Introduction
Tuberculosis (TB) is a major global health problem with over 9 million new cases and 1·5 million TB-related deaths in 2013.1 The Stop TB Strategy 2006-2015 focused on six strategic areas with an aim to reduce TB prevalence and mortality by 50% relative to 1990 levels.2 The centerpiece of this strategy was to expand and enhance access to quality TB diagnosis and treatment, addressing MDR-TB and TB/HIV coinfection, strengthening health systems, engaging public and private providers, empowering patients, and promoting research.
The ambitious goals set forth in the Stop TB Strategy are within reach. The TB mortality rate fell by an estimated 45% between 1990 and 2013 and the TB prevalence rate fell by 41% during the same period.1 Despite this progress, the decline in TB incidence has been very slow – with an estimated 1·5% per year decrease in global TB incidence during 2000 – 2013. This stagnation has led to a greater focus on programs and policies to expand the strategy to also include interventions outside of the traditional curative approach within the health care delivery sphere.
The new “End TB Strategy” was adopted in May 2014 by the World Health Assembly and sets the required interventions to end the global TB epidemic by 2035.3 This strategy places a greater emphasis on preventing TB through addressing social determinants of TB, including poverty alleviation policies and social protection programs. The ILO describes social protection as “nationally defined sets of basic social security guarantees which secure protection aimed at preventing or alleviating poverty, vulnerability and social exclusion”.4 This definition covers protection against: general poverty and social exclusion, lack of affordable access to health care, lack of labor market protections, as well as a lack of work-related income. Examples of social protection programs are cash transfers (both conditional and unconditional), free or subsidized health care, food rations, disability pay, maternity leave, housing subsidies and labor market protections.
In order to achieve long-term epidemiological targets more emphasis is needed on preventive interventions that reduce peoples’ vulnerability for TB infection and for progressing from infection to active TB.5 Despite a call for further research, there is a limited amount of work on the relationship between social protection and tuberculosis, especially in developing countries that have the highest disease burden.
Bhargava et al. reanalyzed data from a social experiment conducted during 1918-1943 in Papworth Village Settlement, England where TB patients were assured stable employment as well as adequate nutrition and housing.6 They found that the children of these patients faced substantially lower risks of developing TB relative to children of TB patients who lived outside of the village. A recent study in The Lancet Infectious Diseases by Reeves et al. examined the relationship between social protection levels and national TB rates.7 The authors examined 21 European nations from 1995 to 2012 using TB statistics from WHO and social protection data from EuroStat. The country-year analysis showed an inverse relationship between social protection spending and TB incidence and mortality rates (r=−0·65 and r=−0·63 respectively), however, an association with TB prevalence rate was not found. Reeves et al. showed the relationship between social protection and TB in relatively wealthy nations with sizeable social protection systems and secure welfare mechanisms. This paper builds upon this work by analyzing this association with a global purview.
Methods
We aim to show the association between levels of social protection, measured as the percentage of national GDP spent on social protection programs (excluding health) and national tuberculosis prevalence, incidence, and mortality rates. Social protection data were obtained from the International Labor Organization (ILO) Social Protection Department's publicly available database.8 In order to produce its World Social Protection Report, ILO provides a global overview of social protection systems, their coverage, benefits, and public expenditures. This data covers the years 2000 – 2012, the dates for which complete and reliable data social protection expenditure are available, and includes over 190 countries.
