Abstract
Objective. To examine the use of individual care plans (ICPs) within primary chronic illness care in the Netherlands, and to explore the relationships between ICP use, patient characteristics, and patient-perceived quality of care. Design. Cross-sectional study using survey data from a panel of chronically ill patients and medical registration data provided by their general practices. Setting and subjects. A sample of 1377 patients with somatic chronic disease(s) randomly selected in general practices throughout the Netherlands, supplemented with a sample of 225 COPD patients, also recruited from general practices. Main outcome measures. (i) Percentage of ICP use based on self-report by chronically ill patients, and (ii) patient-perceived quality of care as assessed using the Patient Assessment of Chronic Illness Care (PACIC). Results. ICP use among the total generic sample was low (9%), but slightly higher (13%) among patients diagnosed with diabetes or COPD, diseases for which disease management programmes have been set up in the Netherlands. Patients with a low educational level and patients with poor(er) self-rated health were more likely to have an ICP. Compared with patients without an ICP, patients with an ICP more often reported that the care they received was patient-centred, proactive, planned, and included collaborative goal setting, problem-solving, and follow-up support. Conclusion and implications. Findings reveal a discrepancy between practice and policy aspirations regarding ICP use in primary chronic illness care. More research is needed to gain insight into the effectiveness of ICPs to improve the quality of chronic illness care in various patient populations.
Keywords: Chronic disease, chronic obstructive pulmonary disease, diabetes mellitus, disease management, general practice, patient care planning, quality of health care, the Netherlands
There is limited knowledge on the use of individual care plans (ICPs) in primary care and the effects of ICPs on the quality of care.
ICP use among chronically ill patients within primary care in the Netherlands is low (less than 10% reported having an ICP in 2011).
Findings suggest that ICPs are more often employed for patients who have a less favourable social background and health.
Patients with an ICP more often feel that the delivered care is structured according to the principles of the Chronic Care Model, compared with patients without an ICP.
Introduction
Several countries have introduced individual care plans (ICPs) in chronic illness care [1–6]. ICPs are intended to help provide chronically ill patients with proactive, holistic, coordinated care that is tailored to their needs and preferences [7]. The starting points of ICPs are the goals that patients and their healthcare provider(s) mutually agree on. Healthcare providers coach patients on achieving these goals and support patients’ self-management. Working with ICPs is expected to improve the quality of chronic illness care, which will subsequently lead to improved health outcomes and quality of life, and reduced healthcare utilization [7].
In the Netherlands, ICPs were introduced as part of the chronic disease management approach that was adopted for several chronic diseases within primary care [3]. Disease management was first introduced for patients with diabetes mellitus (2007), and at a later stage for patients with cardiovascular disease as well as those with a high risk of developing cardiovascular disease (2009) and patients with COPD (2010). In 2012, the Dutch Health Care Inspectorate concluded that ICPs were still hardly used by diabetes care groups within primary care [8]. This conclusion is in line with other (small-scale) studies, which estimate that no more than 10% of Dutch patients with diabetes mellitus type 2 had an ICP [9,10]. There are signs to indicate that the level of ICP implementation is also low in Norway and the United Kingdom [2,11].
Studies (mostly qualitative studies) have identified a complex set of barriers and facilitators related to the organization of healthcare, and characteristics of healthcare providers and patients [11–14]. Recent research among four diabetes care groups (109 general practitioners [GPs]) in the Netherlands showed that GPs especially consider a patient's older age and lack of skills when it comes to discouraging ICP use, in addition to a lack of time on their part [9]. This suggests that ICPs are less often employed for more vulnerable patients. However, in England Burt and colleagues found that more vulnerable patients, i.e. patients living in deprived areas and patients reporting poor health, more often had an ICP [11].
The study by Burt et al. showed positive relationships between patients’ reporting of ICPs and better perceived access, continuity of care, and interpersonal care [11]. However, until now there has been only limited quantitative evidence that using ICPs could improve the quality of chronic illness care.
To increase our knowledge of ICP use in primary care, the present study aimed to:
provide a picture of the nationwide level of ICP implementation in primary chronic illness care in the Netherlands;
gain insight into patient characteristics related to ICP use;
explore the relationship between (patient-reported) ICP use and patient-perceived quality of chronic illness care.
