Mental Composite Score | 52.2 (11.1) | 42.3 (12.7) | 44.0 (12.9) | 44.4 (13.2) | 44.4 (13.5) |
Physical and Mental Health Trajectories Following Injury
The trajectory analysis examining patterns of change in the SF-36 physical component score identified three subgroups. Trajectory 1 (10.4% of the sample) is characterized by a lower baseline level of functioning, followed by a static, low-level of functioning following injury with little improvement over time. Trajectory 2 (65.6%) members have a drastic decline in functioning 1 month after injury, but show small, but consistent improvement for the remainder of the study. Trajectory 3 (24.1%) also has a sharp decline in physical health 1 month post-injury, but has a much faster recovery and reaches near-baseline levels of health by the 12 month follow-up. The second outcome examined, SF-36 mental composite score, had greater variability in outcomes than PCS with 5 distinct trajectories being identified by the analysis. Members of the Trajectory 1 subgroup (9.4%) have low mental health composite scores at baseline and continue to have low scores throughout the rest of the study. Trajectory 2 (14.4%) has a large decrease in mental health post-injury and does not recover over the next twelve months. Trajectory 3 (22.7%) has an initial decrease in mental health scores early after injury, followed by continuous improvement. Trajectory 4 (19.1%) of the population has a steady decline in mental health across most of the study. Lastly, Trajectory 5 (34.3%) has consistently high mental health scores across all phases of recovery. Overall, this analysis demonstrated that physical health tends to improve in similar patterns across subgroups of the population; however they are stratified by the magnitude of their deficits. In contrast, mental health outcomes have greater variation over the course of the study and subgroups vary in both the pattern of change and the magnitude of their deficits. (Figure 1)
Figure 1.
Trajectories of Physical and Mental Health Scores after Injury
Members of the three PCS trajectory subgroups differed significantly on several characteristics. A larger proportion of members in Trajectory 1 were older, with 50% of members belonging to the 46–60 year old age group. In contrast, 50.7% and 68.0% of members in Trajectories 2 and 3, respectively, were between the ages 18 and 35 (p<0.001). PCS trajectory subgroups did not significantly differ in regards to gender, race, or insurance status (p=0.536, p=0.050, p=0.086). Trajectory 3 had the fewest members with ISS greater than 25 (30.6% Trajectory 1, 35.1% Trajectory 2, and 19.6% Trajectory 3; p=0.022). There were no significant differences in hypotension between groups (p=0.580). (Table 3)
Table 3.
PCS Trajectory Characteristics
| Frequency (%) | Group 1 | Group 2 | Group 3 | p value |
|---|---|---|---|---|
| Age Group | <0.001 | |||
| 18–35 | 8 (16.0) | 176 (50.7) | 70 (68.0) | |
| 36–45 | 9 (18.0) | 64 (18.4) | 18 (17.5) | |
| 46–60 | 25 (50.0) | 83 (23.9) | 12 (11.7) | |
| >60 | 8 (16.0) | 24 (6.9) | 3 (2.9) | |
| Gender | 0.536 | |||
| Male | 29 (58.0) | 226 (65.1) | 69 (67.0) | |
| Female | 21 (42.0) | 121 (34.9) | 34 (33.0) | |