TB burden is expressed in terms of annual incidence and mortality, as well as disease prevalence, which represents the number of cases per population at one point in time. These rates are generally expressed per 100,000 people. Estimates from the World Health Organization are derived from population-based national surveys of the prevalence of TB disease, time-series of TB case notification and mortality data from vital registration systems with standard coding of causes of death. Scarcity of data in some countries and incomplete coverage of surveillance are the primary reason for uncertainty in published estimates. In this paper, TB mortality includes deaths due to TB as well as deaths attributed to the combination of TB/HIV, in cases where TB is ruled to be the more immediate cause of death. The Global TB database is publicly available on the WHO website and continuously updated when new data becomes available.9 The method by which WHO estimates these statistics are described in detail in an online technical appendix and are reviewed annually by an expert panel.10
We first examined levels of social protection by each country and then investigated the association between this level and TB rates, without adjusting for any other factors. This descriptive analysis used the most recent year of available data for each country and gives a global picture of the most up to date social protection data. The analysis includes national-level factors that could also influence TB rates. These include a measure of national economic strength measured by GDP per capita (in US$), HIV rates (of those aged 15-49) as HIV is a key co-infection with TB and the strength of the health system, with percentage of GDP spent on health as a proxy.11,12 Further control variables are population density, percentage of foreign-born residents as a way of controlling for levels of immigration, and TB treatment success rate among new cases. This last control variable is meant to represent the strength of the national TB treatment program. We did not include national measures of more proximal risk factors such as alcohol use, malnutrition, or overcrowding despite the evidence of their association with TB.13-15.This was done because we believe these putative risk factors to be downstream on the causal pathway from social protection to tuberculosis.
We were limited by the data availability of these covariates and the model, which relies on complete case analysis, drops down to 664 country-years when these six covariates are all included. This is in comparison to the univariate model of social protection on TB rates, which includes 803 country-years. Nevertheless, the majority of countries that are excluded from the multivariate analysis are small island states that do not have a large TB burden. The 664 observations in the multivariate model include 146 countries, which accounted for over 98% of global TB notifications in 2013.
To account for the clustering of data points within countries we used a country-level fixed effects model. This is preferable to only using robust standard errors as it is able to purge omitted variable bias of time-invariant factors that are not included in the model such as health care delivery models. We were also concerned with the potential colinearity of GDP and levels of social protection in the model (r=0·55). However, all measures in the model have variance inflation factors below 2·5 and the coefficients of these two variables do not change markedly when one variable is excluded from the model.
We examined both first and second order effects of social protection to see if the predicted relationship was linear. Conceptually, the relationship was hypothesized to be curvilinear and thus a model with a squared social protection term was employed. Having a non-linear relationship allows for the marginal change resulting from a one percent of GDP increase in social protection to vary depending on the starting level of social protection in a particular country. This “U-shaped” relationship is helpful as it allows for interpretation of social protection level changes more accurately for individual countries.
We also conducted a sensitivity analysis to test the robustness of this relationship. In order to see if the level of social protection spending took time to affect TB burden rates we tried the same model specifications as described above but lagged (by one year) the measure of social protection levels.
Role of the funding source
None. The corresponding author confirms that he had full access to all the data in the study and had final responsibility for the decision to submit for publication
Results
Table 1 describes the average values of the model covariates by WHO region. These statistics represent average values weighted by each country's population over the years 2000-2013. This table highlights the relatively high burden of HIV in the African region as well as higher percentages of foreign-born persons in Europe and the Americas. Also evidenced by Table 1 are the higher levels of GDP per capita and social protection spending in these two regions.
Table 1.
