Abstract
OBJECTIVE
Real-time magnetic resonance image (rtMRI) guided transcatheter aortic valve replacement (TAVR) has improved visualization, real time imaging, and pinpoint accuracy with device delivery. Unfortunately, performing a TAVR in a MRI scanner can be a difficult task due to limited space and an awkward working environment. Our solution was to design a MRI compatible robot-assisted device to insert and deploy a self-expanding valve from a remote computer console. We present our preliminary results in a swine model.
METHODS
We used an MRI compatible robotic arm and developed a valve delivery module. A 12mm trocar was inserted in the apex of the heart via a subxiphoid incision. The delivery device and nitinol stented prosthesis were mounted on the robot. Two continuous real time imaging planes provided a virtual real time 3D reconstruction. The valve was remotely deployed by the surgeon via a graphic user interface.
RESULTS
In an acute, non-survival study, eight swine underwent robot-assisted rtMRI TAVR for evaluation of feasibility. Device deployment took 61 +/− 5 seconds. Post-deployment necropsy was performed to confirm correlation between imaging and the actual valve position.
CONCLUSIONS
These results demonstrate the feasibility of robotic assisted TAVR using rtMRI guidance. This approach may eliminate some of the challenges of performing a procedure while working inside of an MRI scanner and may improve the success of TAVR. It provides superior visualization during the insertion process, deployment with pinpoint accuracy, and potentially communication between the imaging device and the robotic module which will prevent incorrect or misaligned deployment.
OBJECTIVES
Aortic stenosis is the most common type of valvular heart disease in the United States.1–3 This disease process has a long latency period; however, patients rapidly decline after becoming symptomatic. Previously a patient’s only chance for substantially prolonging survival was to undergo cardiopulmonary bypass with surgical aortic valve replacement.4–6 Unfortunately, some of these patients were not appropriate surgical candidates or are high risk surgical candidates.7, 8 Since approval by the Food and Drug Administration in 2011, transcatheter aortic valve replacement (TAVR) has become a viable treatment option for otherwise inoperable or high risk aortic stenosis patients. 7–9
While there have been multiple advances in valve development and valve delivery technology, the imaging modality has remained unchanged. Currently TAVR is performed with a combination of fluoroscopy and transesophageal echocardiography (TEE), which has multiple limitations. The TAVR procedure currently necessitates various imaging modalities for different stages of the procedure.10, 11 Pre-procedural imaging usually includes echocardiography in combination with multidetector computed tomography (MDCT) or computed tomography (CT) angiogram. The TAVR procedure is most commonly performed with a combination of fluoroscopy and transesophageal echocardiography (TEE). Post-procedural imaging also routinely uses a combination of fluoroscopy and TEE to confirm valve placement and cardiac function. 