Material and methods
Sample
A nationwide sample of adult, non-institutionalized patients with somatic chronic disease(s) was derived from a prospective panel-study in the Netherlands [15]. Each year panel members are recruited from (random samples of) general practices throughout the country, via a standardized procedure (see [15] for a description of this procedure). Panel members participate in two or three surveys a year, for a maximum of four years. Survey topics are self-rated health, use of healthcare, perceived quality of care, and quality of life. The panel-study is registered with the Dutch Data Protection Authority; all data are collected and handled according to the privacy protection guidelines of the Authority.
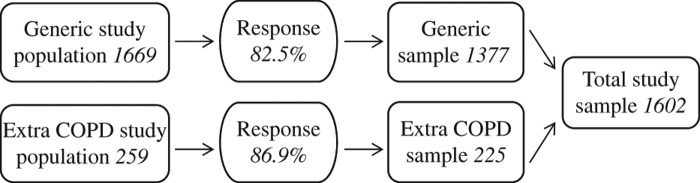
In April 2011, the panel consisted of 1669 patients diagnosed with all types of somatic chronic disease(s), recruited in 2007 to 2010. Of this sample 1377 persons filled in either a postal (n = 1336) or internet (n = 41) questionnaire (response rate 83%). Additionally 225 of 259 COPD patients, who had been recruited from general practices from 2007 till early in 2011 via the same standardized procedure for a disease-specific study, participated in the same survey (response rate 87%). Hence, the total group of participants for this study comprised 1602 chronically ill patients derived from 82 general practices (Figure 1).
Figure 1.
Flowchart study sample.
Data
Outcome measures. Patients indicated whether or not they had an ICP for the management of their chronic disease(s): yes/no. The question was preceded by a short explanation of what is meant by the term ICP.
The Patient Assessment of Chronic Illness Care questionnaire (PACIC) [16] was included to assess the extent to which patients receive care that aligns with the Chronic Care Model (CCM) [17]. The PACIC distinguishes five dimensions of chronic illness care: patient activation, delivery system design/decision support, goal setting, problem-solving/contextual counselling, follow-up/coordination. The 20 items are scored on a five-point scale, from 1 (never) to 5 (always). Scale scores (total and subscales) are computed by averaging the items completed within the (sub)scale. Missing values are replaced by the respondent's mean value of the other items belonging to the (sub)scale, in the case where the respondent filled in at least 50% of the items of a (sub)scale. High scores indicate that the delivered care is perceived as structured according to the principles of the CCM from the patient's perspective.
Patient characteristics. Socio-demographic characteristics included gender, age, and educational level. Patients’ self-reported educational level reflected the highest level of education completed and was classified as low (no, primary, or lower vocational education), intermediate (secondary or intermediate vocational education) and high (higher vocational education or university).
Health literacy was assessed using a brief screening instrument [18], containing three questions: “How often do you have someone help you read materials from your hospital, GP or other health care institutions?”, “How confident are you filling out medical forms by yourself?”, and ‘How often do you have problems learning about your medical condition because of difficulty understanding written information?” These items are scored on a five-point scale (0–4). The scale score is computed by averaging the items within the scale. Missing values are replaced by the sample's mean value of the item, in the case of respondents having only one of the three items missing. A score of ≤ 2 indicates inadequate health literacy.
GPs provided data on the chronic disease(s) diagnosed (coded according to the International Classification of Primary Care [19]). Based on these data, we computed the number of chronic diseases per patient.
Self-rated health was based on the first item of the RAND-36: “In general, would you say your health is: 1 = excellent, 2 = very good, 3 = good, 4 = fair, 5 = poor” [20,21].
Statistical analyses. Statistical analyses were performed in Stata™ version 12 (StataCorp, College Station, TX, USA) [22]. To assess the level of implementation of ICPs, percentages and 95% confidence intervals of patients reporting an ICP among the generic sample were computed. In addition, percentages of patients reporting an ICP were calculated for different diagnostic groups and for patients with one chronic disease or with multimorbidity (i.e. being diagnosed with two or more chronic diseases).