Descriptive Statistics, Overall and by WHO Region (with standard deviations in parentheses)*
| Overall | African | The Americas | Eastern Mediterranean | European | South-East Asian | Western Pacific | |
|---|---|---|---|---|---|---|---|
| TB prevalence rate (per 100,000) | 199·01 (170·35) | 345·48 (184·33) | 43·07 (52·60) | 213·64 (175·10) | 80·82 (115·35) | 338·07 (98·76) | 157·38 (140·48) |
| TB incidence rate (per 100,000) | 136·23 (126·60) | 325·74 (221·53) | 32·66 (38·31) | 142·46 (115·75) | 56·26 (65·21) | 203·98 (48·06) | 100·41 (67·10) |
| TB mortality rate (per 100,000) | 25·75 (39·61) | 98·37 (77·20) | 3·39 (7·43) | 26·17 (25·35) | 7·10 (9·11) | 40·08 (17·35) | 8·50 (13·44) |
| Social protection, excluding health (percent of GDP) | 5·81 (5·67) | 1·90 (1·69) | 9·01 (3·61) | 4·94 (4·66) | 14·26 (5·13) | 1·26 (0·70) | 4·52 (3·53) |
| GDP per capita (2014 US$, thousands) | 8·28 (13·67) | 1·42 (1·75) | 21·19 (19·02) | 1·92 (1·75) | 19·62 (16·60) | 1·22 (0·88) | 6·33 (10·39) |
| Adult HIV rate (per 1,000 adults) | 6·48 (20·40) | 46·08 (48·74) | 4·07 (2·36) | 0·60 (1·06) | 2·22 (1·78) | 2·79 (2·05) | 0·78 (1·08) |
| Health expenditure (percent of GDP) | 5·96 (3·04) | 5·90 (1·91) | 10·28 (4·51) | 4·73 (1·62) | 7·74 (2·16) | 3·78 (0·69) | 5·16 (1·19) |
| Population Density (persons per sq. km.) | 194·96 (267·76) | 81·62 (76·00) | 41·80 (47·65) | 110·92 (79·84) | 120·44 (101·10) | 389·70 (250·74) | 192·03 (354·52) |
| Foreign-born (percent of population) | 2·78 (4·80) | 2·13 (2·54) | 6·11 (6·60) | 1·83 (2·08) | 8·63 (5·04) | 0·54 (0·48) | 0·73 (3·26) |
| TB treatment success rate (percent of new cases) | 81·86 (12·57) | 77·22 (9·92) | 76·09 (10·29) | 84·52 (5·52) | 74·34 (10·64) | 81·46 (13·81) | 89·45 (10.66) |
Averages across years 2000-2012, weighted by country population size
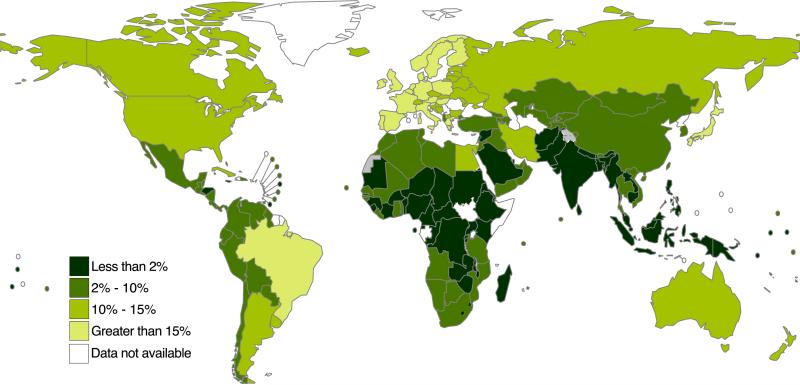
Figure 1 shows individual countries’ social protection levels as a percent of national GDP. The data reflects the latest available year's data for each country in the ILO Social Protection database. The size of the country bubble is relative to its 2013 case notifications with all countries having less than 40,000 cases set to the minimum size in order to properly display the burden in India and China. BRICS and some countries with extreme values were labelled to highlight variations. In general, high-income countries tend to allocate a greater proportion of their GDP to social protection programs. Western Europe is especially generous with several countries expending more than 20% of their GDP on social protection. On the other hand, low-income countries tend to spend very small amount (proportionally) on social protection. Some notable exceptions are Egypt and Brazil which both have notable cash transfer programs (Minhet El-Osra and Bolsa Familia, respectively). The majority of high-burden TB countries, located in sub-Saharan Africa and South-east Asia, allocate less than 10% of their GDP on social protection.
Figure 1.