| Race | 0.050 | |||
| White | 33 (66.0) | 181 (52.2) | 42 (40.8) | |
| Black | 17 (34.0) | 165 (47.6) | 61 (59.2) | |
| Relationship Status | <0.001 | |||
| Married | 22 (44.0) | 107 (30.8) | 25 (24.3) | |
| Divorced | 14 (28.0) | 51 (14.7) | 11 (10.7) | |
| Widowed | 4 (8.0) | 9 (2.6) | 0 (0.0) | |
| Separated | 0 (0.0) | 19 (5.5) | 4 (3.9) | |
| Never Married | 7 (14.0) | 128 (36.9) | 54 (52.4) | |
| Member of an unmarried couple | 3 (6.0) | 33 (9.5) | 9 (8.7) | |
| Employment | <0.001 | |||
| Employed for wages | 12 (24.0) | 179 (51.6) | 65 (63.1) | |
| Self-employed | 8 (16.0) | 49 (14.1) | 9 (8.7) | |
| Out of work more than 1 year | 11 (22.0) | 39 (11.2) | 8 (7.8) | |
| Out of work for less than 1 year | 1 (2.0) | 40 (11.5) | 11 (10.7) | |
| Retired | 2 (4.0) | 12 (3.5) | 0 (0.0) | |
| Unable to work | 15 (30.0) | 9 (2.6) | 3 (2.9) | |
| Individual Income | 0.233 | |||
| Less than $10,000 | 23 (46.0) | 146 (42.1) | 45 (43.7) | |
| $10,000 – less than $15,000 | 7 (14.0) | 36 (10.4) | 13 (12.6) | |
| $15,000 – less than $25,000 | 6 12.0) | 52 (15.0) | 4 (3.9) | |
| $25,000 – less than $35,000 | 6 (12.0) | 34 (9.8) | 8 (7.8) | |
| $35,000 – less than $50,000 | 2 (4.0) | 23 (6.6) | 7 (6.8) | |
| $50,000 – less than $75,000 | 3 (6.0) | 18 (5.2) | 7 (6.8) | |
| $75,000 or more | 1 (2.0) | 16 (4.6) | 11 (10.7) | |
| Don’t know | 2 (4.0) | 22 (6.3) | 8 (7.8) | |
| ISS | 0.022 | |||
| 11 – 15 | 17 (34.7) | 101 (30.3) | 30 (29.4) | |
| 16 – 24 | 17 (34.7) | 115 (34.5) | 52 (51.0) | |
| 25 – 34 | 12 (24.5) | 98 (29.4) | 13 (12.7) | |
| 35 and greater | 3 (6.1) | 19 (5.7) | 7 (6.9) | |
| Hypotension | 0.580 | |||
| No | 43 (89.6) | 301 (91.5) | 96 (94.1) | |
| Yes | 5 (10.4) | 28 (8.5) | 6 (5.9) | |
| Insurance | 0.086 | |||
| Private | 21 (42.0%) | 114 (32.9%) | 36 (35.0%) | |
| Medicare | 7 (14.0%) | 19 (5.5%) | 2 (1.9%) | |
| Medicaid | 6 (12.0%) | 37 (10.7%) | 14 (13.6%) | |
| Self-Pay | 14 (28.0%) | 150 (43.2%) | 47 (45.6%) |
There were several significant differences in characteristics between members of MCS trajectory subgroups. Trajectory 5 had the highest post-injury MCS scores throughout the study period and also had the highest percentage of members over 60 years old (12.4%). Trajectory 1 had the lowest MCS scores at baseline and throughout the study and had the greatest percentage of members in the 46–60 year old category (39.6%). Trajectories 1 and 2 also had significantly more females than Trajectories 3, 4, and 5 (Trajectory 1: 54.2% female, Trajectory 2: 42.4%, Trajectory 3: 31.0%, Trajectory 4: 32.9%, and Trajectory 5: 31.4%; p=0.023). There were no significant differences in the racial make-up of the subgroups. Insurance status differed significantly between the groups (p<0.001), with Trajectory 2 having the highest percentage of members with no insurance (54.5%) and Trajectory 5 having the highest percentage of members with private insurance (44.3%). The ISS differed significantly between subgroups, with Trajectory 4 having the greatest number of members with scores above 25 (31.3% Trajectory 1, 25.4% Trajectory 2, 32.8% Trajectory 3, 51.4% Trajectory 4, and 25.4% Trajectory 5; p=0.024). (Table 4)
Table 4.