To assess whether certain patient characteristics were associated with ICP use, multi-level logistic regression analysis [23] was conducted with data from the total sample. Two models were estimated: a null model taking into account the variance in ICP use between general practices (random part) and a main model in which several patient characteristics (age, educational level, health literacy, type and number of chronic diseases, self-rated health) were added to the fixed part of the model. For the variables in the fixed part, odds ratios with 95% confidence intervals are presented. For the random part, the variance at GP level with the standard error is presented.
To explore the relationship between (patient-reported) ICP use and PACIC scores, two-sample t-tests were conducted with data from the total sample.
Results
Sample characteristics
Characteristics of the generic sample of patients with a chronic illness and of the extra sample of COPD patients are outlined in Table I.
Table I.
Characteristics of the generic sample of patients with chronic somatic illness (n = 1377) and the extra sample of patients diagnosed with COPD (n = 225).
| Generic sample | Additional sample of COPD patients | |||
|---|---|---|---|---|
| n | % | n | % | |
| Patient characteristics: | ||||
| Gender | ||||
| Male | 632 | 46 | 131 | 58 |
| Female | 745 | 54 | 94 | 42 |
| Age: | ||||
| 15–39 years | 69 | 5 | 0 | 0 |
| 40–64 years | 639 | 46 | 91 | 40 |
| 65–74 years | 383 | 28 | 79 | 35 |
| ≥ 75 years | 286 | 21 | 55 | 25 |
| Educational level: | ||||
| Low | 489 | 36 | 119 | 53 |
| Intermediate | 549 | 41 | 71 | 32 |
| High Health literacy:1 |
309 | 23 | 33 | 15 |
| Inadequate | 102 | 8 | 20 | 9 |
| Adequate | 1229 | 92 | 195 | 91 |
| Type of chronic disease diagnosed:2 | ||||
| Asthma | 159 | 12 | 20 | 9 |
| COPD | 146 | 11 | 225 | 100 |
| Other chronic respiratory disease | 70 | 5 | 5 | 2 |
| Cardiovascular disease/high risk | 403 | 29 | 51 | 23 |
| Arthritis | 219 | 16 | 11 | 5 |
| Other chronic musculoskeletal disorder | 136 | 10 | 7 | 3 |
| Cancer | 132 | 10 | 5 | 2 |
| Diabetes mellitus | 332 | 24 | 21 | 9 |
| Thyroid dysfunction | 115 | 8 | 7 | 3 |
| Migraine | 63 | 5 | 1 | 0 |
| Neurological disease | 78 | 6 | 3 | 1 |
| Chronic digestive disorder | 91 | 7 | 8 | 4 |
| Chronic skin disease | 113 | 8 | 4 | 2 |
| Other chronic disease | 225 | 16 | 15 | 7 |
| Number of chronic diseases diagnosed: | ||||
| One | 714 | 52 | 113 | 50 |
| Two | 397 | 29 | 72 | 32 |
| Three or more | 266 | 19 | 40 | 18 |
| Self-rated general health: | ||||
| Excellent | 29 | 2 | 2 | 1 |
| Very good | 136 | 10 | 11 | 5 |
| Good | 735 | 54 | 111 | 49 |
| Fair | 424 | 31 | 85 | 38 |
| Poor | 45 | 3 | 16 | 7 |
Notes: 1Cronbach's alpha was 0.72, indicating good internal consistency. 2Since a proportion of the patients had been diagnosed with more than one chronic disease, these percentages sum up to more than 100.
ICP use
Of the total generic sample answering the question (n = 1234), 9% (95% CI 7–10) reported having an ICP. The use of ICPs among different diagnostic groups varied between 4% (patients with migraine) and 14% (patients with neurological diseases). Among diagnostic groups for which disease management programmes had been developed (before 2011), the proportions of patients reporting an ICP were 13% (diabetes, COPD) and 9% (cardiovascular disease/high risk). Of the patients diagnosed with one chronic disease 8% had an ICP; among those with multimorbidity the figure was 11%.
Patient characteristics associated with ICP use
Table II, model 1 shows that some patient characteristics significantly relate to ICP use. Patients diagnosed with COPD, diabetes mellitus, or another (unspecified) chronic disease are more likely to have an ICP. Furthermore, patients with a low level of education (compared with patients with a high level of education) and patients with poor(er) self-rated health are more likely to have an ICP.
Table II.