Levels of social protection (excluding health) expenditure as a percentage of national GDP
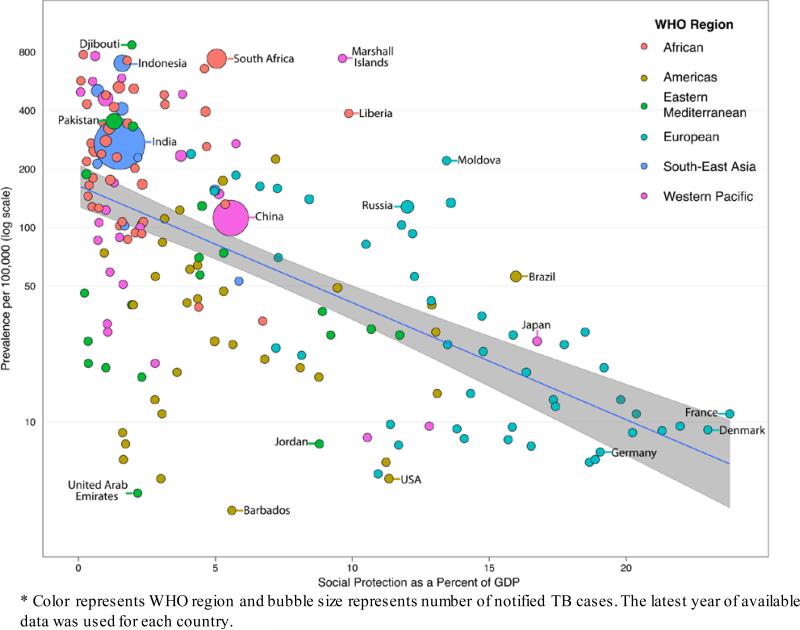
Figure 2 presents the relationship between TB prevalence and social protection levels. The majority of the high – burden countries are grouped in the top-left corner with high prevalence and low levels of social protection. South Africa is a notable outlier, which strengthens the support that this data is best analyzed in a multivariable analysis that includes HIV rates. The figure highlights clear regional effects and a strong inverse relationship between social protection levels and TB Prevalence rates, as shown by the line of best fit and 95% confidence band. The figure also shows that the relationship may not be linear, particularly at very low levels of social protection.
Figure 2.
Bivariate relationship between social protection and TB prevalence rate*
In multivariate models, social protection levels were significantly inversely associated with all three measures of TB burden. This was formally tested using a joint significance test of social protection and its squared term. This effect was observed even when controlling for country-year level covariates and country level fixed effects (Table 2). The sensitivity analysis using a lagged value of social protection did not have a significant between social protection spending and TB prevalence, incidence, or mortality (at the 5% level), however, this modification did not significantly change our model coefficients. (see technical appendix).
Table 2.
Country-level Fixed Effects Regression Models Predicting Tuberculosis Prevalence, Incidence, and Mortality Rates (N=664)
| Prevalence Rate (per 100,000) | Incidence Rate (per 100,000) | Mortality Rate (per 100,000) | |
|---|---|---|---|
| β | β | β | |
| Social protection, excluding health (percent of GDP) | −18·33** (p= 0·009) | −8·16* (p= 0·043) | −5·48** (p= 0·006) |
| Social protection2 | 0·56* (p= 0·049) | 0·23 (p= 0·156) | 0·18* (p= 0·027) |
| GDP per capita (2014 US$, thousands) | −1·75* (p= 0·034) | −0·90 (p= 0·058) | −0·17 (p= 0·469) |
| Adult HIV rate (per 1,000 adults) | 5·54*** (p= 0·000) | 7·22*** (p= 0·000) | 3·47*** (p= 0·000) |
| Health expenditure(percent of GDP) | −2·51 (p= 0·593) | −1·87 (p= 0·488) | −1·15 (p= 0·384) |
| Population density (persons per sq. km.) | −0·016 (p= 0·831) | −0·001 (p= 0·981) | 0·007 (p= 0·731) |
| Foreign-born (percent of population) | 12·27 (p= 0·074) | 5·55 (p= 0·159) | 0·51 (p= 0·789) |
| TB treatment success rate (percent of new cases) | −0·70 (p= 0·131) | −0·15 (p= 0·584) | −0·28* (p= 0·031) |
Notes:
p<0.05
p<0.01
p<0.001. Social protection and its squared term are jointly significant at the .05 level in all three models.