MCS Trajectory Characteristics
| Frequency (%) | Group 1 | Group 2 | Group 3 | Group 4 | Group 5 | p values |
|---|---|---|---|---|---|---|
| Age Group | 0.002 | |||||
| 18–35 | 16 (33.3) | 35 (53.0) | 56 (49.6) | 52 (65.8) | 95 (49.0) | |
| 36–45 | 10 (20.8) | 15 (22.7) | 21 (18.6) | 11 (13.9) | 34 (17.5) | |
| 46–60 | 19 (39.6) | 16 (24.2) | 31 (27.4) | 13 (16.5) | 41 (21.1) | |
| >60 | 3 (6.3) | 0 (0.0) | 5 (4.4) | 3 (3.8) | 24 (12.4) | |
| Gender | 0.023 | |||||
| Male | 22 (45.8) | 38 (57.6) | 78 (69.0) | 53 (67.1) | 133 (68.6) | |
| Female | 26 (54.2) | 28 (42.4) | 35 (31.0) | 26 (32.9) | 61 (31.4) | |
| Race | 0.292 | |||||
| White | 32 (66.7) | 31 (47.0) | 56 (49.6) | 36 (45.6) | 101 (52.1) | |
| Black | 16 (33.3) | 35 (53.0) | 56 (49.6) | 43 (54.4) | 93 (47.9) | |
| Relationship Status | 0.001 | |||||
| Married | 11 (22.9) | 14 (21.2) | 32 (28.3) | 22 (27.8) | 75 (38.7) | |
| Divorced | 17 (35.4) | 10 (15.2) | 16 (14.2) | 10 (12.7) | 23 (11.9) | |
| Widowed | 4 (8.3) | 3 (4.5) | 1 (0.9) | 1 (1.3) | 4 (2.1) | |
| Separated | 1 (2.1) | 6 (9.1) | 6 (5.3) | 3 (3.8) | 7 (3.6) | |
| Never Married | 12 (25.0) | 27 (40.9) | 41 (36.3) | 37 (46.8) | 72 (37.1) | |
| Member of an unmarried couple | 3 (6.3) | 6 (9.1) | 17 (15.0) | 6 (7.6) | 13 (6.7) | |
| Employment | <0.001 | |||||
| Employed for wages | 11 (22.9) | 27 (40.9) | 63 (55.8) | 36 (45.6) | 119 (61.3) | |
| Self-employed | 5 (10.4) | 10 (15.2) | 16 (14.2) | 10 (12.7) | 25 (12.9) | |
| Out of work more than 1 year | 11 (22.9) | 14 (21.2) | 10 (8.8) | 12 (15.2) | 11 (5.7) | |
| Out of work for less than 1 year | 6 (12.5) | 6 (9.1) | 12 (10.6) | 10 (12.7) | 18 (9.3) | |
| Retired | 1 (2.1) | 1 (1.5) | 2 (1.8) | 0 (0.0) | 10 (5.2) | |
| Unable to work | 11 (22.9) | 2 (3.0) | 5 (4.4) | 5 (6.3) | 4 (2.1) | |
| Individual Income | 0.001 | |||||
| Less than $10,000 | 27 (56.3) | 34 (51.5) | 51 (45.1) | 44 (55.7) | 58 (29.9) | |
| $10,000 – less than $15,000 | 5 (10.4) | 8 (12.1) | 13 (11.5) | 7 (8.9) | 23 (11.9) | |
| $15,000 – less than $25,000 | 10 (20.8) | 8 (12.1) | 10 (8.8) | 6 (7.6) | 28 (14.4) | |
| $25,000 – less than $35,000 | 3 (6.3) | 3 (4.5) | 9 (8.0) | 7 (8.9) | 26 (13.4) | |
| $35,000 – less than $50,000 | 2 (4.2) | 2 (3.0) | 8 (7.1) | 5 (6.3) | 15 (7.7) | |
| $50,000 – less than $75,000 | 0 (0.0) | 2 (3.0) | 9 (8.0) | 4 (5.1) | 13 (6.7) | |
| $75,000 or more | 0 (0.0) | 1 (1.5) | 4 (3.5) | 1 (1.3) | 22 (11.3) | |
| Don’t know | 1 (2.1) | 8 (12.1) | 9 (8.0) | 5 (6.3) | 9 (4.6) | |
| ISS | 0.024 | |||||
| 11 – 15 | 11 (22.9) | 18 (28.6) | 38 (34.5) | 16 (20.5) | 65 (35.1) | |
| 16 – 24 | 22 (45.8) | 29 (46.0) | 36 (32.7) | 24 (30.8) | 73 (39.5) | |
| 25 – 34 | 12 (25.0) | 13 (20.6) | 29 (26.4) | 34 (46.3) | 35 (18.9) | |
| 35 and greater | 3 (6.3) | 3 (4.8) | 7 (6.4) | 4 (5.1) | 12 (6.5) | |
| Hypotension | 0.202 | |||||
| No | 44 (91.7) | 60 (96.8) | 100 (91.7) | 67 (85.9) | 169 (92.9) | |
| Yes | 4 (8.3) | 2 (3.2) | 9 (8.3) | 11 (14.1) | 13 (7.1) | |
| Insurance | <0.001 | |||||
| Private | 13 (27.1%) | 13 (19.7%) | 34 (30.1%) | 25 (31.6%) | 86 (44.3%) | |
| Medicare | 9 (18.8%) | 1 (1.5%) | 7 (6.2%) | 1 (1.3%) | 10 (5.2%) | |
| Medicaid | 6 (12.5%) | 11 (16.7%) | 14 (12.4%) | 12 (15.2%) | 14 (7.2%) | |
| Self-Pay | 20 (41.7%) | 36 (54.5%) | 51 (45.1%) | 37 (46.8%) | 67 (34.5%) |
DISCUSSION
In this prospective longitudinal study of 500 moderately to severely injured patients without brain or spinal cord injury, we found that there are distinct sub-populations with varying recovery trajectories for physical and mental health. This is particularly true for mental health where we found five different recovery trajectories. In terms of physical recovery, only about 25% of patients experience the expected recovery trajectory with a sharp initial decline in function from baseline and a gradual return of function over time. The vast majority of injured patients suffer an abrupt decline in physical function with an increase in function over time, but, the recovery trajectory is blunted and has a shallow slope. There is a small subset of patients that were poorly functioning at baseline with no real recovery after injury. The mental health trajectories were more complicated. Two mental health trajectories showed no change over time, while the remaining three were more dynamic. The most concerning trajectory was one in which patients started out with relatively high mental health functioning in the early months after injury, but, this function decayed over time. Overall more than 43% of patients had what would be considered a poor mental health outcome trajectory.