Multilevel logistic regression models to estimate ICP use among chronically ill patients within general practice (n = 1371).
| Model 0 | Model 1 | ||
|---|---|---|---|
| Fixed part | OR (95% CI) | SE | |
| Age, years (ref. 15–64 years): | |||
| 65–74 years | 0.84 (0.54–1.31) | 0.19 | |
| ≥ 75 years | 0.86 (0.52–1.41) | 0.22 | |
| Educational level (ref. = low): | |||
| Intermediate | 1.20 (0.80–1.81) | 0.25 | |
| High | 0.50 (0.27–0.94)* | 0.16 | |
| Health literacy: adequate (ref. = inadequate) | 0.66 (0.37–1.17) | 0.19 | |
| Type of chronic disease diagnosed (ref. = absence of specific disease): | |||
| Asthma | 0.95 (0.47–1.89) | 0.33 | |
| COPD | 1.74 (1.01–2.98)* | 0.48 | |
| Other chronic respiratory disease | 1.39 (0.54–3.54) | 0.66 | |
| Cardiovascular disease / high risk | 1.05 (0.61–1.80) | 0.29 | |
| Arthritis | 0.97 (0.52–1.82) | 0.31 | |
| Other chronic musculoskeletal disorder | 1.42 (0.72–2.80) | 0.49 | |
| Cancer | 1.01 (0.47–2.18) | 0.40 | |
| Diabetes mellitus | 1.78 (1.06–2.98)* | 0.47 | |
| Thyroid dysfunction | 1.12 (0.54–2.35) | 0.42 | |
| Migraine | 0.43 (0.10–1.86) | 0.32 | |
| Neurological disease | 1.76 (0.81–3.84) | 0.70 | |
| Chronic digestive disorder | 1.18 (0.50–2.78) | 0.52 | |
| Chronic skin disease | 0.79 (0.31–1.98) | 0.37 | |
| Other chronic disease | 1.81 (1.05–3.14)* | 0.51 | |
| Multimorbidity present (ref. = absent) | 0.88 (0.47–1.64) | 0.28 | |
| Self-rated general health (ref. = excellent–very good) | |||
| Good | 4.16 (1.28–13.58)* | 2.51 | |
| Fair–poor | 5.51 (1.67–18.15)** | 3.35 |
| Random part | Estimate | SE | Estimate | SE |
|---|---|---|---|---|
| Variance between GP practices | 0.06 | 0.10 | 0.00 | 0.00 |
Notes: Significance levels: *p < 0.05; ** p < 0.01. OR = odds ratio; CI = confidence interval; SE = standard error.
Relationship between ICP use and perceived quality of care
Perceived quality of care was assessed with the PACIC. Cronbach's alpha for the total PACIC scale and the subscales in this study indicated good internal consistency (Table III). Significant differences exist between patients with and without an ICP regarding their PACIC scores (total scale and all five subscales; Table III), indicating that patients with an ICP more often have the experience that the care they receive is patient-centred, proactive, planned, and includes collaborative goal setting, problem-solving, and follow-up support than patients without an ICP.
Table III.
Mean PACIC scores of patients with and without an ICP and results of Student's t-tests for independent samples.
| α | Patients with ICP | Patients without ICP | t | df | p | |||
|---|---|---|---|---|---|---|---|---|
| M (SD) | n | M (SD) | n | |||||
| PACIC total score | 0.93 | 2.67 (1.00) | 116 | 1.94 (0.74) | 741 | –7.636 | 135.75 | < 0.001 |
| Patient activation | 0.83 | 3.33 (1.39) | 120 | 2.76 (1.38) | 764 | –4.210 | 882 | < 0.001 |
| Delivery system design/decision support | 0.68 | 3.19 (1.17) | 120 | 2.60 (1.06) | 757 | –5.622 | 875 | < 0.001 |
| Goal setting | 0.81 | 2.53 (1.15) | 116 | 1.81 (0.91) | 733 | –6.474 | 138.968 | < 0.001 |
| Problem-solving/contextual counselling | 0.93 | 2.85 (1.33) | 113 | 1.75 (1.05) | 713 | –8.331 | 135.206 | < 0.001 |
| Follow-up/coordination | 0.73 | 1.78 (0.91) | 110 | 1.36 (0.57) | 735 | –4.626 | 122.437 | < 0.001 |
Notes: M = mean; SD = standard deviation; t = t-value; df = degrees of freedom; p = significance level.