Higher GDP was associated with lower TB prevalence, incidence, and mortality rates, although only statistically significant in the TB prevalence model. Population density, percent foreign-born, and year were also inversely associated with TB burden rates, however, were not significant in the model. Country-year treatment success rates of new TB patients were inversely related to TB burden but only significant in the mortality model. The percent of the population foreign-born and adult HIV rate positively associated with higher TB rates, although only the latter was significant. Within a country, a one per 1,000 persons drop in the adult HIV rate was associated with a 5·44 per 100,000 reduction in TB prevalence, while holding other factors in the model constant. The effect on incidence is even greater with an equivalent decrease in HIV rate leading to a 7·22 per 100,000 decrease on the rate of new TB cases.
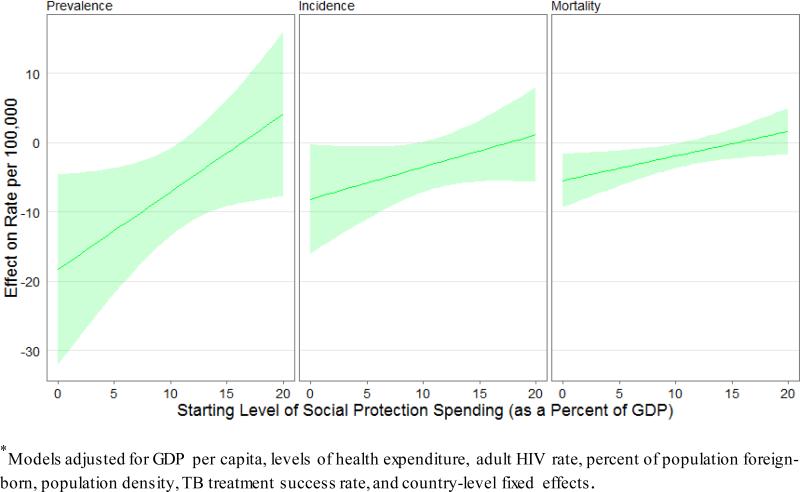
Figure 3 examines the marginal effects of increased social protection level on TB. The greatest predicted impact comes at low levels of social protection. For example, moving from 0% to 1% within a country is associated with an 18·33 person per 100,000 decline in the TB prevalence rate. This same increase in social protection is associated with an 8·16 and 5·48 drop in TB incidence and mortality rates, respectively. However, this relationship is quickly attenuated once a country reaches higher levels of social protection spending. At the 12% of GDP level, the marginal impact of a one percent of GDP increase on social protection spending is no longer significantly related to a drop in TB prevalence, incidence, or mortality. Nevertheless, less than 8% of 2013 TB case notifications derive from countries at or above the social protection spending level of 12% of GDP.
Figure 3.
Effect of a one percent of GDP increase in social protection spending with 95% confidence bands (N=664)*
Limitations
Due to the ecological nature of this study we cannot show a causal relationship between social protection levels and TB rates. However, the clear association found in this analysis supports further research in this area. Bolstering this relationship is the vast amount of evidence on the more proximal poverty-driven risk factors of TB such as malnutrition, overcrowding, and air pollution, as well as poverty as a risk factor for TB itself.14-18 We chose not to control for these measures because we believe them to be on the causal pathway between social protection and TB. To more conclusively explain this causal pathway, we recommend the inclusion of detailed social protection questions to be included in future national tuberculosis prevalence surveys as well as in stand-alone studies on tuberculosis prevention. Furthermore, there is a need for better national social protection data that not only provides overall levels of social protection but also breakdowns of these amounts by type of social protection program.
Incomplete longitudinal country-level data limited us in two ways. Primarily, it mitigated our ability to add more national-level measures related to TB to our models without sacrificing sample size. As our covariates were often derived from disparate sources, each additional merging of datasets resulted in the loss of observations and thus statistical power. This limited sample size also affected our abilities to include interaction terms to see if the effect of social protection on TB rates differs in different settings. One example we would have liked to include would be an interaction between social protection and WHO region; however, we did not have the statistical power to do so.