11–14 Fluoroscopy has multiple limitations including poor soft tissue contrast, a requirement for rapid ventricular pacing, radiation exposure to the patient and surgical team, and a risk of contrast-induced nephropathy. 15–18 Real-time magnetic resonance image (rtMRI) guidance overcomes these limitations with improved soft tissue contrast in addition to a three dimensional visualization of the anatomic structures. MRI has the added benefit in that the pre-procedural, intra-procedural, and post-procedural imaging is completed with one device. rtMRI guidance is proposed to be the future of TAVR. 17, 19, 20 Unfortunately, performing a TAVR procedure while working in the bore of an MRI scanner can be a difficult task due to limited space and a potentially awkward working environment. Our solution was to design a MRI compatible robot-assisted device that was capable of inserting and deploying a self-expanding valve from a remote computer console. We present our preliminary results using this device to perform transapical TAVR in a swine model.
MATERIALS AND METHODS
Magnetic Resonance Imaging System
The imaging system has several components, which includes a 1.5 Tesla MRI, interactive image reconstruction software, and advanced pulse sequence technology.21–23 A Magnetom Aera (Siemens Medical Solutions, Munich, Germany) was used for this experiment, which has a 145 cm long by and 70 cm wide bore. The bore size allows an adequate clearance above the patient for the robot system. The system can generate high-quality images at 5–10 frames per second with low latency for fully interactive, real-time imaging. However, standard imaging sequences were used for pre-procedural planning and post-procedural assessment. Interactive Front End navigation software (Siemens Corporate Research, Munich, Germany), along with an interactive real-time pulse sequence (BEAT_IRTTT), was used for real-time navigation during valve deployment. The Interactive Front End navigation software takes multiple slices, which are obtained in rapid succession and can be simultaneously displayed to provide a three-dimensional rendering. The software allows quick adjustment of the imaging planes to allow for real-time device tracking.21–25
Self-expanding Stent and Delivery Device
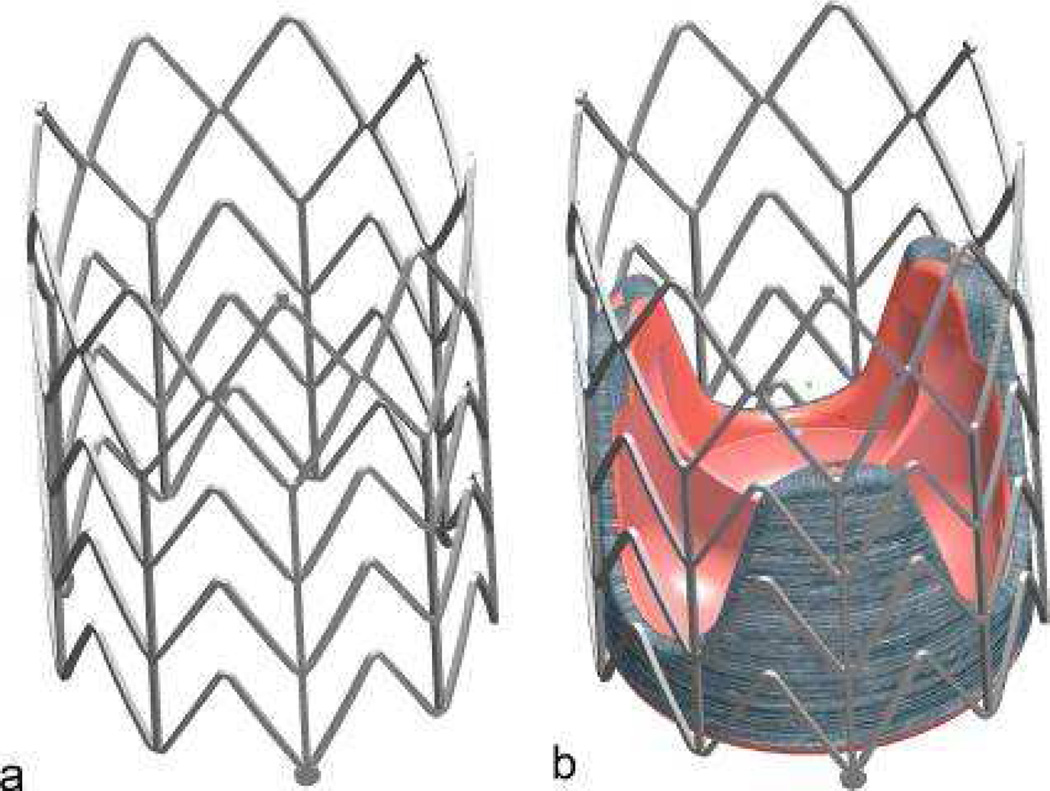
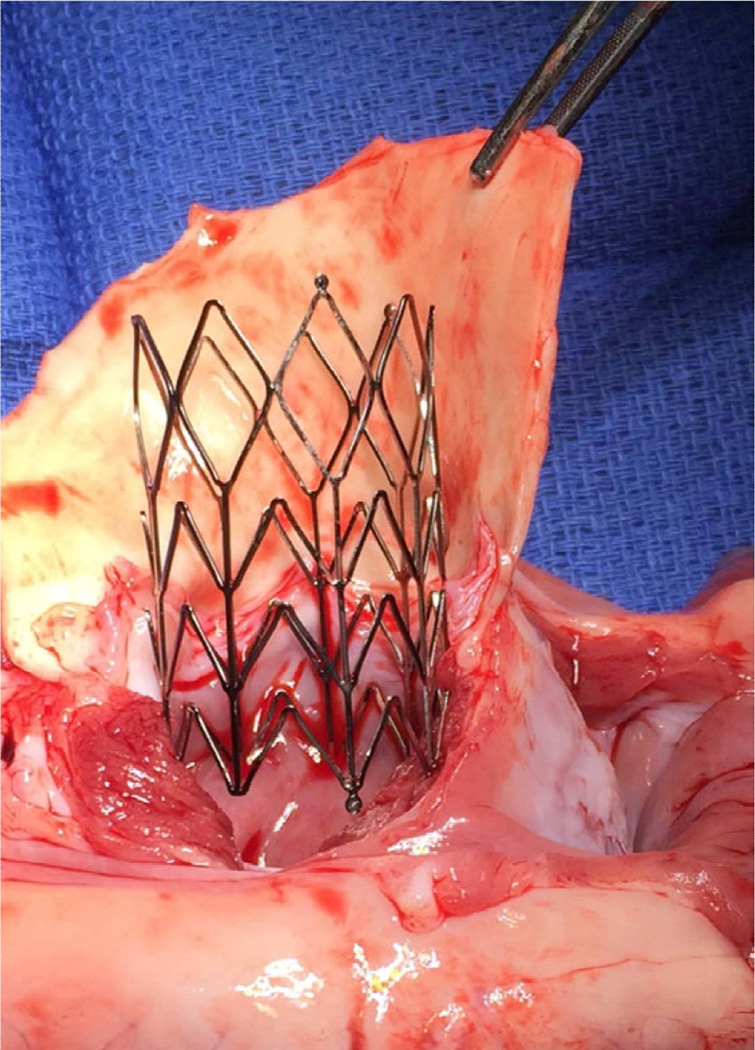
A self-expanding nitinol stent was designed and engineered for the experiment (Figure 1).26 While there are nitinol stents that are commercially available, such as the CoreValve and SAPIEN valve, we designed our own stent for this experiment. While some stents’ geometry utilizes a diamond cell shape, the design my cause increased stress along the stent during the crimping process. Our stent design is based on a chevron shape, which minimizes stress along the chevron cell shape. The chevron shape also prevents stent migration due to the self-anchoring properties of the pointed ends of the chevron. The stent was laser cut from a biocompatible nitinol tube to an expanded diameter of 26mm diameter and a length of 35mm.27 The stent was then compressed with a custom made crimping device and inserted into the delivery device.18 The stent expands to its open configuration upon release from the delivery system.
Figure 1.