The results of this study challenge the prevailing mental model to describe post-injury recovery. This prevailing mental model is most consistent with the one described for recovery from critical illness by Iwashyna and supported by data in injured patients from Holbrook, Zatzick and others [2–4, 14]. In this mental model, injured patients suffer a dramatic decrease in functional ability and overall quality of life soon after injury. In the next year, or years, after injury, quality of life improves but does not return to pre-injury baseline levels or even to levels consistent with general United States population norms. Iwashyna refers to this as the “Big Hit” trajectory [14]. The findings in the current study indicate that the Big Hit trajectory is not the prevailing trajectory experienced by moderate to severely injured patients with non-neurologic injury. Both physical and mental health trajectories are more complex and nuanced in this patient population.
The existence of multiple recovery trajectories after injury has significant clinical, public health and research implications. We know that persistent physical and mental health disability is associated with increased mortality, increased health care utilization, and increased reliance on public support due to lost wages or insurance coverage [15–19]. The current study indicates that over 76.0% have poor physical functional trajectories and 42.9% have poor mental health trajectories. From a clinical standpoint it would be valuable to be able to identify those at risk for poor recovery and intervene to improve long-term outcome. Because of the variability in outcome trajectories, a one-size fits all treatment strategy may not be the best option. Perhaps a more dynamic recovery intervention that involves feedback loops would be more advantageous than a single, standard approach. In the geriatric patient population and in those with dementia, these dynamic, personalized approaches to care have been associated with improved long-term functioning [20–22].
From a research perspective, the results of this study can inform the design of future patient centered outcome studies among injured patient cohorts. For example, because patients may be on varying trajectories, it is important for studies to include more than two time points for outcome assessments. Otherwise, it is not possible to detect patients on different recovery trajectories. Certain endpoints may also be more relevant for patients on specific recovery trajectories. For example, mental health may be more affected over the long-term than physical health. Understanding how the two trajectories inform one another is important to capturing proper variables during the study in order to be able to limit confounding. Another important factor may be that certain subpopulations may be on a more overall downward trajectory even prior to injury. The elderly are a good example. In the elderly, functioning may decline over time rather than improve, and studying the overall rate of decline and the influence varying interventions have on moderating the rate of decline may be a better approach than trying to maximize overall recovery. For patients who have a more relapsing type trajectory, it may be that assessing the patients at a fixed interval of time may not reveal the relapsing nature of the trajectory. More appropriate measures for the relapsing trajectory subtype might be to utilize an outcome other than an absolute outcome measure. A more dynamic outcome might be more appropriate that is scaled over time.
From a public health perspective, while a significant number of resources might be required to implement a system that utilizes dynamic feedback loops to deliver more personalized post-injury support, it is possible that this approach may improve outcomes and reduce costs to the entire healthcare system. Further, trauma centers and trauma systems are well positioned to begin following these outcomes in a prospective manner. Trauma registries and performance improvement programs already exist at the center and system level. Together, the registry and performance improvement programs already form the basis of a feedback loop. At the center and system level, outcomes are continually assessed and processes are revised in order to improve the entire system. By adding patient centered outcome measures in the outpatient setting in association with dynamic, patient centered interventions, outcomes for entire populations of injured patients could be maximized, extending the reach of trauma centers and trauma systems.