This analysis relies on the ILO's broad definition of social protection described above. It would be beneficial to split social protection spending into programmatic areas to investigate how each program's expenditures are associated with TB rates. For example, social protection includes labor protections, which may not be as beneficial at reducing TB burden in countries with a larger informal economy, compared to cash transfer programs. This information was available in the work put forth by Reeves et al. as a result of more sophisticated data in Eurostat, the European Union's statistical office.7 A more refined measurement of social protection on a global scale would be helpful in determining which programs or policies are best at reducing the morbidity and mortality burden associated with TB.
Discussion
There is a clear ecological association between social protection spending (as a percentage of GDP) and TB prevalence, incidence, and mortality. This is especially true in setting with low levels of social protection spending. This work gives support to increased funding for upstream interventions that target the social determinants of tuberculosis, especially poverty alleviation. Although the main responsibility for social protection programs or policies belongs to larger divisions of government, the NTP and its international technical partners could also provide support for these efforts from within their budgets in an effort to control TB.
The results from this analysis could also be used as inputs to dynamic mathematical models that predict the effects of social protection interventions on tuberculosis burden as set forth by Murray et al.19 These parameters will be especially useful when there is sparse data on more proximal poverty-driven risk factors such as overcrowding, malnutrition, or indoor air pollution.
The benefits of increased social protection spending go well beyond tuberculosis and would likely effect rates of other communicable and non-communicable diseases, especially those with a well-documented association with poverty. In fact, a study of OECD countries from 1995 to 2005 found that social expenditure was more closely tied to indicators of health than direct health services expenditure.20 The authors also found that a higher ratio of social spending to health spending was predictive of improved infant mortality and life expectancy after controlling for GDP and the overall level of health expenditures.
Supplementary Material
Research in context.
Evidence before this study
We searched PubMed for publications within the last ten years with the MeSH terms “social protection AND tuberculosis” or “tuberculosis AND poverty”. A great deal of work studies the link between poverty and TB, however, few publications were identified analysing the relationship between social protection and TB. Other than this literature search, we relied on the methods employed by the Reeves et al. article on social protection and TB in Europe. Furthermore, our conceptual model was heavily driven by previously published work on the link between poverty and malnutrition and overcrowding, as well as research on these conditions as risk factors for TB.
Added value of this study
This study shows that there is an inverse relationship between social protection spending and TB prevalence, incidence, and mortality. It is the first paper to do so with a global perspective and to comment particularly on the effect of increased social protection spending on TB in settings with minimal social protection programmes in place.
Implications of all the available evidence
National TB programmes (NTPs) may consider further integration with national social protection programmes run by other divisions of government or NGOs. This work also supports NTPs direct role in introducing TB-sensitive social protection schemes aimed at prevention, in combination with patient support policies. This research gives evidence for TB donors, such as the Global Fund to Fight AIDS, TB, and Malaria, to fund social protection interventions outside of the medical sphere in an effort to control TB.
Acknowledgements
This research was supported by NIH/National Center for Advancing Translational Science (NCATS) UCLA CTSI Grant Number TL1TR000121.
Footnotes
Authors’ contributions
Andrew Siroka conducted the literature review and data collection, cleaning and analysis. He also lead the writing and data interpretation.
Dr. Ninez Ponce assisted in guiding the technical specifications of the model and other aspects of the data analysis.
Dr. Knut Lönnroth assisted in the literature review, data interpretation, and writing.
Declaration of interests
Dr. Lönnroth and Mr. Siroka are employed by the World Health Organization Global TB Programme. Dr. Ponce has no conflicts of interest.
Ethics committee approval
This study was given a waiver from UCLA IRB review.