(a) Self-expanding stent; (b) bioprosthetic valve affixed in self-expanding stent.
A delivery device was also developed for inserting and deploying the stented prosthesis. The delivery device consists of an inner rod and an outer sheath, which are controlled by the robotic delivery module’s pneumatic actuators. The outer sheath also protects the nitinol stent prior to deployment. The delivery device is MRI compatible and fits into a 12mm trocar.27
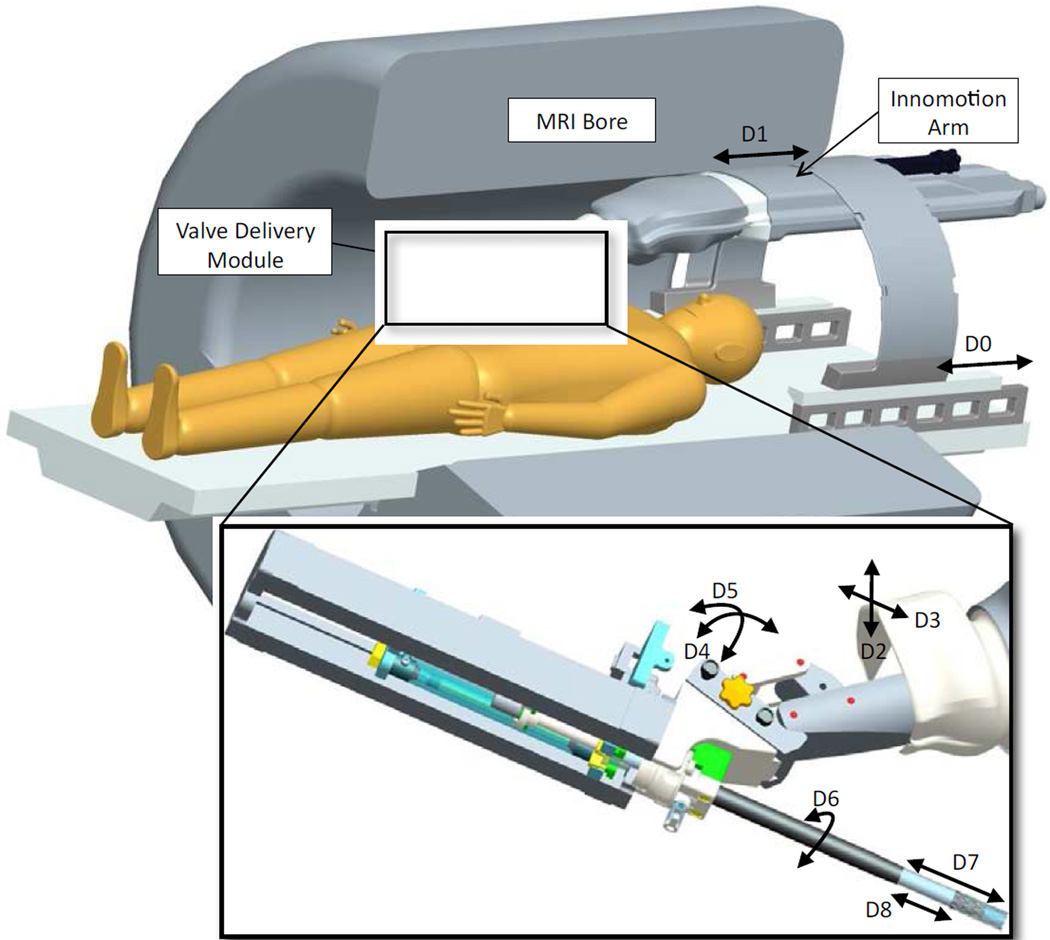
Robot Assistance System
An MRI compatible robotic surgical assistant system was developed to deliver the aortic valve prostheses.28, 29 The robotic assistance system consists of a positioning module,, a valve delivery module, custom designed software program, and a graphical user interface. The positioning module consists of a modified Innomotion MRI compatible robotic arm (Innomedic, Herxheim, Germany). The positioning module was used to hold the valve delivery module and to adjust the planned trajectory of the valve delivery device. The positioning module was modified to hold and manipulate the valve delivery module and has 5 degrees of freedom (DoF). These movements include axial, vertical and horizontal translation as well as pitch and yaw. The valve delivery module has 3 DoF, which includes roll, translation, and insertion of the delivery device. The valve delivery module was designed to work in conjunction with the robotic arm to insert and deploy the stent.23 The combination of the movements between the positioning module and valve delivery module include all the movements that a human would use when inserting and deploying the stent. In order to maintain image quality and prevent heat transfer to the patient, the valve delivery module was made from non-conductive plastic materials, pneumatic actuators and magnetotranslucent fiber-optical encoders. The profile of the valve delivery module and positioning module allow it to fit into a standard closed MRI scanner (Figure 2). The primary control computer used a custom software program to control the robotic system via an optic network. For precision with valve deployment, the accuracy of the linear joints was around one millimeter and the accuracy of the rotational joints was one degree. 30 The interactive control interface allows the user to plot the next move for the delivery device, such as increasing angulation or advancing the delivery device. While the robot is executing maneuver, the user can watch the device in real time. If any movement needs to be modified, the user can start, stop, change, or resume the delivery device motion at any time.
Figure 2.