Discussion
The present study provides evidence that ICP use among chronically ill primary care patients in the Netherlands is low (9% in 2011). Patients with a low educational level and patients with poor(er) self-rated health were more likely to have an ICP. Responses from patients with an ICP showed that they more often feel that the provided care corresponds to the principles of the Chronic Care Model, compared with patients without an ICP.
Strengths and weaknesses
Data for this study were derived from a nationwide sample of patients diagnosed with chronic disease(s) in the Netherlands, which provides the opportunity to generalize our findings regarding ICP use to the Dutch population of non-institutionalized (somatic) chronically ill patients. It should, however, be noted that our findings were based on patients’ self- report. Patients might have misinterpreted the concept of ICP, which could have led to both under- and over-reporting. We tried to avoid misinterpretation by providing a short explanation in the questionnaire of what an ICP is or could look like. Nevertheless, some misunderstanding might have occurred.
Another issue is the cross-sectional design of the study, which does not allow causal interpretation. This means that our findings could indicate that the use of an ICP results in a perception of receiving chronic illness care of a higher quality, but it may also be the other way round. Moreover, there may be factors that lead people to report the use of an ICP, which may also increase the likelihood of people reporting that they have received higher quality chronic illness care. For instance, it is known that patients with a low educational level are generally more positive about the quality of the care they receive than patients with a high educational level [24,25], and in our study patients with a low level of education also more often reported the use of an ICP. On the other hand, it is also well known that patients with poor (self-rated) health are generally less positive about the care they receive than patients with better (self-rated) health [24,25], but in our study patients who rated their health more poorly reported using an ICP more frequently – instead of less frequently – than patients with better self-rated health. The latter finding strengthened our belief that asking patients to report the use of a (concrete) ICP does not evoke an entirely subjective answer that reflects their perception of the quality of care. Nevertheless, it is recommended that future research also makes use of other data sources concerning the use of ICPs (i.e. medical files, reports by healthcare professionals).
Discussion of main findings
Less than 10% of the total generic sample reported having an ICP in April 2011. This result is in line with findings from a study in the United Kingdom, where the National Health Service determined in 2008 that all people with one or more long-term conditions should be offered an ICP within two years [1]. Data from the 2009/2010 General Practice Patient Survey in England showed that only 12% of patients with a long-term condition reported having an ICP [11]. A low implementation level was also found in Norway, where ICPs were introduced in 2001 for patients with long-term and complex needs for coordinated care. Despite legal obligations and national initiatives by health authorities, five years after the introduction the use of ICPs was still low, particularly among general practitioners (GPs) [2].
Diagnostic groups for which disease management programmes have been developed in the Netherlands (before 2011) seem to have a slightly higher chance of having an ICP, though evidence for this was found only among diabetes and COPD patients and not among patients with (an increased risk of) cardiovascular disease, for which a disease management approach was also adopted. Even among patients with diabetes or COPD the proportions reporting an ICP were still low (13%), which supports the findings of previous studies that ICP use within diabetes care – which is considered a forerunner of the disease management approach in the Netherlands – lags behind policy aspirations. In England, where ICPs are also considered an important component of good diabetes care (according to standards of care), it was estimated that only one-third of all diabetic patients had an ICP in 2011 [26].
Current ICP use within primary care in the Netherlands seems to depend, to some extent, on the complexity of a patient's situation: patients with a low level of education and/or poor(er) self-rated health were more likely to report having an ICP. These findings suggest that ICPs are more often employed for patients who have a less favourable social background and health. This is in line with the findings of Burt et al. showing that ICPs are more often reported by patients living in areas of deprivation and patients reporting poorer health [11].
Burt and colleagues concluded that the low level of implementation might reflect uncertainty as to the benefits of ICPs [11]. This might also hold for the Dutch situation: in a previous study we found that both diabetes care providers and type 2 diabetics are not yet convinced of the benefits of ICP use [9]. The present study explored the association between ICP use and patients’ experiences with the quality of chronic illness care. The findings indicate that patients with an ICP more often feel that the care they receive is patient-centred, proactive, planned, and includes collaborative goal setting, problem-solving, and follow-up support, compared with patients without an ICP. These findings are in line with results recently published by Reeves et al., showing a positive relationship between the PACIC total score and ICP use among patients with long-term conditions in the UK [27].