The main strengths of this study are its prospective, longitudinal design and the frequent outcome assessments over the year. However, there are some limitations that should be addressed. To date there is no specific, validated quality of life measure for injured patients. The SF-36 has been used extensively in the injured patient population but it does have some significant ceiling effects [11–13]. That is, the SF-36 has difficulty discriminating at high levels of function. It is possible that with a more sensitive instrument more or different trajectories could be found. It is also possible that the baseline quality of life may not be representative of the true, pre-injury quality of life since the baseline survey was administered after injury and prior to hospital discharge. Further, the findings of this study are limited to the patient population under study. The results cannot be applied to patients with significant head injury or spinal cord injury. Further, the study was a single center study. Quality of life may be influenced by environmental factors and the outcomes from this study may be specific to the region in which it took place. Like any study with less than 100% follow-up at every time point, this study is subject to response bias. Despite robust follow-up at each time point, there is still the chance that patients who followed up were different than those who did follow-up. While this is a possibility, when patients who followed up were compared to those who did not with regard to demographics and injury characteristics, we found significant differences in regards to age (p=0.008) and gender (p<0.001). Those who followed-up throughout the entire study period were more likely to belong to older age groups and more likely to be female, which are both characteristics associated with poorer quality of life outcomes following injury. It is also possible that patients who consented to participate in the study were different in some way from those who were eligible but refused to participate. We found no significant difference between the demographics, injury mechanism or injury severity of those who were eligible and consented and those who were eligible and did not consent to participate in the study. However, there could be some unmeasured differences between groups that could lead to bias in the results of this study
CONCLUSIONS
Despite these limitations, we found that recovery following non-neurologic moderate to severe injury is complex and that the vast majority of patients do not follow similar recovery trajectories. In fact, more than 75% of patients follow a poor physical health recovery trajectory and 42.9% of patients have a poor mental health recovery trajectory. The findings of this study support changes to approaches used to care for injured patients in the recovery period. Further, any quality of life research that takes place using this patient population should take into account the varying recovery trajectories that patients may have and methods should be optimized to take this into consideration.
Footnotes
Presentation Disclosure:
This work was presented in abstract form at the 10th Annual Academic Surgical Congress in Las Vegas Nevada in February 2015.
Author Contributions:
Dr. Zarzaur was responsible for study conception and design, obtaining funding, data acquisition, data analysis, results interpretation, drafting of manuscript, critical revisions of manuscript. Dr. Bell was responsible for data analysis, results interpretation, and critical revisions of the manuscript.
Disclosures
Funding Disclosure:
Research reported in this publication was supported by National Institute of General Medical Sciences of the National Institutes of Health under award number K23GM084427. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Ben L. Zarzaur, Email: bzarzaur@iupui.edu.
Teresa Bell, Email: terebell@iupui.edu.
References
- 1.Centers for Disease Control National Center for Injury Prevention and Control. [Accessed January 23, 2014];WISQARS [database online] http://wisqars.cdc.gov:8080/costT/cost_Part1_Intro.jsp/
- 2.Holbrook TL, Anderson JP, Sieber WJ, Browner D, Hoyt DB. Outcome after major trauma: 12-month and 18-month follow-up results from the Trauma Recovery Project. J Trauma. 1999;46(5):765–71. doi: 10.1097/00005373-199905000-00003. [DOI] [PubMed] [Google Scholar]
- 3.Michaels AJ, Michaels CE, Smith JS, Moon CH, Peterson C, Long WB. Outcome from injury: general health, work status, and satisfaction 12 months after trauma. J Trauma. 2000;48:841–8. doi: 10.1097/00005373-200005000-00007. [DOI] [PubMed] [Google Scholar]