Valve delivery module and robot platform in MRI bore with patient
Animal Surgery Protocol
All experiments were performed in accordance with the protocols approved by the National Institutes of Health Animal Care and Use Committee. Induction included an intramuscular injection of Midazolam (0.5 mg/kg) and Ketamine (25mg/kg). After induction, the animals were intubated and then maintained on mechanical ventilation with Isoflurane (0.5–2.5%). The animals end tidal carbon dioxide, oxygen saturation, arterial blood pressure, and electrocardiographic telemetry were monitored throughout the entire procedure. The animal’s body temperature was maintained with a forced-air warming blanket. Prior the start of the procedure, the animals received intravenous Amiodarone (150mg-300mg) for antiarrhythmic treatment and prior to trocar insertion they were anticoagualted with heparin (300 units/kg). After completion of the experiment, the fully anesthetized animals were euthanized with an intravenous injection of phenobarbital (150mg/kg). We recorded the times and details of the procedures.
Valve Deployment
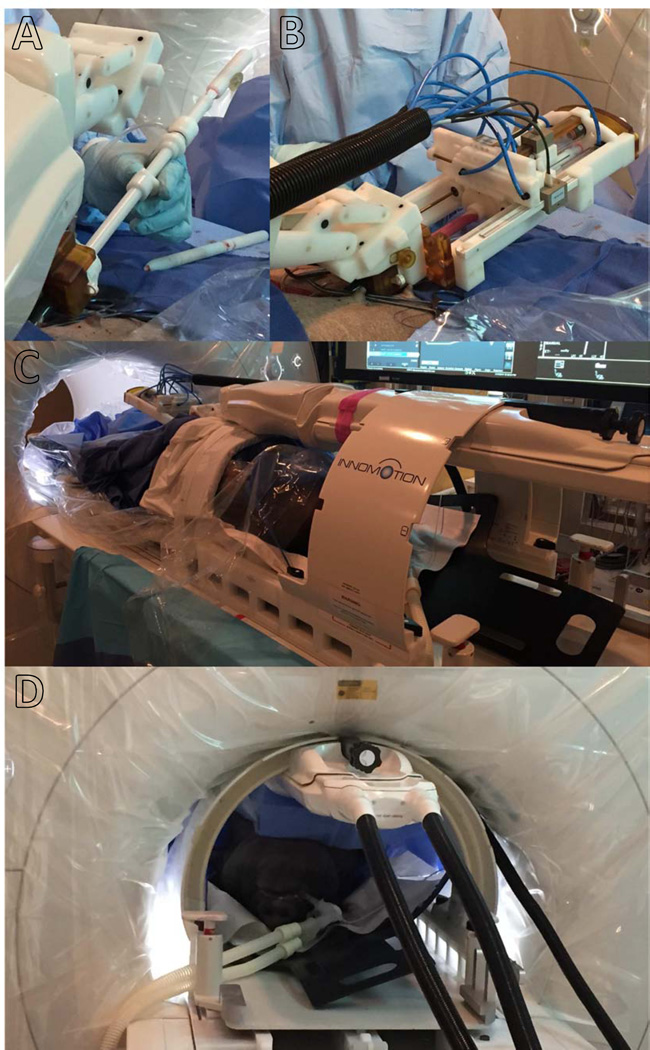
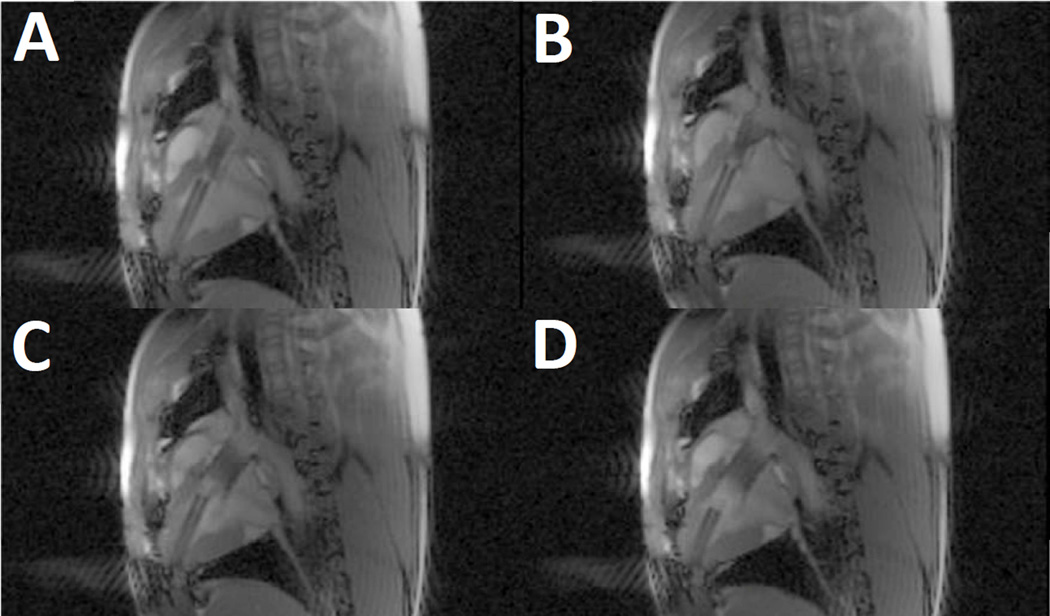
Eight swine weighing between 45 and 55 kg underwent robot-assisted rtMRI-guided TAVR. The animals were sedated and intubated, then prepped and draped in a supine position. A 6cm subxiphoid incision was made and the pericardium was opened. Two concentric purse string sutures were placed around the apex of the heart. An incision was made in the apex and a 12mm trocar was inserted. The swine were then transferred to the MRI and a surface radiofrequency coil was secured to the anterior chest to enhance signal reception. The delivery device was loaded with the stent and the stent and delivery device were inserted into the opening of the trocar (Figure 3a). The positioning module and valve delivery module were then affixed to the MRI table and the delivery device was attached to the valve delivery module (Figure 3b, 3c). The MRI table with the robot and animal were then moved into the bore (Figure 3d). A pre-deployment scan was performed to confirm annulus and aortic root size and so the physician could plan the trajectory of the delivery device. For deployment, two imaging planes (long axis view and short axis view) were used to create a virtual real time three-dimensional reconstruction. The physician was able to adjust the delivery device during insertion and deploy the stent with the robot system via the graphical user interface and software program. The axial slices were shifted as needed to visualize the delivery device and maintain proper orientation for stent delivery. Under rtMRI guidance, the delivery device was advanced until it was across the aortic valve (Figure 4a). Once the delivery device reached the proper position, the device was slowly deployed (Figure 4b). While the stent was partially deployed, the physician could reposition the valve if needed to ensure correct and precise placement. Once the valve was deployed (Figure 4c), the delivery catheter system was withdrawn from the trocar (Figure 4d). Post-deployment images were acquired to confirm the position of the prostheses. Gated CINE-MRI was used to assess valve placement. A necropsy was performed on all animals following valve placement to grossly assess valve placement.17, 21, 23, 31