We conclude that ICP use among chronically ill patients within primary care in the Netherlands is low, even among diagnostic groups for which a nationwide disease-management approach was adopted. This implies that there is a gap between practice and policy aspirations to implement ICPs in primary chronic illness care.
Implications for practice and research
The present study provides evidence that, to some extent, patient characteristics relate to patients’ chances of having an ICP. The question arises as to whether ICPs should be provided to patients in less favourable (health or social) conditions only, or be employed for all chronically ill patients. Knowing that chronic illness demands a proactive approach from patients and healthcare providers to prevent or postpone complications and to maintain the best possible quality of life, it seems undesirable to make such selections based on patient characteristics. Coulter and colleagues also stress that – in contrast to other models – the care planning model encompasses all people with long-term conditions, not just those in high-risk groups [7]. Future research should gain more insight into which approach is preferable.
More knowledge is needed concerning factors that facilitate or impede the implementation of ICPs in chronic illness care, on the level of the patient but also on the level of healthcare providers and organizations (e.g. attitude, time investment, supportive environments). Moreover, while interventions to address the burden of chronic disease should be evidence-based, and use scientifically sound evaluation methods that are practicable in routine settings [28], there is still only limited evidence regarding the (cost-)effectiveness of individualized care planning. Research is urgently needed to gain insight into the (cost-)effectiveness of ICP use in various patient populations within chronic illness care. Such studies should be conducted within the complex setting of day-to-day healthcare, in order to gain a realistic view of contextual evidence [29].
Acknowledgements
The authors wish to thank all participating general practitioners and panel members with chronic diseases. This study formed part of the research programme “National Panel of people with Chronic illness or Disability” (NPCD), which is financed by the Netherlands Ministry of Health, Welfare and Sport and the Netherlands Ministry of Social Affairs and Employment.
Declaration of interest
All authors declare to have no competing interests. The authors alone are responsible for the content and writing of the paper.
References
- Department of Health High quality care for all: NHS Next Stage Review final report. London: Stationery Office; 2008. [Google Scholar]
- Bjerkan J, Richter M, Grimsmo A, Hellesø R, Brender J. Integrated care in Norway: The state of affairs years after regulation by law. Int J Integr Care 2011;11:e001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ministerie van Volksgezondheid, Welzijn en Sport Programmatische aanpak van chronische ziekten, PG/ZP 2.847.918 [Ministry of Health, Welfare and Sport. Programmatic approach to chronic conditions, PG/PZ, 2.847.918]. The Hague, Netherlands: Ministry of Health, Welfare and Sport; 2008. [Google Scholar]
- Australian Government Department of Health and Aged Care Primary care initiatives: Enhanced Primary Care package. Canberra: Australian Government Department of Health and Aged Care; 1999. [Google Scholar]
- Australian Government Department of Health Chronic disease management (formerly Enhanced Primary Care or EPC) – GP services available at: http://www.health.gov.au/internet/main/publishing.nsf/Content/mbIPRImarycare-chronicdiseasemanagement (accessed October 7, 2014). [Google Scholar]
- Russell G, Thille P, Hogg W, Lemelin J. Beyond fighting fires and chasing tails? Chronic illness care plans in Ontario, Canada. Ann Fam Med 2008;6:146–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coulter A, Roberts S, Dixon A. Delivering better services for people with long- term conditions: Building the house of care. London: King's Fund; 2013. [Google Scholar]