References
- 1.World Health Organization . Global TB Report 2014. WHO; Geneva, Switzerland: 2014. [Google Scholar]
- 2.World Health Organization . The Global Plan to Stop TB. Geneva, Switzerland: 2006. [Google Scholar]
- 3.World Health Assembly Secretariat . Global strategy and targets for tuberculosis prevention, care and control after 2015. World Health Organization; Geneva, Switzerland: 2014. [Google Scholar]
- 4.ILO. Social Protection Floors Recommendation. Geneva: 2012. [Google Scholar]
- 5.Lonnroth K, Jaramillo E, Williams BG, Dye C, Raviglione M. Drivers of tuberculosis epidemics: the role of risk factors and social determinants. Soc Sci Med. 2009;68(12):2240. doi: 10.1016/j.socscimed.2009.03.041. [DOI] [PubMed] [Google Scholar]
- 6.Bhargava A, Pai M, Bhargava M, Marais BJ, Menzies D. Can social interventions prevent tuberculosis?: the Papworth experiment (1918-1943) revisited. Am J Respir Crit Care Med. 2012;186(5):442–9. doi: 10.1164/rccm.201201-0023OC. [DOI] [PubMed] [Google Scholar]
- 7.Reeves A, Basu S, McKee M, Stuckler D, Sandgren A, Semenza J. Social protection and tuberculosis control in 21 European countries, 1995-2012: a cross-national statistical modelling analysis. Lancet Infect Dis. 2014;14(11):1105–12. doi: 10.1016/S1473-3099(14)70927-2. [DOI] [PubMed] [Google Scholar]
- 8.International Labour Organization [July 7, 2015];Social Protection Database. http://www.social-protection.org/gimi/gess/ShowSearchIndicators.action.
- 9.World Health Organization Global TB Database. 2015 http://www.who.int/tb/country/data/download/en/
- 10.World Health Organization [January 2, 2015];Technical Appendix - Methods used to estimate the global burden of disease caused by TB. 2014 http://www.who.int/tb/publications/global_report/gtbr14_online_technical_appendix.pdf.
- 11.World Bank Bank W, editor. World Bank Open Data. 2015 http://data.worldbank.org/
- 12.UNAIDS . AIDSinfo. UNAIDS; 2015. http://www.unaids.org/en/dataanalysis/datatools/aidsinfo. [Google Scholar]
- 13.Lonnroth K, Williams BG, Stadlin S, Jaramillo E, Dye C. Alcohol use as a risk factor for tuberculosis - a systematic review. BMC Public Health. 2008;8:289. doi: 10.1186/1471-2458-8-289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lonnroth K, Williams BG, Cegielski P, Dye C. A consistent log-linear relationship between tuberculosis incidence and body mass index. Int J Epidemiol. 2010;39(1):149–55. doi: 10.1093/ije/dyp308. [DOI] [PubMed] [Google Scholar]
- 15.Kirenga BJ, Ssengooba W, Muwonge C, et al. Tuberculosis risk factors among tuberculosis patients in Kampala, Uganda: implications for tuberculosis control. BMC Public Health. 2015;15(1):13. doi: 10.1186/s12889-015-1376-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lin HH, Ezzati M, Murray M. Tobacco smoke, indoor air pollution and tuberculosis: a systematic review and meta-analysis. PLoS Med. 2007;4(1):e20. doi: 10.1371/journal.pmed.0040020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hossain S, Quaiyum MA, Zaman K, et al. Socio economic position in TB prevalence and access to services: results from a population prevalence survey and a facility-based survey in Bangladesh. PLoS One. 2012;7(9):e44980. doi: 10.1371/journal.pone.0044980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Oxlade O, Murray M. Tuberculosis and poverty: why are the poor at greater risk in India? PLoS One. 2012;7(11):e47533. doi: 10.1371/journal.pone.0047533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Murray M, Oxlade O, Lin HH. Modeling social, environmental and biological determinants of tuberculosis. Int J Tuberc Lung Dis. 2011;15(Suppl 2):S64–70. doi: 10.5588/ijtld.10.0535. [DOI] [PubMed] [Google Scholar]
- 20.Bradley EH, Elkins BR, Herrin J, Elbel B. Health and social services expenditures: associations with health outcomes. BMJ Qual Saf. 2011;20(10):826–31. doi: 10.1136/bmjqs.2010.048363. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.