Figure 3.
(a) Insertion of delivery device and nitinol stent; (b) valve delivery module mounted on robotic arm; (c) patient and robot platform; (d) patient and robot platform in MRI scanner.
Figure 4.
Valve deployment from the delivery device. (a) Delivery device advanced across aortic valve; (b) sheath retracting to deploy valve; (c) valve deployed; (d) delivery device backing out.
RESULTS
In an acute, non-survival study, eight swine underwent success robot-assisted rtMRI TAVR for evaluation of feasibility. The subxiphoid incision with trocar placement was 18 minutes +/− 6 minutes. The pre-deployment scan was used to measure the annulus and aortic root size and to plan the trajectory of the delivery device. The annulus sizes were 24mm +/− 3mm. Our custom-designed self-expanding stent with an expanded diameter of 26mm and length of 35mm was used for all eight experiments. There were no issues with stent deployment. The time for deploying the valve under rtMRI guidance was 61 seconds +/− 5 seconds. The post-deployment scans confirmed precise stent placement at 4mm below the annulus in all eight experiments. Post-deployment necropsy confirmed the correlation between imaging and the actual valve position (Figure 5). On necropsy, all eight animals had apposition of the bioprosthesis to the annulus and ascending aorta. All stents were deployed with the proximal end positioned 0 to 3mm below the annulus and without occluding the coronary ostia.
Figure 5.
Necropy showing valve placement.
DISCUSSION
rtMRI has improved soft tissue contrast in addition to a three dimensional visualization of the anatomic structures, unlike traditional imaging for TAVR. In addition rtMRI avoids radiation exposure and contrast media. X-ray fluoroscopy exposes the patients and medical staff to significant doses of ionizing radiation, while rtMRI uses non-ionizing radiation, which has no known deleterious effects to health.32 Unlike fluoroscopy, rtMRI guidance does not require the use of contrast media to aid in visualization.15–17 Contrast media can lead to multiple complications, such as contrast-induced nephropathy and anaphylaxis.33 Gadolinium can be used in a post-deployment, first-pass perfusion to evaluate myocardial perfusion, but it is not required for the procedure.34 rtMRI guidance may be useful for TAVR patients with renal insufficiency, which is a contraindication to the procedure.18, 35
Traditional imaging for TAVR requires multiple imaging modalities; however, we have demonstrated in our previous experiments that rtMRI can be utilized as the only imaging modality for pre-deployment imaging, imaging guidance for valve deployment, and post-deployment scanning in TAVR procedures with a high accuracy of device delivery and reproducibility.17, 22, 23, 36–39 Although rtMRI guided TAVR has come closer to a clinical reality, one of the limitations we realized during our multiple experiments is the difficulty of performing the procedure in the confines of an MRI suite and working inside the bore of an MRI machine. This led us to develop an MRI compatible robot-assisted device to aid in deployment. Our experiment has demonstrated the feasibility of using this device for transapical rtMRI guided TAVR. However, there are some limitations to this delivery method.