- Inspectie voor de Gezondheidszorg, Ministerie van Volksgezondheid, Welzijn en Sport Implementatie zorgstandaard Diabetes na vier jaar onvoldoende gevorderd [Dutch Health Care Inspectorate, Ministry of Health, Welfare and Sport. Implementation of diabetes care standard shows limited progress after four years]. Utrecht, Netherlands: Dutch Health Care Inspectorate, Ministry of Health, Welfare and Sport; 2012. [Google Scholar]
- Jansen D, Rijken M. Evaluatie DVN pilotproject rond de implementatie van de Diabetes Zorgwijzer [Evaluation DVN pilot project on the implementation of the “Zorgwijzer” Diabetes]. Utrecht, Netherlands: NIVEL; 2013. [Google Scholar]
- Van Dijk CE, Korevaar JC. Integrale bekostiging: eerste ervaringen na één jaar invoering [Bundled payment: Initial experiences after one year]. Utrecht, Netherlands: NIVEL; 2011. [Google Scholar]
- Burt J, Roland M, Paddison C, Reeves D, Campbell J, Abel G, et al. Prevalence and benefits of care plans and care planning for people with long-term conditions in England. J Health Serv Res Policy 2012;17:64–71. [DOI] [PubMed] [Google Scholar]
- Year of Care (YOC) Partnership Report of findings from the pilot programme. London: Diabetes UK; 2011. [Google Scholar]
- Walker R, Davison C, Maher AM, Law J, Reilly P, Fordjour G. Introducing personalized care planning into Newham: Outcomes of a pilot project. Diabet Med 2012;29:1074–78. [DOI] [PubMed] [Google Scholar]
- Holum LC.. “It is a good idea, but…” A qualitative study of implementation of “Individual Plan” in Norwegian mental health care. Int J Integr Care 2012;12:e15. [PMC free article] [PubMed] [Google Scholar]
- Rijken M, Van Kerkhof M, Dekker J, Schellevis FG. Comorbidity of chronic diseases: Effects of disease pairs on physical and mental functioning. Qual Life Res 2005;14:45–55. [DOI] [PubMed] [Google Scholar]
- Patient Assessment of Chronic Illness Care (PACIC) Seattle, USA: MacColl Center for Health Care Innovation, Group Health Cooperative; 2004. [Google Scholar]
- Wagner EH. Chronic disease management: What will it take to improve care for chronic illness? Eff Clin Pract 1998;1:2–4. [PubMed] [Google Scholar]
- Chew LD, Bradley KA, Boyko EJ. Brief questions to identify patients with inadequate health literacy. Family Med 2004;36:588–94. [PubMed] [Google Scholar]
- Lamberts H, Wood M. International classification of primary care. Oxford: Oxford University Press; 1987. [Google Scholar]
- Ware JE, Sherbourne CD. The MOS 36-item short form health survey (SF-36), I: Conceptual framework and item selection. Med Care 1992;30:473–83. [PubMed] [Google Scholar]
- Van der Zee K, Sanderman R, Heyink JW, De Haes H. Psychometric qualities of the RAND 36-item Health Survey 1.0: A multidimensional measure of general health status. Int J Behav Med 1996;3:104–22. [DOI] [PubMed] [Google Scholar]
- Stata [computer programme] Version 12 College Station, TX: StataCorp LP, http://www.stata.com. [Google Scholar]
- Snijders TAB, Bosker RJ. Multilevel analysis: An introduction to basic and advanced multilevel modelling. London: Sage Publications; 1999. [Google Scholar]
- Zaslavsky AM, Zaborski LB, Lin Ding MA, Shaul JA, Cioffi MJ, Cleary PD. Adjusting performance measures to ensure equitable plan comparisons. Health Care Financing Rev 2001;22:109–26. [PMC free article] [PubMed] [Google Scholar]
- Elliott MN, Swartz R, Adams J, Spritzer KL, Hays RD. Case-mix adjustment of the National CAHPS benchmarking data 1.0: A violation of model assumptions? Health Serv Res 2001;36:555–73. [PMC free article] [PubMed] [Google Scholar]
- Analysis of Diabetes Primary Care Trust Questionnaire Data 2011 In: State of the nation 2012. London: Diabetes UK; 2012. [Google Scholar]
- Reeves D, Hann M, Rick J, Rowe K, Small N, Burt J, et al. Care plans and care planning in the management of long-term conditions in the UK: A controlled prospective cohort study. Br J Gen Pract 2014:e568–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- RAND Europe DISMEVAL: Developing and validating disease management evaluation methods for European healthcare systems. Final Report. Santa Monica, CA: RAND Corporation; 2012. [Google Scholar]
- De Maeseneer JM, Van Driel ML, Green LA, Van Weel C. The need for research in primary care. Lancet 2003;362: 1314–19. [DOI] [PubMed] [Google Scholar]