- 4.Zatzick D, Jurkovich GJ, Rivara FP, Wang J, Fan MY, Joesch J, Mackenzie A national US study of posttraumatic stress disorder, depression, and work and functional outcomes after hospitalization for traumatic injury. Ann Surg. 2008;248(3):429–37. doi: 10.1097/SLA.0b013e318185a6b8. [DOI] [PubMed] [Google Scholar]
- 5.Greenspan AI, Kellermann AL. Physical and psychological outcomes 8 months after serious gunshot injury. J Trauma. 2002;53:707. doi: 10.1097/00005373-200210000-00015. [DOI] [PubMed] [Google Scholar]
- 6.Wang B, Deveaux L, Li X, Marshall S, Chen X, Stanton B. The impact of youth, family, peer and neighborhood risk factors on developmental trajectories of risk involvement from early through middle adolescence. Soc Sci Med. 2014;106:43–52. doi: 10.1016/j.socscimed.2014.01.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zimmer Z1, Martin LG, Jones BL, Nagin DS. Examining late-life functional limitation trajectories and their associations with underlying onset, recovery, and mortality. J Gerontol B Psychol Sci Soc Sci. 2014;69(2):275–86. doi: 10.1093/geronb/gbt099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jones BL, Nagin DS, Roeder K. A SAS procedure based on mixture models for estimating developmental trajectories. Sociol Methods Res. 2001;29(3):374–93. [Google Scholar]
- 9.Gill TM, Murphy TE, Gahbauer EA, Allore HG. The course of disability before and after a serious fall injury. JAMA Intern Med. 2013;173(19):1780–6. doi: 10.1001/jamainternmed.2013.9063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ferrante LE, Pisani MA, Murphy TE, Gahbauer EA, Leo-Summers LS, Gill TM. Functional Trajectories Among Older Persons Before and After Critical Illness. JAMA Intern Med. 2015;175(4):523–9. doi: 10.1001/jamainternmed.2014.7889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.MacKenzie EJ, McCarthy ML, Ditunno JF, Forrester-Staz C, Gruen GS, Marion DW, Schwab WC Pennsylvania Study Group on Functional Outcomes Following Trauma. Using the SF-36 for characterizing outcome after multiple trauma involving head injury. J Trauma. 2002;52:527–34. doi: 10.1097/00005373-200203000-00018. [DOI] [PubMed] [Google Scholar]
- 12.Ware JE, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473–83. [PubMed] [Google Scholar]
- 13.Kopjar B. The SF-36 health survey: a valid measure of changes in health status after injury. Inj Prev. 1996;2:135–9. doi: 10.1136/ip.2.2.135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Iwashyna TJ. Trajectories of recovery and dysfunction after acute illness, with implications for clinical trial design. Am J Repir Crit Care Med. 2012;186(4):302–4. doi: 10.1164/rccm.201206-1138ED. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.DeSalvo KB, Fan VS, McDonell MB, Fihn SD. Predicting mortality and healthcare utilization with a single question. Health Services Research. 2005;40:1234–46. doi: 10.1111/j.1475-6773.2005.00404.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dominick KL, Ahern FM, Gold CH, Heller DA. Relationship of health-related quality of life to health care utilization and mortality among older adults. Aging Clinical and Experimental Research. 2002;14:499–508. doi: 10.1007/BF03327351. [DOI] [PubMed] [Google Scholar]
- 17.Brown DS, Thompson WW, Zack MM, Arnold SE, Barile JP. Associations between health-related quality of life and mortality in older adults. Prev Sci. 2015;16(1):21–30. doi: 10.1007/s11121-013-0437-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kaplan RM. The significance of quality of life in health care. Quality of Life Research. 2003;12(Suppl 1):3–16. doi: 10.1023/a:1023547632545. [DOI] [PubMed] [Google Scholar]
- 19.Zafar SY, McNeil RB, Thomas CM, Lathan CS, Ayanian JZ, Provenzale D. Population-based assessment of cancer survivors’ financial burden and quality of life: a prospective cohort study. J Oncol Pract. 2015;11(2):145–50. doi: 10.1200/JOP.2014.001542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Callahan CM, Boustani MA, Weiner M, Beck RA, Livin LR, Kellams JJ, et al. Implementing dementia care models in primary care settings:The Aging Brain Care Medical Home. Aging and Mental Health. 2011;15(1):5–12. doi: 10.1080/13607861003801052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Callahan CM, Kroenke K, Counsell SR, Hendrie HC, Perkins AJ, Katon W, et al. Treatment of depression improves physical functioning in older adults. J Am Geriatr Soc. 2005;53(3):367–73. doi: 10.1111/j.1532-5415.2005.53151.x. [DOI] [PubMed] [Google Scholar]
- 22.Boustani MA, Sachs GA, Alder CA, Munger S, Schubert CC, Guerriero Austrom M, et al. Implementing innovative models of dementia care: The Healthy Aging Brain Center. Aging Ment Health. 2011;15(1):13–22. doi: 10.1080/13607863.2010.496445. [DOI] [PMC free article] [PubMed] [Google Scholar]