Some of the limitations of rtMRI imaging and robot assistance include non-MRI compatible implants, complexity and cost of delivery method, device deployment limitations, and effectiveness of our self-expanding nitinol stent. Unlike fluoroscopy and CT, the continuous interaction between an MRI’s magnetic field with ferromagnetic materials lead to potential movement and heating of metallic objects. This can lead to tissue damage as well as damage to electronic circuits. Because of this, patients must be carefully screened prior to rtMRI procedures. Imaging of patients with non-MRI compatible implants such as some implanted cardiac devices is contraindicated. 40–42 Patients with non-MRI compatible implants would be excluded from rtMRI guided TAVR. Another limitation is the complexity and resources that would be required to develop and run a robot-TAVR program. We realize the costs of hybrid MRI suites as well as a robotic delivery device would limit its use to only major centers with high-volume TAVR procedures. The device itself also has several limitations. In its current configuration, the robot assistance system is currently configured for a transapical approach. The device currently cannot advance a guidewire, so it is not able to perform a TAVR from a femoral, subclavian, or axillary access sites. Another limitation was stent migration between post-deployment perfusion and necropsy. All eight stents were precisely deployed at 4mm below the annulus and position was confirmed on post-deployment imaging. However, between post-deployment imaging and necropsy, the stents moved in position between 1mm and 4mm, this could be due the valve design, size mismatch, or the valve shifting during harvest for necropsy. While we are unsure of the exact variable which led to movement, we do know that between deployment and post-deployment imaging, all eight stents were deployed with millimeter precision.
CONCLUSIONS
These results demonstrate the feasibility of robotic assisted TAVR using rtMRI guidance. rtMRI guidance is unique in that this single imaging modality can be successfully utilized for pre-deployment, deployment, and post-deployment imaging; however, performing a TAVR while working in the confines of an MRI bore is an challenging task. rtMRI eliminates the deleterious side effects of traditional imaging for TAVR, which includes radiation exposure and contrast media. Our approach, by using a robotic system, may eliminate some of the challenges and may improve the success of TAVR. It provides superior visualization during the insertion process, deployment with pinpoint accuracy, and potentially communication between the imaging device and the robotic module which will prevent incorrect or misaligned deployment.
Perspective Statement.
Real-time MRI guided TAVR overcomes the limitations of the current imaging modalities. However, performing a TAVR in a MRI scanner can be a difficult task due to limited space. We designed a robot-assisted device to deploy a self-expanding valve. This method provides superior visualization, deployment with pinpoint accuracy, and can prevent misaligned deployment.
Central Message.
We show the feasibility of robot-assisted real-time MRI guided TAVR, which has benefits over current imaging and delivery technologies.
Acknowledgments
Funding: This research received funding from intramural NHLBI
Glossary of Abbreviations
- CT
Computed tomography
- MDCT
Multidetector computed tomography
- rtMRI
Real-time magnetic resonance image
- TAVR
Transcatheter aortic valve replacement
- TEE
Transesophageal echocardiography
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflicts of Interest: no potential conflicts exist for all authors
REFERENCES
- 1.Maganti K, Rigolin VH, Sarano ME, Bonow RO. Valvular heart disease: diagnosis and management. Mayo Clinic proceedings. 2010;85:483–500. doi: 10.4065/mcp.2009.0706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Coffey S, Cox B, Williams MJ. The prevalence, incidence, progression, and risks of aortic valve sclerosis: a systematic review and meta-analysis. Journal of the American College of Cardiology. 2014;63:2852–2861. doi: 10.1016/j.jacc.2014.04.018. [DOI] [PubMed] [Google Scholar]
- 3.Nkomo VT, Gardin JM, Skelton TN, Gottdiener JS, Scott CG, Enriquez-Sarano M. Burden of valvular heart diseases: a population-based study. Lancet. 2006;368:1005–1011. doi: 10.1016/S0140-6736(06)69208-8. [DOI] [PubMed] [Google Scholar]
- 4.Carabello BA. Introduction to aortic stenosis. Circulation research. 2013;113:179–185. doi: 10.1161/CIRCRESAHA.113.300156. [DOI] [PubMed] [Google Scholar]
- 5.Ross J, Jr, Braunwald E. Aortic stenosis. Circulation. 1968;38:61–67. doi: 10.1161/01.cir.38.1s5.v-61. [DOI] [PubMed] [Google Scholar]
- 6.Turina J, Hess OM, Krayenbuhl HP. [Spontaneous course of aortic valve disease and indications for aortic valve replacement] Schweizerische medizinische Wochenschrift. 1988;118:508–516. [PubMed] [Google Scholar]
- 7.Leon MB, Smith CR, Mack M, Miller DC, Moses JW, Svensson LG, Tuzcu EM, Webb JG, Fontana GP, Makkar RR, Brown DL, Block PC, Guyton RA, Pichard AD, Bavaria JE, Herrmann HC, Douglas PS, Petersen JL, Akin JJ, Anderson WN, Wang D, Pocock S. Transcatheter Aortic-Valve Implantation for Aortic Stenosis in Patients Who Cannot Undergo Surgery. New England Journal of Medicine. 2010;363:1597–1607. doi: 10.1056/NEJMoa1008232. [DOI] [PubMed] [Google Scholar]
- 8.Leon MB, Smith CR, Mack M, Miller DC, Moses JW, Svensson LG, Tuzcu EM, Webb JG, Fontana GP, Makkar RR, Brown DL, Block PC, Guyton RA, Pichard AD, Bavaria JE, Herrmann HC, Douglas PS, Petersen JL, Akin JJ, Anderson WN, Wang D, Pocock S. Transcatheter aortic-valve implantation for aortic stenosis in patients who cannot undergo surgery. The New England journal of medicine. 2010;363:1597–1607. doi: 10.1056/NEJMoa1008232. [DOI] [PubMed] [Google Scholar]
- 9.Saeedi M, Thomas A, Shellock FG. Evaluation of MRI issues at 3-Tesla for a transcatheter aortic valve replacement (TAVR) bioprosthesis. Magnetic resonance imaging. 2015 doi: 10.1016/j.mri.2015.01.012. [DOI] [PubMed] [Google Scholar]
- 10.Bloomfield GS, Gillam LD, Hahn RT, Kapadia S, Leipsic J, Lerakis S, Tuzcu M, Douglas PS. A practical guide to multimodality imaging of transcatheter aortic valve replacement. JACC Cardiovasc Imaging. 2012;5:441–455. doi: 10.1016/j.jcmg.2011.12.013. [DOI] [PubMed] [Google Scholar]
- 11.Hahn RT. Use of imaging for procedural guidance during transcatheter aortic valve replacement. Curr Opin Cardiol. 2013;28:512–517. doi: 10.1097/HCO.0b013e3283632b5e. [DOI] [PubMed] [Google Scholar]
- 12.Jilaihawi H, Kashif M, Fontana G, Furugen A, Shiota T, Friede G, Makhija R, Doctor N, Leon MB, Makkar RR. Cross-sectional computed tomographic assessment improves accuracy of aortic annular sizing for transcatheter aortic valve replacement and reduces the incidence of paravalvular aortic regurgitation. J Am Coll Cardiol. 2012;59:1275–1286. doi: 10.1016/j.jacc.2011.11.045. [DOI] [PubMed] [Google Scholar]
- 13.Husser O, Holzamer A, Resch M, Endemann DH, Nunez J, Bodi V, Schmid C, Riegger GA, Gossmann H, Hamer O, Stroszczynski C, Luchner A, Hilker M, Hengstenberg C. Prosthesis sizing for transcatheter aortic valve implantation--comparison of three dimensional transesophageal echocardiography with multislice computed tomography. Int J Cardiol. 2013;168:3431–3438. doi: 10.1016/j.ijcard.2013.04.182. [DOI] [PubMed] [Google Scholar]
- 14.Smith LA, Dworakowski R, Bhan A, Delithanasis I, Hancock J, Maccarthy PA, Wendler O, Thomas MR, Monaghan MJ. Real-time three-dimensional transesophageal echocardiography adds value to transcatheter aortic valve implantation. J Am Soc Echocardiogr. 2013;26:359–369. doi: 10.1016/j.echo.2013.01.014. [DOI] [PubMed] [Google Scholar]
- 15.McCullough PA, Wolyn R, Rocher LL, Levin RN, O'Neill WW. Acute renal failure after coronary intervention: incidence, risk factors, and relationship to mortality. The American journal of medicine. 1997;103:368–375. doi: 10.1016/s0002-9343(97)00150-2. [DOI] [PubMed] [Google Scholar]
- 16.Bruschi G, De Marco F, Martinelli L, Klugmann S. CoreValve(R) transcatheter self-expandable aortic bioprosthesis. Expert review of medical devices. 2013;10:15–26. doi: 10.1586/erd.12.64. [DOI] [PubMed] [Google Scholar]
- 17.Horvath KA, Mazilu D, Guttman M, Zetts A, Hunt T, Li M. Midterm results of transapical aortic valve replacement via real-time magnetic resonance imaging guidance. J Thorac Cardiovasc Surg. 2010;139:424–430. doi: 10.1016/j.jtcvs.2009.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Horvath KA, Mazilu D, Cai J, Kindzelski B, Li M. Transapical sutureless aortic valve implantation under magnetic resonance imaging guidance: Acute and short-term results. J Thorac Cardiovasc Surg. 2015;149:1067–1072. doi: 10.1016/j.jtcvs.2014.10.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Saeed M, Hetts SW, English J, Wilson M. MR fluoroscopy in vascular and cardiac interventions (review) The international journal of cardiovascular imaging. 2012;28:117–137. doi: 10.1007/s10554-010-9774-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Roberts TP, Hassenzahl WV, Hetts SW, Arenson RL. Remote control of catheter tip deflection: an opportunity for interventional MRI. Magnetic resonance in medicine : official journal of the Society of Magnetic Resonance in Medicine / Society of Magnetic Resonance in Medicine. 2002;48:1091–1095. doi: 10.1002/mrm.10325. [DOI] [PubMed] [Google Scholar]
- 21.Guttman MA, Kellman P, Dick AJ, Lederman RJ, McVeigh ER. Real-time accelerated interactive MRI with adaptive TSENSE and UNFOLD. Magn Reson Med. 2003;50:315–321. doi: 10.1002/mrm.10504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.McVeigh ER, Guttman MA, Lederman RJ, Li M, Kocaturk O, Hunt T, Kozlov S, Horvath KA. Real-time interactive MRI-guided cardiac surgery: aortic valve replacement using a direct apical approach. Magnetic resonance in medicine : official journal of the Society of Magnetic Resonance in Medicine / Society of Magnetic Resonance in Medicine. 2006;56:958–964. doi: 10.1002/mrm.21044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Horvath KA, Guttman M, Li M, Lederman RJ, Mazilu D, Kocaturk O, Karmarkar PV, Hunt T, Kozlov S, McVeigh ER. Beating heart aortic valve replacement using real-time MRI guidance. Innovations (Phila) 2007;2:51–55. doi: 10.1097/IMI.0b013e31805b8280. [DOI] [PubMed] [Google Scholar]
- 24.Horvath KA, Li M, Mazilu D, Guttman MA, McVeigh ER. Real-time magnetic resonance imaging guidance for cardiovascular procedures. Seminars in thoracic and cardiovascular surgery. 2007;19:330–335. doi: 10.1053/j.semtcvs.2007.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lederman RJ. Cardiovascular interventional magnetic resonance imaging. Circulation. 2005;112:3009–3017. doi: 10.1161/CIRCULATIONAHA.104.531368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Horvath K, Mazilu D, Li M. Stent for valve replacement. 2012 [Google Scholar]
- 27.Mazilu D, Li M, Kocaturk O, Horvath KA. Self-Expanding Stent and Delivery System for Aortic Valve Replacement. J Med Device. 2012;6:410061–410069. doi: 10.1115/1.4007750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Li M, Mazilu D, Horvath KA. Robotic system for transapical aortic valve replacement with MRI guidance. Med Image Comput Comput Assist Interv. 2008;11:476–484. doi: 10.1007/978-3-540-85990-1_57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Li M, Kapoor A, Mazilu D, Horvath KA. Pneumatic actuated robotic assistant system for aortic valve replacement under MRI guidance. IEEE Trans Biomed Eng. 2011;58:443–451. doi: 10.1109/TBME.2010.2089983. [DOI] [PubMed] [Google Scholar]
- 30.Kapoor A, Wood B, Mazilu D, Horvath KA, Li M. MRI-compatible Hands-on Cooperative Control of a Pneumatically Actuated Robot. IEEE Int Conf Robot Autom. 2009;2009:2681–2686. doi: 10.1109/ROBOT.2009.5152541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Horvath KA, Mazilu D, Cai J, Kindzelski B, Li M. Transapical sutureless aortic valve implantation under magnetic resonance imaging guidance: Acute and short-term results. The Journal of thoracic and cardiovascular surgery. 2014 doi: 10.1016/j.jtcvs.2014.10.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tsekos NV, Khanicheh A, Christoforou E, Mavroidis C. Magnetic resonance-compatible robotic and mechatronics systems for image-guided interventions and rehabilitation: a review study. Annual review of biomedical engineering. 2007;9:351–387. doi: 10.1146/annurev.bioeng.9.121806.160642. [DOI] [PubMed] [Google Scholar]
- 33.Hong SJ, Wong JT, Bloch KJ. Reactions to radiocontrast media. Allergy and asthma proceedings : the official journal of regional and state allergy societies. 2002;23:347–351. [PubMed] [Google Scholar]
- 34.Quail MA, Nordmeyer J, Schievano S, Reinthaler M, Mullen MJ, Taylor AM. Use of cardiovascular magnetic resonance imaging for TAVR assessment in patients with bioprosthetic aortic valves: comparison with computed tomography. European journal of radiology. 2012;81:3912–3917. doi: 10.1016/j.ejrad.2012.07.014. [DOI] [PubMed] [Google Scholar]
- 35.Al-Lamee R, Godino C, Colombo A. Transcatheter aortic valve implantation: current principles of patient and technique selection and future perspectives. Circ Cardiovasc Interv. 2011;4:387–395. doi: 10.1161/CIRCINTERVENTIONS.111.961128. [DOI] [PubMed] [Google Scholar]
- 36.Kahlert P, Parohl N, Albert J, Schafer L, Reinhardt R, Kaiser GM, McDougall I, Decker B, Plicht B, Erbel R, Eggebrecht H, Ladd ME, Quick HH. Towards real-time cardiovascular magnetic resonance guided transarterial CoreValve implantation: in vivo evaluation in swine. J Cardiovasc Magn Reson. 2012;14:21. doi: 10.1186/1532-429X-14-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kahlert P, Eggebrecht H, Plicht B, Kraff O, McDougall I, Decker B, Erbel R, Ladd ME, Quick HH. Towards real-time cardiovascular magnetic resonance-guided transarterial aortic valve implantation: in vitro evaluation and modification of existing devices. J Cardiovasc Magn Reson. 2010;12:58. doi: 10.1186/1532-429X-12-58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Horvath KA, Mazilu D, Kocaturk O, Li M. Transapical aortic valve replacement under real-time magnetic resonance imaging guidance: experimental results with balloon-expandable and self-expanding stents. Eur J Cardiothorac Surg. 2011;39:822–828. doi: 10.1016/j.ejcts.2010.09.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kindzelski BA, Li M, Mazilu D, Hunt T, Horvath KA. Real-time magnetic resonance-guided aortic valve replacement using Engager valve. Ann Thorac Surg. 2014;98:2194–2199. doi: 10.1016/j.athoracsur.2014.09.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kanal E, Borgstede JP, Barkovich AJ, Bell C, Bradley WG, Etheridge S, Felmlee JP, Froelich JW, Hayden J, Kaminski EM, Lester JW, Jr, Scoumis EA, Zaremba LA, Zinninger MD. American College of Radiology White Paper on MR Safety: 2004 update and revisions. AJR American journal of roentgenology. 2004;182:1111–1114. doi: 10.2214/ajr.182.5.1821111. [DOI] [PubMed] [Google Scholar]
- 41.Pohost GM. Editor's page: is CMR safe? J Cardiovasc Magn Reson. 2001;3:ix. doi: 10.1081/jcmr-100107464. [DOI] [PubMed] [Google Scholar]
- 42.Sierra M, Machado C. Magnetic resonance imaging in patients with implantable cardiac devices. Reviews in cardiovascular medicine. 2008;9:232–238. [PubMed] [Google Scholar]